815ec90d126532155f867454fdb49519.ppt
- Количество слайдов: 57
 Sleep and Pain Polly Ashworth Gloucestershire and Herefordshire Pain Management Service Gloucestershire Hospitals NHS Foundation Trust Polly. Ashworth@glos. nhs. uk
Sleep and Pain Polly Ashworth Gloucestershire and Herefordshire Pain Management Service Gloucestershire Hospitals NHS Foundation Trust Polly. Ashworth@glos. nhs. uk
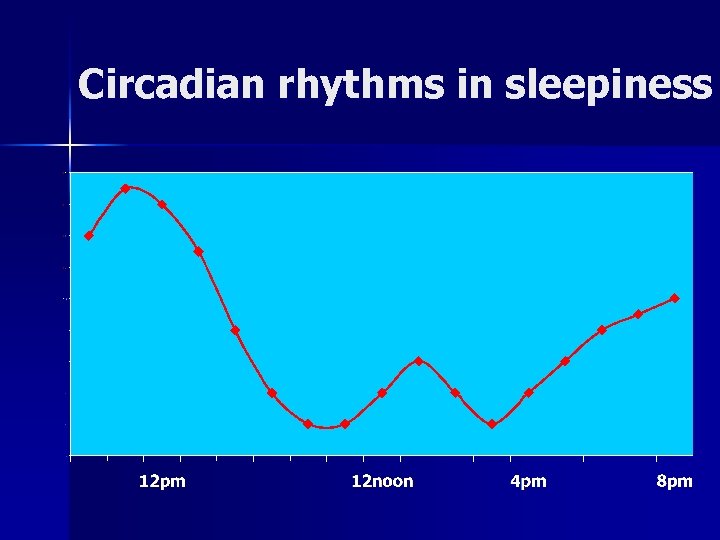 Circadian rhythms in sleepiness
Circadian rhythms in sleepiness
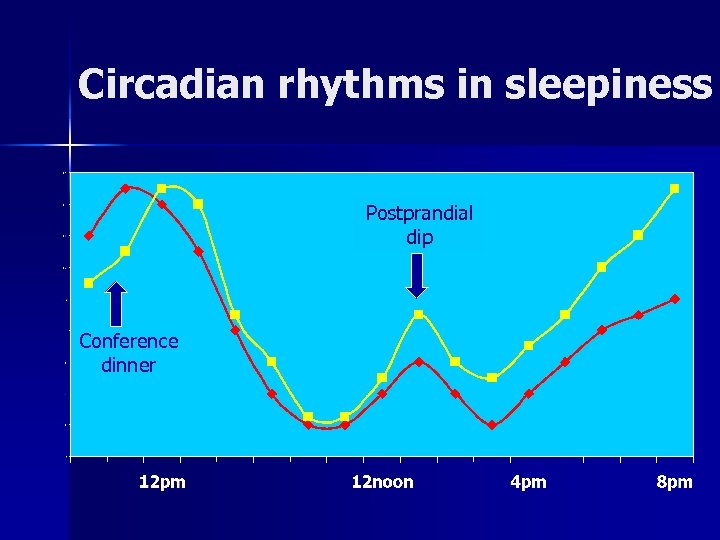 Circadian rhythms in sleepiness Postprandial dip Conference dinner
Circadian rhythms in sleepiness Postprandial dip Conference dinner
 Overview n n n “Normal” sleep and insomnia Sleep and pain Non-pharmacological treatments for insomnia in pain Other sleep disorders Implications
Overview n n n “Normal” sleep and insomnia Sleep and pain Non-pharmacological treatments for insomnia in pain Other sleep disorders Implications
 “Am I normal? ” Total sleep time Sleep onset latency – 30 mins Number/length of awakenings Sleep efficiency – 85%
“Am I normal? ” Total sleep time Sleep onset latency – 30 mins Number/length of awakenings Sleep efficiency – 85%
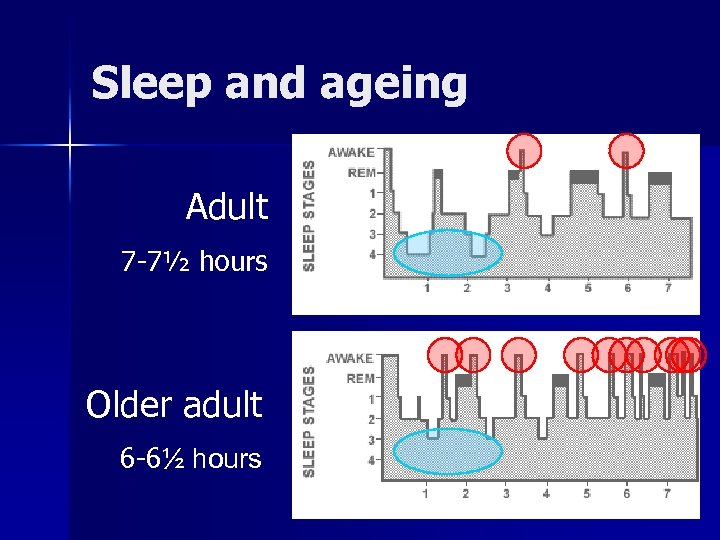 Sleep and ageing Adult 7 -7½ hours Older adult 6 -6½ hours
Sleep and ageing Adult 7 -7½ hours Older adult 6 -6½ hours
 Misperceptions of sleep Poor sleepers underestimate their sleep Retrospective estimates skewed by salience of “bad nights”
Misperceptions of sleep Poor sleepers underestimate their sleep Retrospective estimates skewed by salience of “bad nights”
 Definition of Insomnia More than 30 minutes awake at night n 3+ nights a week n 6+ months duration n Distress or daytime impairment n Non complaining short sleeper
Definition of Insomnia More than 30 minutes awake at night n 3+ nights a week n 6+ months duration n Distress or daytime impairment n Non complaining short sleeper
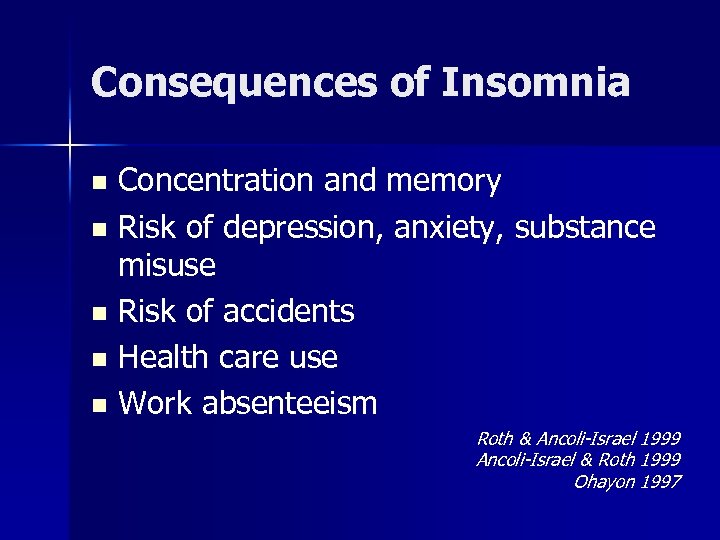 Consequences of Insomnia Concentration and memory n Risk of depression, anxiety, substance misuse n Risk of accidents n Health care use n Work absenteeism n Roth & Ancoli-Israel 1999 Ancoli-Israel & Roth 1999 Ohayon 1997
Consequences of Insomnia Concentration and memory n Risk of depression, anxiety, substance misuse n Risk of accidents n Health care use n Work absenteeism n Roth & Ancoli-Israel 1999 Ancoli-Israel & Roth 1999 Ohayon 1997
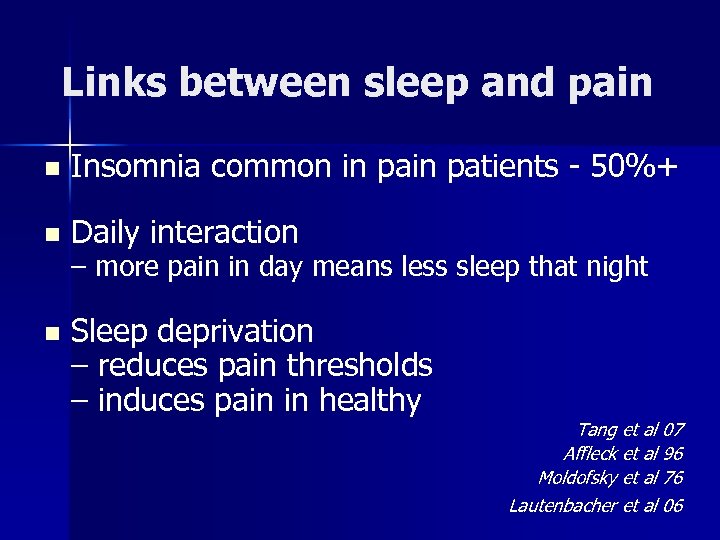 Links between sleep and pain n Insomnia common in patients - 50%+ n Daily interaction n Sleep deprivation – reduces pain thresholds – induces pain in healthy – more pain in day means less sleep that night Tang et al 07 Affleck et al 96 Moldofsky et al 76 Lautenbacher et al 06
Links between sleep and pain n Insomnia common in patients - 50%+ n Daily interaction n Sleep deprivation – reduces pain thresholds – induces pain in healthy – more pain in day means less sleep that night Tang et al 07 Affleck et al 96 Moldofsky et al 76 Lautenbacher et al 06
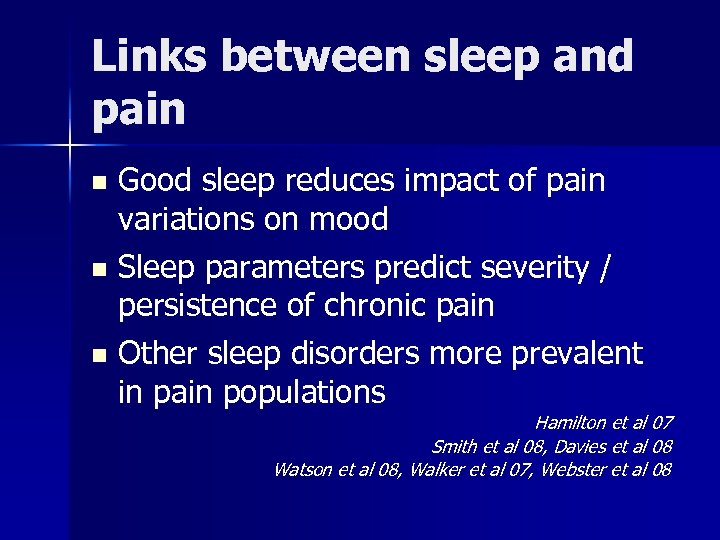 Links between sleep and pain Good sleep reduces impact of pain variations on mood n Sleep parameters predict severity / persistence of chronic pain n Other sleep disorders more prevalent in pain populations n Hamilton et al 07 Smith et al 08, Davies et al 08 Watson et al 08, Walker et al 07, Webster et al 08
Links between sleep and pain Good sleep reduces impact of pain variations on mood n Sleep parameters predict severity / persistence of chronic pain n Other sleep disorders more prevalent in pain populations n Hamilton et al 07 Smith et al 08, Davies et al 08 Watson et al 08, Walker et al 07, Webster et al 08
 Patients’ perspective
Patients’ perspective
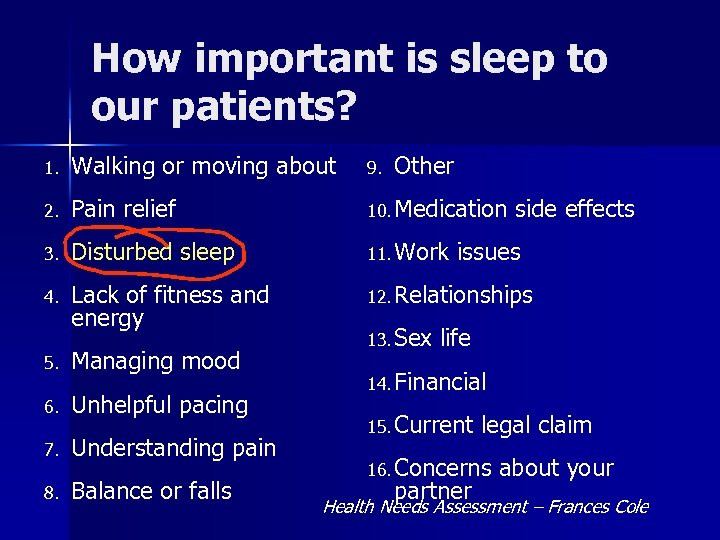 How important is sleep to our patients? 1. Walking or moving about 9. 2. Pain relief 10. Medication 3. Disturbed sleep 11. Work 4. Lack of fitness and energy 12. Relationships 5. Managing mood 6. Unhelpful pacing 7. Understanding pain 8. Balance or falls Other 13. Sex side effects issues life 14. Financial 15. Current legal claim 16. Concerns partner about your Health Needs Assessment – Frances Cole
How important is sleep to our patients? 1. Walking or moving about 9. 2. Pain relief 10. Medication 3. Disturbed sleep 11. Work 4. Lack of fitness and energy 12. Relationships 5. Managing mood 6. Unhelpful pacing 7. Understanding pain 8. Balance or falls Other 13. Sex side effects issues life 14. Financial 15. Current legal claim 16. Concerns partner about your Health Needs Assessment – Frances Cole
 Patients’ experience of sleep and pain “It’s my pain that wakes me up” “I just can’t get comfortable” Pain “Unless my pain improves I’ll never get a decent night’s sleep” Sleep disturbance
Patients’ experience of sleep and pain “It’s my pain that wakes me up” “I just can’t get comfortable” Pain “Unless my pain improves I’ll never get a decent night’s sleep” Sleep disturbance
 Sleep in patients
Sleep in patients
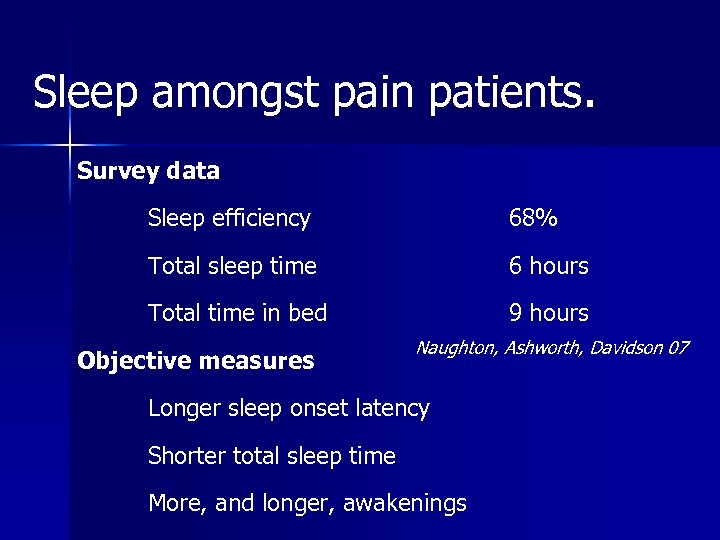 Sleep amongst pain patients. Survey data Sleep efficiency 68% Total sleep time 6 hours Total time in bed 9 hours Objective measures Naughton, Ashworth, Davidson 07 Longer sleep onset latency Shorter total sleep time More, and longer, awakenings
Sleep amongst pain patients. Survey data Sleep efficiency 68% Total sleep time 6 hours Total time in bed 9 hours Objective measures Naughton, Ashworth, Davidson 07 Longer sleep onset latency Shorter total sleep time More, and longer, awakenings
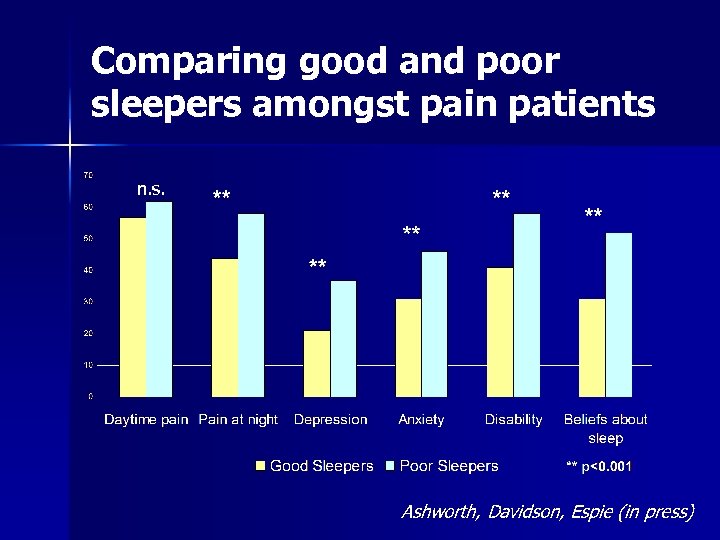 Comparing good and poor sleepers amongst pain patients n. s. Ashworth, Davidson, Espie (in press)
Comparing good and poor sleepers amongst pain patients n. s. Ashworth, Davidson, Espie (in press)
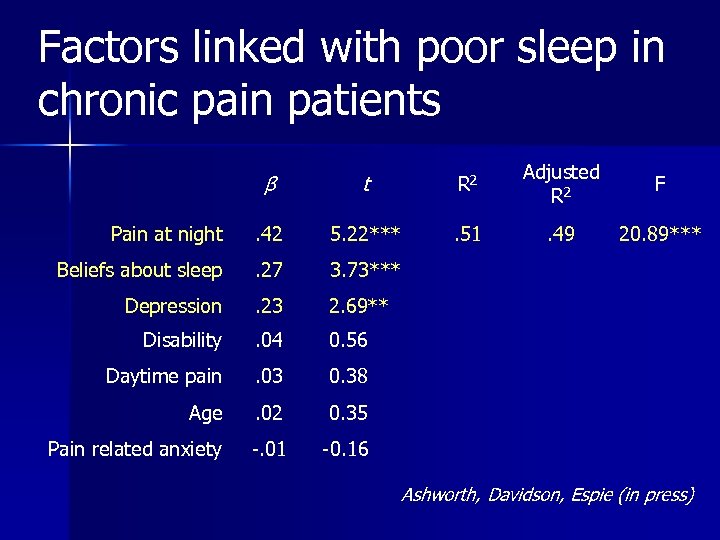 Factors linked with poor sleep in chronic pain patients β t R 2 Adjusted R 2 F Pain at night . 42 5. 22*** . 51 . 49 20. 89*** Beliefs about sleep . 27 3. 73*** Depression . 23 2. 69** Disability . 04 0. 56 Daytime pain . 03 0. 38 Age . 02 0. 35 Pain related anxiety -. 01 -0. 16 Ashworth, Davidson, Espie (in press)
Factors linked with poor sleep in chronic pain patients β t R 2 Adjusted R 2 F Pain at night . 42 5. 22*** . 51 . 49 20. 89*** Beliefs about sleep . 27 3. 73*** Depression . 23 2. 69** Disability . 04 0. 56 Daytime pain . 03 0. 38 Age . 02 0. 35 Pain related anxiety -. 01 -0. 16 Ashworth, Davidson, Espie (in press)
 Pain and Sleep Pain Sleep disturbance
Pain and Sleep Pain Sleep disturbance
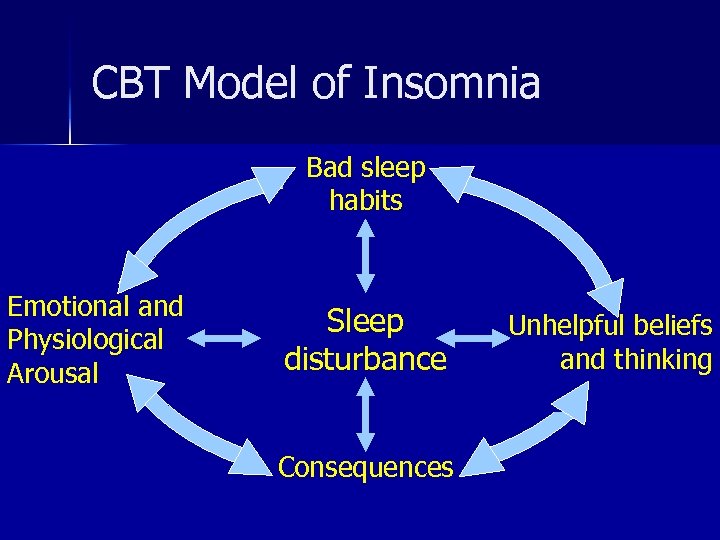 CBT Model of Insomnia Bad sleep habits Emotional and Physiological Arousal Sleep disturbance Consequences Unhelpful beliefs and thinking
CBT Model of Insomnia Bad sleep habits Emotional and Physiological Arousal Sleep disturbance Consequences Unhelpful beliefs and thinking
 How can we help?
How can we help?
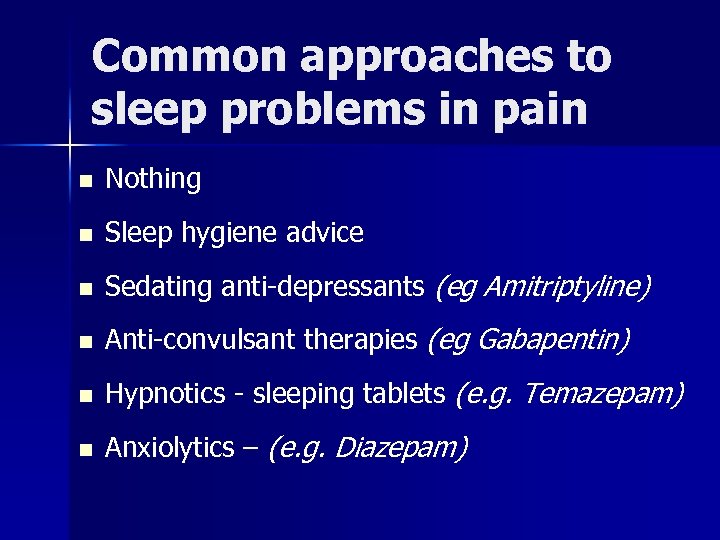 Common approaches to sleep problems in pain n Nothing n Sleep hygiene advice n Sedating anti-depressants (eg Amitriptyline) n Anti-convulsant therapies (eg Gabapentin) n Hypnotics - sleeping tablets (e. g. Temazepam) n Anxiolytics – (e. g. Diazepam)
Common approaches to sleep problems in pain n Nothing n Sleep hygiene advice n Sedating anti-depressants (eg Amitriptyline) n Anti-convulsant therapies (eg Gabapentin) n Hypnotics - sleeping tablets (e. g. Temazepam) n Anxiolytics – (e. g. Diazepam)
 CBT for insomnia – what is it? – does it work if you have pain?
CBT for insomnia – what is it? – does it work if you have pain?
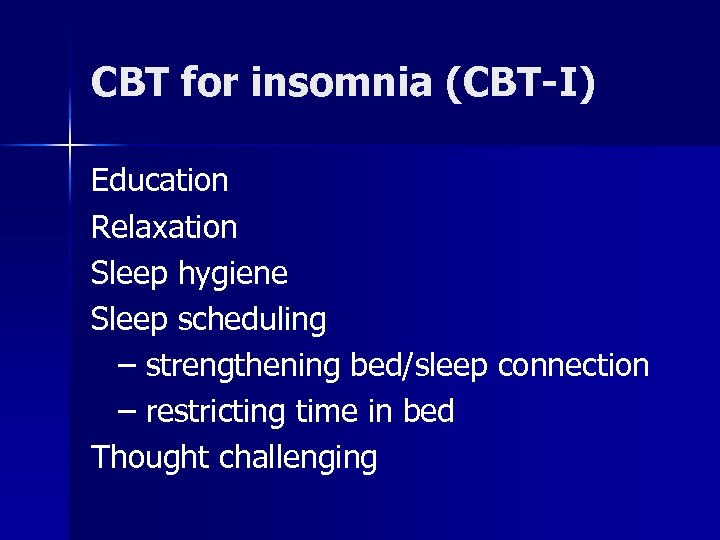 CBT for insomnia (CBT-I) Education Relaxation Sleep hygiene Sleep scheduling – strengthening bed/sleep connection – restricting time in bed Thought challenging
CBT for insomnia (CBT-I) Education Relaxation Sleep hygiene Sleep scheduling – strengthening bed/sleep connection – restricting time in bed Thought challenging
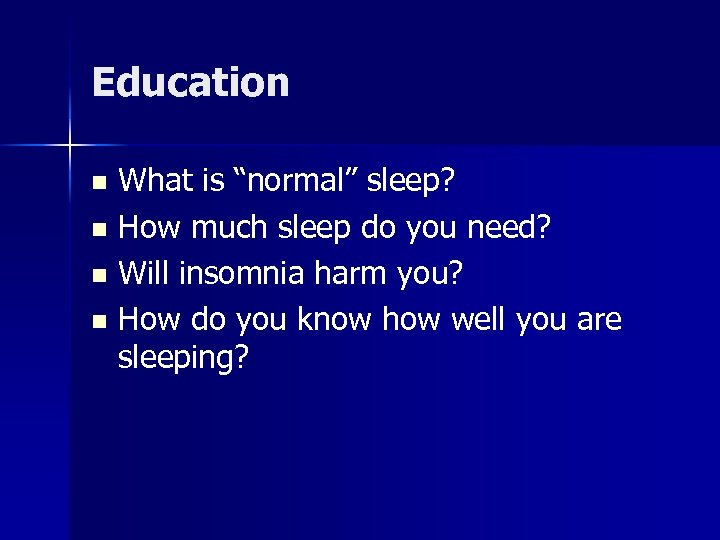 Education What is “normal” sleep? n How much sleep do you need? n Will insomnia harm you? n How do you know how well you are sleeping? n
Education What is “normal” sleep? n How much sleep do you need? n Will insomnia harm you? n How do you know how well you are sleeping? n
 Sleep hygiene n n n Coffee Cigarettes Alcohol Eating Exercise Bedroom Noise/ Temperature/Light n n Alarm clock Mobile Phone
Sleep hygiene n n n Coffee Cigarettes Alcohol Eating Exercise Bedroom Noise/ Temperature/Light n n Alarm clock Mobile Phone
 Sleep scheduling 1 Strengthen the bed/sleep connection n Don’t spend time in bed watching TV, eating etc n Wind down routine (90 minutes) n Go to bed at night only when you are sleepy n If you are not asleep after 20 minutes get up n Get up at the same time each morning n Avoid naps if you can
Sleep scheduling 1 Strengthen the bed/sleep connection n Don’t spend time in bed watching TV, eating etc n Wind down routine (90 minutes) n Go to bed at night only when you are sleepy n If you are not asleep after 20 minutes get up n Get up at the same time each morning n Avoid naps if you can
 Sleep scheduling 2 Restricting time in bed n Find out average sleep time from sleep diary n Agree a sleep “window” of this average length (but not less than 6 -7 hours) n Anchor sleep around regular get up time n Threshold time set for going to bed n When sleep efficiency reaches 90% sleep window increased by 15 mins
Sleep scheduling 2 Restricting time in bed n Find out average sleep time from sleep diary n Agree a sleep “window” of this average length (but not less than 6 -7 hours) n Anchor sleep around regular get up time n Threshold time set for going to bed n When sleep efficiency reaches 90% sleep window increased by 15 mins
 Sleep scheduling example Average sleep time = 7 hours …but time in bed = 10. 5 hours Set sleep window = 7 hours Anchor get up time at 7 am Threshold for going to bed = midnight
Sleep scheduling example Average sleep time = 7 hours …but time in bed = 10. 5 hours Set sleep window = 7 hours Anchor get up time at 7 am Threshold for going to bed = midnight
 Cognitive therapy n n n Challenging dysfunctional beliefs and thoughts about sleep Techniques for “racing mind” Imagery relaxation Putting the day to rest Give up trying
Cognitive therapy n n n Challenging dysfunctional beliefs and thoughts about sleep Techniques for “racing mind” Imagery relaxation Putting the day to rest Give up trying
 3 key messages n Reduce n If time in bed you can’t sleep, get up n Don’t lose sleep over losing sleep
3 key messages n Reduce n If time in bed you can’t sleep, get up n Don’t lose sleep over losing sleep
 Does CBT improve sleep even if you have pain?
Does CBT improve sleep even if you have pain?
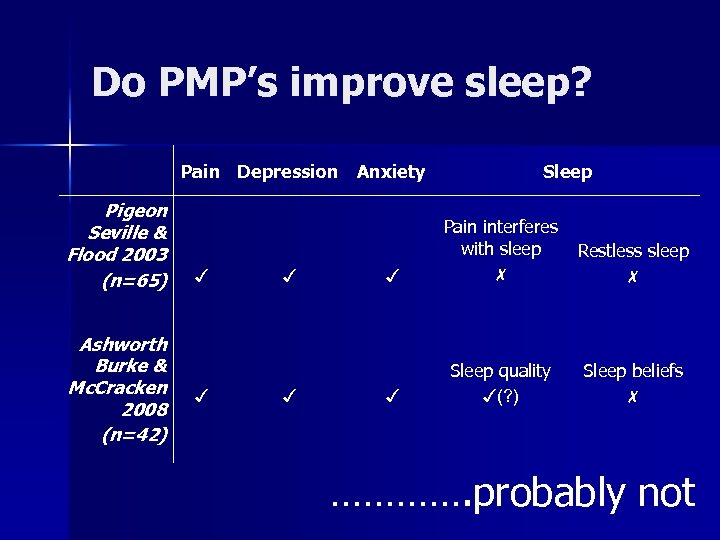 Do PMP’s improve sleep? Pain Depression Pigeon Seville & Flood 2003 (n=65) Ashworth Burke & Mc. Cracken 2008 (n=42) ✓ ✓ Anxiety Sleep ✓ Pain interferes with sleep ✗ Restless sleep ✗ ✓ Sleep quality ✓(? ) Sleep beliefs ✗ …………. probably not
Do PMP’s improve sleep? Pain Depression Pigeon Seville & Flood 2003 (n=65) Ashworth Burke & Mc. Cracken 2008 (n=42) ✓ ✓ Anxiety Sleep ✓ Pain interferes with sleep ✗ Restless sleep ✗ ✓ Sleep quality ✓(? ) Sleep beliefs ✗ …………. probably not
 Does CBT-I work for insomnia if you have pain? Currie et al (2000) n N=60 Benign pain of musculoskeletal origin, but fibromyalgia, and insomnia n Already treated in pain service n 7 x 2½ hour group sessions CBT-I n Baseline sleep efficiency 70%, TST 6 h
Does CBT-I work for insomnia if you have pain? Currie et al (2000) n N=60 Benign pain of musculoskeletal origin, but fibromyalgia, and insomnia n Already treated in pain service n 7 x 2½ hour group sessions CBT-I n Baseline sleep efficiency 70%, TST 6 h
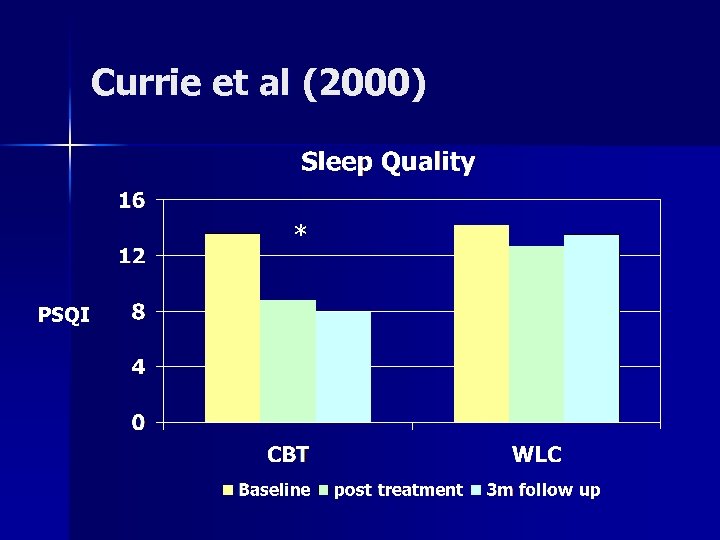 Currie et al (2000) * PSQI
Currie et al (2000) * PSQI
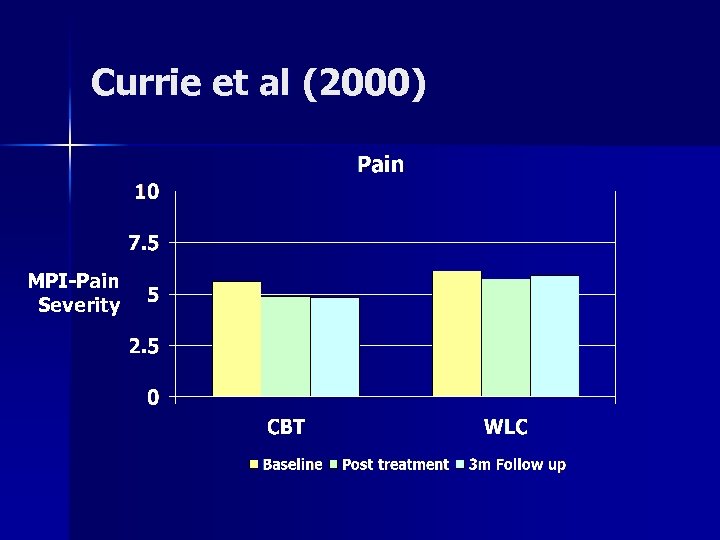 Currie et al (2000) MPI-Pain Severity
Currie et al (2000) MPI-Pain Severity
 Does CBT-I work for insomnia if you have pain? Edinger et al (2005) n n=47 Fibromyalgia and insomnia n Recruited by newspaper advert n Randomised to CBT, Sleep Hygiene, WLC n 6 sessions delivered 1: 1 n Baseline sleep efficiency 80%, TST 7 h
Does CBT-I work for insomnia if you have pain? Edinger et al (2005) n n=47 Fibromyalgia and insomnia n Recruited by newspaper advert n Randomised to CBT, Sleep Hygiene, WLC n 6 sessions delivered 1: 1 n Baseline sleep efficiency 80%, TST 7 h
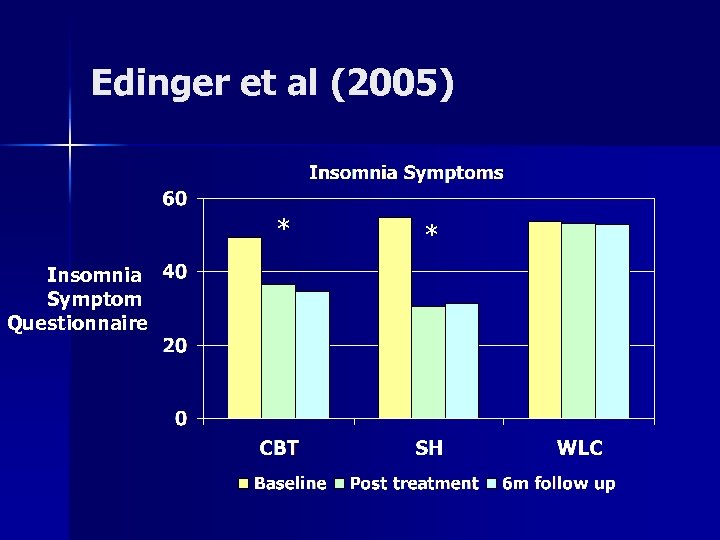 Edinger et al (2005) * Insomnia Symptom Questionnaire *
Edinger et al (2005) * Insomnia Symptom Questionnaire *
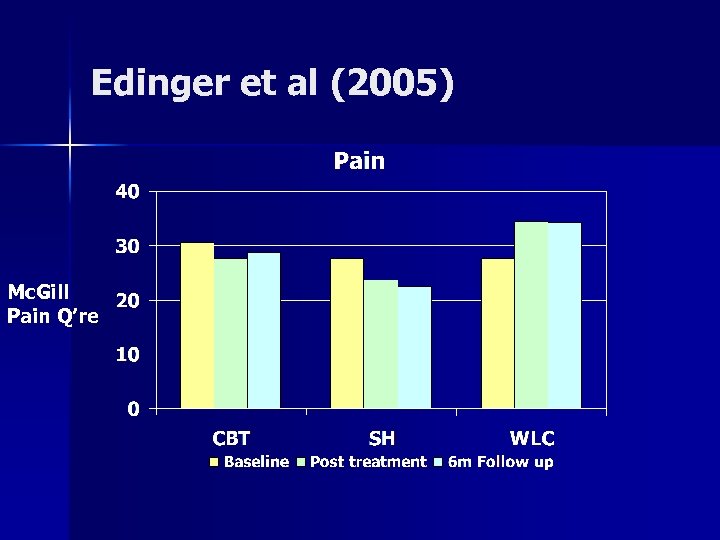 Edinger et al (2005) Mc. Gill Pain Q’re
Edinger et al (2005) Mc. Gill Pain Q’re
 …but we can’t do that….
…but we can’t do that….
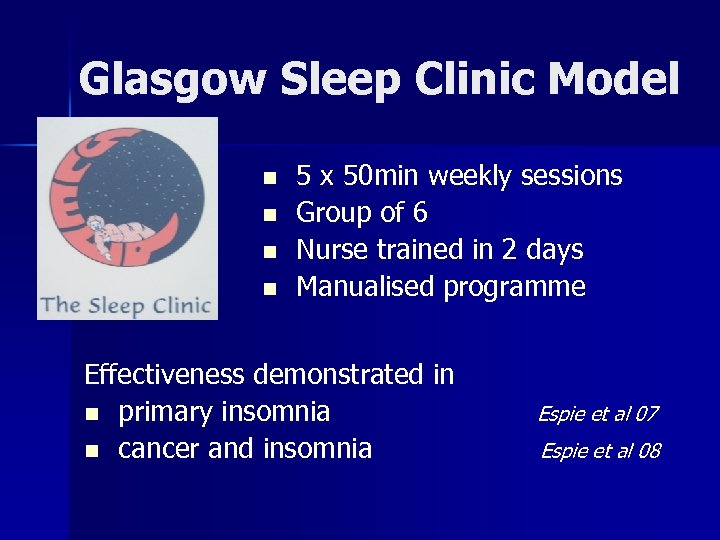 Glasgow Sleep Clinic Model n n 5 x 50 min weekly sessions Group of 6 Nurse trained in 2 days Manualised programme Effectiveness demonstrated in n primary insomnia n cancer and insomnia Espie et al 07 Espie et al 08
Glasgow Sleep Clinic Model n n 5 x 50 min weekly sessions Group of 6 Nurse trained in 2 days Manualised programme Effectiveness demonstrated in n primary insomnia n cancer and insomnia Espie et al 07 Espie et al 08
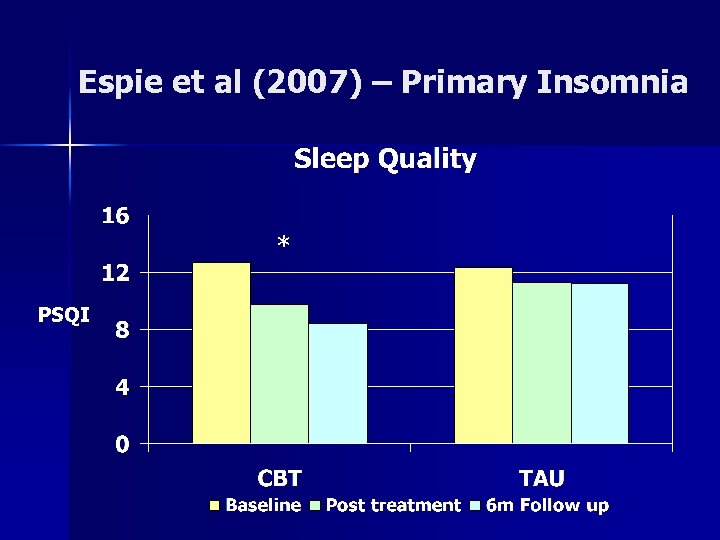 Espie et al (2007) – Primary Insomnia * PSQI
Espie et al (2007) – Primary Insomnia * PSQI
 Other sleep disorders
Other sleep disorders
 Sleep apnoea Features n Excessive daytime sleepiness n Impaired concentration n Snoring (but not always) Links: FMS? Opiate use (75% vs 3% gen pop)
Sleep apnoea Features n Excessive daytime sleepiness n Impaired concentration n Snoring (but not always) Links: FMS? Opiate use (75% vs 3% gen pop)
 Sleep Apnoea • Sleep on your side • Avoid alcohol • Lose weight • Medication review • Continuous Positive Airway Pressure Machine (CPAP)
Sleep Apnoea • Sleep on your side • Avoid alcohol • Lose weight • Medication review • Continuous Positive Airway Pressure Machine (CPAP)
 Restless legs n Uncomfortable sensation and urge to move legs n Worse with rest Immediate and complete relief on movement Worse in evening/early night n More common in people with pain n n (33% FMS vs 3%, Watson et al 08) n May be exacerbated by pain, poor sleep, some medications, or low iron
Restless legs n Uncomfortable sensation and urge to move legs n Worse with rest Immediate and complete relief on movement Worse in evening/early night n More common in people with pain n n (33% FMS vs 3%, Watson et al 08) n May be exacerbated by pain, poor sleep, some medications, or low iron
 Restless Legs Check iron levels n Review medication n General sleep hygiene, exercise, hot bath n Pharmacological therapies n
Restless Legs Check iron levels n Review medication n General sleep hygiene, exercise, hot bath n Pharmacological therapies n
 Conclusions
Conclusions
 Conclusions n Sleep disturbance is important n It’s not just caused by the pain n Cognitive therapy for insomnia works, even if you have pain too n Watch out for other sleep disorders
Conclusions n Sleep disturbance is important n It’s not just caused by the pain n Cognitive therapy for insomnia works, even if you have pain too n Watch out for other sleep disorders
 Implications
Implications
 What can you do next week? 1. Don’t give up on asking about sleep 2. Add to your sleep hygiene advice 3. Recommend CBT-I to people with insomnia and pain 4. Look for other sleep disorders as well as insomnia
What can you do next week? 1. Don’t give up on asking about sleep 2. Add to your sleep hygiene advice 3. Recommend CBT-I to people with insomnia and pain 4. Look for other sleep disorders as well as insomnia
 Useful materials Measures: Pittsburgh Sleep Quality Index Insomnia Symptom Questionnaire Dysfunctional Beliefs About Sleep Scale Epworth Sleepiness Scale Guidelines and patient information leaflets: American Academy of Sleep Medicine www. aasm. org
Useful materials Measures: Pittsburgh Sleep Quality Index Insomnia Symptom Questionnaire Dysfunctional Beliefs About Sleep Scale Epworth Sleepiness Scale Guidelines and patient information leaflets: American Academy of Sleep Medicine www. aasm. org
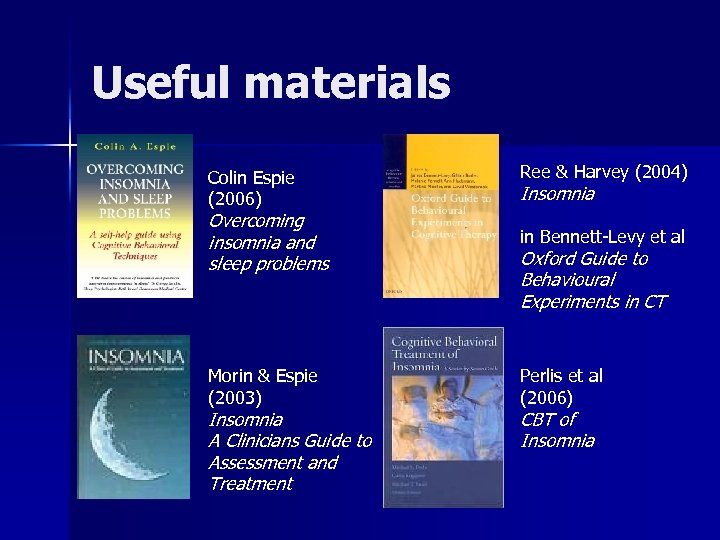 Useful materials Colin Espie (2006) Ree & Harvey (2004) Insomnia Overcoming insomnia and sleep problems in Bennett-Levy et al Morin & Espie (2003) Perlis et al (2006) Insomnia A Clinicians Guide to Assessment and Treatment Oxford Guide to Behavioural Experiments in CT CBT of Insomnia
Useful materials Colin Espie (2006) Ree & Harvey (2004) Insomnia Overcoming insomnia and sleep problems in Bennett-Levy et al Morin & Espie (2003) Perlis et al (2006) Insomnia A Clinicians Guide to Assessment and Treatment Oxford Guide to Behavioural Experiments in CT CBT of Insomnia
 Polly. Ashworth@glos. nhs. uk
Polly. Ashworth@glos. nhs. uk

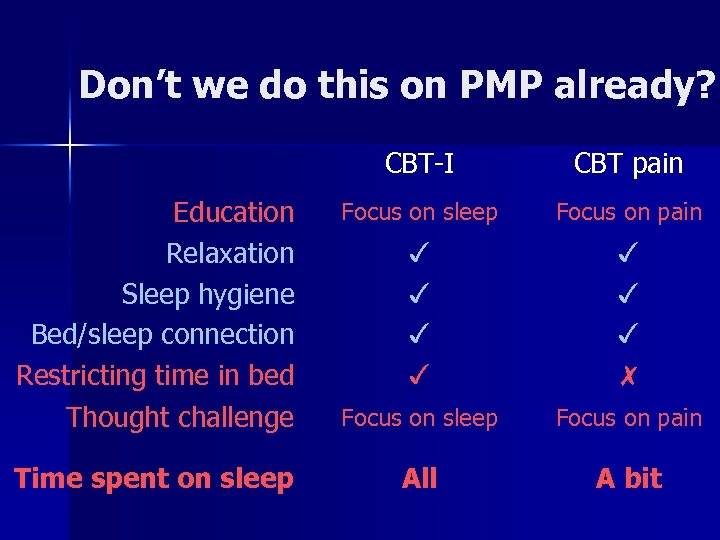 Don’t we do this on PMP already? CBT-I CBT pain Education Relaxation Sleep hygiene Bed/sleep connection Restricting time in bed Thought challenge Focus on sleep Focus on pain ✓ ✓ ✓ ✓ ✗ Focus on sleep Focus on pain Time spent on sleep All A bit
Don’t we do this on PMP already? CBT-I CBT pain Education Relaxation Sleep hygiene Bed/sleep connection Restricting time in bed Thought challenge Focus on sleep Focus on pain ✓ ✓ ✓ ✓ ✗ Focus on sleep Focus on pain Time spent on sleep All A bit


