d017b412932d41f9d9a213814babf01d.ppt
- Количество слайдов: 57

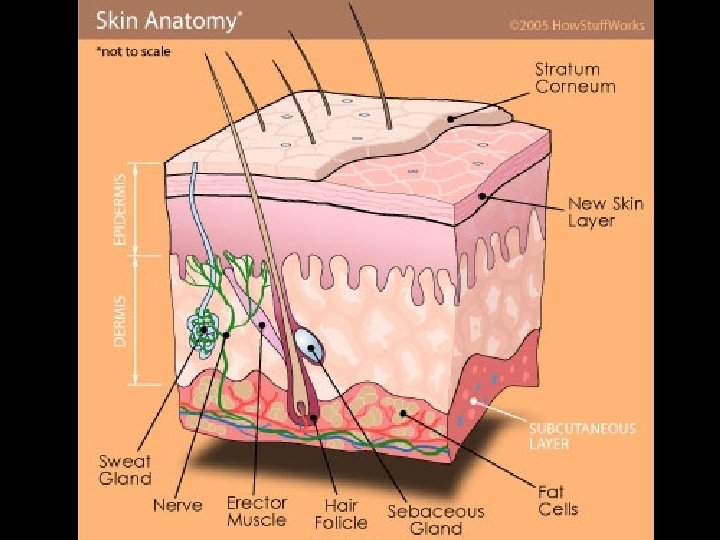
• Skin weighs 9 -11 lbs. and accounts for ~7% of total body weight in the avg. adult. • It is composed of two principle layers: epidermis and dermis. • The epidermis, composed of epithelial cells, is the outermost protective shield of the body. • The dermis layer is composed of fibrous connective tissue, and is the only layer that is vascularized. • The subcutaneous tissue just deep to these layers is called the hypodermis.
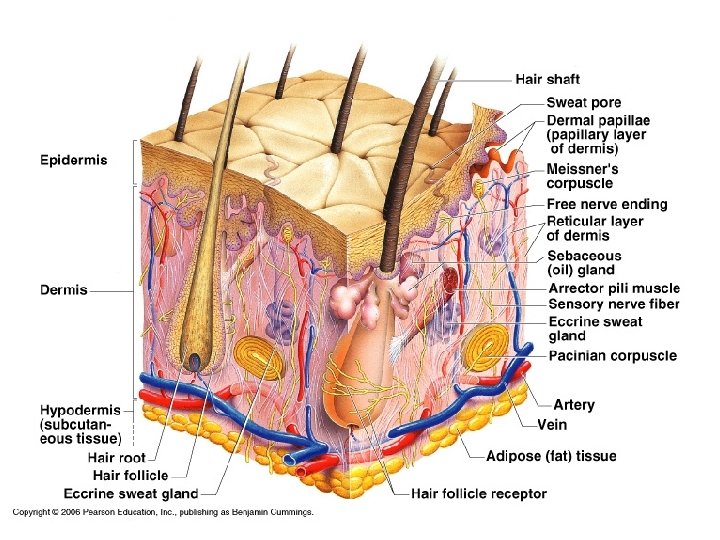
• The hypodermis, also called superficial fascia, because it is superficial to the tough connective tissue wrapping (fascia) of the skeletal muscles, consists of mostly adipose tissue. • It anchors the skin to the underlying structures (mostly to muscles), but loosely enough that the skin can slide rather freely over those structures. • It also acts as a shock absorber and an insulator that prevents heat loss from the body. • It thickens in females around thighs, hips; in males, around the abdomen.
• Structurally the epidermis is a keratinized stratified squamous epithelium consisting of 4 distinct cell types and 4 -5 distinct layers. • The cells of this layer include: keratinocytes, melanocytes, Merkel cells, and Lanerhans’ cells. • Most epidermal cells are keratinocytes, cells that produce keratin, a protein that helps give the epidermis its protective properties. • Tightly connected to one another by desmosomes, the keratinocytes arise in the deepest part of the epidermis from the stratum basale layer and undergo continuous mitosis.
• By the time these cells reach the free surface of the skin, they are dead, scalelike structures. • Millions of these dead cells rub off every day, giving us a totally new epidermis every 4 -6 weeks. • In body areas regularly subjected to friction, such as the hands and feet, both cell production and keratin formation are accelerated. Persistent friction (from a poorly fitting shoe) causes a thickening of the epidermis called a callus. • Merkel cells are associated with a disclike sensory nerve ending; the combo functions as a sensory receptor for touch.
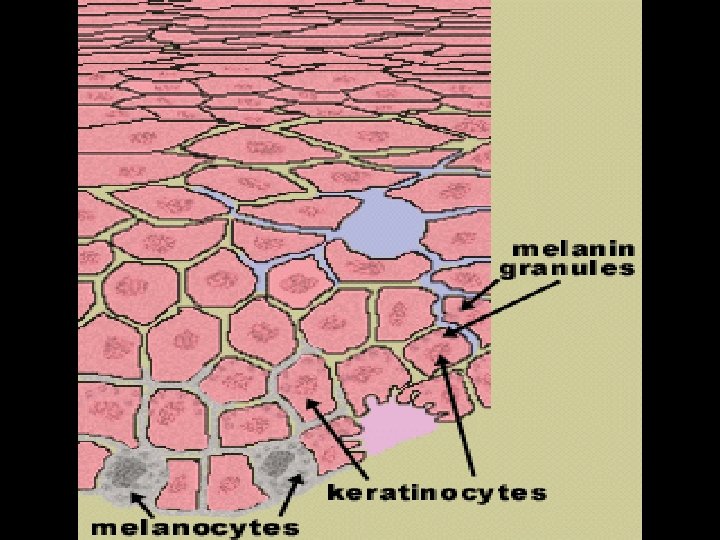
• Melanocytes, epithelial cells that make the pigment melanin, are found in the deepest layer of the epidermis. • The melanin accumulate on the superficial side of the keratinocyte nucleus, forming a pigment shield that protects the nucleus from UV radiation in sunlight. • Star-shaped Langerhans’ cells arise from bone marrow and migrate to the epidermis. • These cells are macrophages that help activate our immune system.
• Variation in epidermal thickness determines if skin is thick or thin. • In thick skin, which covers palms and soles of the feet, the epidermis consists of five layers, or strata. • From deep to superficial these layers are: stratum basale, spinosum, granulosum, lucidum, and corneum. • In thin skin, which covers the rest of the body, the stratum lucidum is absent and the other strata are thinner.
• This is the deepest epidermal layer and is attached to the underlying dermis along a wavy borderline. • It consists of a single row of cells, the youngest keratinocytes. • 10 -25% of the cells in the stratum basale are melanocytes, and their branching processes extend among the surrounding cells into the next layer. • Several layers thick; contains intermediate filaments made of pre-keratin. • Scattered among the keratinocytes are melanin granules and Langerhans’ cells, which are most abundant in this layer.
• 3 -5 cell layers; keratinocytes flatten, their nuclei and organelles begin to disintegrate. • This layer accumulates keratohyaline and lamellated granules. • The keratohyalin granules help to form keratin in the upper layers. The lamellated granules contain a waterproofing glycolipid that slows water loss across the epidermis. • The epidermis relies on capillaries for its nutrients. Above the stratum granulosum, the cells are too far from the dermal capillaries, so they die.
• Appears as a thin translucent band just above the stratum granulosum. • Consists of a few rows of clear, flat, dead keratinoctyes. • 20 -30 layers thick; keratin and the thickened plasma membranes of cells in this stratum protect the skin against abrasion. • Protects deeper cells from water loss. • Avg person sheds 40 lbs of these skin cells in a lifetime.
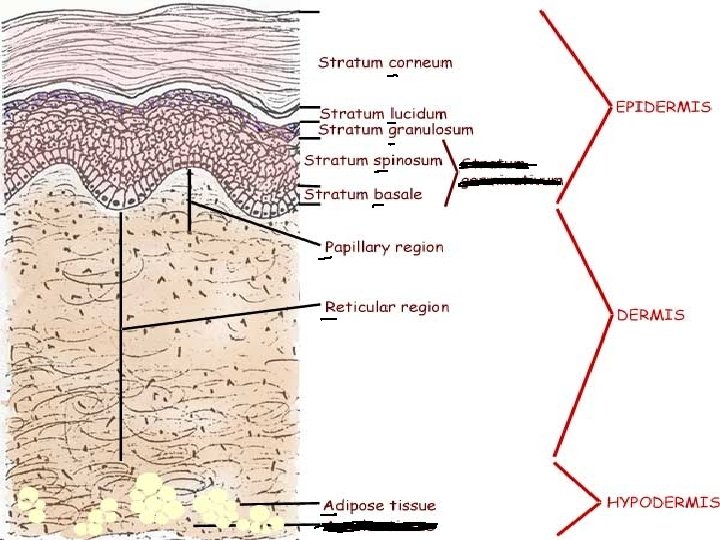
• Its cells are typical of those found in any connective tissue proper: fibroblasts, macrophages, mast cells, and white blood cells. • Heavily embedded with collagen and elastin fibers. • The dermis is richly supplied with nerve fibers, blood vessels, and lymphatic vessels. The major portions of hair follicles, as well as oil and sweat glands, reside in the dermis. • The dermis has two layers: papillary and reticular.
• The thin superficial papillary layer is areolar conn tissue in which the collagen and elastin fibers form a loosely woven mat that is heavily invested with blood vessels. • Its superior surface is called dermal papillae that indent the overlying epidermis. • Many dermal papillae contain capillary loops; others house free nerve endings (pain receptors) and touch receptors called Meissner’s corpuscles. • Epidermal ridges increase friction and enhance the gripping ability; they are genetically unique.
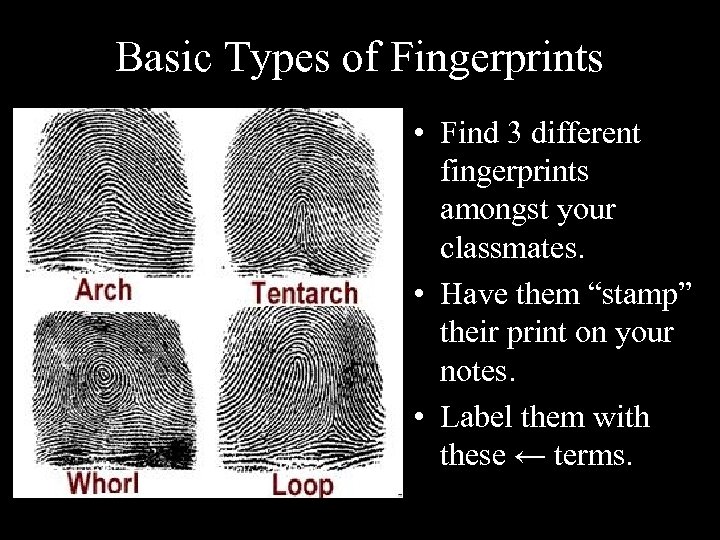
Basic Types of Fingerprints • Find 3 different fingerprints amongst your classmates. • Have them “stamp” their print on your notes. • Label them with these ← terms.
• The deeper reticular layer, 80% of the dermis, is dense irregular connective tissue. • Thick bundles of collagen fibers run in various planes; however, most run parallel to the skin surface. • Separations, or less dense regions, between these bundles form cleavage, or tension, lines in the skin. These externally invisible lines tend to run longitudinally in the skin of the head and limbs and in circular patterns around the neck and trunk.
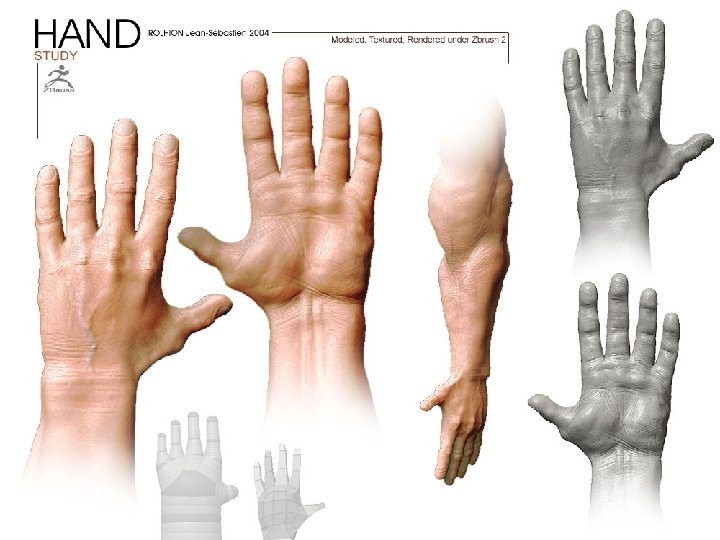
• Cleavage lines are imp. to both surgeons and their patients. When an incision is made parallel to these lines, the skin gapes less and heals faster. • The collagen fibers of the dermis give skin strength and resiliency that prevent most jabs and scrapes from penetrating the dermis. In addition, collagen binds to water keeping the skin hydrated. Elastin fibers provide the stretch-recoil properties of skin. • Flexure lines are dermal folds that occur at or near joints like the wrists, fingers, soles, and toes. They are deep skin creases.
• Three pigments contribute to skin color: melanin, carotene, and hemoglobin. Of these only melanin is made in the skin. • Melanin ranges in color from yellow to reddishbrown to black. Its synthesis depends on an enzyme in melanocytes called tyrosinase. • Melanocytes of black- and brown-skinned people produce many more and darker melanin granules than fair-skinned people. • Prolonged sun exposure causes a substantial melanin buildup, which helps protect the DNA of skin cells from UV radiation by absorbing the light.
• Carotene is a yellow-orange pigment found in certain plant products (carrots). • It tends to accumulate in the stratum corneum and in fatty tissue of the hypodermis. Its color is most obvious in the palms and soles, where the stratum corneum is thickest. • The pinkish hue of fair skin reflects the crimson color of oxygenated hemoglobin in the red blood cells circulating through the dermal capillaries.
Got Carrots?

• Derivatives of the epidermis called skin appendages include: nails, sweat glands, sebaceous (oil) glands, hair follicles, and hair. • Aka sudoriferous glands, sweat glands are distributed over the entire skin surface—about 2. 5 million glands person. • Merocrine sweat glands are more numerous; each is a simple tubular gland. (Ex: palm, forehead) • The secretory part lies in the dermis; the duct extends to open in a pore.
• Merocrine gland secretion, called sweat, is a hypotonic filtrate of blood and is released by exocytosis. It is 99% water, with some salts, microbe-killing substance called dermicidin, and traces of wastes like urea and ammonia. • Its major role—prevent overheating of the body. • Heat-induced sweating begins on the forehead and then spreads inferiorly over the remainder of the body. • Emotionally induced sweating (embarassment, nervousness) begins on the palms, soles, and armpits and then spreads to other body areas.
• Ceruminous (wax) glands are found in the lining of the external ear canal. • They secret a sticky substance called cerumen, or earwax, that is thought to deter insects and block entry of foreign material. • Mammary glands, another variety of specialized sweat glands, secrete milk. • These are simple alveolar glands that are found all over the body except on the palms and soles. They are small on the trunk and limbs, but large on the face, neck, and upper chest.
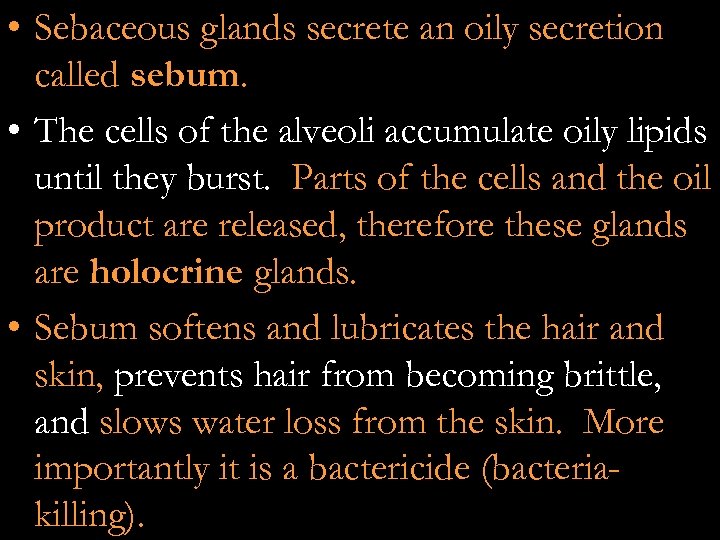
• Sebaceous glands secrete an oily secretion called sebum. • The cells of the alveoli accumulate oily lipids until they burst. Parts of the cells and the oil product are released, therefore these glands are holocrine glands. • Sebum softens and lubricates the hair and skin, prevents hair from becoming brittle, and slows water loss from the skin. More importantly it is a bactericide (bacteriakilling).

• http: //www. youtube. com/watch? v=a. W K 6 q. JFv. Wo. M&list=PLX 4 Rc 6 WZUBx. PF BYv 2 KPj 2 j. V 0 n. A 3 UZM 2 D 5#
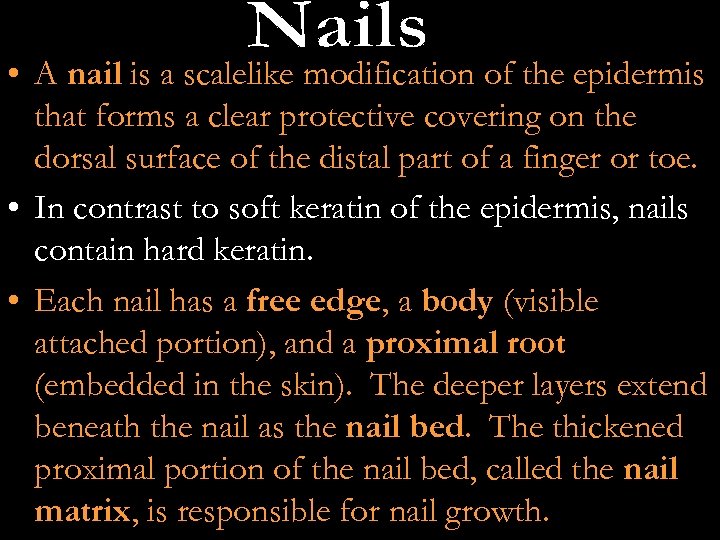
• A nail is a scalelike modification of the epidermis that forms a clear protective covering on the dorsal surface of the distal part of a finger or toe. • In contrast to soft keratin of the epidermis, nails contain hard keratin. • Each nail has a free edge, a body (visible attached portion), and a proximal root (embedded in the skin). The deeper layers extend beneath the nail as the nail bed. The thickened proximal portion of the nail bed, called the nail matrix, is responsible for nail growth.
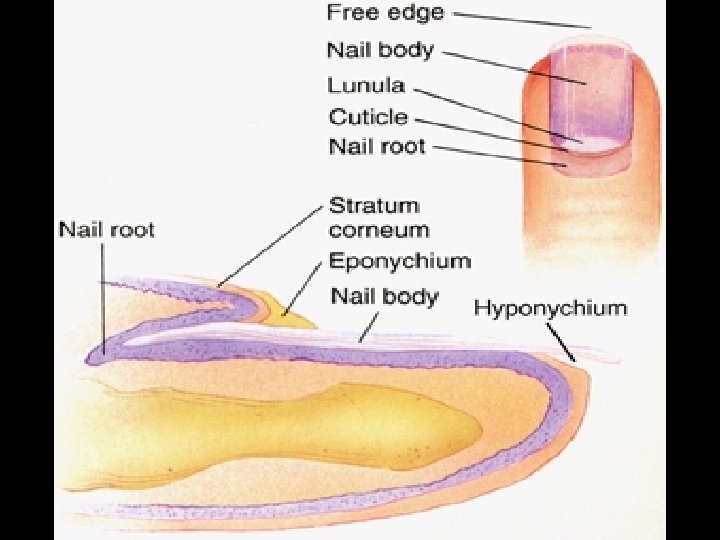
• Nails appear pink because of the rich bed of capillaries in the underlying dermis. • The region that lies over the thick nail matrix appears as a white crescent called the lunula. • The proximal and lateral borders of the nail are overlapped by skin folds called nail folds. • The proximal nail fold projects onto the nail body as the cuticle. • The region beneath the free edge of the nail where dirt and debris tend to accumulate is the hyponychium (the quick).
• Hairs are flexible strands produced by hair follicles that consist of dead, keratinized cells. • The hard keratin that dominates hairs and nails has two advantages over soft keratin: – 1. Tougher and more durable – 2. Individual cells do not flake off. • The chief regions of a hair are the shaft, which projects from the skin, and the root, the part embedded in the skin. • If the shaft is flat the hair is kinked; oval, the hair is silky & wavy; round the hair is straight & coarse.
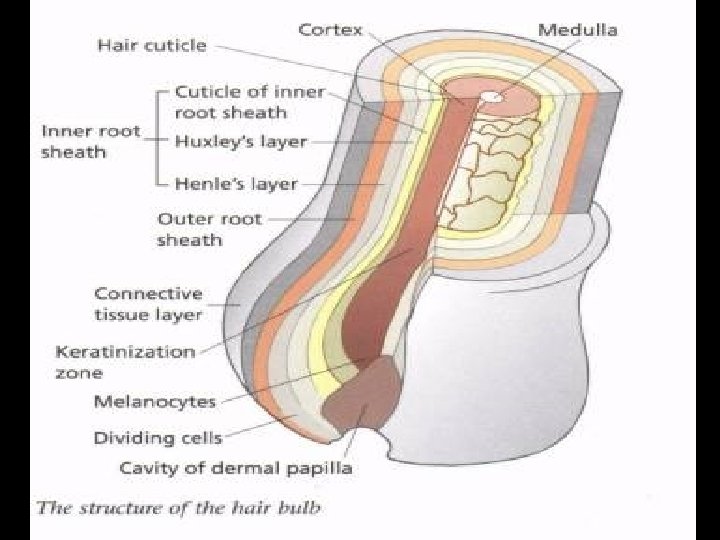
• A hair has 3 concentric layers of keratinized cells. • Its central core, the medulla, consists of large cells and air spaces (absent in fine hairs). • The cortex, a bulky layer surrounding the medulla, consists of several layers of flat cells. • The outermost cuticle is formed from a single layer of cells that overlap one another (like shingles). This arrangement keeps neighboring hairs apart so they don’t mat. • Hair pigment is made by melanocytes at the base of the hair follicle and transferred to the cortical cells. (gray/white hair results when air replaces the melanin)
• Hair follicles extend from the epidermal surface into the dermis. The end of the follicle is expanded forming a hair bulb, and is wrapped by a knot of sensory nerve endings called a root hair plexus (bending the hair stimulates the endings). • A hair papilla protrudes into the hair bulb and contains a knot of capillaries that supplies nutrients to the growing hair. • The wall of a hair follicle is composed of an outer connective tissue root sheath that sandwiches an external & internal root sheath against the hair follicle.
• The skin constitutes at least three types of barriers: chemical, physical, and biological. • Chemical barriers: include skin secretions and melanin. The skin’s surface teems with bacteria, however the acid mantle slows their multiplication. Melanin provides a chemical shield over skin cells’ nuclei. • Physical/Mechanical barriers: the waterproofing lipids of the epidermis block the diffusion of water. Certain substances can be absorbed through the skin.
1. Lipid-soluble—O 2, CO 2, and vitamins like A, D, E, and K 2. Oleoresins—plants like poison ivy and oak 3. Heavy metals—lead, mercury, and nickel • Biological barriers: Langerhans’ cells and DNA. Electrons in DNA absorb UV radiation and transfer it to the atomic nuclei, which heat up, therefore DNA converts potentially destructive radiation into harmless heat.
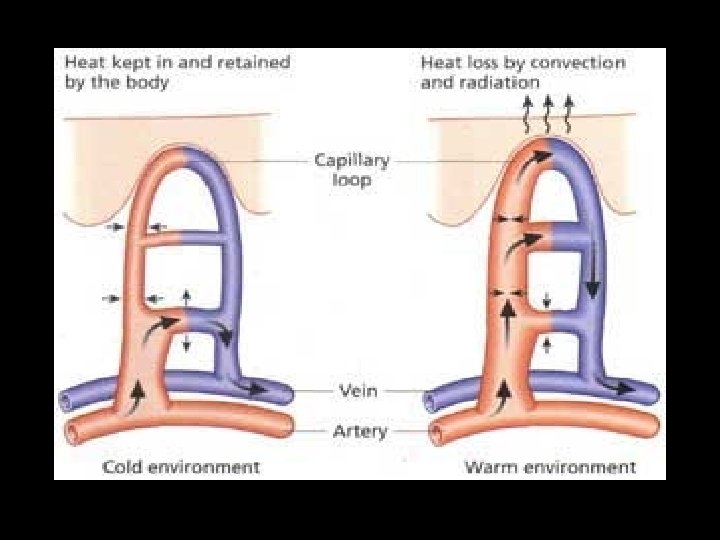
• When body temp rises, blood vessels dilate and sweat glands are stimulated. Evaporation of sweat from the skin surface dissipates body heat and cools the body preventing overheating. • When body temp drops, blood vessels constrict, causing warm blood to bypass the skin temporarily and to remain at the body’s core where vital organs are kept warm.

VIDEO CLIP • https: //www. youtube. com /watch? v=P 5_n. Q_Zd 2 ss
• Most tumors that arise in the skin are benign and do not spread (metastasize) to other body areas. However, some skin tumors are malignant, or cancerous, and invade other body areas. • Interestingly, sunburned skin accelerates its production of Fas, a protein that causes genetically damaged skin cells to commit suicide, thus decreasing the risk of mutations that will cause sun-linked skin cancer. This causes the skin to peel after a sunburn.
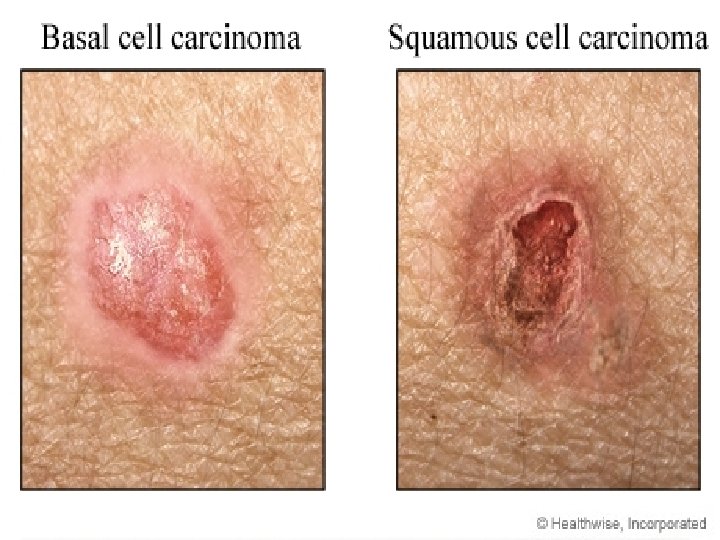
• Least malignant and most common skin cancer; arises from stratum basale layer; over 30% of all white people get it in their lifetime. • The cancer lesions occur mostly on sun-exposed areas of the face as a dome-shaped nodule. • Surgical removal cures this cancer in 99% of cases. • Arises from stratum spinosum. • Lesion appears as a scaly reddened elevated area found mostly on the scalp, ears, and hands. • Grows rapidly and metastasizes if not removed.

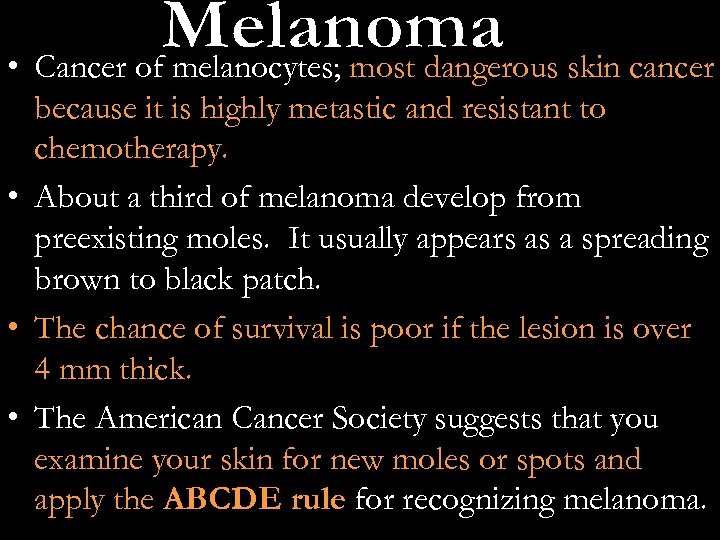
• Cancer of melanocytes; most dangerous skin cancer because it is highly metastic and resistant to chemotherapy. • About a third of melanoma develop from preexisting moles. It usually appears as a spreading brown to black patch. • The chance of survival is poor if the lesion is over 4 mm thick. • The American Cancer Society suggests that you examine your skin for new moles or spots and apply the ABCDE rule for recognizing melanoma.
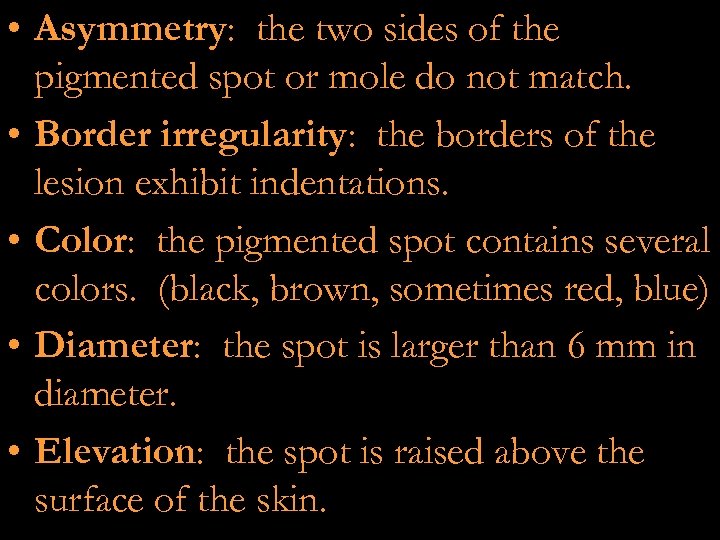
• Asymmetry: the two sides of the pigmented spot or mole do not match. • Border irregularity: the borders of the lesion exhibit indentations. • Color: the pigmented spot contains several colors. (black, brown, sometimes red, blue) • Diameter: the spot is larger than 6 mm in diameter. • Elevation: the spot is raised above the surface of the skin.

VIDEO CLIP • https: //www. youtube. com/watch? v=ao. BDa mu 3 h. HI

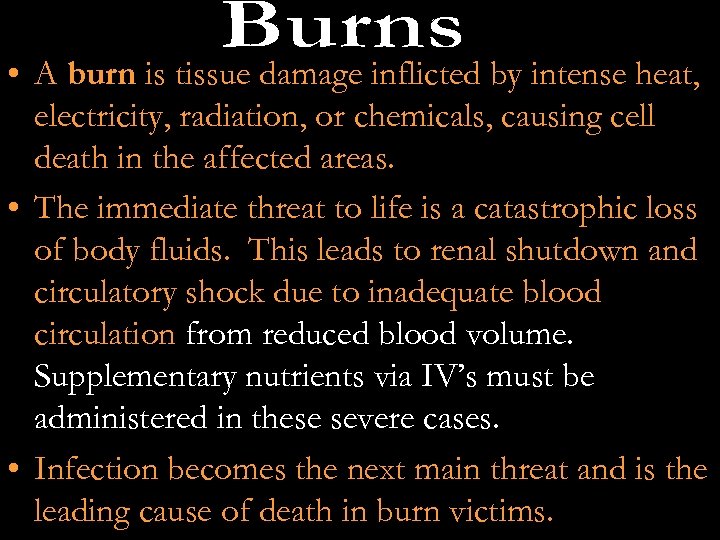
• A burn is tissue damage inflicted by intense heat, electricity, radiation, or chemicals, causing cell death in the affected areas. • The immediate threat to life is a catastrophic loss of body fluids. This leads to renal shutdown and circulatory shock due to inadequate blood circulation from reduced blood volume. Supplementary nutrients via IV’s must be administered in these severe cases. • Infection becomes the next main threat and is the leading cause of death in burn victims.
• First-degree burns: only the epidermis is damaged. (sunburn) • Second-degree burns: injure the epidermis and the upper region of the dermis. (bad sunburn accompanied by blisters) • Third-degree burns: complete destruction of epidermis and dermis. (fire) Skin grafting is usually necessary. • To prepare the burned area for grafting, the eschar (burned skin) must be removed. To prevent infection and fluid loss, the area is flooded with antibiotics and covered temporarily with animal or cadaver skin.


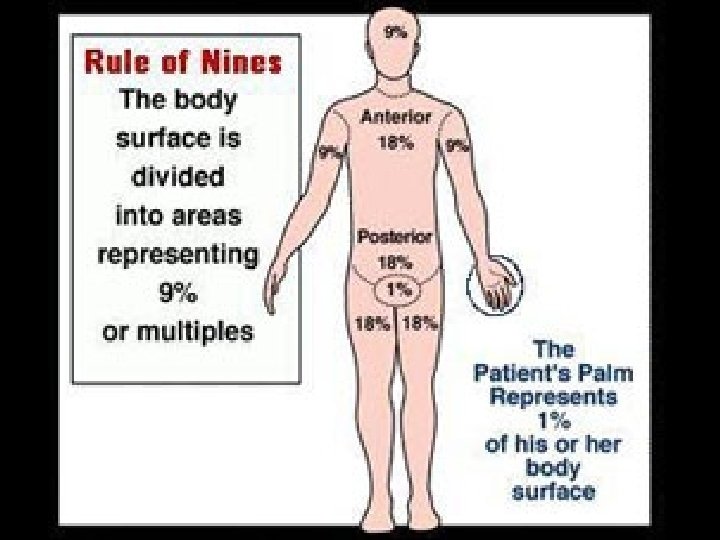
• Then healthy skin, usually from the thigh if it has not been affected, is transplanted to the burn site. • In general, burns are considered critical if any of the following conditions exists: --over 25% of the body has second-degree burns --over 10% of the body has third-degree burns --there are third-degree burns on the face, hands, or feet.
d017b412932d41f9d9a213814babf01d.ppt