Skeletal Muscle.ppt
- Количество слайдов: 193
 Skeletal Muscle Physiology
Skeletal Muscle Physiology





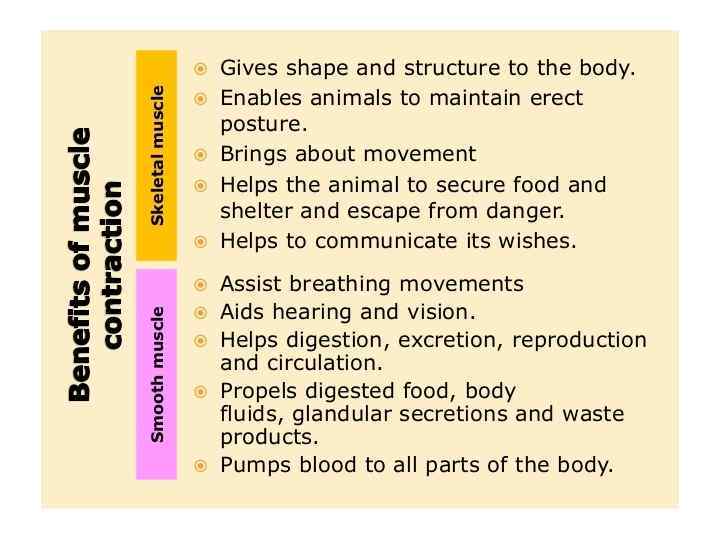
 Muscular System Functions • Body movement (Locomotion) • Maintenance of posture • Respiration – Diaphragm and intercostal contractions • Communication (Verbal and Facial) • Constriction of organs and vessels – Peristalsis of intestinal tract – Vasoconstriction of b. v. and other structures (pupils) • Heart beat • Production of body heat (Thermogenesis)
Muscular System Functions • Body movement (Locomotion) • Maintenance of posture • Respiration – Diaphragm and intercostal contractions • Communication (Verbal and Facial) • Constriction of organs and vessels – Peristalsis of intestinal tract – Vasoconstriction of b. v. and other structures (pupils) • Heart beat • Production of body heat (Thermogenesis)
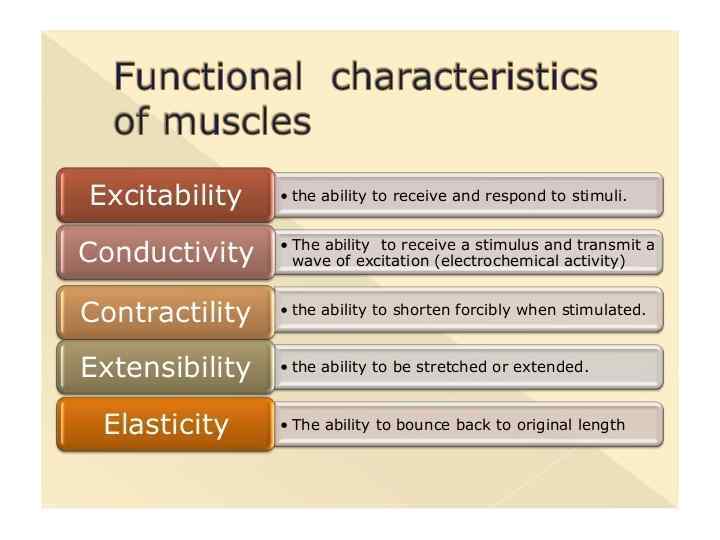
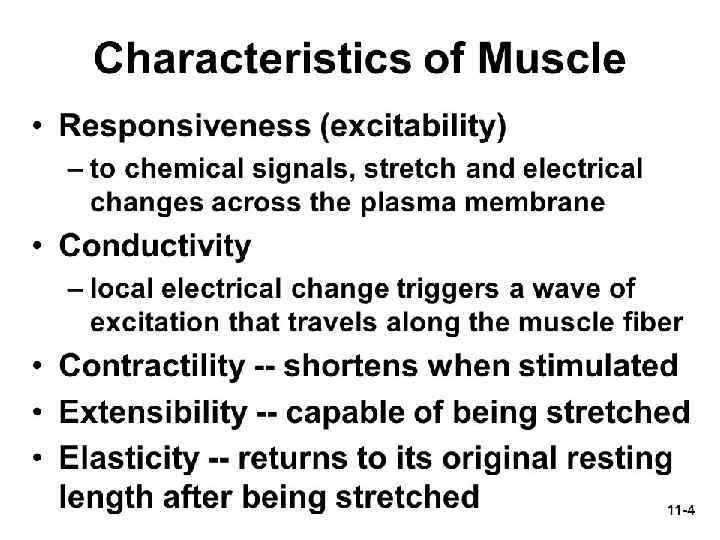
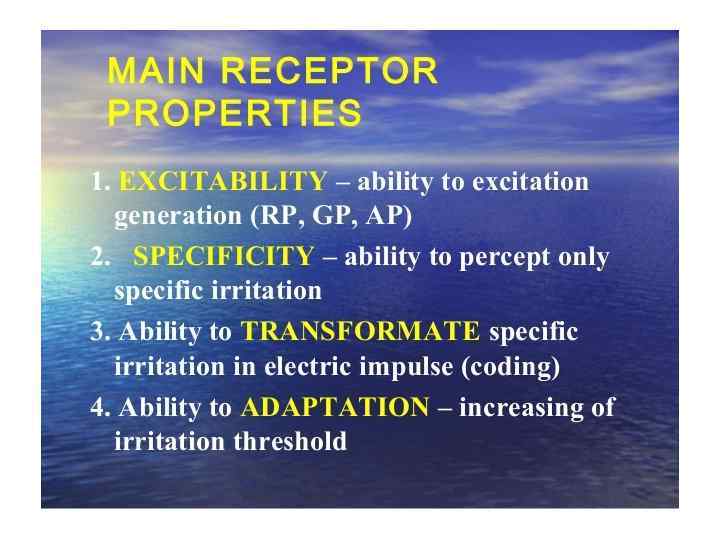
 Properties of Muscle • Excitability: capacity of muscle to respond to a stimulus • Contractility: ability of a muscle to shorten and generate pulling force • Extensibility: muscle can be stretched back to its original length • Elasticity: ability of muscle to recoil to original resting length after stretched
Properties of Muscle • Excitability: capacity of muscle to respond to a stimulus • Contractility: ability of a muscle to shorten and generate pulling force • Extensibility: muscle can be stretched back to its original length • Elasticity: ability of muscle to recoil to original resting length after stretched
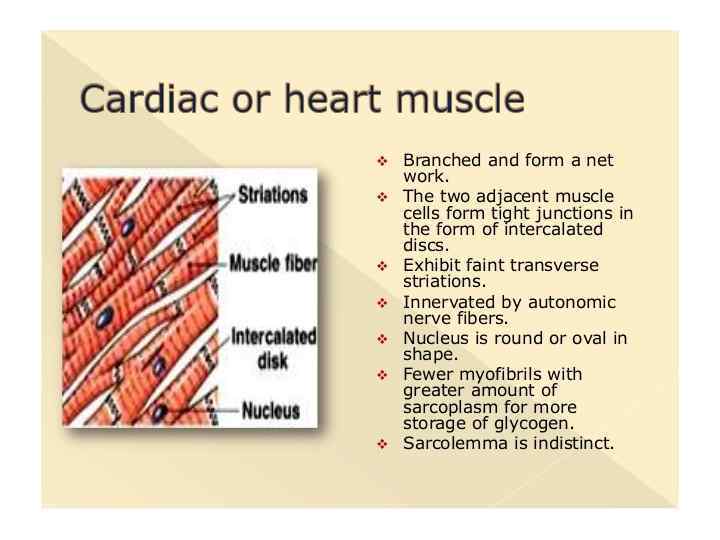
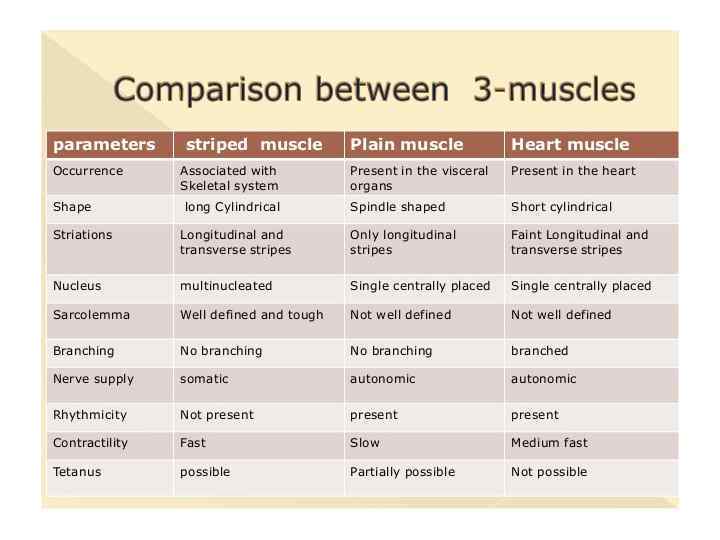
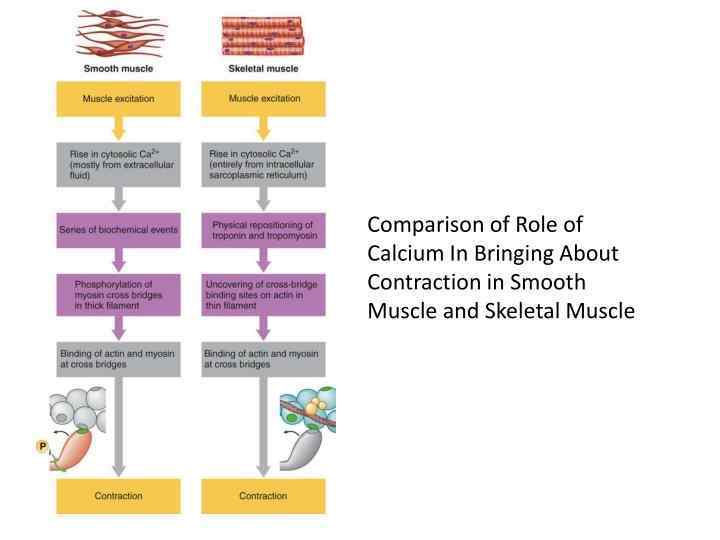
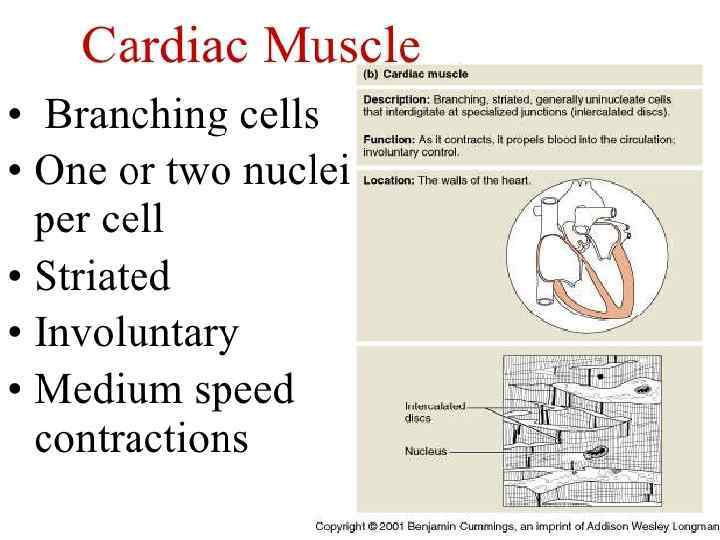
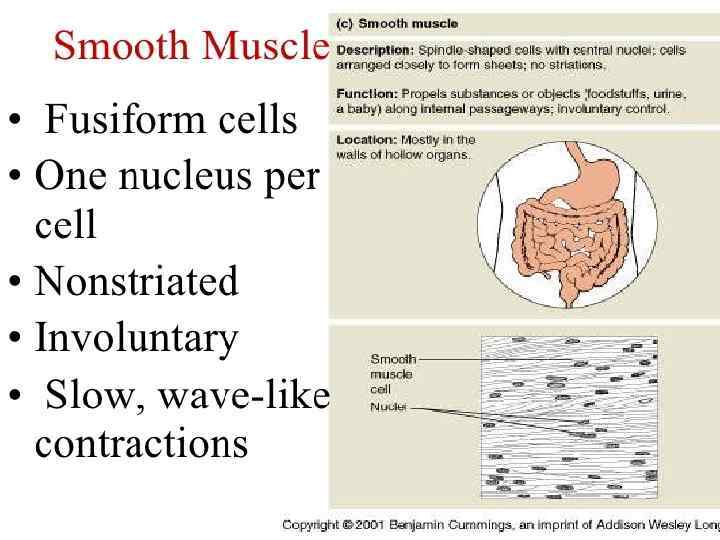
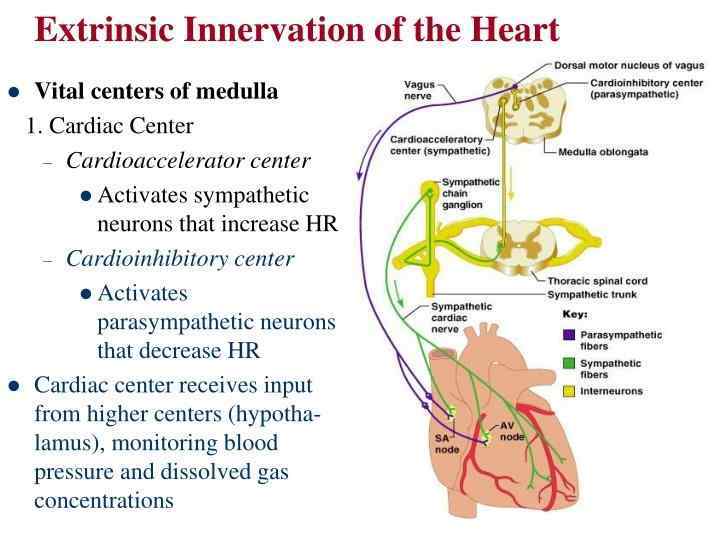
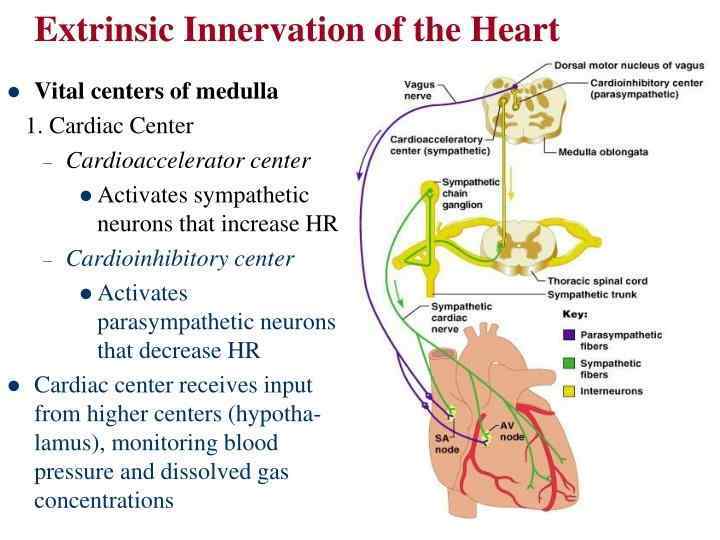
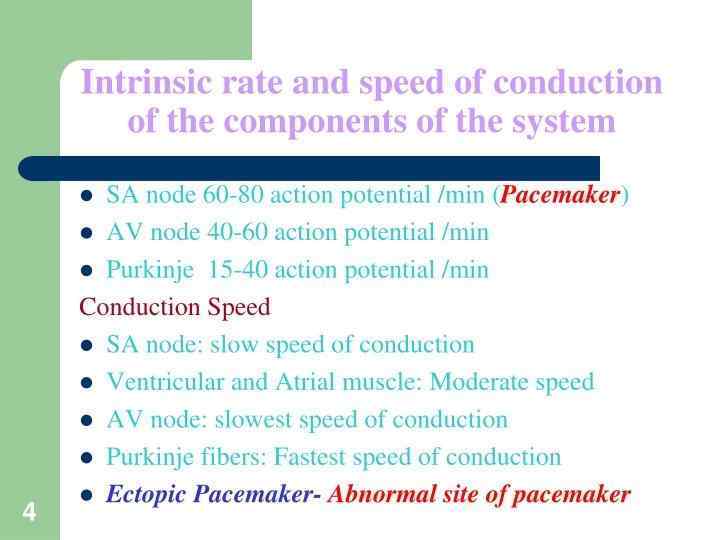
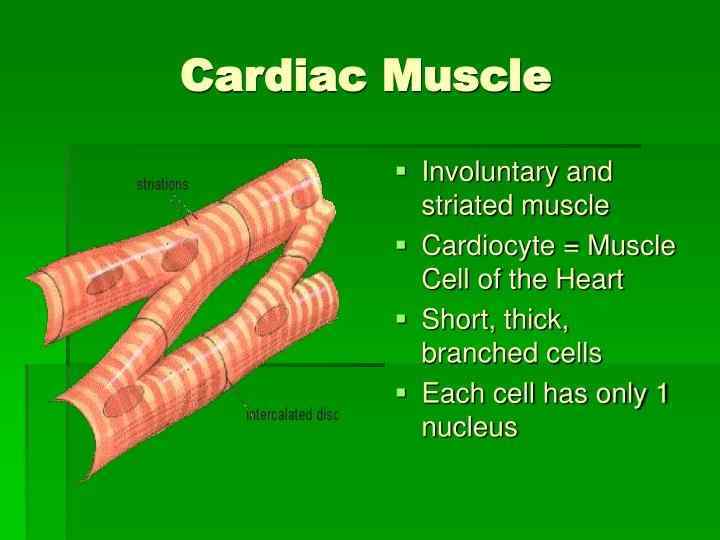
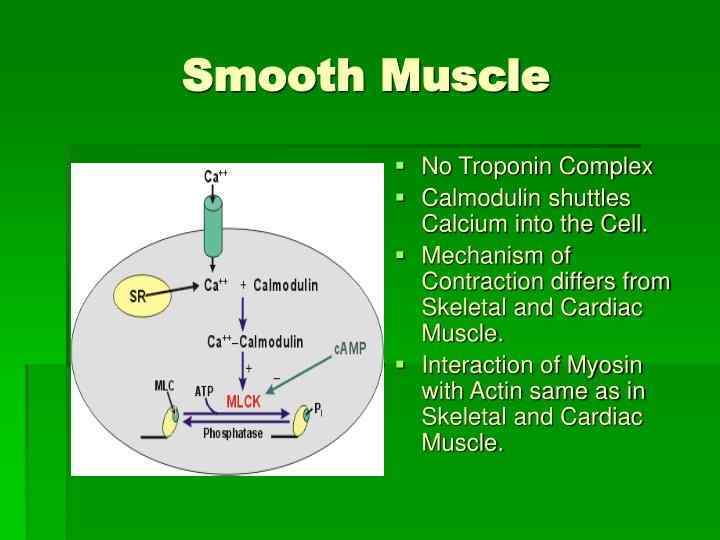
 Types of Muscle • Skeletal – Attached to bones – Makes up 40% of body weight – Responsible for locomotion, facial expressions, posture, respiratory movements, other types of body movement – Voluntary in action; controlled by somatic motor neurons • Smooth – In the walls of hollow organs, blood vessels, eye, glands, uterus, skin – Some functions: propel urine, mix food in digestive tract, dilating/constricting pupils, regulating blood flow, – In some locations, autorhythmic – Controlled involuntarily by endocrine and autonomic nervous systems • Cardiac – Heart: major source of movement of blood – Autorhythmic – Controlled involuntarily by endocrine and autonomic nervous systems
Types of Muscle • Skeletal – Attached to bones – Makes up 40% of body weight – Responsible for locomotion, facial expressions, posture, respiratory movements, other types of body movement – Voluntary in action; controlled by somatic motor neurons • Smooth – In the walls of hollow organs, blood vessels, eye, glands, uterus, skin – Some functions: propel urine, mix food in digestive tract, dilating/constricting pupils, regulating blood flow, – In some locations, autorhythmic – Controlled involuntarily by endocrine and autonomic nervous systems • Cardiac – Heart: major source of movement of blood – Autorhythmic – Controlled involuntarily by endocrine and autonomic nervous systems
 Connective Tissue Sheaths • Connective Tissue of a Muscle – Epimysium. Dense regular c. t. surrounding entire muscle • Separates muscle from surrounding tissues and organs • Connected to the deep fascia – Perimysium. Collagen and elastic fibers surrounding a group of muscle fibers called a fascicle • Contains b. v and nerves – Endomysium. Loose connective tissue that surrounds individual muscle fibers • Also contains b. v. , nerves, and satellite cells (embryonic stem cells function in repair of muscle tissue • Collagen fibers of all 3 layers come together at each end of muscle to form a tendon or aponeurosis.
Connective Tissue Sheaths • Connective Tissue of a Muscle – Epimysium. Dense regular c. t. surrounding entire muscle • Separates muscle from surrounding tissues and organs • Connected to the deep fascia – Perimysium. Collagen and elastic fibers surrounding a group of muscle fibers called a fascicle • Contains b. v and nerves – Endomysium. Loose connective tissue that surrounds individual muscle fibers • Also contains b. v. , nerves, and satellite cells (embryonic stem cells function in repair of muscle tissue • Collagen fibers of all 3 layers come together at each end of muscle to form a tendon or aponeurosis.
 Nerve and Blood Vessel Supply • Motor neurons – stimulate muscle fibers to contract – Neuron axons branch so that each muscle fiber (muscle cell) is innervated – Form a neuromuscular junction (= myoneural junction) • Capillary beds surround muscle fibers – Muscles require large amts of energy – Extensive vascular network delivers necessary oxygen and nutrients and carries away metabolic waste produced by muscle fibers
Nerve and Blood Vessel Supply • Motor neurons – stimulate muscle fibers to contract – Neuron axons branch so that each muscle fiber (muscle cell) is innervated – Form a neuromuscular junction (= myoneural junction) • Capillary beds surround muscle fibers – Muscles require large amts of energy – Extensive vascular network delivers necessary oxygen and nutrients and carries away metabolic waste produced by muscle fibers
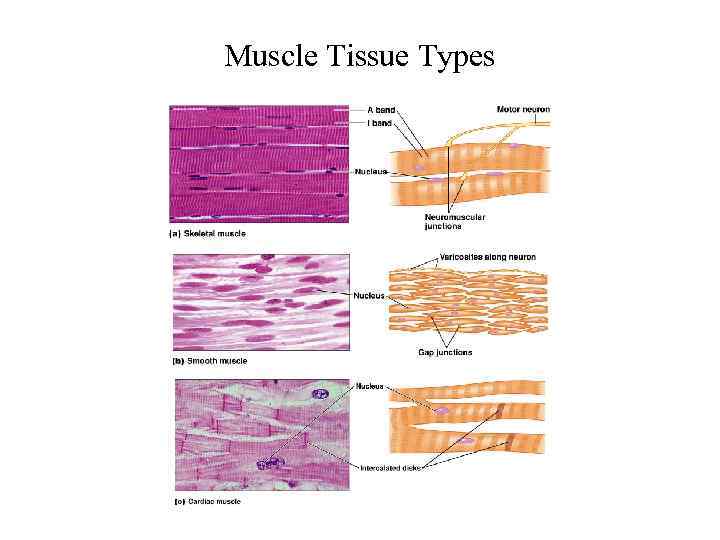 Muscle Tissue Types
Muscle Tissue Types
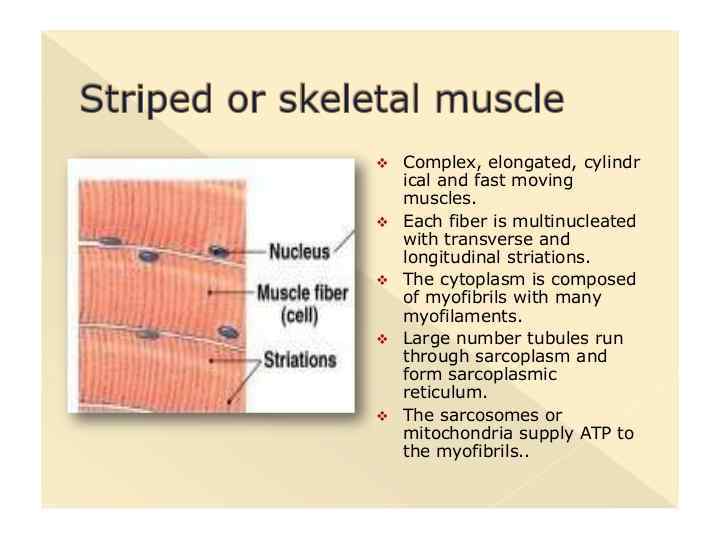
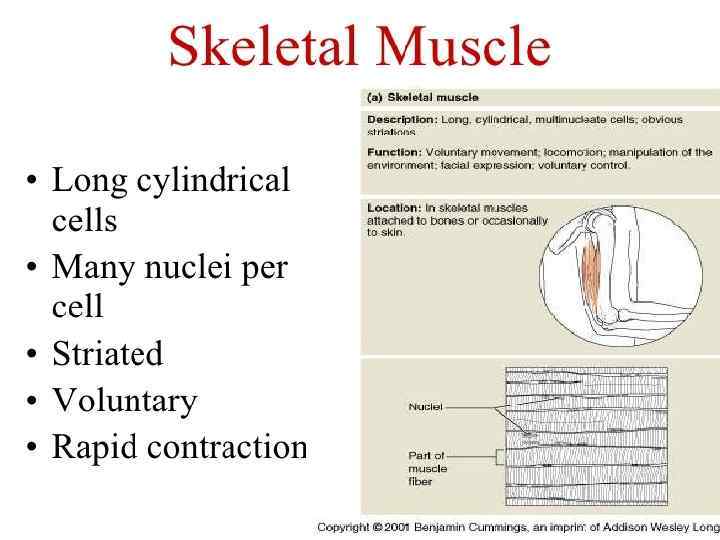
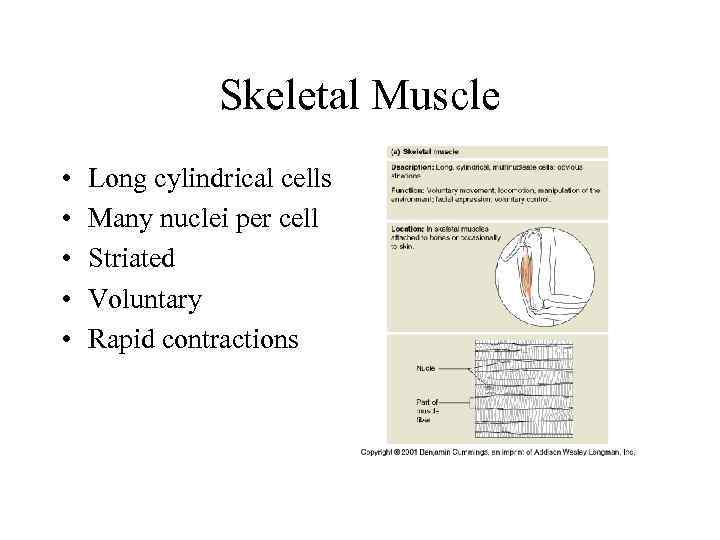 Skeletal Muscle • • • Long cylindrical cells Many nuclei per cell Striated Voluntary Rapid contractions
Skeletal Muscle • • • Long cylindrical cells Many nuclei per cell Striated Voluntary Rapid contractions
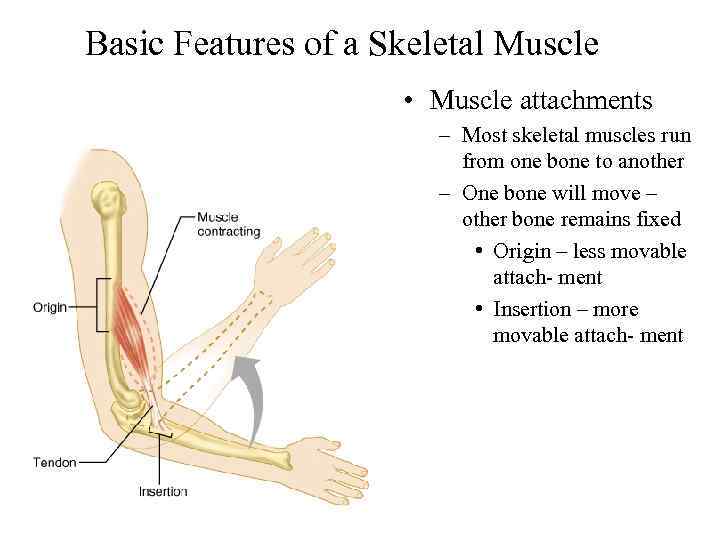 Basic Features of a Skeletal Muscle • Muscle attachments – Most skeletal muscles run from one bone to another – One bone will move – other bone remains fixed • Origin – less movable attach- ment • Insertion – more movable attach- ment
Basic Features of a Skeletal Muscle • Muscle attachments – Most skeletal muscles run from one bone to another – One bone will move – other bone remains fixed • Origin – less movable attach- ment • Insertion – more movable attach- ment
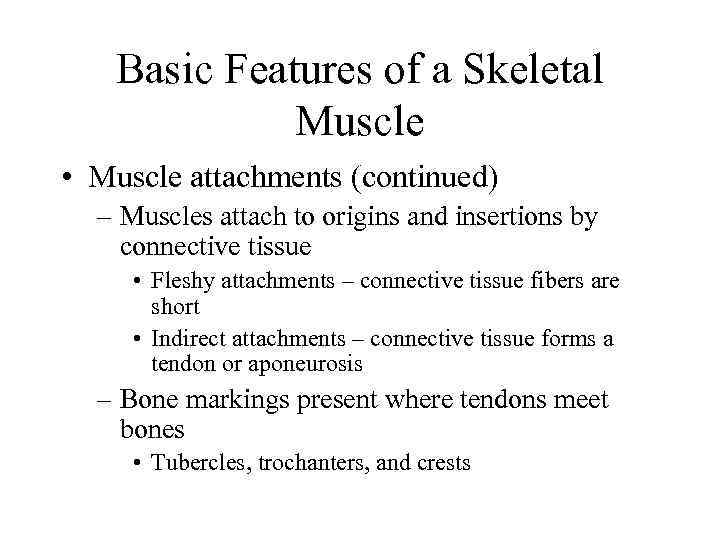 Basic Features of a Skeletal Muscle • Muscle attachments (continued) – Muscles attach to origins and insertions by connective tissue • Fleshy attachments – connective tissue fibers are short • Indirect attachments – connective tissue forms a tendon or aponeurosis – Bone markings present where tendons meet bones • Tubercles, trochanters, and crests
Basic Features of a Skeletal Muscle • Muscle attachments (continued) – Muscles attach to origins and insertions by connective tissue • Fleshy attachments – connective tissue fibers are short • Indirect attachments – connective tissue forms a tendon or aponeurosis – Bone markings present where tendons meet bones • Tubercles, trochanters, and crests
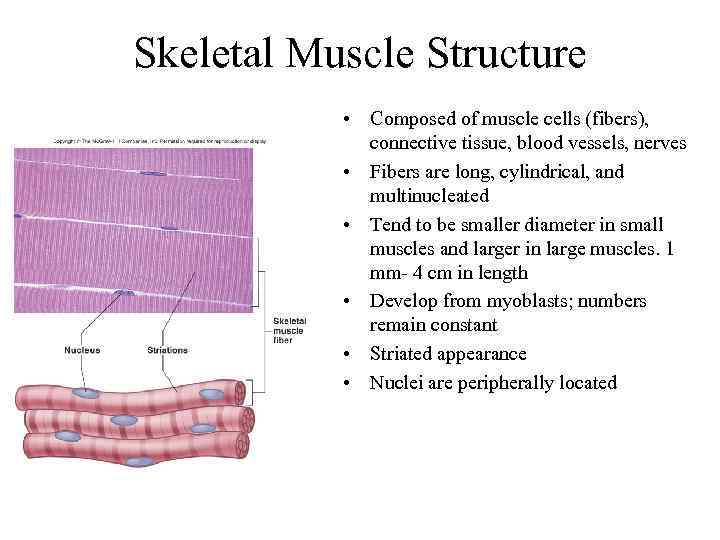 Skeletal Muscle Structure • Composed of muscle cells (fibers), connective tissue, blood vessels, nerves • Fibers are long, cylindrical, and multinucleated • Tend to be smaller diameter in small muscles and larger in large muscles. 1 mm- 4 cm in length • Develop from myoblasts; numbers remain constant • Striated appearance • Nuclei are peripherally located
Skeletal Muscle Structure • Composed of muscle cells (fibers), connective tissue, blood vessels, nerves • Fibers are long, cylindrical, and multinucleated • Tend to be smaller diameter in small muscles and larger in large muscles. 1 mm- 4 cm in length • Develop from myoblasts; numbers remain constant • Striated appearance • Nuclei are peripherally located
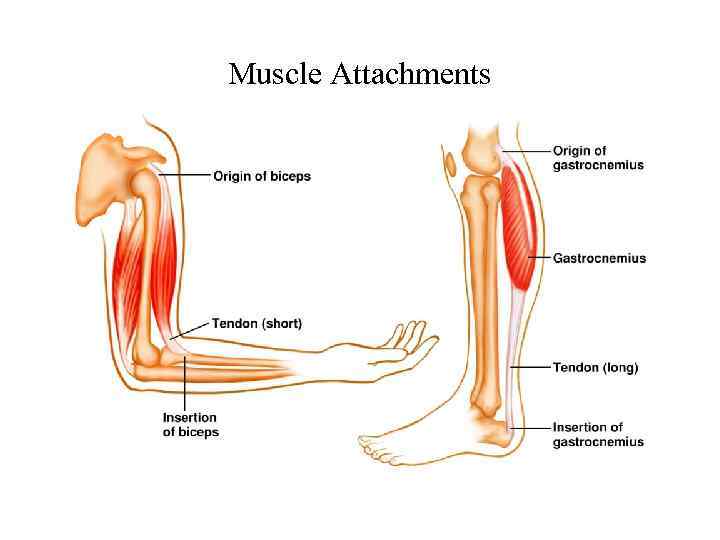 Muscle Attachments
Muscle Attachments
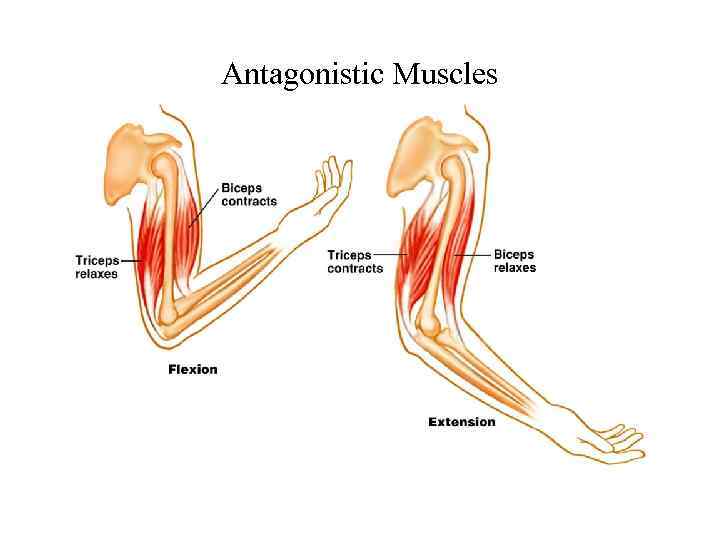 Antagonistic Muscles
Antagonistic Muscles
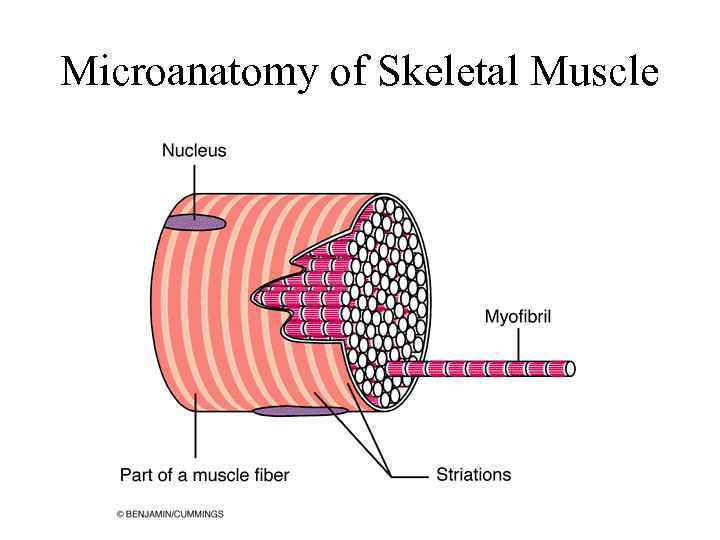 Microanatomy of Skeletal Muscle
Microanatomy of Skeletal Muscle
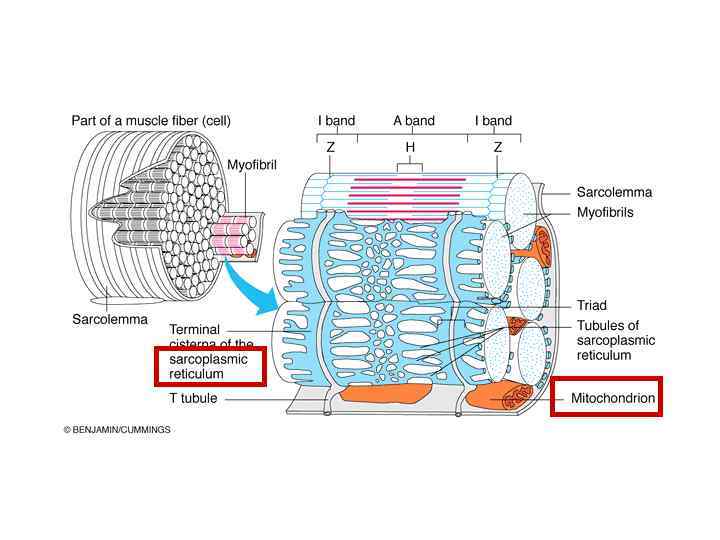
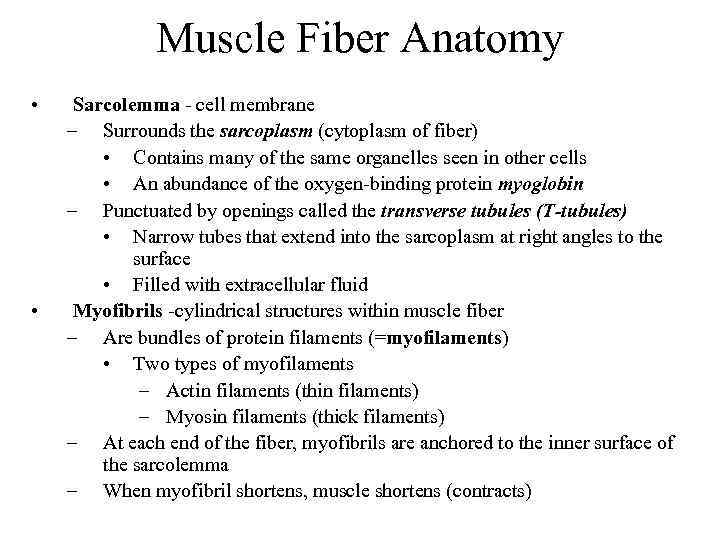 Muscle Fiber Anatomy • • Sarcolemma - cell membrane – Surrounds the sarcoplasm (cytoplasm of fiber) • Contains many of the same organelles seen in other cells • An abundance of the oxygen-binding protein myoglobin – Punctuated by openings called the transverse tubules (T-tubules) • Narrow tubes that extend into the sarcoplasm at right angles to the surface • Filled with extracellular fluid Myofibrils -cylindrical structures within muscle fiber – Are bundles of protein filaments (=myofilaments) • Two types of myofilaments – Actin filaments (thin filaments) – Myosin filaments (thick filaments) – At each end of the fiber, myofibrils are anchored to the inner surface of the sarcolemma – When myofibril shortens, muscle shortens (contracts)
Muscle Fiber Anatomy • • Sarcolemma - cell membrane – Surrounds the sarcoplasm (cytoplasm of fiber) • Contains many of the same organelles seen in other cells • An abundance of the oxygen-binding protein myoglobin – Punctuated by openings called the transverse tubules (T-tubules) • Narrow tubes that extend into the sarcoplasm at right angles to the surface • Filled with extracellular fluid Myofibrils -cylindrical structures within muscle fiber – Are bundles of protein filaments (=myofilaments) • Two types of myofilaments – Actin filaments (thin filaments) – Myosin filaments (thick filaments) – At each end of the fiber, myofibrils are anchored to the inner surface of the sarcolemma – When myofibril shortens, muscle shortens (contracts)
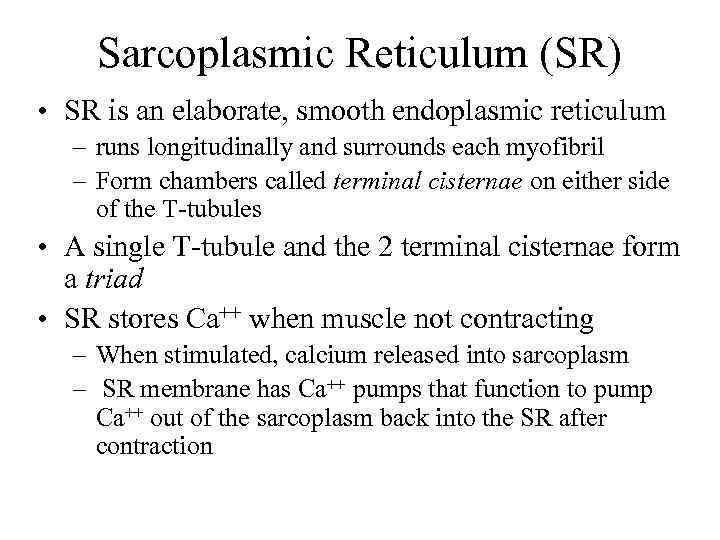 Sarcoplasmic Reticulum (SR) • SR is an elaborate, smooth endoplasmic reticulum – runs longitudinally and surrounds each myofibril – Form chambers called terminal cisternae on either side of the T-tubules • A single T-tubule and the 2 terminal cisternae form a triad • SR stores Ca++ when muscle not contracting – When stimulated, calcium released into sarcoplasm – SR membrane has Ca++ pumps that function to pump Ca++ out of the sarcoplasm back into the SR after contraction
Sarcoplasmic Reticulum (SR) • SR is an elaborate, smooth endoplasmic reticulum – runs longitudinally and surrounds each myofibril – Form chambers called terminal cisternae on either side of the T-tubules • A single T-tubule and the 2 terminal cisternae form a triad • SR stores Ca++ when muscle not contracting – When stimulated, calcium released into sarcoplasm – SR membrane has Ca++ pumps that function to pump Ca++ out of the sarcoplasm back into the SR after contraction
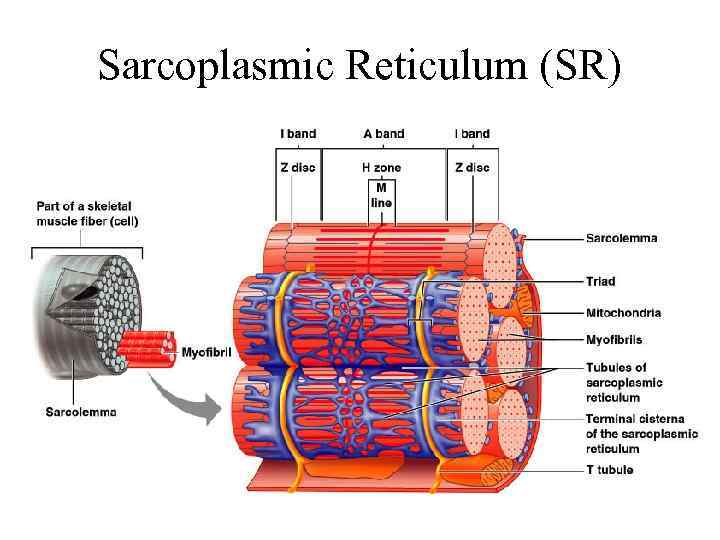 Sarcoplasmic Reticulum (SR)
Sarcoplasmic Reticulum (SR)
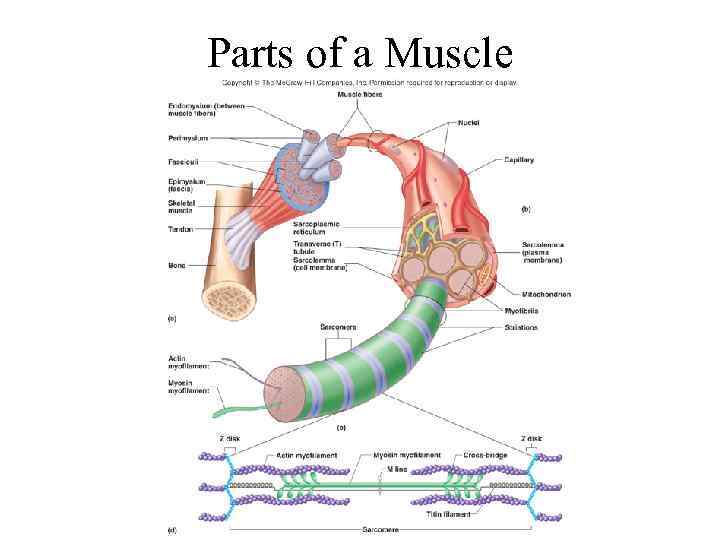 Parts of a Muscle
Parts of a Muscle
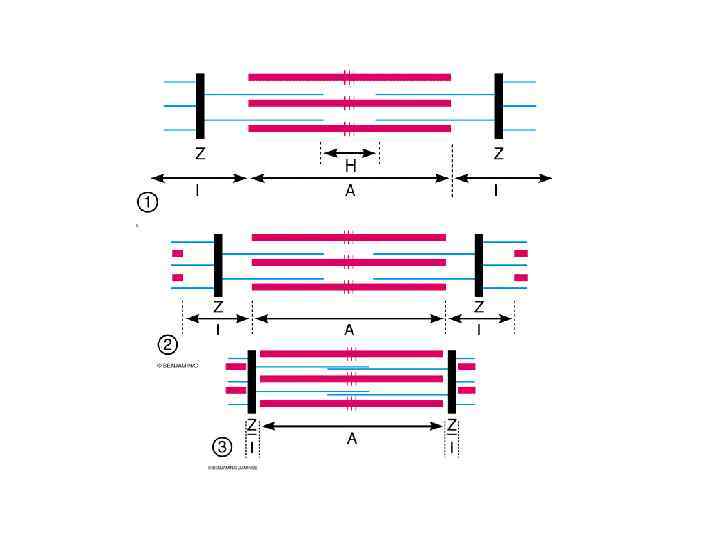
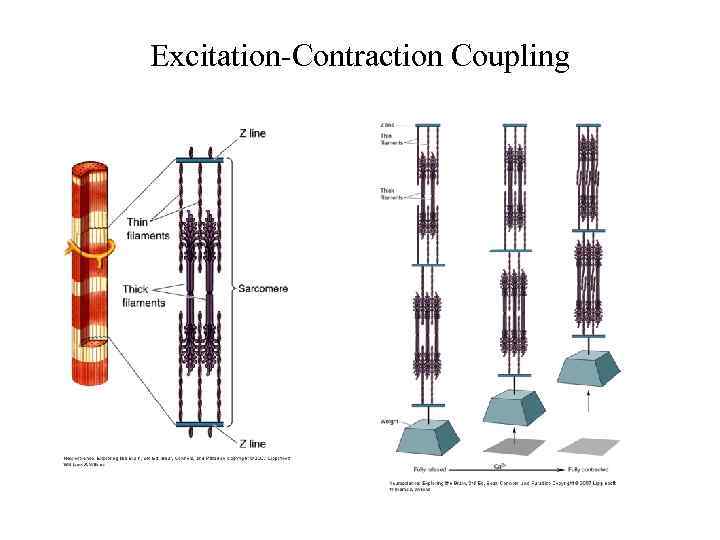
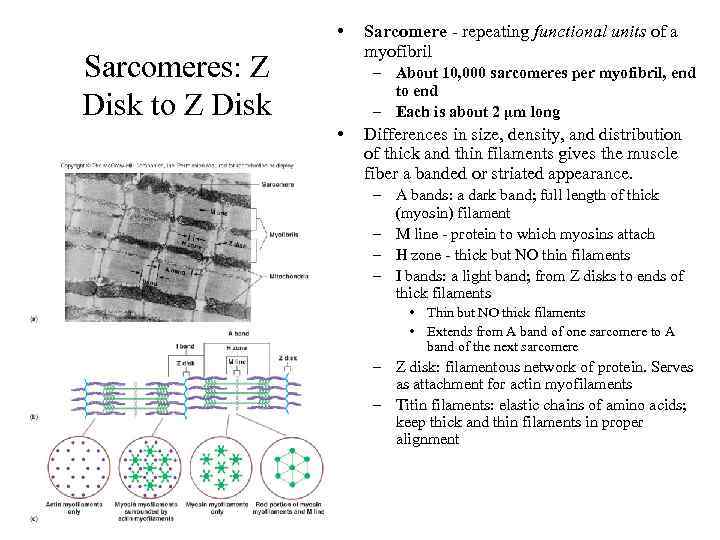 • Sarcomeres: Z Disk to Z Disk Sarcomere - repeating functional units of a myofibril – About 10, 000 sarcomeres per myofibril, end to end – Each is about 2 µm long • Differences in size, density, and distribution of thick and thin filaments gives the muscle fiber a banded or striated appearance. – A bands: a dark band; full length of thick (myosin) filament – M line - protein to which myosins attach – H zone - thick but NO thin filaments – I bands: a light band; from Z disks to ends of thick filaments • Thin but NO thick filaments • Extends from A band of one sarcomere to A band of the next sarcomere – Z disk: filamentous network of protein. Serves as attachment for actin myofilaments – Titin filaments: elastic chains of amino acids; keep thick and thin filaments in proper alignment
• Sarcomeres: Z Disk to Z Disk Sarcomere - repeating functional units of a myofibril – About 10, 000 sarcomeres per myofibril, end to end – Each is about 2 µm long • Differences in size, density, and distribution of thick and thin filaments gives the muscle fiber a banded or striated appearance. – A bands: a dark band; full length of thick (myosin) filament – M line - protein to which myosins attach – H zone - thick but NO thin filaments – I bands: a light band; from Z disks to ends of thick filaments • Thin but NO thick filaments • Extends from A band of one sarcomere to A band of the next sarcomere – Z disk: filamentous network of protein. Serves as attachment for actin myofilaments – Titin filaments: elastic chains of amino acids; keep thick and thin filaments in proper alignment
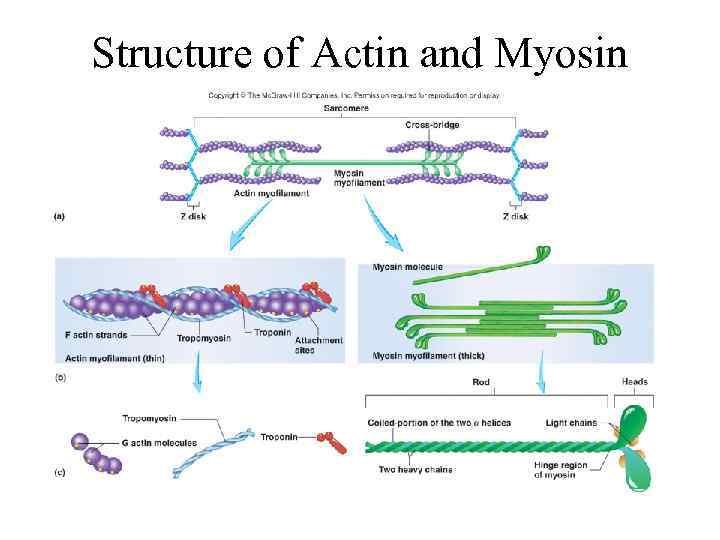 Structure of Actin and Myosin
Structure of Actin and Myosin
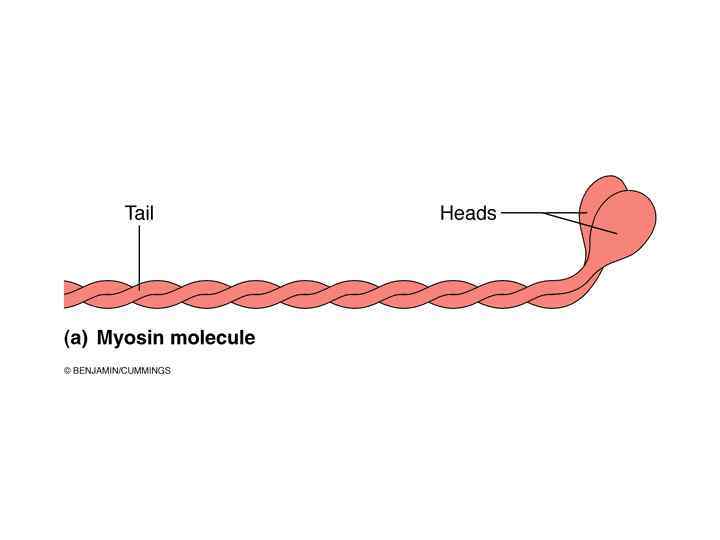
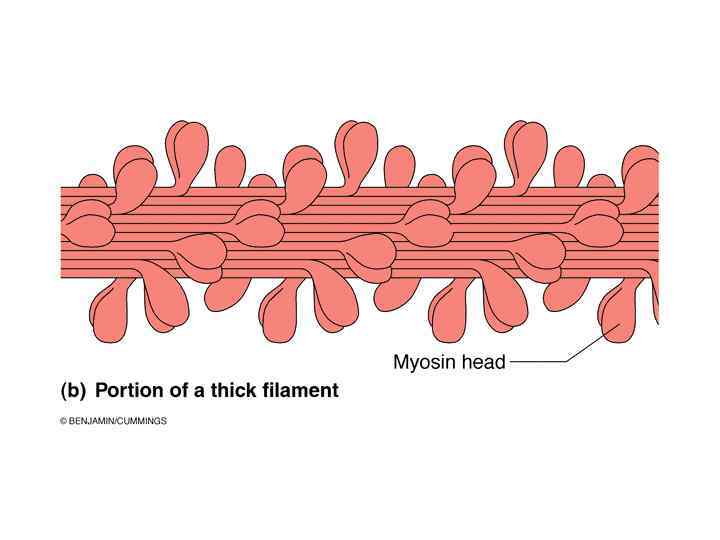
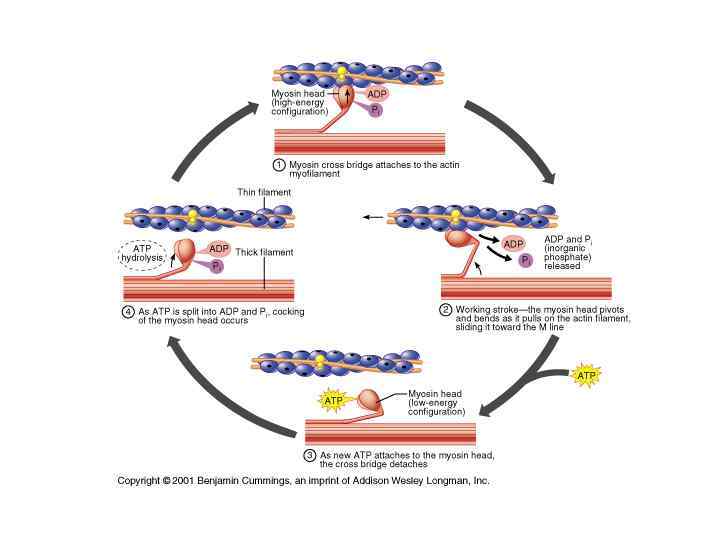
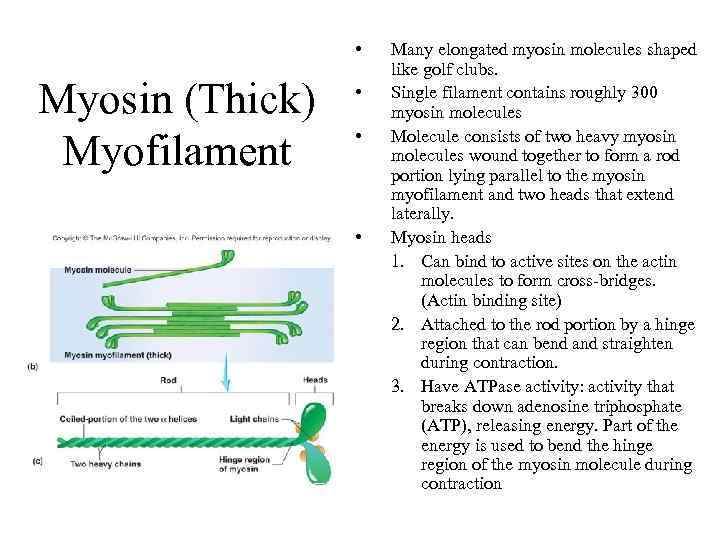 • Myosin (Thick) Myofilament • • • Many elongated myosin molecules shaped like golf clubs. Single filament contains roughly 300 myosin molecules Molecule consists of two heavy myosin molecules wound together to form a rod portion lying parallel to the myosin myofilament and two heads that extend laterally. Myosin heads 1. Can bind to active sites on the actin molecules to form cross-bridges. (Actin binding site) 2. Attached to the rod portion by a hinge region that can bend and straighten during contraction. 3. Have ATPase activity: activity that breaks down adenosine triphosphate (ATP), releasing energy. Part of the energy is used to bend the hinge region of the myosin molecule during contraction
• Myosin (Thick) Myofilament • • • Many elongated myosin molecules shaped like golf clubs. Single filament contains roughly 300 myosin molecules Molecule consists of two heavy myosin molecules wound together to form a rod portion lying parallel to the myosin myofilament and two heads that extend laterally. Myosin heads 1. Can bind to active sites on the actin molecules to form cross-bridges. (Actin binding site) 2. Attached to the rod portion by a hinge region that can bend and straighten during contraction. 3. Have ATPase activity: activity that breaks down adenosine triphosphate (ATP), releasing energy. Part of the energy is used to bend the hinge region of the myosin molecule during contraction
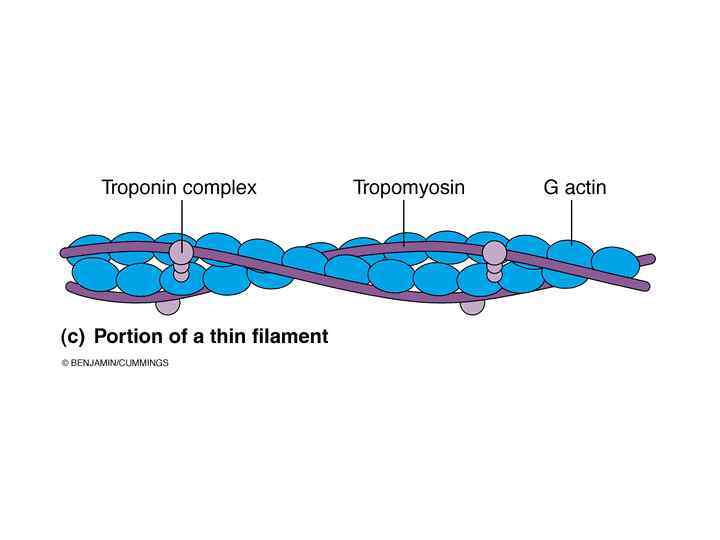
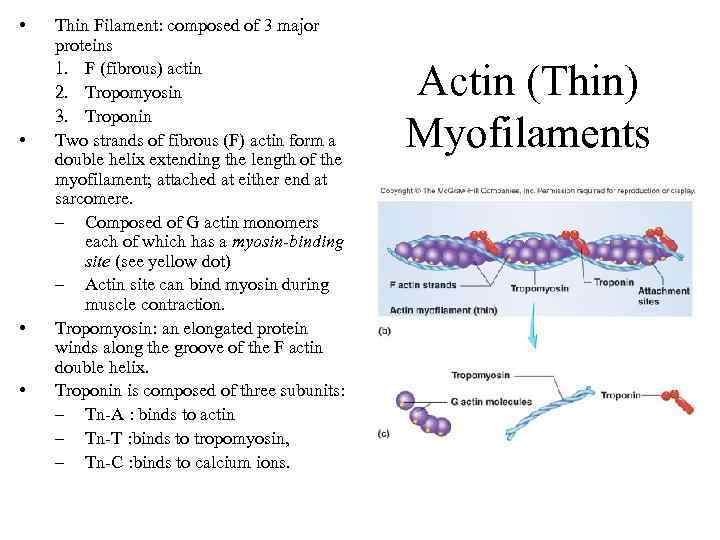 • • Thin Filament: composed of 3 major proteins 1. F (fibrous) actin 2. Tropomyosin 3. Troponin Two strands of fibrous (F) actin form a double helix extending the length of the myofilament; attached at either end at sarcomere. – Composed of G actin monomers each of which has a myosin-binding site (see yellow dot) – Actin site can bind myosin during muscle contraction. Tropomyosin: an elongated protein winds along the groove of the F actin double helix. Troponin is composed of three subunits: – Tn-A : binds to actin – Tn-T : binds to tropomyosin, – Tn-C : binds to calcium ions. Actin (Thin) Myofilaments
• • Thin Filament: composed of 3 major proteins 1. F (fibrous) actin 2. Tropomyosin 3. Troponin Two strands of fibrous (F) actin form a double helix extending the length of the myofilament; attached at either end at sarcomere. – Composed of G actin monomers each of which has a myosin-binding site (see yellow dot) – Actin site can bind myosin during muscle contraction. Tropomyosin: an elongated protein winds along the groove of the F actin double helix. Troponin is composed of three subunits: – Tn-A : binds to actin – Tn-T : binds to tropomyosin, – Tn-C : binds to calcium ions. Actin (Thin) Myofilaments
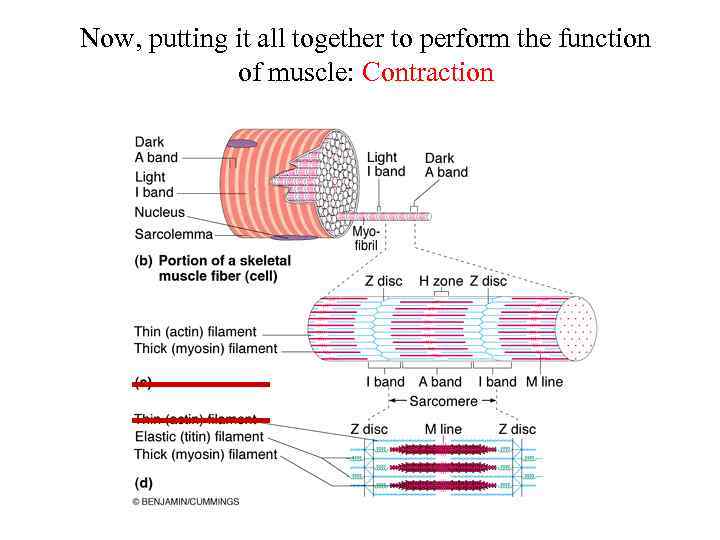 Now, putting it all together to perform the function of muscle: Contraction
Now, putting it all together to perform the function of muscle: Contraction
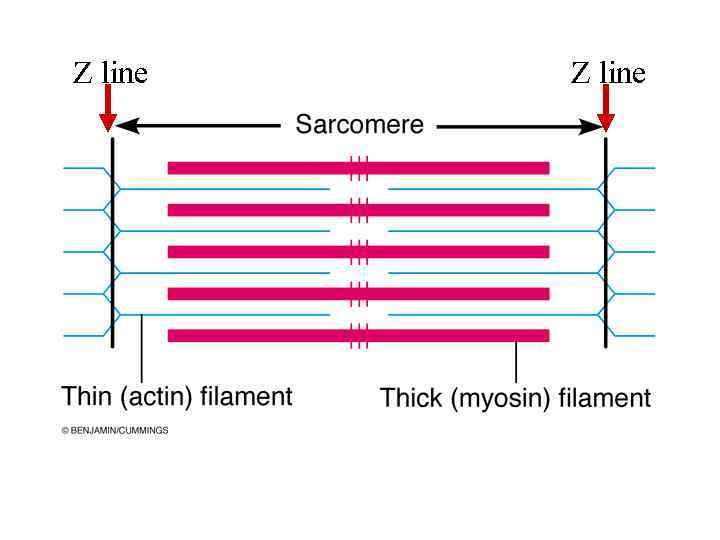 Z line
Z line
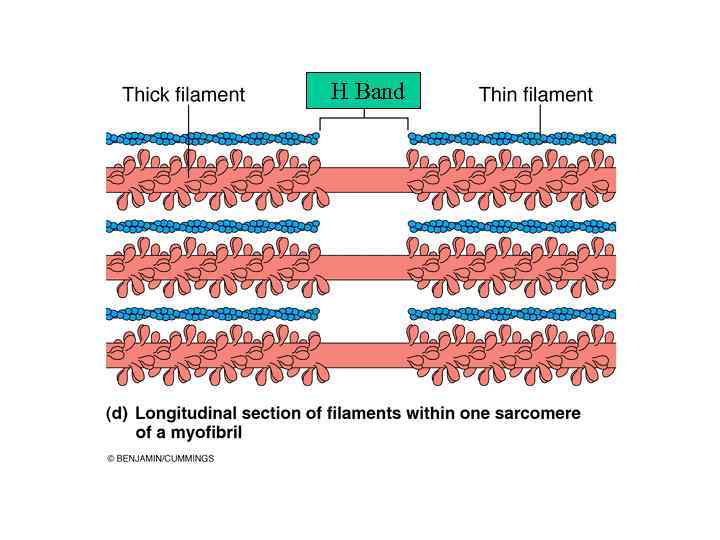 H Band
H Band
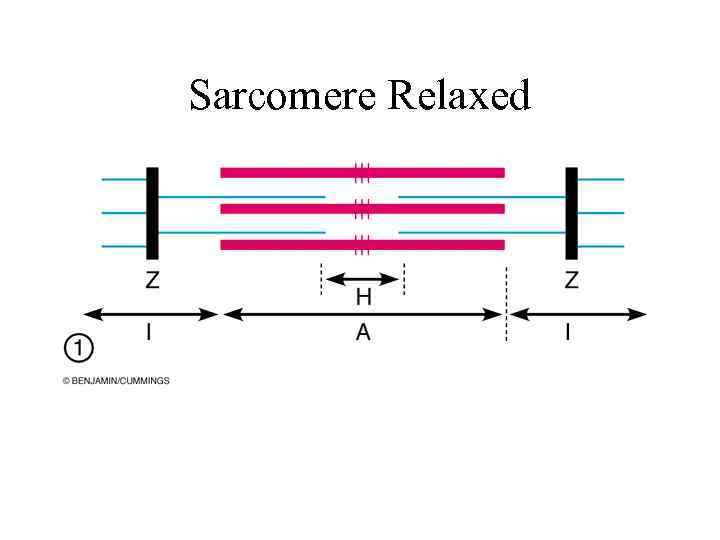 Sarcomere Relaxed
Sarcomere Relaxed
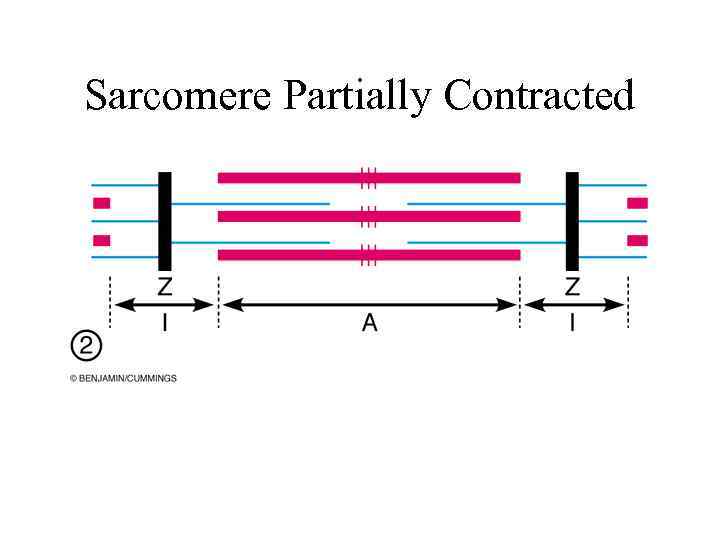 Sarcomere Partially Contracted
Sarcomere Partially Contracted
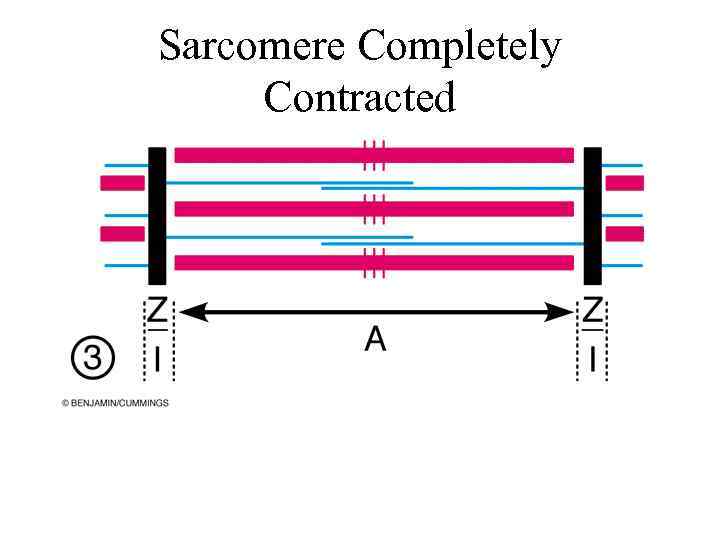 Sarcomere Completely Contracted
Sarcomere Completely Contracted
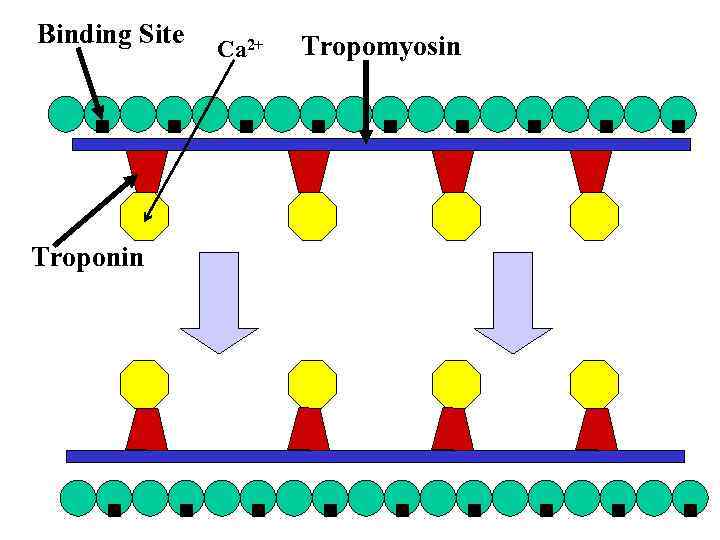 Binding Site Troponin Ca 2+ Tropomyosin
Binding Site Troponin Ca 2+ Tropomyosin
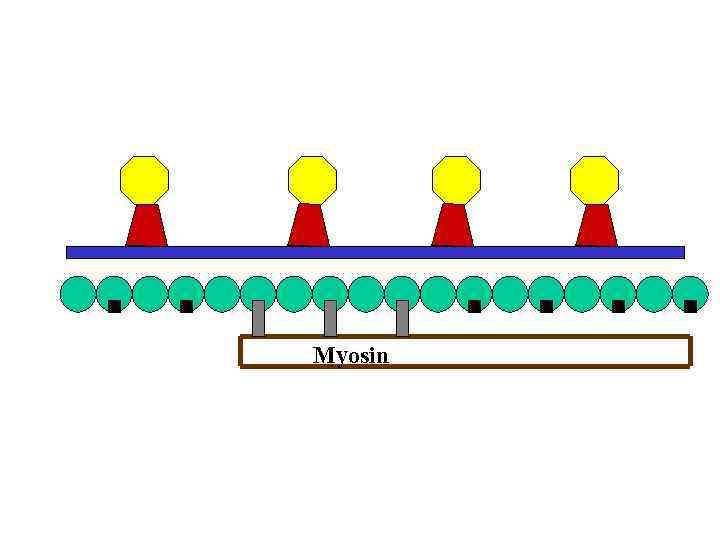 Myosin
Myosin
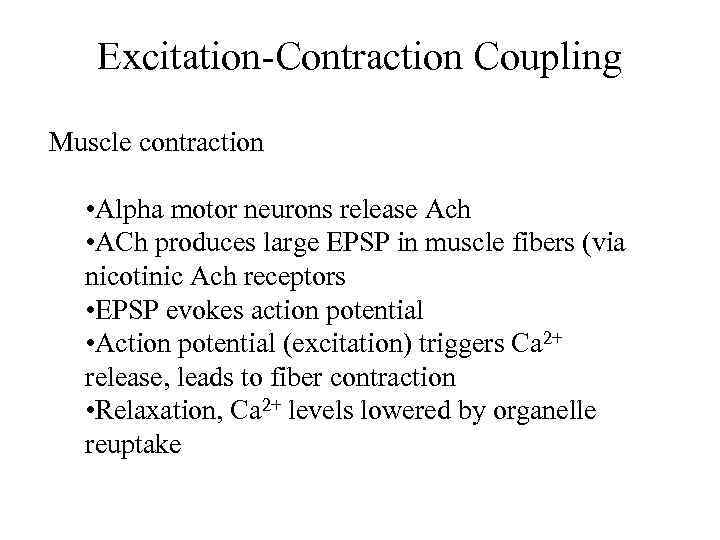 Excitation-Contraction Coupling Muscle contraction • Alpha motor neurons release Ach • ACh produces large EPSP in muscle fibers (via nicotinic Ach receptors • EPSP evokes action potential • Action potential (excitation) triggers Ca 2+ release, leads to fiber contraction • Relaxation, Ca 2+ levels lowered by organelle reuptake
Excitation-Contraction Coupling Muscle contraction • Alpha motor neurons release Ach • ACh produces large EPSP in muscle fibers (via nicotinic Ach receptors • EPSP evokes action potential • Action potential (excitation) triggers Ca 2+ release, leads to fiber contraction • Relaxation, Ca 2+ levels lowered by organelle reuptake
 Excitation-Contraction Coupling
Excitation-Contraction Coupling
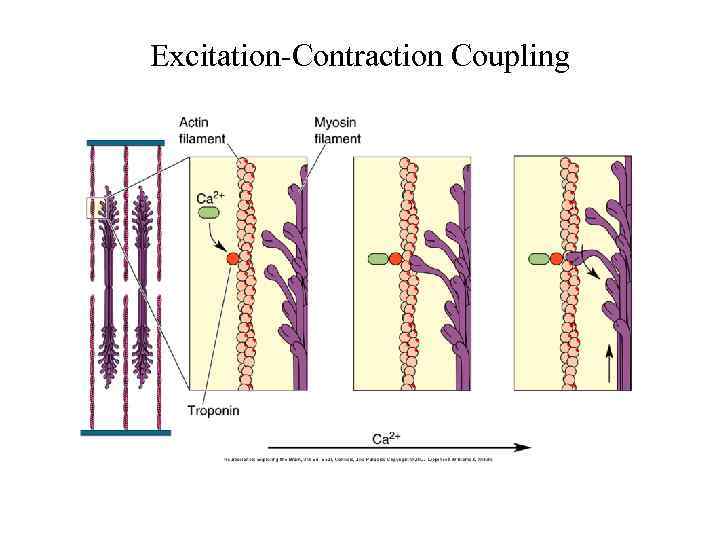 Excitation-Contraction Coupling
Excitation-Contraction Coupling
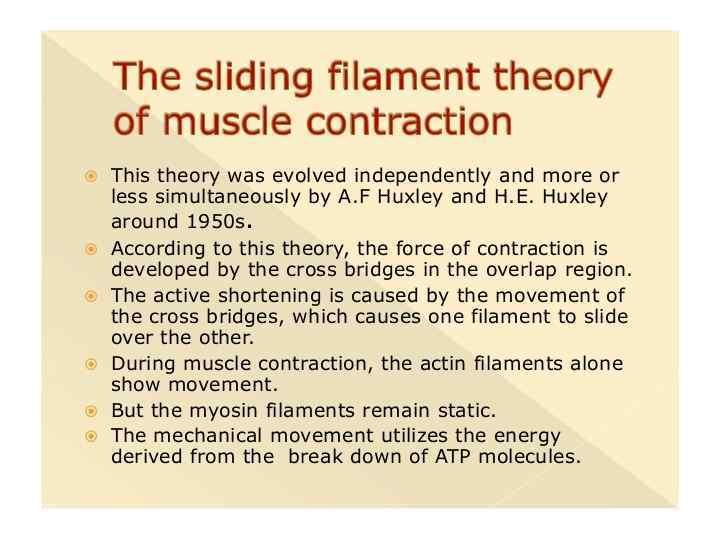
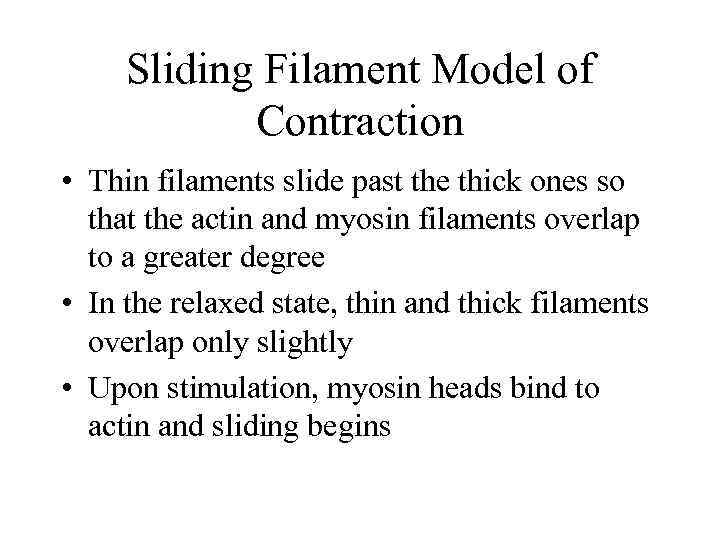 Sliding Filament Model of Contraction • Thin filaments slide past the thick ones so that the actin and myosin filaments overlap to a greater degree • In the relaxed state, thin and thick filaments overlap only slightly • Upon stimulation, myosin heads bind to actin and sliding begins
Sliding Filament Model of Contraction • Thin filaments slide past the thick ones so that the actin and myosin filaments overlap to a greater degree • In the relaxed state, thin and thick filaments overlap only slightly • Upon stimulation, myosin heads bind to actin and sliding begins
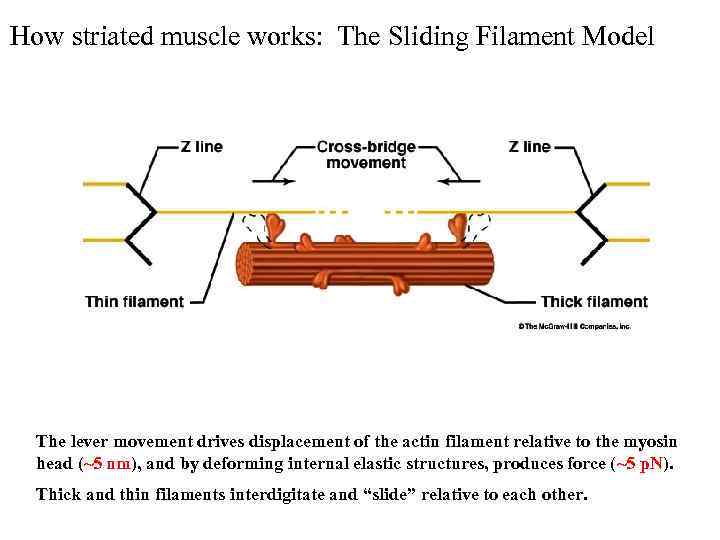 How striated muscle works: The Sliding Filament Model The lever movement drives displacement of the actin filament relative to the myosin head (~5 nm), and by deforming internal elastic structures, produces force (~5 p. N). Thick and thin filaments interdigitate and “slide” relative to each other.
How striated muscle works: The Sliding Filament Model The lever movement drives displacement of the actin filament relative to the myosin head (~5 nm), and by deforming internal elastic structures, produces force (~5 p. N). Thick and thin filaments interdigitate and “slide” relative to each other.
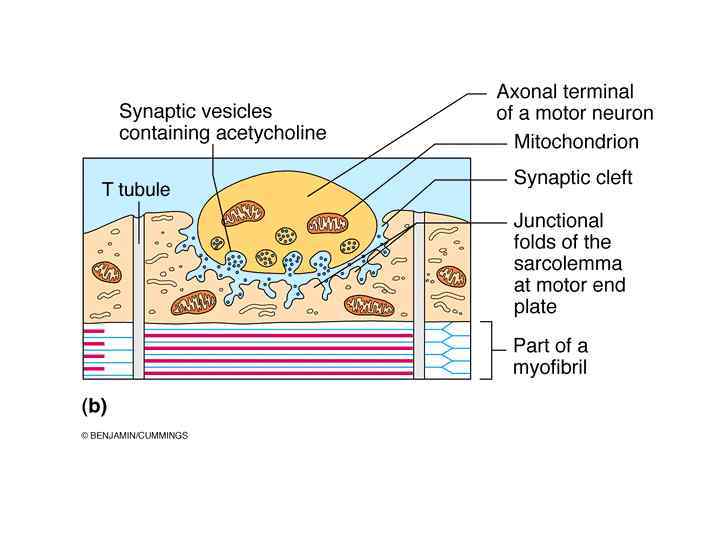
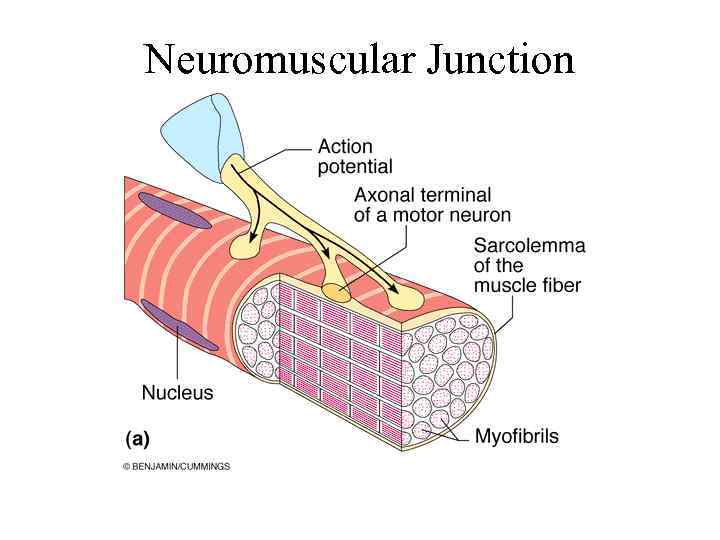 Neuromuscular Junction
Neuromuscular Junction
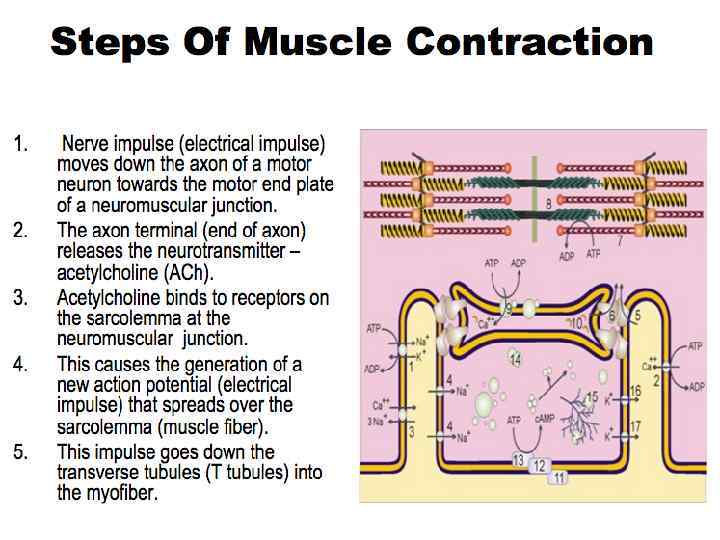
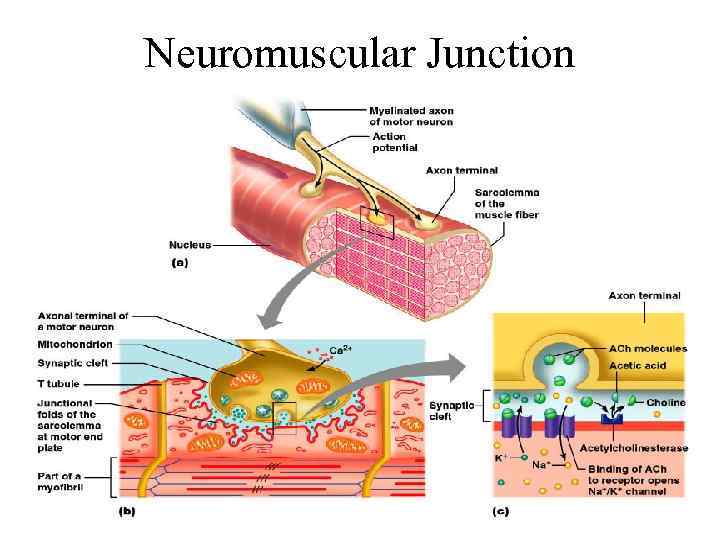
 Neuromuscular Junction • Region where the motor neuron stimulates the muscle fiber • The neuromuscular junction is formed by : 1. End of motor neuron axon (axon terminal) • Terminals have small membranous sacs (synaptic vesicles) that contain the neurotransmitter acetylcholine (ACh) 2. The motor end plate of a muscle • A specific part of the sarcolemma that contains ACh receptors • Though exceedingly close, axonal ends and muscle fibers are always separated by a space called the synaptic cleft
Neuromuscular Junction • Region where the motor neuron stimulates the muscle fiber • The neuromuscular junction is formed by : 1. End of motor neuron axon (axon terminal) • Terminals have small membranous sacs (synaptic vesicles) that contain the neurotransmitter acetylcholine (ACh) 2. The motor end plate of a muscle • A specific part of the sarcolemma that contains ACh receptors • Though exceedingly close, axonal ends and muscle fibers are always separated by a space called the synaptic cleft
 Neuromuscular Junction
Neuromuscular Junction
 Motor Unit: The Nerve-Muscle Functional Unit • A motor unit is a motor neuron and all the muscle fibers it supplies • The number of muscle fibers per motor unit can vary from a few (4 -6) to hundreds (1200 -1500) • Muscles that control fine movements (fingers, eyes) have small motor units • Large weight-bearing muscles (thighs, hips) have large motor units
Motor Unit: The Nerve-Muscle Functional Unit • A motor unit is a motor neuron and all the muscle fibers it supplies • The number of muscle fibers per motor unit can vary from a few (4 -6) to hundreds (1200 -1500) • Muscles that control fine movements (fingers, eyes) have small motor units • Large weight-bearing muscles (thighs, hips) have large motor units
 Motor Unit: The Nerve-Muscle Functional Unit • Muscle fibers from a motor unit are spread throughout the muscle – Not confined to one fascicle • Therefore, contraction of a single motor unit causes weak contraction of the entire muscle • Stronger and stronger contractions of a muscle require more and more motor units being stimulated (recruited)
Motor Unit: The Nerve-Muscle Functional Unit • Muscle fibers from a motor unit are spread throughout the muscle – Not confined to one fascicle • Therefore, contraction of a single motor unit causes weak contraction of the entire muscle • Stronger and stronger contractions of a muscle require more and more motor units being stimulated (recruited)
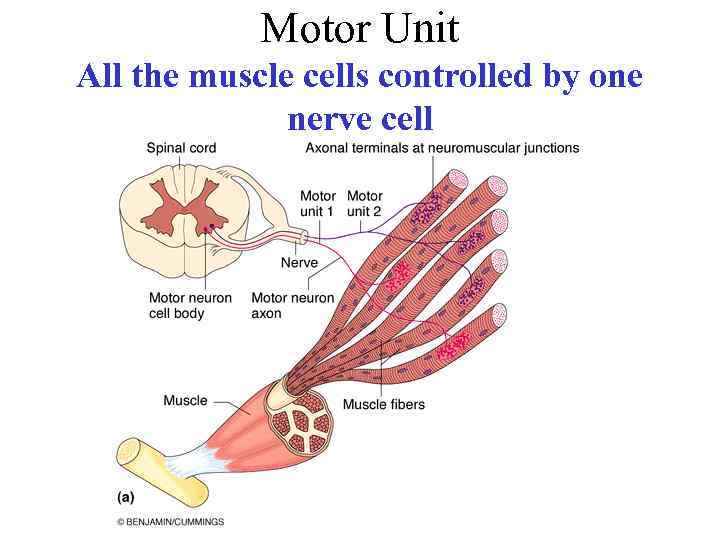 Motor Unit All the muscle cells controlled by one nerve cell
Motor Unit All the muscle cells controlled by one nerve cell
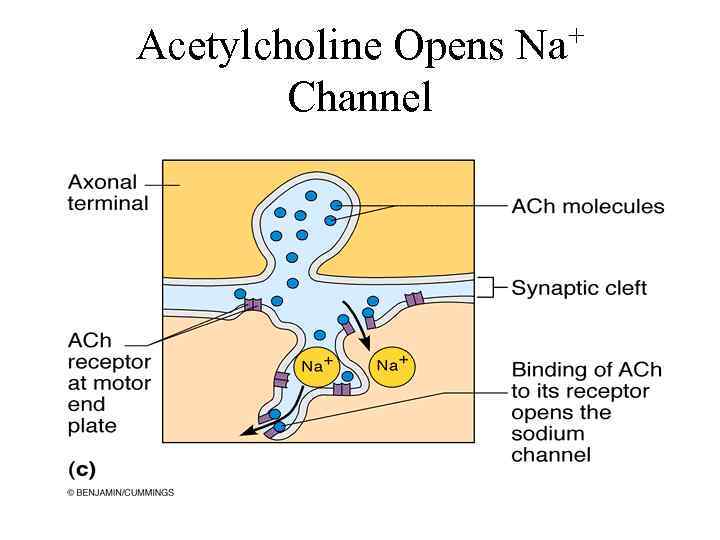 Acetylcholine Opens Na+ Channel
Acetylcholine Opens Na+ Channel
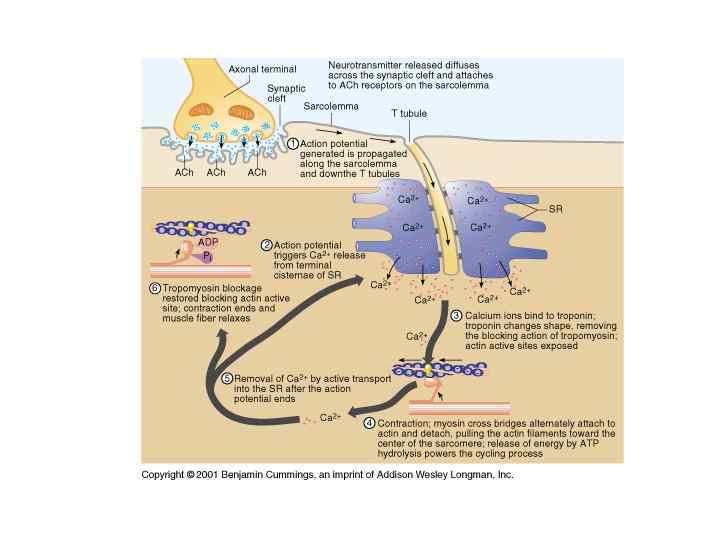
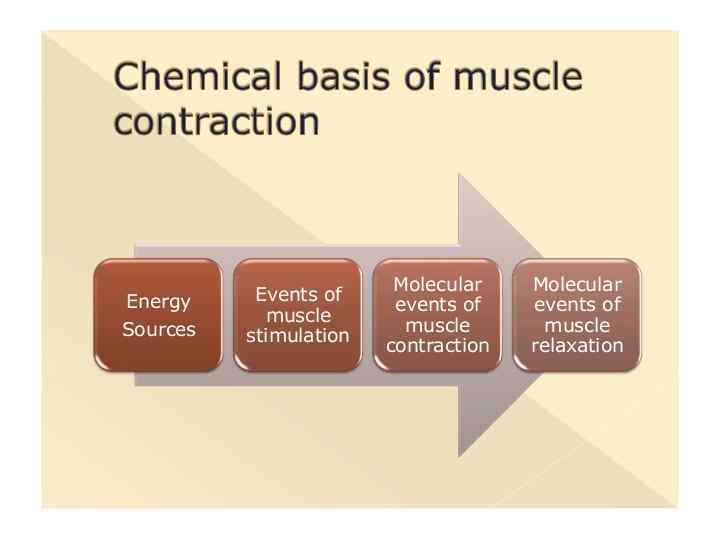
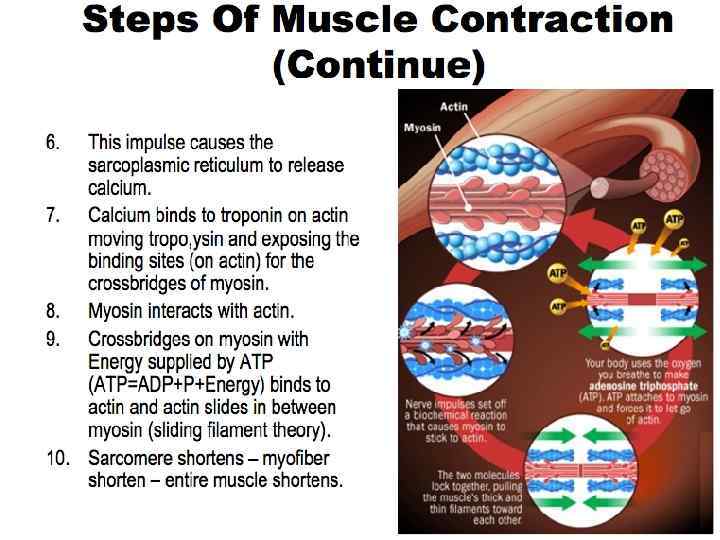
 Muscle Contraction Summary • Nerve impulse reaches myoneural junction • Acetylcholine is released from motor neuron • Ach binds with receptors in the muscle membrane to allow sodium to enter • Sodium influx will generate an action potential in the sarcolemma
Muscle Contraction Summary • Nerve impulse reaches myoneural junction • Acetylcholine is released from motor neuron • Ach binds with receptors in the muscle membrane to allow sodium to enter • Sodium influx will generate an action potential in the sarcolemma
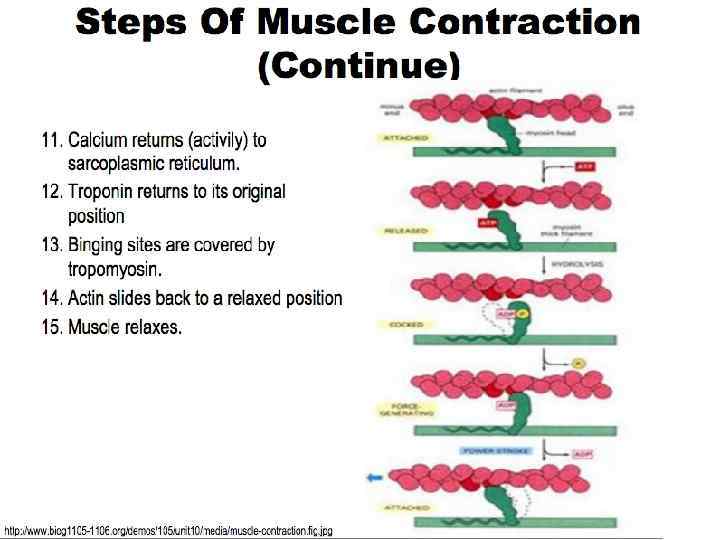
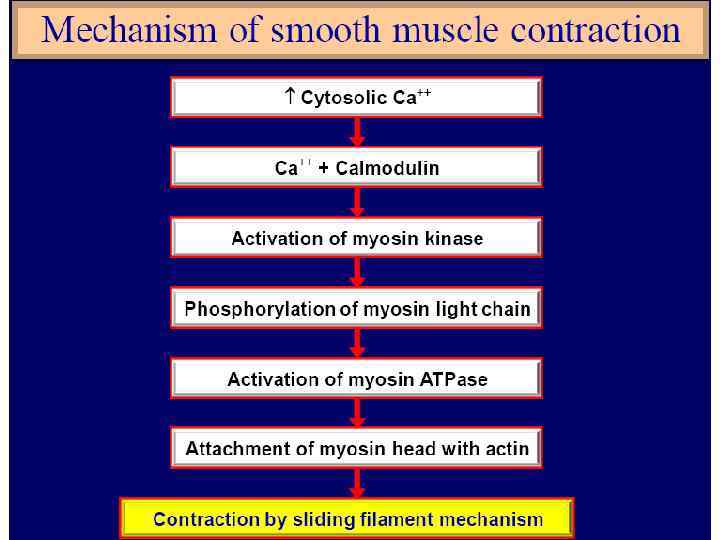
 Muscle Contraction (Cont’d) • Action potential travels down T tubule • Sarcoplamic reticulum releases calcium • Calcium binds with troponin to move the troponin, tropomyosin complex • Binding sites in the actin filament are exposed
Muscle Contraction (Cont’d) • Action potential travels down T tubule • Sarcoplamic reticulum releases calcium • Calcium binds with troponin to move the troponin, tropomyosin complex • Binding sites in the actin filament are exposed
 Muscle Contraction (cont’d) • Myosin head attach to binding sites and create a power stroke • ATP detaches myosin heads and energizes them for another contaction • When action potentials cease the muscle stop contracting
Muscle Contraction (cont’d) • Myosin head attach to binding sites and create a power stroke • ATP detaches myosin heads and energizes them for another contaction • When action potentials cease the muscle stop contracting
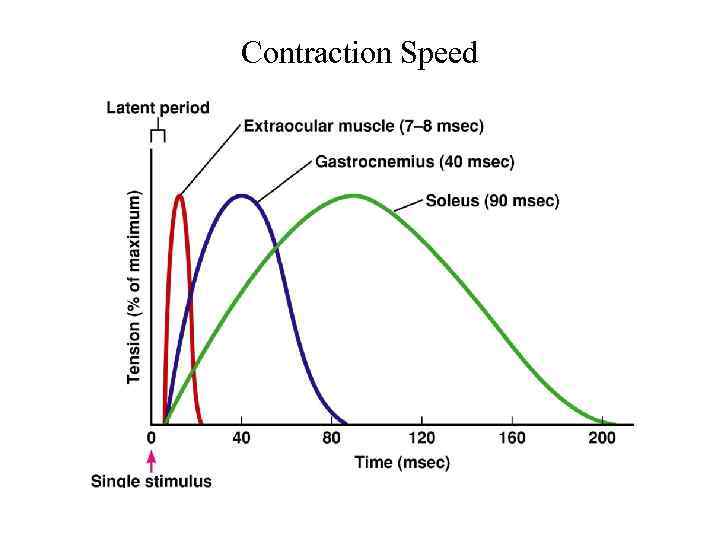 Contraction Speed
Contraction Speed
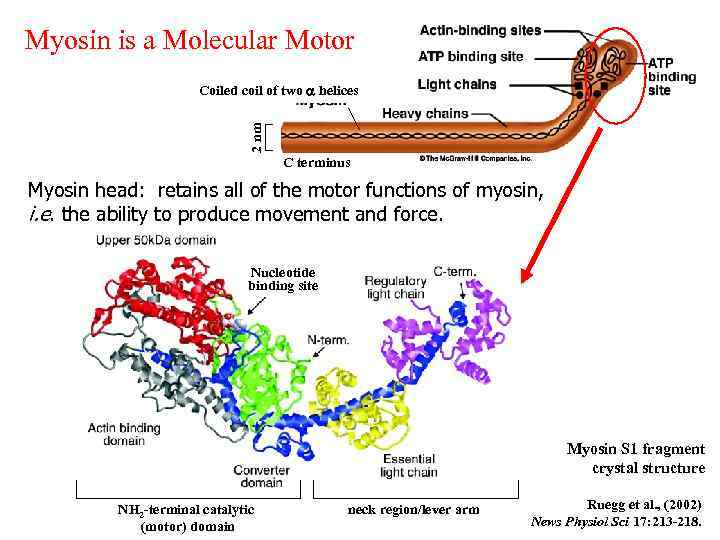 Myosin is a Molecular Motor Myosin is a hexamer: 2 myosin heavy chains 4 myosin light chains 2 nm Coiled coil of two a helices C terminus Myosin head: retains all of the motor functions of myosin, i. e. the ability to produce movement and force. Nucleotide binding site Myosin S 1 fragment crystal structure NH 2 -terminal catalytic (motor) domain neck region/lever arm Ruegg et al. , (2002) News Physiol Sci 17: 213 -218.
Myosin is a Molecular Motor Myosin is a hexamer: 2 myosin heavy chains 4 myosin light chains 2 nm Coiled coil of two a helices C terminus Myosin head: retains all of the motor functions of myosin, i. e. the ability to produce movement and force. Nucleotide binding site Myosin S 1 fragment crystal structure NH 2 -terminal catalytic (motor) domain neck region/lever arm Ruegg et al. , (2002) News Physiol Sci 17: 213 -218.
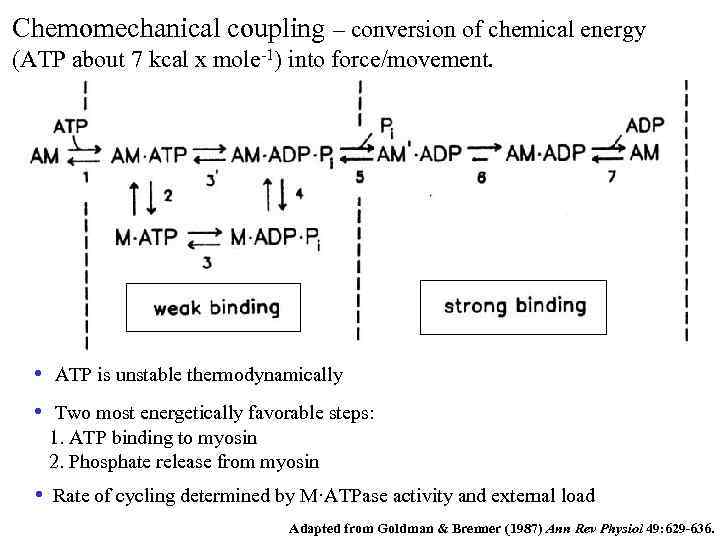 Chemomechanical coupling – conversion of chemical energy (ATP about 7 kcal x mole-1) into force/movement. • ATP is unstable thermodynamically • Two most energetically favorable steps: 1. ATP binding to myosin 2. Phosphate release from myosin • Rate of cycling determined by M·ATPase activity and external load Adapted from Goldman & Brenner (1987) Ann Rev Physiol 49: 629 -636.
Chemomechanical coupling – conversion of chemical energy (ATP about 7 kcal x mole-1) into force/movement. • ATP is unstable thermodynamically • Two most energetically favorable steps: 1. ATP binding to myosin 2. Phosphate release from myosin • Rate of cycling determined by M·ATPase activity and external load Adapted from Goldman & Brenner (1987) Ann Rev Physiol 49: 629 -636.
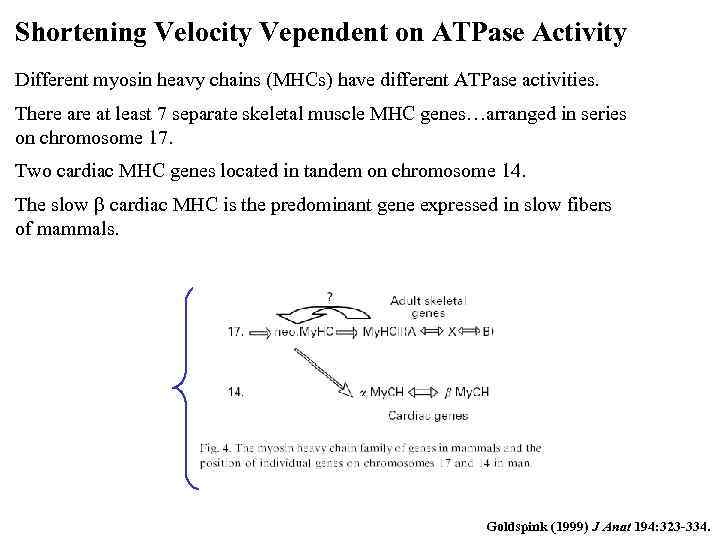 Shortening Velocity Vependent on ATPase Activity Different myosin heavy chains (MHCs) have different ATPase activities. There at least 7 separate skeletal muscle MHC genes…arranged in series on chromosome 17. Two cardiac MHC genes located in tandem on chromosome 14. The slow b cardiac MHC is the predominant gene expressed in slow fibers of mammals. Goldspink (1999) J Anat 194: 323 -334.
Shortening Velocity Vependent on ATPase Activity Different myosin heavy chains (MHCs) have different ATPase activities. There at least 7 separate skeletal muscle MHC genes…arranged in series on chromosome 17. Two cardiac MHC genes located in tandem on chromosome 14. The slow b cardiac MHC is the predominant gene expressed in slow fibers of mammals. Goldspink (1999) J Anat 194: 323 -334.
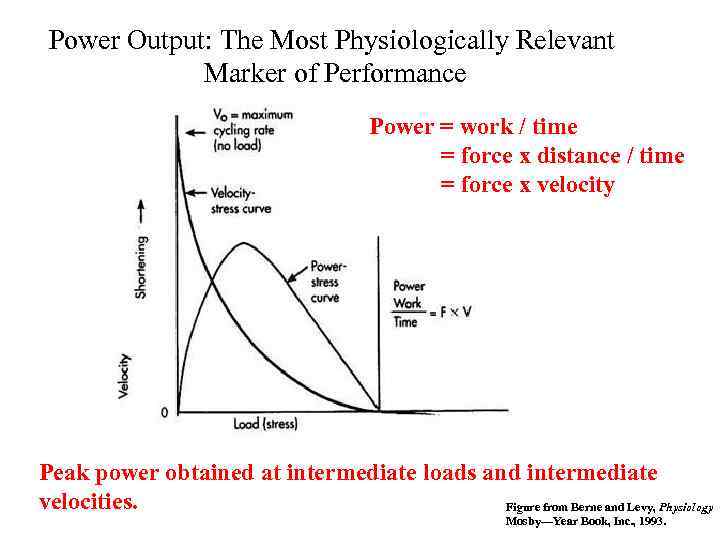 Power Output: The Most Physiologically Relevant Marker of Performance Power = work / time = force x distance / time = force x velocity Peak power obtained at intermediate loads and intermediate velocities. Figure from Berne and Levy, Physiology Mosby—Year Book, Inc. , 1993.
Power Output: The Most Physiologically Relevant Marker of Performance Power = work / time = force x distance / time = force x velocity Peak power obtained at intermediate loads and intermediate velocities. Figure from Berne and Levy, Physiology Mosby—Year Book, Inc. , 1993.
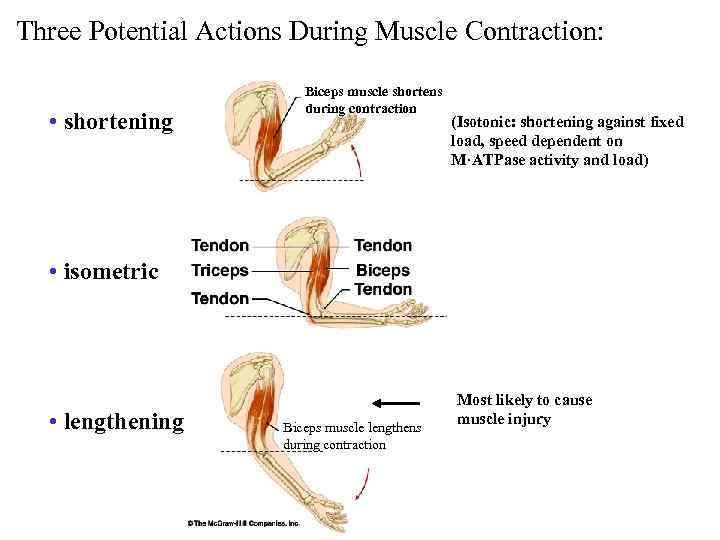 Three Potential Actions During Muscle Contraction: • shortening Biceps muscle shortens during contraction (Isotonic: shortening against fixed load, speed dependent on M·ATPase activity and load) • isometric • lengthening Biceps muscle lengthens during contraction Most likely to cause muscle injury
Three Potential Actions During Muscle Contraction: • shortening Biceps muscle shortens during contraction (Isotonic: shortening against fixed load, speed dependent on M·ATPase activity and load) • isometric • lengthening Biceps muscle lengthens during contraction Most likely to cause muscle injury
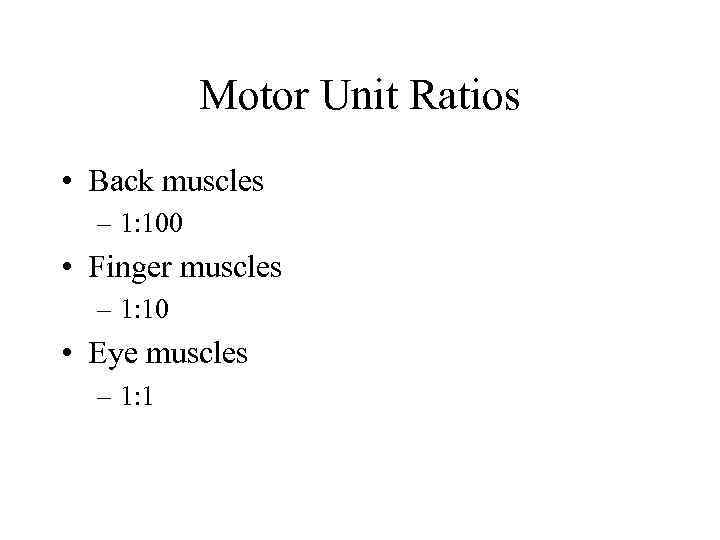 Motor Unit Ratios • Back muscles – 1: 100 • Finger muscles – 1: 10 • Eye muscles – 1: 1
Motor Unit Ratios • Back muscles – 1: 100 • Finger muscles – 1: 10 • Eye muscles – 1: 1
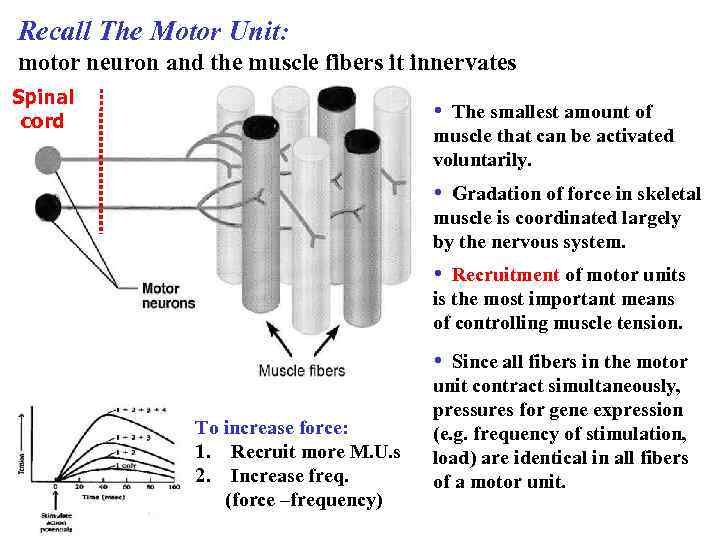 Recall The Motor Unit: motor neuron and the muscle fibers it innervates Spinal cord • The smallest amount of muscle that can be activated voluntarily. • Gradation of force in skeletal muscle is coordinated largely by the nervous system. • Recruitment of motor units is the most important means of controlling muscle tension. • Since all fibers in the motor To increase force: 1. Recruit more M. U. s 2. Increase freq. (force –frequency) unit contract simultaneously, pressures for gene expression (e. g. frequency of stimulation, load) are identical in all fibers of a motor unit.
Recall The Motor Unit: motor neuron and the muscle fibers it innervates Spinal cord • The smallest amount of muscle that can be activated voluntarily. • Gradation of force in skeletal muscle is coordinated largely by the nervous system. • Recruitment of motor units is the most important means of controlling muscle tension. • Since all fibers in the motor To increase force: 1. Recruit more M. U. s 2. Increase freq. (force –frequency) unit contract simultaneously, pressures for gene expression (e. g. frequency of stimulation, load) are identical in all fibers of a motor unit.
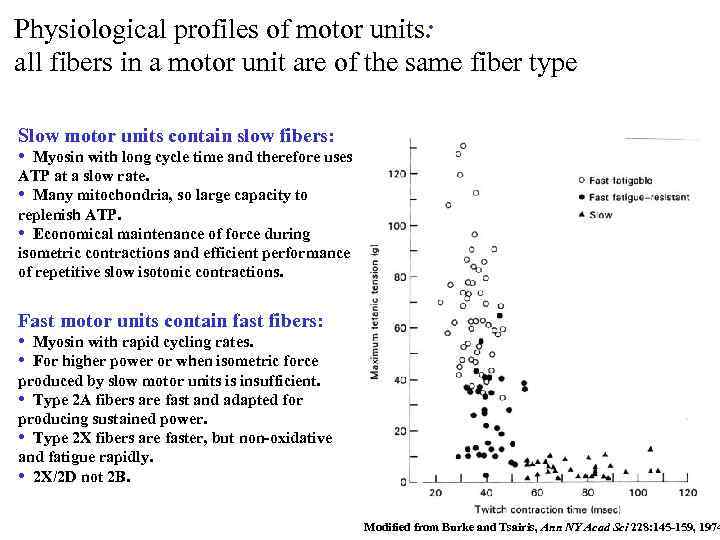 Physiological profiles of motor units: all fibers in a motor unit are of the same fiber type Slow motor units contain slow fibers: • Myosin with long cycle time and therefore uses ATP at a slow rate. • Many mitochondria, so large capacity to replenish ATP. • Economical maintenance of force during isometric contractions and efficient performance of repetitive slow isotonic contractions. Fast motor units contain fast fibers: • Myosin with rapid cycling rates. • For higher power or when isometric force produced by slow motor units is insufficient. • Type 2 A fibers are fast and adapted for producing sustained power. • Type 2 X fibers are faster, but non-oxidative and fatigue rapidly. • 2 X/2 D not 2 B. Modified from Burke and Tsairis, Ann NY Acad Sci 228: 145 -159, 1974
Physiological profiles of motor units: all fibers in a motor unit are of the same fiber type Slow motor units contain slow fibers: • Myosin with long cycle time and therefore uses ATP at a slow rate. • Many mitochondria, so large capacity to replenish ATP. • Economical maintenance of force during isometric contractions and efficient performance of repetitive slow isotonic contractions. Fast motor units contain fast fibers: • Myosin with rapid cycling rates. • For higher power or when isometric force produced by slow motor units is insufficient. • Type 2 A fibers are fast and adapted for producing sustained power. • Type 2 X fibers are faster, but non-oxidative and fatigue rapidly. • 2 X/2 D not 2 B. Modified from Burke and Tsairis, Ann NY Acad Sci 228: 145 -159, 1974
 Increased use: strength training Early gains in strength appear to be predominantly due to neural factors…optimizing recruitment patterns. Long term gains almost solely the result of hypertrophy i. e. increased size.
Increased use: strength training Early gains in strength appear to be predominantly due to neural factors…optimizing recruitment patterns. Long term gains almost solely the result of hypertrophy i. e. increased size.
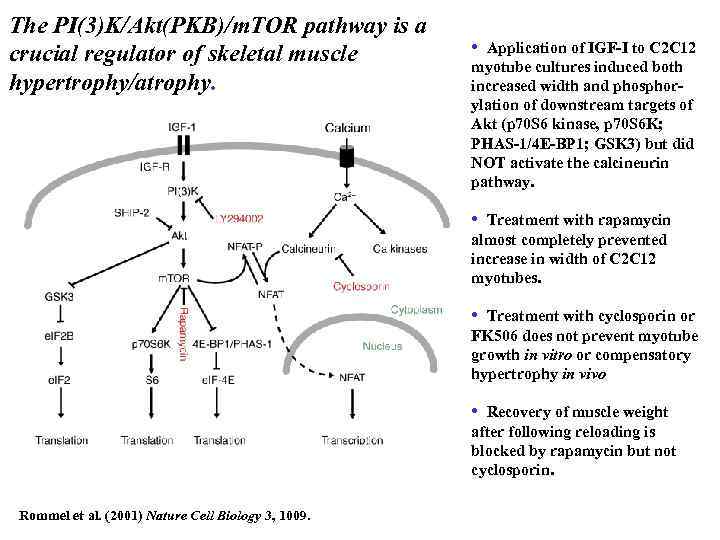 The PI(3)K/Akt(PKB)/m. TOR pathway is a crucial regulator of skeletal muscle hypertrophy/atrophy. • Application of IGF-I to C 2 C 12 myotube cultures induced both increased width and phosphorylation of downstream targets of Akt (p 70 S 6 kinase, p 70 S 6 K; PHAS-1/4 E-BP 1; GSK 3) but did NOT activate the calcineurin pathway. • Treatment with rapamycin almost completely prevented increase in width of C 2 C 12 myotubes. • Treatment with cyclosporin or FK 506 does not prevent myotube growth in vitro or compensatory hypertrophy in vivo • Recovery of muscle weight after following reloading is blocked by rapamycin but not cyclosporin. Rommel et al. (2001) Nature Cell Biology 3, 1009.
The PI(3)K/Akt(PKB)/m. TOR pathway is a crucial regulator of skeletal muscle hypertrophy/atrophy. • Application of IGF-I to C 2 C 12 myotube cultures induced both increased width and phosphorylation of downstream targets of Akt (p 70 S 6 kinase, p 70 S 6 K; PHAS-1/4 E-BP 1; GSK 3) but did NOT activate the calcineurin pathway. • Treatment with rapamycin almost completely prevented increase in width of C 2 C 12 myotubes. • Treatment with cyclosporin or FK 506 does not prevent myotube growth in vitro or compensatory hypertrophy in vivo • Recovery of muscle weight after following reloading is blocked by rapamycin but not cyclosporin. Rommel et al. (2001) Nature Cell Biology 3, 1009.
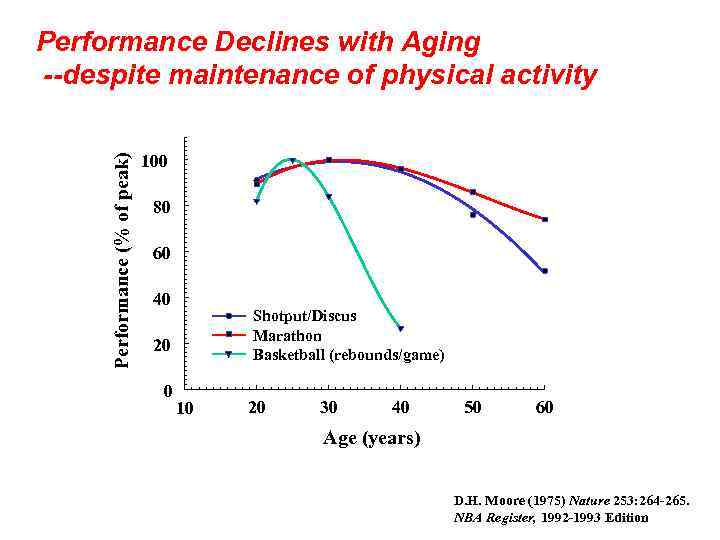 Performance (% of peak) Performance Declines with Aging --despite maintenance of physical activity 100 80 60 40 Shotput/Discus Marathon Basketball (rebounds/game) 20 0 10 20 30 40 50 60 Age (years) D. H. Moore (1975) Nature 253: 264 -265. NBA Register, 1992 -1993 Edition
Performance (% of peak) Performance Declines with Aging --despite maintenance of physical activity 100 80 60 40 Shotput/Discus Marathon Basketball (rebounds/game) 20 0 10 20 30 40 50 60 Age (years) D. H. Moore (1975) Nature 253: 264 -265. NBA Register, 1992 -1993 Edition
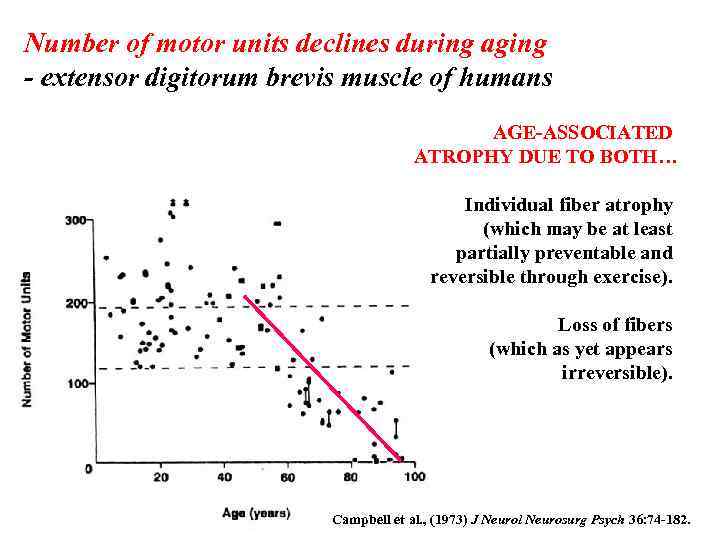 Number of motor units declines during aging - extensor digitorum brevis muscle of humans AGE-ASSOCIATED ATROPHY DUE TO BOTH… Individual fiber atrophy (which may be at least partially preventable and reversible through exercise). Loss of fibers (which as yet appears irreversible). Campbell et al. , (1973) J Neurol Neurosurg Psych 36: 74 -182.
Number of motor units declines during aging - extensor digitorum brevis muscle of humans AGE-ASSOCIATED ATROPHY DUE TO BOTH… Individual fiber atrophy (which may be at least partially preventable and reversible through exercise). Loss of fibers (which as yet appears irreversible). Campbell et al. , (1973) J Neurol Neurosurg Psych 36: 74 -182.
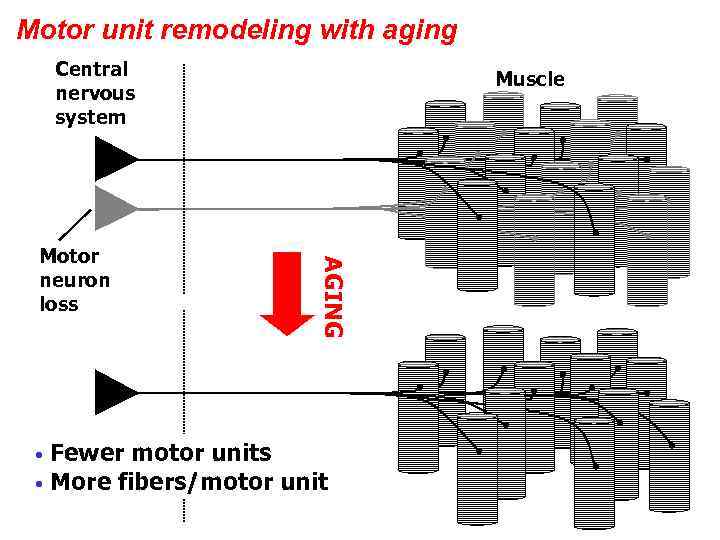 Motor unit remodeling with aging Central nervous system AGING Motor neuron loss Muscle Fewer motor units • More fibers/motor unit •
Motor unit remodeling with aging Central nervous system AGING Motor neuron loss Muscle Fewer motor units • More fibers/motor unit •
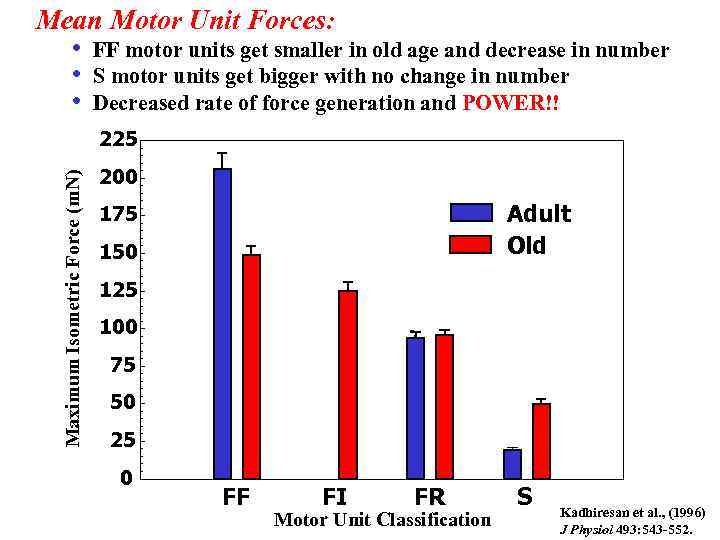 Mean Motor Unit Forces: • FF motor units get smaller in old age and decrease in number • S motor units get bigger with no change in number • Decreased rate of force generation and POWER!! Maximum Isometric Force (m. N) 225 200 Adult Old 175 150 125 100 75 50 25 0 FF FI FR Motor Unit Classification S Kadhiresan et al. , (1996) J Physiol 493: 543 -552.
Mean Motor Unit Forces: • FF motor units get smaller in old age and decrease in number • S motor units get bigger with no change in number • Decreased rate of force generation and POWER!! Maximum Isometric Force (m. N) 225 200 Adult Old 175 150 125 100 75 50 25 0 FF FI FR Motor Unit Classification S Kadhiresan et al. , (1996) J Physiol 493: 543 -552.
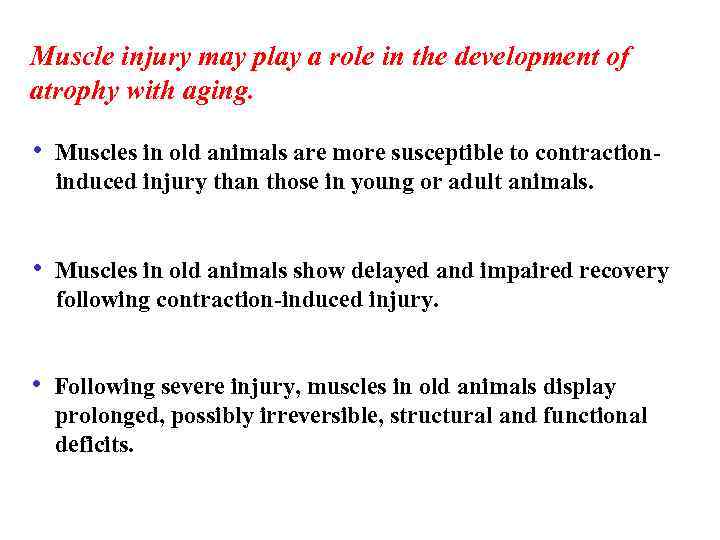 Muscle injury may play a role in the development of atrophy with aging. • Muscles in old animals are more susceptible to contraction induced injury than those in young or adult animals. • Muscles in old animals show delayed and impaired recovery following contraction-induced injury. • Following severe injury, muscles in old animals display prolonged, possibly irreversible, structural and functional deficits.
Muscle injury may play a role in the development of atrophy with aging. • Muscles in old animals are more susceptible to contraction induced injury than those in young or adult animals. • Muscles in old animals show delayed and impaired recovery following contraction-induced injury. • Following severe injury, muscles in old animals display prolonged, possibly irreversible, structural and functional deficits.
 Disorders of Muscle Tissue • Muscle tissues experience few disorders – Heart muscle is the exception – Skeletal muscle – remarkably resistant to infection – Smooth muscle – problems stem from external irritants
Disorders of Muscle Tissue • Muscle tissues experience few disorders – Heart muscle is the exception – Skeletal muscle – remarkably resistant to infection – Smooth muscle – problems stem from external irritants
 Disorders of Muscle Tissue • Muscular dystrophy – a group of inherited muscle destroying disease – Affected muscles enlarge with fat and connective tissue – Muscles degenerate • Types of muscular dystrophy – Duchenne muscular dystrophy – Myotonic dystrophy
Disorders of Muscle Tissue • Muscular dystrophy – a group of inherited muscle destroying disease – Affected muscles enlarge with fat and connective tissue – Muscles degenerate • Types of muscular dystrophy – Duchenne muscular dystrophy – Myotonic dystrophy
 Disorders of Muscle Tissue • Myofascial pain syndrome – pain is caused by tightened bands of muscle fibers • Fibromyalgia – a mysterious chronic-pain syndrome – Affects mostly women – Symptoms – fatigue, sleep abnormalities, severe musculoskeletal pain, and headache
Disorders of Muscle Tissue • Myofascial pain syndrome – pain is caused by tightened bands of muscle fibers • Fibromyalgia – a mysterious chronic-pain syndrome – Affects mostly women – Symptoms – fatigue, sleep abnormalities, severe musculoskeletal pain, and headache
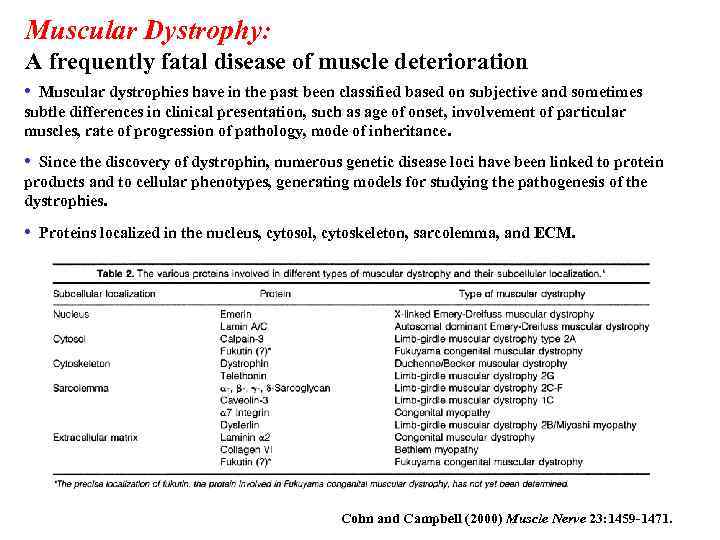 Muscular Dystrophy: A frequently fatal disease of muscle deterioration • Muscular dystrophies have in the past been classified based on subjective and sometimes subtle differences in clinical presentation, such as age of onset, involvement of particular muscles, rate of progression of pathology, mode of inheritance. • Since the discovery of dystrophin, numerous genetic disease loci have been linked to protein products and to cellular phenotypes, generating models for studying the pathogenesis of the dystrophies. • Proteins localized in the nucleus, cytosol, cytoskeleton, sarcolemma, and ECM. Cohn and Campbell (2000) Muscle Nerve 23: 1459 -1471.
Muscular Dystrophy: A frequently fatal disease of muscle deterioration • Muscular dystrophies have in the past been classified based on subjective and sometimes subtle differences in clinical presentation, such as age of onset, involvement of particular muscles, rate of progression of pathology, mode of inheritance. • Since the discovery of dystrophin, numerous genetic disease loci have been linked to protein products and to cellular phenotypes, generating models for studying the pathogenesis of the dystrophies. • Proteins localized in the nucleus, cytosol, cytoskeleton, sarcolemma, and ECM. Cohn and Campbell (2000) Muscle Nerve 23: 1459 -1471.
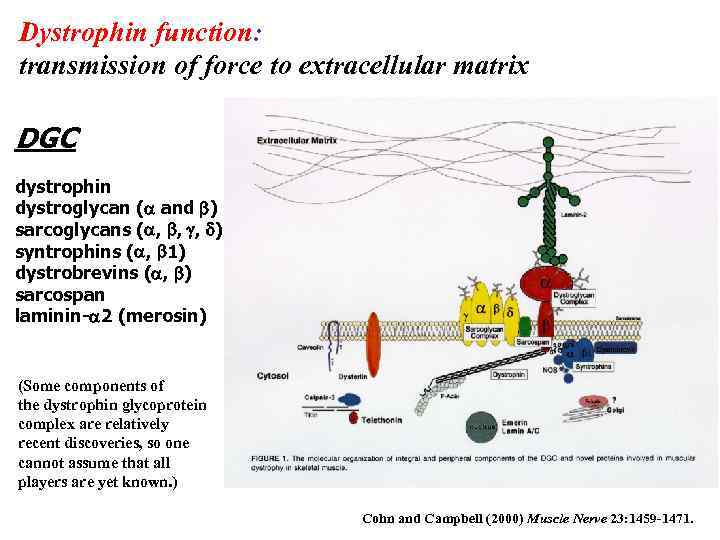 Dystrophin function: transmission of force to extracellular matrix DGC dystrophin dystroglycan (a and b) sarcoglycans (a, b, g, d) syntrophins (a, b 1) dystrobrevins (a, b) sarcospan laminin-a 2 (merosin) (Some components of the dystrophin glycoprotein complex are relatively recent discoveries, so one cannot assume that all players are yet known. ) Cohn and Campbell (2000) Muscle Nerve 23: 1459 -1471.
Dystrophin function: transmission of force to extracellular matrix DGC dystrophin dystroglycan (a and b) sarcoglycans (a, b, g, d) syntrophins (a, b 1) dystrobrevins (a, b) sarcospan laminin-a 2 (merosin) (Some components of the dystrophin glycoprotein complex are relatively recent discoveries, so one cannot assume that all players are yet known. ) Cohn and Campbell (2000) Muscle Nerve 23: 1459 -1471.
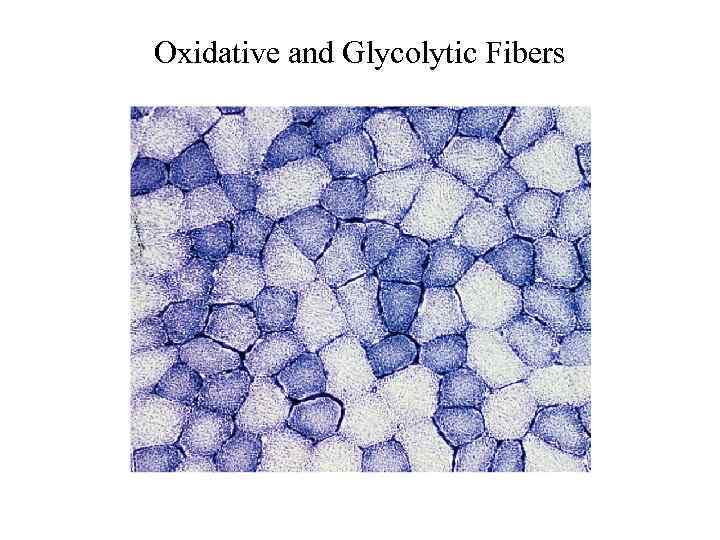 Oxidative and Glycolytic Fibers
Oxidative and Glycolytic Fibers
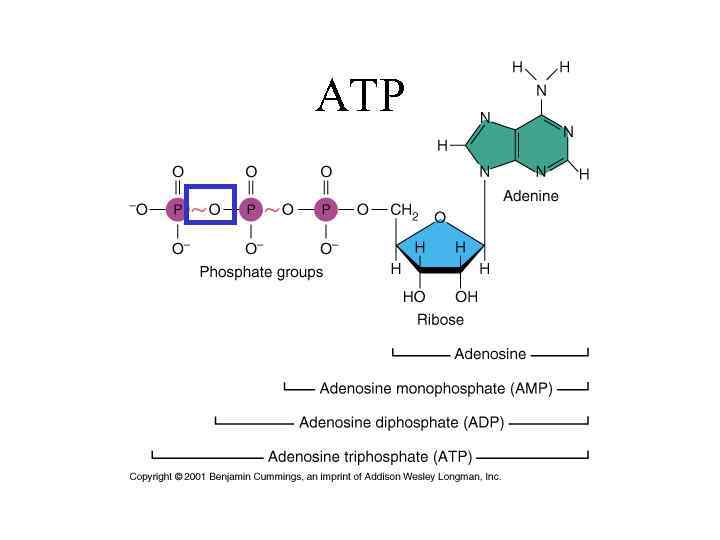 ATP
ATP
 Creatine • Molecule capable of storing ATP energy Creatine + ATP Creatine phosphate + ADP
Creatine • Molecule capable of storing ATP energy Creatine + ATP Creatine phosphate + ADP
 Creatine Phosphate • Molecule with stored ATP energy Creatine phosphate + ADP Creatine + ATP
Creatine Phosphate • Molecule with stored ATP energy Creatine phosphate + ADP Creatine + ATP
 Muscle Fatigue • Lack of oxygen causes ATP deficit • Lactic acid builds up from anaerobic respiration
Muscle Fatigue • Lack of oxygen causes ATP deficit • Lactic acid builds up from anaerobic respiration
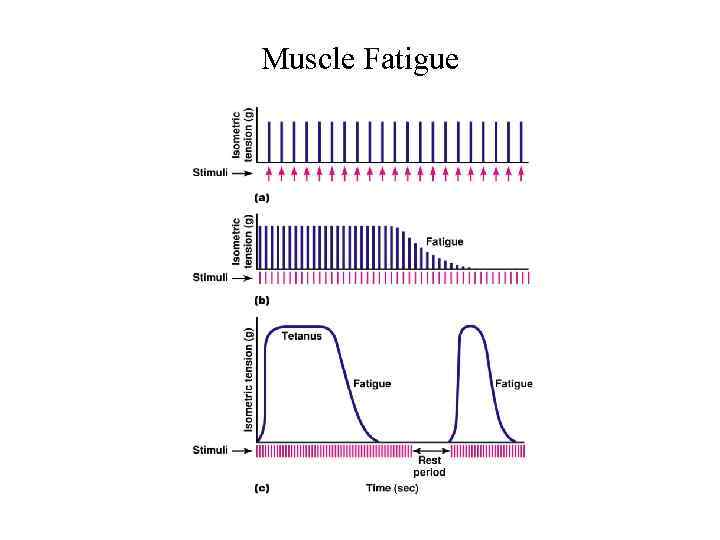 Muscle Fatigue
Muscle Fatigue
 Muscle Atrophy • Weakening and shrinking of a muscle • May be caused – Immobilization – Loss of neural stimulation
Muscle Atrophy • Weakening and shrinking of a muscle • May be caused – Immobilization – Loss of neural stimulation
 Muscle Hypertrophy • • Enlargement of a muscle More capillaries More mitochondria Caused by – Strenuous exercise – Steroid hormones
Muscle Hypertrophy • • Enlargement of a muscle More capillaries More mitochondria Caused by – Strenuous exercise – Steroid hormones
 Steroid Hormones • Stimulate muscle growth and hypertrophy
Steroid Hormones • Stimulate muscle growth and hypertrophy
 Muscle Tonus • Tightness of a muscle • Some fibers always contracted
Muscle Tonus • Tightness of a muscle • Some fibers always contracted
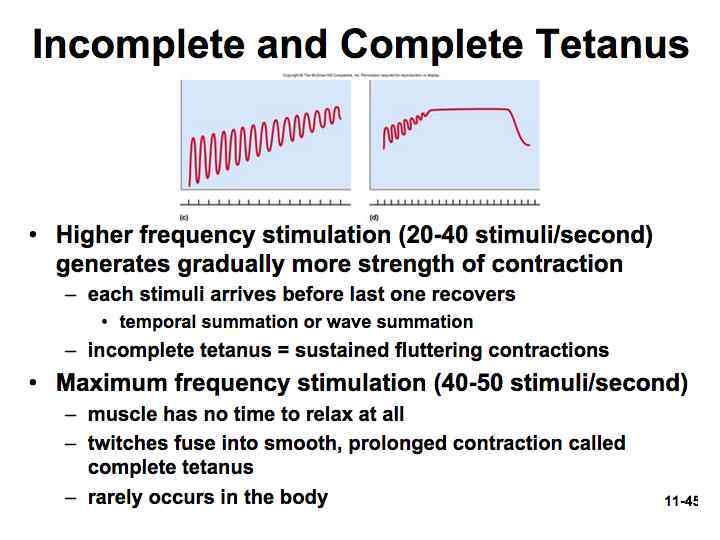
 Tetany • Sustained contraction of a muscle • Result of a rapid succession of nerve impulses
Tetany • Sustained contraction of a muscle • Result of a rapid succession of nerve impulses
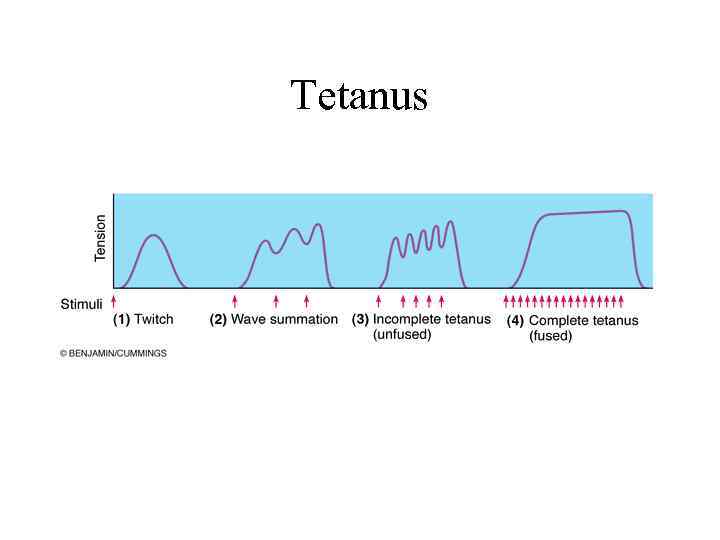 Tetanus
Tetanus
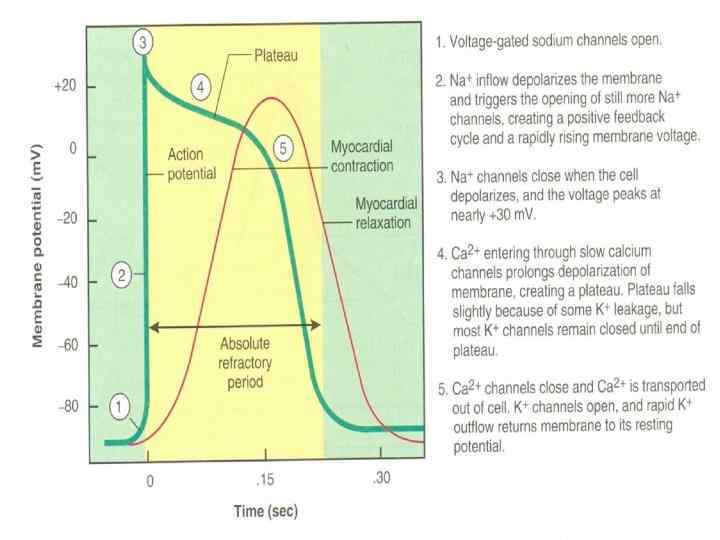
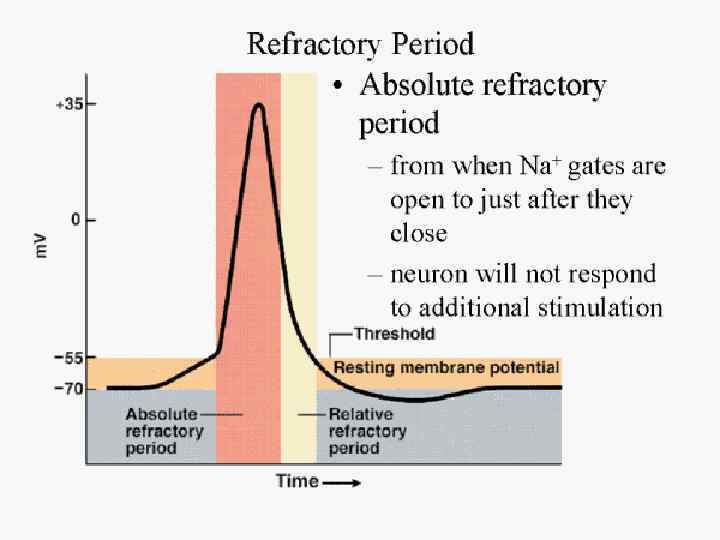
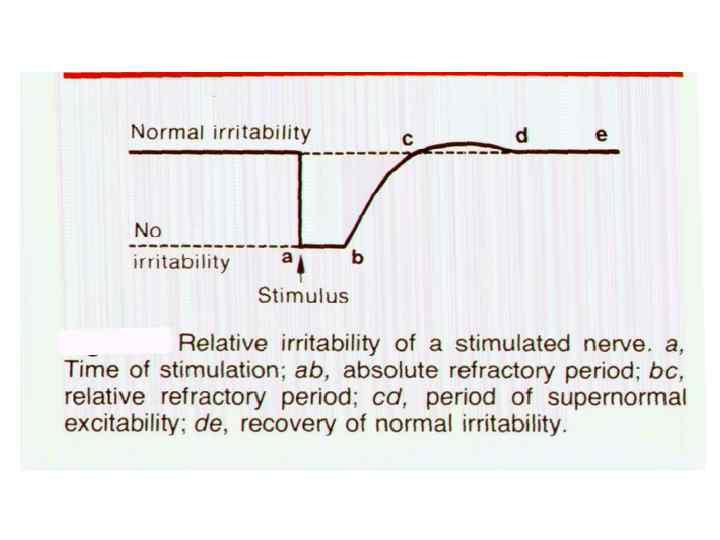
 Refractory Period • Brief period of time in which muscle cells will not respond to a stimulus
Refractory Period • Brief period of time in which muscle cells will not respond to a stimulus
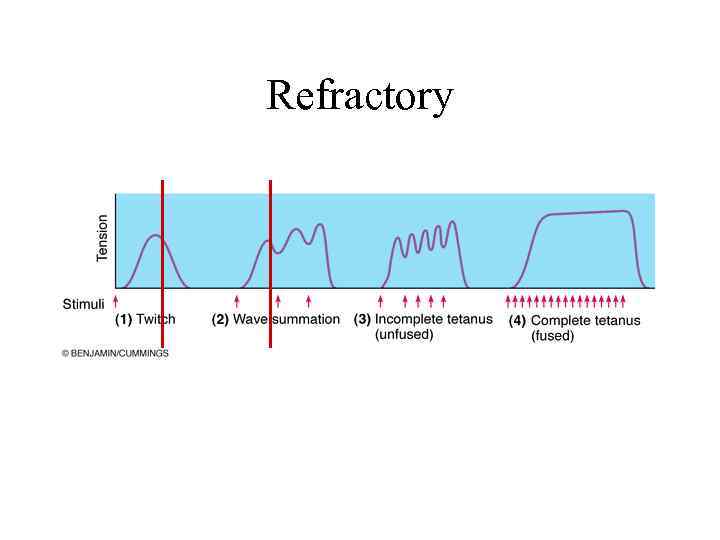 Refractory
Refractory
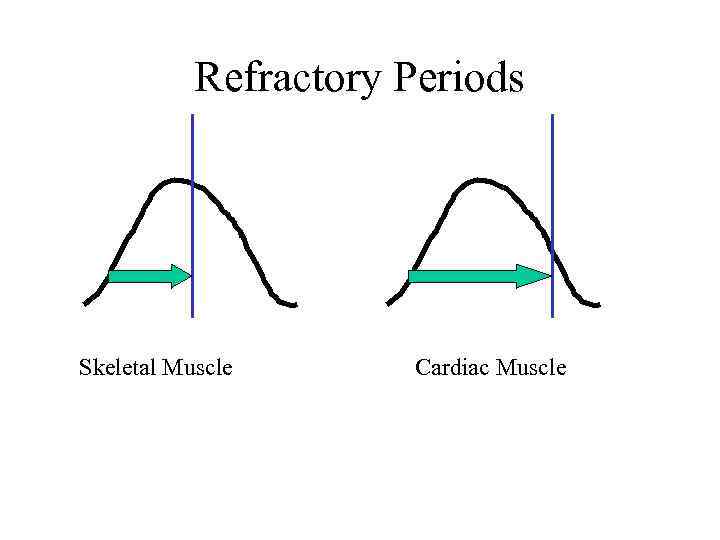 Refractory Periods Skeletal Muscle Cardiac Muscle
Refractory Periods Skeletal Muscle Cardiac Muscle
 Isometric Contraction • Produces no movement • Used in – Standing – Sitting – Posture
Isometric Contraction • Produces no movement • Used in – Standing – Sitting – Posture
 Isotonic Contraction • Produces movement • Used in – Walking – Moving any part of the body
Isotonic Contraction • Produces movement • Used in – Walking – Moving any part of the body
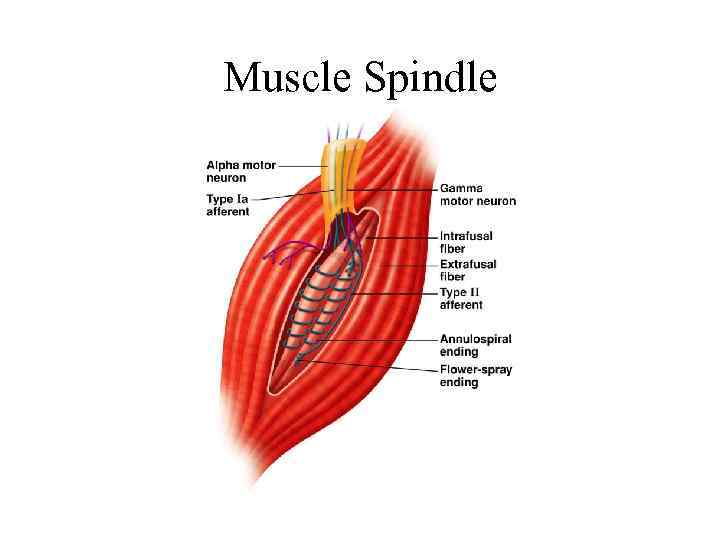 Muscle Spindle
Muscle Spindle
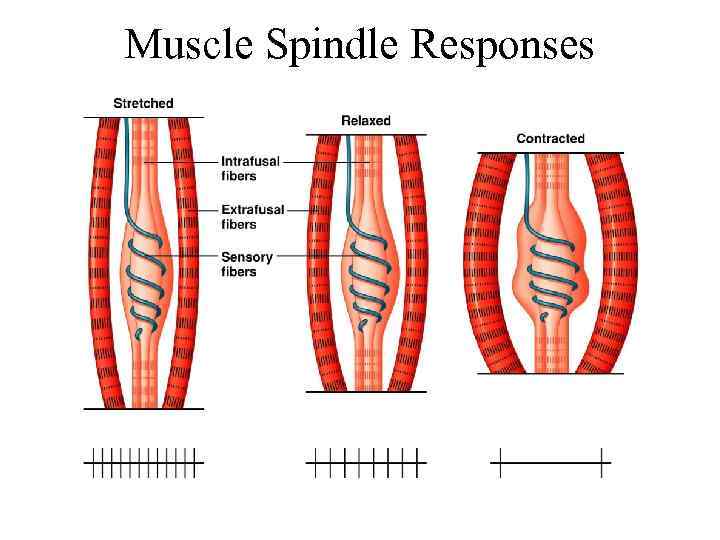 Muscle Spindle Responses
Muscle Spindle Responses
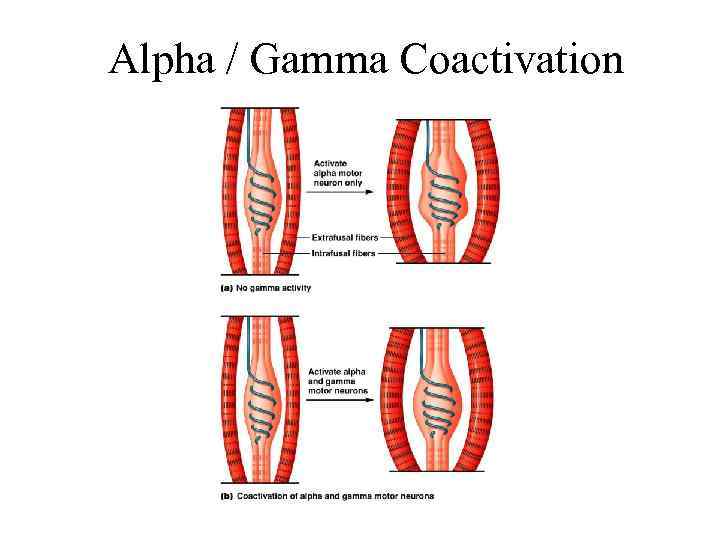 Alpha / Gamma Coactivation
Alpha / Gamma Coactivation
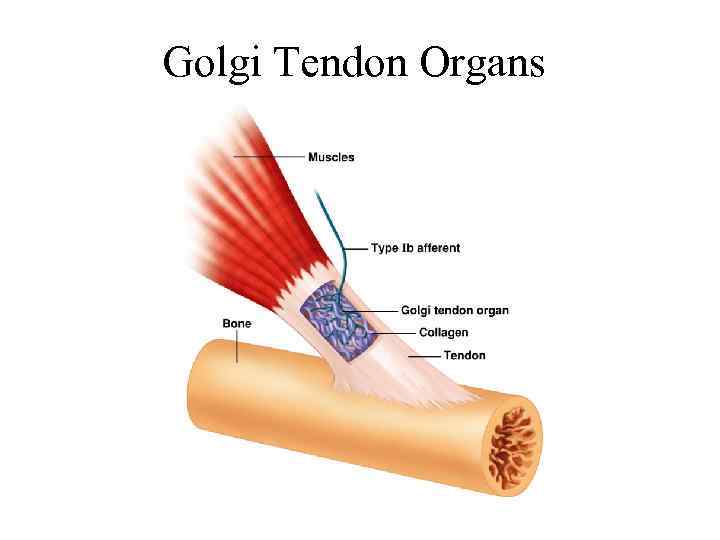 Golgi Tendon Organs
Golgi Tendon Organs
 Developmental Aspects: Regeneration • Cardiac and skeletal muscle become amitotic, but can lengthen and thicken • Myoblast-like satellite cells show very limited regenerative ability • Cardiac cells lack satellite cells • Smooth muscle has good regenerative ability • There is a biological basis for greater strength in men than in women • Women’s skeletal muscle makes up 36% of their body mass • Men’s skeletal muscle makes up 42% of their body mass
Developmental Aspects: Regeneration • Cardiac and skeletal muscle become amitotic, but can lengthen and thicken • Myoblast-like satellite cells show very limited regenerative ability • Cardiac cells lack satellite cells • Smooth muscle has good regenerative ability • There is a biological basis for greater strength in men than in women • Women’s skeletal muscle makes up 36% of their body mass • Men’s skeletal muscle makes up 42% of their body mass
 Developmental Aspects: Male and Female • These differences are due primarily to the male sex hormone testosterone • With more muscle mass, men are generally stronger than women • Body strength per unit muscle mass, however, is the same in both sexes
Developmental Aspects: Male and Female • These differences are due primarily to the male sex hormone testosterone • With more muscle mass, men are generally stronger than women • Body strength per unit muscle mass, however, is the same in both sexes
 Developmental Aspects: Age Related • With age, connective tissue increases and muscle fibers decrease • Muscles become stringier and more sinewy • By age 80, 50% of muscle mass is lost (sarcopenia) • Decreased density of capillaries in muscle • Reduced stamina • Increased recovery time • Regular exercise reverses sarcopenia
Developmental Aspects: Age Related • With age, connective tissue increases and muscle fibers decrease • Muscles become stringier and more sinewy • By age 80, 50% of muscle mass is lost (sarcopenia) • Decreased density of capillaries in muscle • Reduced stamina • Increased recovery time • Regular exercise reverses sarcopenia
 19 -116
19 -116
 19 -117
19 -117
 19 -118
19 -118
 19 -119
19 -119
 19 -120
19 -120
 19 -121
19 -121
 19 -122
19 -122
 19 -123
19 -123
 19 -124
19 -124
 19 -125
19 -125
 19 -126
19 -126
 19 -127
19 -127
 19 -128
19 -128
 19 -129
19 -129
 19 -130
19 -130
 19 -131
19 -131
 19 -132
19 -132
 19 -133
19 -133
 19 -134
19 -134
 135
135
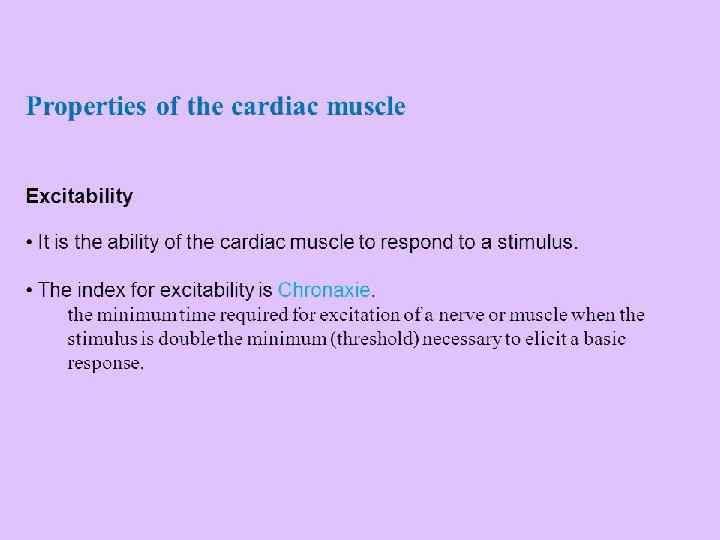
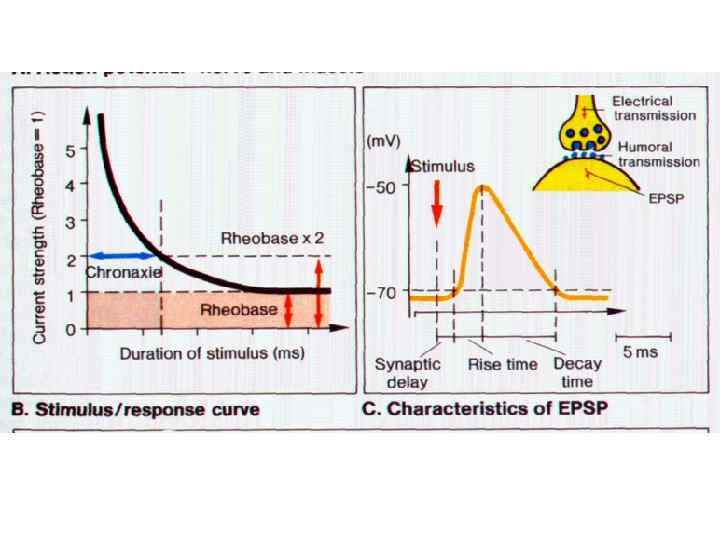
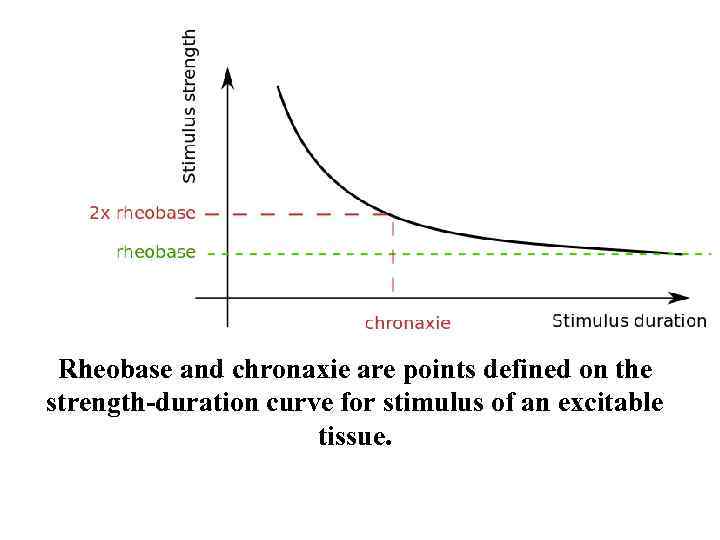 Rheobase and chronaxie are points defined on the strength-duration curve for stimulus of an excitable tissue.
Rheobase and chronaxie are points defined on the strength-duration curve for stimulus of an excitable tissue.
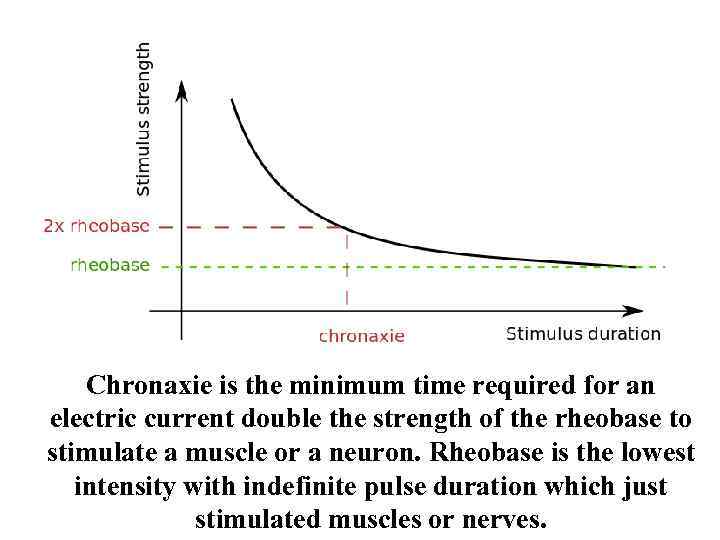 Chronaxie is the minimum time required for an electric current double the strength of the rheobase to stimulate a muscle or a neuron. Rheobase is the lowest intensity with indefinite pulse duration which just stimulated muscles or nerves.
Chronaxie is the minimum time required for an electric current double the strength of the rheobase to stimulate a muscle or a neuron. Rheobase is the lowest intensity with indefinite pulse duration which just stimulated muscles or nerves.
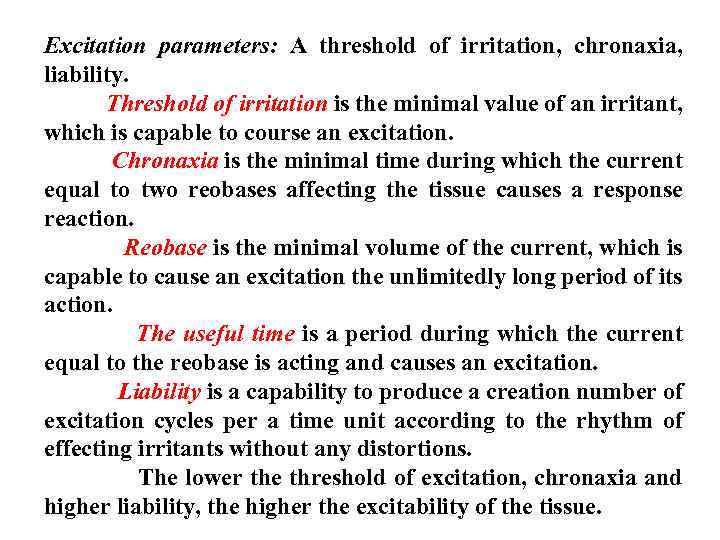 Excitation parameters: A threshold of irritation, chronaxia, liability. Threshold of irritation is the minimal value of an irritant, which is capable to course an excitation. Chronaxia is the minimal time during which the current equal to two reobases affecting the tissue causes a response reaction. Reobase is the minimal volume of the current, which is capable to cause an excitation the unlimitedly long period of its action. The useful time is a period during which the current equal to the reobase is acting and causes an excitation. Liability is a capability to produce a creation number of excitation cycles per a time unit according to the rhythm of effecting irritants without any distortions. The lower the threshold of excitation, chronaxia and higher liability, the higher the excitability of the tissue.
Excitation parameters: A threshold of irritation, chronaxia, liability. Threshold of irritation is the minimal value of an irritant, which is capable to course an excitation. Chronaxia is the minimal time during which the current equal to two reobases affecting the tissue causes a response reaction. Reobase is the minimal volume of the current, which is capable to cause an excitation the unlimitedly long period of its action. The useful time is a period during which the current equal to the reobase is acting and causes an excitation. Liability is a capability to produce a creation number of excitation cycles per a time unit according to the rhythm of effecting irritants without any distortions. The lower the threshold of excitation, chronaxia and higher liability, the higher the excitability of the tissue.
 Physiology as the science. Bioelectrical phenomena in excitable tissues
Physiology as the science. Bioelectrical phenomena in excitable tissues
 Defining of “physiology” notion • Physiology is the science about the regularities of organisms‘ vital activity in connection with the external environment.
Defining of “physiology” notion • Physiology is the science about the regularities of organisms‘ vital activity in connection with the external environment.
 Method of physiology • a) Observation • This is the method in which the scientists don‘t mix in course of vital processes. They only make use of vision and description of all changes. On the base of this changes they make conclusions. • b) Experiment • There are two kinds of experiments: acute and chronic. Acute experiment was doing with the helps of anesthesia. It may be accompanied by cut off the nerves, introduction the different substances. The chronic experiment was doing in vital animals, for example, after the acute experiment scientists can used the observation.
Method of physiology • a) Observation • This is the method in which the scientists don‘t mix in course of vital processes. They only make use of vision and description of all changes. On the base of this changes they make conclusions. • b) Experiment • There are two kinds of experiments: acute and chronic. Acute experiment was doing with the helps of anesthesia. It may be accompanied by cut off the nerves, introduction the different substances. The chronic experiment was doing in vital animals, for example, after the acute experiment scientists can used the observation.
 Method of physiology • c) Examination • This is the method of examine the patient with different diseases, for example, with using the different apparatuses. • d) Simulation • We can simulation different processes as a laboratory simulation or realistic simulation, for example, apparatus of artificial kidney or apparatus of artificial circulation. It may be the simulation the different processes by means of computers.
Method of physiology • c) Examination • This is the method of examine the patient with different diseases, for example, with using the different apparatuses. • d) Simulation • We can simulation different processes as a laboratory simulation or realistic simulation, for example, apparatus of artificial kidney or apparatus of artificial circulation. It may be the simulation the different processes by means of computers.
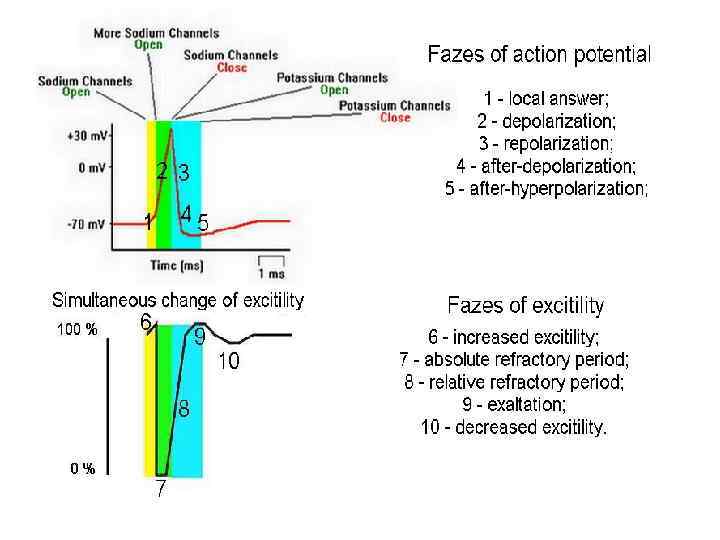
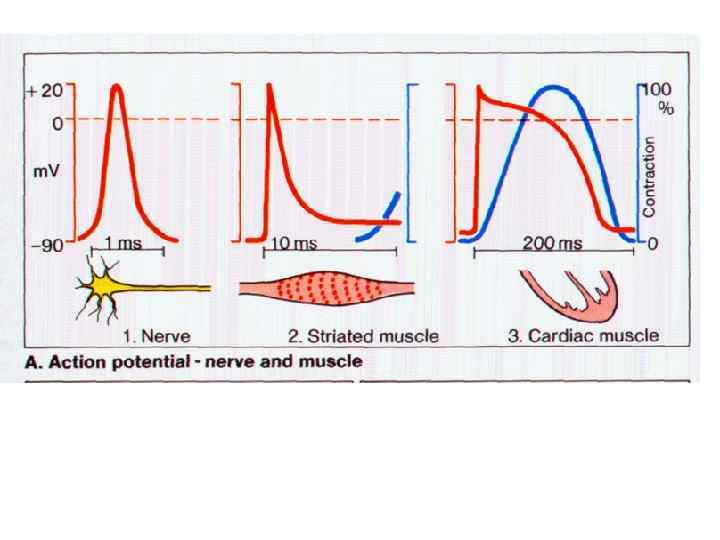
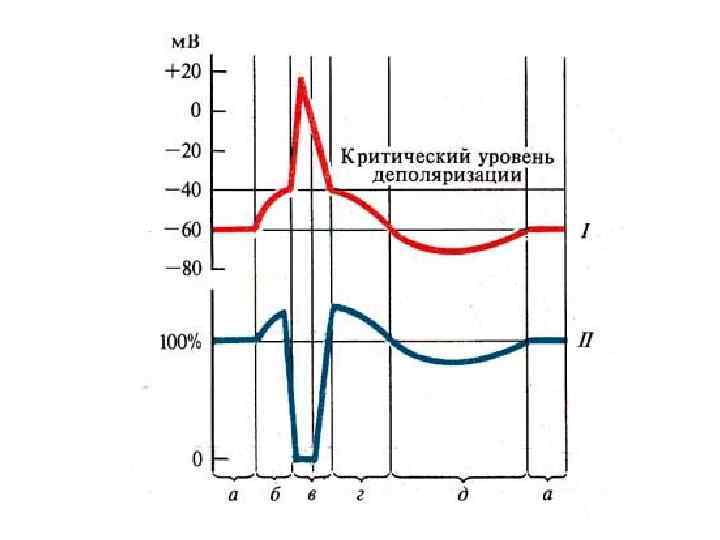
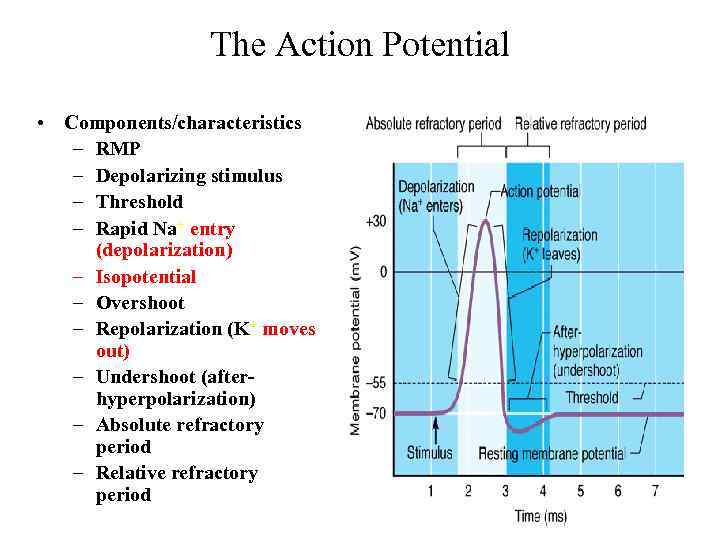 The Action Potential • Components/characteristics – RMP – Depolarizing stimulus – Threshold – Rapid Na+ entry (depolarization) – Isopotential – Overshoot – Repolarization (K+ moves out) – Undershoot (afterhyperpolarization) – Absolute refractory period – Relative refractory period
The Action Potential • Components/characteristics – RMP – Depolarizing stimulus – Threshold – Rapid Na+ entry (depolarization) – Isopotential – Overshoot – Repolarization (K+ moves out) – Undershoot (afterhyperpolarization) – Absolute refractory period – Relative refractory period
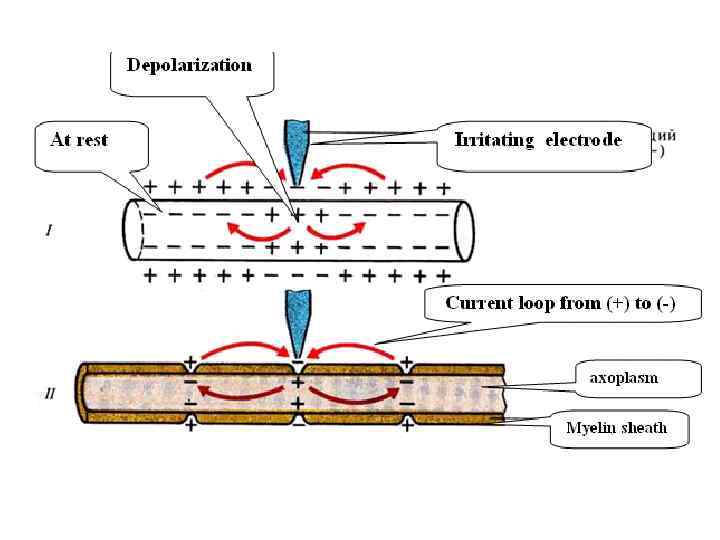
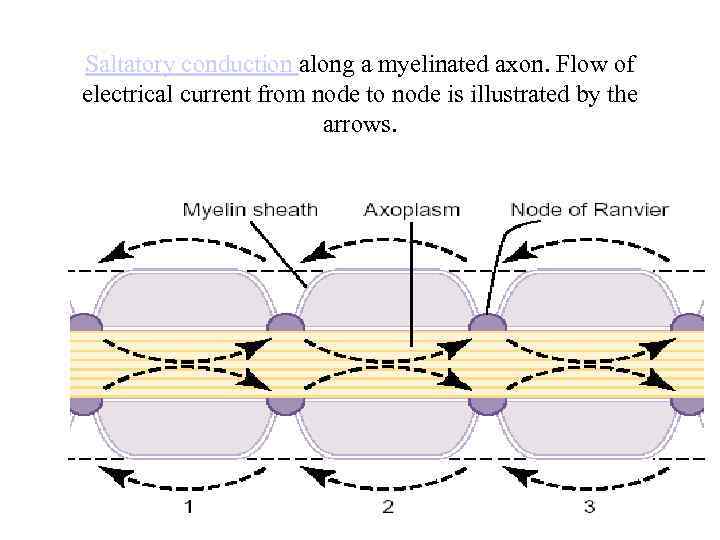 Saltatory conduction along a myelinated axon. Flow of electrical current from node to node is illustrated by the arrows.
Saltatory conduction along a myelinated axon. Flow of electrical current from node to node is illustrated by the arrows.
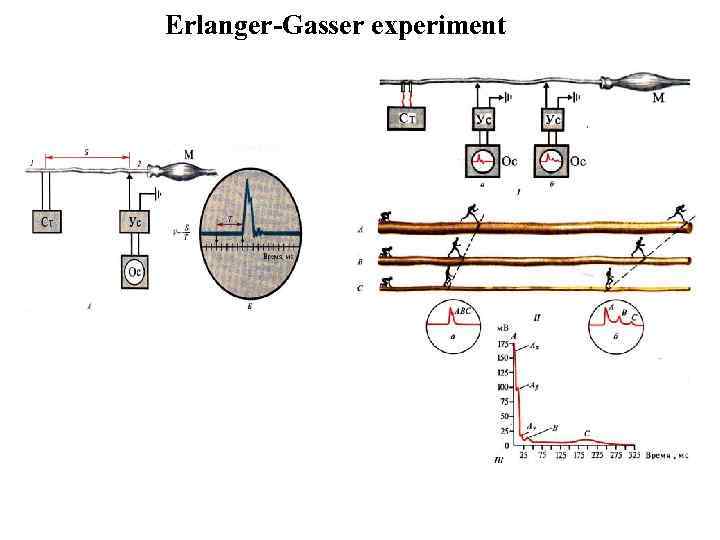 Erlanger-Gasser experiment
Erlanger-Gasser experiment
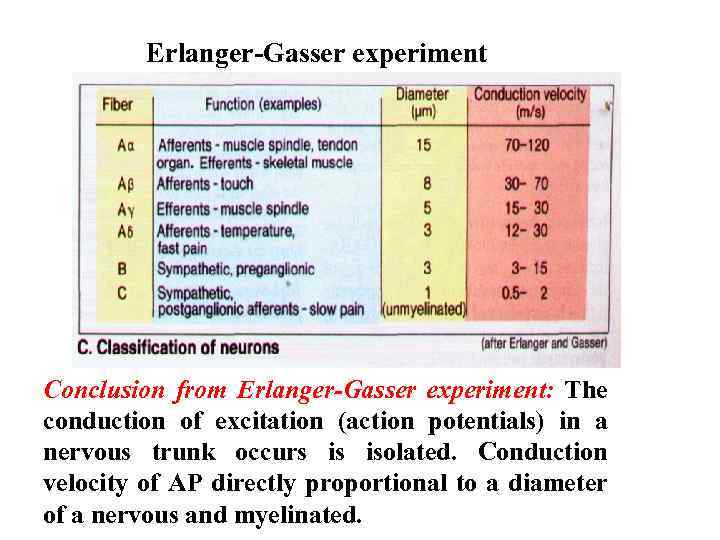 Erlanger-Gasser experiment Conclusion from Erlanger-Gasser experiment: The conduction of excitation (action potentials) in a nervous trunk occurs is isolated. Conduction velocity of AP directly proportional to a diameter of a nervous and myelinated.
Erlanger-Gasser experiment Conclusion from Erlanger-Gasser experiment: The conduction of excitation (action potentials) in a nervous trunk occurs is isolated. Conduction velocity of AP directly proportional to a diameter of a nervous and myelinated.
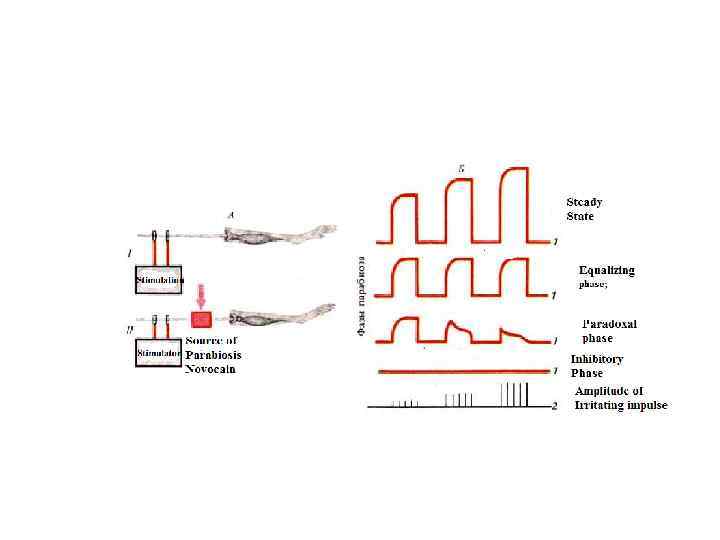
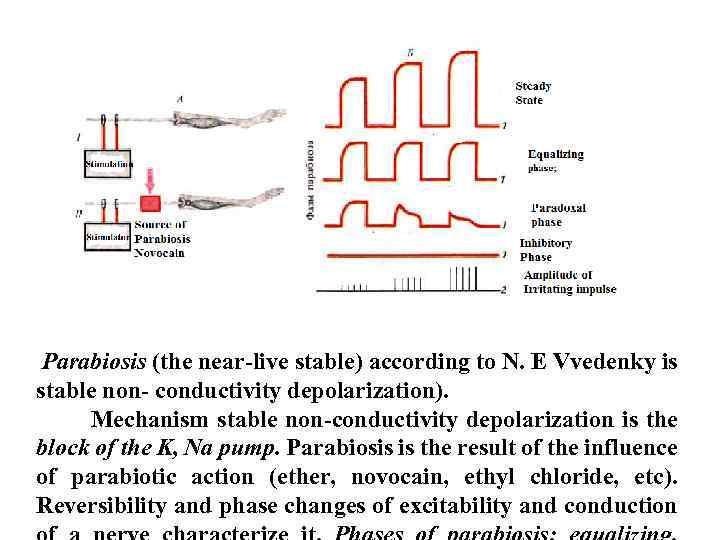 Parabiosis (the near-live stable) according to N. E Vvedenky is stable non- conductivity depolarization). Mechanism stable non-conductivity depolarization is the block of the K, Na pump. Parabiosis is the result of the influence of parabiotic action (ether, novocain, ethyl chloride, etc). Reversibility and phase changes of excitability and conduction
Parabiosis (the near-live stable) according to N. E Vvedenky is stable non- conductivity depolarization). Mechanism stable non-conductivity depolarization is the block of the K, Na pump. Parabiosis is the result of the influence of parabiotic action (ether, novocain, ethyl chloride, etc). Reversibility and phase changes of excitability and conduction
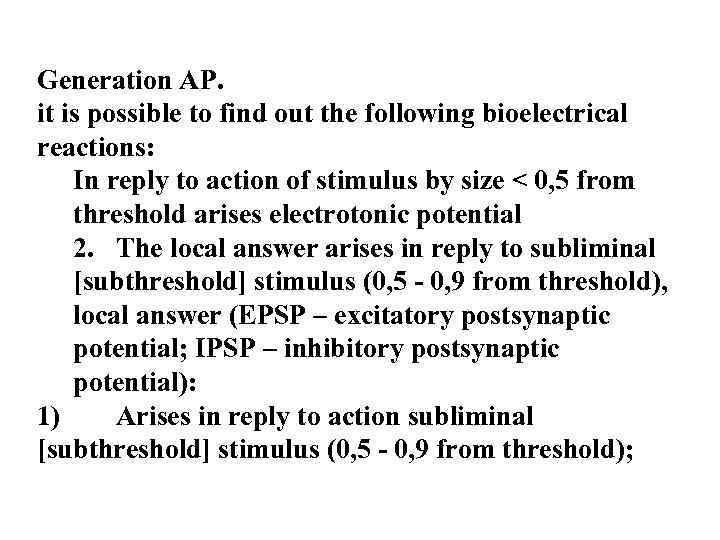 Generation AP. it is possible to find out the following bioelectrical reactions: In reply to action of stimulus by size < 0, 5 from threshold arises electrotonic potential 2. The local answer arises in reply to subliminal [subthreshold] stimulus (0, 5 - 0, 9 from threshold), local answer (EPSP – excitatory postsynaptic potential; IPSP – inhibitory postsynaptic potential): 1) Arises in reply to action subliminal [subthreshold] stimulus (0, 5 - 0, 9 from threshold);
Generation AP. it is possible to find out the following bioelectrical reactions: In reply to action of stimulus by size < 0, 5 from threshold arises electrotonic potential 2. The local answer arises in reply to subliminal [subthreshold] stimulus (0, 5 - 0, 9 from threshold), local answer (EPSP – excitatory postsynaptic potential; IPSP – inhibitory postsynaptic potential): 1) Arises in reply to action subliminal [subthreshold] stimulus (0, 5 - 0, 9 from threshold);
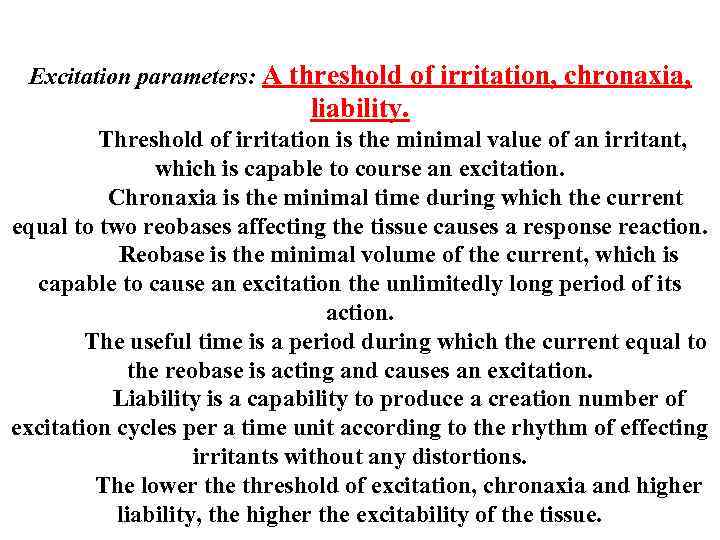 Excitation parameters: A threshold of irritation, chronaxia, liability. Threshold of irritation is the minimal value of an irritant, which is capable to course an excitation. Chronaxia is the minimal time during which the current equal to two reobases affecting the tissue causes a response reaction. Reobase is the minimal volume of the current, which is capable to cause an excitation the unlimitedly long period of its action. The useful time is a period during which the current equal to the reobase is acting and causes an excitation. Liability is a capability to produce a creation number of excitation cycles per a time unit according to the rhythm of effecting irritants without any distortions. The lower the threshold of excitation, chronaxia and higher liability, the higher the excitability of the tissue.
Excitation parameters: A threshold of irritation, chronaxia, liability. Threshold of irritation is the minimal value of an irritant, which is capable to course an excitation. Chronaxia is the minimal time during which the current equal to two reobases affecting the tissue causes a response reaction. Reobase is the minimal volume of the current, which is capable to cause an excitation the unlimitedly long period of its action. The useful time is a period during which the current equal to the reobase is acting and causes an excitation. Liability is a capability to produce a creation number of excitation cycles per a time unit according to the rhythm of effecting irritants without any distortions. The lower the threshold of excitation, chronaxia and higher liability, the higher the excitability of the tissue.
 Emil Du Bois-Reymond, 1818— 1896 Rise time or rate of rise of the leading edge of the pulse Refers to the time it takes to get from zero to maximal amplitude within each pulse Law of Dubois Reymond—determines whethere will be a physiological response when the current is applied Stimulus must be of adequate amplitude (intensity) Voltage change must be rapid enough Phase duration must be long enough Refers to the time from when the individual phase of a current leaves the isoelectric (zero) line to when it returns Must be long enough to overcome the capacitance of the targeted nerve Strength–duration curve—relationship of
Emil Du Bois-Reymond, 1818— 1896 Rise time or rate of rise of the leading edge of the pulse Refers to the time it takes to get from zero to maximal amplitude within each pulse Law of Dubois Reymond—determines whethere will be a physiological response when the current is applied Stimulus must be of adequate amplitude (intensity) Voltage change must be rapid enough Phase duration must be long enough Refers to the time from when the individual phase of a current leaves the isoelectric (zero) line to when it returns Must be long enough to overcome the capacitance of the targeted nerve Strength–duration curve—relationship of
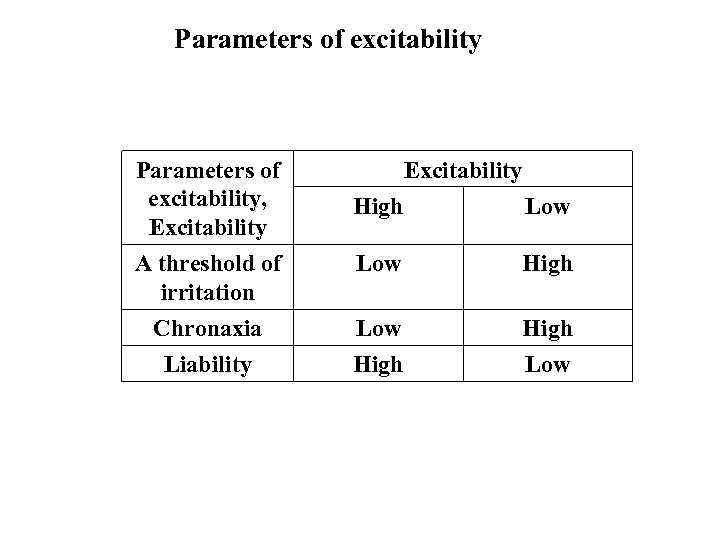 Parameters of excitability Parameters of excitability, Excitability High Low A threshold of irritation Chronaxia Liability Low High Low
Parameters of excitability Parameters of excitability, Excitability High Low A threshold of irritation Chronaxia Liability Low High Low
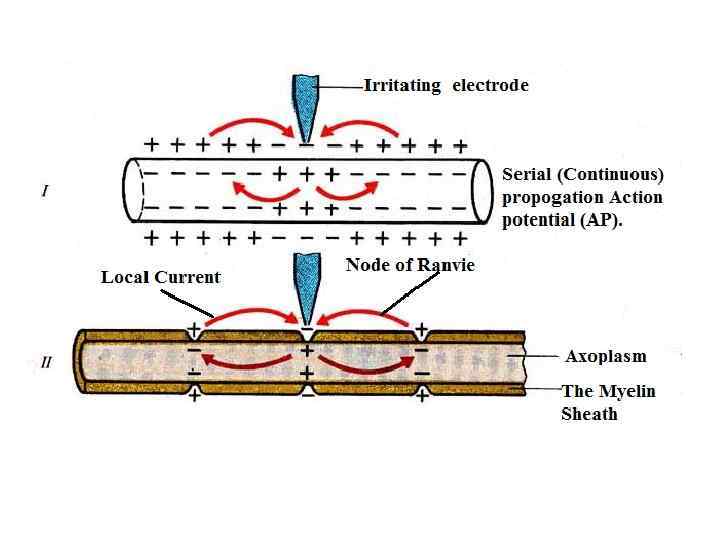
 In non-myeliminated fibers an excitation is conducted serial and in myeliminated fibers – saltatoricly (somersault) (from one node of Ranvier to another)
In non-myeliminated fibers an excitation is conducted serial and in myeliminated fibers – saltatoricly (somersault) (from one node of Ranvier to another)
 Physiological properties of nerve fibers: excitability, conductivity, contractility, and lability. Excitability and lability of a nerve fiber is higher and the refractory period is shorter than in the muscular tissue. Conduction of an excitation is a special function of nerve fibers.
Physiological properties of nerve fibers: excitability, conductivity, contractility, and lability. Excitability and lability of a nerve fiber is higher and the refractory period is shorter than in the muscular tissue. Conduction of an excitation is a special function of nerve fibers.
 Laws conduction of excitation via nerve fibers, The law of two-way conduction via a nerve fiber, The law of the anatomic and physiologic integrity, The law of an isolated conduction of excitation through a nerve fiber (Gasser and Erlanger, 1937). Types of nerve fibers: A, B, C. They are characterized according to the conduction rate diameter, the structure (myelinated – nonmyelinated).
Laws conduction of excitation via nerve fibers, The law of two-way conduction via a nerve fiber, The law of the anatomic and physiologic integrity, The law of an isolated conduction of excitation through a nerve fiber (Gasser and Erlanger, 1937). Types of nerve fibers: A, B, C. They are characterized according to the conduction rate diameter, the structure (myelinated – nonmyelinated).
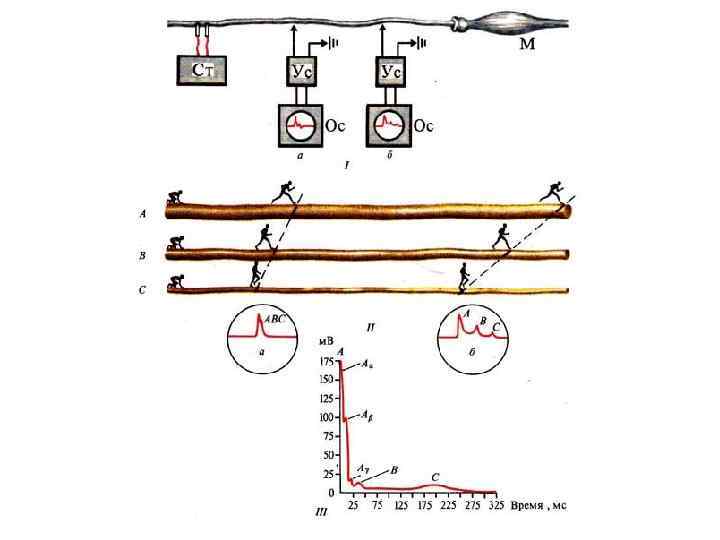
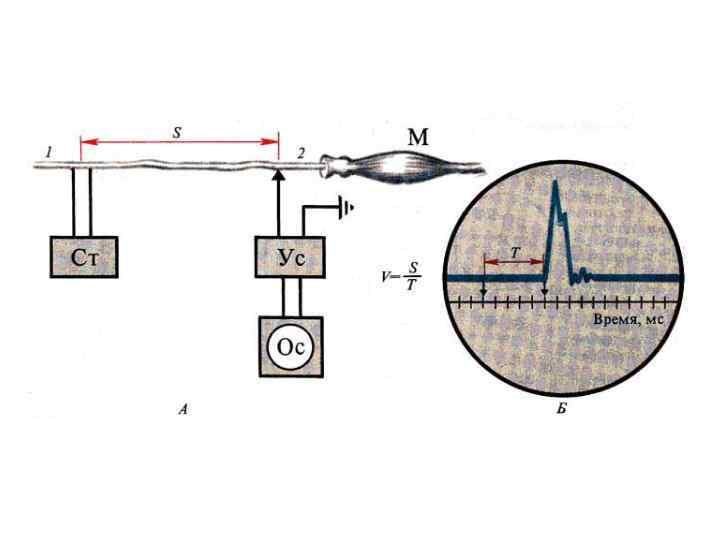
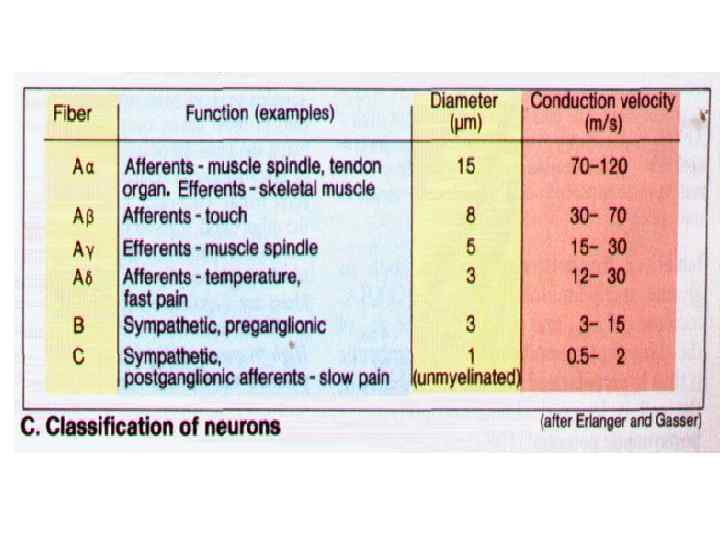
 Conclusion from Erlanger-Gasser experiment: The conduction of excitation (action potentials) in a nervous trunk occurs is isolated. Conduction velocity of AP directly proportional to a diameter of a nervous and myelinated.
Conclusion from Erlanger-Gasser experiment: The conduction of excitation (action potentials) in a nervous trunk occurs is isolated. Conduction velocity of AP directly proportional to a diameter of a nervous and myelinated.
 Generation AP. it is possible to find out the following bioelectrical reactions: In reply to action of stimulus by size < 0, 5 from threshold arises electrotonic potential 2. The local answer arises in reply to subliminal [subthreshold] stimulus (0, 5 - 0, 9 from threshold), local answer (EPSP – excitatory postsynaptic potential; IPSP – inhibitory postsynaptic potential): 1) Arises in reply to action subliminal [subthreshold] stimulus (0, 5 - 0, 9 from threshold);
Generation AP. it is possible to find out the following bioelectrical reactions: In reply to action of stimulus by size < 0, 5 from threshold arises electrotonic potential 2. The local answer arises in reply to subliminal [subthreshold] stimulus (0, 5 - 0, 9 from threshold), local answer (EPSP – excitatory postsynaptic potential; IPSP – inhibitory postsynaptic potential): 1) Arises in reply to action subliminal [subthreshold] stimulus (0, 5 - 0, 9 from threshold);
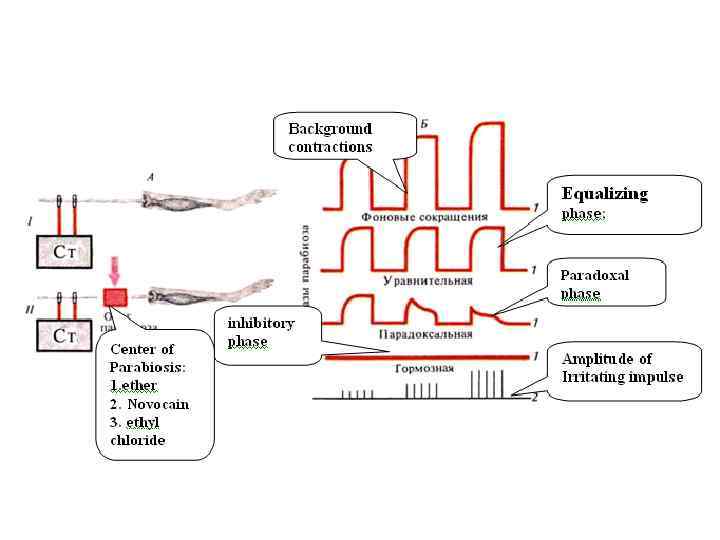
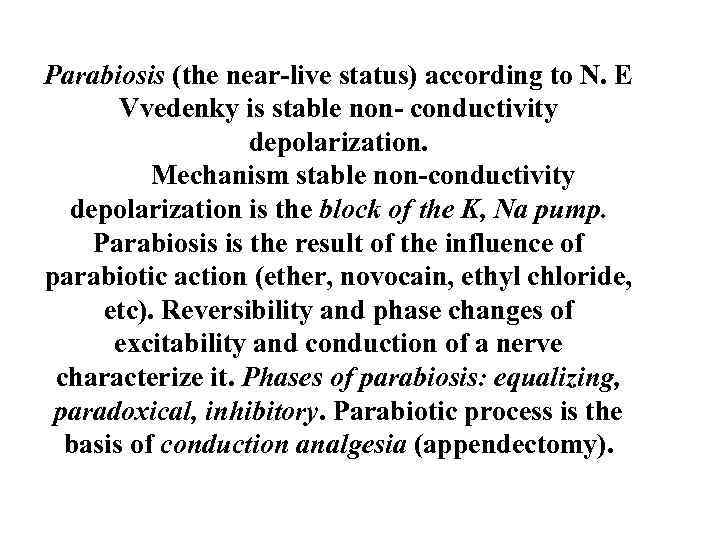 Parabiosis (the near-live status) according to N. E Vvedenky is stable non- conductivity depolarization. Mechanism stable non-conductivity depolarization is the block of the K, Na pump. Parabiosis is the result of the influence of parabiotic action (ether, novocain, ethyl chloride, etc). Reversibility and phase changes of excitability and conduction of a nerve characterize it. Phases of parabiosis: equalizing, paradoxical, inhibitory. Parabiotic process is the basis of conduction analgesia (appendectomy).
Parabiosis (the near-live status) according to N. E Vvedenky is stable non- conductivity depolarization. Mechanism stable non-conductivity depolarization is the block of the K, Na pump. Parabiosis is the result of the influence of parabiotic action (ether, novocain, ethyl chloride, etc). Reversibility and phase changes of excitability and conduction of a nerve characterize it. Phases of parabiosis: equalizing, paradoxical, inhibitory. Parabiotic process is the basis of conduction analgesia (appendectomy).
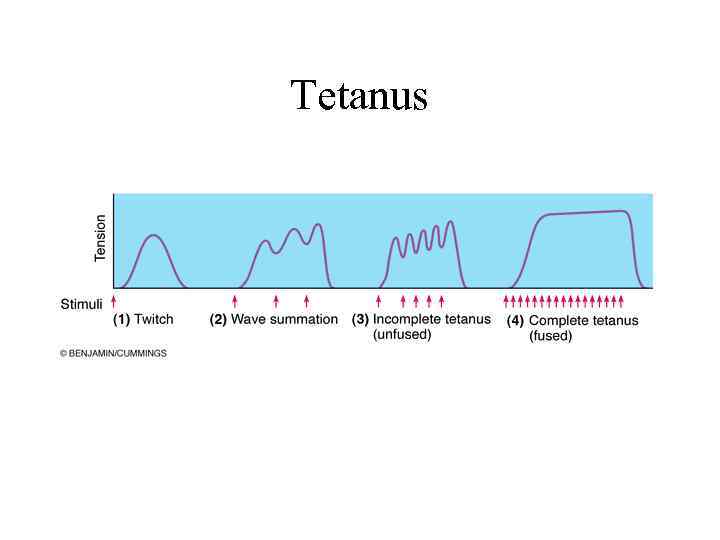 Tetanus
Tetanus
 Refractory Period • Brief period of time in which muscle cells will not respond to a stimulus
Refractory Period • Brief period of time in which muscle cells will not respond to a stimulus
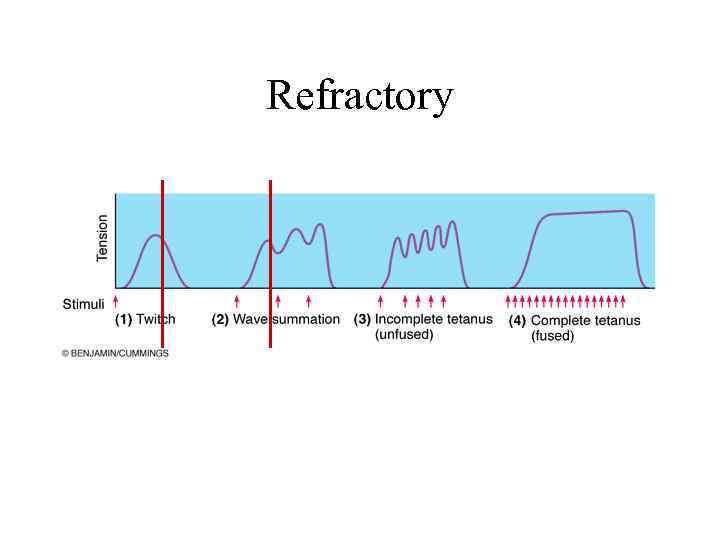 Refractory
Refractory
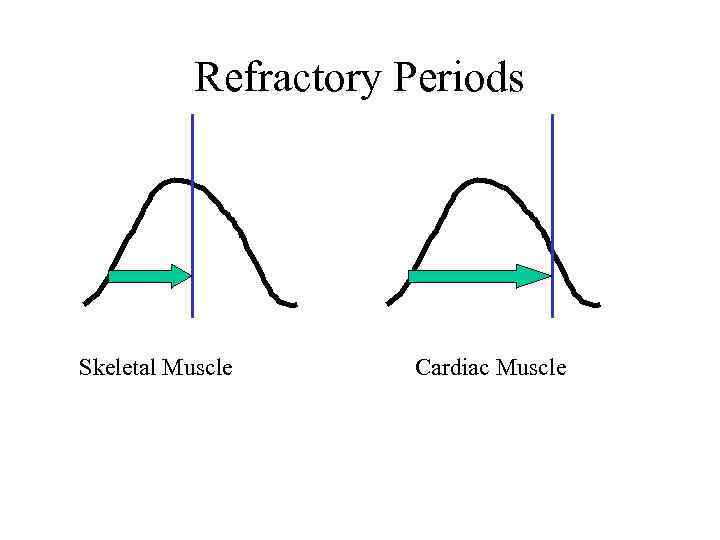 Refractory Periods Skeletal Muscle Cardiac Muscle
Refractory Periods Skeletal Muscle Cardiac Muscle
 Isometric Contraction • Produces no movement • Used in – Standing – Sitting – Posture
Isometric Contraction • Produces no movement • Used in – Standing – Sitting – Posture