df64da42f06caa715bff8664bb1e21af.ppt
- Количество слайдов: 27
SEVERE SEPSIS&SEPTIC SHOCK IN PEDIATRICS. Abdel Razzaq Abu Mayaleh, MD PRCS _ New Hospital - Hebron Based partially on www. picucourse. org
INTRODUCTION § SEPSIS: - it’s an infection plus systemic manifestation of infection. § § § SEVERE SEPSIS : - Sepsis plus sepsis-induced organ dysfunction or tissue hypo perfusion. . SEPTIC SHOCK: - sepsis-induced hypotension persisting despite adequate fluid resuscitation and elevated lactate. § HYPOTENTION: - S. BP < 70 + 2 ×wt. (80 + 2 × wt) § SHOCK: - § DO 2 < VO 2
A clinician, armed with the sepsis bundles, attacks the three heads of severe sepsis: hypotension, hypoperfusion and organ dysfunction. Crit Care Med 2004; 320(Suppl): S 595 S 597
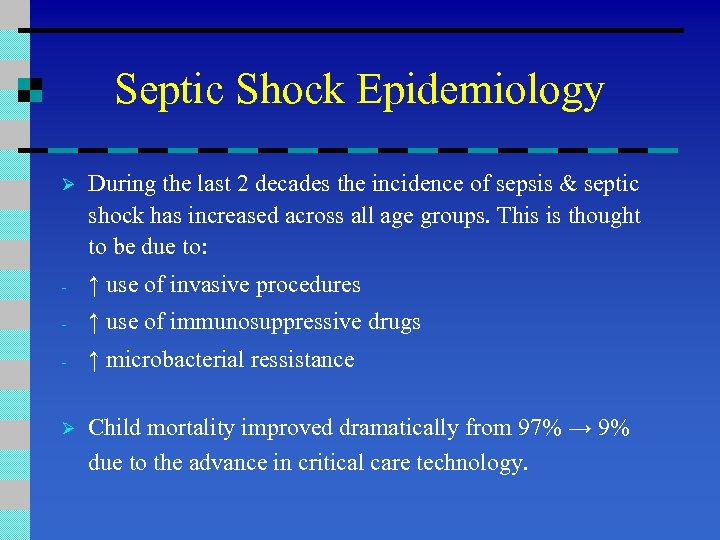
Septic Shock Epidemiology Ø During the last 2 decades the incidence of sepsis & septic shock has increased across all age groups. This is thought to be due to: - ↑ use of invasive procedures - ↑ use of immunosuppressive drugs - ↑ microbacterial ressistance Ø Child mortality improved dramatically from 97% → 9% due to the advance in critical care technology.
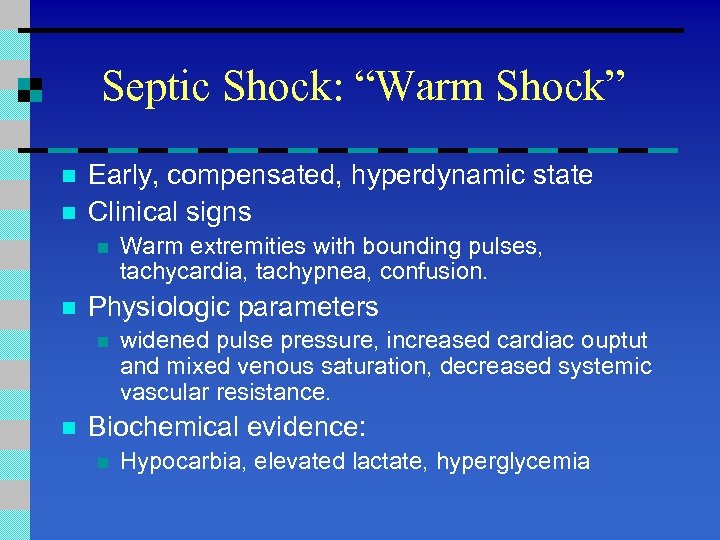
Septic Shock: “Warm Shock” n n Early, compensated, hyperdynamic state Clinical signs n n Physiologic parameters n n Warm extremities with bounding pulses, tachycardia, tachypnea, confusion. widened pulse pressure, increased cardiac ouptut and mixed venous saturation, decreased systemic vascular resistance. Biochemical evidence: n Hypocarbia, elevated lactate, hyperglycemia
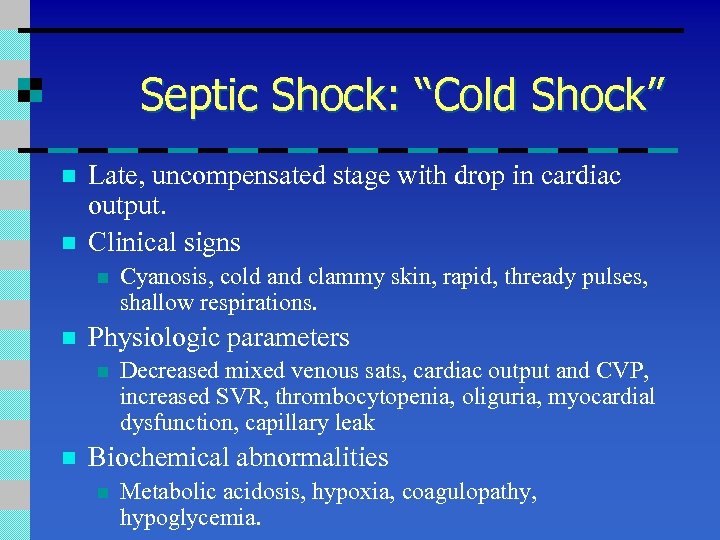
Septic Shock: “Cold Shock” n n Late, uncompensated stage with drop in cardiac output. Clinical signs n n Physiologic parameters n n Cyanosis, cold and clammy skin, rapid, thready pulses, shallow respirations. Decreased mixed venous sats, cardiac output and CVP, increased SVR, thrombocytopenia, oliguria, myocardial dysfunction, capillary leak Biochemical abnormalities n Metabolic acidosis, hypoxia, coagulopathy, hypoglycemia.
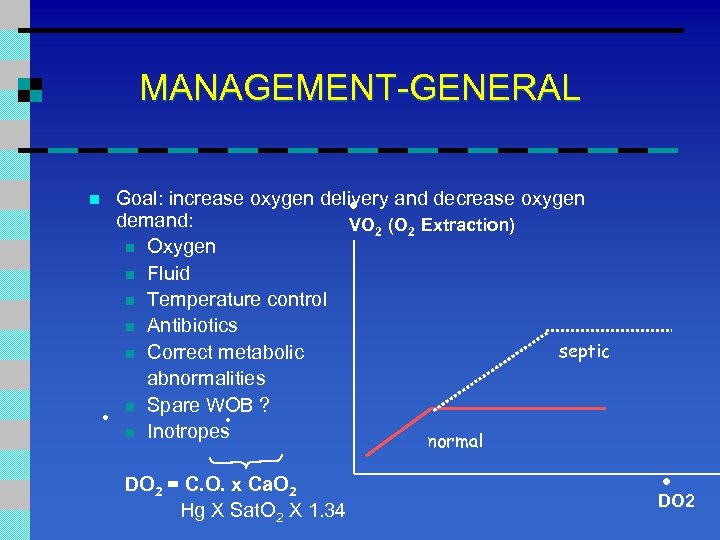
MANAGEMENT-GENERAL . n . Goal: increase oxygen delivery and decrease oxygen demand: VO 2 (O 2 Extraction) n Oxygen n Fluid n Temperature control n Antibiotics septic n Correct metabolic abnormalities n Spare WOB ? . n Inotropes normal DO 2 = C. O. x Ca. O 2 Hg X Sat. O 2 X 1. 34 . DO 2
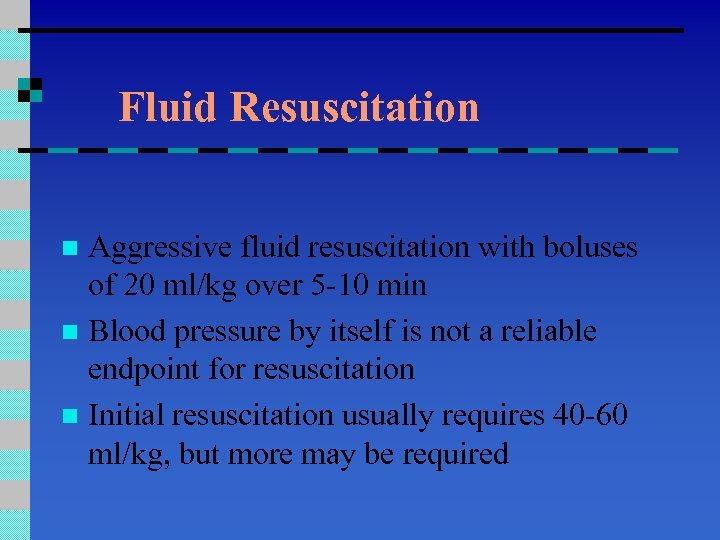
Fluid Resuscitation Aggressive fluid resuscitation with boluses of 20 ml/kg over 5 -10 min n Blood pressure by itself is not a reliable endpoint for resuscitation n Initial resuscitation usually requires 40 -60 ml/kg, but more may be required n
Therapeutic Endpoints n n n Capillary refill < 2 sec Warm extremities Urine output > 1 ml/kg/hr Normal mental status Decreased lactate Central venous O 2 saturation > 70%
Hemodynamic Support n n n Hemodynamic profile may be variable Dopamine for hypotension Epinephrine or norepinephrine for dopaminerefractory shock Dobutamine for low cardiac output state Inhaled NO useful in neonates with post-partum pulmonary hypertension and sepsis
Other Therapies n n Steroids: recommended for children with catecholamine resistance and suspected or proven adrenal insufficiency. Activated protein C not studied adequately in children yet. GM-CSF shown to be of benefit in neonates with sepsis and neutropenia. Extracorporeal membrane oxygenation (ECMO) may be considered in children with refractory shock or respiratory failure.
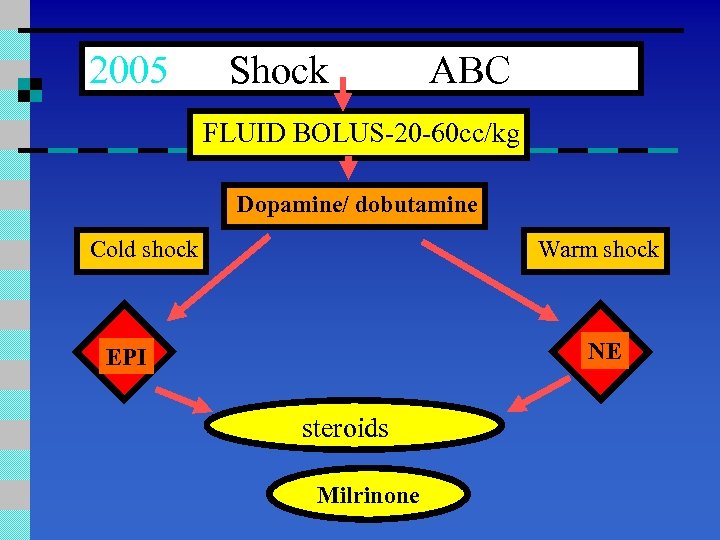
2005 Shock ABC FLUID BOLUS-20 -60 cc/kg Dopamine/ dobutamine Cold shock Warm shock NE EPI steroids Milrinone
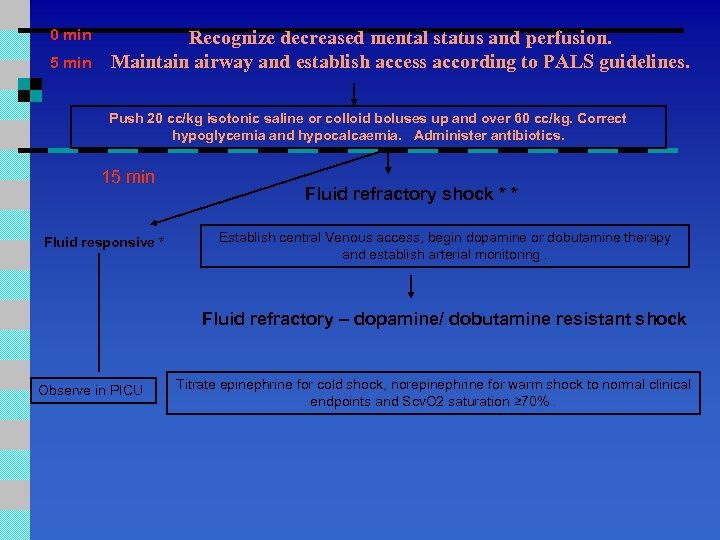
0 min 5 min Recognize decreased mental status and perfusion. Maintain airway and establish access according to PALS guidelines. Push 20 cc/kg isotonic saline or colloid boluses up and over 60 cc/kg. Correct hypoglycemia and hypocalcaemia. Administer antibiotics. 15 min Fluid responsive * Fluid refractory shock * * Establish central Venous access, begin dopamine or dobutamine therapy and establish arterial monitoring. Fluid refractory – dopamine/ dobutamine resistant shock Observe in PICU Titrate epinephrine for cold shock, norepinephrine for warm shock to normal clinical endpoints and Scv. O 2 saturation ≥ 70%.
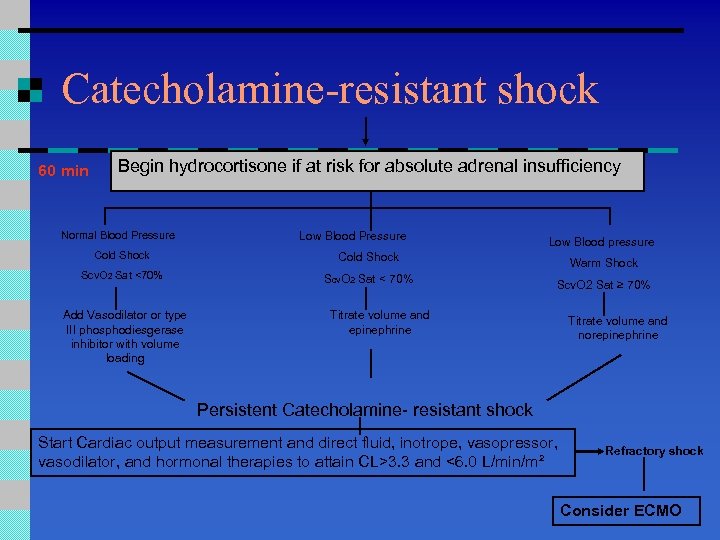
Catecholamine-resistant shock 60 min Begin hydrocortisone if at risk for absolute adrenal insufficiency Normal Blood Pressure Low Blood pressure Cold Shock Scv. O 2 Sat <70% Warm Shock Scv. O 2 Sat < 70% Scv. O 2 Sat ≥ 70% Add Vasodilator or type III phosphodiesgerase inhibitor with volume loading Titrate volume and epinephrine Titrate volume and norepinephrine Persistent Catecholamine- resistant shock Start Cardiac output measurement and direct fluid, inotrope, vasopressor, vasodilator, and hormonal therapies to attain CL>3. 3 and <6. 0 L/min/m² Refractory shock Consider ECMO
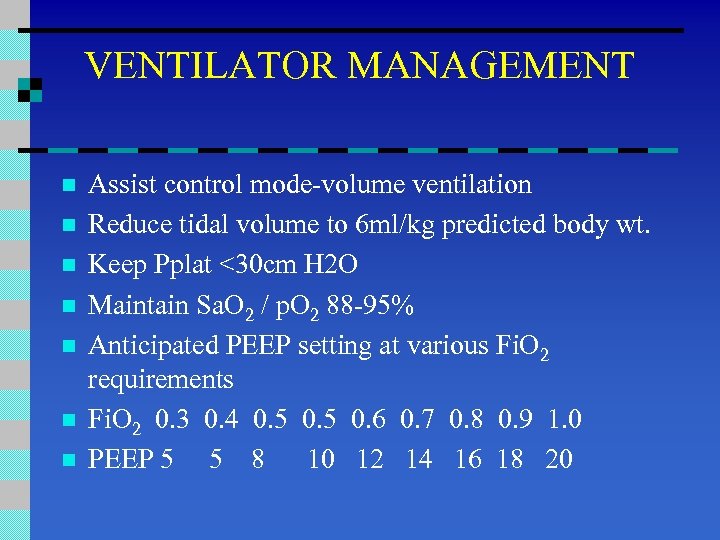
VENTILATOR MANAGEMENT n n n n Assist control mode-volume ventilation Reduce tidal volume to 6 ml/kg predicted body wt. Keep Pplat <30 cm H 2 O Maintain Sa. O 2 / p. O 2 88 -95% Anticipated PEEP setting at various Fi. O 2 requirements Fi. O 2 0. 3 0. 4 0. 5 0. 6 0. 7 0. 8 0. 9 1. 0 PEEP 5 5 8 10 12 14 16 18 20
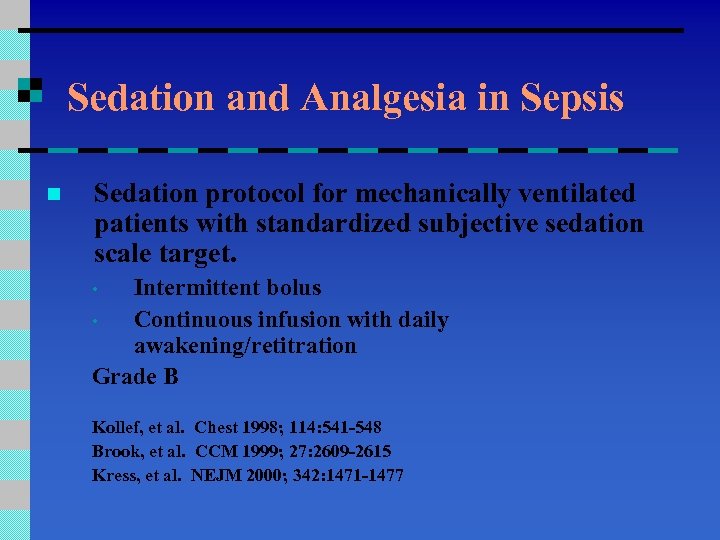
Sedation and Analgesia in Sepsis n Sedation protocol for mechanically ventilated patients with standardized subjective sedation scale target. Intermittent bolus • Continuous infusion with daily awakening/retitration Grade B • Kollef, et al. Chest 1998; 114: 541 -548 Brook, et al. CCM 1999; 27: 2609 -2615 Kress, et al. NEJM 2000; 342: 1471 -1477
Neuromuscular Blockers n n Avoid if possible Used longer than 2 -3 hrs n n PRN bolus Continuous infusion with twitch monitor Grade E
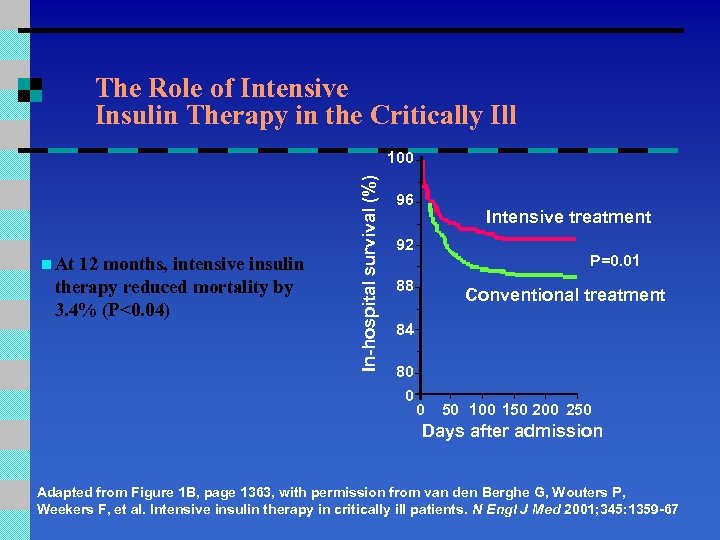
The Role of Intensive Insulin Therapy in the Critically Ill n At 12 months, intensive insulin therapy reduced mortality by 3. 4% (P<0. 04) In-hospital survival (%) 100 96 Intensive treatment 92 P=0. 01 88 Conventional treatment 84 80 0 0 50 100 150 200 250 Days after admission Adapted from Figure 1 B, page 1363, with permission from van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med 2001; 345: 1359 -67
Glucose Control n After initial stabilization n Glucose < 150 mg/d. L Continuous infusion insulin and glucose or feeding (enteral preferred) Monitoring Initially q 30– 60 mins n After stabilization q 4 h Grade D n
Bicarbonate Therapy Ø Bicarbonate therapy not recommended to improve hemodynamics in patients with lactate induced p. H >7. 15 Grade C Cooper, et al. Ann Intern Med 1990; 112: 492 -498 Mathieu, et al. CCM 1991; 19: 1352 -1356
Primary Stress Ulcer Risk Factors Frequently Present in Severe Sepsis Mechanical ventilation n Coagulopathy n Hypotension n
Choice of Agents for Stress Ulcer Prophylaxis H 2 receptor blockers n Role of proton pump inhibitors n Grade C Cook DJ, et al. Am J Med 1991; 91: 519 -527
Blood Product Administration Red Blood Cells Tissue hypoperfusion resolved No extenuating circumstances n n n Coronary artery disease Acute hemorrhage Lactic acidosis Transfuse < 7. 0 g/dl to maintain 7. 0 -9. 0 g/d. L Grade B
Blood Product Administration n Do not use erythropoietin to treat sepsisrelated anemia. Erythropoietin may be used for other accepted reasons. Grade B
Blood Product Administration Fresh frozen plasma • Bleeding • Planned invasive procedures. Grade E
Blood Product Administration • Do not use antithrombin therapy. Grade B Warren et al. JAMA 2001; 1869 -1878
Blood Product Administration n Platelet administration n Transfuse for < 5000/mm 3 Transfuse for 5000/mm 3 – 30, 000/mm 3 with significant bleeding risk Transfuse < 50, 000/mm 3 for invasive procedures or bleeding Grade E
df64da42f06caa715bff8664bb1e21af.ppt