761ac2719d5e577c68c093bffef7f4ba.ppt
- Количество слайдов: 57
 Sepsis and Septic Shock: An Update for the Primary Care Provider National Association for Pediatric Nurse Practitioners Western NY branch, November 2016 Meeting Amanda B. Hassinger, MD, MS Director of Quality & Patient Safety Division of Pediatric Critical Care Women & Children’s Hospital of Buffalo Assistant Professor, Department of Pediatrics University at Buffalo Jacobs School of Medicine and Biomedical Sciences
Sepsis and Septic Shock: An Update for the Primary Care Provider National Association for Pediatric Nurse Practitioners Western NY branch, November 2016 Meeting Amanda B. Hassinger, MD, MS Director of Quality & Patient Safety Division of Pediatric Critical Care Women & Children’s Hospital of Buffalo Assistant Professor, Department of Pediatrics University at Buffalo Jacobs School of Medicine and Biomedical Sciences
 Disclosure • No financial conflicts to report
Disclosure • No financial conflicts to report
 Objectives 1. 2. 3. 4. 5. The evolution of the definition of sepsis Recent epidemiology Outpatient sepsis management Progress on outcomes CMS and NY State Mandates
Objectives 1. 2. 3. 4. 5. The evolution of the definition of sepsis Recent epidemiology Outpatient sepsis management Progress on outcomes CMS and NY State Mandates
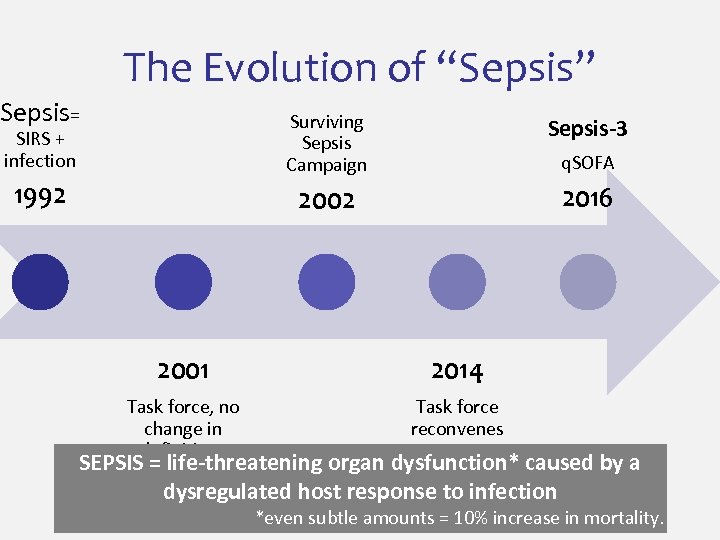 The Evolution of “Sepsis” Sepsis= SIRS + infection Surviving Sepsis Campaign Sepsis-3 1992 2002 2016 q. SOFA 2001 2014 Task force, no change in definitions Task force reconvenes SEPSIS = life-threatening organ dysfunction* caused by a dysregulated host response to infection *even subtle amounts = 10% increase in mortality.
The Evolution of “Sepsis” Sepsis= SIRS + infection Surviving Sepsis Campaign Sepsis-3 1992 2002 2016 q. SOFA 2001 2014 Task force, no change in definitions Task force reconvenes SEPSIS = life-threatening organ dysfunction* caused by a dysregulated host response to infection *even subtle amounts = 10% increase in mortality.
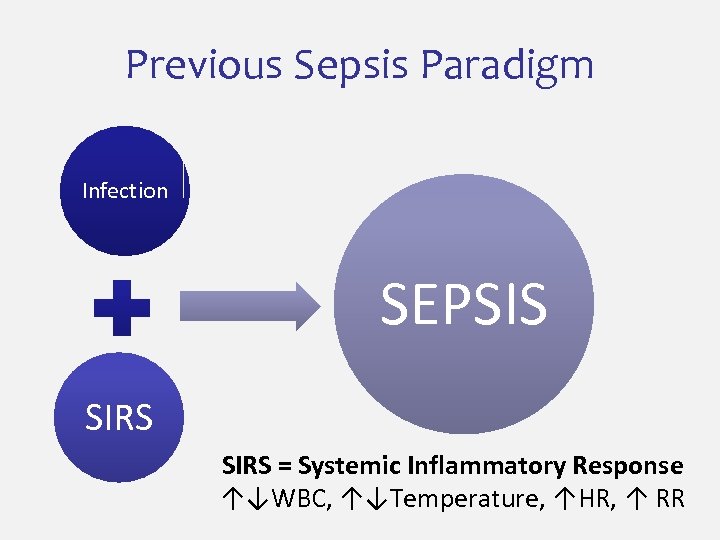 Previous Sepsis Paradigm Infection SEPSIS SIRS = Systemic Inflammatory Response ↑↓WBC, ↑↓Temperature, ↑HR, ↑ RR
Previous Sepsis Paradigm Infection SEPSIS SIRS = Systemic Inflammatory Response ↑↓WBC, ↑↓Temperature, ↑HR, ↑ RR
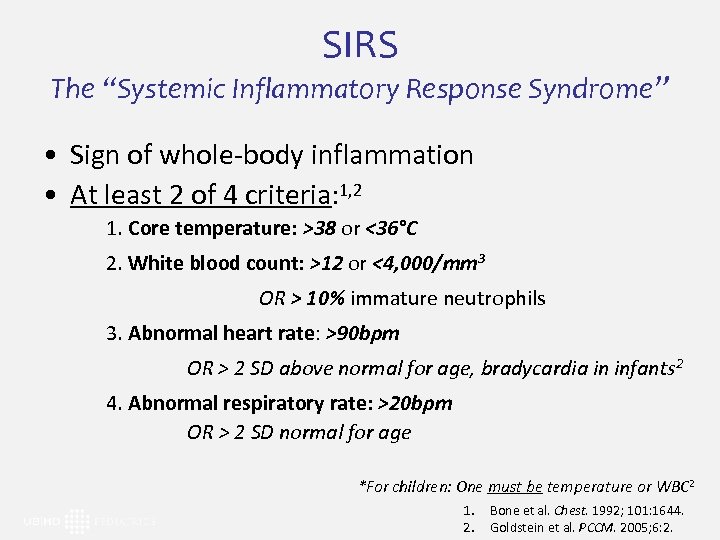 SIRS The “Systemic Inflammatory Response Syndrome” • Sign of whole-body inflammation • At least 2 of 4 criteria: 1, 2 1. Core temperature: >38 or <36°C 2. White blood count: >12 or <4, 000/mm 3 OR > 10% immature neutrophils 3. Abnormal heart rate: >90 bpm OR > 2 SD above normal for age, bradycardia in infants 2 4. Abnormal respiratory rate: >20 bpm OR > 2 SD normal for age *For children: One must be temperature or WBC 2 1. 2. Bone et al. Chest. 1992; 101: 1644. Goldstein et al. PCCM. 2005; 6: 2.
SIRS The “Systemic Inflammatory Response Syndrome” • Sign of whole-body inflammation • At least 2 of 4 criteria: 1, 2 1. Core temperature: >38 or <36°C 2. White blood count: >12 or <4, 000/mm 3 OR > 10% immature neutrophils 3. Abnormal heart rate: >90 bpm OR > 2 SD above normal for age, bradycardia in infants 2 4. Abnormal respiratory rate: >20 bpm OR > 2 SD normal for age *For children: One must be temperature or WBC 2 1. 2. Bone et al. Chest. 1992; 101: 1644. Goldstein et al. PCCM. 2005; 6: 2.
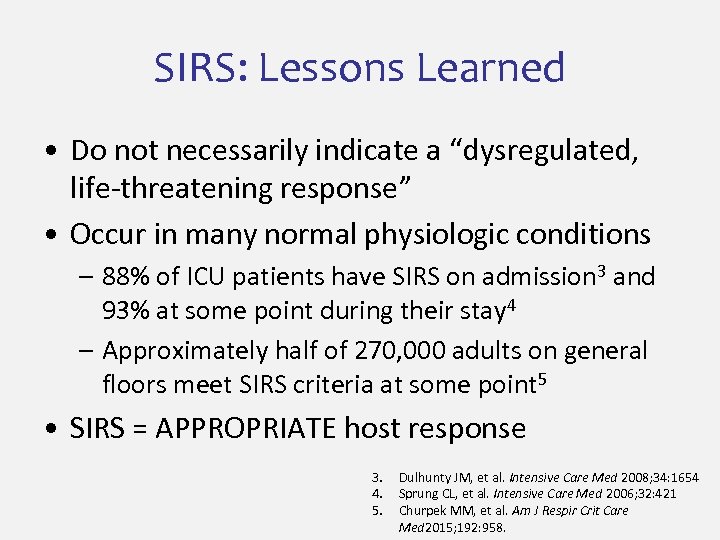 SIRS: Lessons Learned • Do not necessarily indicate a “dysregulated, life-threatening response” • Occur in many normal physiologic conditions – 88% of ICU patients have SIRS on admission 3 and 93% at some point during their stay 4 – Approximately half of 270, 000 adults on general floors meet SIRS criteria at some point 5 • SIRS = APPROPRIATE host response 3. 4. 5. Dulhunty JM, et al. Intensive Care Med 2008; 34: 1654 Sprung CL, et al. Intensive Care Med 2006; 32: 421 Churpek MM, et al. Am J Respir Crit Care Med 2015; 192: 958.
SIRS: Lessons Learned • Do not necessarily indicate a “dysregulated, life-threatening response” • Occur in many normal physiologic conditions – 88% of ICU patients have SIRS on admission 3 and 93% at some point during their stay 4 – Approximately half of 270, 000 adults on general floors meet SIRS criteria at some point 5 • SIRS = APPROPRIATE host response 3. 4. 5. Dulhunty JM, et al. Intensive Care Med 2008; 34: 1654 Sprung CL, et al. Intensive Care Med 2006; 32: 421 Churpek MM, et al. Am J Respir Crit Care Med 2015; 192: 958.
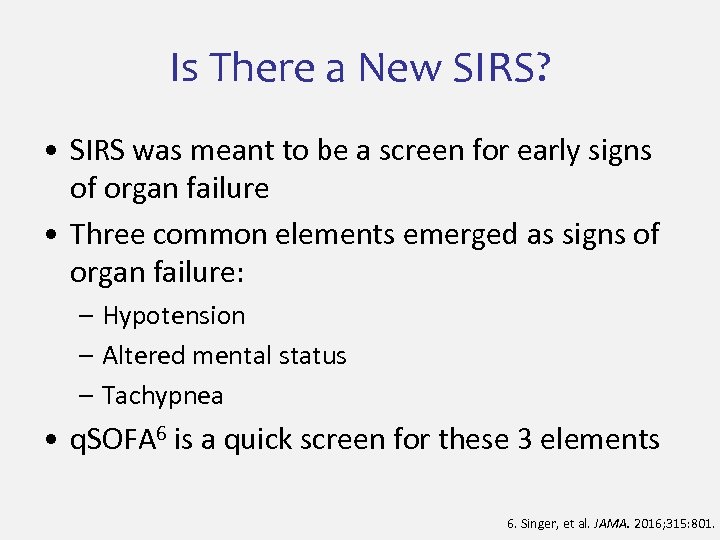 Is There a New SIRS? • SIRS was meant to be a screen for early signs of organ failure • Three common elements emerged as signs of organ failure: – Hypotension – Altered mental status – Tachypnea • q. SOFA 6 is a quick screen for these 3 elements 6. Singer, et al. JAMA. 2016; 315: 801.
Is There a New SIRS? • SIRS was meant to be a screen for early signs of organ failure • Three common elements emerged as signs of organ failure: – Hypotension – Altered mental status – Tachypnea • q. SOFA 6 is a quick screen for these 3 elements 6. Singer, et al. JAMA. 2016; 315: 801.
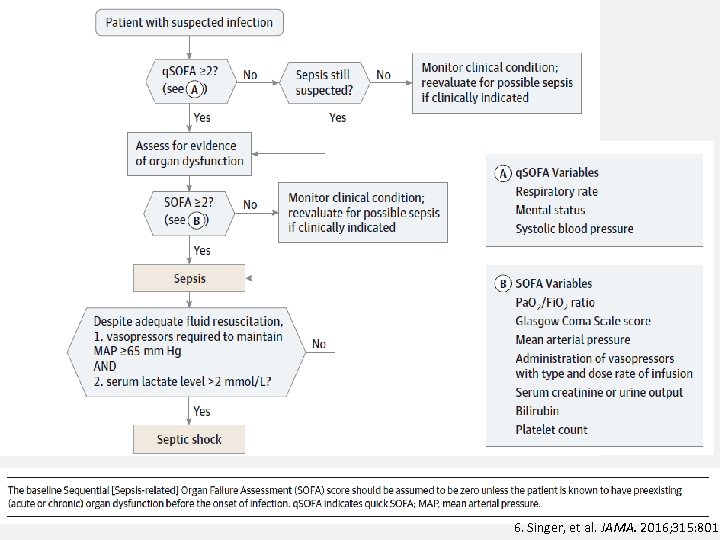 6. Singer, et al. JAMA. 2016; 315: 801.
6. Singer, et al. JAMA. 2016; 315: 801.
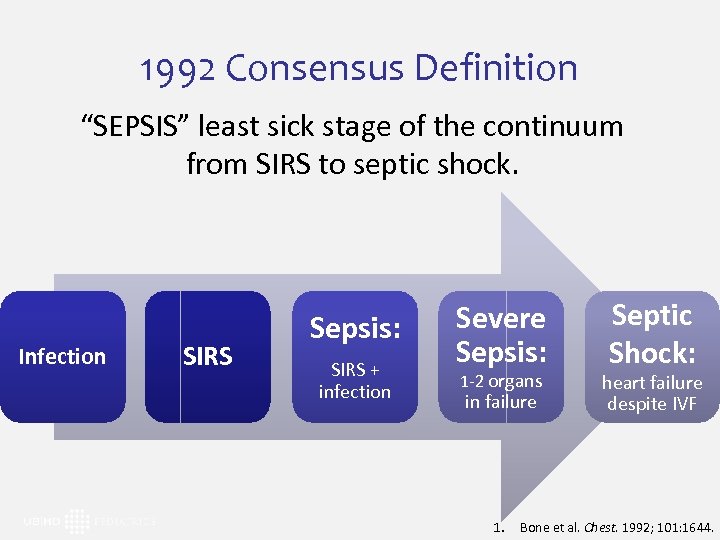 1992 Consensus Definition “SEPSIS” least sick stage of the continuum from SIRS to septic shock. Infection SIRS Sepsis: SIRS + infection Severe Sepsis: 1 -2 organs in failure 1. Septic Shock: heart failure despite IVF Bone et al. Chest. 1992; 101: 1644.
1992 Consensus Definition “SEPSIS” least sick stage of the continuum from SIRS to septic shock. Infection SIRS Sepsis: SIRS + infection Severe Sepsis: 1 -2 organs in failure 1. Septic Shock: heart failure despite IVF Bone et al. Chest. 1992; 101: 1644.
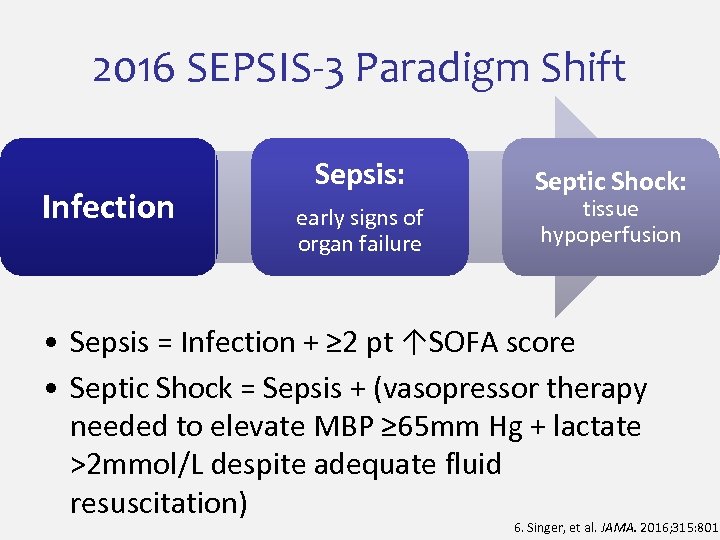 2016 SEPSIS-3 Paradigm Shift Infection Sepsis: early signs of organ failure Septic Shock: tissue hypoperfusion • Sepsis = Infection + ≥ 2 pt ↑SOFA score • Septic Shock = Sepsis + (vasopressor therapy needed to elevate MBP ≥ 65 mm Hg + lactate >2 mmol/L despite adequate fluid resuscitation) 6. Singer, et al. JAMA. 2016; 315: 801.
2016 SEPSIS-3 Paradigm Shift Infection Sepsis: early signs of organ failure Septic Shock: tissue hypoperfusion • Sepsis = Infection + ≥ 2 pt ↑SOFA score • Septic Shock = Sepsis + (vasopressor therapy needed to elevate MBP ≥ 65 mm Hg + lactate >2 mmol/L despite adequate fluid resuscitation) 6. Singer, et al. JAMA. 2016; 315: 801.
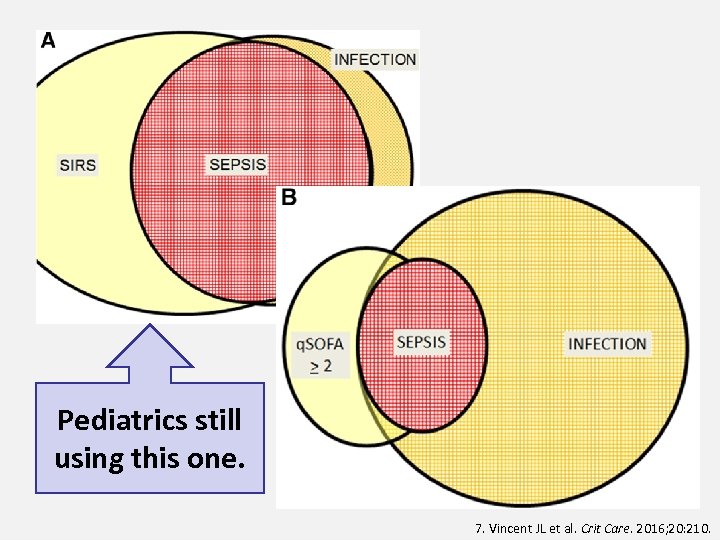 Pediatrics still using this one. 7. Vincent JL et al. Crit Care. 2016; 20: 210.
Pediatrics still using this one. 7. Vincent JL et al. Crit Care. 2016; 20: 210.
 The Epidemiology of Sepsis • True incidence is unknown • Likely the leading cause of mortality and critical illness worldwide – “Septicemia” #9 on the CDC list of COD in 20008 • Annually, $20 -25 billion of total US hospital costs (5. 2% of all costs)8, 9 • Increasing in incidence in all age-groups 9 8. 9. Vincent JL, et al. Lancet. 2013; 381: 774. Gaieski DF, et al. Crit Care Med. 2013; 41: 1167.
The Epidemiology of Sepsis • True incidence is unknown • Likely the leading cause of mortality and critical illness worldwide – “Septicemia” #9 on the CDC list of COD in 20008 • Annually, $20 -25 billion of total US hospital costs (5. 2% of all costs)8, 9 • Increasing in incidence in all age-groups 9 8. 9. Vincent JL, et al. Lancet. 2013; 381: 774. Gaieski DF, et al. Crit Care Med. 2013; 41: 1167.
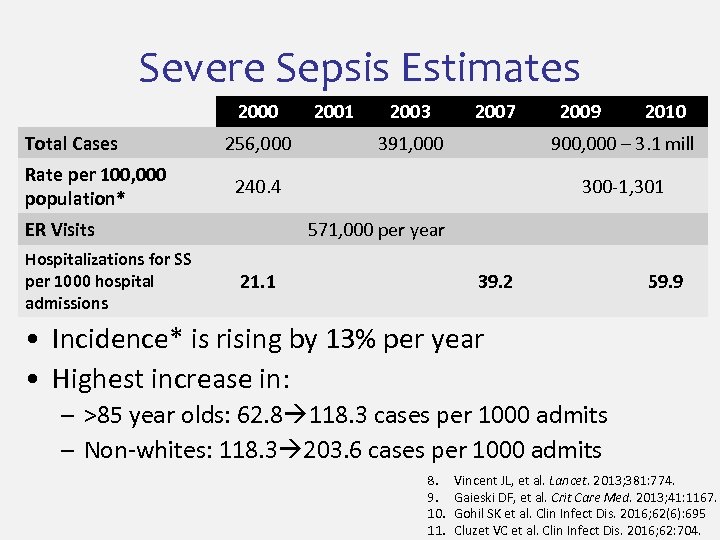 Severe Sepsis Estimates 2000 Total Cases Rate per 100, 000 population* 256, 000 2003 2007 391, 000 2009 2010 900, 000 – 3. 1 mill 240. 4 ER Visits Hospitalizations for SS per 1000 hospital admissions 2001 300 -1, 301 571, 000 per year 21. 1 39. 2 59. 9 • Incidence* is rising by 13% per year • Highest increase in: – >85 year olds: 62. 8 118. 3 cases per 1000 admits – Non-whites: 118. 3 203. 6 cases per 1000 admits 8. 9. 10. 11. Vincent JL, et al. Lancet. 2013; 381: 774. Gaieski DF, et al. Crit Care Med. 2013; 41: 1167. Gohil SK et al. Clin Infect Dis. 2016; 62(6): 695 Cluzet VC et al. Clin Infect Dis. 2016; 62: 704.
Severe Sepsis Estimates 2000 Total Cases Rate per 100, 000 population* 256, 000 2003 2007 391, 000 2009 2010 900, 000 – 3. 1 mill 240. 4 ER Visits Hospitalizations for SS per 1000 hospital admissions 2001 300 -1, 301 571, 000 per year 21. 1 39. 2 59. 9 • Incidence* is rising by 13% per year • Highest increase in: – >85 year olds: 62. 8 118. 3 cases per 1000 admits – Non-whites: 118. 3 203. 6 cases per 1000 admits 8. 9. 10. 11. Vincent JL, et al. Lancet. 2013; 381: 774. Gaieski DF, et al. Crit Care Med. 2013; 41: 1167. Gohil SK et al. Clin Infect Dis. 2016; 62(6): 695 Cluzet VC et al. Clin Infect Dis. 2016; 62: 704.
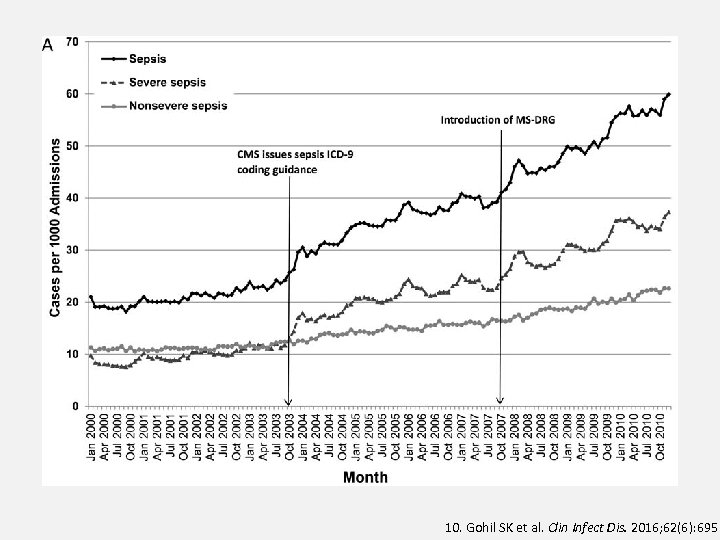 10. Gohil SK et al. Clin Infect Dis. 2016; 62(6): 695
10. Gohil SK et al. Clin Infect Dis. 2016; 62(6): 695
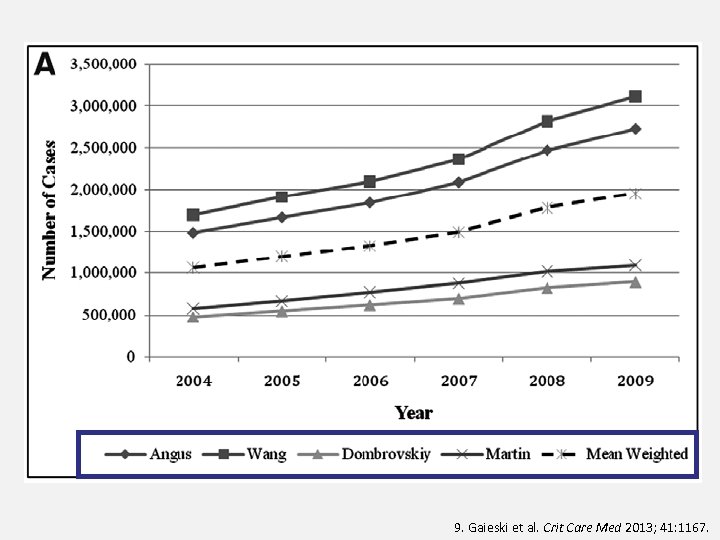 9. Gaieski et al. Crit Care Med 2013; 41: 1167.
9. Gaieski et al. Crit Care Med 2013; 41: 1167.
 Adult Sepsis Epidemiology • Incidence has risen over the last 20 years – Due to aging population, more co-morbidities – Actual incidence rise is confirmed in data from the UK, Croatia, Australia, New Zealand 11 – Likely slower than reported • Proven by stable US hospital admission rates • Overall mortality related to sepsis has been increasing while case-fatality is decreasing = “overuse” of the term in less sick patients 11. Cluzet VC et al. Clin Infect Dis. 2016; 62: 704.
Adult Sepsis Epidemiology • Incidence has risen over the last 20 years – Due to aging population, more co-morbidities – Actual incidence rise is confirmed in data from the UK, Croatia, Australia, New Zealand 11 – Likely slower than reported • Proven by stable US hospital admission rates • Overall mortality related to sepsis has been increasing while case-fatality is decreasing = “overuse” of the term in less sick patients 11. Cluzet VC et al. Clin Infect Dis. 2016; 62: 704.
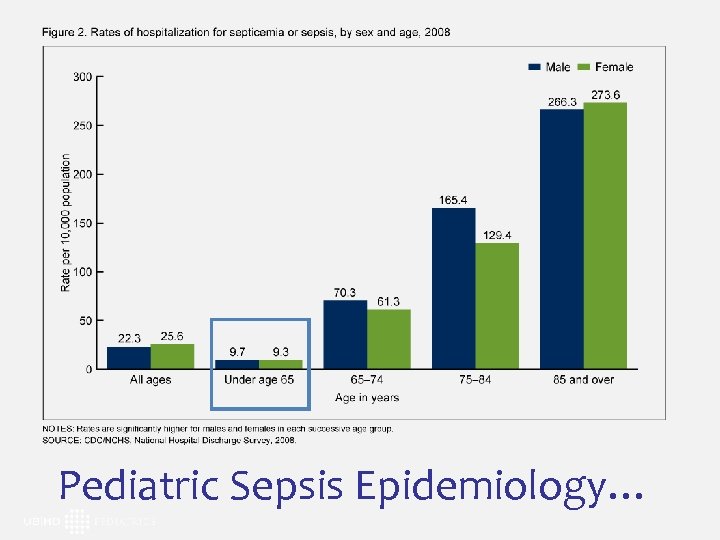 Pediatric Sepsis Epidemiology…
Pediatric Sepsis Epidemiology…
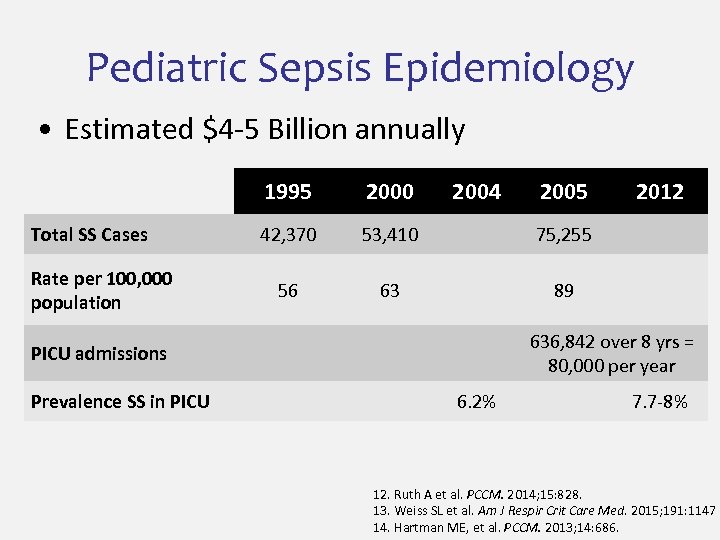 Pediatric Sepsis Epidemiology • Estimated $4 -5 Billion annually 1995 Total SS Cases Rate per 100, 000 population 2000 2004 42, 370 53, 410 75, 255 56 63 89 2012 636, 842 over 8 yrs = 80, 000 per year PICU admissions Prevalence SS in PICU 2005 6. 2% 7. 7 -8% 12. Ruth A et al. PCCM. 2014; 15: 828. 13. Weiss SL et al. Am J Respir Crit Care Med. 2015; 191: 1147 14. Hartman ME, et al. PCCM. 2013; 14: 686.
Pediatric Sepsis Epidemiology • Estimated $4 -5 Billion annually 1995 Total SS Cases Rate per 100, 000 population 2000 2004 42, 370 53, 410 75, 255 56 63 89 2012 636, 842 over 8 yrs = 80, 000 per year PICU admissions Prevalence SS in PICU 2005 6. 2% 7. 7 -8% 12. Ruth A et al. PCCM. 2014; 15: 828. 13. Weiss SL et al. Am J Respir Crit Care Med. 2015; 191: 1147 14. Hartman ME, et al. PCCM. 2013; 14: 686.
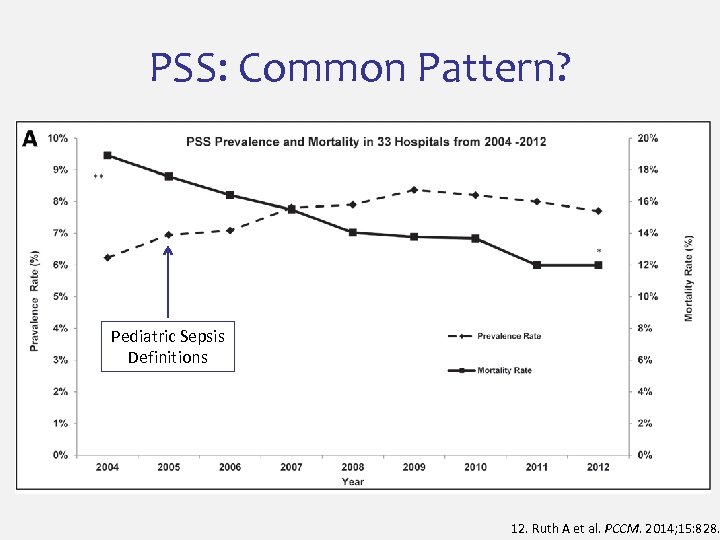 PSS: Common Pattern? Pediatric Sepsis Definitions 12. Ruth A et al. PCCM. 2014; 15: 828.
PSS: Common Pattern? Pediatric Sepsis Definitions 12. Ruth A et al. PCCM. 2014; 15: 828.
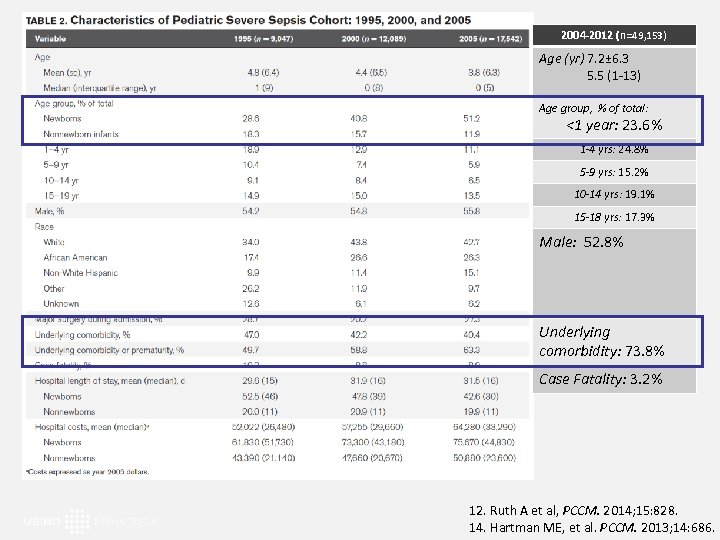 2004 -2012 (n =49, 153) Age (yr) 7. 2± 6. 3 5. 5 (1 -13) Age group, % of total: <1 year: 23. 6% 1 -4 yrs: 24. 8% 5 -9 yrs: 15. 2% 10 -14 yrs: 19. 1% 15 -18 yrs: 17. 3% Male: 52. 8% Underlying comorbidity: 73. 8% Case Fatality: 3. 2% 12. Ruth A et al, PCCM. 2014; 15: 828. 14. Hartman ME, et al. PCCM. 2013; 14: 686.
2004 -2012 (n =49, 153) Age (yr) 7. 2± 6. 3 5. 5 (1 -13) Age group, % of total: <1 year: 23. 6% 1 -4 yrs: 24. 8% 5 -9 yrs: 15. 2% 10 -14 yrs: 19. 1% 15 -18 yrs: 17. 3% Male: 52. 8% Underlying comorbidity: 73. 8% Case Fatality: 3. 2% 12. Ruth A et al, PCCM. 2014; 15: 828. 14. Hartman ME, et al. PCCM. 2013; 14: 686.
 Pediatric Sepsis Epidemiology • Incidence has risen over the last 20 years – Very low birth weight infants, more comorbidities – Likely slower rise in incidence than reported • Overall mortality related to sepsis has been increasing while case-fatality is decreasing = “overuse” of the term in less sick patients
Pediatric Sepsis Epidemiology • Incidence has risen over the last 20 years – Very low birth weight infants, more comorbidities – Likely slower rise in incidence than reported • Overall mortality related to sepsis has been increasing while case-fatality is decreasing = “overuse” of the term in less sick patients
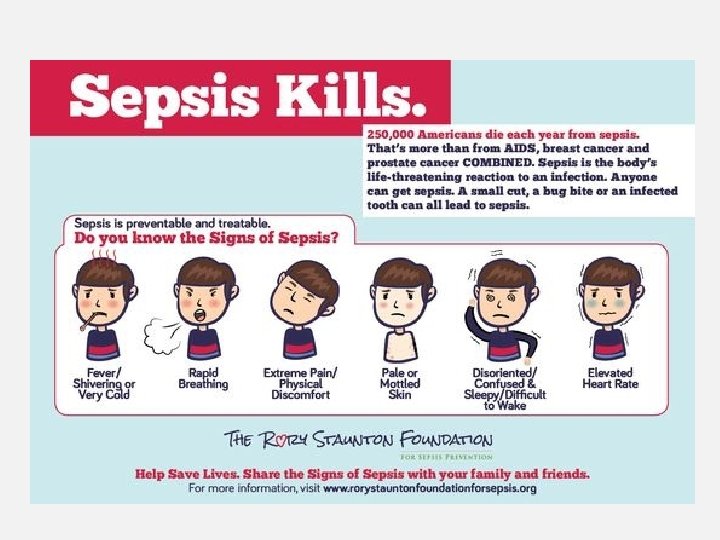
 Outpatient Sepsis Management 1. Recognition 2. RECOGNITION 3. Early RECOGNITION!
Outpatient Sepsis Management 1. Recognition 2. RECOGNITION 3. Early RECOGNITION!
 What does “Sepsis” Look Like?
What does “Sepsis” Look Like?
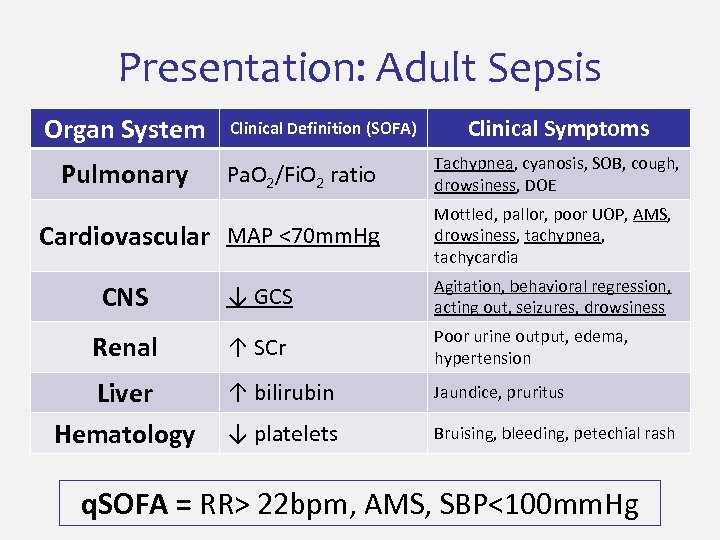 Presentation: Adult Sepsis Organ System Pulmonary Clinical Definition (SOFA) Pa. O 2/Fi. O 2 ratio Cardiovascular MAP <70 mm. Hg Clinical Symptoms Tachypnea, cyanosis, SOB, cough, drowsiness, DOE Mottled, pallor, poor UOP, AMS, drowsiness, tachypnea, tachycardia CNS ↓ GCS Agitation, behavioral regression, acting out, seizures, drowsiness Renal ↑ SCr Poor urine output, edema, hypertension ↑ bilirubin Jaundice, pruritus ↓ platelets Bruising, bleeding, petechial rash Liver Hematology q. SOFA = RR> 22 bpm, AMS, SBP<100 mm. Hg
Presentation: Adult Sepsis Organ System Pulmonary Clinical Definition (SOFA) Pa. O 2/Fi. O 2 ratio Cardiovascular MAP <70 mm. Hg Clinical Symptoms Tachypnea, cyanosis, SOB, cough, drowsiness, DOE Mottled, pallor, poor UOP, AMS, drowsiness, tachypnea, tachycardia CNS ↓ GCS Agitation, behavioral regression, acting out, seizures, drowsiness Renal ↑ SCr Poor urine output, edema, hypertension ↑ bilirubin Jaundice, pruritus ↓ platelets Bruising, bleeding, petechial rash Liver Hematology q. SOFA = RR> 22 bpm, AMS, SBP<100 mm. Hg
 “Pediatric” SS ≠ “Small Adult” Sepsis • • Children frequently get infections “Normal” varies significantly by age Children are poor historians Early stages more subtle, pediatric cases recognized later • Hypotension is a very late sign
“Pediatric” SS ≠ “Small Adult” Sepsis • • Children frequently get infections “Normal” varies significantly by age Children are poor historians Early stages more subtle, pediatric cases recognized later • Hypotension is a very late sign
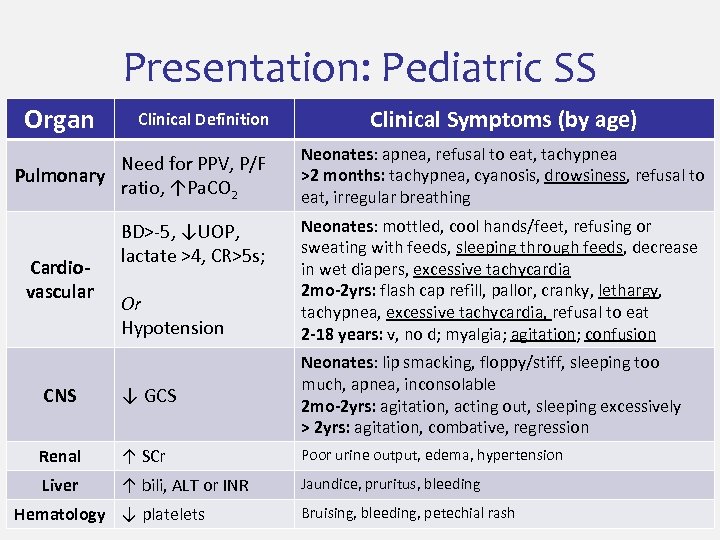 Presentation: Pediatric SS Organ Clinical Definition Need for PPV, P/F Pulmonary ratio, ↑Pa. CO 2 Cardiovascular BD>-5, ↓UOP, lactate >4, CR>5 s; Or Hypotension Clinical Symptoms (by age) Neonates: apnea, refusal to eat, tachypnea >2 months: tachypnea, cyanosis, drowsiness, refusal to eat, irregular breathing Neonates: mottled, cool hands/feet, refusing or sweating with feeds, sleeping through feeds, decrease in wet diapers, excessive tachycardia 2 mo-2 yrs: flash cap refill, pallor, cranky, lethargy, tachypnea, excessive tachycardia, refusal to eat 2 -18 years: v, no d; myalgia; agitation; confusion CNS ↓ GCS Neonates: lip smacking, floppy/stiff, sleeping too much, apnea, inconsolable 2 mo-2 yrs: agitation, acting out, sleeping excessively > 2 yrs: agitation, combative, regression Renal ↑ SCr Poor urine output, edema, hypertension Liver ↑ bili, ALT or INR Jaundice, pruritus, bleeding Hematology ↓ platelets Bruising, bleeding, petechial rash
Presentation: Pediatric SS Organ Clinical Definition Need for PPV, P/F Pulmonary ratio, ↑Pa. CO 2 Cardiovascular BD>-5, ↓UOP, lactate >4, CR>5 s; Or Hypotension Clinical Symptoms (by age) Neonates: apnea, refusal to eat, tachypnea >2 months: tachypnea, cyanosis, drowsiness, refusal to eat, irregular breathing Neonates: mottled, cool hands/feet, refusing or sweating with feeds, sleeping through feeds, decrease in wet diapers, excessive tachycardia 2 mo-2 yrs: flash cap refill, pallor, cranky, lethargy, tachypnea, excessive tachycardia, refusal to eat 2 -18 years: v, no d; myalgia; agitation; confusion CNS ↓ GCS Neonates: lip smacking, floppy/stiff, sleeping too much, apnea, inconsolable 2 mo-2 yrs: agitation, acting out, sleeping excessively > 2 yrs: agitation, combative, regression Renal ↑ SCr Poor urine output, edema, hypertension Liver ↑ bili, ALT or INR Jaundice, pruritus, bleeding Hematology ↓ platelets Bruising, bleeding, petechial rash
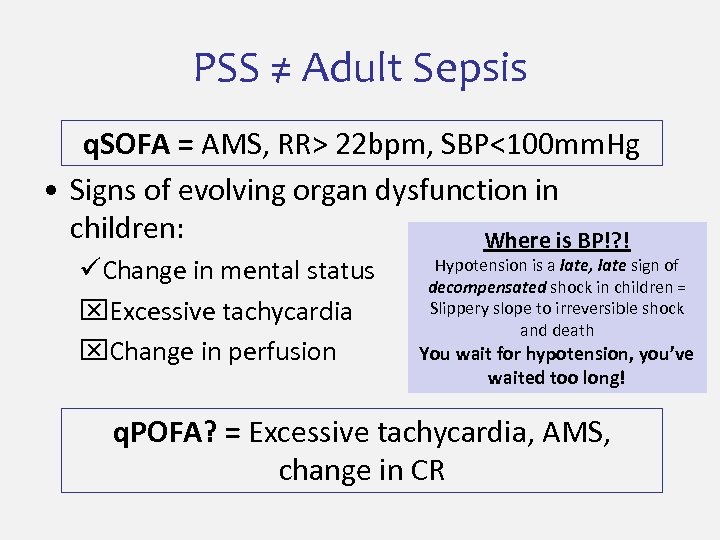 PSS ≠ Adult Sepsis q. SOFA = AMS, RR> 22 bpm, SBP<100 mm. Hg • Signs of evolving organ dysfunction in children: Where is BP!? ! üChange in mental status x. Excessive tachycardia x. Change in perfusion Hypotension is a late, late sign of decompensated shock in children = Slippery slope to irreversible shock and death You wait for hypotension, you’ve waited too long! q. POFA? = Excessive tachycardia, AMS, change in CR
PSS ≠ Adult Sepsis q. SOFA = AMS, RR> 22 bpm, SBP<100 mm. Hg • Signs of evolving organ dysfunction in children: Where is BP!? ! üChange in mental status x. Excessive tachycardia x. Change in perfusion Hypotension is a late, late sign of decompensated shock in children = Slippery slope to irreversible shock and death You wait for hypotension, you’ve waited too long! q. POFA? = Excessive tachycardia, AMS, change in CR
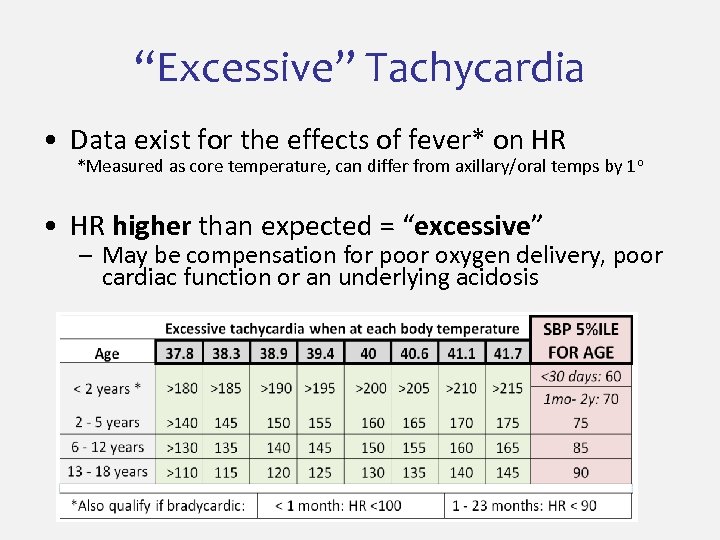 “Excessive” Tachycardia • Data exist for the effects of fever* on HR *Measured as core temperature, can differ from axillary/oral temps by 1 o • HR higher than expected = “excessive” – May be compensation for poor oxygen delivery, poor cardiac function or an underlying acidosis
“Excessive” Tachycardia • Data exist for the effects of fever* on HR *Measured as core temperature, can differ from axillary/oral temps by 1 o • HR higher than expected = “excessive” – May be compensation for poor oxygen delivery, poor cardiac function or an underlying acidosis
 Outpatient Sepsis Management 1. RECOGNITION 2. Source identification
Outpatient Sepsis Management 1. RECOGNITION 2. Source identification
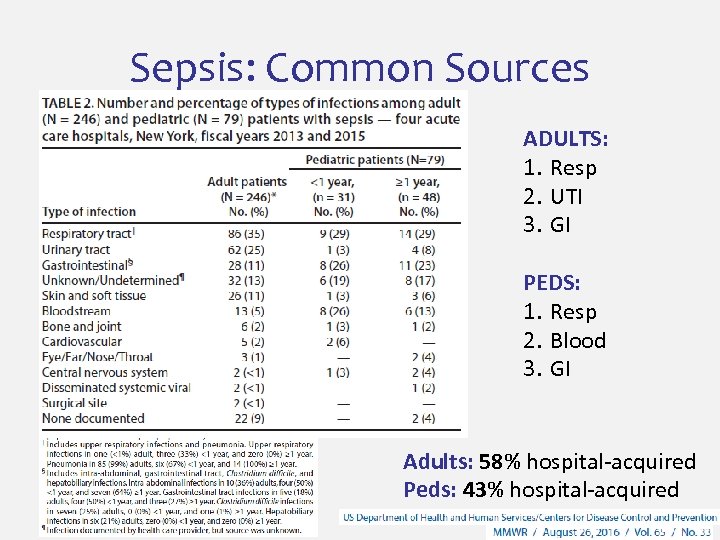 Sepsis: Common Sources ADULTS: 1. Resp 2. UTI 3. GI PEDS: 1. Resp 2. Blood 3. GI Adults: 58% hospital-acquired Peds: 43% hospital-acquired
Sepsis: Common Sources ADULTS: 1. Resp 2. UTI 3. GI PEDS: 1. Resp 2. Blood 3. GI Adults: 58% hospital-acquired Peds: 43% hospital-acquired
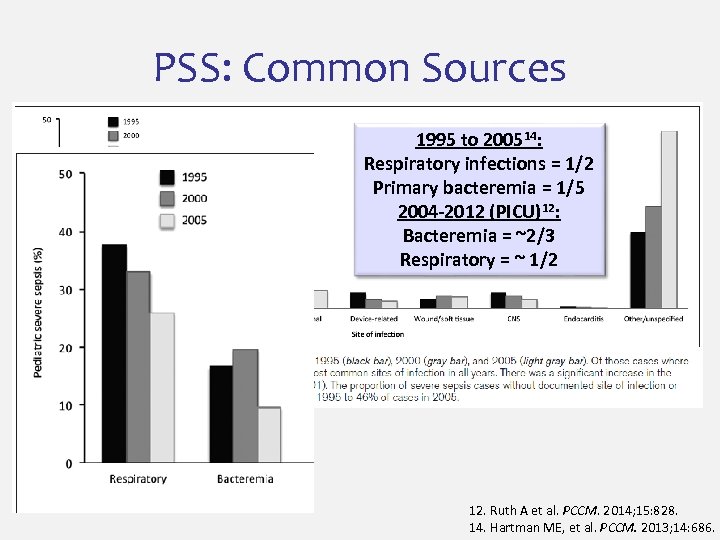 PSS: Common Sources 1995 to 200514: Respiratory infections = 1/2 Primary bacteremia = 1/5 2004 -2012 (PICU)12: Bacteremia = ~2/3 Respiratory = ~ 1/2 12. Ruth A et al. PCCM. 2014; 15: 828. 14. Hartman ME, et al. PCCM. 2013; 14: 686.
PSS: Common Sources 1995 to 200514: Respiratory infections = 1/2 Primary bacteremia = 1/5 2004 -2012 (PICU)12: Bacteremia = ~2/3 Respiratory = ~ 1/2 12. Ruth A et al. PCCM. 2014; 15: 828. 14. Hartman ME, et al. PCCM. 2013; 14: 686.
 Outpatient Sepsis Management 1. RECOGNITION 2. Source identification 3. Empiric antibiotics
Outpatient Sepsis Management 1. RECOGNITION 2. Source identification 3. Empiric antibiotics
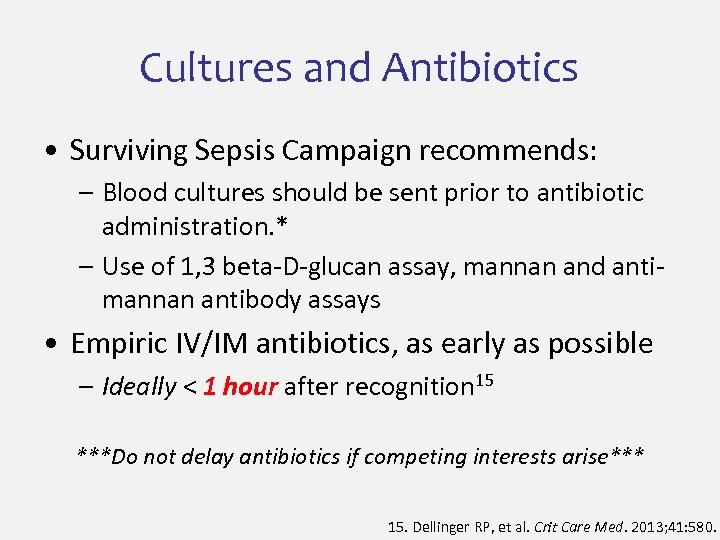 Cultures and Antibiotics • Surviving Sepsis Campaign recommends: – Blood cultures should be sent prior to antibiotic administration. * – Use of 1, 3 beta-D-glucan assay, mannan and antimannan antibody assays • Empiric IV/IM antibiotics, as early as possible – Ideally < 1 hour after recognition 15 ***Do not delay antibiotics if competing interests arise*** 15. Dellinger RP, et al. Crit Care Med. 2013; 41: 580.
Cultures and Antibiotics • Surviving Sepsis Campaign recommends: – Blood cultures should be sent prior to antibiotic administration. * – Use of 1, 3 beta-D-glucan assay, mannan and antimannan antibody assays • Empiric IV/IM antibiotics, as early as possible – Ideally < 1 hour after recognition 15 ***Do not delay antibiotics if competing interests arise*** 15. Dellinger RP, et al. Crit Care Med. 2013; 41: 580.
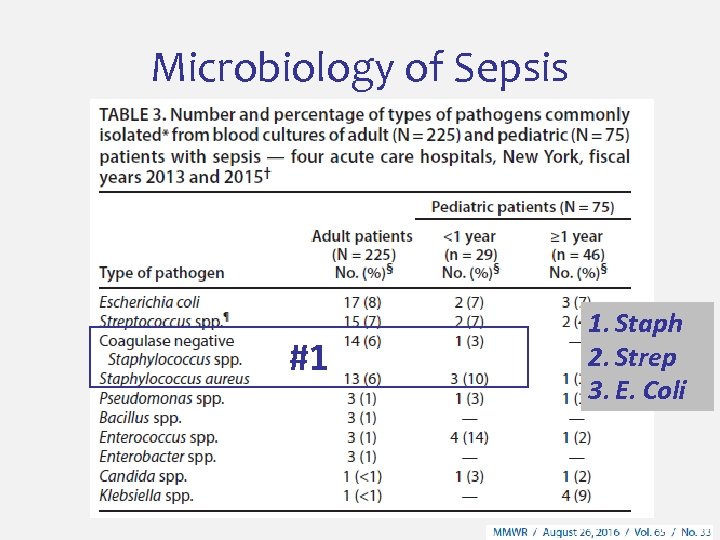 Microbiology of Sepsis #1 1. Staph 2. Strep 3. E. Coli
Microbiology of Sepsis #1 1. Staph 2. Strep 3. E. Coli
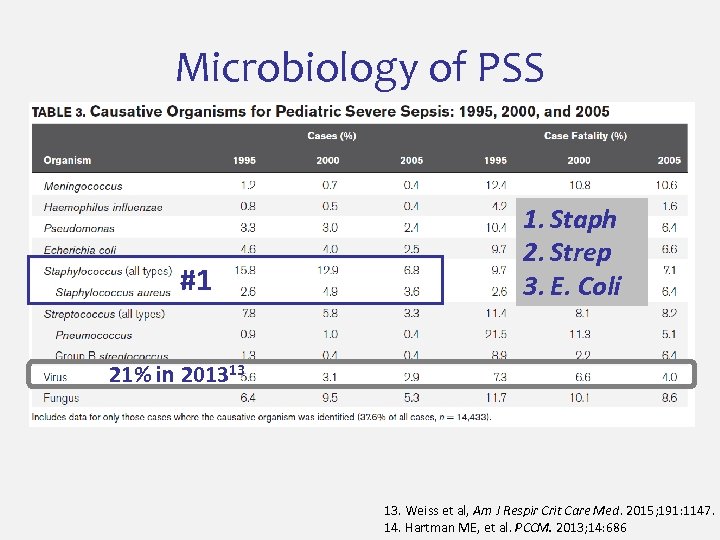 Microbiology of PSS #1 1. Staph 2. Strep 3. E. Coli 21% in 201313 13. Weiss et al, Am J Respir Crit Care Med. 2015; 191: 1147. 14. Hartman ME, et al. PCCM. 2013; 14: 686
Microbiology of PSS #1 1. Staph 2. Strep 3. E. Coli 21% in 201313 13. Weiss et al, Am J Respir Crit Care Med. 2015; 191: 1147. 14. Hartman ME, et al. PCCM. 2013; 14: 686
 Choice of Antibiotics • Broad spectrum – Gram + Gram - mixed infections • Depends on: – Local antibiograms – Suspected source – Patient circumstances
Choice of Antibiotics • Broad spectrum – Gram + Gram - mixed infections • Depends on: – Local antibiograms – Suspected source – Patient circumstances
![Risk Group Antibiotics Dosage Previously Healthy Ceftriaxone 50 mg/kg/dose IV [max 2000 mg] Vancomycin Risk Group Antibiotics Dosage Previously Healthy Ceftriaxone 50 mg/kg/dose IV [max 2000 mg] Vancomycin](https://present5.com/presentation/761ac2719d5e577c68c093bffef7f4ba/image-38.jpg) Risk Group Antibiotics Dosage Previously Healthy Ceftriaxone 50 mg/kg/dose IV [max 2000 mg] Vancomycin 15 mg/kg/dose IV [max 1500 mg] Vancomycin 15 mg/kg/dose [max 1500 mg] + + Immune Piperacillin/Tazobactam Compromised +/- 100 mg/kg/dose Piperacillin [max 4. 5 g] Tobramycin 2. 5 mg/kg/dose Vancomycin 15 mg/kg/dose IV [max 1500 mg] Ceftriaxone 50 mg/kg/dose [max 2000 mg] Azithromycin (? PNA) 10 mg/kg/dose [max 500 mg] Intraabdominal Piperacillin/Tazobactam 100 mg/kg/dose Piperacillin [max 4. 5 g] Neonate Ampicillin + Gent OR Cefotaxime 50 mg/kg/dose IV Sickle Cell + + 2. 5 mg/kg/dose IV / 50 mg/kg/dose IV Abstracted from Kaleida Health WCHOB Pediatric Severe Sepsis Protocol
Risk Group Antibiotics Dosage Previously Healthy Ceftriaxone 50 mg/kg/dose IV [max 2000 mg] Vancomycin 15 mg/kg/dose IV [max 1500 mg] Vancomycin 15 mg/kg/dose [max 1500 mg] + + Immune Piperacillin/Tazobactam Compromised +/- 100 mg/kg/dose Piperacillin [max 4. 5 g] Tobramycin 2. 5 mg/kg/dose Vancomycin 15 mg/kg/dose IV [max 1500 mg] Ceftriaxone 50 mg/kg/dose [max 2000 mg] Azithromycin (? PNA) 10 mg/kg/dose [max 500 mg] Intraabdominal Piperacillin/Tazobactam 100 mg/kg/dose Piperacillin [max 4. 5 g] Neonate Ampicillin + Gent OR Cefotaxime 50 mg/kg/dose IV Sickle Cell + + 2. 5 mg/kg/dose IV / 50 mg/kg/dose IV Abstracted from Kaleida Health WCHOB Pediatric Severe Sepsis Protocol
 Outpatient Sepsis Management 1. 2. 3. 4. Recognition Source identification Antibiotics Prompt referral to a higher level of care if showing signs of organ failure Early recognition and treatment is life-saving!
Outpatient Sepsis Management 1. 2. 3. 4. Recognition Source identification Antibiotics Prompt referral to a higher level of care if showing signs of organ failure Early recognition and treatment is life-saving!
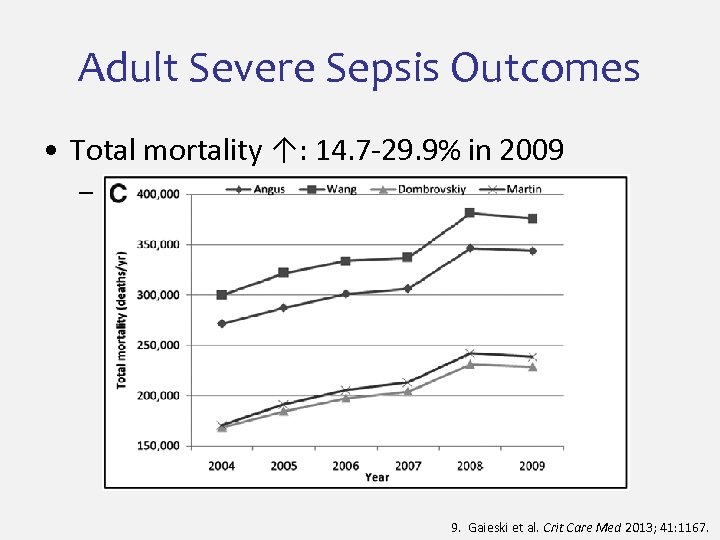 Adult Severe Sepsis Outcomes • Total mortality ↑: 14. 7 -29. 9% in 2009 – 229, 044 deaths in 2009 (#3 COD) 9. Gaieski et al. Crit Care Med 2013; 41: 1167.
Adult Severe Sepsis Outcomes • Total mortality ↑: 14. 7 -29. 9% in 2009 – 229, 044 deaths in 2009 (#3 COD) 9. Gaieski et al. Crit Care Med 2013; 41: 1167.
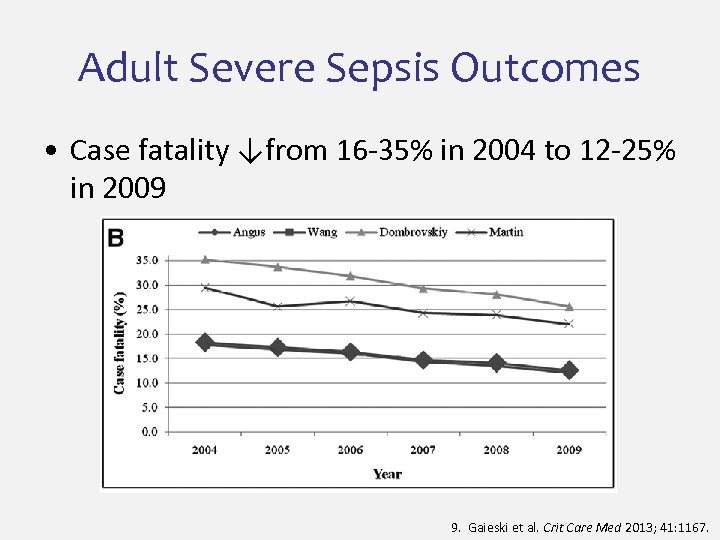 Adult Severe Sepsis Outcomes • Case fatality ↓from 16 -35% in 2004 to 12 -25% in 2009 9. Gaieski et al. Crit Care Med 2013; 41: 1167.
Adult Severe Sepsis Outcomes • Case fatality ↓from 16 -35% in 2004 to 12 -25% in 2009 9. Gaieski et al. Crit Care Med 2013; 41: 1167.
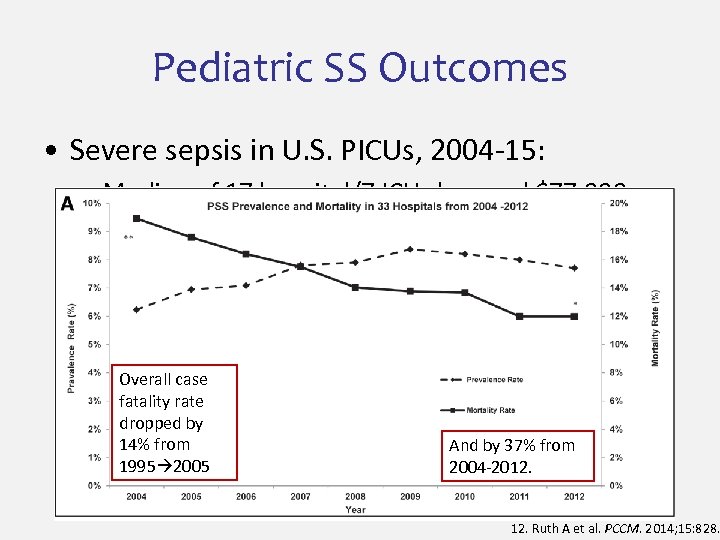 Pediatric SS Outcomes • Severe sepsis in U. S. PICUs, 2004 -15: – Median of 17 hospital/7 ICU days and $77, 000 – Mortality down-trending, but still >10% Overall case fatality rate dropped by 14% from 1995 2005 And by 37% from 2004 -2012. Ruth A et al. PCCM. 2014; 15: 828.
Pediatric SS Outcomes • Severe sepsis in U. S. PICUs, 2004 -15: – Median of 17 hospital/7 ICU days and $77, 000 – Mortality down-trending, but still >10% Overall case fatality rate dropped by 14% from 1995 2005 And by 37% from 2004 -2012. Ruth A et al. PCCM. 2014; 15: 828.
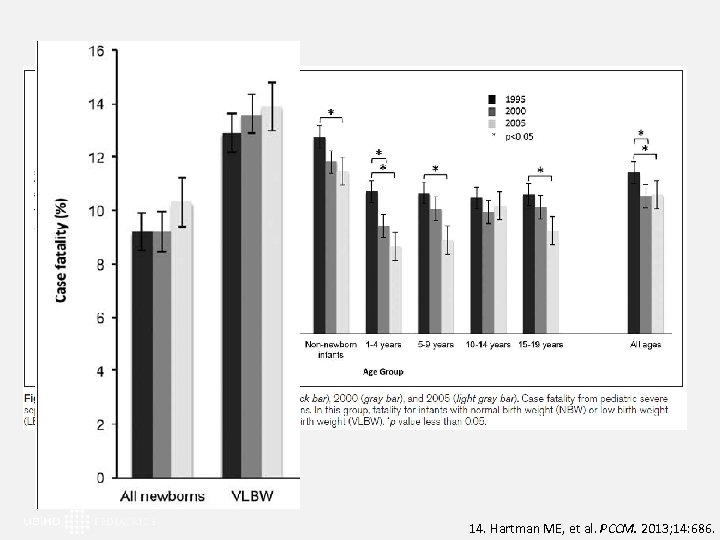 14. Hartman ME, et al. PCCM. 2013; 14: 686.
14. Hartman ME, et al. PCCM. 2013; 14: 686.
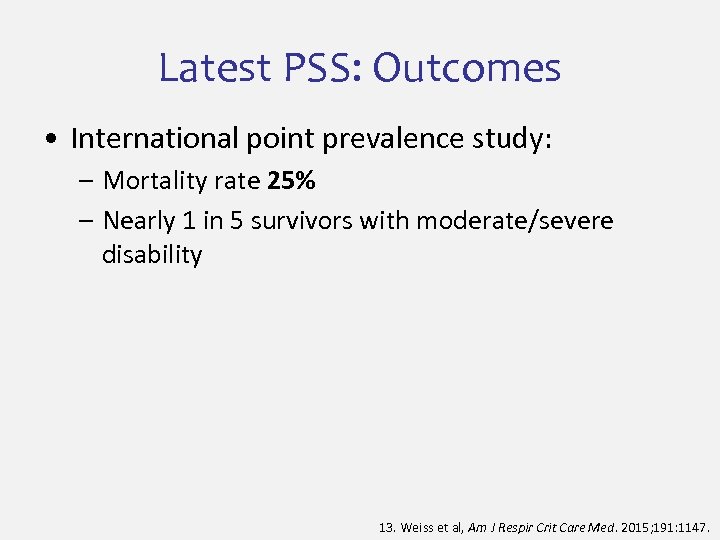 Latest PSS: Outcomes • International point prevalence study: – Mortality rate 25% – Nearly 1 in 5 survivors with moderate/severe disability 13. Weiss et al, Am J Respir Crit Care Med. 2015; 191: 1147.
Latest PSS: Outcomes • International point prevalence study: – Mortality rate 25% – Nearly 1 in 5 survivors with moderate/severe disability 13. Weiss et al, Am J Respir Crit Care Med. 2015; 191: 1147.
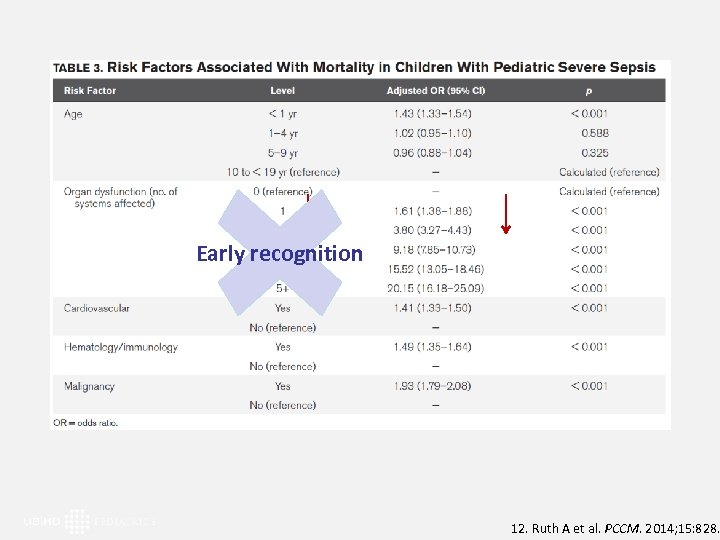 Early recognition 12. Ruth A et al. PCCM. 2014; 15: 828.
Early recognition 12. Ruth A et al. PCCM. 2014; 15: 828.
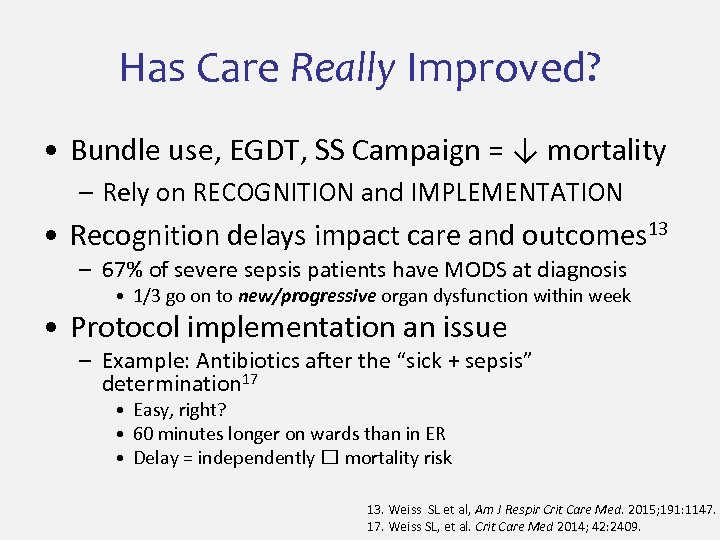 Has Care Really Improved? • Bundle use, EGDT, SS Campaign = ↓ mortality – Rely on RECOGNITION and IMPLEMENTATION • Recognition delays impact care and outcomes 13 – 67% of severe sepsis patients have MODS at diagnosis • 1/3 go on to new/progressive organ dysfunction within week • Protocol implementation an issue – Example: Antibiotics after the “sick + sepsis” determination 17 • Easy, right? • 60 minutes longer on wards than in ER • Delay = independently mortality risk 13. Weiss SL et al, Am J Respir Crit Care Med. 2015; 191: 1147. 17. Weiss SL, et al. Crit Care Med 2014; 42: 2409.
Has Care Really Improved? • Bundle use, EGDT, SS Campaign = ↓ mortality – Rely on RECOGNITION and IMPLEMENTATION • Recognition delays impact care and outcomes 13 – 67% of severe sepsis patients have MODS at diagnosis • 1/3 go on to new/progressive organ dysfunction within week • Protocol implementation an issue – Example: Antibiotics after the “sick + sepsis” determination 17 • Easy, right? • 60 minutes longer on wards than in ER • Delay = independently mortality risk 13. Weiss SL et al, Am J Respir Crit Care Med. 2015; 191: 1147. 17. Weiss SL, et al. Crit Care Med 2014; 42: 2409.
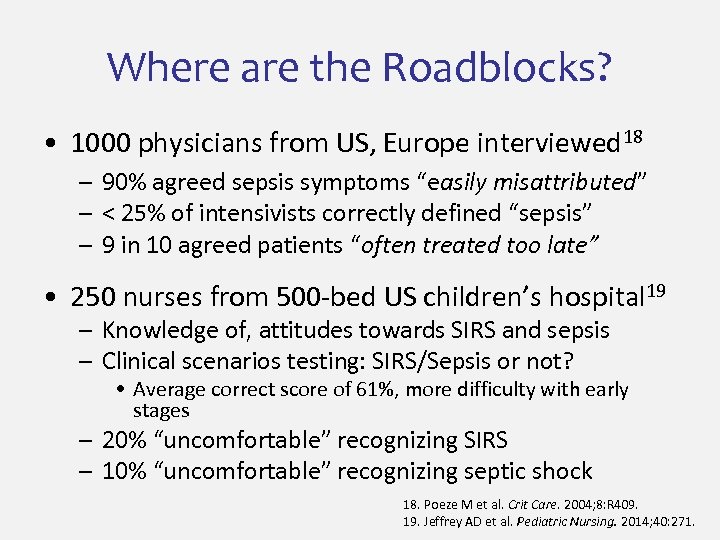 Where are the Roadblocks? • 1000 physicians from US, Europe interviewed 18 – 90% agreed sepsis symptoms “easily misattributed” – < 25% of intensivists correctly defined “sepsis” – 9 in 10 agreed patients “often treated too late” • 250 nurses from 500 -bed US children’s hospital 19 – Knowledge of, attitudes towards SIRS and sepsis – Clinical scenarios testing: SIRS/Sepsis or not? • Average correct score of 61%, more difficulty with early stages – 20% “uncomfortable” recognizing SIRS – 10% “uncomfortable” recognizing septic shock 18. Poeze M et al. Crit Care. 2004; 8: R 409. 19. Jeffrey AD et al. Pediatric Nursing. 2014; 40: 271.
Where are the Roadblocks? • 1000 physicians from US, Europe interviewed 18 – 90% agreed sepsis symptoms “easily misattributed” – < 25% of intensivists correctly defined “sepsis” – 9 in 10 agreed patients “often treated too late” • 250 nurses from 500 -bed US children’s hospital 19 – Knowledge of, attitudes towards SIRS and sepsis – Clinical scenarios testing: SIRS/Sepsis or not? • Average correct score of 61%, more difficulty with early stages – 20% “uncomfortable” recognizing SIRS – 10% “uncomfortable” recognizing septic shock 18. Poeze M et al. Crit Care. 2004; 8: R 409. 19. Jeffrey AD et al. Pediatric Nursing. 2014; 40: 271.
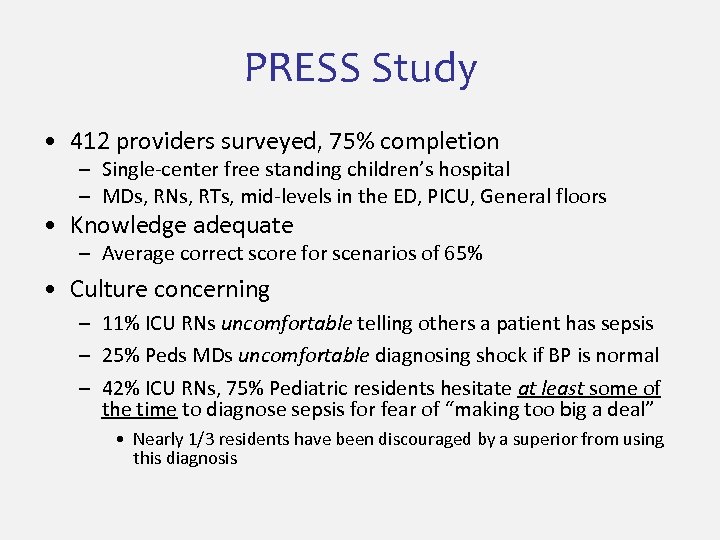 PRESS Study • 412 providers surveyed, 75% completion – Single-center free standing children’s hospital – MDs, RNs, RTs, mid-levels in the ED, PICU, General floors • Knowledge adequate – Average correct score for scenarios of 65% • Culture concerning – 11% ICU RNs uncomfortable telling others a patient has sepsis – 25% Peds MDs uncomfortable diagnosing shock if BP is normal – 42% ICU RNs, 75% Pediatric residents hesitate at least some of the time to diagnose sepsis for fear of “making too big a deal” • Nearly 1/3 residents have been discouraged by a superior from using this diagnosis
PRESS Study • 412 providers surveyed, 75% completion – Single-center free standing children’s hospital – MDs, RNs, RTs, mid-levels in the ED, PICU, General floors • Knowledge adequate – Average correct score for scenarios of 65% • Culture concerning – 11% ICU RNs uncomfortable telling others a patient has sepsis – 25% Peds MDs uncomfortable diagnosing shock if BP is normal – 42% ICU RNs, 75% Pediatric residents hesitate at least some of the time to diagnose sepsis for fear of “making too big a deal” • Nearly 1/3 residents have been discouraged by a superior from using this diagnosis
 To Make a Cultural Change… • Challenges to recognition and management everywhere – Inpatient & outpatient – Across disciplines, departments, provider roles WHERE DO WE GO FROM HERE?
To Make a Cultural Change… • Challenges to recognition and management everywhere – Inpatient & outpatient – Across disciplines, departments, provider roles WHERE DO WE GO FROM HERE?
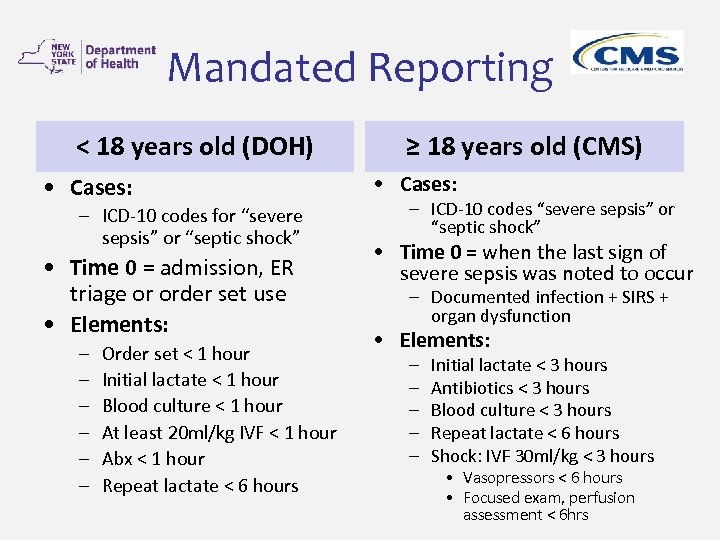 Mandated Reporting < 18 years old (DOH) • Cases: – ICD-10 codes for “severe sepsis” or “septic shock” • Time 0 = admission, ER triage or order set use • Elements: – – – Order set < 1 hour Initial lactate < 1 hour Blood culture < 1 hour At least 20 ml/kg IVF < 1 hour Abx < 1 hour Repeat lactate < 6 hours ≥ 18 years old (CMS) • Cases: – ICD-10 codes “severe sepsis” or “septic shock” • Time 0 = when the last sign of severe sepsis was noted to occur – Documented infection + SIRS + organ dysfunction • Elements: – – – Initial lactate < 3 hours Antibiotics < 3 hours Blood culture < 3 hours Repeat lactate < 6 hours Shock: IVF 30 ml/kg < 3 hours • Vasopressors < 6 hours • Focused exam, perfusion assessment < 6 hrs
Mandated Reporting < 18 years old (DOH) • Cases: – ICD-10 codes for “severe sepsis” or “septic shock” • Time 0 = admission, ER triage or order set use • Elements: – – – Order set < 1 hour Initial lactate < 1 hour Blood culture < 1 hour At least 20 ml/kg IVF < 1 hour Abx < 1 hour Repeat lactate < 6 hours ≥ 18 years old (CMS) • Cases: – ICD-10 codes “severe sepsis” or “septic shock” • Time 0 = when the last sign of severe sepsis was noted to occur – Documented infection + SIRS + organ dysfunction • Elements: – – – Initial lactate < 3 hours Antibiotics < 3 hours Blood culture < 3 hours Repeat lactate < 6 hours Shock: IVF 30 ml/kg < 3 hours • Vasopressors < 6 hours • Focused exam, perfusion assessment < 6 hrs
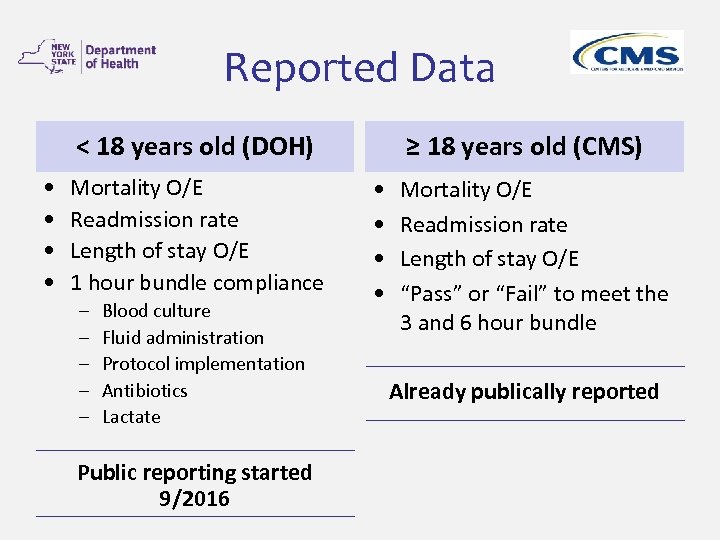 Reported Data < 18 years old (DOH) • • Mortality O/E Readmission rate Length of stay O/E 1 hour bundle compliance – – – Blood culture Fluid administration Protocol implementation Antibiotics Lactate Public reporting started 9/2016 ≥ 18 years old (CMS) • • Mortality O/E Readmission rate Length of stay O/E “Pass” or “Fail” to meet the 3 and 6 hour bundle Already publically reported
Reported Data < 18 years old (DOH) • • Mortality O/E Readmission rate Length of stay O/E 1 hour bundle compliance – – – Blood culture Fluid administration Protocol implementation Antibiotics Lactate Public reporting started 9/2016 ≥ 18 years old (CMS) • • Mortality O/E Readmission rate Length of stay O/E “Pass” or “Fail” to meet the 3 and 6 hour bundle Already publically reported
 TBD… What is the impact of state mandated reporting in an era of anti-microbial stewardship and overuse of ERs and UCC?
TBD… What is the impact of state mandated reporting in an era of anti-microbial stewardship and overuse of ERs and UCC?
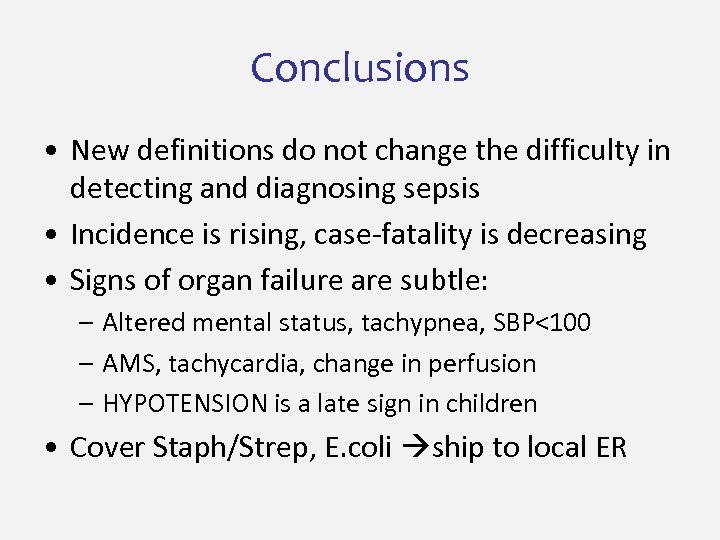 Conclusions • New definitions do not change the difficulty in detecting and diagnosing sepsis • Incidence is rising, case-fatality is decreasing • Signs of organ failure are subtle: – Altered mental status, tachypnea, SBP<100 – AMS, tachycardia, change in perfusion – HYPOTENSION is a late sign in children • Cover Staph/Strep, E. coli ship to local ER
Conclusions • New definitions do not change the difficulty in detecting and diagnosing sepsis • Incidence is rising, case-fatality is decreasing • Signs of organ failure are subtle: – Altered mental status, tachypnea, SBP<100 – AMS, tachycardia, change in perfusion – HYPOTENSION is a late sign in children • Cover Staph/Strep, E. coli ship to local ER
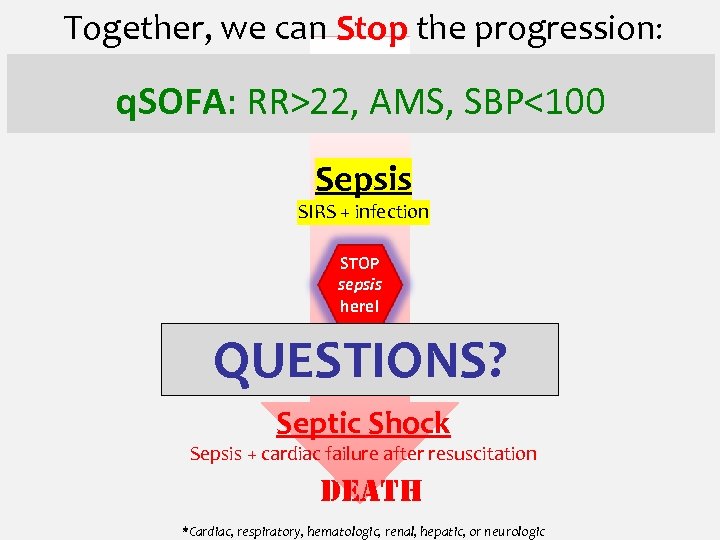 Together, we can Stop the progression: Systemic inflammatory response syndrome (SIRS) q. SOFA: or temp or or WBC RR>22, AMS, SBP<100 RR or HR Sepsis SIRS + infection STOP sepsis here! Severe Sepsis QUESTIONS? Sepsis + 2+ organ failures* Septic Shock Sepsis + cardiac failure after resuscitation DEATH *Cardiac, respiratory, hematologic, renal, hepatic, or neurologic
Together, we can Stop the progression: Systemic inflammatory response syndrome (SIRS) q. SOFA: or temp or or WBC RR>22, AMS, SBP<100 RR or HR Sepsis SIRS + infection STOP sepsis here! Severe Sepsis QUESTIONS? Sepsis + 2+ organ failures* Septic Shock Sepsis + cardiac failure after resuscitation DEATH *Cardiac, respiratory, hematologic, renal, hepatic, or neurologic
 References 1. Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992; 101: 1644 -1655. 2. Goldstein B, Giroir B, Randolph A. International Consensus Conference on Pediatric Sepsis. International Pediatric Sepsis Consensus Conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 2005; 6: 2 -8. 3. Dulhunty JM, Lipman J, Finfer S. Does severe non-infectious SIRS differ from severe sepsis? Results from a multi-centre Australian and New Zealand intensive care unit study. Intensive Care Med. 2008; 34: 1654 -61. 4. Sprung CL, Sakr Y, Vincent JL, Le Gall JR, Reinhart K, Ranieri VM, et al. An evaluation of systemic inflammatory response syndrome signs in the Sepsis Occurrence in Acutely Ill Patients (SOAP) study. Intensive Care Med. 2006; 32: 421 -7. 5. Churpek MM, Zadravecz FJ, Winslow C, Howell MD, Edelson DP. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015; 192: 958 -64. 6. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315(8): 801 -810. 7. Vincent JL, Martin GS, Levy MM. q. SOFA does not replace SIRS in the definition of sepsis. Critical Care. 2016; 20: 210. 8. Vincent JL, Opal S, Marshall JC, Tracey KJ. Sepsis definitions: time for change. Lancet 2013; 381: 774 -5 9. Gaieski DF, Edwards JM, Kallan MJ, Carr BG. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013; 41: 1167 -1174.
References 1. Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992; 101: 1644 -1655. 2. Goldstein B, Giroir B, Randolph A. International Consensus Conference on Pediatric Sepsis. International Pediatric Sepsis Consensus Conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 2005; 6: 2 -8. 3. Dulhunty JM, Lipman J, Finfer S. Does severe non-infectious SIRS differ from severe sepsis? Results from a multi-centre Australian and New Zealand intensive care unit study. Intensive Care Med. 2008; 34: 1654 -61. 4. Sprung CL, Sakr Y, Vincent JL, Le Gall JR, Reinhart K, Ranieri VM, et al. An evaluation of systemic inflammatory response syndrome signs in the Sepsis Occurrence in Acutely Ill Patients (SOAP) study. Intensive Care Med. 2006; 32: 421 -7. 5. Churpek MM, Zadravecz FJ, Winslow C, Howell MD, Edelson DP. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015; 192: 958 -64. 6. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315(8): 801 -810. 7. Vincent JL, Martin GS, Levy MM. q. SOFA does not replace SIRS in the definition of sepsis. Critical Care. 2016; 20: 210. 8. Vincent JL, Opal S, Marshall JC, Tracey KJ. Sepsis definitions: time for change. Lancet 2013; 381: 774 -5 9. Gaieski DF, Edwards JM, Kallan MJ, Carr BG. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013; 41: 1167 -1174.
 References 10. Gohil SK, Cao C, Phelan M, Tjoa T, Rhee C, Platt R, Huang SS for the Centers for Disease Control and Prevention Epicenters Program. Impact of policies on the rise in sepsis incidence, 2000 -2010. Clin Infect Dis. 2016; 62(6): 695 -703. 11. Cluzet VC, Lautenbach E. We are seeing more sepsis… but are we seeing the whole picture? Clin Infect Dis. 2016; 62(6): 704 -6. 12. Ruth A, Mc. Cracken CE, Fortenberry JD, et al. Pediatric severe sepsis: current trends and outcomes from the Pediatric Health Information Systems database. Pediatr Crit Care Med 2014; 15: 828 -838. 13. Weiss SL, Fitzgerald JC, Pappachan J, et al. Global epidemiology of pediatric severe sepsis: The sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med 2015; 191: 1147 -1157. 14. Hartman ME, Linde-Zwirble WT, Angus DC, Watson RS: Trends in the epidemiology of pediatric severe sepsis. Pediatr Crit Care Med 2013, 14(7): 686 -693. 15. Novosad SA, Sapiano MRP, Grigg C, Lake J et al. Vital signs: Epidemiology of Sepsis: Prevalence of health care factors and opportunities for prevention. MMWR 2016; 65: 33: 864 -869. 16. Dellinger et al for the International Surviving Sepsis Campaign Guidelines Committee. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock. Intensive Care Med 2013; 39(2): 165 -228. 17. Weiss SL, Fitzgerald JC, Balamuth F, et al. Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit Care Med 2014; 42: 2409 -2417. 18. Poeze M, Ramsay G, Gerlach H, et al. An international sepsis survey: A study of doctors’ knowledge and perception about sepsis. Critical Care 2004; 8: R 409 -R 413. 19. Jeffrey AD, Mutsch KS, Knapp L. Knowledge and recognition of SIRS and sepsis among pediatric nurses. Pediatric Nursing 2014; 40: 271 -278.
References 10. Gohil SK, Cao C, Phelan M, Tjoa T, Rhee C, Platt R, Huang SS for the Centers for Disease Control and Prevention Epicenters Program. Impact of policies on the rise in sepsis incidence, 2000 -2010. Clin Infect Dis. 2016; 62(6): 695 -703. 11. Cluzet VC, Lautenbach E. We are seeing more sepsis… but are we seeing the whole picture? Clin Infect Dis. 2016; 62(6): 704 -6. 12. Ruth A, Mc. Cracken CE, Fortenberry JD, et al. Pediatric severe sepsis: current trends and outcomes from the Pediatric Health Information Systems database. Pediatr Crit Care Med 2014; 15: 828 -838. 13. Weiss SL, Fitzgerald JC, Pappachan J, et al. Global epidemiology of pediatric severe sepsis: The sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med 2015; 191: 1147 -1157. 14. Hartman ME, Linde-Zwirble WT, Angus DC, Watson RS: Trends in the epidemiology of pediatric severe sepsis. Pediatr Crit Care Med 2013, 14(7): 686 -693. 15. Novosad SA, Sapiano MRP, Grigg C, Lake J et al. Vital signs: Epidemiology of Sepsis: Prevalence of health care factors and opportunities for prevention. MMWR 2016; 65: 33: 864 -869. 16. Dellinger et al for the International Surviving Sepsis Campaign Guidelines Committee. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock. Intensive Care Med 2013; 39(2): 165 -228. 17. Weiss SL, Fitzgerald JC, Balamuth F, et al. Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit Care Med 2014; 42: 2409 -2417. 18. Poeze M, Ramsay G, Gerlach H, et al. An international sepsis survey: A study of doctors’ knowledge and perception about sepsis. Critical Care 2004; 8: R 409 -R 413. 19. Jeffrey AD, Mutsch KS, Knapp L. Knowledge and recognition of SIRS and sepsis among pediatric nurses. Pediatric Nursing 2014; 40: 271 -278.


