fea51575421a8f1eacc151d71b0857cf.ppt
- Количество слайдов: 60
Senses and Sense-ability: Low Vision Rehabilitation Tiffany L. Chan, O. D. , F. A. A. O. Assistant Professor of Ophthalmology Lions Vision Rehabilitation Center The Wilmer Eye Institute, Johns Hopkins University
Goals for today’s talk Understand the utility of Low Vision Rehabilitation Identify Low Vision patients Gain knowledge about educating and counseling patients with vision loss (Patient case example)
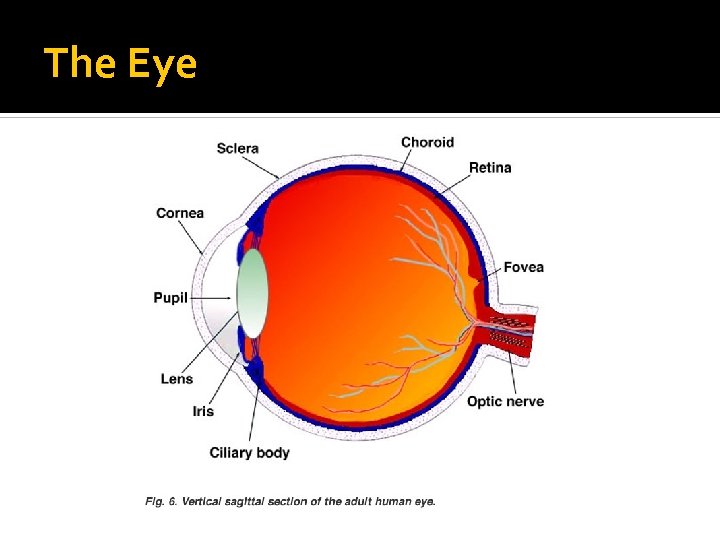
The Eye
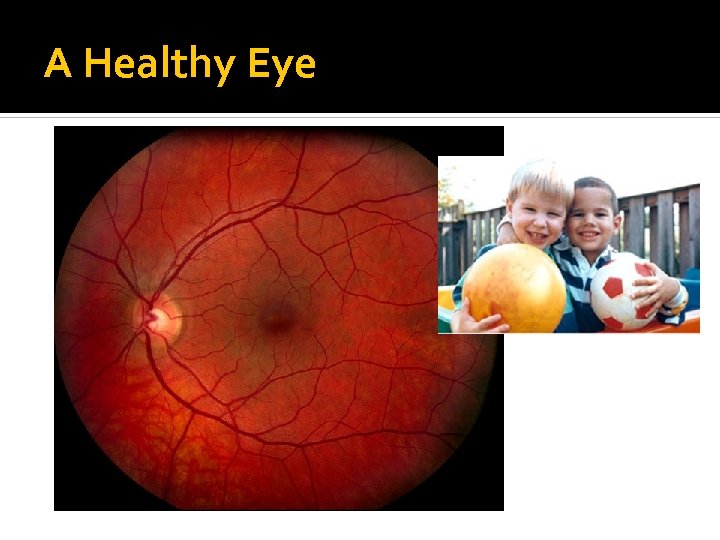
A Healthy Eye
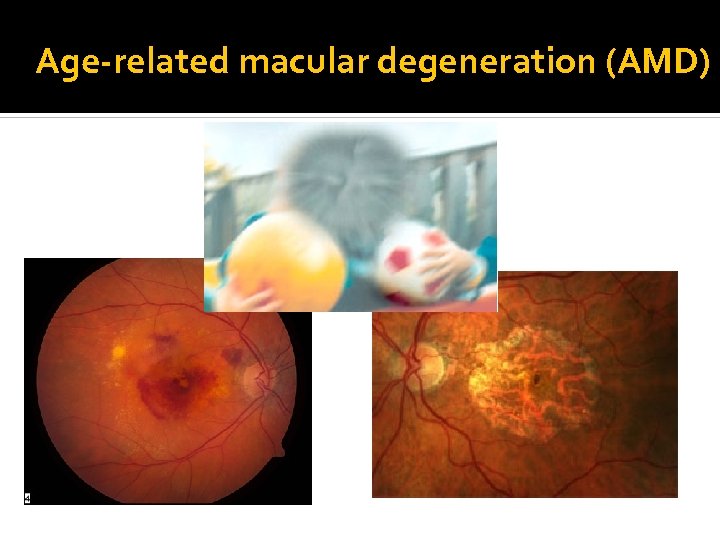
Age-related macular degeneration (AMD)
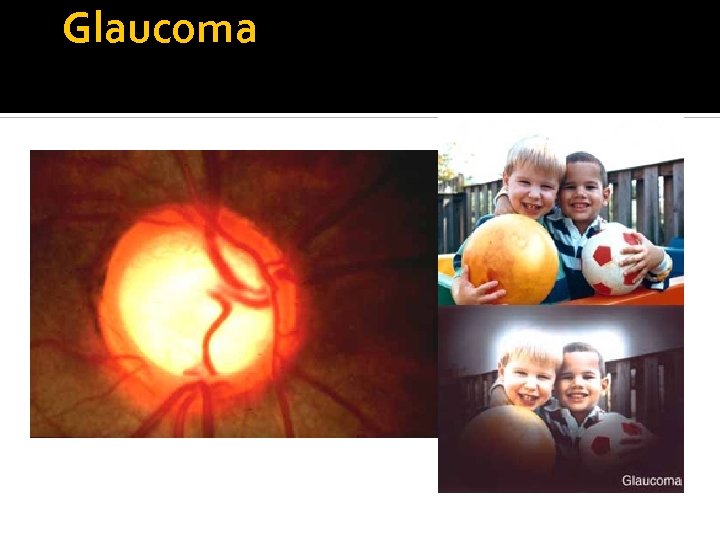
Glaucoma
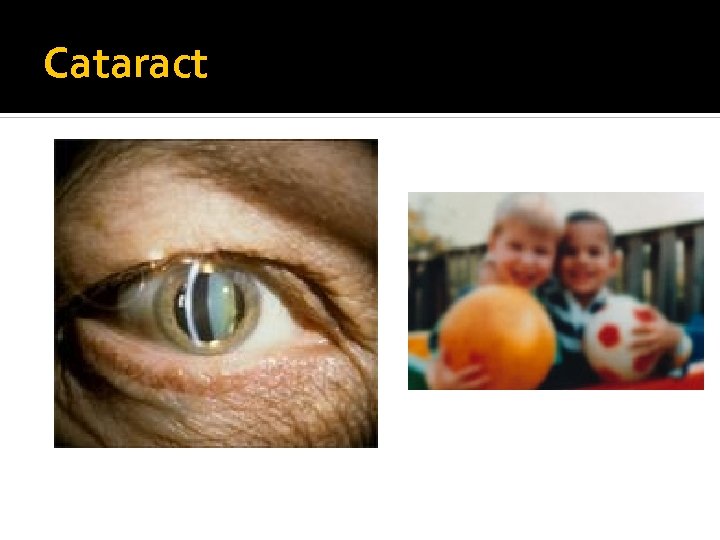
Cataract
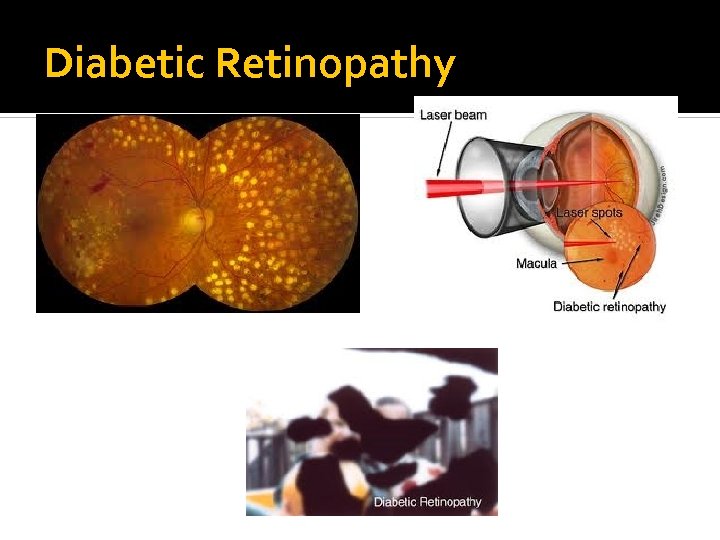
Diabetic Retinopathy
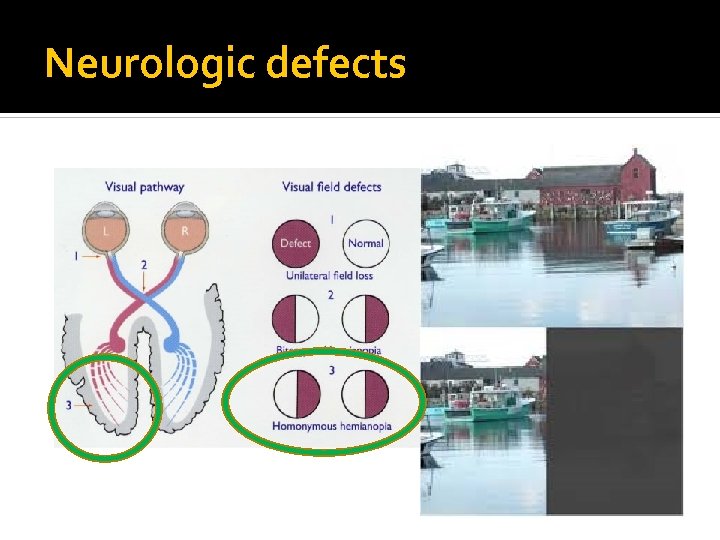
Neurologic defects
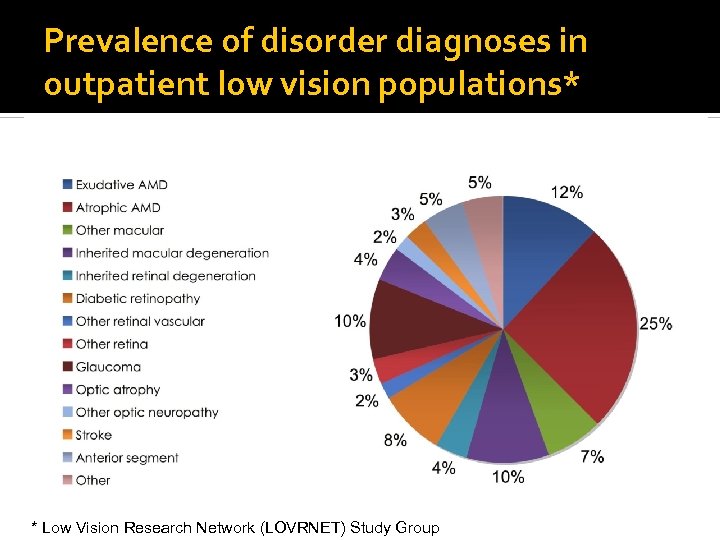
Prevalence of disorder diagnoses in outpatient low vision populations* * Low Vision Research Network (LOVRNET) Study Group
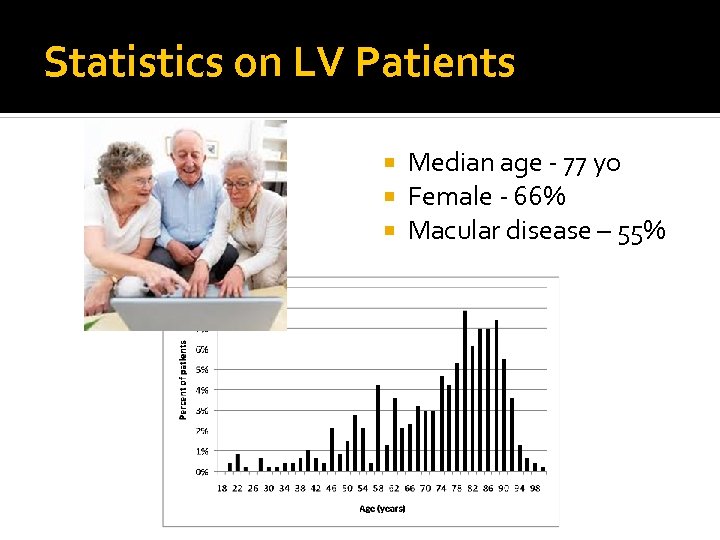
Statistics on LV Patients Median age - 77 yo Female - 66% Macular disease – 55%
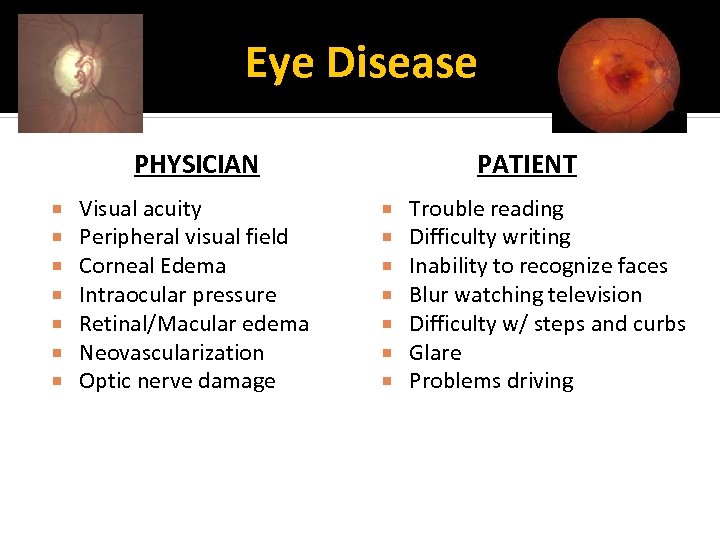
Eye Disease PHYSICIAN Visual acuity Peripheral visual field Corneal Edema Intraocular pressure Retinal/Macular edema Neovascularization Optic nerve damage PATIENT Trouble reading Difficulty writing Inability to recognize faces Blur watching television Difficulty w/ steps and curbs Glare Problems driving
Defining “Low Vision” (LV) Any chronic uncorrectable visual impairment that limits daily functioning ▪ When ordinary eyeglasses, contact lenses or surgery cannot provide sharp vision
Low Vision Facts Leading cause of disability in daily living among Americans The WHO estimates that over 135 million people are visually disabled, and nearly 45 million people are blind Incidence of LV cases from age-related eye disease is expected to double over the next 25 years
Vision Impairment • Can cause major safety concerns ▪ Increased risk of falls ▪ Difficulty with medication management ▪ Kitchen accidents Stove/oven turned off Cutting food Seeing when food is properly cooked
The “Team” approach to care Nurses Physicians ▪ Ophthalmology, PM&R, Geriatric Medicine, etc. Low Vision specialists Occupational, Physical, Rehabilitation Therapists; Speech and Language Pathologists Orientation and Mobility specialist Social workers Teachers for the Visually Impaired
Goal of Low Vision Rehab To maximize the patient’s remaining sight to enhance function and independence ▪ Visually assistive equipment (VAE) ▪ Sensory substitution (i. e. Hearing or touch) No surgical or medical interventions Not “fixing” vision
When to refer patients? Problems with activities of daily living Difficulty reading and writing Driving concerns / questionable renewals Safety in mobility Evaluating rehab options in high risk eye procedures Post –procedure with remaining vision impairment
Low Vision Examination
Clinical Evaluation of the Low Vision Patient Observations Case History Visual Acuity measure(s) Contrast sensitivity Refraction Visual Field Medical evaluation Assessment/Plan
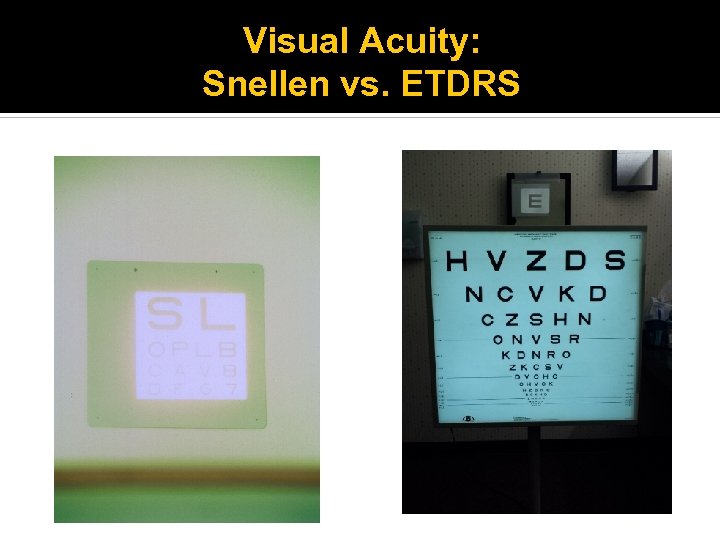
Visual Acuity: Snellen vs. ETDRS

Trial Frame Refraction
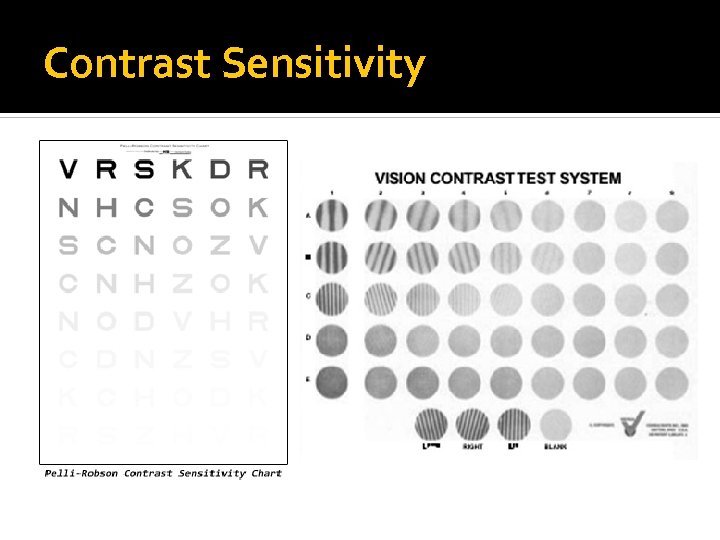
Contrast Sensitivity
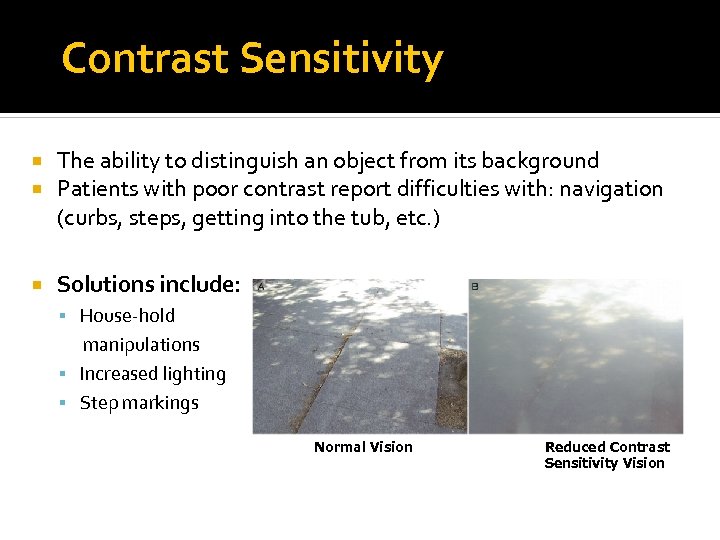
Contrast Sensitivity The ability to distinguish an object from its background Patients with poor contrast report difficulties with: navigation (curbs, steps, getting into the tub, etc. ) Solutions include: House-hold manipulations Increased lighting Step markings Normal Vision Reduced Contrast Sensitivity Vision
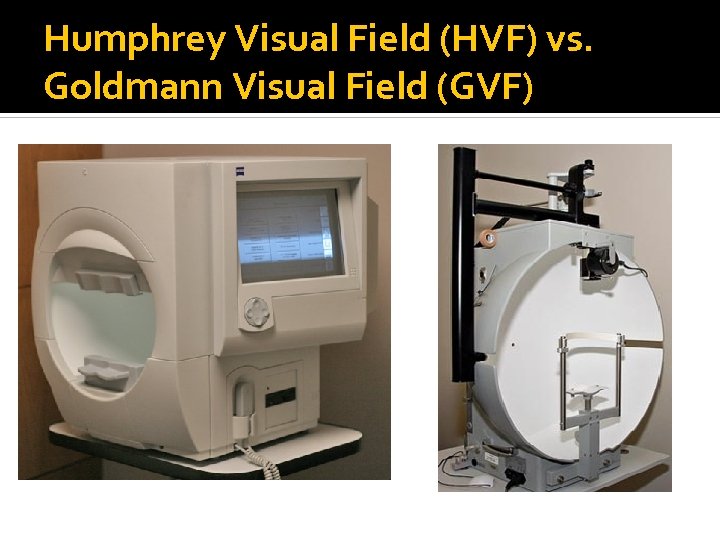
Humphrey Visual Field (HVF) vs. Goldmann Visual Field (GVF)
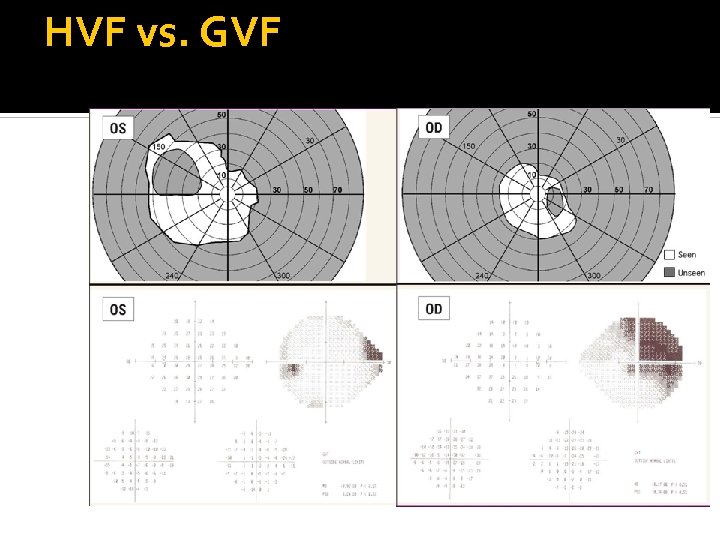
HVF vs. GVF
Low Vision Therapy Magnification Contrast Enhancement Lighting Control Glare Non-optical aids Recommend Appropriate Resources
Reading Spot reading Sorting Mail Reading a Menu Medication Label Continuous Text Reading (Leisure reading) Books Magazines Newspaper
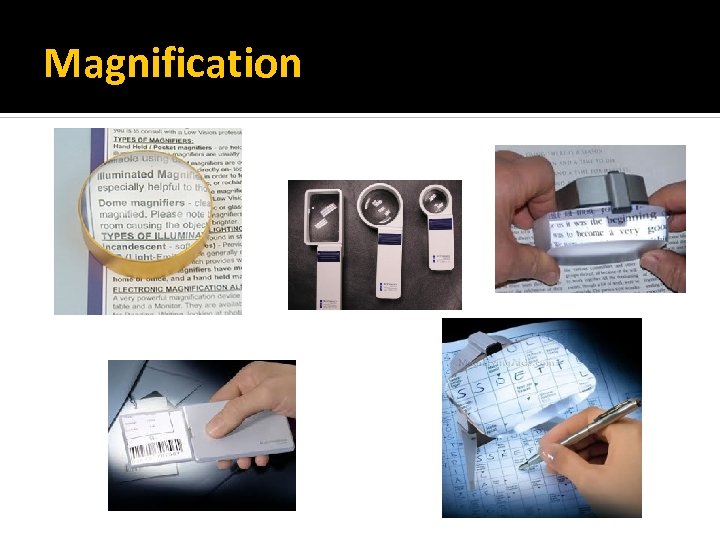
Magnification
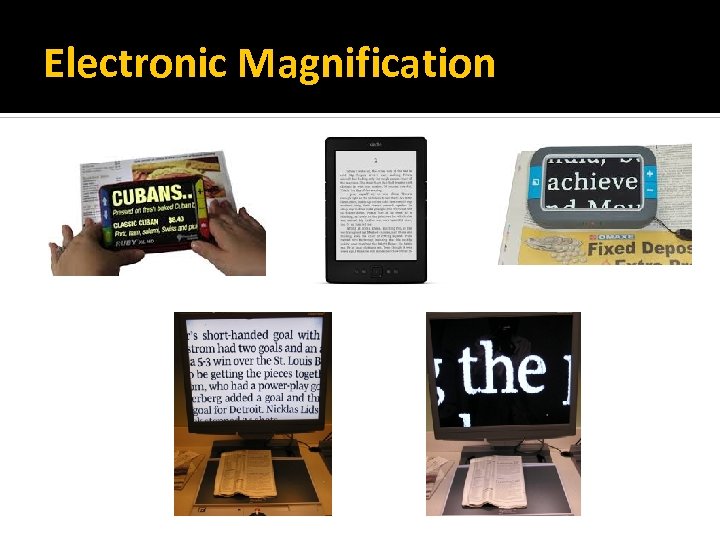
Electronic Magnification
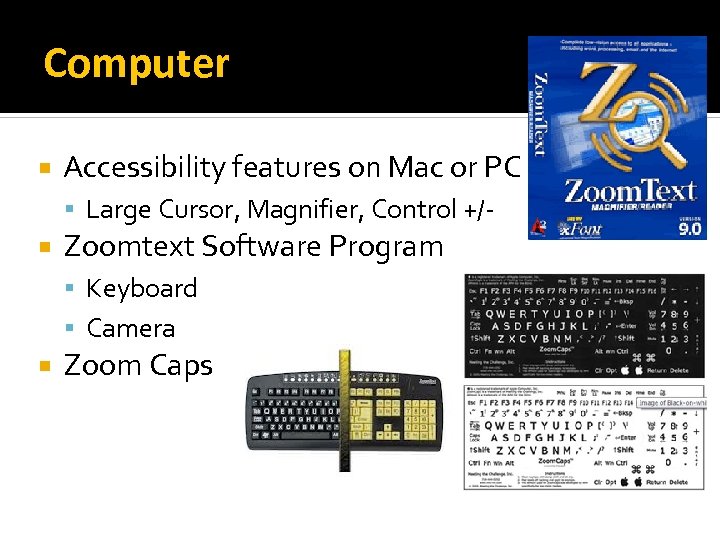
Computer Accessibility features on Mac or PC Large Cursor, Magnifier, Control +/- Zoomtext Software Program Keyboard Camera Zoom Caps
Writing 20/20 Pens Bold lined paper Line guides Large print checks

Home Safety
Community Mobility Sighted Guide Visual Scanning Strategies Within the clinic Navigate throughout hospital Orientation and Mobility Specialist
Division of Rehabilitation Services (DORS) Vocational Rehabilitation (≤ 55 yo) Goal: maintain or re-gain employment Provision of visually assistive equipment (VAE) Work-site assessment Career training / Job placement assistance Independent Living Older Blind (>55 yo) Goal: Independence Provision of visually assistive equipment (VAE) Home Visit (ADLs / safety)
Blind Industries and Services of Maryland (BISM) Non-visual skills training • Computer (JAWS) • Braille • Orientation &Mobility / travel • Cooking Educational seminars/ Field Trips • Diabetes management • Baltimore Museum of Art
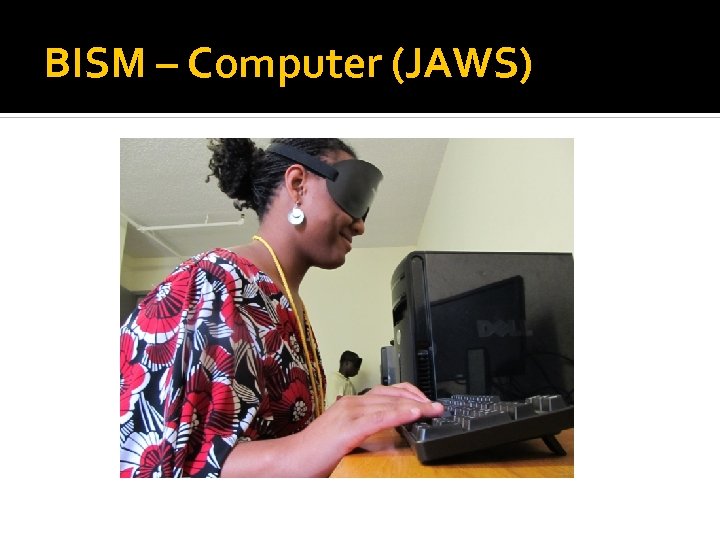
BISM – Computer (JAWS)
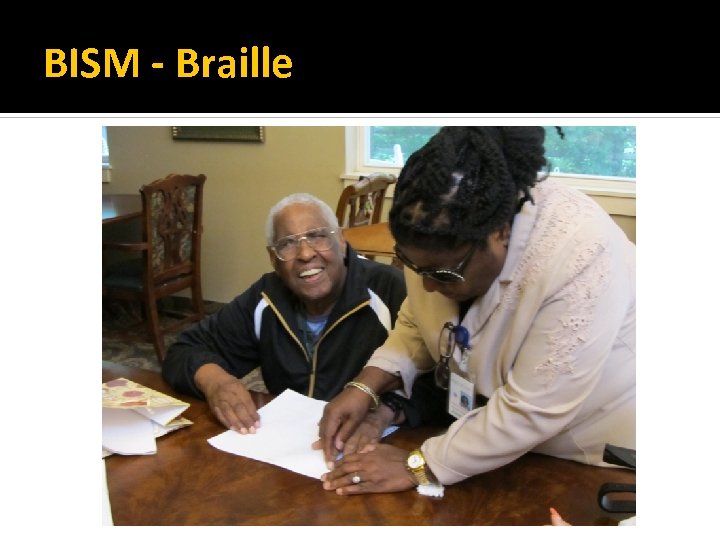
BISM - Braille

BISM – Orientation & Mobility
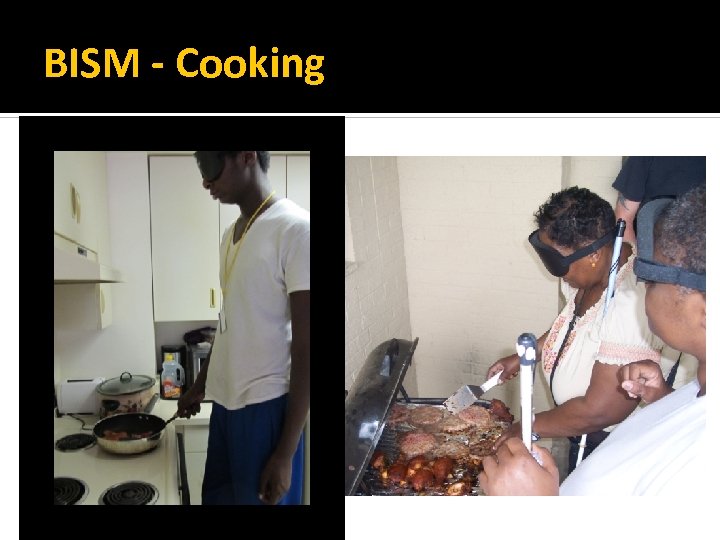
BISM - Cooking

BISM - Zipline
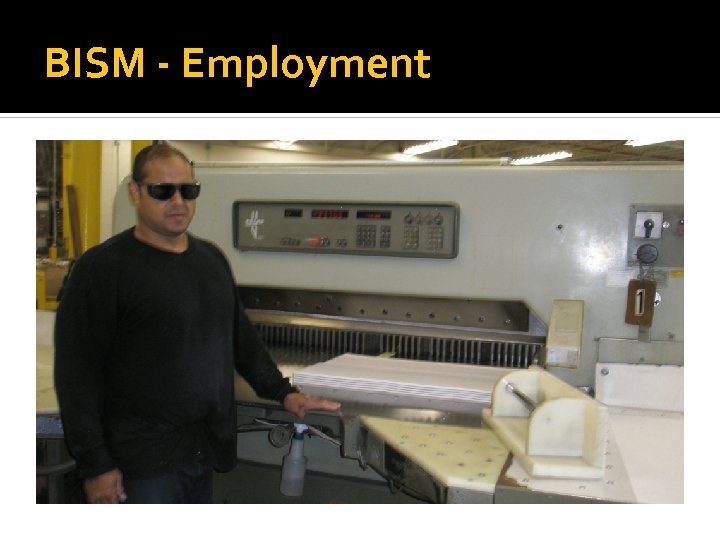
BISM - Employment
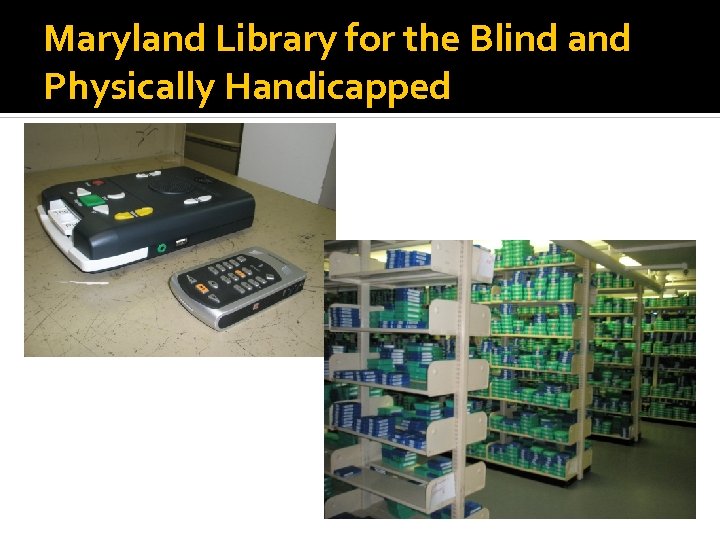
Maryland Library for the Blind and Physically Handicapped
The Seeing Eye – Dog Guide
Additional Resources Veterans Affairs Medical Center (VAMC) Division of Rehabilitation Services (DORS) Blind Industries and Services of Maryland (BISM) Maryland Library for the Blind and Physically Handicapped Orientation and Mobility (O&M) Guide dogs (e. g. “The Seeing Eye”) Driving evaluation/training Support groups Social Workers State and Federal Organizations

Vision Rehabilitation Service • Dr. Judith Goldstein • E. Baltimore • Green Spring Station • Dr. Tiffany Chan • E. Baltimore • Bel Air • Bayview • Dr. Alexis Malkin • E. Baltimore • Dr. Nicole Ross (Fellow) • E. Baltimore • Green Spring Station • Jim Deremeik • Rehabilitation Therapist • Kristen Lindeman • Occupational Therapist • Kim Soistman • Staff • Chantal Haberman • Office Manager
Conclusion • The goals of LVR are to maximize function and independence LVR “Treatment” ▪ Visually assistive equipment ▪ Visual skills training ▪ Referral to appropriate resources There is always something that can be done!!
Questions?
Patient Case
Mrs. Smith 84 yo Caucasian female CC: Trouble reading • Books, newspapers • Menus at restaurants • Medication bottles Referred by Wilmer Retina Service • Non-neovascular age-related macular degeneration (AMD) both eyes • Dense cataract both eyes (patient does not want surgery)
Low Vision Functional History Reading / Computer • Difficulty reading books and newspaper (has • • given up reading for pleasure) Able to read headlines and large print Difficulty reading menus at restaurants Cannot read medication bottles Tried an OTC magnifier, but didn’t seem to help much Visual Information / Seeing Driving Mobility Visual Motor Skills / ADLs
Low Vision Functional History Reading / Computer Visual Information / Seeing • Watches a large, 52” television, sitting 14 feet away • Sometimes moves closer, like when an Oriole’s game is on Driving Mobility Visual Motor Skills / ADLs
Low Vision Functional History Reading / Computer Visual Information / Seeing Driving • Very limited to local and familiar areas (i. e. grocery store, church, etc. ) • Family lives near-by and can drive her Mobility Visual Motor Skills / ADLs
Low Vision Functional History Reading / Computer Visual Information / Seeing Driving Mobility • No falls • Travels independently • More careful walking on poorly lit curbs or stairs • Glare: wears transition lenses and feels they darken sufficiently in the bright sunlight Visual Motor Skills / ADLs
Low Vision Functional History Reading / Computer Visual Information / Seeing Driving Mobility Visual Motor Skills / ADLs • Lives alone in a two story house (family lives near-by) • Manages ADLs independently (cooking, laundry, shopping, etc. ) • Difficulty seeing appliances, especially in poor lighting • Sometimes hard to read labels and price tags at the grocery store
Medical History • Diabetes mellitus (oral meds) • Hypertension • High Cholesterol • Manages own meds • Tries to keep pill bottles organized • Sometimes forgets if she has taken a pill • Rarely measures blood sugar • Hard to see the glucometer
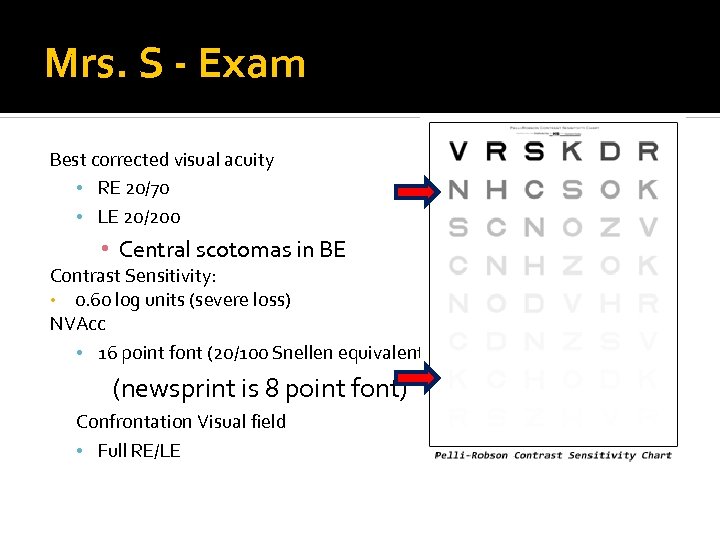
Mrs. S - Exam Best corrected visual acuity • RE 20/70 • LE 20/200 • Central scotomas in BE Contrast Sensitivity: • 0. 60 log units (severe loss) NVAcc • 16 point font (20/100 Snellen equivalent) (newsprint is 8 point font) Confrontation Visual field • Full RE/LE
LVR Recommendations (a. k. a. continuous reading) • E-reader (i. e. Kindle) Pleasure reading: • Increased font • Reverse contrast • • Large print books Directed light source Spot reading: • Illuminated hand magnifier ▪ For medication bottles, menus and packaged directions
LVR Recommendations Medication Management • • Pill Box Large print/Talking glucometer (additional resources if IDDM: Insulin pen (hear clicks)) Home Visit • • • Mark appliances Assess lighting Safety evaluation
Thank you!
fea51575421a8f1eacc151d71b0857cf.ppt