d7e94133b7fafd8dd36f5b2f526ac511.ppt
- Количество слайдов: 48
 Self Harm AWARENESS Frances Dodd & Rachael Wall – Primary Mental Health Workers
Self Harm AWARENESS Frances Dodd & Rachael Wall – Primary Mental Health Workers
 Learning Aims: • To define what self-harm is. • To look at signs and symptoms that children and young people (CYP) may present with. • What to say to them. • Who to share information with. • Where to signpost. • To raise awareness of the value of self-harm to CYP. • To raise awareness of potential trigger times. • To look at suggested ways of working with CYP that self-harm. • To reflect on our own feelings when working with CYP that self-harm. • To recognise our professional boundaries and when to ask for support. The overall aim of this session is to increase awareness with regard to self-harm amongst universal staff to facilitate positive work with CYP in an integrated way that best supports their needs
Learning Aims: • To define what self-harm is. • To look at signs and symptoms that children and young people (CYP) may present with. • What to say to them. • Who to share information with. • Where to signpost. • To raise awareness of the value of self-harm to CYP. • To raise awareness of potential trigger times. • To look at suggested ways of working with CYP that self-harm. • To reflect on our own feelings when working with CYP that self-harm. • To recognise our professional boundaries and when to ask for support. The overall aim of this session is to increase awareness with regard to self-harm amongst universal staff to facilitate positive work with CYP in an integrated way that best supports their needs
 What is Self-Harm? Self-harm describes a wide range of things that people do to themselves in a deliberate and usually hidden way. In the vast majority of cases self-harm remains a secretive behaviour that can go on for a long time without being discovered. Self-harm can involve: • • Cutting, often to the arms using razor blades, or broken glass. Burning using cigarettes or caustic agents. Punching and bruising. Inserting or swallowing objects. Head banging. Hair pulling. Restrictive or binge eating. Overdosing. (Mental Health Foundation 2006)
What is Self-Harm? Self-harm describes a wide range of things that people do to themselves in a deliberate and usually hidden way. In the vast majority of cases self-harm remains a secretive behaviour that can go on for a long time without being discovered. Self-harm can involve: • • Cutting, often to the arms using razor blades, or broken glass. Burning using cigarettes or caustic agents. Punching and bruising. Inserting or swallowing objects. Head banging. Hair pulling. Restrictive or binge eating. Overdosing. (Mental Health Foundation 2006)
 • Self-injury is any act which involves deliberately inflicting pain and/or injury to one’s own body, but without suicidal intent. (Working with self-injury: A Practice Guide L. Arnold & A. Magill, 1996) • Self-injury is an expression of acute psychological distress. It is an act done to oneself, by oneself, with the intention of helping oneself rather than killing oneself. Paradoxically, damage is done to the body in an attempt to preserve the integrity of the mind. (Sutton & Martinson 2003)
• Self-injury is any act which involves deliberately inflicting pain and/or injury to one’s own body, but without suicidal intent. (Working with self-injury: A Practice Guide L. Arnold & A. Magill, 1996) • Self-injury is an expression of acute psychological distress. It is an act done to oneself, by oneself, with the intention of helping oneself rather than killing oneself. Paradoxically, damage is done to the body in an attempt to preserve the integrity of the mind. (Sutton & Martinson 2003)
 Incidence • It's almost impossible to say how many young people are self-harming. This is because very few CYP tell anyone what's going on, so it's incredibly difficult to keep records or have an accurate idea of scale. • Studies indicate 1 in 15 young people within the general population have engaged in self harm behaviour. In 2014, figures were published suggesting a 70% increase in 10 -14 year olds attending A&E for self-harm related reasons over the preceding 2 years. • Rare in children under 12 years of age. • Risk increases during adolescence. • Self harm behaviour more common in females (5: 1). • Often repeat attempts.
Incidence • It's almost impossible to say how many young people are self-harming. This is because very few CYP tell anyone what's going on, so it's incredibly difficult to keep records or have an accurate idea of scale. • Studies indicate 1 in 15 young people within the general population have engaged in self harm behaviour. In 2014, figures were published suggesting a 70% increase in 10 -14 year olds attending A&E for self-harm related reasons over the preceding 2 years. • Rare in children under 12 years of age. • Risk increases during adolescence. • Self harm behaviour more common in females (5: 1). • Often repeat attempts.
 What is acceptable? • The cutting, carving and scratching of skin can be an attempt to control overwhelming emotions, feelings of helplessness, and for some is a way to manage anger or shame. Cutting is a way to manage self-punishment, self-hate or selfnurturance. In its simplest form, cutting is a physical solution to a psychic wound. It is a deliberate, private act that can be habitual or isolated in occurrence. It is not attention seeking behaviour, not meant to be manipulative, nor is it a conscious attempt to end one’s life. (Azar, 1995; Carll, 2003; Froeschle & Moyer, 2004; Kress White, 2003; Levenkron, 1999; Strong 1999)
What is acceptable? • The cutting, carving and scratching of skin can be an attempt to control overwhelming emotions, feelings of helplessness, and for some is a way to manage anger or shame. Cutting is a way to manage self-punishment, self-hate or selfnurturance. In its simplest form, cutting is a physical solution to a psychic wound. It is a deliberate, private act that can be habitual or isolated in occurrence. It is not attention seeking behaviour, not meant to be manipulative, nor is it a conscious attempt to end one’s life. (Azar, 1995; Carll, 2003; Froeschle & Moyer, 2004; Kress White, 2003; Levenkron, 1999; Strong 1999)
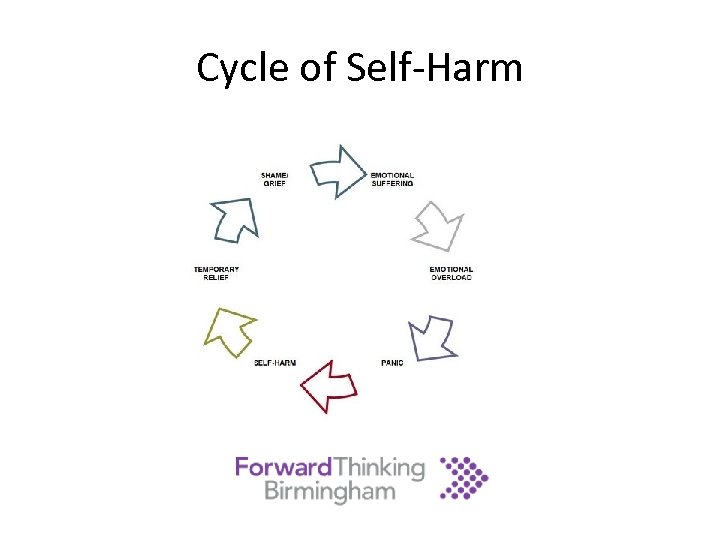 Cycle of Self-Harm
Cycle of Self-Harm
 Common Traits/Signs and Symptoms • Expressions of anger were discouraged while growing up. • Co-existing problems with obsessive-compulsive disorder, substance abuse or eating disorders. • A lack of the necessary skills to express strong emotions in a healthy way. • Limited social support network. • Changes in behaviour/demeanour/appearance/academic achievement/attendance. • Reluctance to participate in sports or to remove layers of clothing eg in hot weather. • Isolation.
Common Traits/Signs and Symptoms • Expressions of anger were discouraged while growing up. • Co-existing problems with obsessive-compulsive disorder, substance abuse or eating disorders. • A lack of the necessary skills to express strong emotions in a healthy way. • Limited social support network. • Changes in behaviour/demeanour/appearance/academic achievement/attendance. • Reluctance to participate in sports or to remove layers of clothing eg in hot weather. • Isolation.
 MYTHS…. Is self-harm attention seeking? Self-harm is often seen as a cry for help, a ploy to gain attention or as manipulation. However more often than not self-harm is a very private and hidden behaviour that does not involve anyone else The more serious the injury, the more serious the problem? It is important to take all injuries seriously as the nature of the wound does not represent the extent of the anguish being experienced They must like the pain? Self-harm is not about liking pain. It is a way to cope with thoughts and feelings that are depressing or distressing and to regain some control over how you feel Self-harm is the problem, if we stop this then the person will be fine? Self harm is rarely the problem, but a solution until other issues are resolved. It is the reasons that lie behind self-harm that need to be addressed in order to aid recovery
MYTHS…. Is self-harm attention seeking? Self-harm is often seen as a cry for help, a ploy to gain attention or as manipulation. However more often than not self-harm is a very private and hidden behaviour that does not involve anyone else The more serious the injury, the more serious the problem? It is important to take all injuries seriously as the nature of the wound does not represent the extent of the anguish being experienced They must like the pain? Self-harm is not about liking pain. It is a way to cope with thoughts and feelings that are depressing or distressing and to regain some control over how you feel Self-harm is the problem, if we stop this then the person will be fine? Self harm is rarely the problem, but a solution until other issues are resolved. It is the reasons that lie behind self-harm that need to be addressed in order to aid recovery
 Why? • Self-harming is a result of not having learned how to identify or express difficult feelings in a healthy way. • Self-harm serves a function for the person who does it. • Self-harm can regulate strong emotions. • Deliberate self-harming can distract from emotional pain and stop feelings of numbness. • Self-inflicted violence is a way to express things that cannot be put into words. • Self-harming behaviour can exert a sense of control over your body. • Self punishment or self-hate may be involved. Some people who self-harm have a childhood history of physical, sexual and emotional abuse. • Self-harming can also be a self-soothing behaviour for someone who does not have other means to calm intense emotions. BECAUSE IT WORKS…
Why? • Self-harming is a result of not having learned how to identify or express difficult feelings in a healthy way. • Self-harm serves a function for the person who does it. • Self-harm can regulate strong emotions. • Deliberate self-harming can distract from emotional pain and stop feelings of numbness. • Self-inflicted violence is a way to express things that cannot be put into words. • Self-harming behaviour can exert a sense of control over your body. • Self punishment or self-hate may be involved. Some people who self-harm have a childhood history of physical, sexual and emotional abuse. • Self-harming can also be a self-soothing behaviour for someone who does not have other means to calm intense emotions. BECAUSE IT WORKS…
 28 June 2013 - Standards of care for people who self-harm must be improved, says NICE • The National Institute for Health and Care Excellence (NICE) has published a quality standard to improve the quality of care and support for children, young people, and adults who self-harm • The term self-harm is used to refer to any act of self-injury or self-poisoning carried out by a person, irrespective of their motivation. This commonly involves self-injury by cutting or self-poisoning with medication. Hospitals in England deal with around 220, 000 episodes of self-harm by 150, 000 people each year The Manchester Self Harm Project: influencing national guidelines and government strategy. • A wide range of mental health problems are associated with self-harm, including borderline personality disorder, depression, bipolar disorder, schizophrenia, and drug and alcohol use disorders. People who self-harm are 50 to 100 times more likely to die by suicide in the 12 -month period after an episode than people who do not self-harm Owens D, Horrocks J, House A: Fatal and non-fatal repetition of self-harm. Br J Psychiatry 2002; 181: 193 -199, and Hawton K, Fagg J: Suicide and other causes of death, following attempted suicide. Br J Psychiatry 1988; 152: 359 -366
28 June 2013 - Standards of care for people who self-harm must be improved, says NICE • The National Institute for Health and Care Excellence (NICE) has published a quality standard to improve the quality of care and support for children, young people, and adults who self-harm • The term self-harm is used to refer to any act of self-injury or self-poisoning carried out by a person, irrespective of their motivation. This commonly involves self-injury by cutting or self-poisoning with medication. Hospitals in England deal with around 220, 000 episodes of self-harm by 150, 000 people each year The Manchester Self Harm Project: influencing national guidelines and government strategy. • A wide range of mental health problems are associated with self-harm, including borderline personality disorder, depression, bipolar disorder, schizophrenia, and drug and alcohol use disorders. People who self-harm are 50 to 100 times more likely to die by suicide in the 12 -month period after an episode than people who do not self-harm Owens D, Horrocks J, House A: Fatal and non-fatal repetition of self-harm. Br J Psychiatry 2002; 181: 193 -199, and Hawton K, Fagg J: Suicide and other causes of death, following attempted suicide. Br J Psychiatry 1988; 152: 359 -366
 Feelings experienced when asked to work with C/YP that self-harm? • • • Scared? Isolated? Anxious? Inadequate? Overwhelmed? Out of your depth/comfort zone? These reactions are recognised as being typical emotional responses. However, to work effectively with C/YP that present with emotional health issues you need to feel safe and confident…
Feelings experienced when asked to work with C/YP that self-harm? • • • Scared? Isolated? Anxious? Inadequate? Overwhelmed? Out of your depth/comfort zone? These reactions are recognised as being typical emotional responses. However, to work effectively with C/YP that present with emotional health issues you need to feel safe and confident…
 Universal Staff • Do not be afraid to talk to the C/YP if you notice or suspect any self-harming behaviour. • Be aware of your own feelings with regard to self-harm and how this may be communicated in your tone of voice or non-verbals. • Directly address your observations in a matter of fact way, this shows acceptance and the C/YP will either engage with you or not. It is not a reflection on you if they do not engage, it is merely an indication of their denial or of their fear of consequences. • Do not get drawn in to keeping anything a secret, instead, explain that you will have to share your concerns with the appropriate people (this also applies if they deny selfharming). • If they want to know what will happen next, then reassure them that they are not in trouble, that they will be offered support and that their wishes will be taken into consideration. • Discuss the support available to the C/YP and encourage them to engage.
Universal Staff • Do not be afraid to talk to the C/YP if you notice or suspect any self-harming behaviour. • Be aware of your own feelings with regard to self-harm and how this may be communicated in your tone of voice or non-verbals. • Directly address your observations in a matter of fact way, this shows acceptance and the C/YP will either engage with you or not. It is not a reflection on you if they do not engage, it is merely an indication of their denial or of their fear of consequences. • Do not get drawn in to keeping anything a secret, instead, explain that you will have to share your concerns with the appropriate people (this also applies if they deny selfharming). • If they want to know what will happen next, then reassure them that they are not in trouble, that they will be offered support and that their wishes will be taken into consideration. • Discuss the support available to the C/YP and encourage them to engage.
 D O C U M E N T S U P E R V I S I O N How to help if working 1: 1? • Acknowledge there is a problem. The young person is probably hurting on the inside and may need professional help to stop their behaviour. • Accept this is not about them being a bad person. . . This is about recognising that a behaviour that has previously helped them to handle their feelings has become a problem. • Either be, or facilitate the finding of, one person they trust to help. This could be a friend, teacher, counsellor, or relative. Encourage the sharing of this issue in a safe environment.
D O C U M E N T S U P E R V I S I O N How to help if working 1: 1? • Acknowledge there is a problem. The young person is probably hurting on the inside and may need professional help to stop their behaviour. • Accept this is not about them being a bad person. . . This is about recognising that a behaviour that has previously helped them to handle their feelings has become a problem. • Either be, or facilitate the finding of, one person they trust to help. This could be a friend, teacher, counsellor, or relative. Encourage the sharing of this issue in a safe environment.
 How to help if working 1: 1? • If there is time and they wish to engage, try to help them identify what “triggers” the self-harming behaviour…then encourage the development of ways to either avoid or address those triggers. • Recognise that self-injury is an attempt to self-soothe…then encourage them to find and develop better ways of calming and soothing themselves. • Work together to find out what function the self-injury is serving. . . then encourage them to replace acts of self-harm with more appropriate and healthy ways of expressing anger, sadness and fear.
How to help if working 1: 1? • If there is time and they wish to engage, try to help them identify what “triggers” the self-harming behaviour…then encourage the development of ways to either avoid or address those triggers. • Recognise that self-injury is an attempt to self-soothe…then encourage them to find and develop better ways of calming and soothing themselves. • Work together to find out what function the self-injury is serving. . . then encourage them to replace acts of self-harm with more appropriate and healthy ways of expressing anger, sadness and fear.
 Assessments Assessment is defined as the primary evaluation as it is provides the benchmark from which the effects of subsequent interventions can be measured. This can then evidence cost effective provision in the face of changing outcomes, targets and policies in an NHS presently undergoing radical change, reform and uncertainty (No Health without Mental Health 2011) Assessments that are used within FTB: SDQ RCADS Good assessments underpin successful referrals
Assessments Assessment is defined as the primary evaluation as it is provides the benchmark from which the effects of subsequent interventions can be measured. This can then evidence cost effective provision in the face of changing outcomes, targets and policies in an NHS presently undergoing radical change, reform and uncertainty (No Health without Mental Health 2011) Assessments that are used within FTB: SDQ RCADS Good assessments underpin successful referrals
 SDQ • SDQ is a behavioural screening tool (Goodman 1997). • It is widely used (and therefore understood) because it has a simple format that can be used with children as young as 8, is brief and has proved to be cost effective (Glazebrook et al 2003). • It is used by Forward Thinking Birmingham and the Children and Young People’s Improved access to Psychological Therapies project (CYP IAPT). • It invites input from different sources and provides a focus on strength factors instead of being solely problem orientated. • This benefits the assessment process in a multi agency approach as the professionals involved share both the language and the focus which is to improve outcomes for C/YP as opposed to addressing problems.
SDQ • SDQ is a behavioural screening tool (Goodman 1997). • It is widely used (and therefore understood) because it has a simple format that can be used with children as young as 8, is brief and has proved to be cost effective (Glazebrook et al 2003). • It is used by Forward Thinking Birmingham and the Children and Young People’s Improved access to Psychological Therapies project (CYP IAPT). • It invites input from different sources and provides a focus on strength factors instead of being solely problem orientated. • This benefits the assessment process in a multi agency approach as the professionals involved share both the language and the focus which is to improve outcomes for C/YP as opposed to addressing problems.
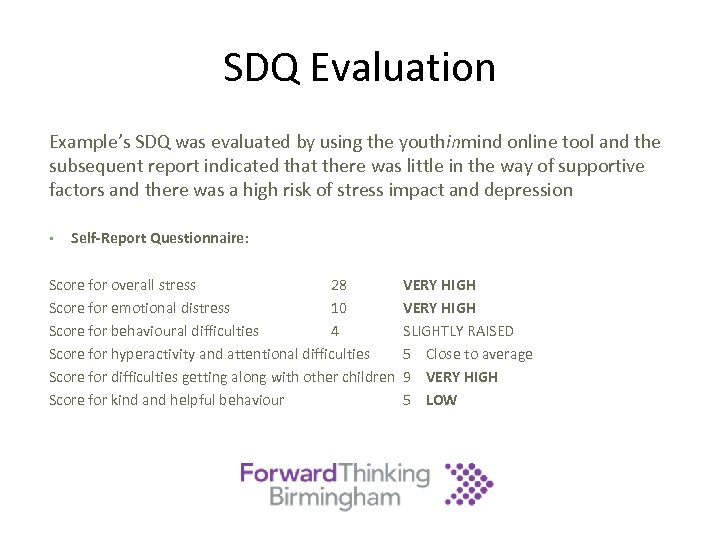 SDQ Evaluation Example’s SDQ was evaluated by using the youthinmind online tool and the subsequent report indicated that there was little in the way of supportive factors and there was a high risk of stress impact and depression • Self-Report Questionnaire: Score for overall stress 28 Score for emotional distress 10 Score for behavioural difficulties 4 Score for hyperactivity and attentional difficulties Score for difficulties getting along with other children Score for kind and helpful behaviour VERY HIGH SLIGHTLY RAISED 5 Close to average 9 VERY HIGH 5 LOW
SDQ Evaluation Example’s SDQ was evaluated by using the youthinmind online tool and the subsequent report indicated that there was little in the way of supportive factors and there was a high risk of stress impact and depression • Self-Report Questionnaire: Score for overall stress 28 Score for emotional distress 10 Score for behavioural difficulties 4 Score for hyperactivity and attentional difficulties Score for difficulties getting along with other children Score for kind and helpful behaviour VERY HIGH SLIGHTLY RAISED 5 Close to average 9 VERY HIGH 5 LOW
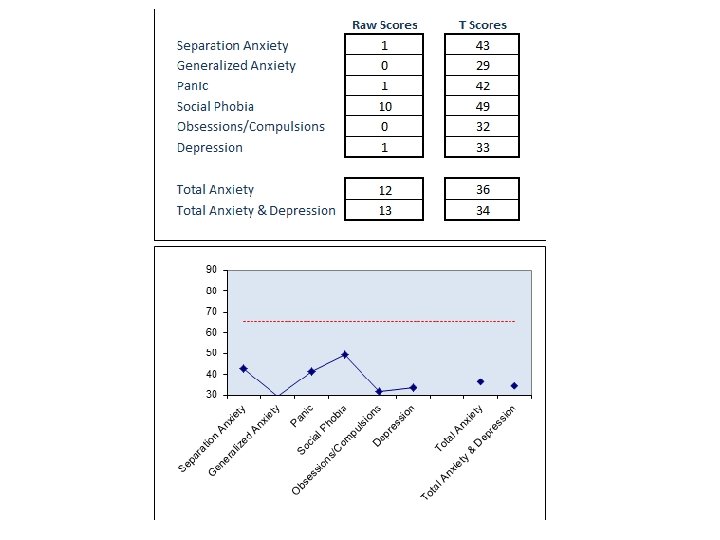
 RCADS • RCADS- revised anxiety and depression scale • The Revised Children’s Anxiety and Depression Scale (RCADS) is a valid and reliable 47 -item self-report questionnaire that measures the frequency of anxiety and depressive symptoms in children and Young people • Assesses client’s experience of symptoms related to depression and five DSM-IV anxiety disorders; separation anxiety, generalised anxiety, OCD, panic disorders and social anxiety • They assists therapists in their initial clinical impressions, diagnostic formulations and treatment planning • Comparisons of pre/post scores can reveal treatment-related changes in symptoms of anxiety and depression
RCADS • RCADS- revised anxiety and depression scale • The Revised Children’s Anxiety and Depression Scale (RCADS) is a valid and reliable 47 -item self-report questionnaire that measures the frequency of anxiety and depressive symptoms in children and Young people • Assesses client’s experience of symptoms related to depression and five DSM-IV anxiety disorders; separation anxiety, generalised anxiety, OCD, panic disorders and social anxiety • They assists therapists in their initial clinical impressions, diagnostic formulations and treatment planning • Comparisons of pre/post scores can reveal treatment-related changes in symptoms of anxiety and depression
 How to help? • • Reassure the C/YP. Be positive and accepting. ? Inform parents. Inform GP. Inform other professionals involved with the C/YP including the DSP at school Make appropriate referrals (FTB, Open Door or other counselling agency). Offer what emotional health support you are able to. Recognise your own professional boundaries of competence and request support as required. IF THERE ARE SERIOUS CONCERNS REGARDING THE C/YP’S SAFETY THEN ENSURE THEY ARE ACCOMPANIED TO THE NEAREST HOSPITAL FOR AN IMMEDIATE MENTAL HEALTH ASSESSMENT OR PHONE 999 FOR AN AMBULANCE TO TAKE THEM – Never worry about making a wrong call. Share information and concerns and remember that the child’s needs are paramount (Working Together to Safeguard Children 2013)
How to help? • • Reassure the C/YP. Be positive and accepting. ? Inform parents. Inform GP. Inform other professionals involved with the C/YP including the DSP at school Make appropriate referrals (FTB, Open Door or other counselling agency). Offer what emotional health support you are able to. Recognise your own professional boundaries of competence and request support as required. IF THERE ARE SERIOUS CONCERNS REGARDING THE C/YP’S SAFETY THEN ENSURE THEY ARE ACCOMPANIED TO THE NEAREST HOSPITAL FOR AN IMMEDIATE MENTAL HEALTH ASSESSMENT OR PHONE 999 FOR AN AMBULANCE TO TAKE THEM – Never worry about making a wrong call. Share information and concerns and remember that the child’s needs are paramount (Working Together to Safeguard Children 2013)
 Alternative Coping Strategies: PRESENTING EMOTION = ANGER • Squeeze ice • Do something that will give you a sharp sensation, like biting a lemon • Exercise • Snap a rubber band against your wrist The logic behind these things is that, when you are angry, you have a lot of energy. Most of these are ways to release that energy without self-injuring… PRESENTING EMOTION = SADNESS, DEPRESSION • • Take a bath, put bubbles in it Read a book that you like. Read a children’s book – they usually have happy endings Get yourself a present Watch a funny movie The idea behind most of these is to cheer yourself up somehow…
Alternative Coping Strategies: PRESENTING EMOTION = ANGER • Squeeze ice • Do something that will give you a sharp sensation, like biting a lemon • Exercise • Snap a rubber band against your wrist The logic behind these things is that, when you are angry, you have a lot of energy. Most of these are ways to release that energy without self-injuring… PRESENTING EMOTION = SADNESS, DEPRESSION • • Take a bath, put bubbles in it Read a book that you like. Read a children’s book – they usually have happy endings Get yourself a present Watch a funny movie The idea behind most of these is to cheer yourself up somehow…
 Alternative Coping Strategies: PRESENTING EMOTION = ADDICTION • • • Draw or write on yourself with a red pen or marker Paint yourself with red paint Squeeze ice Snap a rubber band against your wrist Cry Exercise The point here is to create feelings and sensations similar to those you experience while hurting yourself. Some of these things create visual images like those you may want to see, like scars or blood. Others release endorphins, which is what happens when you hurt yourself and what gives you the feeling of euphoria… WAIT. . WAIT……WAIT…. . …WAIT…………. WAI T…
Alternative Coping Strategies: PRESENTING EMOTION = ADDICTION • • • Draw or write on yourself with a red pen or marker Paint yourself with red paint Squeeze ice Snap a rubber band against your wrist Cry Exercise The point here is to create feelings and sensations similar to those you experience while hurting yourself. Some of these things create visual images like those you may want to see, like scars or blood. Others release endorphins, which is what happens when you hurt yourself and what gives you the feeling of euphoria… WAIT. . WAIT……WAIT…. . …WAIT…………. WAI T…
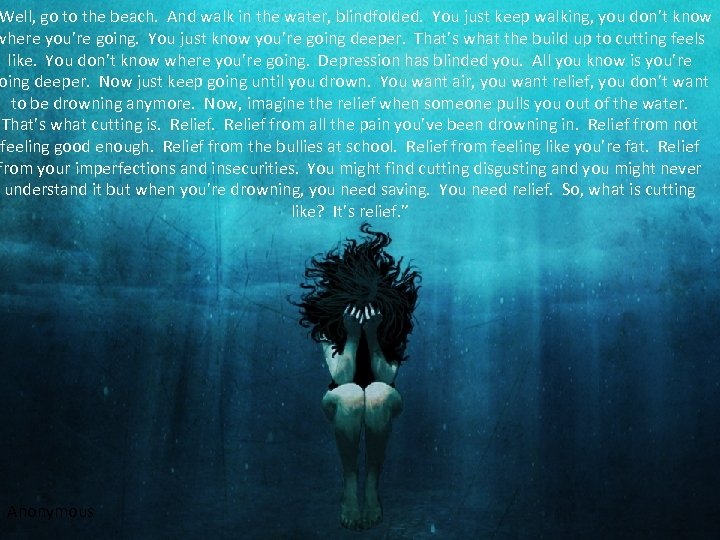 Well, go to the beach. And walk in the water, blindfolded. You just keep walking, you don’t know where you’re going. You just know you’re going deeper. That’s what the build up to cutting feels like. You don’t know where you’re going. Depression has blinded you. All you know is you’re oing deeper. Now just keep going until you drown. You want air, you want relief, you don’t want to be drowning anymore. Now, imagine the relief when someone pulls you out of the water. That’s what cutting is. Relief from all the pain you’ve been drowning in. Relief from not feeling good enough. Relief from the bullies at school. Relief from feeling like you’re fat. Relief from your imperfections and insecurities. You might find cutting disgusting and you might never understand it but when you’re drowning, you need saving. You need relief. So, what is cutting like? It’s relief. ” Anonymous
Well, go to the beach. And walk in the water, blindfolded. You just keep walking, you don’t know where you’re going. You just know you’re going deeper. That’s what the build up to cutting feels like. You don’t know where you’re going. Depression has blinded you. All you know is you’re oing deeper. Now just keep going until you drown. You want air, you want relief, you don’t want to be drowning anymore. Now, imagine the relief when someone pulls you out of the water. That’s what cutting is. Relief from all the pain you’ve been drowning in. Relief from not feeling good enough. Relief from the bullies at school. Relief from feeling like you’re fat. Relief from your imperfections and insecurities. You might find cutting disgusting and you might never understand it but when you’re drowning, you need saving. You need relief. So, what is cutting like? It’s relief. ” Anonymous
 E M O T I O N A L H E A L T H S U P P O R T When working with C/YP ensure that: • The venue is appropriate with regards to it being private, accessible, C/YP friendly and free from interruptions. • The seating is conducive to a support session - awareness of power differential as a potential barrier to communication. • Confidentiality boundaries are established (with C/YP, families and other professionals). • Boundaries of engagement are established (? up to 6 sessions then review). • Engage with whatever the C/YP brings for discussion (not necessarily the selfharm).
E M O T I O N A L H E A L T H S U P P O R T When working with C/YP ensure that: • The venue is appropriate with regards to it being private, accessible, C/YP friendly and free from interruptions. • The seating is conducive to a support session - awareness of power differential as a potential barrier to communication. • Confidentiality boundaries are established (with C/YP, families and other professionals). • Boundaries of engagement are established (? up to 6 sessions then review). • Engage with whatever the C/YP brings for discussion (not necessarily the selfharm).
 E M O T I O N A L H E A L T H S U P P O R T When working with C/YP ensure that: • Open questions and active listening are used and work is done to minimise uncertainty: be welcoming, elicit the C/YP’s expectations of the service - ensure they know why they are being seen and explain your role clearly (purpose of meeting, future work/support). • The difficult questions get asked – asking the question will not lead to the behaviour and will give permission for discussion. • What is shared is acknowledged and how the C/YP may feel following disclosure (vulnerable, scared) – recognise and acknowledge distress. • Appreciate they have chosen you to confide in. • The C/YP is aware of what will happen next.
E M O T I O N A L H E A L T H S U P P O R T When working with C/YP ensure that: • Open questions and active listening are used and work is done to minimise uncertainty: be welcoming, elicit the C/YP’s expectations of the service - ensure they know why they are being seen and explain your role clearly (purpose of meeting, future work/support). • The difficult questions get asked – asking the question will not lead to the behaviour and will give permission for discussion. • What is shared is acknowledged and how the C/YP may feel following disclosure (vulnerable, scared) – recognise and acknowledge distress. • Appreciate they have chosen you to confide in. • The C/YP is aware of what will happen next.
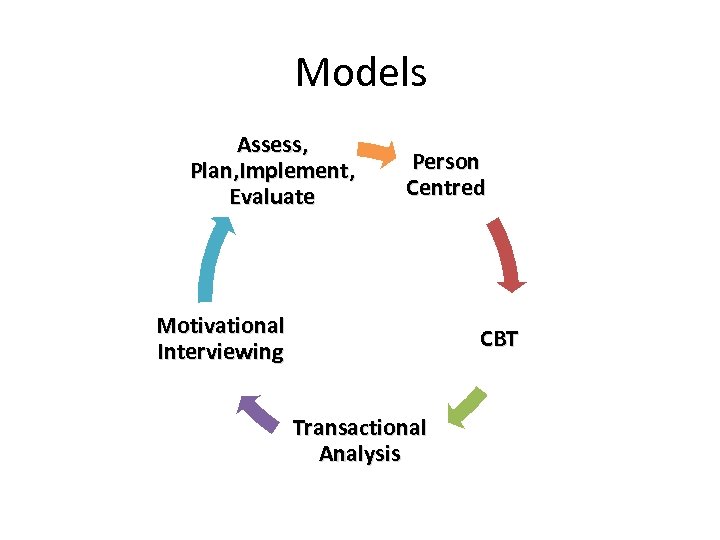 Models Assess, Plan, Implement, Evaluate Person Centred Motivational Interviewing CBT Transactional Analysis
Models Assess, Plan, Implement, Evaluate Person Centred Motivational Interviewing CBT Transactional Analysis
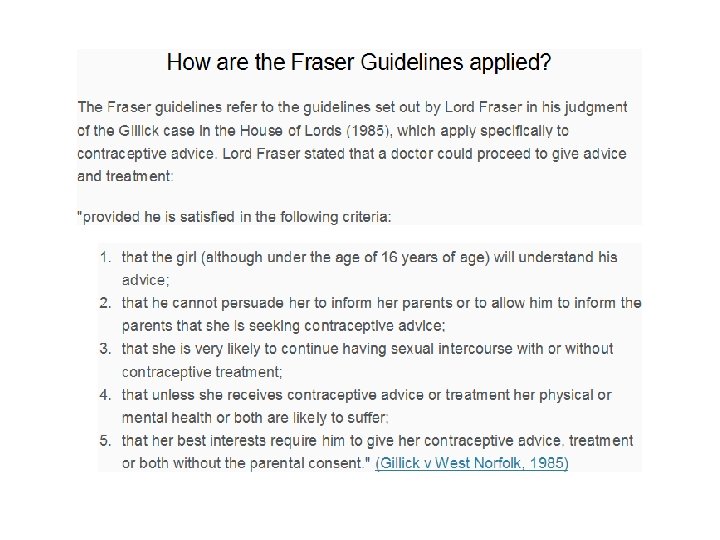
 Information Sharing • Ensure confidentiality boundaries are discussed and agreed with the C/YP, their family and professionals. • If the C/YP does not want their parents informed with regard to selfharming then do everything possible to persuade them to do so. If they still decline then apply the Fraser Guidelines and work accordingly.
Information Sharing • Ensure confidentiality boundaries are discussed and agreed with the C/YP, their family and professionals. • If the C/YP does not want their parents informed with regard to selfharming then do everything possible to persuade them to do so. If they still decline then apply the Fraser Guidelines and work accordingly.
 Signposting • Open Door will see C/YP without parental consent on 0121 454 1116 • FTB will offer support and advice for professionals on 0300 0099 • Childline – 0800 1111 • Focus Helpline – 0800 027 2127 • National Self-Harm Network – 0800 622 6000 • • Samaritans – 08457 90 90 90 • Youth 2 Youth – 020 8896 3675
Signposting • Open Door will see C/YP without parental consent on 0121 454 1116 • FTB will offer support and advice for professionals on 0300 0099 • Childline – 0800 1111 • Focus Helpline – 0800 027 2127 • National Self-Harm Network – 0800 622 6000 • • Samaritans – 08457 90 90 90 • Youth 2 Youth – 020 8896 3675
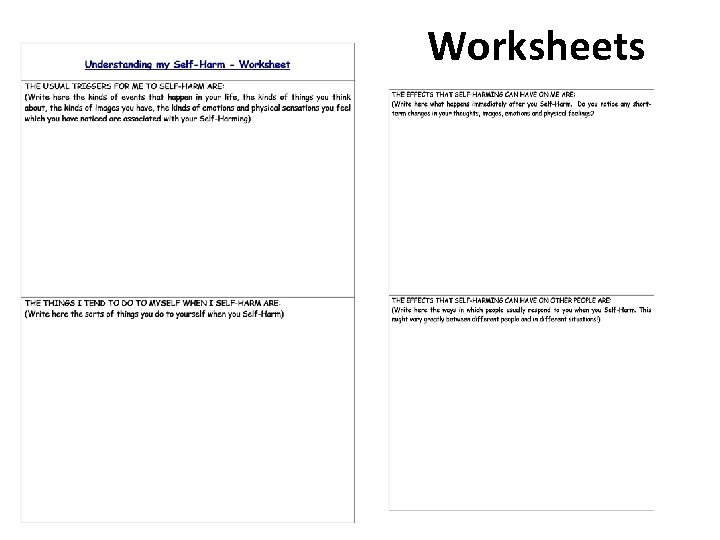 Worksheets
Worksheets
 Worksheets Feelings Worksheet http: //www. stem 4. org. uk/ Why not try the Calm Harm app? Calm Harm provides tasks that help you resist or manage the urge to self harm. You can add your own tasks too and it’s completely private and password protected.
Worksheets Feelings Worksheet http: //www. stem 4. org. uk/ Why not try the Calm Harm app? Calm Harm provides tasks that help you resist or manage the urge to self harm. You can add your own tasks too and it’s completely private and password protected.
 Case Study 1 • Symran is 15 years old and lives with her aunt as her relationship with mom is volatile. • Previous Social Care involvement due to DA. • Dad has left the family home and has no contact with Symran. • Symran has been self-harming by cutting her legs for the last 6 months. • Has stated she ‘does not want to be here anymore’ but denies suicidal intent as she does not want to leave her younger sister on her own. Emotional or Mental Health?
Case Study 1 • Symran is 15 years old and lives with her aunt as her relationship with mom is volatile. • Previous Social Care involvement due to DA. • Dad has left the family home and has no contact with Symran. • Symran has been self-harming by cutting her legs for the last 6 months. • Has stated she ‘does not want to be here anymore’ but denies suicidal intent as she does not want to leave her younger sister on her own. Emotional or Mental Health?
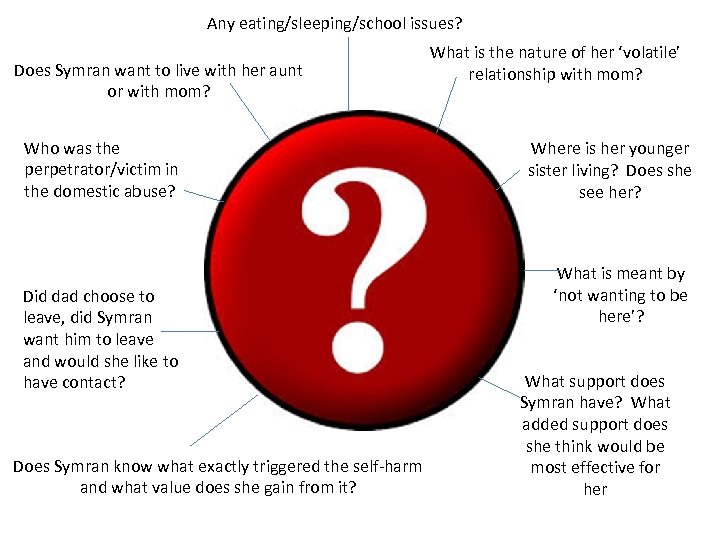 Any eating/sleeping/school issues? Does Symran want to live with her aunt or with mom? Who was the perpetrator/victim in the domestic abuse? Did dad choose to leave, did Symran want him to leave and would she like to have contact? Does Symran know what exactly triggered the self-harm and what value does she gain from it? What is the nature of her ‘volatile’ relationship with mom? Where is her younger sister living? Does she see her? What is meant by ‘not wanting to be here’? What support does Symran have? What added support does she think would be most effective for her
Any eating/sleeping/school issues? Does Symran want to live with her aunt or with mom? Who was the perpetrator/victim in the domestic abuse? Did dad choose to leave, did Symran want him to leave and would she like to have contact? Does Symran know what exactly triggered the self-harm and what value does she gain from it? What is the nature of her ‘volatile’ relationship with mom? Where is her younger sister living? Does she see her? What is meant by ‘not wanting to be here’? What support does Symran have? What added support does she think would be most effective for her
 • Symran’s relationship with mom is stressful and argumentative but not physically violent. • Symran wanted to live with her aunt but did not want to be separated from her sister who is with mom. • She does not worry about her sister’s safety, she misses her company. • Dad was the perpetrator of the domestic abuse and although she witnessed his physical attacks on her mom, she misses him and would like contact. • Symran started cutting herself when dad left and she feels that it provides a release from overwhelming emotions. • Symran recognises that ‘not wanting to be here’ is an indication that her emotions are at a level where her self-harming is no longer effective and that she would like some support. • Symran has no support at present as her Social worker no longer provides contact and she has told nobody about her self-harming as she feels ashamed. • No eating, sleeping or school issues.
• Symran’s relationship with mom is stressful and argumentative but not physically violent. • Symran wanted to live with her aunt but did not want to be separated from her sister who is with mom. • She does not worry about her sister’s safety, she misses her company. • Dad was the perpetrator of the domestic abuse and although she witnessed his physical attacks on her mom, she misses him and would like contact. • Symran started cutting herself when dad left and she feels that it provides a release from overwhelming emotions. • Symran recognises that ‘not wanting to be here’ is an indication that her emotions are at a level where her self-harming is no longer effective and that she would like some support. • Symran has no support at present as her Social worker no longer provides contact and she has told nobody about her self-harming as she feels ashamed. • No eating, sleeping or school issues.
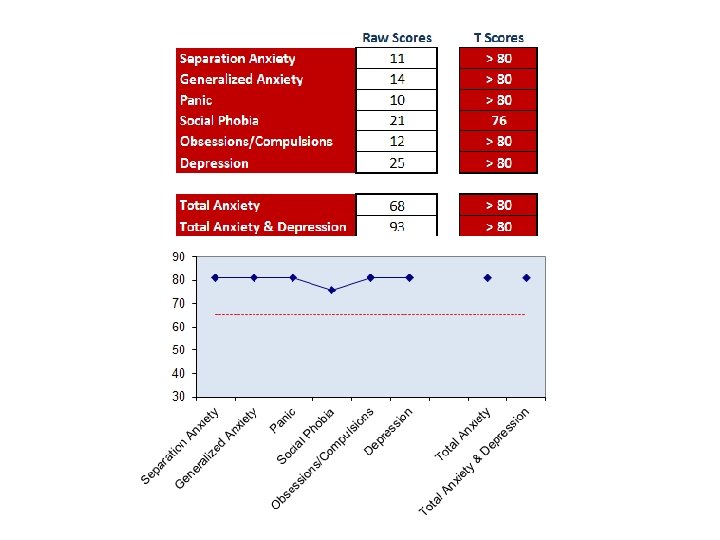
 Emotional: Symran has a complicated home situation which is causing her distress. She has witnessed domestic abuse between her parents. She has lost her dad and the support she received from her Social Worker. Her issues are apparent only at home, she is achieving academically at school. She states she does not want to die but that she finds her situation overwhelming. • She has no sleeping or eating issues. • She has friends but does not choose to confide in them. • She wants to have professional/confidential support. • • • Action: • A safety plan was agreed between Symran, mom, aunt and school and Symran agreed to alert identified people should her mood begin to sink. • Symran was referred for emotional health counselling via FTB, her GP was informed and following a referral to MASH a family support worker was allocated to facilitate contact with dad and to mediate with the family as a whole. • RCADS and SDQs completed and evaluated.
Emotional: Symran has a complicated home situation which is causing her distress. She has witnessed domestic abuse between her parents. She has lost her dad and the support she received from her Social Worker. Her issues are apparent only at home, she is achieving academically at school. She states she does not want to die but that she finds her situation overwhelming. • She has no sleeping or eating issues. • She has friends but does not choose to confide in them. • She wants to have professional/confidential support. • • • Action: • A safety plan was agreed between Symran, mom, aunt and school and Symran agreed to alert identified people should her mood begin to sink. • Symran was referred for emotional health counselling via FTB, her GP was informed and following a referral to MASH a family support worker was allocated to facilitate contact with dad and to mediate with the family as a whole. • RCADS and SDQs completed and evaluated.
 Discharge: • Following 12 weeks of CBT therapy, Symran was much happier with her domestic situation as she was made aware of her potential choices which gave her a sense of control. • Mom had taken the issues seriously and was being supportive and facilitating frequent contact between Symran and her sister. • Mom was also receiving emotional health support for herself. • Supervised contact with dad was being arranged. • Symran no longer had thoughts of ‘not wanting to be here’ and although she was still self-harming, she felt that it was at a minimal level which she could manage with the help of her family support worker.
Discharge: • Following 12 weeks of CBT therapy, Symran was much happier with her domestic situation as she was made aware of her potential choices which gave her a sense of control. • Mom had taken the issues seriously and was being supportive and facilitating frequent contact between Symran and her sister. • Mom was also receiving emotional health support for herself. • Supervised contact with dad was being arranged. • Symran no longer had thoughts of ‘not wanting to be here’ and although she was still self-harming, she felt that it was at a minimal level which she could manage with the help of her family support worker.
 Case Study 2 • Nia is a 13 year old girl who was referred into FTB by her school due to recent changes in her behaviour • She seemed isolated and distracted in school and her grades had started to slip. • When teachers approached her about this she explained she hears up to 15 different voices at a time. • She said these voices tell her to do bad things she knows she shouldn’t. • When school addressed the issue with mum she was also concerned and disclosed she had found suicidal notes in Nia’s bedroom Emotional or Mental Health?
Case Study 2 • Nia is a 13 year old girl who was referred into FTB by her school due to recent changes in her behaviour • She seemed isolated and distracted in school and her grades had started to slip. • When teachers approached her about this she explained she hears up to 15 different voices at a time. • She said these voices tell her to do bad things she knows she shouldn’t. • When school addressed the issue with mum she was also concerned and disclosed she had found suicidal notes in Nia’s bedroom Emotional or Mental Health?
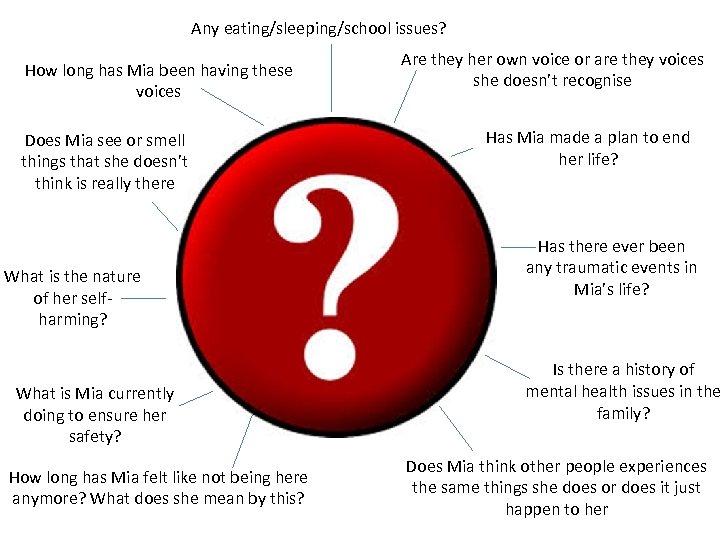 Any eating/sleeping/school issues? How long has Mia been having these voices Does Mia see or smell things that she doesn’t think is really there What is the nature of her selfharming? What is Mia currently doing to ensure her safety? How long has Mia felt like not being here anymore? What does she mean by this? Are they her own voice or are they voices she doesn’t recognise Has Mia made a plan to end her life? Has there ever been any traumatic events in Mia’s life? Is there a history of mental health issues in the family? Does Mia think other people experiences the same things she does or does it just happen to her
Any eating/sleeping/school issues? How long has Mia been having these voices Does Mia see or smell things that she doesn’t think is really there What is the nature of her selfharming? What is Mia currently doing to ensure her safety? How long has Mia felt like not being here anymore? What does she mean by this? Are they her own voice or are they voices she doesn’t recognise Has Mia made a plan to end her life? Has there ever been any traumatic events in Mia’s life? Is there a history of mental health issues in the family? Does Mia think other people experiences the same things she does or does it just happen to her
 • Mia’s cousin was tragically killed in a car accident approximately a year ago- mum reports this is when she started noticing a change in Nia • Mum also reports that there is a family history of depression • Mia explained that she does wish to end her life and doesn’t know what has stopped her doing this- she doesn’t have a plan as of yet. • She self-harms on a regular basis by cutting her wrists using sharp objects she finds at school. • Mia explains that the voices she hears are not her own voice but the voices of other people she does not recognise- they have been present for a few months • These voices distract her during lessons and tell her to do things she knows she shouldn’t. This can vary from shouting out in class or running in front of a bus. • She also reports seeing 2 men, one dressing in red the other in black. She sais these figures can appear at any time but she does not know if anyone else sees them. • Mia’s sleeping pattern is very disturbed and she is losing weight due to a loss of appetite.
• Mia’s cousin was tragically killed in a car accident approximately a year ago- mum reports this is when she started noticing a change in Nia • Mum also reports that there is a family history of depression • Mia explained that she does wish to end her life and doesn’t know what has stopped her doing this- she doesn’t have a plan as of yet. • She self-harms on a regular basis by cutting her wrists using sharp objects she finds at school. • Mia explains that the voices she hears are not her own voice but the voices of other people she does not recognise- they have been present for a few months • These voices distract her during lessons and tell her to do things she knows she shouldn’t. This can vary from shouting out in class or running in front of a bus. • She also reports seeing 2 men, one dressing in red the other in black. She sais these figures can appear at any time but she does not know if anyone else sees them. • Mia’s sleeping pattern is very disturbed and she is losing weight due to a loss of appetite.
 Emotional or Mental Health? • Mental health: • As mental health issues run in the family, Mia was already more susceptible to suffering with her own mental health. • It became apparent that the loss of Mia’s cousin, whom she was very close to acted as a triggering factor for Mia’s onset. • This may have occurred when experiencing stress/trauma later on in her life, or it may have never occurred at all. • She is experiencing a psychotic episode where she has lost touch with reality- she is having visual and auditory hallucinations. • Action: • Mia was referred into Forward Thinking Birmingham following a choice appointment in order to receive a psychiatric assessment. • It was felt necessary to prescribe Mia anti-psychotic medication which greatly improved her psychotic symptoms and helped to improve the quality of her sleep
Emotional or Mental Health? • Mental health: • As mental health issues run in the family, Mia was already more susceptible to suffering with her own mental health. • It became apparent that the loss of Mia’s cousin, whom she was very close to acted as a triggering factor for Mia’s onset. • This may have occurred when experiencing stress/trauma later on in her life, or it may have never occurred at all. • She is experiencing a psychotic episode where she has lost touch with reality- she is having visual and auditory hallucinations. • Action: • Mia was referred into Forward Thinking Birmingham following a choice appointment in order to receive a psychiatric assessment. • It was felt necessary to prescribe Mia anti-psychotic medication which greatly improved her psychotic symptoms and helped to improve the quality of her sleep
 Learning Points: • Agree the plan of care with the C/YP. • No evidence does not mean no issue or need ‘Voice of the Child’ (Children Act 2004). • ‘Attention seeking’ is an indication of need as it could be due to neglect and generally occurs when C/YP feel unable to manage their emotions or behaviour. • Make every contact count (NICE 2006). • Share information (with peers, safeguarding, parents, outside agencies). • Recognise limits and ask for advice when appropriate (when feeling unsure or uncomfortable). • • Awareness of and signposting to other agencies (https: //forwardthinkingbirmingham. org. uk/)
Learning Points: • Agree the plan of care with the C/YP. • No evidence does not mean no issue or need ‘Voice of the Child’ (Children Act 2004). • ‘Attention seeking’ is an indication of need as it could be due to neglect and generally occurs when C/YP feel unable to manage their emotions or behaviour. • Make every contact count (NICE 2006). • Share information (with peers, safeguarding, parents, outside agencies). • Recognise limits and ask for advice when appropriate (when feeling unsure or uncomfortable). • • Awareness of and signposting to other agencies (https: //forwardthinkingbirmingham. org. uk/)
 Learning Points: • Universal input is not for an emergency response, advise re 999, GP, A&E, parents. • Ensure the most appropriate person makes referrals/offers support. • Universal staff are not Mental Health Professionals and are not required to deliver Mental Health Interventions. • Provide Emotional Health support and evidence an improvement in outcome for the C/YP. • Take advantage of existing training and request specifics.
Learning Points: • Universal input is not for an emergency response, advise re 999, GP, A&E, parents. • Ensure the most appropriate person makes referrals/offers support. • Universal staff are not Mental Health Professionals and are not required to deliver Mental Health Interventions. • Provide Emotional Health support and evidence an improvement in outcome for the C/YP. • Take advantage of existing training and request specifics.
 Celebrities known to have self harmed…
Celebrities known to have self harmed…
 Angelina Jolie • The 35 -year-old mum of six has revealed how she and her boyfriend cut each other with knives when she was just 14. • She said: "I dated my first boyfriend when I was 14. I lived with him for two years, with my mum. I had started having sex, but sex didn't feel enough and emotions didn't feel enough. And in a moment of wanting to find something honest, I grabbed a knife and cut him, he cut me back and we had this exchange of something. ”
Angelina Jolie • The 35 -year-old mum of six has revealed how she and her boyfriend cut each other with knives when she was just 14. • She said: "I dated my first boyfriend when I was 14. I lived with him for two years, with my mum. I had started having sex, but sex didn't feel enough and emotions didn't feel enough. And in a moment of wanting to find something honest, I grabbed a knife and cut him, he cut me back and we had this exchange of something. ”
 If you have concerns regarding working with C/YP that self-harm Share your concerns and seek advice and support Frances Dodd & Rachael Wall Forward Thinking Birmingham Blakesley Centre 102 Blakesley Road Yardley Birmingham B 25 8 RN Tel 0121 683 6151 FTB Access 0300 0099
If you have concerns regarding working with C/YP that self-harm Share your concerns and seek advice and support Frances Dodd & Rachael Wall Forward Thinking Birmingham Blakesley Centre 102 Blakesley Road Yardley Birmingham B 25 8 RN Tel 0121 683 6151 FTB Access 0300 0099



