9a40453ffe1190de46f632a8f95227e3.ppt
- Количество слайдов: 69
 School Crisis Postvention This training is part of an ongoing collaboration between the Tennessee Department of Education and Vanderbilt Community Mental Health Center
School Crisis Postvention This training is part of an ongoing collaboration between the Tennessee Department of Education and Vanderbilt Community Mental Health Center
 Tennessee Schools PREPARE P roviding Support R eaching E ducators P arents/Students A nd R estoring community with E ffective interventions
Tennessee Schools PREPARE P roviding Support R eaching E ducators P arents/Students A nd R estoring community with E ffective interventions
 What is TSP? Tennessee Schools PREPARE is a program designed to develop and then disseminate information to school districts that will assist all schools in advancing and maturing their “after the crisis” response plans. TSP is an ongoing dialogue with all stakeholders, an ecological process enabling Tennessee schools to respond to crises with effective, best practice interventions.
What is TSP? Tennessee Schools PREPARE is a program designed to develop and then disseminate information to school districts that will assist all schools in advancing and maturing their “after the crisis” response plans. TSP is an ongoing dialogue with all stakeholders, an ecological process enabling Tennessee schools to respond to crises with effective, best practice interventions.
 National Advisory Committee on Children and Terrorism Recommendations to the Secretary-2003 o There is a tremendous need for basic knowledge about appropriate treatments and interventions that support psychological and social resilience in children and family in an attempt to reduce risks for later disorders and/or disabilities
National Advisory Committee on Children and Terrorism Recommendations to the Secretary-2003 o There is a tremendous need for basic knowledge about appropriate treatments and interventions that support psychological and social resilience in children and family in an attempt to reduce risks for later disorders and/or disabilities
 Recommendations cont. o Current data points to the importance of early intervention in promoting post disaster resilience in children and families o Effective post disaster psychological and emotional functioning of parents and caretakers predict better outcomes in children
Recommendations cont. o Current data points to the importance of early intervention in promoting post disaster resilience in children and families o Effective post disaster psychological and emotional functioning of parents and caretakers predict better outcomes in children
 Like it or not o The reach of schools extends far beyond the borders of the classroom and contemporary schools play a critical role in the life of their communities o Parents and others responsible for children often look to schools to keep children safe and to provide direction about how best to support them, especially in times of crisis
Like it or not o The reach of schools extends far beyond the borders of the classroom and contemporary schools play a critical role in the life of their communities o Parents and others responsible for children often look to schools to keep children safe and to provide direction about how best to support them, especially in times of crisis
 School Crisis Postvention Today’s Agenda o Leadership before a crisis o What is in a Postvention crisis plan? o Restoring Community – first day back to school o Skills for Clinical Crisis Team Members n Group skills n Cultural competence n Identifying children in need of referral n Individual counseling skills for traumatized children
School Crisis Postvention Today’s Agenda o Leadership before a crisis o What is in a Postvention crisis plan? o Restoring Community – first day back to school o Skills for Clinical Crisis Team Members n Group skills n Cultural competence n Identifying children in need of referral n Individual counseling skills for traumatized children
 Leadership BEFORE a crisis o The district develops a district crisis team o Each school selects and trains it’s own crisis team n n n n Principal Vice Principal Safety Officer Counselors, social workers, psychologists School nurse School Secretary Other faculty or staff (teachers, janitor, security guard etc. )
Leadership BEFORE a crisis o The district develops a district crisis team o Each school selects and trains it’s own crisis team n n n n Principal Vice Principal Safety Officer Counselors, social workers, psychologists School nurse School Secretary Other faculty or staff (teachers, janitor, security guard etc. )
 o These a to hel re all “prof p you e r stud ssionals” v ents. Who d olunteering o you trust?
o These a to hel re all “prof p you e r stud ssionals” v ents. Who d olunteering o you trust?
 Working with community professionals o Identify licensed professionals in the community that you may allow into the school post emergency o Have the crisis team establish a relationship with these community professionals o If the professionals are trained in mental health Postvention, and willing to work with your crisis team, try to meet annually together.
Working with community professionals o Identify licensed professionals in the community that you may allow into the school post emergency o Have the crisis team establish a relationship with these community professionals o If the professionals are trained in mental health Postvention, and willing to work with your crisis team, try to meet annually together.
 Postvention Leadership BEFORE a crisis o Develop a complete “live” crisis Postvention plan that includes a continually updated telephone list of your crisis team, identified community supports, and district personnel that either need to be notified or could be available to assist post crisis. Have after hour phone numbers of all, including identified community support agencies! Postvention team members must keep the Postvention plan and phone tree bedside and in their car at all times!
Postvention Leadership BEFORE a crisis o Develop a complete “live” crisis Postvention plan that includes a continually updated telephone list of your crisis team, identified community supports, and district personnel that either need to be notified or could be available to assist post crisis. Have after hour phone numbers of all, including identified community support agencies! Postvention team members must keep the Postvention plan and phone tree bedside and in their car at all times!
 What is in a Postvention Crisis Plan? o Complete after hours telephone chain including numbers of district personnel and community support agencies. (as mentioned above) o Identification of Crisis team members. o Identification of regional or district crisis team. n Major crises may traumatize the “in house” Postvention team – district personnel should be available to help with such emergencies. o Identification of a Media Liaison Person
What is in a Postvention Crisis Plan? o Complete after hours telephone chain including numbers of district personnel and community support agencies. (as mentioned above) o Identification of Crisis team members. o Identification of regional or district crisis team. n Major crises may traumatize the “in house” Postvention team – district personnel should be available to help with such emergencies. o Identification of a Media Liaison Person
 Cr Ma isis nu al o Identification of a Family Liaison Person n n To offer support to the effected family or families To liaison regarding funeral and memorial activities To help the family gather student’s personal belongings in the event of a death To offer referrals as requested o Suggestions for informing students of unexpected loss of life (fellow students, faculty, or staff) o Suggestions for how to handle classroom discussions regarding the tragedy. o Identification of a crisis center location with a telephone, manned all day by a member of the crisis team
Cr Ma isis nu al o Identification of a Family Liaison Person n n To offer support to the effected family or families To liaison regarding funeral and memorial activities To help the family gather student’s personal belongings in the event of a death To offer referrals as requested o Suggestions for informing students of unexpected loss of life (fellow students, faculty, or staff) o Suggestions for how to handle classroom discussions regarding the tragedy. o Identification of a crisis center location with a telephone, manned all day by a member of the crisis team
 o Identification of rooms to be set aside for individual and group counseling o A plan for calling in substitute teachers, and/or a plan to relieve teachers who will need additional time to grieve/debrief. o In the event of a student death, a plan to have counselors follow the students schedule to provide extra support in those classrooms.
o Identification of rooms to be set aside for individual and group counseling o A plan for calling in substitute teachers, and/or a plan to relieve teachers who will need additional time to grieve/debrief. o In the event of a student death, a plan to have counselors follow the students schedule to provide extra support in those classrooms.
 o In the event of a student death, suggestions for how staff can best deal with the “empty desk, empty locker” phenomenon. n Helpful suggestion – principal to bring (or request crisis team member bring) individual flower stems to school, students can have an in class “ritual” of putting flowers on deceased student’s desk, later they can be brought to family. (Also students can make paper flowers for a wreath for the locker, create a memory book for the family, cards for the family etc. )
o In the event of a student death, suggestions for how staff can best deal with the “empty desk, empty locker” phenomenon. n Helpful suggestion – principal to bring (or request crisis team member bring) individual flower stems to school, students can have an in class “ritual” of putting flowers on deceased student’s desk, later they can be brought to family. (Also students can make paper flowers for a wreath for the locker, create a memory book for the family, cards for the family etc. )
 o Formulation of school policy on Funerals and In School memorials n Each school needs to set a policy on funeral attendance n Students and faculty may want to memorialize the death in some way on school premises. This may include rituals such as a moment of silence, planting a tree, dedicating a game or event in the person’s memory etc. n The policy on in school memorials can be developed with student leaders – ideas to be considered include flying flag at half mass, year book memorials, special events dedicated to deceased student etc. n Have consistency across situations where there is loss of life so as to not hurt or offend families o Some Postvention plans will include sample letters that can be sent out to parents, other principals will prefer to run all communication through the media liaison and the district media consultant.
o Formulation of school policy on Funerals and In School memorials n Each school needs to set a policy on funeral attendance n Students and faculty may want to memorialize the death in some way on school premises. This may include rituals such as a moment of silence, planting a tree, dedicating a game or event in the person’s memory etc. n The policy on in school memorials can be developed with student leaders – ideas to be considered include flying flag at half mass, year book memorials, special events dedicated to deceased student etc. n Have consistency across situations where there is loss of life so as to not hurt or offend families o Some Postvention plans will include sample letters that can be sent out to parents, other principals will prefer to run all communication through the media liaison and the district media consultant.
 o Postvention plans should articulate the need for before and after school all staff meetings. (if the nature of the crisis effects the whole school) o Principals should require the staff to participate in these meetings because typically the most traumatized individuals will not seek out help o Teachers and staff closest to the tragedy should be grouped separately and offered critical incident debriefing. For example, if one grade level is particularly effected, that grade level team should be given the opportunity to meet separately before school with a counselor or outside professional working specifically with them.
o Postvention plans should articulate the need for before and after school all staff meetings. (if the nature of the crisis effects the whole school) o Principals should require the staff to participate in these meetings because typically the most traumatized individuals will not seek out help o Teachers and staff closest to the tragedy should be grouped separately and offered critical incident debriefing. For example, if one grade level is particularly effected, that grade level team should be given the opportunity to meet separately before school with a counselor or outside professional working specifically with them.
 o TEACHERS SHOULD NOT BE EXPECTED TO HANDLE DISTRAUGHT CHILDREN WITHOUT ADEQUATE HELP FOR THEMSELVES !!
o TEACHERS SHOULD NOT BE EXPECTED TO HANDLE DISTRAUGHT CHILDREN WITHOUT ADEQUATE HELP FOR THEMSELVES !!
 o Include a plan for disseminating information n The Crisis team meets early before the all staff meeting, or perhaps works the night before to gather the facts and decide how to disseminate information to the school community. The crisis team can write up a statement that is read in all first classes of the day at the same time, or the Principal can use the announcement time with follow up from the teachers. This written statement can be used for a variety of purposes through out the day so that the school community communicates with one voice.
o Include a plan for disseminating information n The Crisis team meets early before the all staff meeting, or perhaps works the night before to gather the facts and decide how to disseminate information to the school community. The crisis team can write up a statement that is read in all first classes of the day at the same time, or the Principal can use the announcement time with follow up from the teachers. This written statement can be used for a variety of purposes through out the day so that the school community communicates with one voice.
 o Plan to offer special services to like groups after the tragedy – for example, a student’s best friends, sports team, family members at school etc. One member of the Postvention team should be assigned to determine “what groups” will likely need extra assistance. In addition a crisis team member will need to check with teachers for several days, helping teachers identify students who may need “extra” assistance. o Have information in your plan about how to call in interpreters or send home information in other languages
o Plan to offer special services to like groups after the tragedy – for example, a student’s best friends, sports team, family members at school etc. One member of the Postvention team should be assigned to determine “what groups” will likely need extra assistance. In addition a crisis team member will need to check with teachers for several days, helping teachers identify students who may need “extra” assistance. o Have information in your plan about how to call in interpreters or send home information in other languages
 Parent/Community meeting o Depending on the scope of the crisis, there may need to be a plan for an evening parent/community meeting. The principal, crisis response team, and crisis consultant should speak at the meeting, emphasizing what to expect in the grieving process, how to help students with the traumatic event, and where to go for help if symptoms do not subside over time.
Parent/Community meeting o Depending on the scope of the crisis, there may need to be a plan for an evening parent/community meeting. The principal, crisis response team, and crisis consultant should speak at the meeting, emphasizing what to expect in the grieving process, how to help students with the traumatic event, and where to go for help if symptoms do not subside over time.
 Evaluation o A proposal should be in the crisis plan to evaluate the Postvention intervention several weeks following the crisis.
Evaluation o A proposal should be in the crisis plan to evaluate the Postvention intervention several weeks following the crisis.
 Tennessee Suicide Prevention Network o In case of a suicide or an attempted suicide call TSPN for support, suggestions, and on site assistance: TSPN at (615)297 -1077 Scott Ridgway, M. S. director Website: www. tspn. org
Tennessee Suicide Prevention Network o In case of a suicide or an attempted suicide call TSPN for support, suggestions, and on site assistance: TSPN at (615)297 -1077 Scott Ridgway, M. S. director Website: www. tspn. org
 Restoring Community – a typical first day back to school o Crisis team plans how to disseminate information o All staff meeting before school (mandatory) o Staff most effected has time for small group debriefing o In the event of a student/teacher death, counselors follow the student/teacher schedule, and offer debriefing to classes
Restoring Community – a typical first day back to school o Crisis team plans how to disseminate information o All staff meeting before school (mandatory) o Staff most effected has time for small group debriefing o In the event of a student/teacher death, counselors follow the student/teacher schedule, and offer debriefing to classes
 Restoring Community continued…. o Students are identified who may need individual or group o o counseling and are offered such by school or community professionals A counseling room is set up and manned all day so that students can “self refer” themselves to counseling Food and drinks are brought to the teachers lounge, and a crisis team member is available there for supporting teachers. Parents can be involved by bringing food for the teacher’s lounge A simple mourning ritual may be put in place for the “empty desk” or locker.
Restoring Community continued…. o Students are identified who may need individual or group o o counseling and are offered such by school or community professionals A counseling room is set up and manned all day so that students can “self refer” themselves to counseling Food and drinks are brought to the teachers lounge, and a crisis team member is available there for supporting teachers. Parents can be involved by bringing food for the teacher’s lounge A simple mourning ritual may be put in place for the “empty desk” or locker.
 Restoring Community continued…. o Teachers receive training in the morning preparing them to work with their students o Students may be offered appropriate activities to combat “learned helplessness” (making wreaths, cards etc. ) o A mandatory staff meeting is also held at the end of the day, to debrief how the day went, identify areas that need further attention, and begin to evaluate the Postvention.
Restoring Community continued…. o Teachers receive training in the morning preparing them to work with their students o Students may be offered appropriate activities to combat “learned helplessness” (making wreaths, cards etc. ) o A mandatory staff meeting is also held at the end of the day, to debrief how the day went, identify areas that need further attention, and begin to evaluate the Postvention.
 Skills for Clinical Crisis Team Members o Psycho-education o Psychological first aid o Cultural Sensitivity o Crisis Debriefing o Identification and referral of students/faculty who need mental health assistance o Short-term crisis and/or bereavement counseling techniques
Skills for Clinical Crisis Team Members o Psycho-education o Psychological first aid o Cultural Sensitivity o Crisis Debriefing o Identification and referral of students/faculty who need mental health assistance o Short-term crisis and/or bereavement counseling techniques
 Psycho-education o Psychological effects of trauma exposure: n Recurrent dreams/nightmares n Intrusive thoughts or flashbacks n Sleep and/or appetite disturbance n Diminished interest in activities n Exaggerated startle response n Memory and concentration difficulties n Avoidance of activities which recall the event n Disturbing images or memories of the event n Feelings of detachment n A pattern of re-enactment in behavior or play
Psycho-education o Psychological effects of trauma exposure: n Recurrent dreams/nightmares n Intrusive thoughts or flashbacks n Sleep and/or appetite disturbance n Diminished interest in activities n Exaggerated startle response n Memory and concentration difficulties n Avoidance of activities which recall the event n Disturbing images or memories of the event n Feelings of detachment n A pattern of re-enactment in behavior or play
 Typical Reactions to Trauma by Developmental Stages
Typical Reactions to Trauma by Developmental Stages
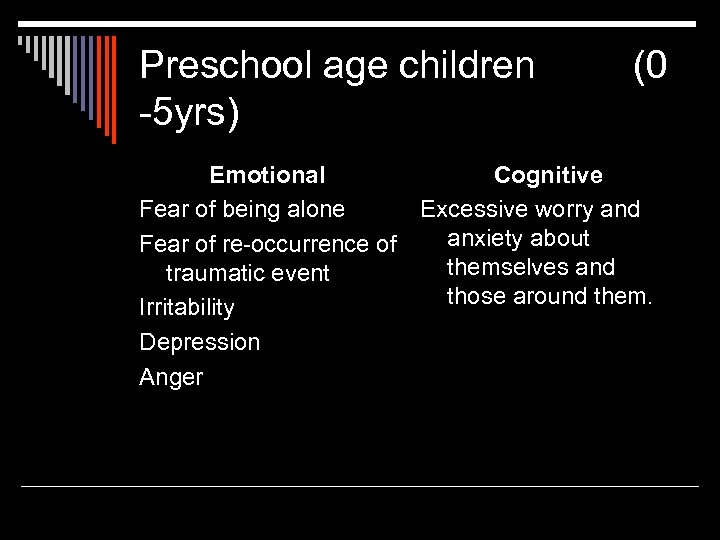 Preschool age children -5 yrs) (0 Emotional Cognitive Fear of being alone Excessive worry and anxiety about Fear of re-occurrence of themselves and traumatic event those around them. Irritability Depression Anger
Preschool age children -5 yrs) (0 Emotional Cognitive Fear of being alone Excessive worry and anxiety about Fear of re-occurrence of themselves and traumatic event those around them. Irritability Depression Anger
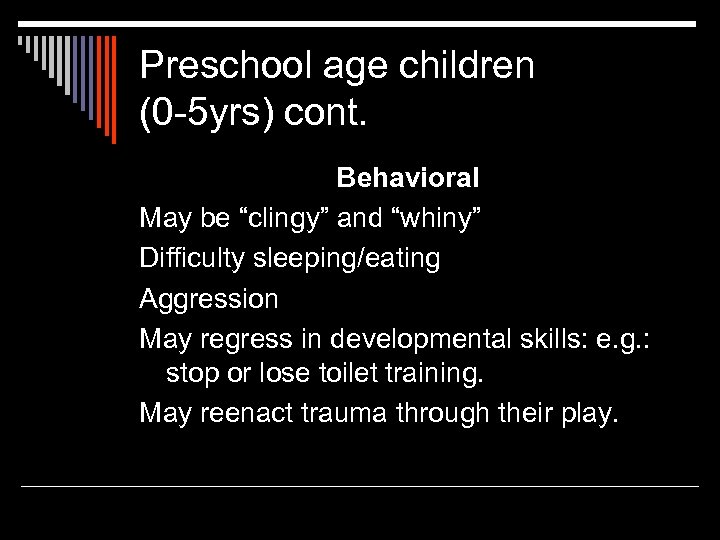 Preschool age children (0 -5 yrs) cont. Behavioral May be “clingy” and “whiny” Difficulty sleeping/eating Aggression May regress in developmental skills: e. g. : stop or lose toilet training. May reenact trauma through their play.
Preschool age children (0 -5 yrs) cont. Behavioral May be “clingy” and “whiny” Difficulty sleeping/eating Aggression May regress in developmental skills: e. g. : stop or lose toilet training. May reenact trauma through their play.
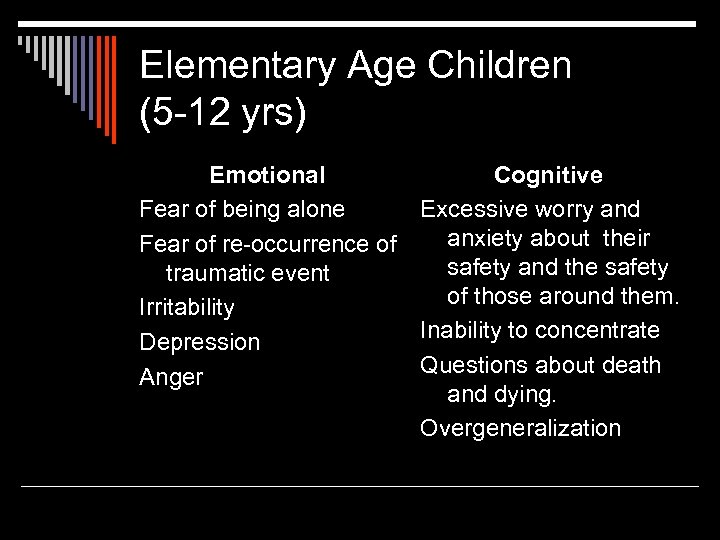 Elementary Age Children (5 -12 yrs) Emotional Cognitive Fear of being alone Excessive worry and anxiety about their Fear of re-occurrence of safety and the safety traumatic event of those around them. Irritability Inability to concentrate Depression Questions about death Anger and dying. Overgeneralization
Elementary Age Children (5 -12 yrs) Emotional Cognitive Fear of being alone Excessive worry and anxiety about their Fear of re-occurrence of safety and the safety traumatic event of those around them. Irritability Inability to concentrate Depression Questions about death Anger and dying. Overgeneralization
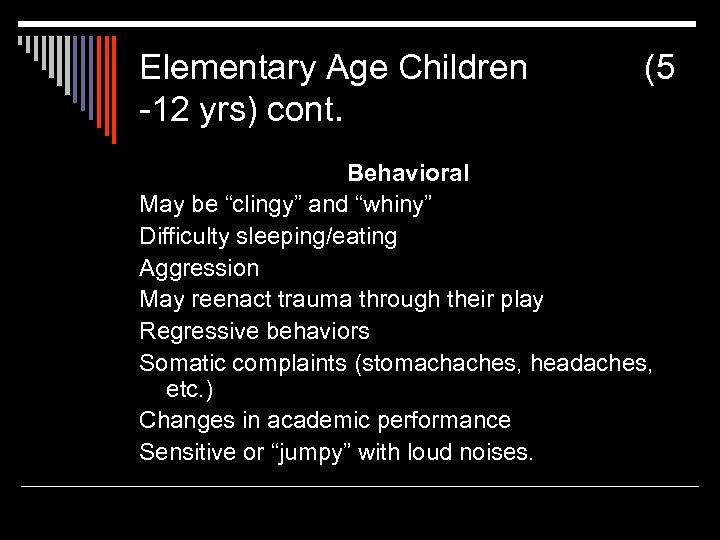 Elementary Age Children -12 yrs) cont. (5 Behavioral May be “clingy” and “whiny” Difficulty sleeping/eating Aggression May reenact trauma through their play Regressive behaviors Somatic complaints (stomachaches, headaches, etc. ) Changes in academic performance Sensitive or “jumpy” with loud noises.
Elementary Age Children -12 yrs) cont. (5 Behavioral May be “clingy” and “whiny” Difficulty sleeping/eating Aggression May reenact trauma through their play Regressive behaviors Somatic complaints (stomachaches, headaches, etc. ) Changes in academic performance Sensitive or “jumpy” with loud noises.
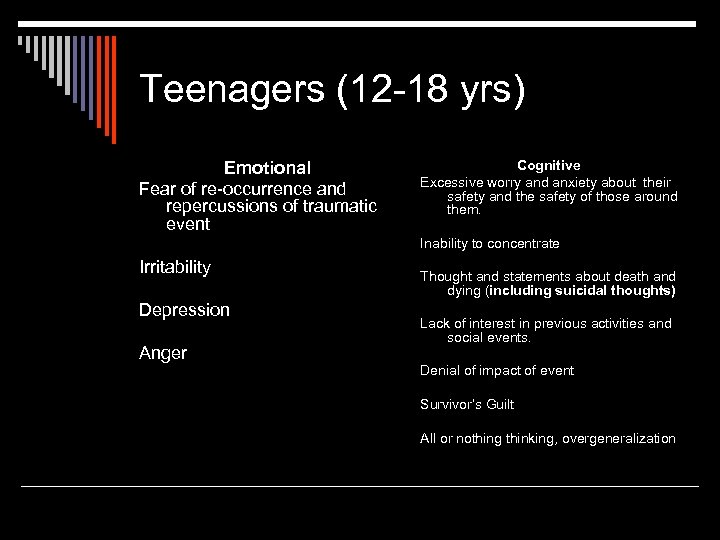 Teenagers (12 -18 yrs) Emotional Fear of re-occurrence and repercussions of traumatic event Cognitive Excessive worry and anxiety about their safety and the safety of those around them. Inability to concentrate Irritability Depression Anger Thought and statements about death and dying (including suicidal thoughts) Lack of interest in previous activities and social events. Denial of impact of event Survivor’s Guilt All or nothing thinking, overgeneralization
Teenagers (12 -18 yrs) Emotional Fear of re-occurrence and repercussions of traumatic event Cognitive Excessive worry and anxiety about their safety and the safety of those around them. Inability to concentrate Irritability Depression Anger Thought and statements about death and dying (including suicidal thoughts) Lack of interest in previous activities and social events. Denial of impact of event Survivor’s Guilt All or nothing thinking, overgeneralization
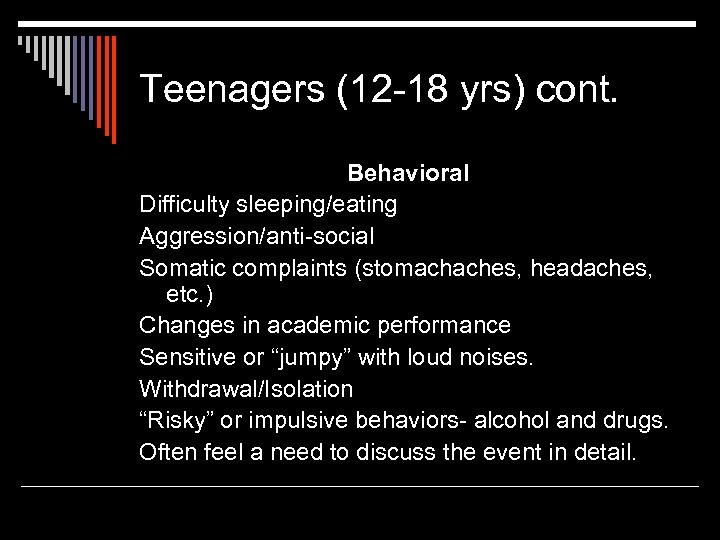 Teenagers (12 -18 yrs) cont. Behavioral Difficulty sleeping/eating Aggression/anti-social Somatic complaints (stomachaches, headaches, etc. ) Changes in academic performance Sensitive or “jumpy” with loud noises. Withdrawal/Isolation “Risky” or impulsive behaviors- alcohol and drugs. Often feel a need to discuss the event in detail.
Teenagers (12 -18 yrs) cont. Behavioral Difficulty sleeping/eating Aggression/anti-social Somatic complaints (stomachaches, headaches, etc. ) Changes in academic performance Sensitive or “jumpy” with loud noises. Withdrawal/Isolation “Risky” or impulsive behaviors- alcohol and drugs. Often feel a need to discuss the event in detail.
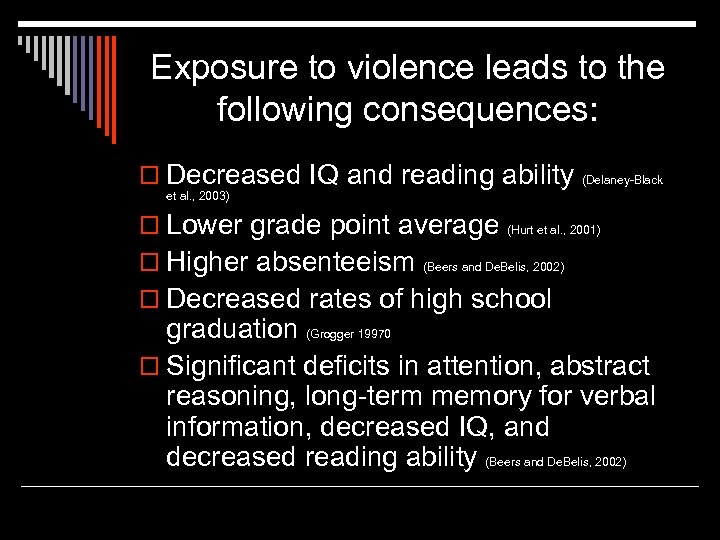 Exposure to violence leads to the following consequences: o Decreased IQ and reading ability (Delaney-Black et al. , 2003) o Lower grade point average o Higher absenteeism (Hurt et al. , 2001) (Beers and De. Belis, 2002) o Decreased rates of high school graduation (Grogger 19970 o Significant deficits in attention, abstract reasoning, long-term memory for verbal information, decreased IQ, and decreased reading ability (Beers and De. Belis, 2002)
Exposure to violence leads to the following consequences: o Decreased IQ and reading ability (Delaney-Black et al. , 2003) o Lower grade point average o Higher absenteeism (Hurt et al. , 2001) (Beers and De. Belis, 2002) o Decreased rates of high school graduation (Grogger 19970 o Significant deficits in attention, abstract reasoning, long-term memory for verbal information, decreased IQ, and decreased reading ability (Beers and De. Belis, 2002)
 “The Body Keeps Score” (Bessel Van der Kolk) o Physiological aspects of trauma exposure n n n “Fight or flight” hormones – emergency system Opiate system Can vacillate between the above cycling between “flooding” and “numbing” Trauma reminders (or triggers) can set off above Repeated exposure to trauma associated with structural changes in the brain
“The Body Keeps Score” (Bessel Van der Kolk) o Physiological aspects of trauma exposure n n n “Fight or flight” hormones – emergency system Opiate system Can vacillate between the above cycling between “flooding” and “numbing” Trauma reminders (or triggers) can set off above Repeated exposure to trauma associated with structural changes in the brain
 Psychological First Aid (Pynoos and Nadar 1988) First aid for feelings o The reduction of the initial distress caused by traumatic events and the fostering of short and long term adaptive functioning. Psychological First Aid is typically utilized in the immediate aftermath of a large scale disaster, when survivors are disoriented and in need of stabilization.
Psychological First Aid (Pynoos and Nadar 1988) First aid for feelings o The reduction of the initial distress caused by traumatic events and the fostering of short and long term adaptive functioning. Psychological First Aid is typically utilized in the immediate aftermath of a large scale disaster, when survivors are disoriented and in need of stabilization.
 Psychological First Aid Core Actions o Contact and Engagement: respond to contacts initiated by affected persons, or initiate contacts in a non-intrusive, compassionate, and helpful manner o Safety and Comfort: enhance immediate and ongoing safety, and provide physical and emotional comfort o Stabilization: calm and orient emotionallyoverwhelmed/distraught survivors
Psychological First Aid Core Actions o Contact and Engagement: respond to contacts initiated by affected persons, or initiate contacts in a non-intrusive, compassionate, and helpful manner o Safety and Comfort: enhance immediate and ongoing safety, and provide physical and emotional comfort o Stabilization: calm and orient emotionallyoverwhelmed/distraught survivors
 Psychological First Aid cont. o Information Gathering: Current Needs and Concerns: identify immediate needs and concerns, gather additional information, and tailor Psychological First Aid interventions o Practical Assistance: offer practical help to the survivor in addressing immediate needs and concerns o Connection with social support: help establish brief or ongoing contacts with primary support persons or other sources of support, including family members, friends, and community resources
Psychological First Aid cont. o Information Gathering: Current Needs and Concerns: identify immediate needs and concerns, gather additional information, and tailor Psychological First Aid interventions o Practical Assistance: offer practical help to the survivor in addressing immediate needs and concerns o Connection with social support: help establish brief or ongoing contacts with primary support persons or other sources of support, including family members, friends, and community resources
 Psychological First Aid cont. o Information on coping: provide information about stress reactions and coping to reduce distress and promote adaptive functioning o Linkage with collaborative services: link survivors with needed services, and inform them about available services that may be needed in the future. n n Explanation of Psychological First Aid taken from The National Center for Child Traumatic Stress, Field Operations Guide
Psychological First Aid cont. o Information on coping: provide information about stress reactions and coping to reduce distress and promote adaptive functioning o Linkage with collaborative services: link survivors with needed services, and inform them about available services that may be needed in the future. n n Explanation of Psychological First Aid taken from The National Center for Child Traumatic Stress, Field Operations Guide
 “Defusing” skills – Immediately Post Crisis, (within 12 hours) o This classroom defusing protocol is adapted from the George Everly and Jeffrey Mitchell model (1999) elaborated in Johnson et al. (1999) n n A brief, structured, discussion of the event within a small group context Introduction phase: Clearly state the purpose and format of the discussion. Set the following rules. Let each other speak, don’t interrupt, tell what happened if you wish, (or just listen), don’t criticize, and keep what’s said in the room
“Defusing” skills – Immediately Post Crisis, (within 12 hours) o This classroom defusing protocol is adapted from the George Everly and Jeffrey Mitchell model (1999) elaborated in Johnson et al. (1999) n n A brief, structured, discussion of the event within a small group context Introduction phase: Clearly state the purpose and format of the discussion. Set the following rules. Let each other speak, don’t interrupt, tell what happened if you wish, (or just listen), don’t criticize, and keep what’s said in the room
 “Defusing” skills cont. n n Exploration phase – the leader asks students to describe what happened and works toward pulling together consistency in the stories, and a sense of shared group experience. The leader can also ask for initial reactions from those students willing to share. Information phase – the leader summarizes students thoughts, clarifies misconceptions, normalizes student reactions. The leader also offers additional information as appropriate, outlines what he/she knows might happen next, and gives “stress management” tips.
“Defusing” skills cont. n n Exploration phase – the leader asks students to describe what happened and works toward pulling together consistency in the stories, and a sense of shared group experience. The leader can also ask for initial reactions from those students willing to share. Information phase – the leader summarizes students thoughts, clarifies misconceptions, normalizes student reactions. The leader also offers additional information as appropriate, outlines what he/she knows might happen next, and gives “stress management” tips.
 Critical Incident Stress Management Seven Phases of Debriefing (Mitchell model) Post Crisis 1 -10 days; 3 -4 wks for mass disasters o Introduction: development of group format, exploring the limits of confidentiality, and expected outcomes. o Fact Phase: clarify the facts, each member’s role, and discuss personal understanding of the event. o Thought Phase: reflect on the immediate thoughts as group members experienced or learned about the event. o Reaction Phase: members identify the most traumatic aspects of the event for them while voluntary discussion of emotions, validation, and support is provided.
Critical Incident Stress Management Seven Phases of Debriefing (Mitchell model) Post Crisis 1 -10 days; 3 -4 wks for mass disasters o Introduction: development of group format, exploring the limits of confidentiality, and expected outcomes. o Fact Phase: clarify the facts, each member’s role, and discuss personal understanding of the event. o Thought Phase: reflect on the immediate thoughts as group members experienced or learned about the event. o Reaction Phase: members identify the most traumatic aspects of the event for them while voluntary discussion of emotions, validation, and support is provided.
 Critical Incident Stress Management Seven Phases of Debriefing o Symptom Phase: return members to cognitive processing of event while identifying possible symptoms and reactions. o Teaching Phase: Normalize members reaction to traumatic event while emphasizing members symptoms should gradually get better and exposure will assist the process. o Closure/Re-Entry: summarize event and review main reactions, develop coping plan and identify members support systems.
Critical Incident Stress Management Seven Phases of Debriefing o Symptom Phase: return members to cognitive processing of event while identifying possible symptoms and reactions. o Teaching Phase: Normalize members reaction to traumatic event while emphasizing members symptoms should gradually get better and exposure will assist the process. o Closure/Re-Entry: summarize event and review main reactions, develop coping plan and identify members support systems.
 Crisis Management Briefings (CMB) Everly, 2001 (any time post crisis) o Bring together a large group o Offer a didactic presentation n Spokesperson presents the facts n Healthcare professional presents information about normal reactions to trauma n Healthcare professional offers self care strategies, referral resources, and handouts re. the above n There is a question and answer period
Crisis Management Briefings (CMB) Everly, 2001 (any time post crisis) o Bring together a large group o Offer a didactic presentation n Spokesperson presents the facts n Healthcare professional presents information about normal reactions to trauma n Healthcare professional offers self care strategies, referral resources, and handouts re. the above n There is a question and answer period
 Cultural Competence Sensitivity to culture is important in treating traumatized children o “A group whose characteristic response to illness is different from the dominant culture is likely to be labeled “abnormal”” (Mc. Goldrick 1996) n Latino children may manifest PTSD symptoms as “susto” (fright or soul loss) n Native Americans may develop “ghost sickness” n Different cultures have their own traditions and rituals for coping with trauma and stress o
Cultural Competence Sensitivity to culture is important in treating traumatized children o “A group whose characteristic response to illness is different from the dominant culture is likely to be labeled “abnormal”” (Mc. Goldrick 1996) n Latino children may manifest PTSD symptoms as “susto” (fright or soul loss) n Native Americans may develop “ghost sickness” n Different cultures have their own traditions and rituals for coping with trauma and stress o
 Ethnic Differences in Mental Health (Mc. Goldrick 1996) o Many studies have shown that people differ in the following: n n n Their experience of pain What they label as a symptom How they communicate about their pain or symptoms Their beliefs about its cause Their attitudes toward helpers The treatment they desire or expect
Ethnic Differences in Mental Health (Mc. Goldrick 1996) o Many studies have shown that people differ in the following: n n n Their experience of pain What they label as a symptom How they communicate about their pain or symptoms Their beliefs about its cause Their attitudes toward helpers The treatment they desire or expect
 Cultural/Ethnic differences in Bereavement, funeral traditions o Cultural, ethnic, and religious views and practices vary widely regarding death and funeral rites. n n n Some religions and cultures prohibit cremation, others require it Some religions require immediate burial (24 hours) In some cultures it is not appropriate to send flowers to the funeral home Bereavement practices vary widely, including “how long” it is “normal” to grieve Suicide is viewed differently in cultures and religions. Orthodox Jews and Lakota Native Americans share the tradition of “tearing clothing” as part of bereavement rituals
Cultural/Ethnic differences in Bereavement, funeral traditions o Cultural, ethnic, and religious views and practices vary widely regarding death and funeral rites. n n n Some religions and cultures prohibit cremation, others require it Some religions require immediate burial (24 hours) In some cultures it is not appropriate to send flowers to the funeral home Bereavement practices vary widely, including “how long” it is “normal” to grieve Suicide is viewed differently in cultures and religions. Orthodox Jews and Lakota Native Americans share the tradition of “tearing clothing” as part of bereavement rituals
 Cultural/Ethnic differences in Bereavement, funeral traditions o Working with cultural diversity requires knowledge and sensitivity o Being sensitive to others requires your own internal examination of biases o Do not assume that because a person has declared that they are of a specific faith that they will necessarily adhere to all the associated customs. There will be many variations and interpretations
Cultural/Ethnic differences in Bereavement, funeral traditions o Working with cultural diversity requires knowledge and sensitivity o Being sensitive to others requires your own internal examination of biases o Do not assume that because a person has declared that they are of a specific faith that they will necessarily adhere to all the associated customs. There will be many variations and interpretations
 What makes it difficult for us to be “culturally competent”? ? o “For most people, including Americans, the distinguishing mark of cross-cultural interaction is the disappearance of the familiar guideposts that allow them to act without thinking in their own culture. Routine matters become problems that require planning or conscious decisions. They may not know when to shake hands, nod their heads, ask a question, express an opinion, or maintain silence. ” o (Tramonte, Michael R. 1996)
What makes it difficult for us to be “culturally competent”? ? o “For most people, including Americans, the distinguishing mark of cross-cultural interaction is the disappearance of the familiar guideposts that allow them to act without thinking in their own culture. Routine matters become problems that require planning or conscious decisions. They may not know when to shake hands, nod their heads, ask a question, express an opinion, or maintain silence. ” o (Tramonte, Michael R. 1996)
 Cultural/Ethnic differences in Bereavement, funeral traditions o The crisis team member who has been working closely with the family of a deceased child (or faculty member) should check with the family regarding any potential “in school” memorials, and the appropriateness of the school response (sending flowers etc).
Cultural/Ethnic differences in Bereavement, funeral traditions o The crisis team member who has been working closely with the family of a deceased child (or faculty member) should check with the family regarding any potential “in school” memorials, and the appropriateness of the school response (sending flowers etc).
 Identification and referral of students who need mental health assistance o Counselors/psychologists/social workers will want to assess whether the student was directly or indirectly exposed to a perceived or real traumatic event o Assess symptoms including re-experiencing the traumatic event, avoidance, emotional numbing, increased arousal, sleep and appetite disturbance etc. o Are the symptoms interfering with the student’s functioning?
Identification and referral of students who need mental health assistance o Counselors/psychologists/social workers will want to assess whether the student was directly or indirectly exposed to a perceived or real traumatic event o Assess symptoms including re-experiencing the traumatic event, avoidance, emotional numbing, increased arousal, sleep and appetite disturbance etc. o Are the symptoms interfering with the student’s functioning?
 Identification and referral of students who need mental health assistance o Is there any evidence of suicidality? (thoughts, threats, actions) o Have intense symptoms lasted over a month? Over 3 months? o Is the child “at risk” due to other environmental factors or previous trauma? o Has the student exhibited significant behavior changes?
Identification and referral of students who need mental health assistance o Is there any evidence of suicidality? (thoughts, threats, actions) o Have intense symptoms lasted over a month? Over 3 months? o Is the child “at risk” due to other environmental factors or previous trauma? o Has the student exhibited significant behavior changes?
 Identification and referral of students who need mental health assistance o Student exhibits a high level of emotionality after the majority of peers return to more typical behavior o Students who are intentionally hurting themselves, or have an increase in other self harming behaviors including abusing alcohol/drugs o Students who do not improve with the individual and group interventions school personnel are able to provide
Identification and referral of students who need mental health assistance o Student exhibits a high level of emotionality after the majority of peers return to more typical behavior o Students who are intentionally hurting themselves, or have an increase in other self harming behaviors including abusing alcohol/drugs o Students who do not improve with the individual and group interventions school personnel are able to provide
 Helpful school-based interventions that can be administered by trained school personnel (counselors, social workers, psychologists) o Psycho-education n Educate students and their families about “normal” reactions to “abnormal” situations. Discuss and “normalize” trauma symptoms. It is typically also helpful to discuss “survivor’s guilt” when loss of life is involved. o Utilize evidence based trauma treatment concepts including Stress Inoculation Therapy, Cognitive Behavioral Therapy, and Exposure Therapies. Many “segments” of these protocols can “stand alone” and be very useful in helping students control symptoms.
Helpful school-based interventions that can be administered by trained school personnel (counselors, social workers, psychologists) o Psycho-education n Educate students and their families about “normal” reactions to “abnormal” situations. Discuss and “normalize” trauma symptoms. It is typically also helpful to discuss “survivor’s guilt” when loss of life is involved. o Utilize evidence based trauma treatment concepts including Stress Inoculation Therapy, Cognitive Behavioral Therapy, and Exposure Therapies. Many “segments” of these protocols can “stand alone” and be very useful in helping students control symptoms.
 o STRESS INOCULATION THERAPY (SIT) Donald Meichenbaum, Ph. D 1972 (as detailed in Mannarino and Cohen Child and Parent Trauma Focused CBT protocol) n n Encourages the use of optimal coping skills Can help protect children from some of the negative effects of stress Is taught before exposure strategies are utilized Stress inoculation therapy has 3 components RELAXATION, THOUGHT STOPPING, and COGNITIVE COPING
o STRESS INOCULATION THERAPY (SIT) Donald Meichenbaum, Ph. D 1972 (as detailed in Mannarino and Cohen Child and Parent Trauma Focused CBT protocol) n n Encourages the use of optimal coping skills Can help protect children from some of the negative effects of stress Is taught before exposure strategies are utilized Stress inoculation therapy has 3 components RELAXATION, THOUGHT STOPPING, and COGNITIVE COPING
 Relaxation o Helps treat PTSD symptoms of hyper-vigilance, increased startle response, agitation, difficulty sleeping o Deep Breathing i. e. “belly breathing”. Teach child to breathe in deeply so that the lower abdomen protrudes during inhalation, and recedes during exhalation. n Younger children can lay on the floor and put a book or stuffed animal on their lower abdomen n After the child masters this have the child count to 5 slowly while breathing through the nose, and count to 5 while slowly exhaling through the mouth
Relaxation o Helps treat PTSD symptoms of hyper-vigilance, increased startle response, agitation, difficulty sleeping o Deep Breathing i. e. “belly breathing”. Teach child to breathe in deeply so that the lower abdomen protrudes during inhalation, and recedes during exhalation. n Younger children can lay on the floor and put a book or stuffed animal on their lower abdomen n After the child masters this have the child count to 5 slowly while breathing through the nose, and count to 5 while slowly exhaling through the mouth
 Relaxation n Teach older children to focus their mind on the feeling of their breath moving in and out. As they become aware of other thoughts do not fight them, just notice them and return their mind to focus on their breath moving in and out. The goal is not to judge, reject, or focus on the thought, simply to learn to redirect the mind to your breathing.
Relaxation n Teach older children to focus their mind on the feeling of their breath moving in and out. As they become aware of other thoughts do not fight them, just notice them and return their mind to focus on their breath moving in and out. The goal is not to judge, reject, or focus on the thought, simply to learn to redirect the mind to your breathing.
 Stress Inoculation Therapy Relaxation cont. o Progressive muscle relaxation n Demonstrate to child the difference between stiff and relaxed muscles (can use spaghetti before and after cooked, tin soldier vs. Raggedy Ann doll etc) Instruct children to first tense and then relax muscles, starting with the toes, then the foot, ankle etc. all the way up to the head, until every muscle has been relaxed. (best done lying down) Children can be instructed to use this technique when trying to go to sleep, or when bothered by intrusive recollections of the trauma
Stress Inoculation Therapy Relaxation cont. o Progressive muscle relaxation n Demonstrate to child the difference between stiff and relaxed muscles (can use spaghetti before and after cooked, tin soldier vs. Raggedy Ann doll etc) Instruct children to first tense and then relax muscles, starting with the toes, then the foot, ankle etc. all the way up to the head, until every muscle has been relaxed. (best done lying down) Children can be instructed to use this technique when trying to go to sleep, or when bothered by intrusive recollections of the trauma
 Stress Inoculation Training Thought Stopping o Designed to “short circuit” the cycle of negative thinking which can be problematic for traumatized children o Teaches children that they can have control over their thoughts
Stress Inoculation Training Thought Stopping o Designed to “short circuit” the cycle of negative thinking which can be problematic for traumatized children o Teaches children that they can have control over their thoughts
 HOW TO TEACH THOUGHT STOPPING 1. Talk to children about telling their mind to stop (say “go away” or “snap out of it” or “stop”) 2. Replace that unwanted thought with a welcomed one. It is useful to have children prepare for thought stopping by having a positive thought or mental image ready –such as thinking about a special happy event, place, or experience. It may be helpful for children to visualize a “perfect moment” such as hitting a home run.
HOW TO TEACH THOUGHT STOPPING 1. Talk to children about telling their mind to stop (say “go away” or “snap out of it” or “stop”) 2. Replace that unwanted thought with a welcomed one. It is useful to have children prepare for thought stopping by having a positive thought or mental image ready –such as thinking about a special happy event, place, or experience. It may be helpful for children to visualize a “perfect moment” such as hitting a home run.
 HOW TO TEACH THOUGHT STOPPING 3. The mental picture can be drawn and taken home as a prompt to use in thought stopping at home. Also, the more details in this image (smell, sound, taste, sight etc) the more useful the image is likely to be for the child.
HOW TO TEACH THOUGHT STOPPING 3. The mental picture can be drawn and taken home as a prompt to use in thought stopping at home. Also, the more details in this image (smell, sound, taste, sight etc) the more useful the image is likely to be for the child.
 Stress Inoculation Training Cognitive Coping Skills o Cognitive Coping refers to exercise positive thinking rest Eat well acceptance “learned optimism” o Help child practice the skill of focusing on the positive instead of the negative aspects of a given situation o Is there anything positive in a trauma? Child might be “stronger”, more compassionate towards others, more thankful for family members, etc. o Help child recognize that in spite of the trauma they “are coping” and often quite well.
Stress Inoculation Training Cognitive Coping Skills o Cognitive Coping refers to exercise positive thinking rest Eat well acceptance “learned optimism” o Help child practice the skill of focusing on the positive instead of the negative aspects of a given situation o Is there anything positive in a trauma? Child might be “stronger”, more compassionate towards others, more thankful for family members, etc. o Help child recognize that in spite of the trauma they “are coping” and often quite well.
 Teach positive self talk! Examples: I can get through this Things are hard now, but they will get better. I still have a family and they will help me Lots of people care about me and my family Some things have changed, but lots of things are the same as they were before this happened (I still do well in school, I still have friends etc) o I’m strong, I lived through it o o o OPTIMISM CAN BE LEARNED AND PRACTICED. ENCOURAGE CHILDREN TO PRACTICE POSITIVE SELF-STATEMENTS
Teach positive self talk! Examples: I can get through this Things are hard now, but they will get better. I still have a family and they will help me Lots of people care about me and my family Some things have changed, but lots of things are the same as they were before this happened (I still do well in school, I still have friends etc) o I’m strong, I lived through it o o o OPTIMISM CAN BE LEARNED AND PRACTICED. ENCOURAGE CHILDREN TO PRACTICE POSITIVE SELF-STATEMENTS
 Common cognitive distortions of traumatized children o I should have been able to keep it (the traumatic o o o event) from happening My family will never be okay again It is my responsibility to become “the man of the house” now that my dad is dead I will never get back to normal/happy again The world will never be safe again I can’t trust anyone any more School will never be safe again
Common cognitive distortions of traumatized children o I should have been able to keep it (the traumatic o o o event) from happening My family will never be okay again It is my responsibility to become “the man of the house” now that my dad is dead I will never get back to normal/happy again The world will never be safe again I can’t trust anyone any more School will never be safe again
 Persistent Exposure in trauma treatment o Exposure strategies have consistently been shown to be o o o useful in trauma treatment The “heart” of the treatment typically involves the child (or parent) “telling the trauma narrative” Stress inoculation strategies and/or other “containment” strategies must be taught first Exposure aspects of the treatment are beyond the scope of today’s presentation (and may not always be appropriate for the school setting) School personnel need to know however that processing and talking about the trauma is good for students who initiate such discussions. Students should not be “forced” to speak about the traumatic event.
Persistent Exposure in trauma treatment o Exposure strategies have consistently been shown to be o o o useful in trauma treatment The “heart” of the treatment typically involves the child (or parent) “telling the trauma narrative” Stress inoculation strategies and/or other “containment” strategies must be taught first Exposure aspects of the treatment are beyond the scope of today’s presentation (and may not always be appropriate for the school setting) School personnel need to know however that processing and talking about the trauma is good for students who initiate such discussions. Students should not be “forced” to speak about the traumatic event.
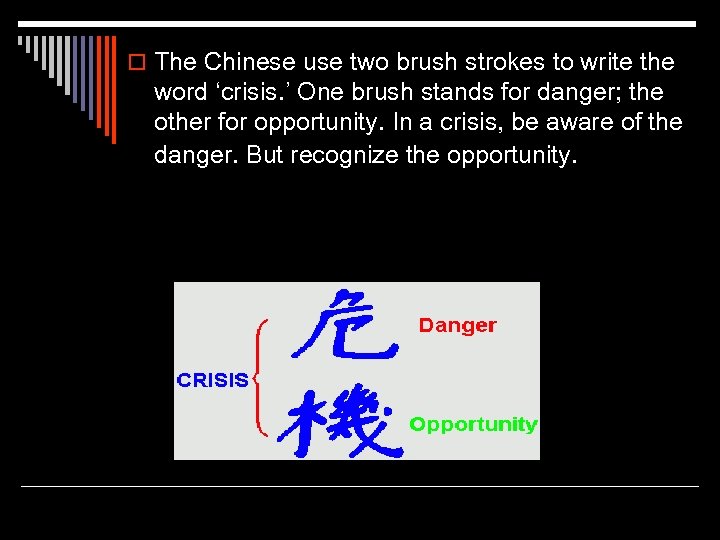 o The Chinese use two brush strokes to write the word ‘crisis. ’ One brush stands for danger; the other for opportunity. In a crisis, be aware of the danger. But recognize the opportunity.
o The Chinese use two brush strokes to write the word ‘crisis. ’ One brush stands for danger; the other for opportunity. In a crisis, be aware of the danger. But recognize the opportunity.


