93a211b3c4b29d6e6b747d5cfd05b7fb.ppt
- Количество слайдов: 100
SBIRT: Reducing Alcohol Related Morbidity and Mortality in Primary Care J. Paul Seale, MD, Principal Investigator Sylvia Shellenberger, Ph. D, Director of Training Denice Crowe Clark, MFT, Project Coordinator Department of Family Medicine Mercer University School of Medicine The Southeastern Consortium for Substance Abuse Training (SECSAT) Funded by Grant 1 U 79 T 1020278 -01 Substance Abuse and Mental Health Services Administration (SAMHSA) 1
SECSAT Key Personnel: Mercer Project Staff J. Paul Seale, MD, PI Denice Crowe Clark, MFT Project Coordinator Sylvia Shellenberger, Ph. D Director of Training J. Aaron Johnson, Ph. D Director of Evaluation Bonnie Cole, JD, MFT Standardized Patient Trainer 2
SECSAT Key Personnel: Site Coordinators David Miller, MD Wake Forest UBMC IM Residency Winston-Salem, NC David Parish, MD Mercer University School of Medicine IM Residency Macon, GA J. Paul Seale, MD Mercer University School of Medicine FM Residency Macon, GA Hunter Woodall, MD An. Med Health FM Residency Anderson, SC 3
Module 1 A Objectives n n Describe the importance of alcohol misuse as a health issue Examine the evidence base for alcohol screening brief intervention & referral to treatment (SBIRT) Outline the rationale for implementing SBIRT in primary health care Provide an overview of the steps in “SECSAT” Project 4
What is SBIRT? Screening Brief Intervention Referral to Treatment 5
What is SBIRT? n SBIRT is a comprehensive, integrated, evidence-based approach to the delivery of early intervention and treatment services for individuals with substance use problems or risk. Burge et al, 2009 6
What is SBIRT? n n n Screening quickly assesses the severity of substance use and identifies the appropriate level of treatment. Brief Intervention focuses on increasing insight and awareness regarding substance use and motivation toward behavioral change. Referral to Treatment provides those identified as needing more extensive treatment with access to specialty care. 7
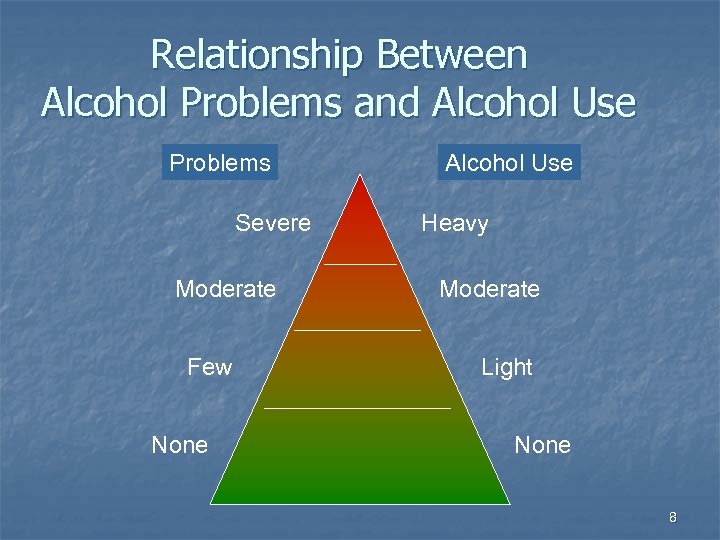
Relationship Between Alcohol Problems and Alcohol Use Problems Severe Moderate Few None Alcohol Use Heavy Moderate Light None 8
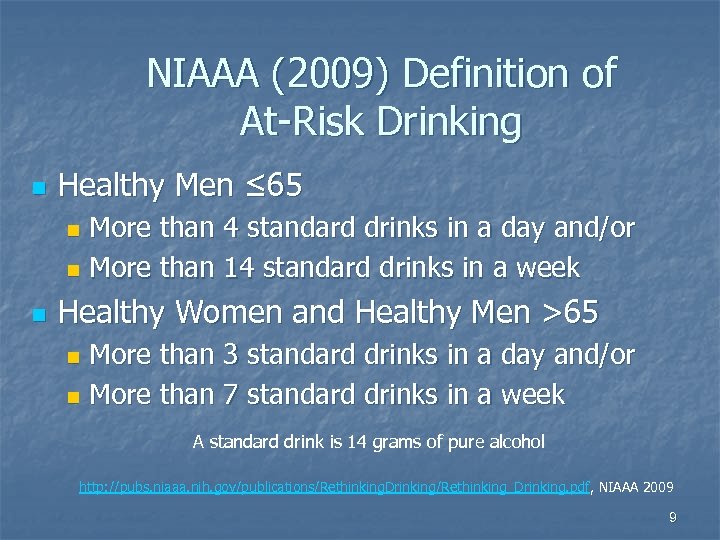
NIAAA (2009) Definition of At-Risk Drinking n Healthy Men ≤ 65 More than 4 standard drinks in a day and/or n More than 14 standard drinks in a week n n Healthy Women and Healthy Men >65 More than 3 standard drinks in a day and/or n More than 7 standard drinks in a week n A standard drink is 14 grams of pure alcohol http: //pubs. niaaa. nih. gov/publications/Rethinking. Drinking/Rethinking_Drinking. pdf, NIAAA 2009 9
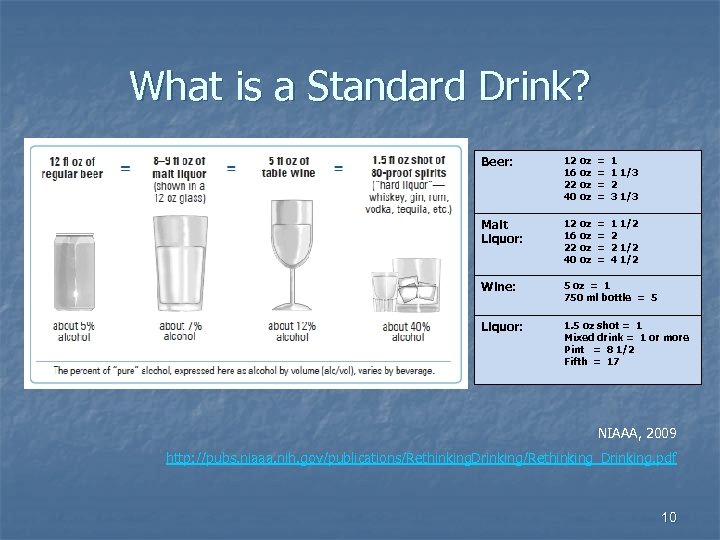
What is a Standard Drink? Beer: 12 oz 16 oz 22 oz 40 oz = = 1 1 1/3 2 3 1/3 Malt Liquor: 12 oz 16 oz 22 oz 40 oz = = 1 1/2 2 2 1/2 4 1/2 Wine: 5 oz = 1 750 ml bottle = 5 Liquor: 1. 5 oz shot = 1 Mixed drink = 1 or more Pint = 8 1/2 Fifth = 17 NIAAA, 2009 http: //pubs. niaaa. nih. gov/publications/Rethinking. Drinking/Rethinking_Drinking. pdf 10

Why is Management of Alcohol Misuse Important to Primary Care Physicians? n n n Prevalence Morbidity and mortality Barrier to treatment of chronic conditions Cost & time saving Potential for effective intervention 11
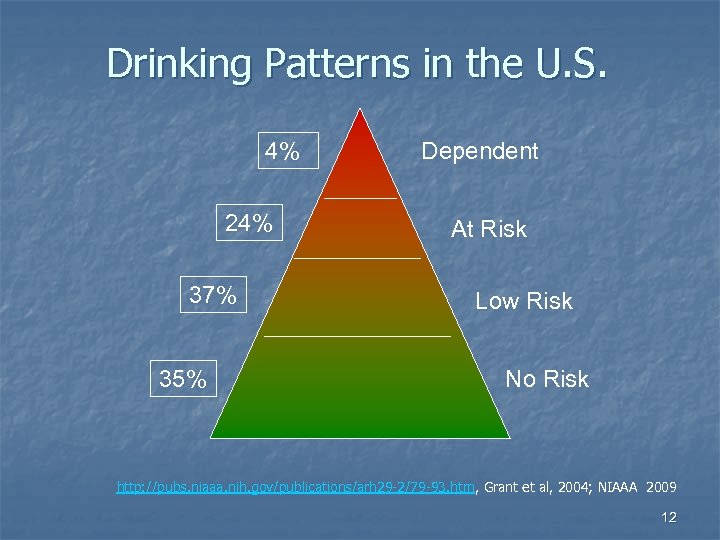
Drinking Patterns in the U. S. 4% 24% 37% 35% Dependent At Risk Low Risk No Risk http: //pubs. niaaa. nih. gov/publications/arh 29 -2/79 -93. htm, Grant et al, 2004; NIAAA 2009 12

Who Needs Attention? Nearly 3 in 10 exceed limits but most (24%) do not have alcohol dependence At Risk (19%) Functionally Dependent (3%) Abuse (5%) Willenbring, 2010; NIAAA, 2009 Severely Dependent (1%) 13
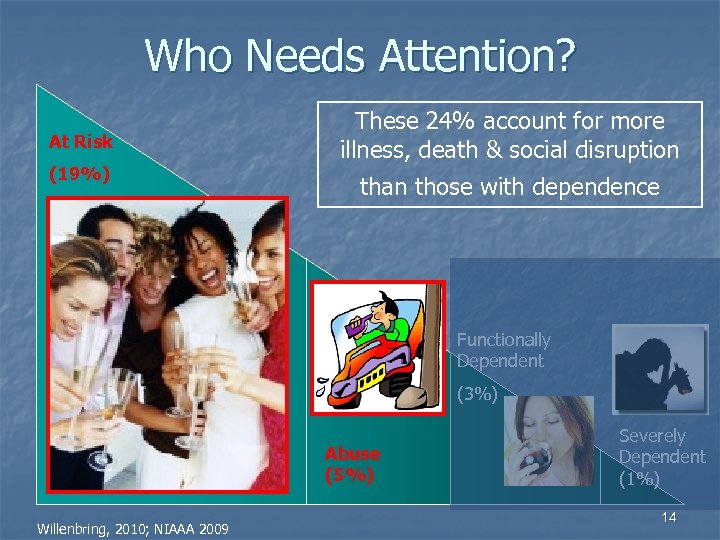
Who Needs Attention? At Risk (19%) These 24% account for more illness, death & social disruption than those with dependence Functionally Dependent (3%) Abuse (5%) Willenbring, 2010; NIAAA 2009 Severely Dependent (1%) 14
Alcohol Misuse is Commonly Encountered by Primary Care Physicians n n 7 -20% of primary care patients exhibit patterns of alcohol misuse 24 -31% of patients in ERs 22% of minor trauma patients 50% of severely-injured trauma patients Fiellin et al, 2000; D’Onofrio & Degutis, 2002 15
Why Important: Morbidity & Mortality n n n Alcohol is the third leading cause of preventable death in the US (CDC), (76, 000 deaths, or 5% of all deaths in 2001) Alcohol is attributable to 4 -8% of Disability. Adjusted Life Years (DALYs) in the US (WHO). Globally, alcohol causes morbidity and mortality at a higher rate than tobacco (WHO). http: //www. cdc. gov/mmwr/preview/mmwrhtml/mm 5337 a 2. htm, CDC, 2004; http: //www. who. int/substance_abuse/facts/alcohol/en/index. html, WHO, 2010; http: //www. who. int/substance_abuse/publications/en/APDSSummary. pdf; WHO, 2002 16
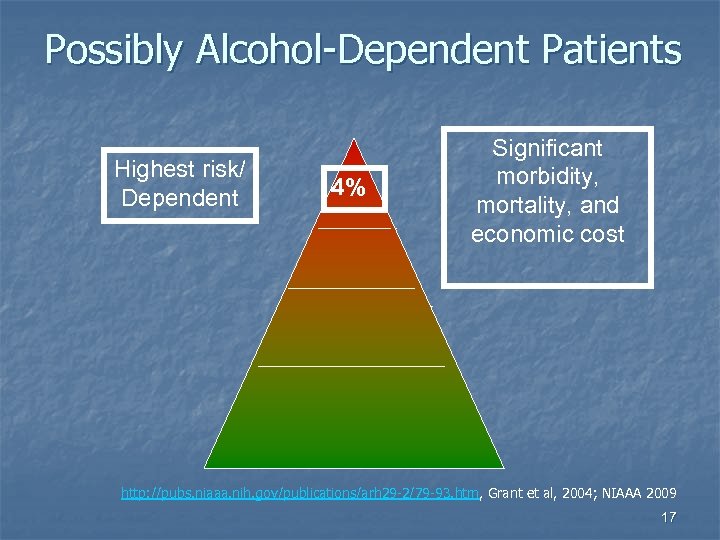
Possibly Alcohol-Dependent Patients Highest risk/ Dependent 4% Significant morbidity, mortality, and economic cost http: //pubs. niaaa. nih. gov/publications/arh 29 -2/79 -93. htm, Grant et al, 2004; NIAAA 2009 17
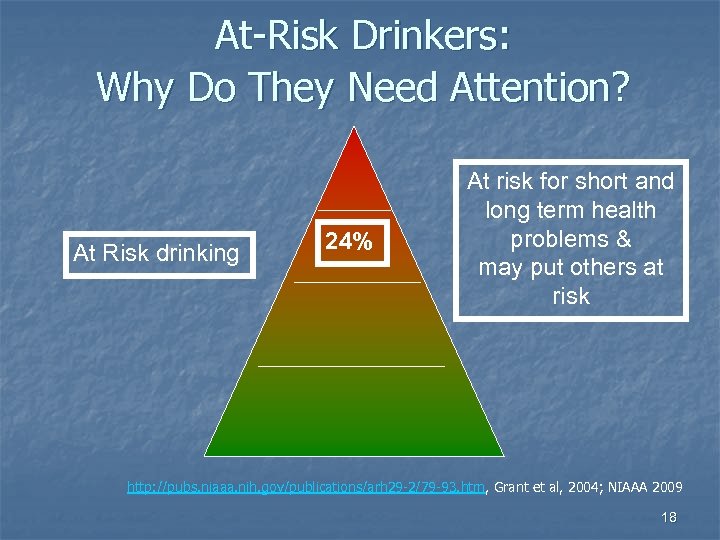
At-Risk Drinkers: Why Do They Need Attention? At Risk drinking 24% At risk for short and long term health problems & may put others at risk http: //pubs. niaaa. nih. gov/publications/arh 29 -2/79 -93. htm, Grant et al, 2004; NIAAA 2009 18
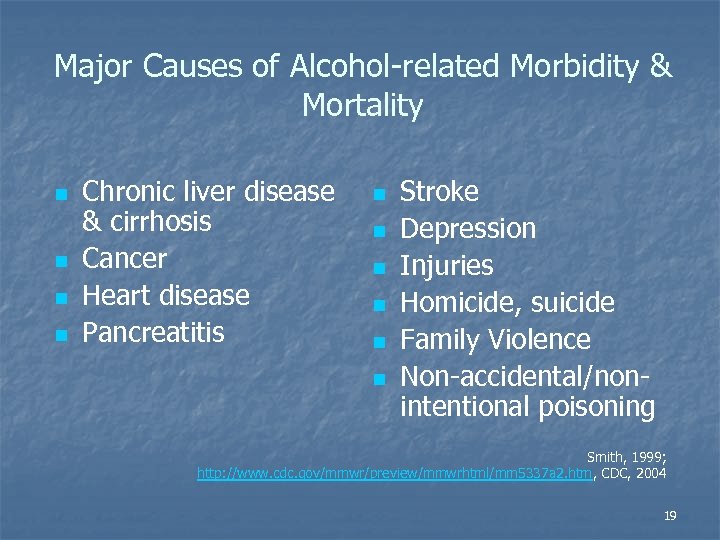
Major Causes of Alcohol-related Morbidity & Mortality n n Chronic liver disease & cirrhosis Cancer Heart disease Pancreatitis n n n Stroke Depression Injuries Homicide, suicide Family Violence Non-accidental/nonintentional poisoning Smith, 1999; http: //www. cdc. gov/mmwr/preview/mmwrhtml/mm 5337 a 2. htm, CDC, 2004 19
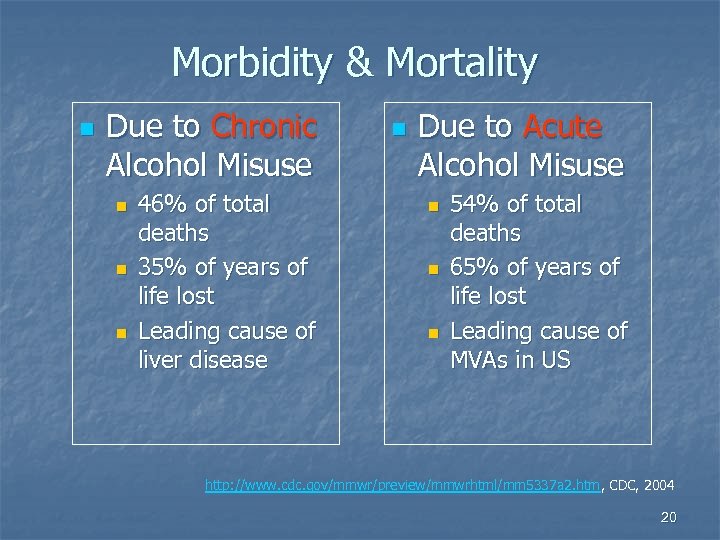
Morbidity & Mortality n Due to Chronic Alcohol Misuse n n n 46% of total deaths 35% of years of life lost Leading cause of liver disease n Due to Acute Alcohol Misuse n n n 54% of total deaths 65% of years of life lost Leading cause of MVAs in US http: //www. cdc. gov/mmwr/preview/mmwrhtml/mm 5337 a 2. htm, CDC, 2004 20
Why Important: Morbidity n n Alcohol interacts with many medications Exacerbates numerous chronic medical conditions (HTN, DM, PUD, etc. ) Rehm et al, 2002; Stranges et al, 2004; http: //pubs. niaaa. nih. gov/publications/aa 26. htm, NIAAA 2000; http: //pubs. niaaa. nih. gov/publications/Medicine/medicine. htm, NIAAA 2007 21
Alcohol Misuse Complicates Treatment of Chronic Medical Conditions 22
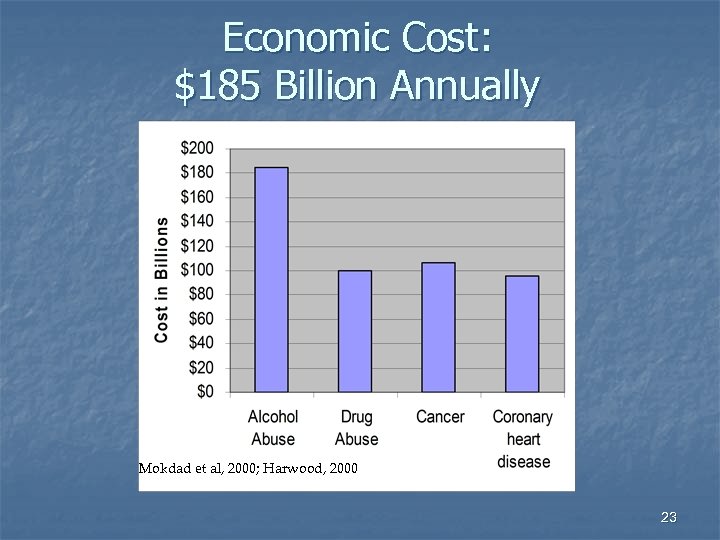
Economic Cost: $185 Billion Annually Mokdad et al, 2000; Harwood, 2000 23
Increasing Patient Recognition of Alcohol as a Health Issue n Expectation that health care providers will give sound advice about alcohol Potential benefits for cardiovascular conditions n Potential breast cancer risk among women n http: //www. niaaa. nih. gov/FAQs/General-English/default. htm#heart; NIAAA 2007; http: //pubs. niaaa. nih. gov/publications/brochurewomen/women. htm#drinking; NIAAA 2008 24
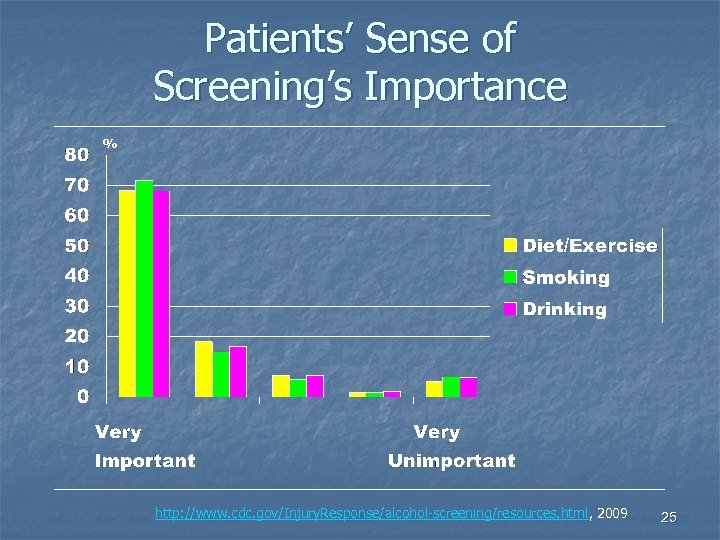
Patients’ Sense of Screening’s Importance % http: //www. cdc. gov/Injury. Response/alcohol-screening/resources. html, 2009 25
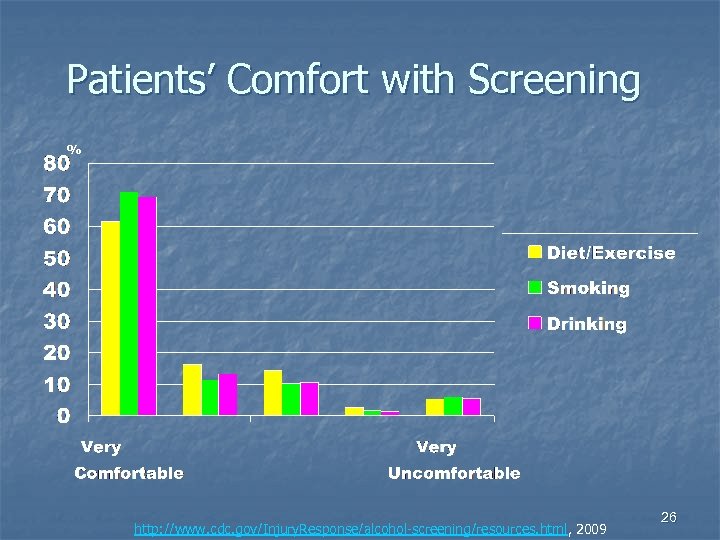
Patients’ Comfort with Screening % http: //www. cdc. gov/Injury. Response/alcohol-screening/resources. html, 2009 26
Why SBIRT? n n n At-risk drinking is common At-risk drinking increases risk for trauma and other health problems At-risk drinking exacerbates chronic health problems At-risk drinking often goes undetected Patients are more open to change than you might expect You can make a difference! Adapted from Burge et al, 2009 27
What is the Evidence Base for SBIRT? n Does SBIRT really change patients’ drinking behavior? 28
Brief Intervention Works! n SBIRT meta-analyses & reviews: More than 34 randomized controlled trials n Focused primarily on at risk and problem drinkers n Result in 10 -30% reduction in alcohol consumption at 12 months n Moyer et al, 2002; Whitlock et al, 2004; Bertholet et al, 2005; Kaner et al, 2007 29
Net Percentage Reduction in Mean Drinks Per Week (USPSTF review) n 9 high quality studies reviewed 3 single intervention studies resulted in reductions in weekly alcohol consumption ranging from 6 -19% n 6 multi-contact intervention studies resulted in reductions in weekly alcohol consumption ranging from 7 -34% n http: //www. ahrq. gov/clinic/3 rduspstf/alcohol/alcomissum. htm, Whitlock et al, 2004 30
US Preventive Services Task Force: SBIRT Recommended for All Adult PC Patients n n n Class B recommendation (flu shots, cholesterol screening, SBIRT) “…good evidence that screening in primary care can accurately identify patients whose levels of alcohol consumption…place them at risk for increased morbidity and mortality” “…good evidence that brief behavioral counseling interventions…produce small to moderate reductions in alcohol consumption” http: //www. ahrq. gov/clinic/uspstf/uspsdrin. htm; USPSTF, 2004 31

SBIRT & Joint Commission Accreditation n Currently being considered by the Joint Commission as a requirement for hospital accreditation Performance measures in development in 2009 for tobacco and alcohol use Pilot testing in hospitals began in 2010 The Joint Commission, November 2009 http: //www. jointcommission. org/Performance. Measurement 32
Nursing Involvement Significantly Increases Clinician Intervention Rates n n Vital Signs Study: clinicians were 12 x more likely to intervene if nurses screened for at -risk drinking as part of vital signs Healthy Habits Study: clinicians were 3 x more likely to intervene with at-risk drinkers if given alcohol assessment results by the nurse Seale et al, 2005; Seale et al, 2010 33
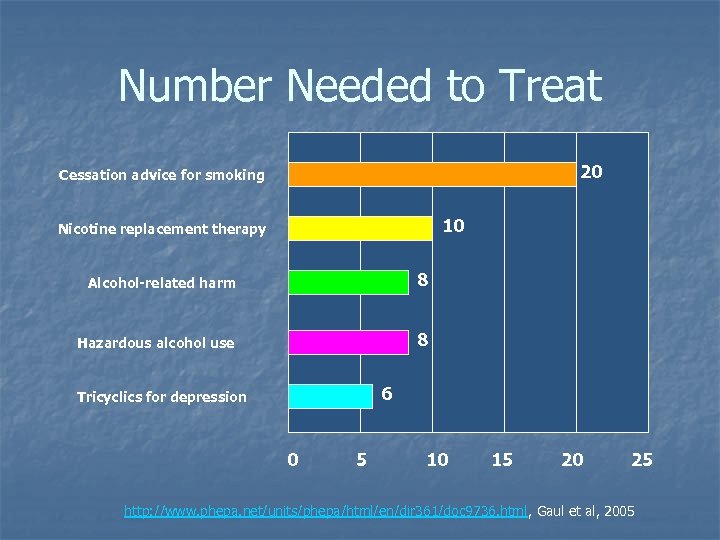
Number Needed to Treat 20 Cessation advice for smoking 10 Nicotine replacement therapy Alcohol-related harm 8 Hazardous alcohol use 8 6 Tricyclics for depression 0 5 10 15 20 25 http: //www. phepa. net/units/phepa/html/en/dir 361/doc 9736. html, Gaul et al, 2005
What Does This Mean for Your Patients? Calculate based on the numbers of adult patients you see per week… For example, if n n n You see on average 40 patients per week If 20% of these patients are at risk (8 patients) With brief intervention, 1 patient weekly is likely to lower his/her risk http: //www. phepa. net/units/phepa/html/en/dir 361/doc 9736. html, Gaul et al, 2005
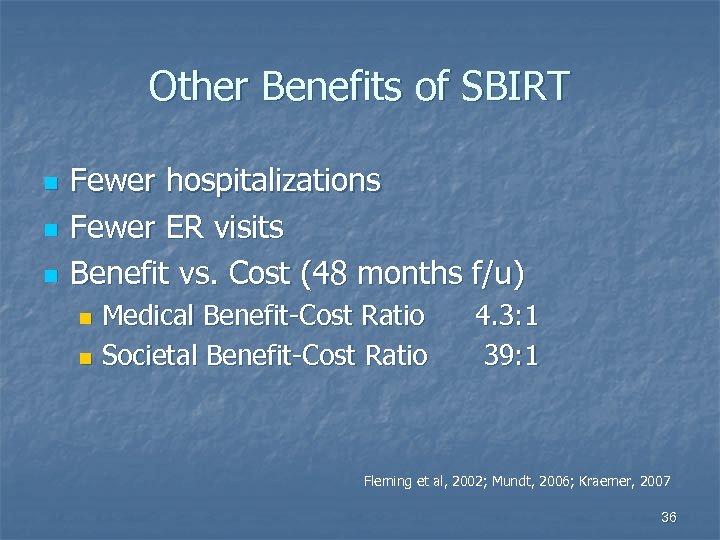
Other Benefits of SBIRT n n n Fewer hospitalizations Fewer ER visits Benefit vs. Cost (48 months f/u) Medical Benefit-Cost Ratio n Societal Benefit-Cost Ratio n 4. 3: 1 39: 1 Fleming et al, 2002; Mundt, 2006; Kraemer, 2007 36
SBIRT is Underutilized in Primary Care n n Less than half of self-reported problem drinkers are asked by their PC physicians about their alcohol consumption or advised to quit drinking or cut back. Most PC physicians prefer not to counsel nondependent problem drinkers themselves. D’Amico et al, 2005; Spandorfer et al, 1999 37
SBIRT Can Be Effectively Implemented in Primary Care n n Effective models exist for implementing screening and brief intervention in residency training. Trained clinicians typically intervene with more than 70% of patients. Seale et al, 2005; Adams et al, 1998 38
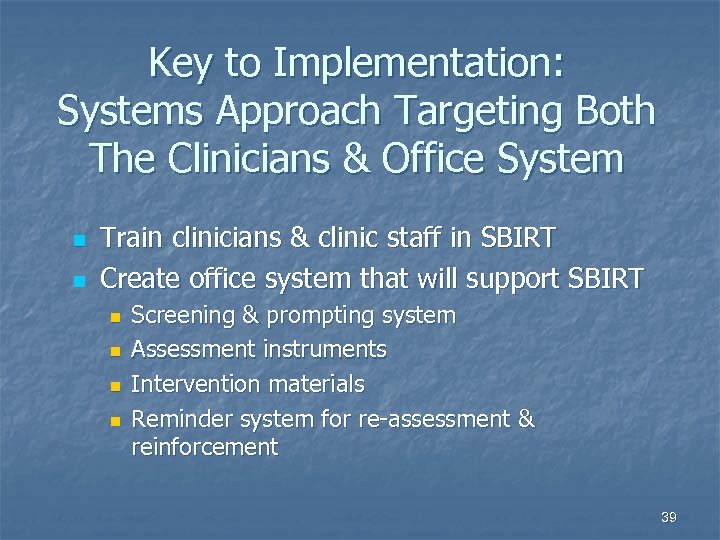
Key to Implementation: Systems Approach Targeting Both The Clinicians & Office System n n Train clinicians & clinic staff in SBIRT Create office system that will support SBIRT n n Screening & prompting system Assessment instruments Intervention materials Reminder system for re-assessment & reinforcement 39
5 Basic Components of This Project’s SBIRT System n n n Prescreening of all patients usingle question screen Screening of all prescreen-positive patients using the Alcohol Use Disorders Identification Test (AUDIT) Clinician Interventions for all screen-positive patients Referral for patients desiring more help Follow-up (re-assessment & reinforcement) at future visits 40
Summary of Module 1 A n n Alcohol misuse is a major cause of morbidity & mortality in the US SBIRT is effective in decreasing at risk drinking & its related consequences Clinician training & systems intervention are effective in implementing primary care SBIRT protocols Training Modules 1 B & 1 C will equip this clinic to effectively perform SBIRT—stay tuned! 41
Module 1 B The Procedures of Screening, Brief Intervention & Referral to Treatment 42
Objectives for Module 1 B n n n Describe the procedures of SBIRT Practice using and scoring the Healthy Habits Prescreen and the Healthy Lifestyles Screen (AUDIT) Review the steps of the intervention for at- risk drinkers Review added steps for those possibly dependent Practice conducting interventions 43
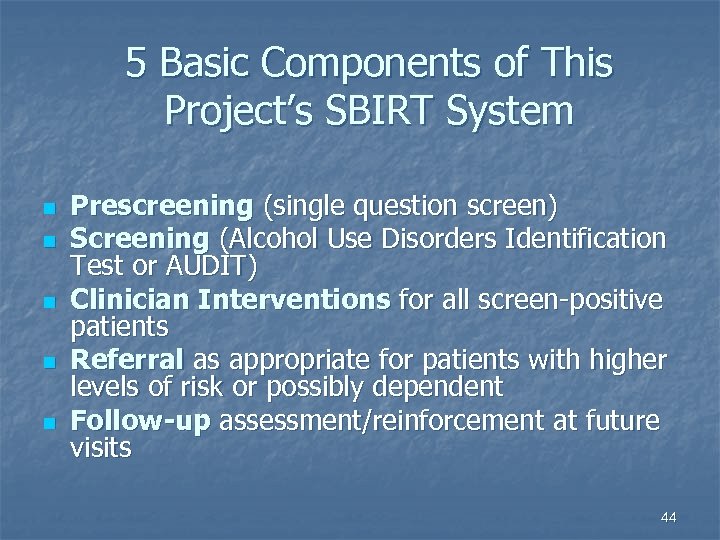
5 Basic Components of This Project’s SBIRT System n n n Prescreening (single question screen) Screening (Alcohol Use Disorders Identification Test or AUDIT) Clinician Interventions for all screen-positive patients Referral as appropriate for patients with higher levels of risk or possibly dependent Follow-up assessment/reinforcement at future visits 44

STEP 1: Prescreen is routinely performed every 6 -12 months Tool: Single alcohol screening question (SASQ - NIAAA) 45
Single Question: n “How many times in the past 12 months have you had X or more drinks in a day? ” X = 5 for men n X = 4 for women n n Positive screen = one or more times in the past year 46
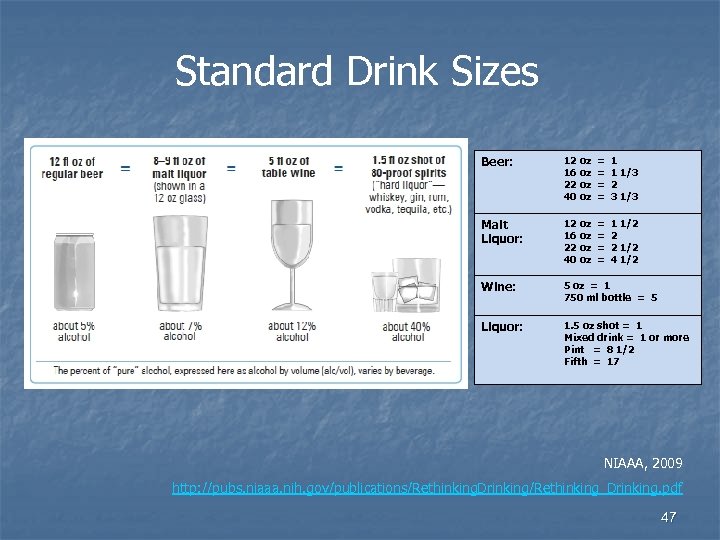
Standard Drink Sizes Beer: 12 oz 16 oz 22 oz 40 oz = = 1 1 1/3 2 3 1/3 Malt Liquor: 12 oz 16 oz 22 oz 40 oz = = 1 1/2 2 2 1/2 4 1/2 Wine: 5 oz = 1 750 ml bottle = 5 Liquor: 1. 5 oz shot = 1 Mixed drink = 1 or more Pint = 8 1/2 Fifth = 17 NIAAA, 2009 http: //pubs. niaaa. nih. gov/publications/Rethinking. Drinking/Rethinking_Drinking. pdf 47
Process When Prescreen is Positive n n n Patient is given the Healthy Lifestyles Screen (AUDIT) Patient completes the AUDIT and gives it to his/her clinician Physician performs intervention 48
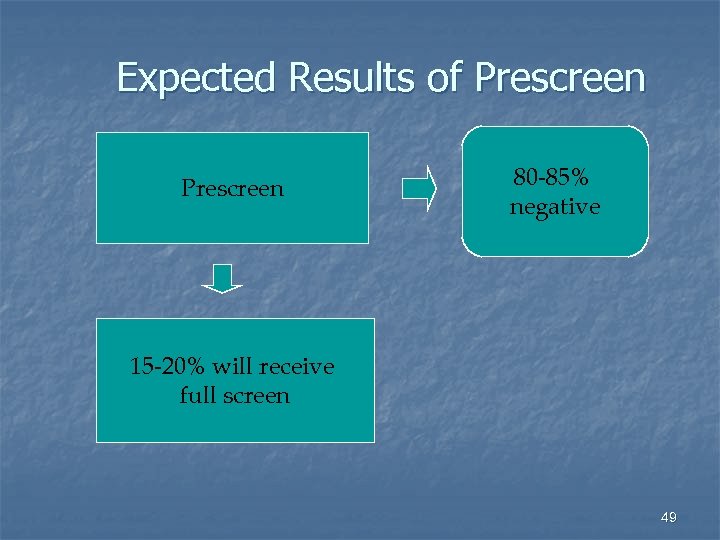
Expected Results of Prescreen 80 -85% negative 15 -20% will receive full screen 49
Step 2: Screening 50
51
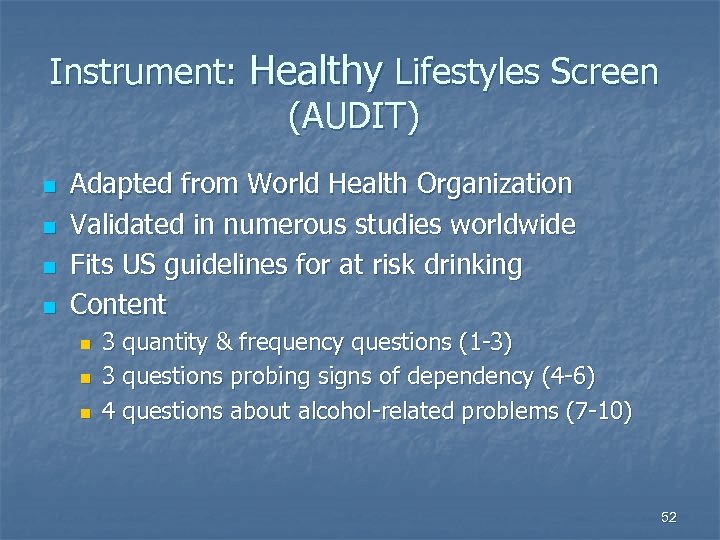
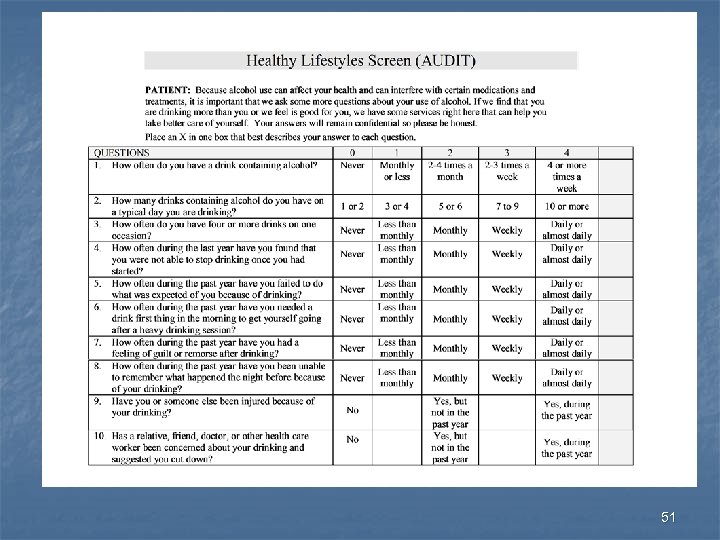
Instrument: Healthy Lifestyles Screen (AUDIT) n n Adapted from World Health Organization Validated in numerous studies worldwide Fits US guidelines for at risk drinking Content n n n 3 quantity & frequency questions (1 -3) 3 questions probing signs of dependency (4 -6) 4 questions about alcohol-related problems (7 -10) 52
Screening Procedures 1. 2. 3. 4. 5. Patient completes form Patient gives form to clinician Clinician notes items marked Clinician calculates the score Clinician obtains & documents recent alcohol & drug use 53
AUDIT Screen – Scoring n n Note numbers in top shaded row Enter checked number for each question Enter total score of 10 questions Ask the 3 questions under Provider Use Only (frequency, quantity, drugs) 54
View Video One Nursing staff Asking Healthy Habits Prescreen & Giving Healthy Lifestyles Screen (AUDIT) 55
Clinicians: Practice Scoring Healthy Lifestyles Screen (AUDIT) Nursing staff: Practice Giving Healthy Habits Prescreen & Administering AUDIT 56
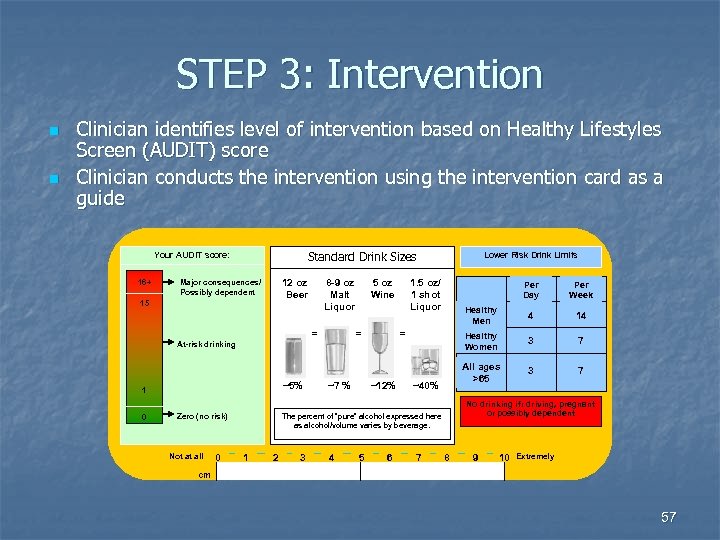
STEP 3: Intervention n n Clinician identifies level of intervention based on Healthy Lifestyles Screen (AUDIT) score Clinician conducts the intervention using the intervention card as a guide Standard Drink Sizes Lower Risk Drink Limits 12 oz 8 -9 oz 5 oz 1. 5 oz/ Beer Malt Wine 1 shot Liquor Per Day Per Week Healthy Men 4 14 Healthy Women 3 7 All ages >65 3 7 Your AUDIT score: 16+ Major consequences/ Possibly dependent 15 = At-risk drinking = ~5% ~7 % ~12% ~40% 1 0 = Zero (no risk) Not at all 0 No drinking if: driving, pregnant or possibly dependent The percent of “pure” alcohol expressed here as alcohol/volume varies by beverage. 1 2 3 4 5 6 7 8 9 10 Extremely cm 57
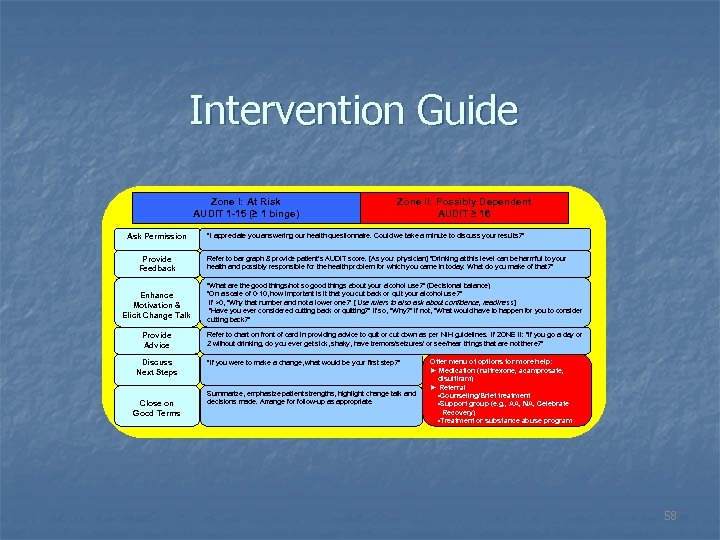
Intervention Guide Zone I: At Risk AUDIT 1 -15 (≥ 1 binge) Ask Permission Provide Feedback Zone II: Possibly Dependent AUDIT ≥ 16 “I appreciate you answering our health questionnaire. Could we take a minute to discuss your results? ” Refer to bar graph & provide patient’s AUDIT score. [As your physician] “Drinking at this level can be harmful to your health and possibly responsible for the health problem for which you came in today. What do you make of that? ” Enhance Motivation & Elicit Change Talk “What are the good things/not so good things about your alcohol use? ” (Decisional balance) “On a scale of 0 -10, how important is it that you cut back or quit your alcohol use? ” If >0, “Why that number and not a lower one? ” [ Use rulers to also ask about confidence, readiness] “Have you ever considered cutting back or quitting? ” If so, “Why? ” If not, “What would have to happen for you to consider cutting back? ” Provide Advice Refer to chart on front of card in providing advice to quit or cut down as per NIH guidelines. If ZONE II: “If you go a day or 2 without drinking, do you ever get sick, shaky, have tremors/seizures/ or see/hear things that are not there? ” Discuss Next Steps Close on Good Terms “If you were to make a change, what would be your first step? ” Summarize, emphasize patient strengths, highlight change talk and decisions made. Arrange for follow-up as appropriate. Offer menu of options for more help: ► Medication (naltrexone, acamprosate, disulfiram) ► Referral • Counseling/Brief treatment • Support group (e. g. , AA, NA, Celebrate Recovery) • Treatment or substance abuse program 58
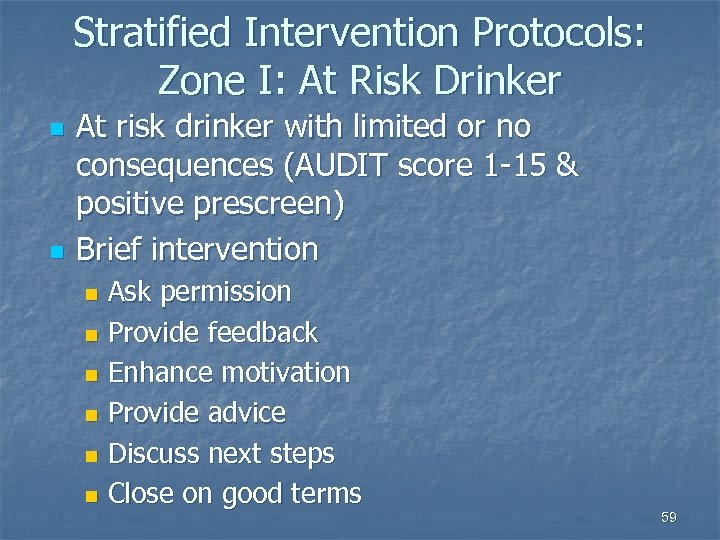
Stratified Intervention Protocols: Zone I: At Risk Drinker n n At risk drinker with limited or no consequences (AUDIT score 1 -15 & positive prescreen) Brief intervention Ask permission n Provide feedback n Enhance motivation n Provide advice n Discuss next steps n Close on good terms n 59
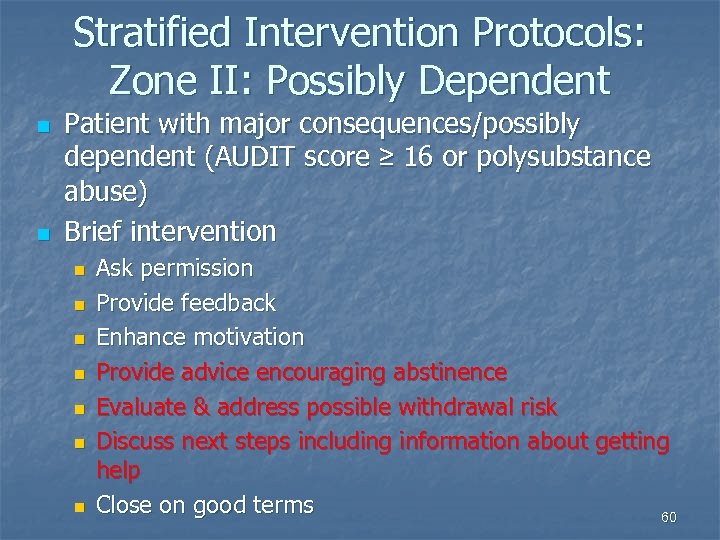
Stratified Intervention Protocols: Zone II: Possibly Dependent n n Patient with major consequences/possibly dependent (AUDIT score ≥ 16 or polysubstance abuse) Brief intervention n n n Ask permission Provide feedback Enhance motivation Provide advice encouraging abstinence Evaluate & address possible withdrawal risk Discuss next steps including information about getting help Close on good terms 60
How to Use the Intervention Guide 61
Step 1: Ask for Permission n “I appreciate your answering our health questionnaire. Could we take a minute to discuss your results? ” 62
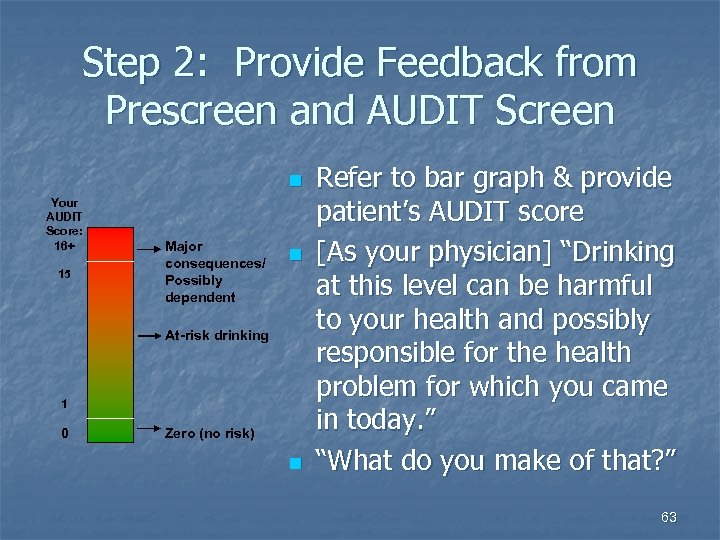
Step 2: Provide Feedback from Prescreen and AUDIT Screen n Your AUDIT Score: 16+ 15 Major consequences/ Possibly dependent n At-risk drinking 1 0 Zero (no risk) n Refer to bar graph & provide patient’s AUDIT score [As your physician] “Drinking at this level can be harmful to your health and possibly responsible for the health problem for which you came in today. ” “What do you make of that? ” 63
Step 3: Enhance Motivation: Decisional Balance n n Ask, “What are some of the good/not-so-good things about your alcohol use? ” Summarize both sides of their thinking n On the one hand… and on the other hand… 64
Step 3: Enhance Motivation: Rulers n n n “On a scale of 0 to 10, how important is it for you to cut back or quit your alcohol use? ” [Clarify whether discussing quitting or cutting back. ] If > 0, ask “Why that number and not a lower one? ” [Also ask about confidence, readiness] Explore asking “Have you ever considered cutting back (or quitting)? If so, “Why? ” If not, “What would have to happen for you to consider cutting back (or quitting)? ” 10 0 65
Step 3: Enhance Motivation: Summarize, Highlight Change Talk 10 0 n Summarize information from decisional balance and rulers highlighting change talk in particular 66
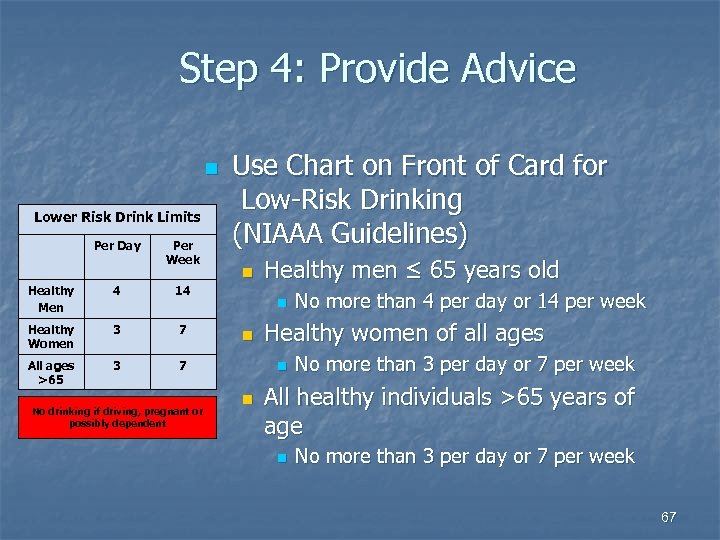
Step 4: Provide Advice n Lower Risk Drink Limits Per Day Per Week Healthy Men 4 3 7 All ages >65 3 n 14 Healthy Women Use Chart on Front of Card for Low-Risk Drinking (NIAAA Guidelines) 7 No drinking if driving, pregnant or possibly dependent Healthy men ≤ 65 years old n n Healthy women of all ages n n No more than 4 per day or 14 per week No more than 3 per day or 7 per week All healthy individuals >65 years of age n No more than 3 per day or 7 per week 67
Inform All Patients of the Risks of Drinking: n n When driving—this causes the largest proportion of alcohol-related death and disability When pregnant or considering pregnancyalcohol is the most frequent cause of preventable birth defects When contraindicated by a medical condition or medication If a history of failed attempts to cut back 68
Step 5: Discuss Next Steps n “If you were to make a change, what would be your first step? ” 69
Step 6: Close on Good Terms n n n Summarize Emphasize patient strengths Highlight change talk List decisions made regarding next steps Arrange for followup as appropriate 70
View Video Two Clinician Intervention for At-risk Drinker 71

Practice Intervention with Patient with At-Risk Drinking 72
Dealing with Time Pressure n n Do your brief intervention over multiple visits At the first visit, use 1 minute to cover the first three steps n n n Ask permission to discuss alcohol use Provide feedback on patient’s risk level Offer advice to reduce drinking at least to low risk levels Invite the patient to discuss alcohol use at a future visit Investing a few minutes now may avoid a greater problem later n n 73
Zone II: Added Steps for Those Patients with Possible Alcohol Dependence & Polysubstance Abuse n n AUDIT score of ≥ 16 indicates possible dependence on alcohol Advice is to stop Assess withdrawal risk Discuss other resources available if patient is interested 74
Intervention Steps for Possibly Dependent Patients (AUDIT ≥ 16) n Brief intervention n n n n Ask permission Provide feedback Enhance motivation Provide advice encouraging abstinence Assess & address possible withdrawal risk With permission, offer menu of other helps Discuss Next Steps Close on Good Terms 75
Withdrawal Assessment: n “Some people have the following after a day or two without drinking. Have you ever had these symptoms? ” Felt sick or shaky n Tremors n Nausea n Heart racing n Seizures n Seen or heard things that were not there n 76
Two Options for Addressing Potential Withdrawal n Arrange withdrawal treatment immediately Transfer to detox unit or treatment center n Outpatient detox where appropriate n n Tell patient what to do if these symptoms occur Present to ED/Detox Center n Call on-call physician n n Document what you do in the patient’s chart 77
Red Zone Offers Information on Getting Help n Menu of options Offer menu of options for more help: ► Medication (naltrexone, acamprosate, disulfiram, suboxone, methadone) ► Referral • Support group (e. g. , AA, NA, Celebrate Recovery) • In-house counseling (Brief treatment) • Treatment or substance abuse program Medication: (naltrexone, acamprosate, or disulfiram) n Referral n Self-help/support group (e. g. , Alcoholics Anonymous, Celebrate Recovery, etc. ) n In-house counseling (brief treatment) n Treatment or substance abuse program n 78
Referral to Treatment n Local treatment referral sources Detox n Inpatient n Outpatient n Faith-based n Long-term residential n 79
Get Help: Procedures n n Ask permission to tell the patient about resources that have helped other patients If the patient is interested, attempt to make contact with referral sources while patient is still in your office, if possible Ambivalence is common—encourage treatment providers or AA contacts to call the patient, if patient agrees Get patient’s “best phone number(s)” 80
Tips to Enhance Intervention n n Resist the urge to fix the patient at this visit—behavior change starts with “seed planting” Focus on building rapport Avoid labeling (don’t say “alcoholic”) Encourage self efficacy based on past successes “Look at successes you have had in the past” n 81
View Video Three Clinician Intervention for Patients with Major Consequences & Possible Dependence 82

Cultural Competence & SBIRT DON’Ts n n n Label Judge Assume alcohol is viewed the same in the patient’s culture as in yours Stereotype Use stigmatized language DO’s n n n Consider cultural context of drinking Work collaboratively Show empathy Build trust Elicit patient concerns about drinking 83
Practice Intervention with Patient Who is Possibly Dependent 84
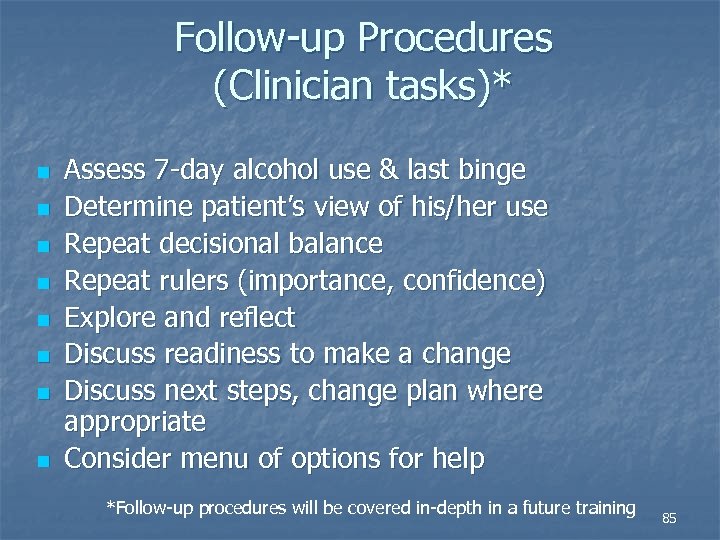
Follow-up Procedures (Clinician tasks)* n n n n Assess 7 -day alcohol use & last binge Determine patient’s view of his/her use Repeat decisional balance Repeat rulers (importance, confidence) Explore and reflect Discuss readiness to make a change Discuss next steps, change plan where appropriate Consider menu of options for help *Follow-up procedures will be covered in-depth in a future training 85
Module 1 C Establishing Office Systems 86
Objective for This Module n n n Introduce Implementation Committee & their areas of responsibility Clarify any questions regarding procedures Give information on locating SBIRT materials Summarize documentation & coding Suggest channels & procedures for feedback 87

SBIRT Committee Members n n n n n Faculty—Drs. Seale, Boltri & Mc. Laurin Residents—Drs. Ansari & Chhabria Screening & Nursing--Denise Gary, RN Brief Int. & Brief Tx--Denice Clark, MFT Referrals—Tim Prather Medical Records--Keisha Hill Administration—Leslie Scarbary, RN Suboxone—Seale, Mc. Laurin, Davis-Smith Evaluation—Dr. Johnson 88
Where to Find SBIRT Materials: All materials can be found in black notebooks in the MD stands outside clinic rooms n n n Healthy Habits Prescreen Information (salmon sheet)* Healthy Lifestyles Screens (AUDITs)* Intervention Cards Brochures Referral resource sheets *These items are also kept behind the nurses’ desk with check-in materials 89
Nursing Procedures & Documentation n When patients are put in the rooms, nurses will check for completed salmon sheets If sheet is blank, they will ask the tobacco & alcohol questions , fill in answers and give out blue & pink sheets for positive answers to tobacco or alcohol questions n If AUDIT is given, mark checkbox on physician’s office note for the day n 90
Physician Documentation Guidelines—DOCUMENT! n n Problem: Clinicians frequently fail to document alcohol-related diagnoses and interventions Results: Failure to reinforce interventions at future visits n Other providers lack important clinical information when caring for these patients n Potential medicolegal risk n 91
Documentation System: Goals n Designed to Remind provider to follow up on alcohol consumption n Alert other providers to at risk or problem drinking n Protect patients from stigma or discrimination n Respect current privacy legislation n 92
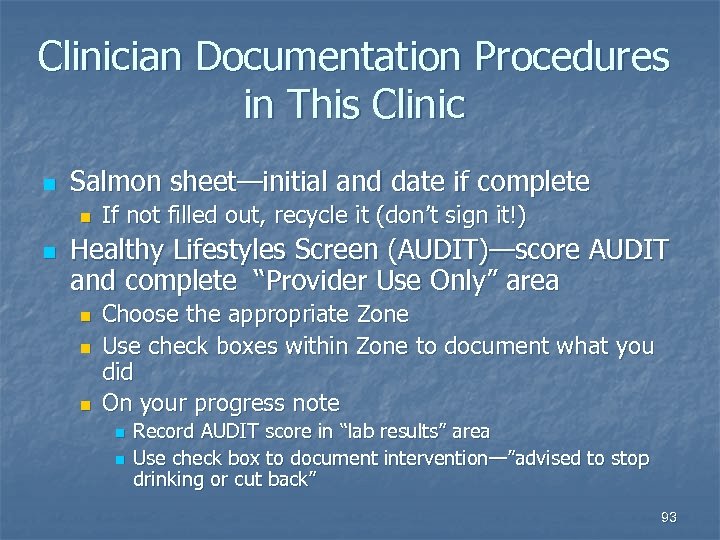
Clinician Documentation Procedures in This Clinic n Salmon sheet—initial and date if complete n n If not filled out, recycle it (don’t sign it!) Healthy Lifestyles Screen (AUDIT)—score AUDIT and complete “Provider Use Only” area n n n Choose the appropriate Zone Use check boxes within Zone to document what you did On your progress note n n Record AUDIT score in “lab results” area Use check box to document intervention—”advised to stop drinking or cut back” 93
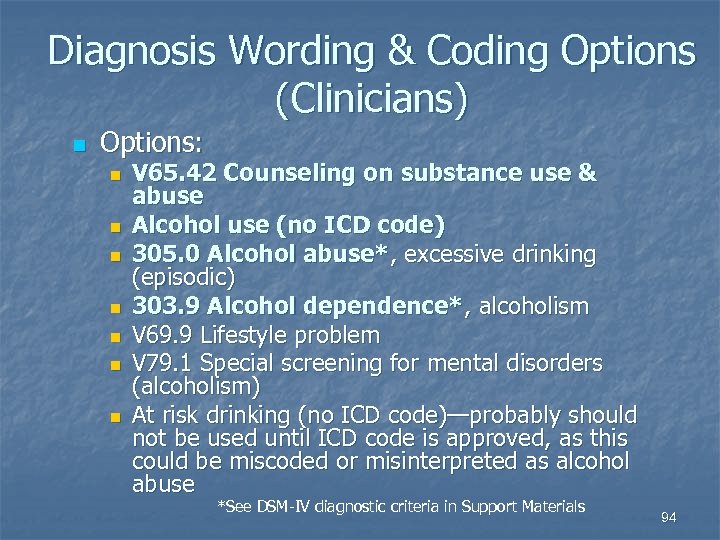
Diagnosis Wording & Coding Options (Clinicians) n Options: n n n n V 65. 42 Counseling on substance use & abuse Alcohol use (no ICD code) 305. 0 Alcohol abuse*, excessive drinking (episodic) 303. 9 Alcohol dependence*, alcoholism V 69. 9 Lifestyle problem V 79. 1 Special screening for mental disorders (alcoholism) At risk drinking (no ICD code)—probably should not be used until ICD code is approved, as this could be miscoded or misinterpreted as alcohol abuse *See DSM-IV diagnostic criteria in Support Materials 94
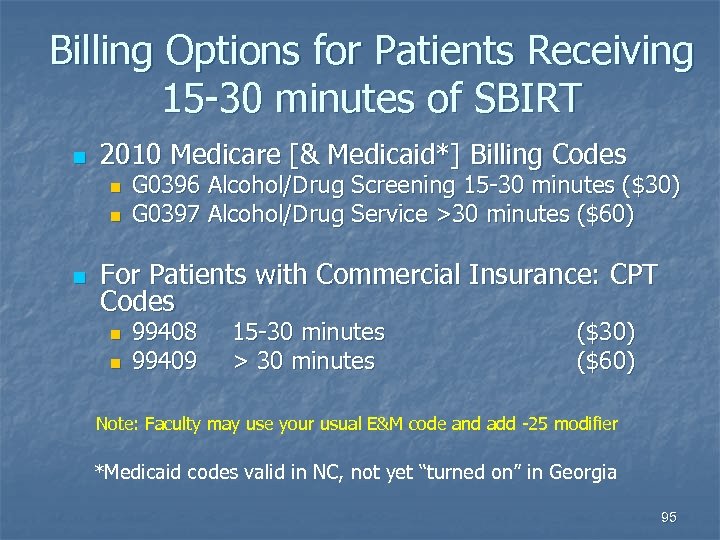
Billing Options for Patients Receiving 15 -30 minutes of SBIRT n 2010 Medicare [& Medicaid*] Billing Codes n n n G 0396 Alcohol/Drug Screening 15 -30 minutes ($30) G 0397 Alcohol/Drug Service >30 minutes ($60) For Patients with Commercial Insurance: CPT Codes n n 99408 99409 15 -30 minutes > 30 minutes ($30) ($60) Note: Faculty may use your usual E&M code and add -25 modifier *Medicaid codes valid in NC, not yet “turned on” in Georgia 95
Other Billing Options n Since most interventions involve greater time spent or greater complexity, document and code for your work n n If time and complexity criteria are met, nonresidents may code 99214 or 99215 In your private practice, have/train a non. MD to do SBIRT n n Advantage: less rushed, often will use 15 minutes or more Can then use CPT or G codes and generate $30 -$60 per BI 96
Options for Protecting Privacy & Confidentiality n n Nationally, there is no consensus or clear guideline about whether Regulation 42 CFR Part 2, which requires special confidentiality measures for mental health and substance abuse treatment, applies to SBIRT activities Each individual practice should make its own decision regarding how to manage SBIRT patient records 97
Options for Protecting Privacy & Confidentiality n n Most primary care clinicians do not use special confidentiality measures for mental health diagnoses made in the context of routine primary care office practice Some clinicians use more general terms describing behavior (“alcohol use”), not diagnoses Some place AUDITs in chart areas separate from office notes , others file them with progress notes A few practices place AUDITs in protected areas requiring special release of information 98
Privacy Protections at This Clinic n n n AUDITs are filed with progress note for the day No Special Precautions for SBIRT Documentation HIPAA precautions are considered adequate privacy protection 99
Questions re SBIRT Procedures? n Good luck! n Call us with any questions n Where to call for help: Dr Seale’s pager #1248 n Denice Clark’s extension 3 -5731 n 100
93a211b3c4b29d6e6b747d5cfd05b7fb.ppt