7343e0876f5c9369602b8b6af21d5026.ppt
- Количество слайдов: 106
San Francisco Community Clinic Consortium Behavioral Health Presentation Presented by HFS Consultants Regina Boyle January 14, 2010
Behavioral Health Training Today’s Topics • Overview of Behavioral Health Services • Federal & State Health Regulations (BH) • Legal Issues Regarding Behavioral Health • Billing & Coding Issues for Behavioral Health • Charting • State Plan Amendment • Licensing and Intermittent Clinic Issues • HRSA Change of Scope Issues • State Change of Scope Rate Request • Medicare Enrollment • Reimbursement and Allowable Expenses
Today’s Format • Four Presentations • Legal • Billing, Coding, Charting • PPS, HRSA, Licensing, Enrollment • Reimbursement • Facilitate Questions During & After Presentation • Wrap Up and Follow up Questions • Tool Kit Reference
FQHC and the Provision of Mental Health Services: Key Legal Issues Regina M. Boyle Attorney at Law 2220 Capitol Avenue, Second Floor Sacramento, California 95816 Tel: (916) 930 -0936/Fax: (916) 930 -0938 Email: cliniclaw@gmail. com
Key Legal Issues Behavioral Health Services May Be Delivered By: • Physicians – primary care or psychiatrists • Clinical Psychologists • Licensed Clinical Social Workers • Nurse Practitioners • Physicians Assistants
Key Legal Issues Medicare/Medi-Cal Qualifications for Mental Health Providers Physicians, Clinical Psychologists, Licensed Clinical Social Workers, Nurse Practitioners and Physician Assistants are providers of FQHC “core services” and are defined by Medicare law for both Medi-Cal and Medicare.

Key Legal Issues Be certain that the professional delivering the services: • Meets licensing requirements; • Meets Medicare/Medi-Cal professional training qualifications; • Is delivering services within the scope of their professional license.
Key Legal Issues Contracting with Health Care Professionals • State and federal law contain various prohibitions on self-referral and compensation of health care providers and certain others for the referral of patients (unearned compensation). • Generally, these rules are intended to limit the impact of health care provider conflicts of interest, and to reduce financial incentives which may result in the provision of medically unnecessary services to patients.
Key Legal Issues Legal Counsel’s Review • FQHC staff should be familiar with the requirements for meeting the Stark exception/Anti-Kickback Safe Harbors for employment and personal services agreements. • However, these rules are complicated, and in many respects counter-intuitive, and violations may result in ruinous civil and criminal fines and penalties, including possible mandatory exclusion from Medicare/Medicaid. • It is therefore essential that FQHCs have proposed contracts prepared or reviewed by competent legal counsel who is familiar with State and Federal Fraud and Abuse laws in order to ensure that agreements are in full compliance with state and federal referral and compensation laws.

Key Legal Issues Outpatient Mental Health Treatment Limitation • Impacts reimbursement of a specific range of services that are provided to Medicare beneficiaries – does not limit coverage of services outside this range • Phased out from 2010 – 2014 (Section 102 of the Medicare Improvements for Patients and Providers Act (MIPPA) of 2008)
Key Legal Issues Outpatient Mental Health Treatment Limitation Does Not apply to Medi-Cal, but: • FQHCs must ensure that Medi-Cal is not attributing phantom income for visits for mental health services paid at the discounted rate; • DHCS Audits and Investigation is aware of the problem; • This awareness does not mean that A&I staff will avoid making the mistake.
Key Legal Issues Mandatory Medicaid Coverage of Behavioral Health Services: Clinical psychology (CP) and Licensed Clinical Social Worker (LCSW) services must be reimbursed in an FQHC/RHC regardless of whether or not they are otherwise covered by the State Medicaid Plan.
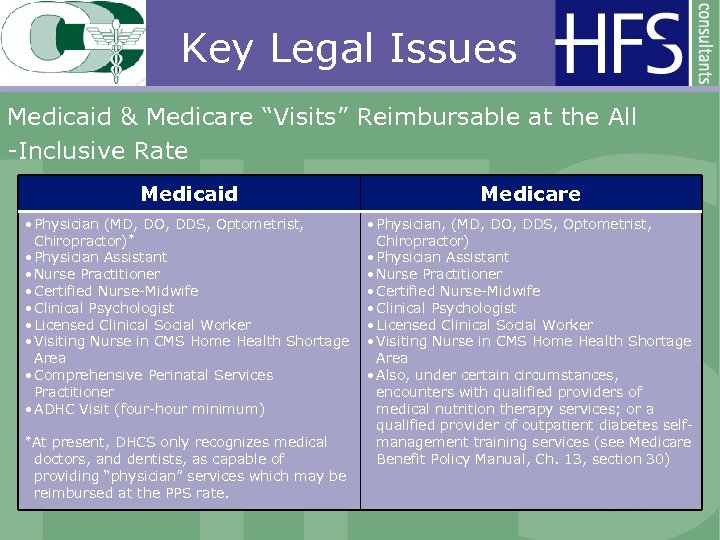
Key Legal Issues Medicaid & Medicare “Visits” Reimbursable at the All -Inclusive Rate Medicaid Medicare • Physician (MD, DO, DDS, Optometrist, Chiropractor)* • Physician Assistant • Nurse Practitioner • Certified Nurse-Midwife • Clinical Psychologist • Licensed Clinical Social Worker • Visiting Nurse in CMS Home Health Shortage Area • Comprehensive Perinatal Services Practitioner • ADHC Visit (four-hour minimum) *At present, DHCS only recognizes medical doctors, and dentists, as capable of providing “physician” services which may be reimbursed at the PPS rate. • Physician, (MD, DO, DDS, Optometrist, Chiropractor) • Physician Assistant • Nurse Practitioner • Certified Nurse-Midwife • Clinical Psychologist • Licensed Clinical Social Worker • Visiting Nurse in CMS Home Health Shortage Area • Also, under certain circumstances, encounters with qualified providers of medical nutrition therapy services; or a qualified provider of outpatient diabetes selfmanagement training services (see Medicare Benefit Policy Manual, Ch. 13, section 30)
Key Legal Issues Mandatory Medicaid Coverage of Behavioral Health Services • HRSA PIN 2004 -05 and attached letter from Dennis Smith, CMS’ Director of the Center for Medicaid & State Operations; • Clarified that so long as the services of CPs and LCSWs were within the practitioner’s scope of practice, State Medicaid Agencies were required to pay FQHCs/RHCs for their services.
Key Legal Issues California’s Elimination of Optional Psychology Benefit • Neither LCSW nor CP services are otherwise covered by Medi-Cal; • Only covered by Medi-Cal by virtue of federal law (42 U. S. C. § 1396 a(a)(10)(A), 1396 d(a)(3)(C); Calif. Welfare & Inst. Code § 14132. 100(a) and (g)).
Key Legal Issues
Key Legal Issues
Key Legal Issues HRSA Scope of Project Approval • Sites/services are not eligible for enhanced Medicare/Medi-Cal reimbursement unless they have first been added to the FQHC’s Scope of Project. • Approval is only retroactive to date complete application is received by HRSA.
Key Legal Issues HRSA Scope of Project Approval HRSA PINs/PALs: • New Scope Verification Process, PAL# 09 -11; • Policy for Special Populations-Only Grantees Requesting a Change in Scope to Add a New Target Population, PIN # 09 -05; • Specialty Services and Health Centers’ Scope of Project, PIN 09 -02; • Defining Scope of Project and Policy for Requesting Changes, PIN # 08 -01 and Technical Revision 09 -03; • FQHC Look-Alikes follow PIN # 09 -06 and Technical Revision 09 -07.
Key Legal Issues HRSA Scope of Project Approval • BPHC PIN # 2009 -02 addresses policy regarding the addition of “Specialty Services” to an FQHC’s Scope of Project; • “Specialty Services” are defined by BPHC as services that are not within the definition of “required primary health services” set out in 42 U. S. C. § 254 b(b)(1).
Key Legal Issues HRSA Scope of Project Approval • HRSA views the following as “specialty services” that are subject to the additional requirements of PIN 2009 -02: • Psychiatry services; • LCSW services; • Clinical Psychology services; • As well as any services falling within the definition of “additional health services” in 42 U. S. C. sec. 254 b(b)(2).
Key Legal Issues Medi-Cal Utilization Controls • Medi-Cal Provider Manual states that FQHCs must follow the “Medi-Service” limitations. • Refers to 22 CCR § 51304 – interpreted by DHCS as limiting beneficiaries to 2 visits in any calendar month from the following list: • Chiropractors, Acupuncturists, Psychologists, Physical Therapists, Occupational Therapists, Speech Pathologists, Audiologists Podiatrists, Practitioners of Prayer or Spiritual Healing.
Key Legal Issues Medi-Cal Utilization Controls There is NO emergency exception from the Medi-Service quantity limit – there may be a professional obligation to a patient needing services in excess of the quantity limits.
Key Legal Issues Medi-Cal Utilization Controls Adoption of NPI numbers now permits FQHCs to use Automated Eligibility Verification System (AEVS) for making Medi-Service reservations.
Key Legal Issues Medi-Cal Utilization Controls Psychiatrists subject to the utilization control in 22 Calif. Code of Regulations § 51305(d), limiting non-emergency psychiatry services to a maximum of eight visits in any 120 -day period without prior authorization.
Key Legal Issues Medi-Cal Utilization Controls • FQHCs must maintain in their records documentation in lieu of obtaining a TAR, since they are exempt from the TAR process, but not the recordkeeping requirements. • For emergency psychiatry visits, documentation must demonstrate services are “emergency services” and meet requirements of 22 CCR § 51056 that are applicable to emergency services.
Key Legal Issues Medi-Cal Utilization Controls For non-emergency psychiatry services beyond the limit of 8, the medical record must include a “total treatment plan” including the specific information required by 22 CCR sec. 51305 (d)(2).
Key Legal Issues Importance of Recordkeeping • OIG Report “Medicare Payments for 2003 Part B Mental Health Services: Medical Necessity, Documentation and Coding” (http: //www. oig. hhs. gov/oeisearch. html); • The report concluded that forty-seven percent of the mental health services allowed by Medicare in 2003 did not meet program requirements, resulting in approximately $718 million in improper payments.
Key Legal Issues Importance of Recordkeeping • Medi-Cal providers are required to keep, maintain, and have readily retrievable, such records as are necessary to fully disclose the type and extent of services provided to a Medi. Cal beneficiary. • 22 CCR section 51476 sets out the basic recordkeeping requirements, and includes additional requirements applicable to psychiatric and psychological services (patient logs, appointment books or similar documents showing the date and time allotted for appointment of each patient or group of patients, and the time actually spent with such patient).
Key Legal Issues Importance of Recordkeeping • Joint Commission Resources: “A Practical Guide to Documentation in Behavioral Health Care. ” • Accredited or not, FQHCs can benefit from adopting standards developed by either the Joint Commission or AAAHC for ambulatory settings, and specific to behavioral health services.
Key Legal Issues Facility Licensing requirements for Community Clinics Clinic policies and procedures should be updated to reflect new or expanded services; • See 22 C. C. R. §§ 75026 – 75039 in particular
Key Legal Issues Facility Licensing Requirements for Community Clinics Policy regarding reporting “unusual occurrences” should be reviewed and updated if necessary – 22 C. C. R. §§ 75030 and 75053: • Occurrences such as epidemic outbreaks, poisonings, fires, major accidents, deaths from unnatural causes or other catastrophes and unusual occurrences which threaten the welfare, safety or health of patients, personnel or visitors shall be reported by the facility within 24 hours either by telephone (and confirmed in writing) or by telegraph to the local health officer and the Department. • An incident report shall be retained on file by the facility for one year.
Key Legal Issues California Department of Health Care Services’ Four Walls Rule • The provider (physician, nurse practitioner, physician assistant, nurse- midwife, clinical psychologist, clinical social worker, and visiting nurse) has a written contract with the FQHC to provide the services; • The services are furnished only to FQHC patients at the location other than the FQHC (i. e. the FQHC is sending their staff off-site to treat the patient); • The patient must be treated at that location rather than at the FQHC for health or medical reasons; and • The services provided are of the type commonly furnished in the FQHC setting.
Key Legal Issues California Department of Health Care Services’ Four Walls Rule • Like the application of the Medi-Service limit to FQHC “core services”, the legality of the four walls rule has been repeatedly questioned. • DO NOT IGNORE THESE RULES. • If you question the rules, challenge them in court before acting contrary to CDHCS stated policy.
Key Legal Issues Contracting with Counties & CMSP Short-Doyle – FQHCs that have contracts with counties to provide behavioral health services should be certain to include language in contracts ensuring that the county is not making a claim under Medicaid for the patients that are being treated by the FQHC – avoid risk of double-payment by CMS.
Key Legal Issues Contracting with Counties & CMSP • CMSP policies on what are and are not covered services is particularly vague in the area of mental health. Key problems are: • CMSP reliance on, and confusion about, Medi. Cal rules relating to Short-Doyle; • CMSP confusion about differences between Medi -Cal FQHC and “clinic services” benefits; • FQHCs should define covered services in contact before providing services to CMSP beneficiaries.
Key Legal Issues Sliding Fee Scale Requirements • Discounts to all patients below 200% FPL; • Patients between 101 -200% FPL receive a discount; • Patients below 100% FPL receive a 100% discount, however most organizations require a nominal fee; • Nominal fee varies, but $10 seems to be the most common fee for medical services; • “Nominal fee” cannot serve as barrier to care and no patient may be turned away due to inability to pay for services; • Ryan White HIV patients are eligible for the sliding fee scale and an annual payment cap (cap is set at a % of patient’s annual income).
Key Legal Issues 340 B Discount Drug Program • California recently eliminated the Medicaid carve-out for FQHCs and other “covered entities”, impacting providers with patients utilizing costly pharmaceuticals. • The Impact was muted by the October 28, 2009, Medi-Cal Pharmacy Provider Bulletin #714 DHCS stated the following: • Covered entities do not have to dispense 340 B program drugs when a payment is made to a covered entity as part of a bundled, composite or all-inclusive rate. Reimbursement will be based on applicable rates for the services rendered (i. e. your PPS rate). • The requirement to dispense 340 B program drugs applies to the Medi-Cal FFS program and rebate-eligible County Organized Health System (COHS) plans. Reimbursement is based on the applicable contract rates with the individual plans. • A 340 B program contract pharmacy may dispense non-340 B program drugs to Medi-Cal recipients even if the beneficiary is considered a “patient” of the covered entity. The pharmacy can bill for such non-340 B program drugs under the billing requirements in W&I Code, Section 14105. 455. This applies to Medi-Cal FFS and rebate-eligible COHS plans.
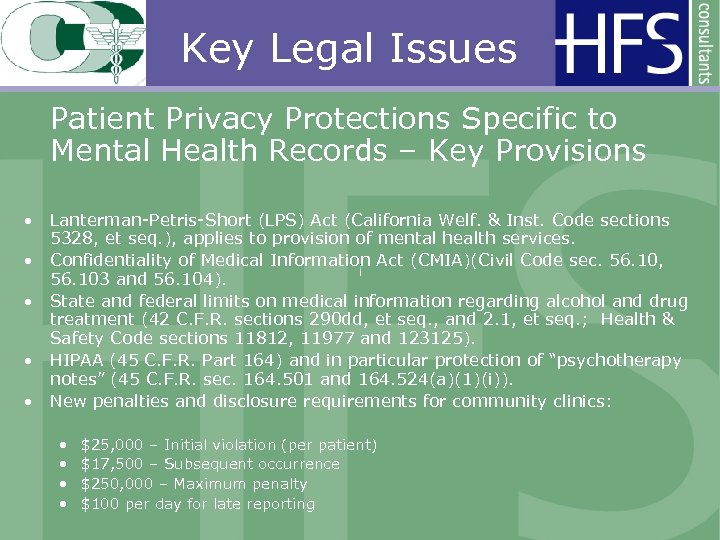
Key Legal Issues Patient Privacy Protections Specific to Mental Health Records – Key Provisions • Lanterman-Petris-Short (LPS) Act (California Welf. & Inst. Code sections 5328, et seq. ), applies to provision of mental health services. • Confidentiality of Medical Information Act (CMIA)(Civil Code sec. 56. 10, 56. 103 and 56. 104). • State and federal limits on medical information regarding alcohol and drug treatment (42 C. F. R. sections 290 dd, et seq. , and 2. 1, et seq. ; Health & Safety Code sections 11812, 11977 and 123125). • HIPAA (45 C. F. R. Part 164) and in particular protection of “psychotherapy notes” (45 C. F. R. sec. 164. 501 and 164. 524(a)(1)(i)). • New penalties and disclosure requirements for community clinics: • • $25, 000 – Initial violation (per patient) $17, 500 – Subsequent occurrence $250, 000 – Maximum penalty $100 per day for late reporting
FQHC Mental Health Documentation, Coding and Billing Carrol Hope Manager HFS Consultants
Psychological Services Psychology services are federally required core services for FQHCs and remain reimbursable for all beneficiaries when rendered by a licensed psychologist, or by a licensed clinical social worker in the FQHC.
Psychology Service Defined “Service” Defined means all care, treatment or procedures provided to a recipient by an individual practitioner on one occasion
Supporting Documentation • The documentation retained in the beneficiary’s medical record must contain legible and complete details of the psychology service visit. • To meet the requirements for both compliance and medical billing.
Medical Records Documentation
PRINCIPLES OF MEDICAL RECORD DOCUMENTATION • Medical records contain treatment history and relevant experiences pertaining to the care of the individual. • Medical records are a legal document supporting the services rendered and billed.
PRINCIPLES OF MEDICAL RECORD DOCUMENTATION • Key elements of the medical record • The reason for the patient encounter; • All services provided to the patient; • Clearly explain services, procedures, and supplies; • Clearly provide for a reasonable medical rationale for the setting ; and • Should be sufficient for another provider to take over the care of the patient. © HFS Consultants July 2007
Psychiatric Documentation Each outpatient visit must include: • Symptoms or complaints • Progress to date in objective, observable terms • Functional status • Assessment, clinical impression, or diagnosis • Plan for future care • Prognosis
HIPAA and Medical Records HIPAA laws require specific guidelines on the patient’s right to access his or her medical records. • For as long as the records are maintained • Request must be in writing (State law) • Summary may be substituted for copies Some exclusions apply-Exclusions to patient rights to access medical information • Psychotherapy notes as defined by HIPAA • Psychiatric records (state law) • Information may cause the patient to harm self or others
Coding CPT, HCPC, ICD 9
Unique Billing Method Billing Psychology services rendered in an FQHC • Federally Qualified Health Clinics (FQHC’s) use unique two digit procedure codes that have a rate per visit on their provider master file record • FQHC facilities use the following pervisit codes to bill for services rendered to Medi-Cal
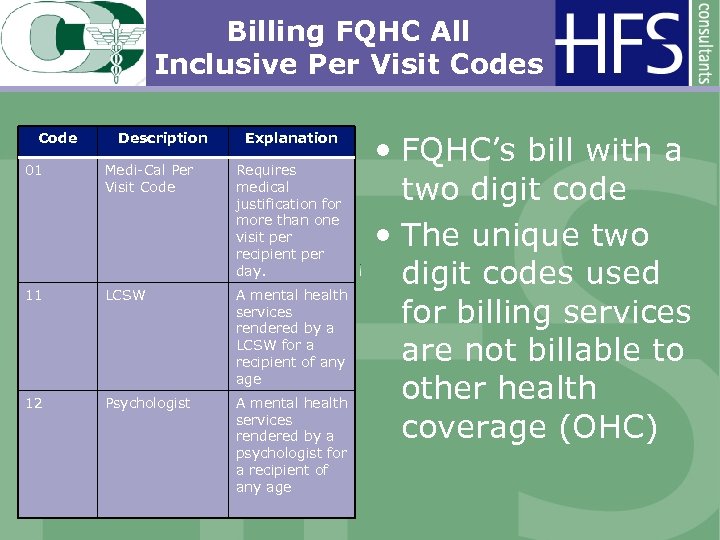
Billing FQHC All Inclusive Per Visit Codes Code Description Explanation 01 Medi-Cal Per Visit Code Requires medical justification for more than one visit per recipient per day. 11 LCSW A mental health services rendered by a LCSW for a recipient of any age 12 Psychologist A mental health services rendered by a psychologist for a recipient of any age • FQHC’s bill with a two digit code • The unique two digit codes used for billing services are not billable to other health coverage (OHC)
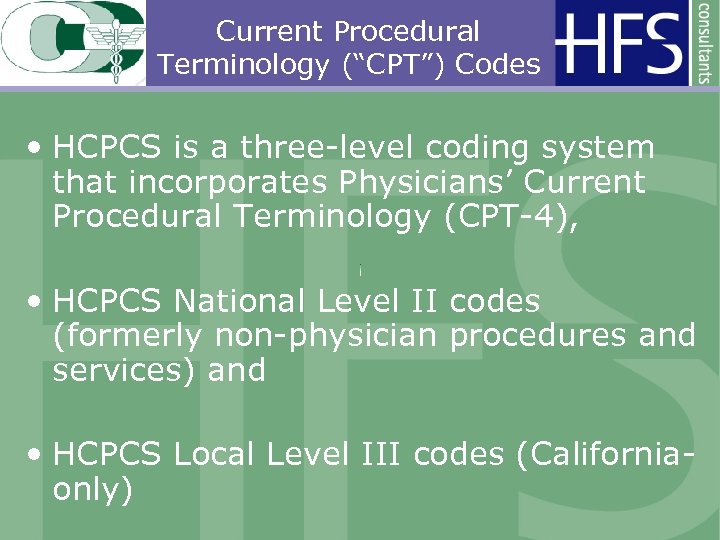
Current Procedural Terminology (“CPT”) Codes • HCPCS is a three-level coding system that incorporates Physicians’ Current Procedural Terminology (CPT-4), • HCPCS National Level II codes (formerly non-physician procedures and services) and • HCPCS Local Level III codes (Californiaonly)
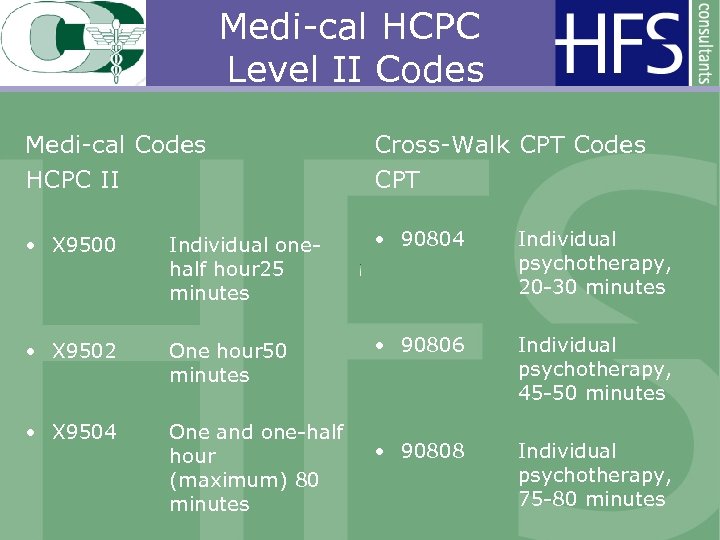
Medi-cal HCPC Level II Codes Medi-cal Codes HCPC II Cross-Walk CPT Codes CPT • X 9500 Individual onehalf hour 25 minutes • 90804 Individual psychotherapy, 20 -30 minutes • X 9502 One hour 50 minutes • 90806 Individual psychotherapy, 45 -50 minutes • X 9504 One and one-half hour (maximum) 80 minutes • 90808 Individual psychotherapy, 75 -80 minutes
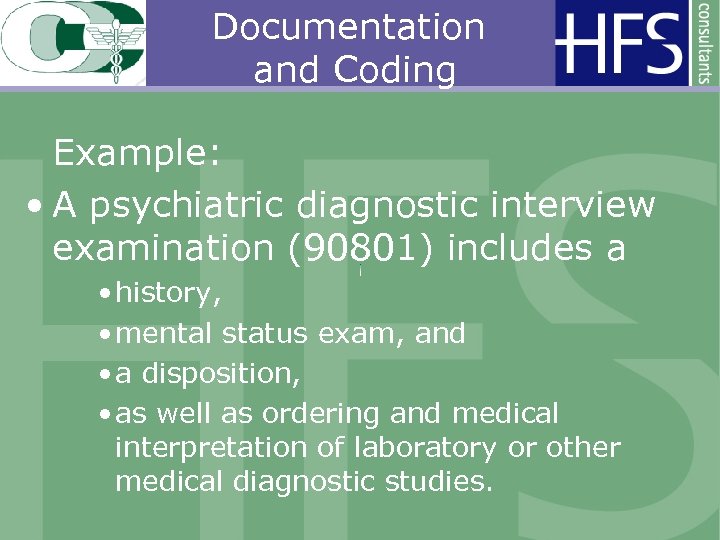
Documentation and Coding Example: • A psychiatric diagnostic interview examination (90801) includes a • history, • mental status exam, and • a disposition, • as well as ordering and medical interpretation of laboratory or other medical diagnostic studies.
Documentation and Coding Diagnostic Interview 90801 The diagnostic interview may include communication with • family or • other sources, • and in certain circumstances, other informants will be seen in lieu of the patient.
Documentation and Coding Diagnostic Interview 90801 • The psychiatrist obtains a complete medical and psychiatric history from the patient and/or family and establishes a tentative diagnosis. • Two digit FQHC code 13 Psychiatrist for FQHC billing, 1 Unit or • CPT 90801 for other health coverage • Medi-cal fee-for-service
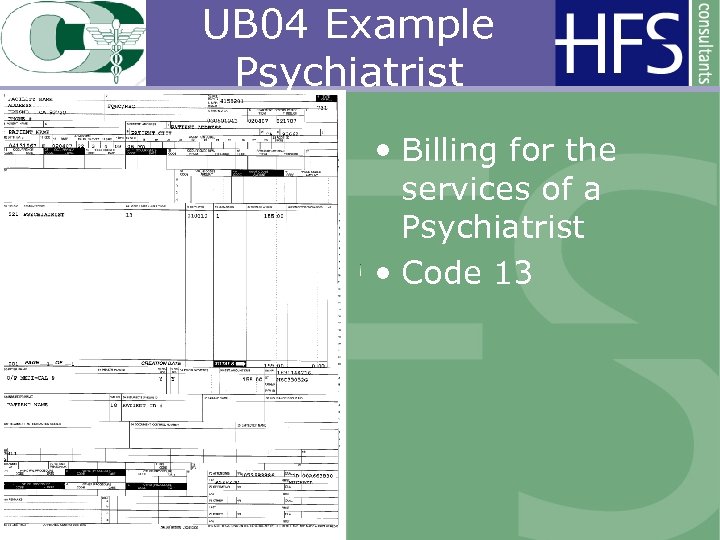
UB 04 Example Psychiatrist • Billing for the services of a Psychiatrist • Code 13
Evaluation and Management An evaluation and management (E/M) service may be substituted for the initial interview procedure, provided all required elements of the E/M service billed are fulfilled.
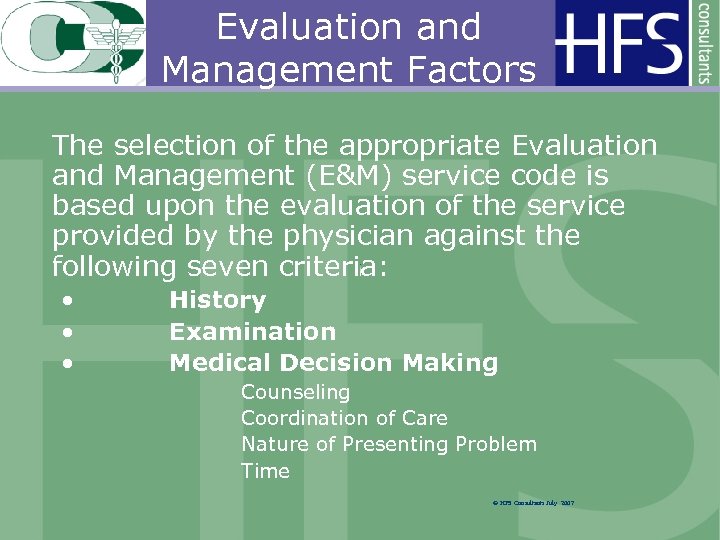
Evaluation and Management Factors The selection of the appropriate Evaluation and Management (E&M) service code is based upon the evaluation of the service provided by the physician against the following seven criteria: • • • History Examination Medical Decision Making Counseling Coordination of Care Nature of Presenting Problem Time © HFS Consultants July 2007
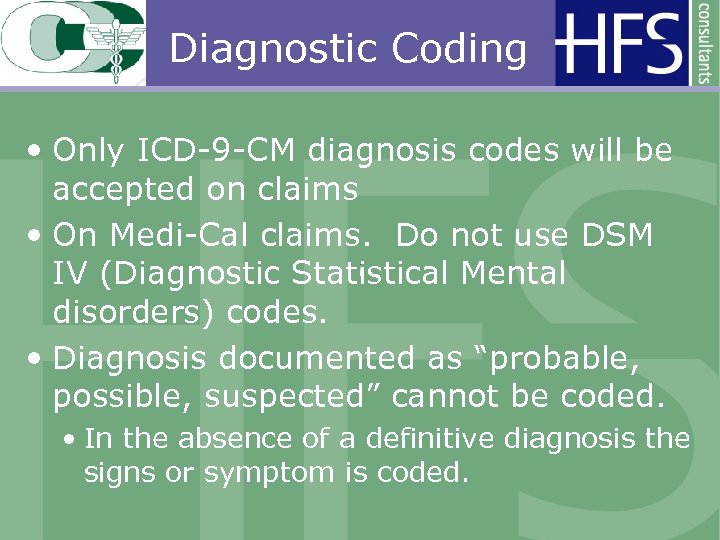
Diagnostic Coding • Only ICD-9 -CM diagnosis codes will be accepted on claims • On Medi-Cal claims. Do not use DSM IV (Diagnostic Statistical Mental disorders) codes. • Diagnosis documented as “probable, possible, suspected” cannot be coded. • In the absence of a definitive diagnosis the signs or symptom is coded.
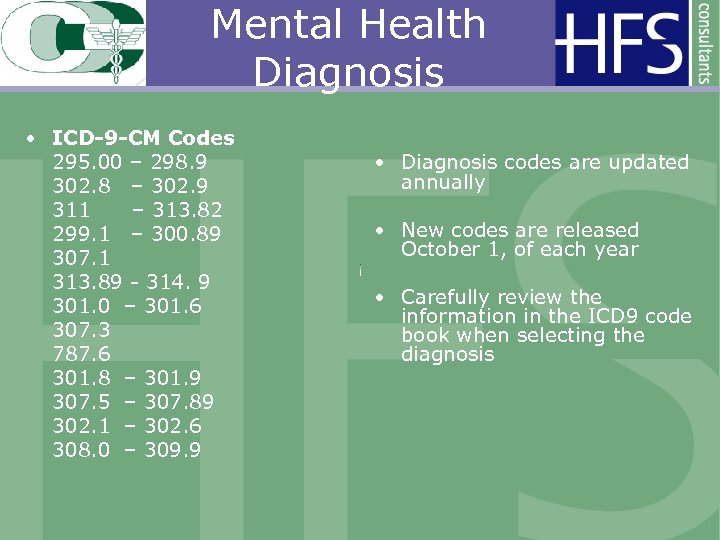
Mental Health Diagnosis • ICD-9 -CM Codes 295. 00 – 298. 9 302. 8 – 302. 9 311 – 313. 82 299. 1 – 300. 89 307. 1 313. 89 - 314. 9 301. 0 – 301. 6 307. 3 787. 6 301. 8 – 301. 9 307. 5 – 307. 89 302. 1 – 302. 6 308. 0 – 309. 9 • Diagnosis codes are updated annually • New codes are released October 1, of each year • Carefully review the information in the ICD 9 code book when selecting the diagnosis
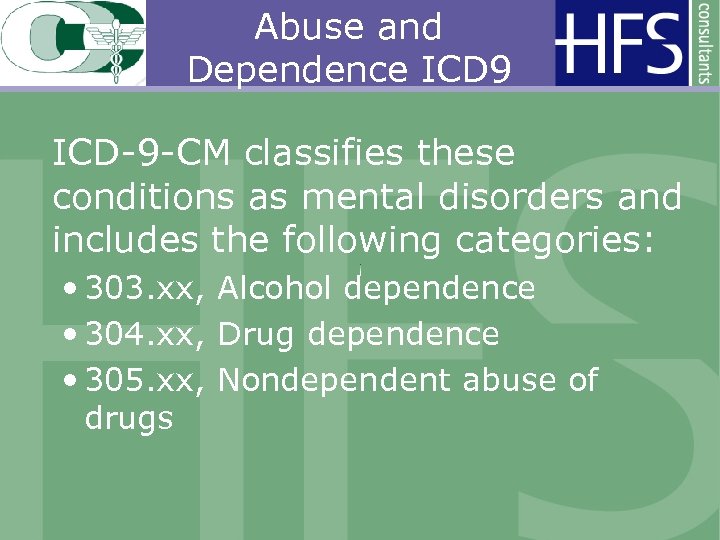
Abuse and Dependence ICD 9 ICD-9 -CM classifies these conditions as mental disorders and includes the following categories: • 303. xx, Alcohol dependence • 304. xx, Drug dependence • 305. xx, Nondependent abuse of drugs
Example ICD 9 Drug Dependence Drug dependence is classified to category 304. The fourth-digit subcategory identifies the type of drug involved as follows: • 304. 0, Opioid type dependence • 304. 1, Sedative, hypnotic, or anxiolytic dependence • 304. 2, Cocaine dependence
Overview of the Coding Process Review the: • Medical Record for codeable service • ICD-9 -CM diagnostic codes assigned to the highest degree of specificity • ICD-9 -CM diagnostic codes for validity • HCPCS/CPT codes assigned to ensure that they are correct • ICD-9 -CM codes assigned correlate © HFS Consultants July 2007
• It is important to remember that the medical record documentation must support the ICD-9 -CM and CPT codes selected. © HFS Consultants July 2007

BILLING
Billing FQHC’s bill with two digit codes • UB 04 claim forms, codes are entered into the field number 44 • Enter the two digit code that identifies the services provided in the FQHC
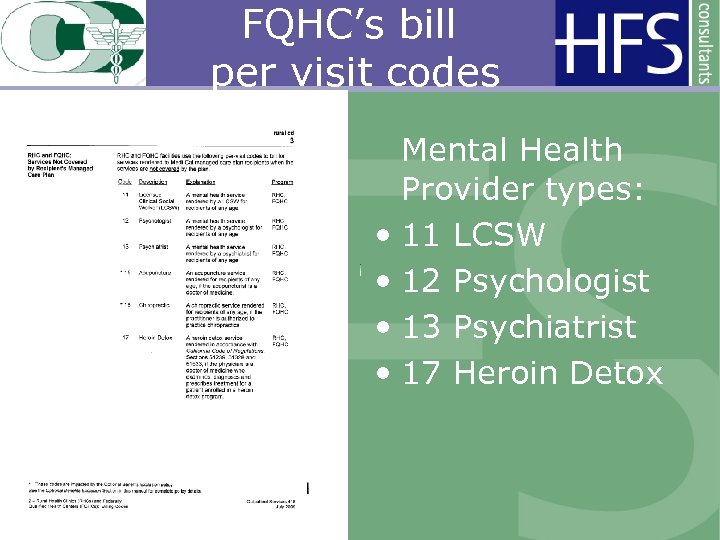
FQHC’s bill per visit codes Mental Health Provider types: • 11 LCSW • 12 Psychologist • 13 Psychiatrist • 17 Heroin Detox
UB 04 Example FQHC • Example of billing for a Clinical Psychologist • Code 12
Psychologist or LCSW • Psychology services are reimbursable for all eligible beneficiaries when rendered by a licensed psychologist or by a licensed clinical social worker in the FQHC. • Medical justification is required to be documented in the Remarks field (Box 80)/Reserved for Local Use field (Box 19) or as an attachment to the claim for psychology services for FQHCs.
Billing Example Remarks Code 80 for Psychology • The following is an example of documentation required in the remarks on the claim or as an attachment for psychology services: • Example: “The psychology service visit is provided as a core service for an FQHC. ”
• Encounters are billed in units • Encounters with more than 1 health professional and multiple encounters with same health professional which take place on same day and location are billed as 1 unit

UB 04 Example FQHC • Billing for the services of an LCSW • Code 11
FQHC Bill Types • 0521–Clinic visit by member to FQHC • 0522–Home visit by FQHC practitioner • 0524–Visit by FQHC practitioner to member in covered Part A stay at SNF
Deductible and Coinsurance • No Part B deductible is applied to FQHC services • Coinsurance is 20% of billed charges • FQHC can waive collection of all or part of coinsurance CMS IOM Publication 100 -02, Medicare Benefit Policy Manual, Chapter 13, Section 20
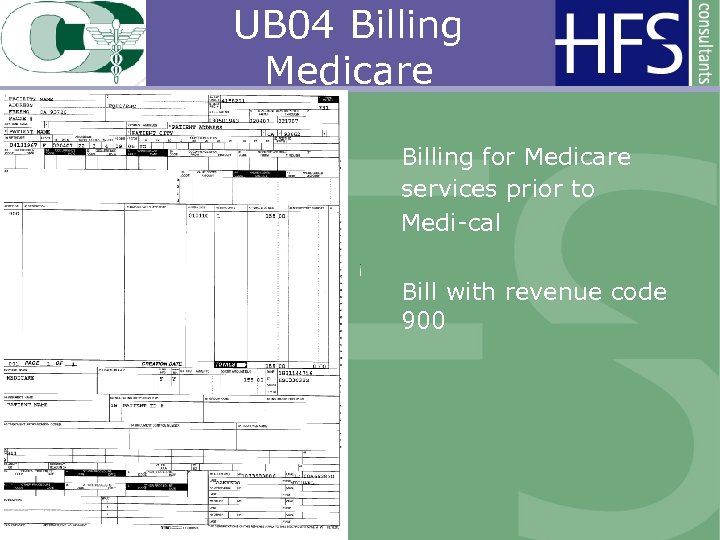
UB 04 Billing Medicare Billing for Medicare services prior to Medi-cal Bill with revenue code 900
Billing for Beneficiaries With Other Health Coverage • Providers may not refuse to provide Medi-Cal-covered services to eligible recipients with other health coverage (OHC). • Providers are required to exhaust the recipient’s OHC before billing Medi-Cal.
Example HCFA 1500 • Billing other health coverage (OHC) on HCFA 1500 • Billable provider services are not accepted on UB 04 to carriers other than Medi-cal or Medicare
Claim Billing Time Limits • Claims must be submitted to Medical within six months form the date of service. • Commercial carriers such as Blue Cross, Blue Shield for example, are billed on a HCFA 1500 claim form. • The general rule is sixty days from the date of service.
Resources Web site addresses • DHS Medical Manual http: //files. medical. ca. gov/pubsdoco/Manuals_menu. asp • CMS www. cms. hhs. gov/Manuals/IOM/list. asp/ www. cms. hhs. gov/Transmittals/ – Access transmittals – Provider updates and CMS forms
PPS, Licensing & Scope Issues PPS SPA BH Impact on PPS HRSA Scope Change Enrollment Steve Rousso Principal HFS Consultants
What is PPS? • “Prospective Payment System” • Definition: Method of reimbursement for Rural Health Clinics and Federally Qualified Health Centers (FQHC) • Does not apply to FQHCs that participate under the 1115 Medicaid Demonstration project for Los Angeles County
State Plan Amendment • “SPA” • Defines eligible visits • Defines eligible providers • Defines reimbursement system • Defines change in scope for rate requests including qualifying events • “A must read”
State Plan Amendment
State Plan Amendment
Is PPS Just a Medi-Cal Process? • It is, but there is a separate system for Medicare enrollment and Medicare rates • Upper Payment limit for urban FQHCs is: (everybody in this room) • $125. 72 per visit • What are you billing now for BH?
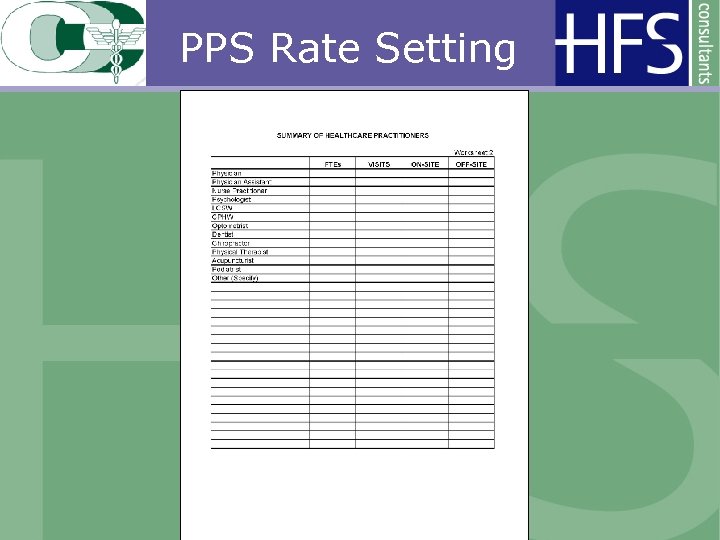
PPS Rate Setting
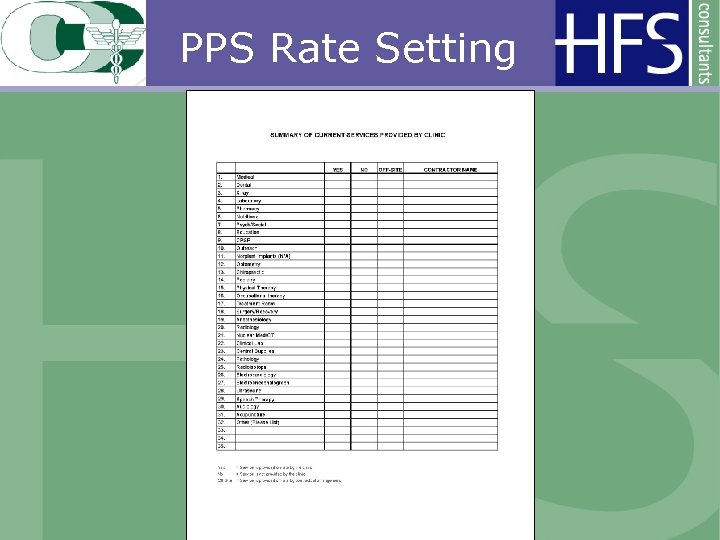
PPS Rate Setting
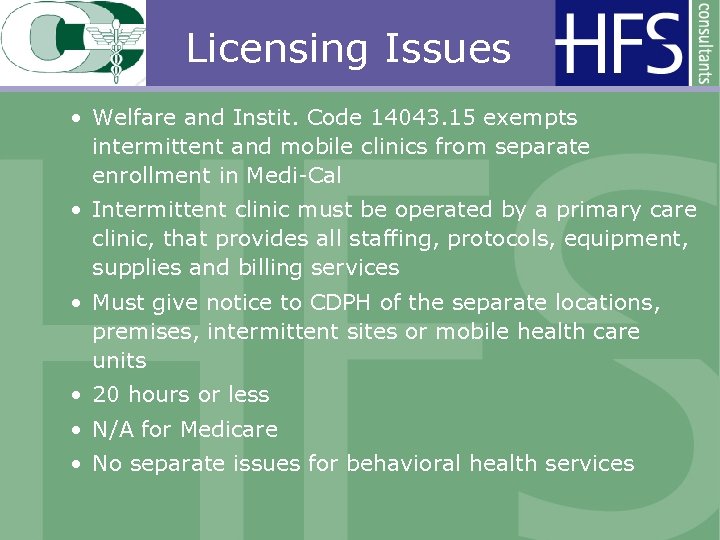
Licensing Issues • Welfare and Instit. Code 14043. 15 exempts intermittent and mobile clinics from separate enrollment in Medi-Cal • Intermittent clinic must be operated by a primary care clinic, that provides all staffing, protocols, equipment, supplies and billing services • Must give notice to CDPH of the separate locations, premises, intermittent sites or mobile health care units • 20 hours or less • N/A for Medicare • No separate issues for behavioral health services
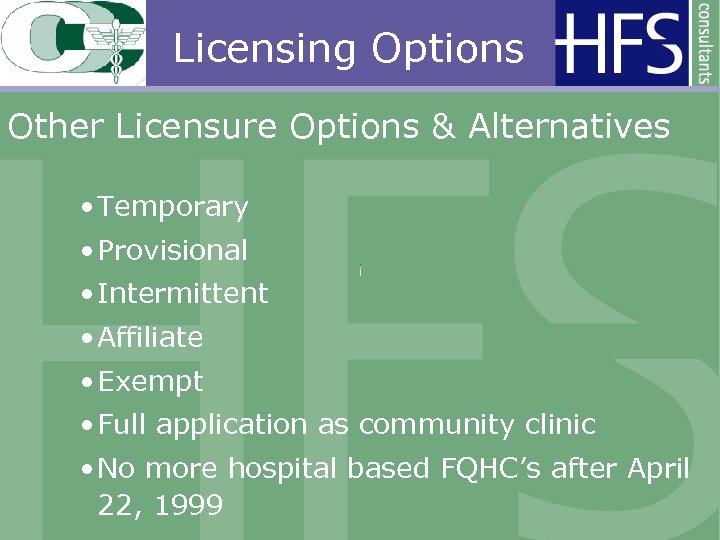
Licensing Options Other Licensure Options & Alternatives • Temporary • Provisional • Intermittent • Affiliate • Exempt • Full application as community clinic • No more hospital based FQHC’s after April 22, 1999
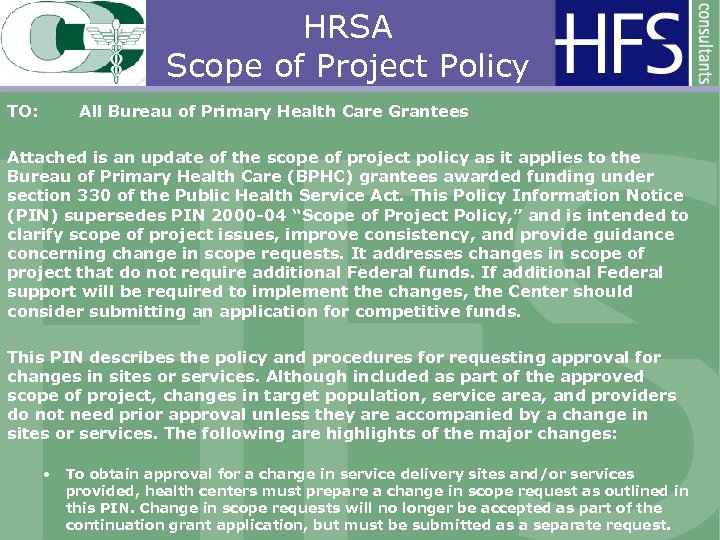
HRSA Scope of Project Policy TO: All Bureau of Primary Health Care Grantees Attached is an update of the scope of project policy as it applies to the Bureau of Primary Health Care (BPHC) grantees awarded funding under section 330 of the Public Health Service Act. This Policy Information Notice (PIN) supersedes PIN 2000 -04 “Scope of Project Policy, ” and is intended to clarify scope of project issues, improve consistency, and provide guidance concerning change in scope requests. It addresses changes in scope of project that do not require additional Federal funds. If additional Federal support will be required to implement the changes, the Center should consider submitting an application for competitive funds. This PIN describes the policy and procedures for requesting approval for changes in sites or services. Although included as part of the approved scope of project, changes in target population, service area, and providers do not need prior approval unless they are accompanied by a change in sites or services. The following are highlights of the major changes: • To obtain approval for a change in service delivery sites and/or services provided, health centers must prepare a change in scope request as outlined in this PIN. Change in scope requests will no longer be accepted as part of the continuation grant application, but must be submitted as a separate request.
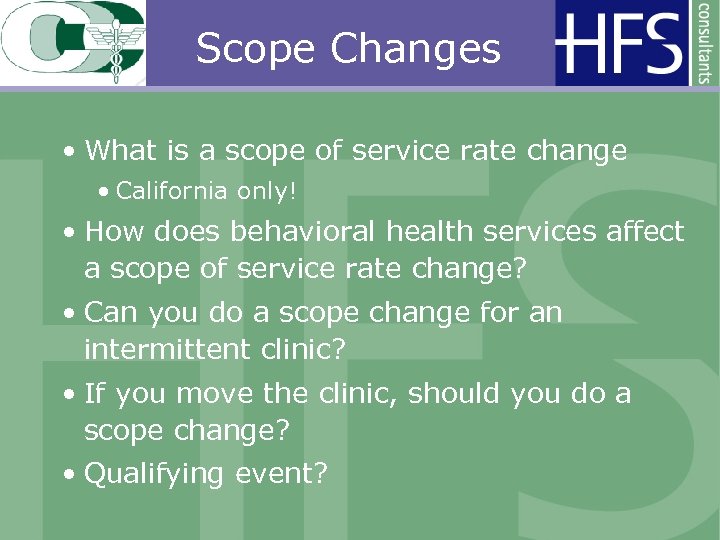
Scope Changes • What is a scope of service rate change • California only! • How does behavioral health services affect a scope of service rate change? • Can you do a scope change for an intermittent clinic? • If you move the clinic, should you do a scope change? • Qualifying event?
Scope of Services Change Instructions
Scope Changes Some Basic Rules • Need final PPS rate • Qualifying event • Our costs went up, who cares! • PPS vs. cost/visit – 1. 75% increase? • Been asked to lower PPS rate • 20% decrease in difference • 5 months after fiscal year end • Effective first day of new fiscal year
Medicare Enrollment Where to Begin? • Do you have an NPI for the site? • If not, enroll here: https: //nppes. cms. hhs. gov/NPPES/Static. Forward. do? forward=static. npistart • NPI’s should be site specific – multiple sites, get multiple numbers (easier to track payments). • NPI is primary identifier for each site and physician

Medicare Enrollment Need an application? • Go here: http: //www. cms. hhs. gov/Medicare. Provider. Sup. Enroll/0 2_Enrollment. Applications. asp#Top. Of. Page • Which application to use? • What do you need to enroll? • Provider location? (855 A) • Part B services? (855 B) • Add/link a physician to a group? (855 R, maybe 855 I)
CMS 855 I Enrollment Individual Practitioner
Questions? • PPS • SPA • Licensing • HRSA • Scope Change Rate Requests • Medicare Enrollment • Other
Reimbursement for Behavioral Health John Pfeiffer Principal HFS Consultants
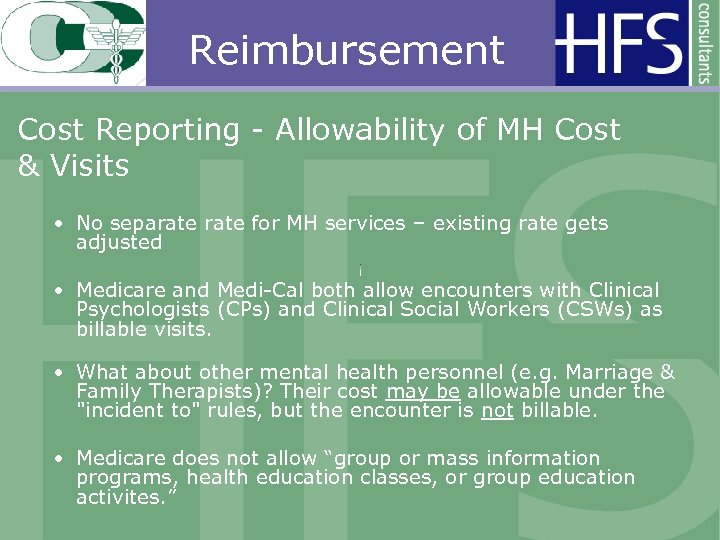
Reimbursement Cost Reporting - Allowability of MH Cost & Visits • No separate for MH services – existing rate gets adjusted • Medicare and Medi-Cal both allow encounters with Clinical Psychologists (CPs) and Clinical Social Workers (CSWs) as billable visits. • What about other mental health personnel (e. g. Marriage & Family Therapists)? Their cost may be allowable under the "incident to" rules, but the encounter is not billable. • Medicare does not allow “group or mass information programs, health education classes, or group education activites. ”
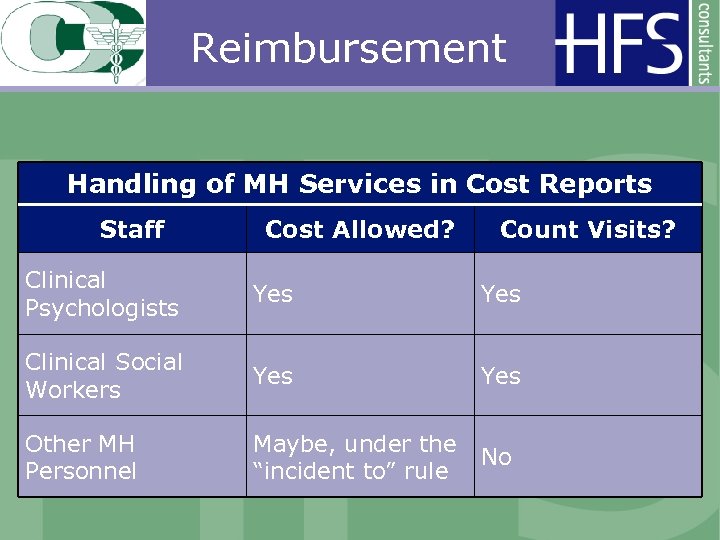
Reimbursement Handling of MH Services in Cost Reports Staff Cost Allowed? Count Visits? Clinical Psychologists Yes Clinical Social Workers Yes Other MH Personnel Maybe, under the No “incident to” rule
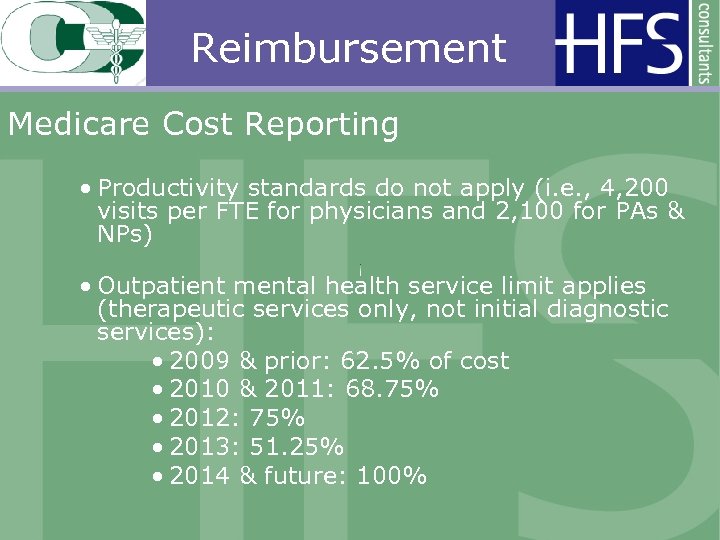
Reimbursement Medicare Cost Reporting • Productivity standards do not apply (i. e. , 4, 200 visits per FTE for physicians and 2, 100 for PAs & NPs) • Outpatient mental health service limit applies (therapeutic services only, not initial diagnostic services): • 2009 & prior: 62. 5% of cost • 2010 & 2011: 68. 75% • 2012: 75% • 2013: 51. 25% • 2014 & future: 100%
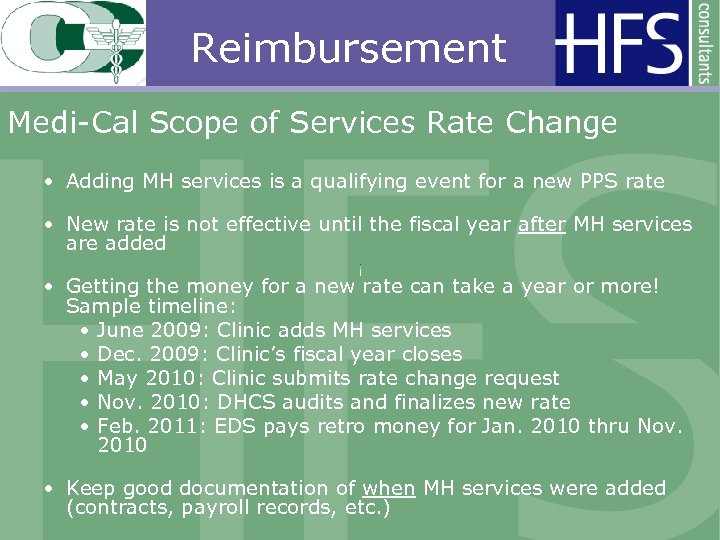
Reimbursement Medi-Cal Scope of Services Rate Change • Adding MH services is a qualifying event for a new PPS rate • New rate is not effective until the fiscal year after MH services are added • Getting the money for a new rate can take a year or more! Sample timeline: • June 2009: Clinic adds MH services • Dec. 2009: Clinic’s fiscal year closes • May 2010: Clinic submits rate change request • Nov. 2010: DHCS audits and finalizes new rate • Feb. 2011: EDS pays retro money for Jan. 2010 thru Nov. 2010 • Keep good documentation of when MH services were added (contracts, payroll records, etc. )
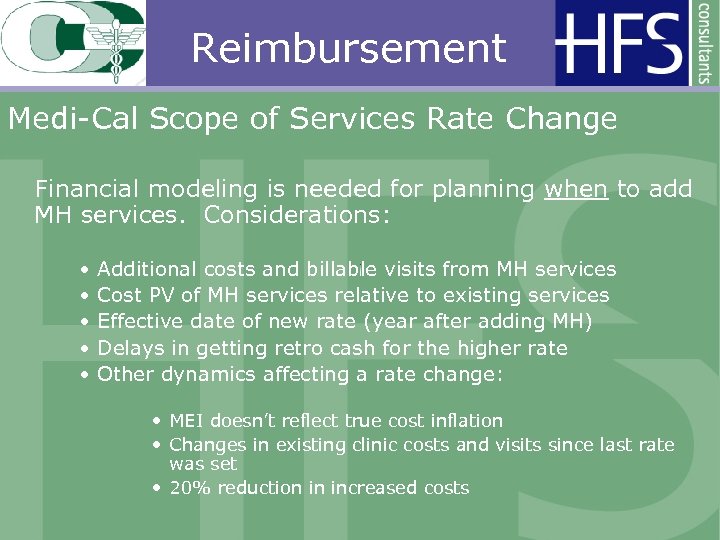
Reimbursement Medi-Cal Scope of Services Rate Change Financial modeling is needed for planning when to add MH services. Considerations: • • • Additional costs and billable visits from MH services Cost PV of MH services relative to existing services Effective date of new rate (year after adding MH) Delays in getting retro cash for the higher rate Other dynamics affecting a rate change: • MEI doesn’t reflect true cost inflation • Changes in existing clinic costs and visits since last rate was set • 20% reduction in increased costs

Reimbursement Medi-Cal Scope of Services Rate Change • If MH services have a lower cost PV than the clinic’s existing cost PV, then adding them will lower the rate. Thus, it would appear best to add services near the end of the fiscal year. BUT ON THE OTHER HAND… • If you add MH services at the beginning of the year, you will have more billable Medi-Cal visits, albeit at the existing (presumably lower) rate. SO WHICH IS BETTER: ADDING THE SERVICES EARLIER OR LATER?
Reimbursement Other Cost Reporting Issues • Medi-Cal Code 18 (Medi-Cal mgd. care) and Code 20 (Medicare Advantage) rates • Medi-Cal PPS reconciliations • Home Office Cost Reports – required by Medi-Cal • Appeals
7343e0876f5c9369602b8b6af21d5026.ppt