7809c011489590bed3243009c7eac2f4.ppt
- Количество слайдов: 19
 Safer Systems for a Safer NHS Dr. Maureen Baker CBE DM FRCGP Clinical Director for Patient Safety NHS Connecting for Health
Safer Systems for a Safer NHS Dr. Maureen Baker CBE DM FRCGP Clinical Director for Patient Safety NHS Connecting for Health
 Overview • • • The NHS The National Programme for IT (NPf. IT) Development of patient safety movement Safety management systems NHS Connecting for Health (NHS CFH) Clinical Safety Management System • Experience so far • Next steps
Overview • • • The NHS The National Programme for IT (NPf. IT) Development of patient safety movement Safety management systems NHS Connecting for Health (NHS CFH) Clinical Safety Management System • Experience so far • Next steps
 The National Programme for IT in the NHS in England • Established 2002 • Has a number of central features and programmes (National Spine; Choose and Book; GP 2 GP; National Care Record Service; Picture Archive and Communications Service; Electronic Prescription Service) • Local Service Providers • Estimated cost £ 12. 4 Billion over 10 years (contracts, training and implementation) • Being delivered by NHS Connecting for Health
The National Programme for IT in the NHS in England • Established 2002 • Has a number of central features and programmes (National Spine; Choose and Book; GP 2 GP; National Care Record Service; Picture Archive and Communications Service; Electronic Prescription Service) • Local Service Providers • Estimated cost £ 12. 4 Billion over 10 years (contracts, training and implementation) • Being delivered by NHS Connecting for Health
 Some definitions • Patient Safety - freedom from accidental harm to individuals receiving healthcare • Patient Safety Incident - an episode when something goes wrong in healthcare resulting in potential or actual harm to patients
Some definitions • Patient Safety - freedom from accidental harm to individuals receiving healthcare • Patient Safety Incident - an episode when something goes wrong in healthcare resulting in potential or actual harm to patients
 NPSA Report on Safety in NPf. IT • National Patient Safety Agency (NPSA) established 2001 • Report commissioned 2004 • Conducted by NPSA Risk Advisor
NPSA Report on Safety in NPf. IT • National Patient Safety Agency (NPSA) established 2001 • Report commissioned 2004 • Conducted by NPSA Risk Advisor
 Report Findings • Not identifying safety as a benefit to drive the programme • No formal risk assessment • No formal safety management system • Reliance on clinicians to instinctively address patient safety problems • NPf. IT not addressing safety in structured, proactive manner and other safety critical industries would
Report Findings • Not identifying safety as a benefit to drive the programme • No formal risk assessment • No formal safety management system • Reliance on clinicians to instinctively address patient safety problems • NPf. IT not addressing safety in structured, proactive manner and other safety critical industries would
 Safety Critical Industries with Safety Approach Aviation Railways Oil and Gas Construction Nuclear Military
Safety Critical Industries with Safety Approach Aviation Railways Oil and Gas Construction Nuclear Military
![NHS CFH Clinical Safety Management System [CSMS] • • Based on principles of IEC NHS CFH Clinical Safety Management System [CSMS] • • Based on principles of IEC](https://present5.com/presentation/7809c011489590bed3243009c7eac2f4/image-8.jpg) NHS CFH Clinical Safety Management System [CSMS] • • Based on principles of IEC 61508 Light touch, yet robust Three key pieces of documentation Practical and pragmatic - in place for almost 4 years • Supplemented by established Safety Incident Management Process
NHS CFH Clinical Safety Management System [CSMS] • • Based on principles of IEC 61508 Light touch, yet robust Three key pieces of documentation Practical and pragmatic - in place for almost 4 years • Supplemented by established Safety Incident Management Process
 NHS CFH CSMS Deliverables • • Hazard assessment Safety case Safety closure report Clinical Authority to Release (CATR) (Includes ‘caveats’)
NHS CFH CSMS Deliverables • • Hazard assessment Safety case Safety closure report Clinical Authority to Release (CATR) (Includes ‘caveats’)
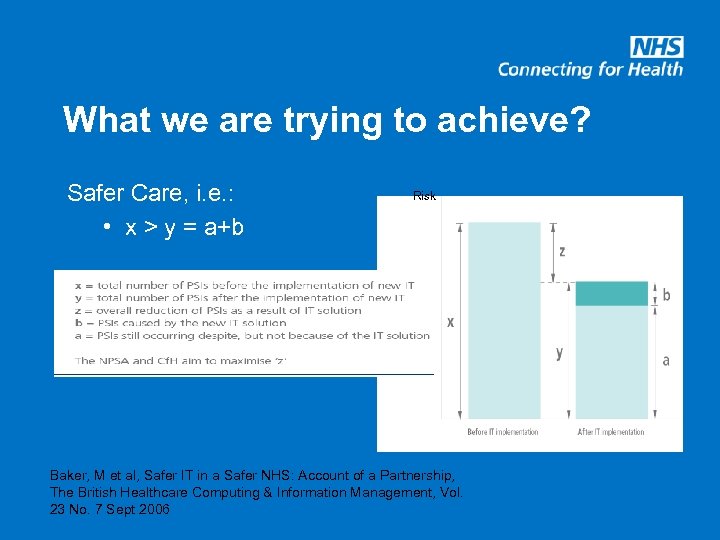 What we are trying to achieve? Safer Care, i. e. : • x > y = a+b Risk Baker, M et al, Safer IT in a Safer NHS: Account of a Partnership, The British Healthcare Computing & Information Management, Vol. 23 No. 7 Sept 2006
What we are trying to achieve? Safer Care, i. e. : • x > y = a+b Risk Baker, M et al, Safer IT in a Safer NHS: Account of a Partnership, The British Healthcare Computing & Information Management, Vol. 23 No. 7 Sept 2006
 Safety Incident Management System • Incidents related to Health IT reported and logged • Assessed and managed by Clinical Safety Group (clinicians and safety engineers) • Aim to ‘make safe’ (remove potential for harm) with 24 hours • 442 incidents reported since 2005 • 97% made safe within 24 hours
Safety Incident Management System • Incidents related to Health IT reported and logged • Assessed and managed by Clinical Safety Group (clinicians and safety engineers) • Aim to ‘make safe’ (remove potential for harm) with 24 hours • 442 incidents reported since 2005 • 97% made safe within 24 hours
 NHS IT – What can go wrong? • Patient identification (wrong notes, wrong results, wrong procedure) • Data migration (re-start discontinued drugs, incorrect preservation of meaning) • Data mapping (mapped to non-identical preparation, e. g. long-acting or slow release) • Data corruption (over-writing of info on NHS Spine)
NHS IT – What can go wrong? • Patient identification (wrong notes, wrong results, wrong procedure) • Data migration (re-start discontinued drugs, incorrect preservation of meaning) • Data mapping (mapped to non-identical preparation, e. g. long-acting or slow release) • Data corruption (over-writing of info on NHS Spine)
 Safety Workstreams in NHS CFH • Safe IT systems (as safe as design and forethought will allow) • Safety Incident Management Process • Training for accreditation and safe implementation • Technology for patient safety
Safety Workstreams in NHS CFH • Safe IT systems (as safe as design and forethought will allow) • Safety Incident Management Process • Training for accreditation and safe implementation • Technology for patient safety
 Accredited Clinician Programme • Dedicated training in principles of safety and risk as applied to Health IT • Since 2005 over 680 delegates have been trained, approx 60% are clinicians • Clinicians must be registered with appropriate regulatory body • Supports clinical input to activity by appropriately trained and qualified clinicians
Accredited Clinician Programme • Dedicated training in principles of safety and risk as applied to Health IT • Since 2005 over 680 delegates have been trained, approx 60% are clinicians • Clinicians must be registered with appropriate regulatory body • Supports clinical input to activity by appropriately trained and qualified clinicians
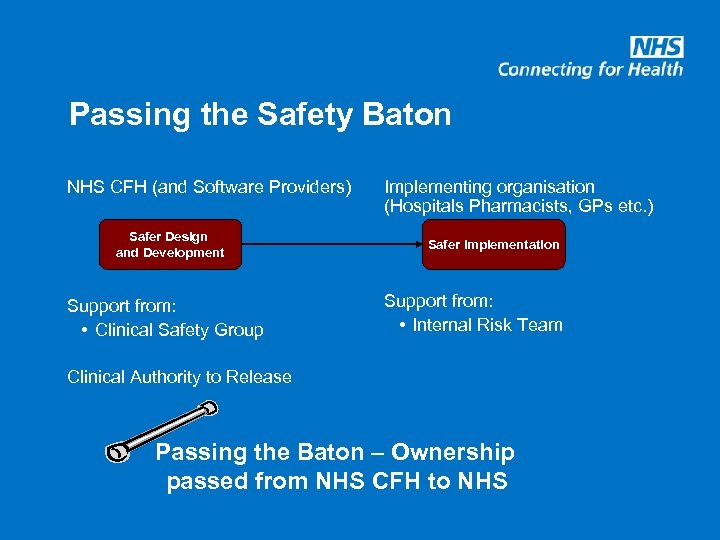 Passing the Safety Baton NHS CFH (and Software Providers) Safer Design and Development Support from: • Clinical Safety Group Implementing organisation (Hospitals Pharmacists, GPs etc. ) Safer Implementation Support from: • Internal Risk Team Clinical Authority to Release Passing the Baton – Ownership passed from NHS CFH to NHS
Passing the Safety Baton NHS CFH (and Software Providers) Safer Design and Development Support from: • Clinical Safety Group Implementing organisation (Hospitals Pharmacists, GPs etc. ) Safer Implementation Support from: • Internal Risk Team Clinical Authority to Release Passing the Baton – Ownership passed from NHS CFH to NHS
 Implementation Network • Aimed at individuals in NHS Trusts with direct responsibility for significant IT implementations • Develop a community of interest • Explicitly designed to facilitate networking and peer support • Dedicated website • Buddying • Could be used in support of ‘User Standard’
Implementation Network • Aimed at individuals in NHS Trusts with direct responsibility for significant IT implementations • Develop a community of interest • Explicitly designed to facilitate networking and peer support • Dedicated website • Buddying • Could be used in support of ‘User Standard’
 Technology for Patient Safety • Right Patient Right Care (tracking technologies – Radio Frequency Identification (RFID); wristband datasets; NHS number) • Safer prescribing (prompts + alerts, tallman) • Safer handover (core dataset) • Electronic risk assessment tool for Venous Thromboembolism (VTE) • Tracking of results • Deteriorating patients
Technology for Patient Safety • Right Patient Right Care (tracking technologies – Radio Frequency Identification (RFID); wristband datasets; NHS number) • Safer prescribing (prompts + alerts, tallman) • Safer handover (core dataset) • Electronic risk assessment tool for Venous Thromboembolism (VTE) • Tracking of results • Deteriorating patients
 Next Steps • Focus on design and human factors for inherently safe systems • Support implementation of standards (NHS and international) for suppliers and users • Passing the safety baton • Identification and safe implementation of technology for safer care
Next Steps • Focus on design and human factors for inherently safe systems • Support implementation of standards (NHS and international) for suppliers and users • Passing the safety baton • Identification and safe implementation of technology for safer care
 Conclusion • Healthcare is a safety critical industry • IT systems don’t deliver care, but are used by clinicians in the delivery of care • Good safety practice requires proactive work systems as safe as design and forethought will allow • Also reactive systems to detect and manage errors • All encompassed in CSMS and within emerging Standards
Conclusion • Healthcare is a safety critical industry • IT systems don’t deliver care, but are used by clinicians in the delivery of care • Good safety practice requires proactive work systems as safe as design and forethought will allow • Also reactive systems to detect and manage errors • All encompassed in CSMS and within emerging Standards


