6754b38da6ae411b9a8d5ed6cfa90bf1.ppt
- Количество слайдов: 45
 SAFE ANAESTHESIA PRACTICE Dr. J. Edward Johnson
SAFE ANAESTHESIA PRACTICE Dr. J. Edward Johnson
 What do you mean by that ? Safety of the Anaesthetist ? Safety of the Surgeon ? Safety of the Patient ?
What do you mean by that ? Safety of the Anaesthetist ? Safety of the Surgeon ? Safety of the Patient ?
 SAFE ANAESTHESIA PRACTICE Protocals Crisis Tips Management and Tricks for Anaesthesia
SAFE ANAESTHESIA PRACTICE Protocals Crisis Tips Management and Tricks for Anaesthesia
 PROTOCALS
PROTOCALS
 International Standards for a Safe Practice of Anaesthesia 2010 Developed by the International Task Force on Anaesthesia Safety Adopted by the World Federation of Societies of Anaesthesiologists (WFSA)
International Standards for a Safe Practice of Anaesthesia 2010 Developed by the International Task Force on Anaesthesia Safety Adopted by the World Federation of Societies of Anaesthesiologists (WFSA)
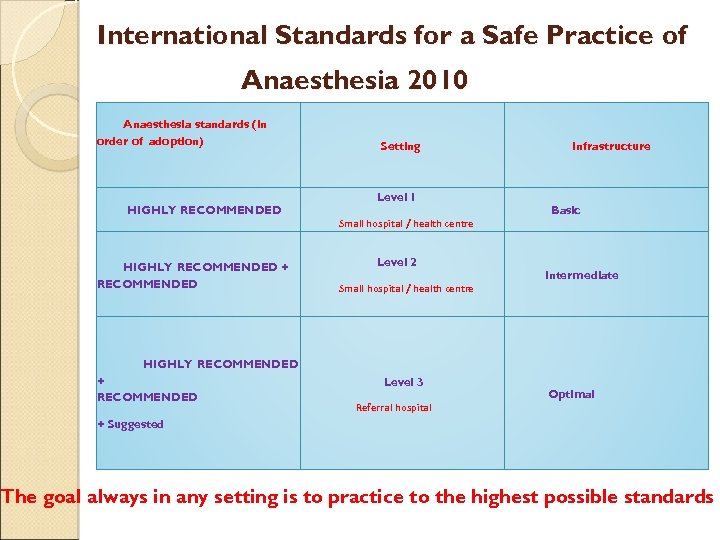 International Standards for a Safe Practice of Anaesthesia 2010 Anaesthesia standards (in order of adoption) HIGHLY RECOMMENDED + RECOMMENDED Setting Level 1 Small hospital / health centre Level 2 Small hospital / health centre Infrastructure Basic Intermediate HIGHLY RECOMMENDED + RECOMMENDED Level 3 Referral hospital Optimal + Suggested The goal always in any setting is to practice to the highest possible standards
International Standards for a Safe Practice of Anaesthesia 2010 Anaesthesia standards (in order of adoption) HIGHLY RECOMMENDED + RECOMMENDED Setting Level 1 Small hospital / health centre Level 2 Small hospital / health centre Infrastructure Basic Intermediate HIGHLY RECOMMENDED + RECOMMENDED Level 3 Referral hospital Optimal + Suggested The goal always in any setting is to practice to the highest possible standards
 "HIGHLY RECOMMENDED" Minimum standards that would be expected in all anaesthesia care for elective surgical procedures “Mandatory" standards
"HIGHLY RECOMMENDED" Minimum standards that would be expected in all anaesthesia care for elective surgical procedures “Mandatory" standards
 Peri-anaesthetic care and monitoring standards Pre-anaesthetic care Pre-anaesthesia checks Monitoring during anaesthesia
Peri-anaesthetic care and monitoring standards Pre-anaesthetic care Pre-anaesthesia checks Monitoring during anaesthesia
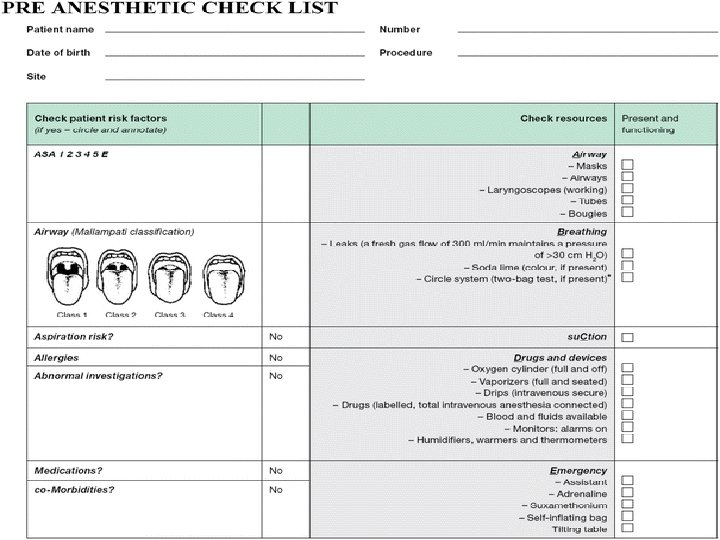
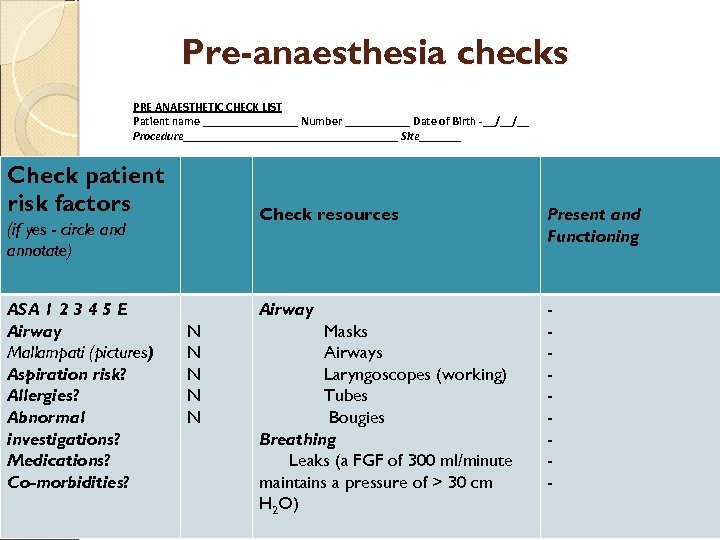 Pre-anaesthesia checks PRE ANAESTHETIC CHECK LIST Patient name ________ Number ______ Date of Birth __/__/__ Procedure__________________ Site_______ Check patient risk factors Check resources ASA 1 2 3 4 5 E Airway Mallampati (pictures) Aspiration risk? Allergies? Abnormal investigations? Medications? Co-morbidities? N N N Present and Functioning Airway (if yes - circle and annotate) - Masks Airways Laryngoscopes (working) Tubes Bougies Breathing Leaks (a FGF of 300 ml/minute maintains a pressure of > 30 cm H 2 O)
Pre-anaesthesia checks PRE ANAESTHETIC CHECK LIST Patient name ________ Number ______ Date of Birth __/__/__ Procedure__________________ Site_______ Check patient risk factors Check resources ASA 1 2 3 4 5 E Airway Mallampati (pictures) Aspiration risk? Allergies? Abnormal investigations? Medications? Co-morbidities? N N N Present and Functioning Airway (if yes - circle and annotate) - Masks Airways Laryngoscopes (working) Tubes Bougies Breathing Leaks (a FGF of 300 ml/minute maintains a pressure of > 30 cm H 2 O)
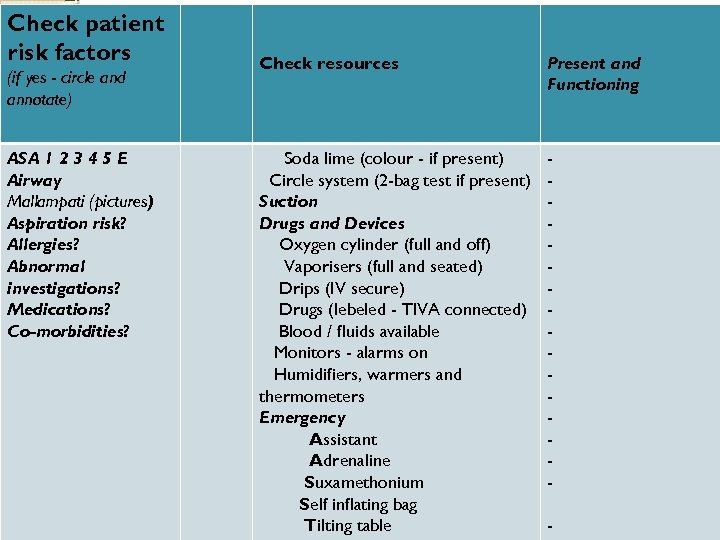 Check patient risk factors (if yes - circle and annotate) ASA 1 2 3 4 5 E Airway Mallampati (pictures) Aspiration risk? Allergies? Abnormal investigations? Medications? Co-morbidities? Check resources Present and Functioning Soda lime (colour - if present) Circle system (2 -bag test if present) Suction Drugs and Devices Oxygen cylinder (full and off) Vaporisers (full and seated) Drips (IV secure) Drugs (lebeled - TIVA connected) Blood / fluids available Monitors - alarms on Humidifiers, warmers and thermometers Emergency Assistant Adrenaline Suxamethonium Self inflating bag Tilting table -
Check patient risk factors (if yes - circle and annotate) ASA 1 2 3 4 5 E Airway Mallampati (pictures) Aspiration risk? Allergies? Abnormal investigations? Medications? Co-morbidities? Check resources Present and Functioning Soda lime (colour - if present) Circle system (2 -bag test if present) Suction Drugs and Devices Oxygen cylinder (full and off) Vaporisers (full and seated) Drips (IV secure) Drugs (lebeled - TIVA connected) Blood / fluids available Monitors - alarms on Humidifiers, warmers and thermometers Emergency Assistant Adrenaline Suxamethonium Self inflating bag Tilting table -
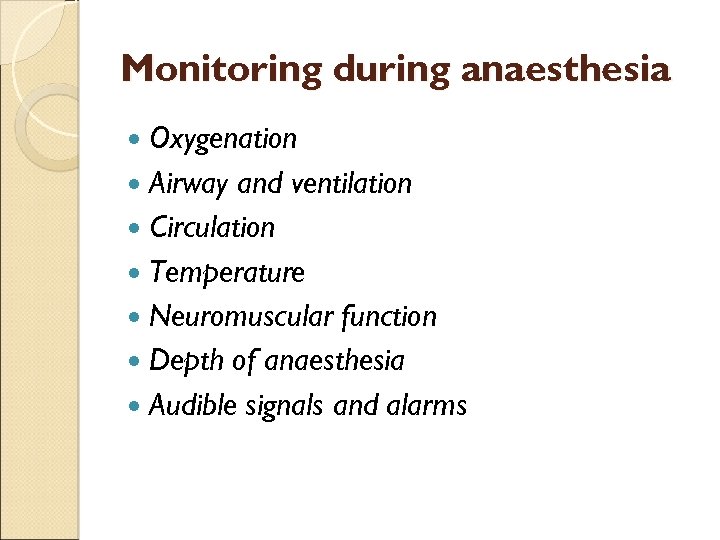 Monitoring during anaesthesia Oxygenation Airway and ventilation Circulation Temperature Neuromuscular function Depth of anaesthesia Audible signals and alarms
Monitoring during anaesthesia Oxygenation Airway and ventilation Circulation Temperature Neuromuscular function Depth of anaesthesia Audible signals and alarms
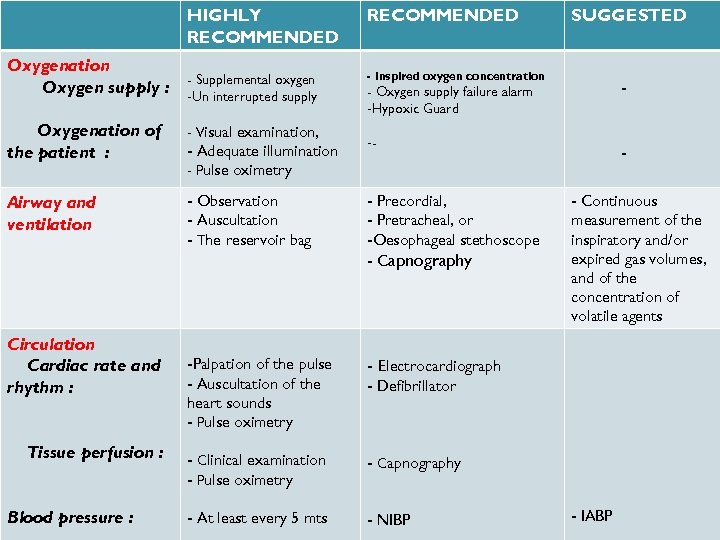 HIGHLY RECOMMENDED Oxygenation Supplemental Oxygen supply : -Un interruptedoxygen supply - Inspired oxygen concentration Oxygenation of the patient : - Visual examination, -- Airway and ventilation - Observation - Auscultation - The reservoir bag - Precordial, - Pretracheal, or -Oesophageal stethoscope - Capnography -Palpation of the pulse - Auscultation of the heart sounds - Pulse oximetry - Electrocardiograph - Clinical examination - Pulse oximetry - Capnography - At least every 5 mts - NIBP SUGGESTED Circulation Cardiac rate and rhythm : Tissue perfusion : Blood pressure : - Adequate illumination - Pulse oximetry - - Oxygen supply failure alarm -Hypoxic Guard - Continuous measurement of the inspiratory and/or expired gas volumes, and of the concentration of volatile agents - Defibrillator - IABP
HIGHLY RECOMMENDED Oxygenation Supplemental Oxygen supply : -Un interruptedoxygen supply - Inspired oxygen concentration Oxygenation of the patient : - Visual examination, -- Airway and ventilation - Observation - Auscultation - The reservoir bag - Precordial, - Pretracheal, or -Oesophageal stethoscope - Capnography -Palpation of the pulse - Auscultation of the heart sounds - Pulse oximetry - Electrocardiograph - Clinical examination - Pulse oximetry - Capnography - At least every 5 mts - NIBP SUGGESTED Circulation Cardiac rate and rhythm : Tissue perfusion : Blood pressure : - Adequate illumination - Pulse oximetry - - Oxygen supply failure alarm -Hypoxic Guard - Continuous measurement of the inspiratory and/or expired gas volumes, and of the concentration of volatile agents - Defibrillator - IABP
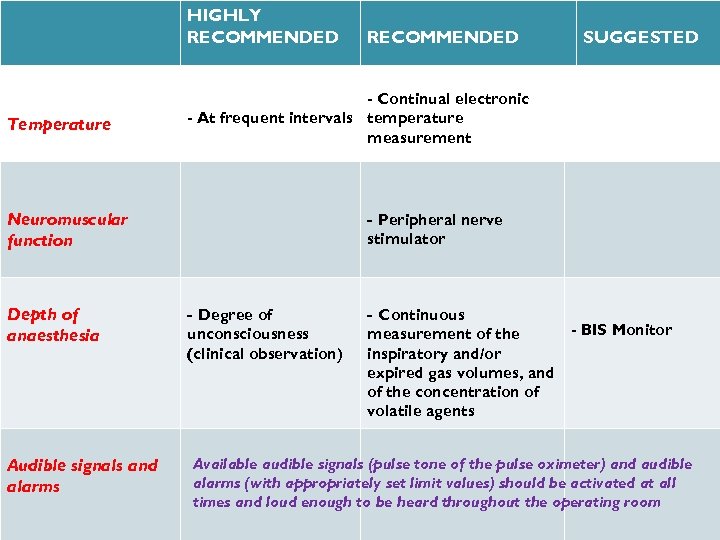 HIGHLY RECOMMENDED Temperature Audible signals and alarms SUGGESTED - Continual electronic - At frequent intervals temperature measurement Neuromuscular function Depth of anaesthesia RECOMMENDED - Peripheral nerve stimulator - Degree of - Continuous unconsciousness (clinical observation) measurement of the inspiratory and/or expired gas volumes, and of the concentration of volatile agents - BIS Monitor Available audible signals (pulse tone of the pulse oximeter) and audible alarms (with appropriately set limit values) should be activated at all times and loud enough to be heard throughout the operating room
HIGHLY RECOMMENDED Temperature Audible signals and alarms SUGGESTED - Continual electronic - At frequent intervals temperature measurement Neuromuscular function Depth of anaesthesia RECOMMENDED - Peripheral nerve stimulator - Degree of - Continuous unconsciousness (clinical observation) measurement of the inspiratory and/or expired gas volumes, and of the concentration of volatile agents - BIS Monitor Available audible signals (pulse tone of the pulse oximeter) and audible alarms (with appropriately set limit values) should be activated at all times and loud enough to be heard throughout the operating room
 Crisis Management during anaesthesia
Crisis Management during anaesthesia
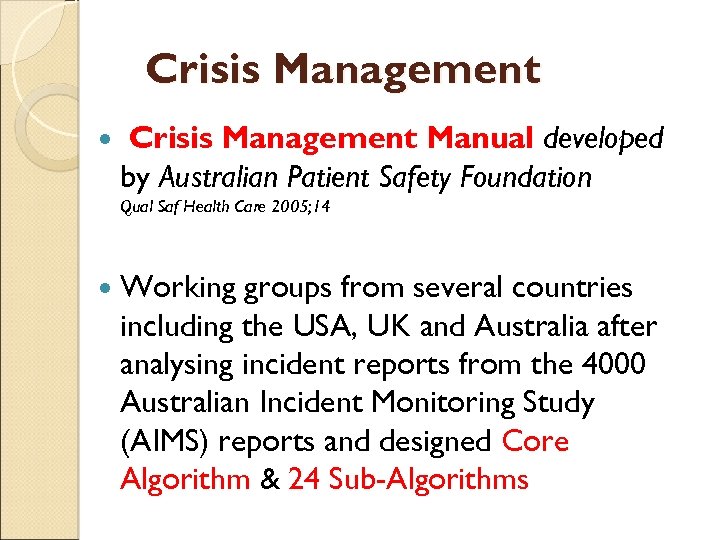 Crisis Management Manual developed by Australian Patient Safety Foundation Qual Saf Health Care 2005; 14 Working groups from several countries including the USA, UK and Australia after analysing incident reports from the 4000 Australian Incident Monitoring Study (AIMS) reports and designed Core Algorithm & 24 Sub-Algorithms
Crisis Management Manual developed by Australian Patient Safety Foundation Qual Saf Health Care 2005; 14 Working groups from several countries including the USA, UK and Australia after analysing incident reports from the 4000 Australian Incident Monitoring Study (AIMS) reports and designed Core Algorithm & 24 Sub-Algorithms
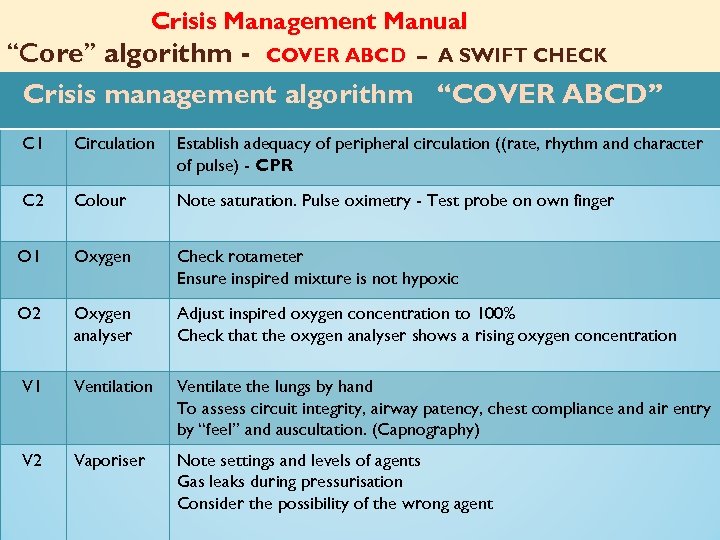 Crisis Management Manual ‘‘Core’’ algorithm - COVER ABCD – A SWIFT CHECK Crisis management algorithm ‘‘COVER ABCD’’ C 1 Circulation Establish adequacy of peripheral circulation ((rate, rhythm and character of pulse) - CPR C 2 Colour Note saturation. Pulse oximetry - Test probe on own finger O 1 Oxygen Check rotameter Ensure inspired mixture is not hypoxic O 2 Oxygen analyser Adjust inspired oxygen concentration to 100% Check that the oxygen analyser shows a rising oxygen concentration V 1 Ventilation Ventilate the lungs by hand To assess circuit integrity, airway patency, chest compliance and air entry by ‘‘feel’’ and auscultation. (Capnography) V 2 Vaporiser Note settings and levels of agents Gas leaks during pressurisation Consider the possibility of the wrong agent
Crisis Management Manual ‘‘Core’’ algorithm - COVER ABCD – A SWIFT CHECK Crisis management algorithm ‘‘COVER ABCD’’ C 1 Circulation Establish adequacy of peripheral circulation ((rate, rhythm and character of pulse) - CPR C 2 Colour Note saturation. Pulse oximetry - Test probe on own finger O 1 Oxygen Check rotameter Ensure inspired mixture is not hypoxic O 2 Oxygen analyser Adjust inspired oxygen concentration to 100% Check that the oxygen analyser shows a rising oxygen concentration V 1 Ventilation Ventilate the lungs by hand To assess circuit integrity, airway patency, chest compliance and air entry by ‘‘feel’’ and auscultation. (Capnography) V 2 Vaporiser Note settings and levels of agents Gas leaks during pressurisation Consider the possibility of the wrong agent
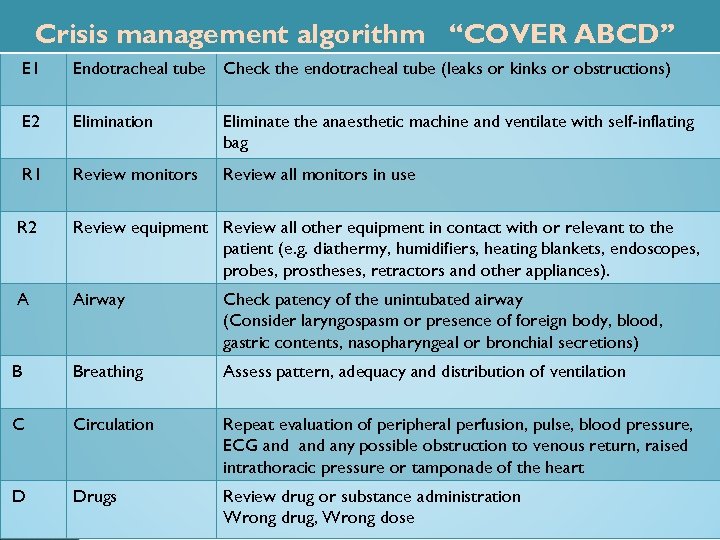 Crisis management algorithm ‘‘COVER ABCD’’ E 1 Endotracheal tube Check the endotracheal tube (leaks or kinks or obstructions) E 2 Elimination Eliminate the anaesthetic machine and ventilate with self-inflating bag R 1 Review monitors Review all monitors in use R 2 Review equipment Review all other equipment in contact with or relevant to the patient (e. g. diathermy, humidifiers, heating blankets, endoscopes, probes, prostheses, retractors and other appliances). A Airway Check patency of the unintubated airway (Consider laryngospasm or presence of foreign body, blood, gastric contents, nasopharyngeal or bronchial secretions) B Breathing Assess pattern, adequacy and distribution of ventilation C Circulation Repeat evaluation of peripheral perfusion, pulse, blood pressure, ECG and any possible obstruction to venous return, raised intrathoracic pressure or tamponade of the heart D Drugs Review drug or substance administration Wrong drug, Wrong dose
Crisis management algorithm ‘‘COVER ABCD’’ E 1 Endotracheal tube Check the endotracheal tube (leaks or kinks or obstructions) E 2 Elimination Eliminate the anaesthetic machine and ventilate with self-inflating bag R 1 Review monitors Review all monitors in use R 2 Review equipment Review all other equipment in contact with or relevant to the patient (e. g. diathermy, humidifiers, heating blankets, endoscopes, probes, prostheses, retractors and other appliances). A Airway Check patency of the unintubated airway (Consider laryngospasm or presence of foreign body, blood, gastric contents, nasopharyngeal or bronchial secretions) B Breathing Assess pattern, adequacy and distribution of ventilation C Circulation Repeat evaluation of peripheral perfusion, pulse, blood pressure, ECG and any possible obstruction to venous return, raised intrathoracic pressure or tamponade of the heart D Drugs Review drug or substance administration Wrong drug, Wrong dose
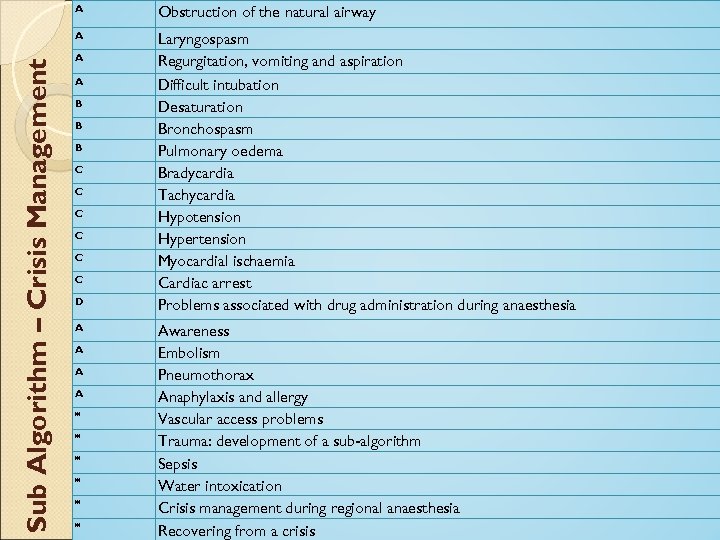 Obstruction of the natural airway A Sub Algorithm – Crisis Management A Laryngospasm Regurgitation, vomiting and aspiration Difficult intubation Desaturation Bronchospasm Pulmonary oedema Bradycardia Tachycardia Hypotension Hypertension Myocardial ischaemia Cardiac arrest Problems associated with drug administration during anaesthesia A A B B B C C C D A A * * * Awareness Embolism Pneumothorax Anaphylaxis and allergy Vascular access problems Trauma: development of a sub-algorithm Sepsis Water intoxication Crisis management during regional anaesthesia Recovering from a crisis
Obstruction of the natural airway A Sub Algorithm – Crisis Management A Laryngospasm Regurgitation, vomiting and aspiration Difficult intubation Desaturation Bronchospasm Pulmonary oedema Bradycardia Tachycardia Hypotension Hypertension Myocardial ischaemia Cardiac arrest Problems associated with drug administration during anaesthesia A A B B B C C C D A A * * * Awareness Embolism Pneumothorax Anaphylaxis and allergy Vascular access problems Trauma: development of a sub-algorithm Sepsis Water intoxication Crisis management during regional anaesthesia Recovering from a crisis
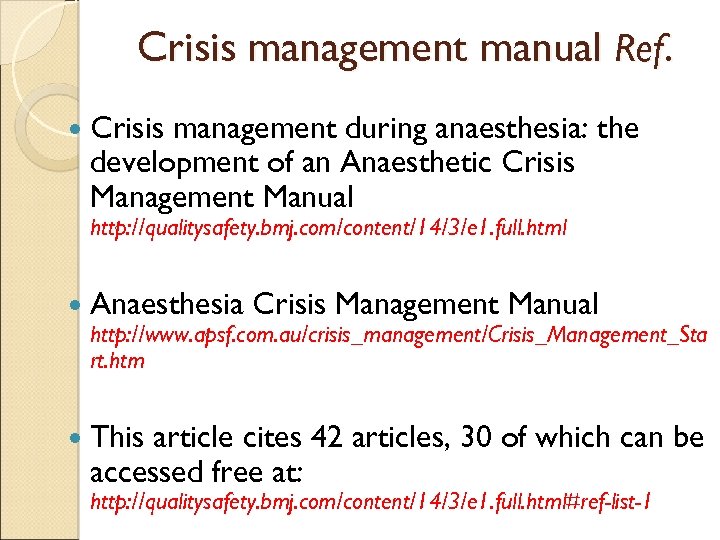 Crisis management manual Ref. Crisis management during anaesthesia: the development of an Anaesthetic Crisis Management Manual http: //qualitysafety. bmj. com/content/14/3/e 1. full. html Anaesthesia Crisis Management Manual This article cites 42 articles, 30 of which can be accessed free at: http: //www. apsf. com. au/crisis_management/Crisis_Management_Sta rt. htm http: //qualitysafety. bmj. com/content/14/3/e 1. full. html#ref-list-1
Crisis management manual Ref. Crisis management during anaesthesia: the development of an Anaesthetic Crisis Management Manual http: //qualitysafety. bmj. com/content/14/3/e 1. full. html Anaesthesia Crisis Management Manual This article cites 42 articles, 30 of which can be accessed free at: http: //www. apsf. com. au/crisis_management/Crisis_Management_Sta rt. htm http: //qualitysafety. bmj. com/content/14/3/e 1. full. html#ref-list-1
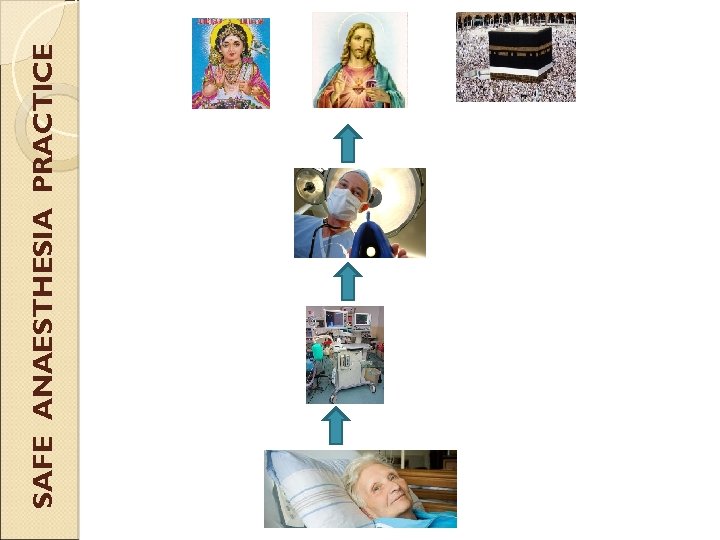
 Where Safety Starts ? Patient Facilities, Equipment, and Medications Surgeon’s Skill Anaesthetist’s Skill
Where Safety Starts ? Patient Facilities, Equipment, and Medications Surgeon’s Skill Anaesthetist’s Skill
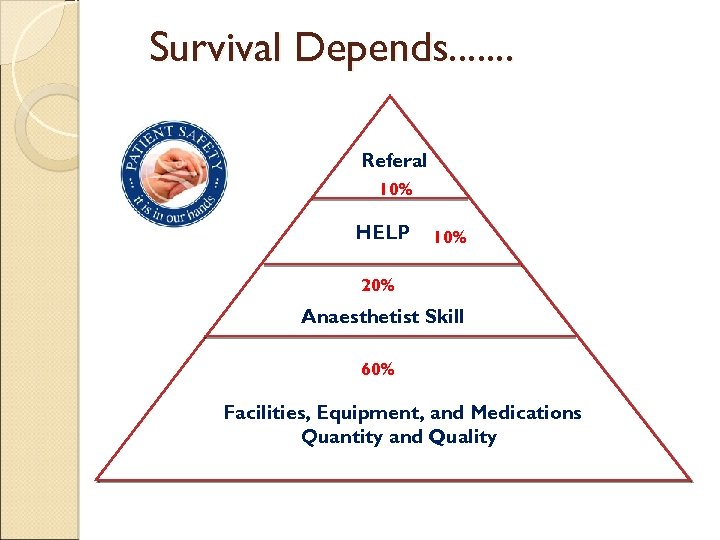 Survival Depends. . . . Referal 10% HELP 10% 20% Anaesthetist Skill 60% Facilities, Equipment, and Medications Quantity and Quality
Survival Depends. . . . Referal 10% HELP 10% 20% Anaesthetist Skill 60% Facilities, Equipment, and Medications Quantity and Quality
 Where Safety Starts ? Patient - Optimized patient (CVS, Renal, Liver) ASA risk Well controlled Hypertension Well controlled Diabetes Haemodynamically stabilsed
Where Safety Starts ? Patient - Optimized patient (CVS, Renal, Liver) ASA risk Well controlled Hypertension Well controlled Diabetes Haemodynamically stabilsed
 Medication All drugs should be clearly labelled The label on both ampoule and syringe should be read carefully before the drug is drawn up or injected Ideally drugs should be drawn up and labelled by the anaesthetist who administers them.
Medication All drugs should be clearly labelled The label on both ampoule and syringe should be read carefully before the drug is drawn up or injected Ideally drugs should be drawn up and labelled by the anaesthetist who administers them.
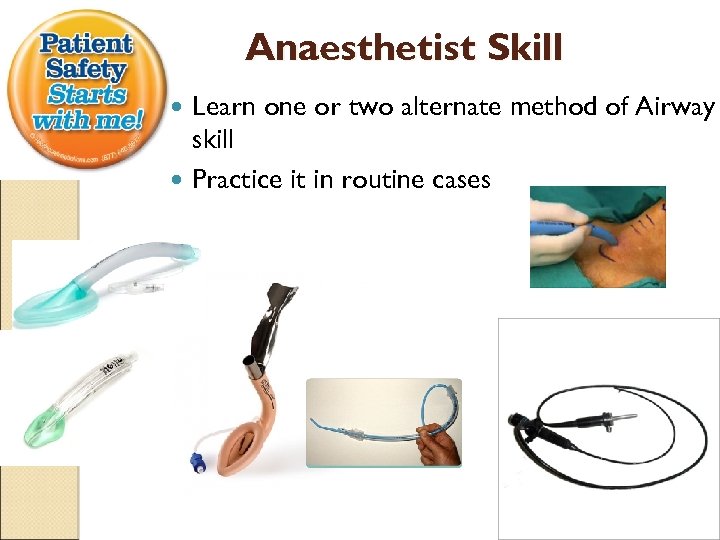 Anaesthetist Skill Learn one or two alternate method of Airway skill Practice it in routine cases
Anaesthetist Skill Learn one or two alternate method of Airway skill Practice it in routine cases
 Post Crisis
Post Crisis
 Counseling Pre operative counseling - Possible complication - Remote complication • Post operative counseling - The Swiss Foundation for Patient Safety has published guidelines describing the actions to take after an adverse event has occurred.
Counseling Pre operative counseling - Possible complication - Remote complication • Post operative counseling - The Swiss Foundation for Patient Safety has published guidelines describing the actions to take after an adverse event has occurred.
 Recommendations for senior staff members A severe medical error is an emergency Confidence between the senior staff and the involved professional Involved professionals need a professional and objective discussion with, as well as emotional support from, peers in their department Seniors should offer support for the disclosing conversation with the patient and/or the relatives A professional work-up of that case based on facts is important for analysis and learning out of medical error. Ex. .
Recommendations for senior staff members A severe medical error is an emergency Confidence between the senior staff and the involved professional Involved professionals need a professional and objective discussion with, as well as emotional support from, peers in their department Seniors should offer support for the disclosing conversation with the patient and/or the relatives A professional work-up of that case based on facts is important for analysis and learning out of medical error. Ex. .
 Recommendations for colleagues Be aware that such an adverse event could happen to you also Offer time to discuss the case with your colleague. Listen to what your colleague wants to tell and support him/her with your professional expertise Address any culture of blame either directly from within the team or by any other colleagues
Recommendations for colleagues Be aware that such an adverse event could happen to you also Offer time to discuss the case with your colleague. Listen to what your colleague wants to tell and support him/her with your professional expertise Address any culture of blame either directly from within the team or by any other colleagues
 Recommendations for healthcare professionals directly involved in an adverse event Do not suppress any feelings of emotion you may encounter after your involvement in a medical error Talk through what has happened with a dependable colleague or senior member of staff. This is not weakness. This represents appropriate professional behaviour Take part in a formal debriefing session. Try to draw conclusions and learn from this event. Ex. . If possible talk to your patient/their relatives and engage with them in open disclosure conversations If you experience any uncertainties regarding the management of future cases seek support from colleagues or seniors
Recommendations for healthcare professionals directly involved in an adverse event Do not suppress any feelings of emotion you may encounter after your involvement in a medical error Talk through what has happened with a dependable colleague or senior member of staff. This is not weakness. This represents appropriate professional behaviour Take part in a formal debriefing session. Try to draw conclusions and learn from this event. Ex. . If possible talk to your patient/their relatives and engage with them in open disclosure conversations If you experience any uncertainties regarding the management of future cases seek support from colleagues or seniors
 Tips and Tricks for Anaesthesia
Tips and Tricks for Anaesthesia
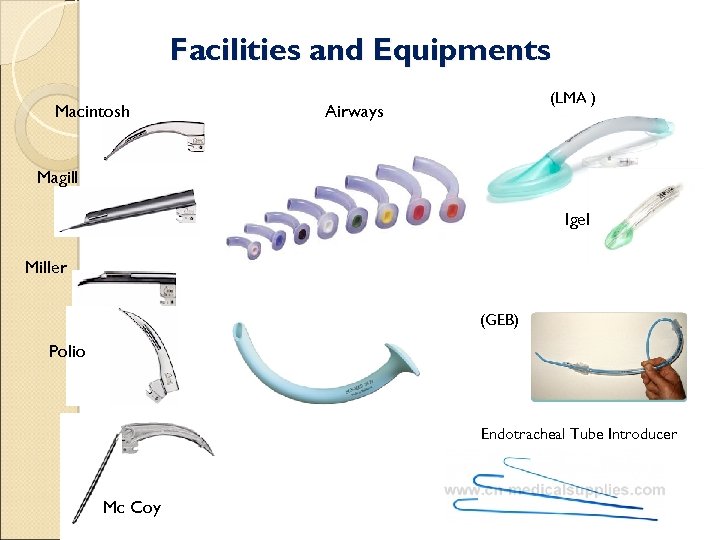 Facilities and Equipments Macintosh (LMA ) Airways Magill Igel Miller (GEB) Polio Endotracheal Tube Introducer Mc Coy
Facilities and Equipments Macintosh (LMA ) Airways Magill Igel Miller (GEB) Polio Endotracheal Tube Introducer Mc Coy
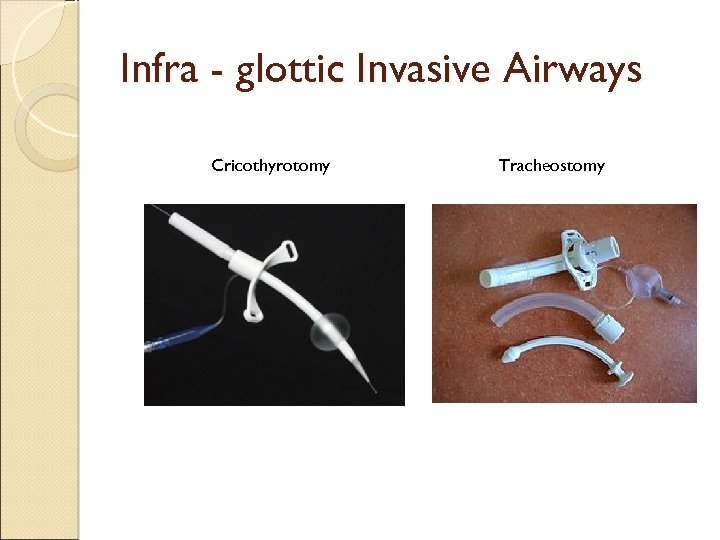 Infra - glottic Invasive Airways Cricothyrotomy Tracheostomy
Infra - glottic Invasive Airways Cricothyrotomy Tracheostomy
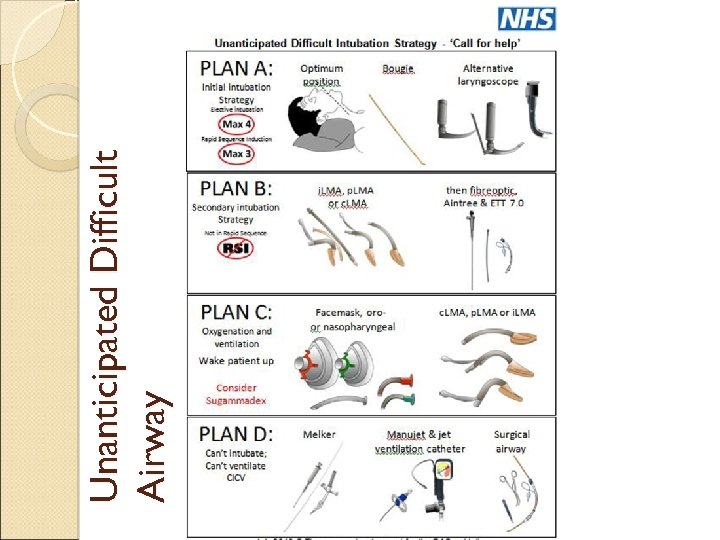 Unanticipated Difficult Airway
Unanticipated Difficult Airway
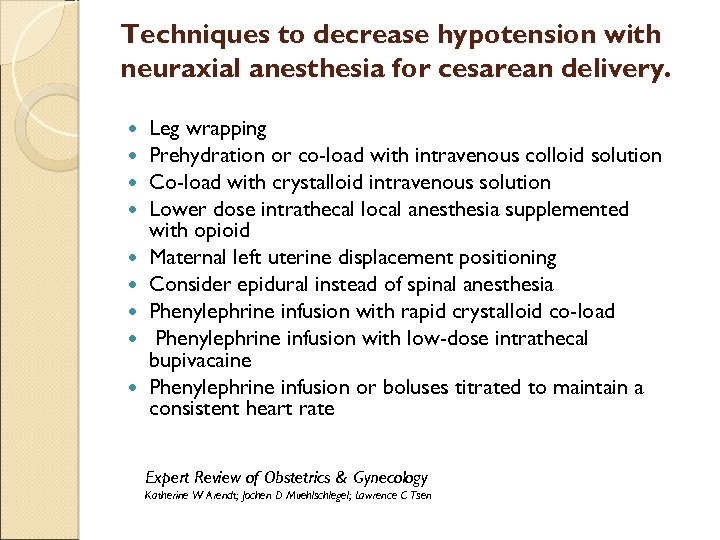 Techniques to decrease hypotension with neuraxial anesthesia for cesarean delivery. Leg wrapping Prehydration or co-load with intravenous colloid solution Co-load with crystalloid intravenous solution Lower dose intrathecal local anesthesia supplemented with opioid Maternal left uterine displacement positioning Consider epidural instead of spinal anesthesia Phenylephrine infusion with rapid crystalloid co-load Phenylephrine infusion with low-dose intrathecal bupivacaine Phenylephrine infusion or boluses titrated to maintain a consistent heart rate Expert Review of Obstetrics & Gynecology Katherine W Arendt; Jochen D Muehlschlegel; Lawrence C Tsen
Techniques to decrease hypotension with neuraxial anesthesia for cesarean delivery. Leg wrapping Prehydration or co-load with intravenous colloid solution Co-load with crystalloid intravenous solution Lower dose intrathecal local anesthesia supplemented with opioid Maternal left uterine displacement positioning Consider epidural instead of spinal anesthesia Phenylephrine infusion with rapid crystalloid co-load Phenylephrine infusion with low-dose intrathecal bupivacaine Phenylephrine infusion or boluses titrated to maintain a consistent heart rate Expert Review of Obstetrics & Gynecology Katherine W Arendt; Jochen D Muehlschlegel; Lawrence C Tsen
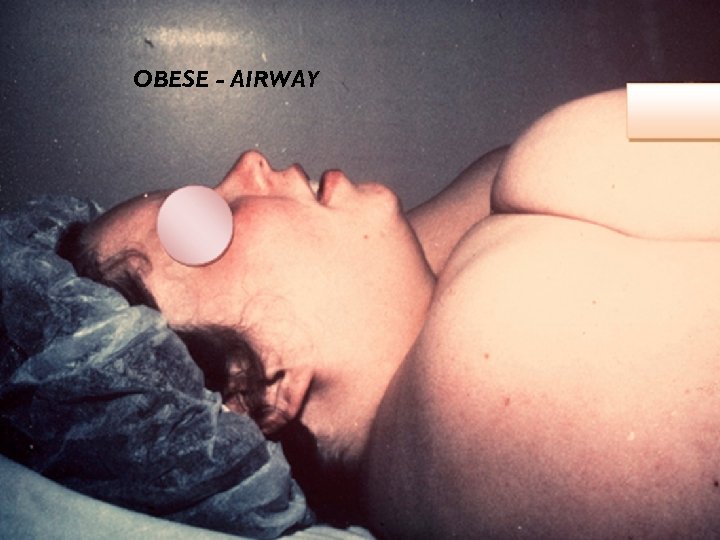 OBESE - AIRWAY
OBESE - AIRWAY
 AIRWAY CORRECTION Build a BIG RAMPPPP
AIRWAY CORRECTION Build a BIG RAMPPPP
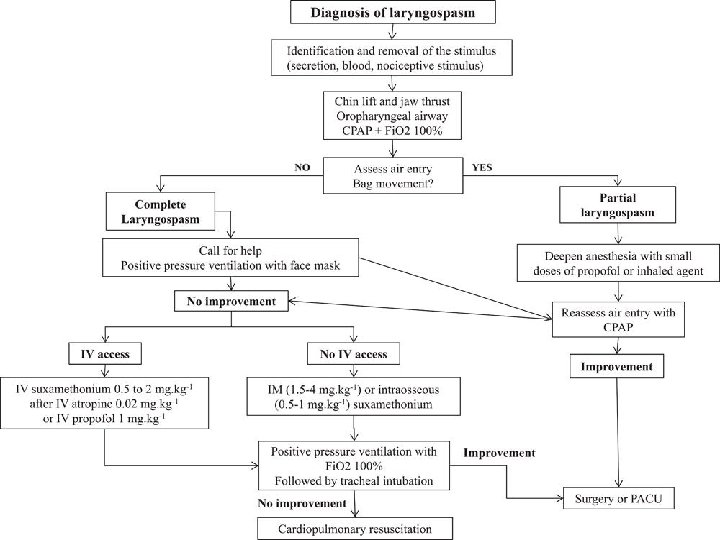
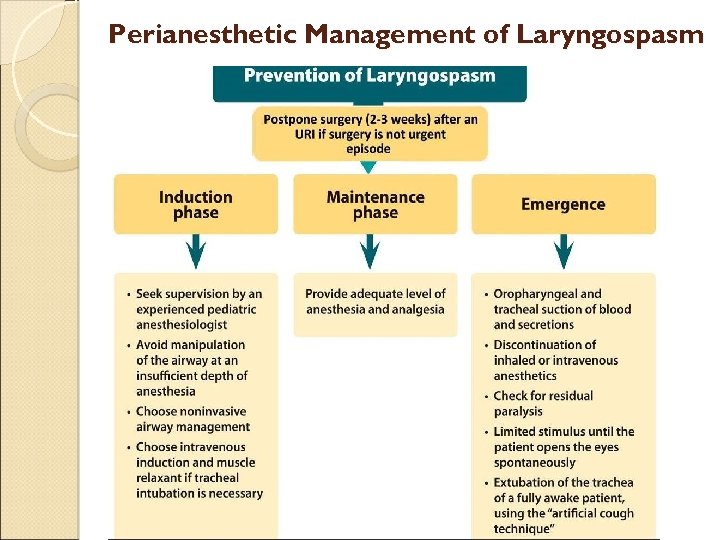 Perianesthetic Management of Laryngospasm
Perianesthetic Management of Laryngospasm
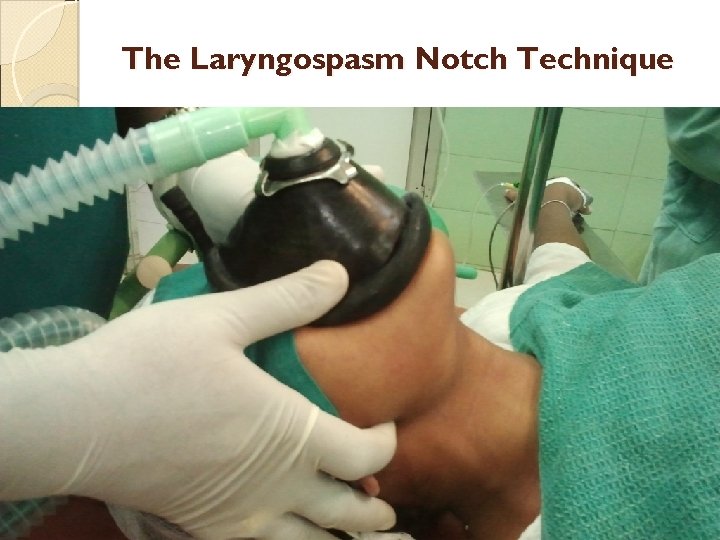 The Laryngospasm Notch Technique
The Laryngospasm Notch Technique
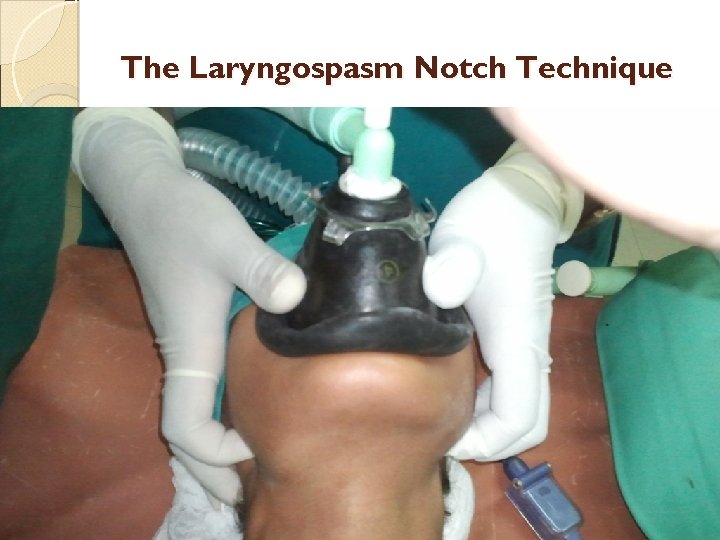 The Laryngospasm Notch Technique
The Laryngospasm Notch Technique
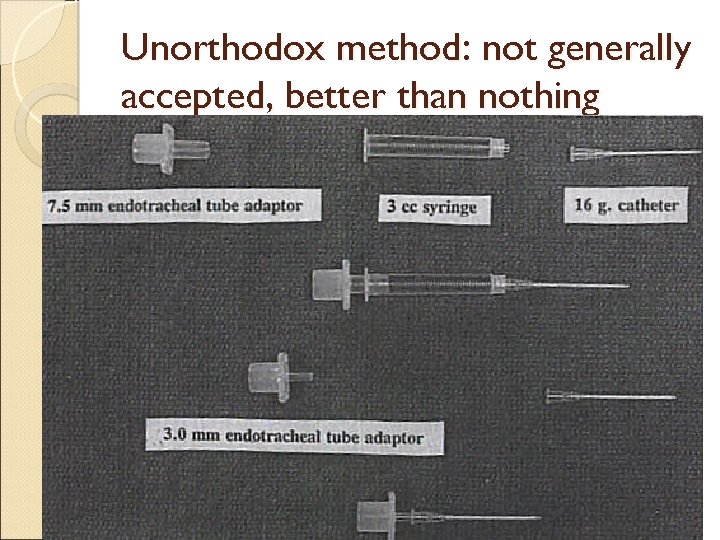 Unorthodox method: not generally accepted, better than nothing
Unorthodox method: not generally accepted, better than nothing
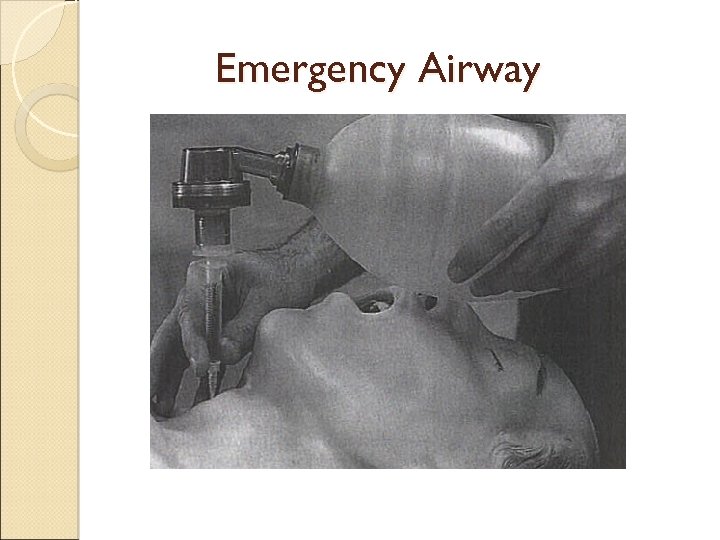 Emergency Airway
Emergency Airway
 SAFE ANAESTHESIA PRACTICE
SAFE ANAESTHESIA PRACTICE
 Thank you
Thank you


