1a02e2f7ae42b6d054184a16d9134650.ppt
- Количество слайдов: 36
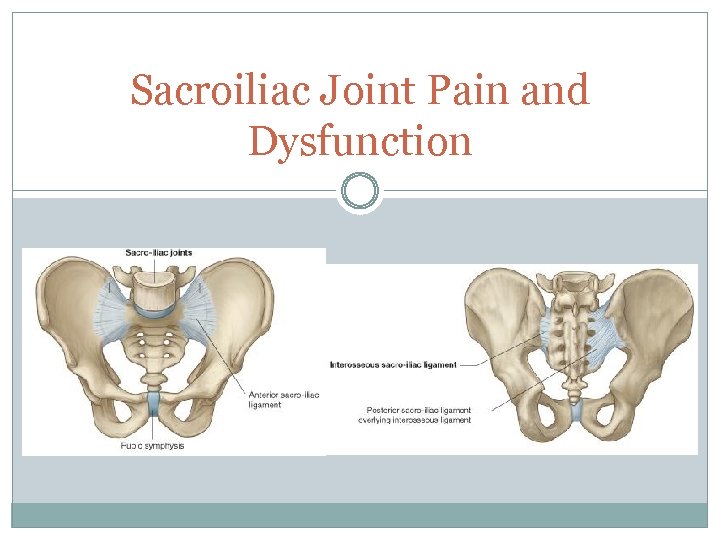 Sacroiliac Joint Pain and Dysfunction
Sacroiliac Joint Pain and Dysfunction
 Source of LBP SIJ source of LBP 15 -38% of cases In a 2010 study the cause of subjects with SIJ was: Idiopathic: 30%, Overload of work injury: 26% Fall: 24%, MVA: 9%, Other incidents: 11% Also includes Pelvic Girdle Pain. Approx 20% of pregnant women in large cohort studies.
Source of LBP SIJ source of LBP 15 -38% of cases In a 2010 study the cause of subjects with SIJ was: Idiopathic: 30%, Overload of work injury: 26% Fall: 24%, MVA: 9%, Other incidents: 11% Also includes Pelvic Girdle Pain. Approx 20% of pregnant women in large cohort studies.
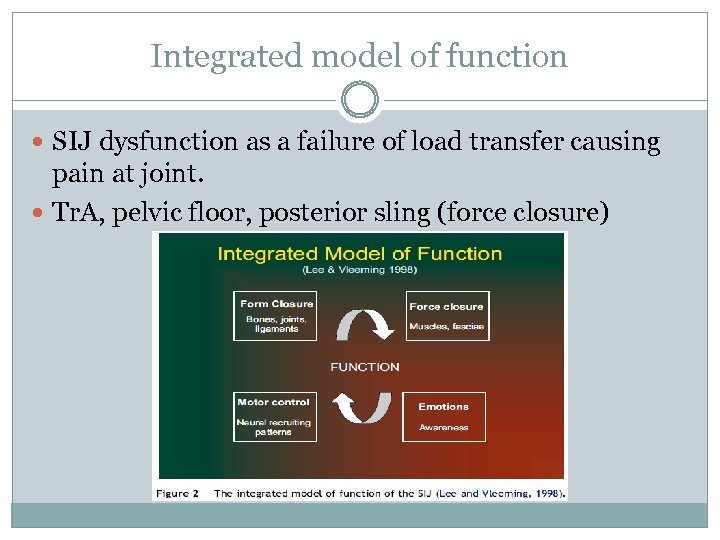 Integrated model of function SIJ dysfunction as a failure of load transfer causing pain at joint. Tr. A, pelvic floor, posterior sling (force closure)
Integrated model of function SIJ dysfunction as a failure of load transfer causing pain at joint. Tr. A, pelvic floor, posterior sling (force closure)
 Differential Diagnosis SIJ pain can refer into buttock, iliac crest, groin, abdomen, leg and foot. Possible dysfunction or pain from lumbar intervertebral discs or facet joints. Fortin et al (1994, 2003): potential pain distribution along sciatic nerve mimics a herniated lumbar disc Screen hip condtions, neuro, as required Rule out other conditions if only mm trigger point referring pain
Differential Diagnosis SIJ pain can refer into buttock, iliac crest, groin, abdomen, leg and foot. Possible dysfunction or pain from lumbar intervertebral discs or facet joints. Fortin et al (1994, 2003): potential pain distribution along sciatic nerve mimics a herniated lumbar disc Screen hip condtions, neuro, as required Rule out other conditions if only mm trigger point referring pain
 International Association for Study of Pain For a complete Dx of pain of SIJ origin: Pain in SIJ region, Pain reproduced by clinical tests selectively stressing the joint Pain completely relieved by selective delivery of local anaesthetic.
International Association for Study of Pain For a complete Dx of pain of SIJ origin: Pain in SIJ region, Pain reproduced by clinical tests selectively stressing the joint Pain completely relieved by selective delivery of local anaesthetic.
 History, characteristics of SIJ pain Pain maps: never above L 5, may refer down leg Patients may describe as sciatica Pain is recurring, triggered by bending, lifting Commonly idiopathic Initial episodes and MOI: pregnancy, trauma from fall or MVA, hard braking, transverse force on pelvis Worse when loaded, eg standing, walking Possible changes in bladder habits
History, characteristics of SIJ pain Pain maps: never above L 5, may refer down leg Patients may describe as sciatica Pain is recurring, triggered by bending, lifting Commonly idiopathic Initial episodes and MOI: pregnancy, trauma from fall or MVA, hard braking, transverse force on pelvis Worse when loaded, eg standing, walking Possible changes in bladder habits
 Mitchell et al (2012) clinical review SIJ is more likely the source of pain if: a) The patient points to the PSIS as the source of pain. b) Pain is predominantly below the L 5 level c) The sacral sulcus is tender.
Mitchell et al (2012) clinical review SIJ is more likely the source of pain if: a) The patient points to the PSIS as the source of pain. b) Pain is predominantly below the L 5 level c) The sacral sulcus is tender.
 SIJ as origin of pain (Diagnostic anaesthetic injection is reference standard) Van der Wurf (2006): All subjects that responded to the SI joint block had symptoms located at the Fortin area (3 cm medially by 10 cm vertically inferior to the PSIS) All subjects that did NOT respond to the SI joint block had symptoms at the Tuber area (just inferolateral to the ischial tuberosity) Pain in the Fortin area but not Tuber, patients may have SIJ pain But if they have pain in the Tuber but not the Fortin area it can rule out SIJ pain (sensitive)
SIJ as origin of pain (Diagnostic anaesthetic injection is reference standard) Van der Wurf (2006): All subjects that responded to the SI joint block had symptoms located at the Fortin area (3 cm medially by 10 cm vertically inferior to the PSIS) All subjects that did NOT respond to the SI joint block had symptoms at the Tuber area (just inferolateral to the ischial tuberosity) Pain in the Fortin area but not Tuber, patients may have SIJ pain But if they have pain in the Tuber but not the Fortin area it can rule out SIJ pain (sensitive)
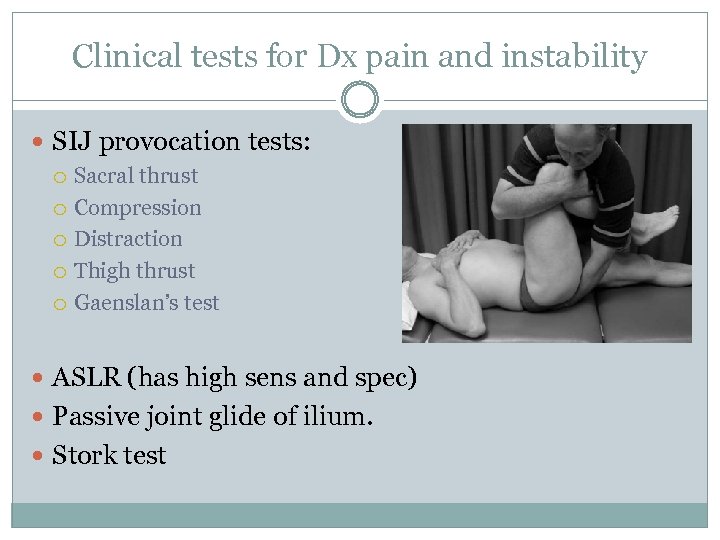 Clinical tests for Dx pain and instability SIJ provocation tests: Sacral thrust Compression Distraction Thigh thrust Gaenslan’s test ASLR (has high sens and spec) Passive joint glide of ilium. Stork test
Clinical tests for Dx pain and instability SIJ provocation tests: Sacral thrust Compression Distraction Thigh thrust Gaenslan’s test ASLR (has high sens and spec) Passive joint glide of ilium. Stork test
 Laslett et al. (2005) 3/6 +ve provocation tests had Sens: 94%, Spec: 78% for diagnosing SIJ pain. If Gaenslan’s test is excluded, 2/4 +ve tests Sens: 88%, Spec 78% In order of highest individual sens and spec: 1. 2. 3. 4. Thigh thrust Distraction Compression Sacral thrust Rule out SIJ if all tests do not provoke pain
Laslett et al. (2005) 3/6 +ve provocation tests had Sens: 94%, Spec: 78% for diagnosing SIJ pain. If Gaenslan’s test is excluded, 2/4 +ve tests Sens: 88%, Spec 78% In order of highest individual sens and spec: 1. 2. 3. 4. Thigh thrust Distraction Compression Sacral thrust Rule out SIJ if all tests do not provoke pain
 Hancock et al. (2007) Tests for LBP as disc, facet joint or SIJ as source Changes and degeneration on MRI increased probability of disc as source. (+LR approx 1 -5 for each feature on MRI) Centralisation of pain increases likelihood of disc as source (+LR=2. 8 (95% CI 1. 4 -5. 3) Helps rule out disc in absence of these signs No tests for facet joint were informative
Hancock et al. (2007) Tests for LBP as disc, facet joint or SIJ as source Changes and degeneration on MRI increased probability of disc as source. (+LR approx 1 -5 for each feature on MRI) Centralisation of pain increases likelihood of disc as source (+LR=2. 8 (95% CI 1. 4 -5. 3) Helps rule out disc in absence of these signs No tests for facet joint were informative
 Laslett (2008). Clinical Prediction Rule SIJCPR: Chronic LBP populations with: 3+ SIJ provocation tests +ve Symptoms that cannot be made to centralise have a 77% probability for SIJ pain. If also pregnant, probability increased to 89%
Laslett (2008). Clinical Prediction Rule SIJCPR: Chronic LBP populations with: 3+ SIJ provocation tests +ve Symptoms that cannot be made to centralise have a 77% probability for SIJ pain. If also pregnant, probability increased to 89%
 Other common associated impairments Weak core Weak glutes Tight or previously injured hip and back muscles Malalignments Leg length discrepancies
Other common associated impairments Weak core Weak glutes Tight or previously injured hip and back muscles Malalignments Leg length discrepancies
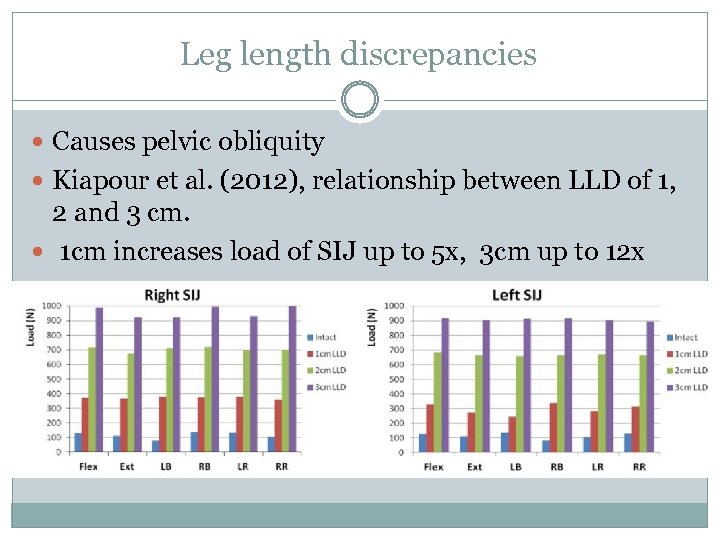 Leg length discrepancies Causes pelvic obliquity Kiapour et al. (2012), relationship between LLD of 1, 2 and 3 cm. 1 cm increases load of SIJ up to 5 x, 3 cm up to 12 x
Leg length discrepancies Causes pelvic obliquity Kiapour et al. (2012), relationship between LLD of 1, 2 and 3 cm. 1 cm increases load of SIJ up to 5 x, 3 cm up to 12 x
 Malalignments Innominate shears, sup and inferior Innominate rotations, anterior and post Innominate in flare and out flare Sacral torsions, flex and ext Unilateral sacral lesions, flex and ext.
Malalignments Innominate shears, sup and inferior Innominate rotations, anterior and post Innominate in flare and out flare Sacral torsions, flex and ext Unilateral sacral lesions, flex and ext.
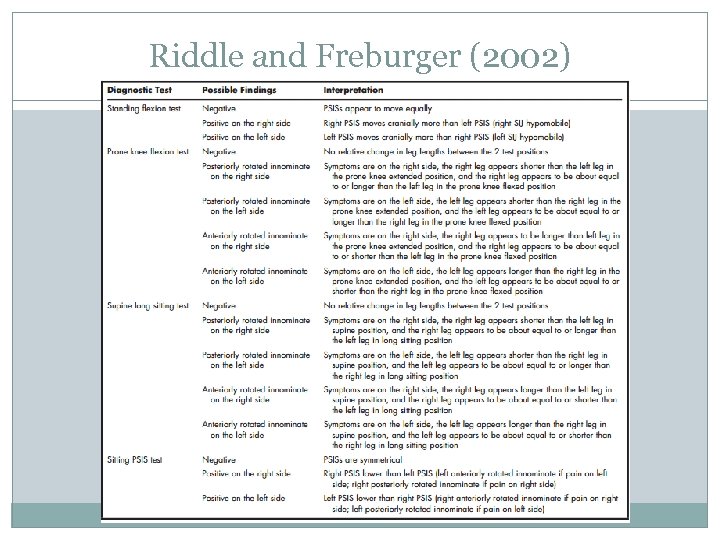 Riddle and Freburger (2002)
Riddle and Freburger (2002)
 Stork test – Muscle activity Barbara Hungerford (2003, 2004) hip flexion in standing EMG acitvity: Subjects with no hx of pain (control): Feedfoward activation of OI, lumbar multifidus. Biceps fem, add longus, glutes, TFL after initiation of motion. Subjects with PGP: Onset of OI, multifidus and glute max significantly delayed on symptomatic side Biceps fem activation significantly earlier
Stork test – Muscle activity Barbara Hungerford (2003, 2004) hip flexion in standing EMG acitvity: Subjects with no hx of pain (control): Feedfoward activation of OI, lumbar multifidus. Biceps fem, add longus, glutes, TFL after initiation of motion. Subjects with PGP: Onset of OI, multifidus and glute max significantly delayed on symptomatic side Biceps fem activation significantly earlier
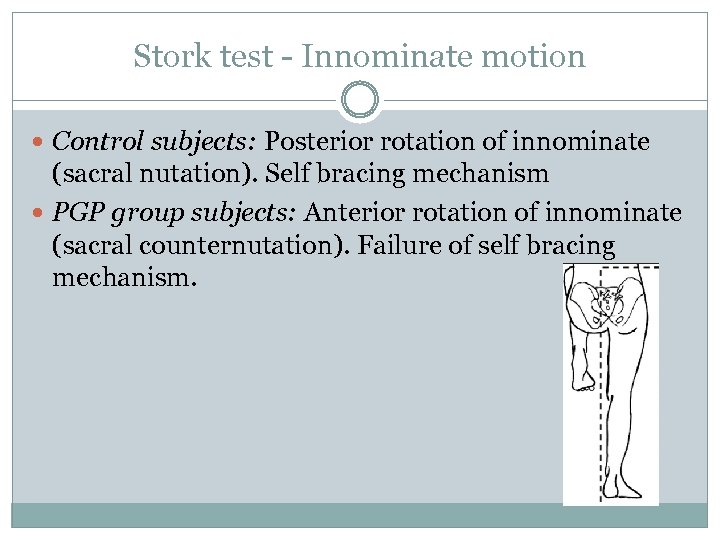 Stork test - Innominate motion Control subjects: Posterior rotation of innominate (sacral nutation). Self bracing mechanism PGP group subjects: Anterior rotation of innominate (sacral counternutation). Failure of self bracing mechanism.
Stork test - Innominate motion Control subjects: Posterior rotation of innominate (sacral nutation). Self bracing mechanism PGP group subjects: Anterior rotation of innominate (sacral counternutation). Failure of self bracing mechanism.
 Stork test – Intratherapist reliability Hungerford et al. (2007) 3 pt scale: PSIS neutral/ cephalad/caudad direction 2 pt scale: -ve= neutral or caudad. +ve= cephalad 33 subjects, 3 therapists Good inter-rater reliability for 2 pt scale. Agreement between therapists occurred: 91. 9% (L), 89. 9% (R) Moderate reliability for 3 pt scale: 82. 8%(L), 79. 8%(R)
Stork test – Intratherapist reliability Hungerford et al. (2007) 3 pt scale: PSIS neutral/ cephalad/caudad direction 2 pt scale: -ve= neutral or caudad. +ve= cephalad 33 subjects, 3 therapists Good inter-rater reliability for 2 pt scale. Agreement between therapists occurred: 91. 9% (L), 89. 9% (R) Moderate reliability for 3 pt scale: 82. 8%(L), 79. 8%(R)
 Physiotherapeutic treatments for SIJ pain Address entire abdomino-lumbo-sacro-pelvic-hip complex. Correct malalignments of pelvis and spine + address any deficiencies and restrictions found in PE Muscle energy technique and taping Myofascial release and dry needling of trigger points Exs for stablisation, muscle activation and targeting weak links + imbalances. Tr. A and the multifidus may increase tension on posterior SI ligaments and posterior layer of the thoracolumbar fascia, hence causing a nutation force on the sacrum
Physiotherapeutic treatments for SIJ pain Address entire abdomino-lumbo-sacro-pelvic-hip complex. Correct malalignments of pelvis and spine + address any deficiencies and restrictions found in PE Muscle energy technique and taping Myofascial release and dry needling of trigger points Exs for stablisation, muscle activation and targeting weak links + imbalances. Tr. A and the multifidus may increase tension on posterior SI ligaments and posterior layer of the thoracolumbar fascia, hence causing a nutation force on the sacrum

 Allison et al. (2008) Feedfoward responses of Tr. A are directionally specific and act asymmetrically Tr. A is a feedfoward muscle and preactivates other trunk mm during rapid arm raising. The ipsilateral Tr. A lagged behind that of the contralateral side Contradicts earlier studies stating the bilateral feedfoward responses are highly consistent in healthy controls and how this isolated activation contributes substantially to segmental stability of the lumbar spine.
Allison et al. (2008) Feedfoward responses of Tr. A are directionally specific and act asymmetrically Tr. A is a feedfoward muscle and preactivates other trunk mm during rapid arm raising. The ipsilateral Tr. A lagged behind that of the contralateral side Contradicts earlier studies stating the bilateral feedfoward responses are highly consistent in healthy controls and how this isolated activation contributes substantially to segmental stability of the lumbar spine.
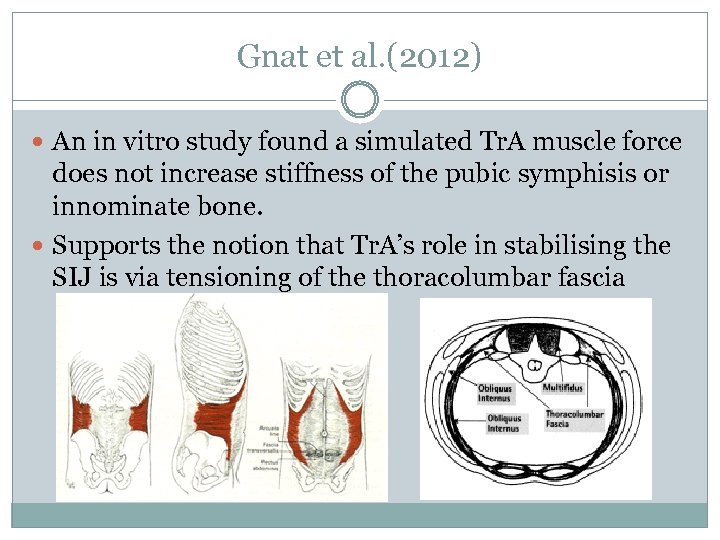 Gnat et al. (2012) An in vitro study found a simulated Tr. A muscle force does not increase stiffness of the pubic symphisis or innominate bone. Supports the notion that Tr. A’s role in stabilising the SIJ is via tensioning of the thoracolumbar fascia
Gnat et al. (2012) An in vitro study found a simulated Tr. A muscle force does not increase stiffness of the pubic symphisis or innominate bone. Supports the notion that Tr. A’s role in stabilising the SIJ is via tensioning of the thoracolumbar fascia
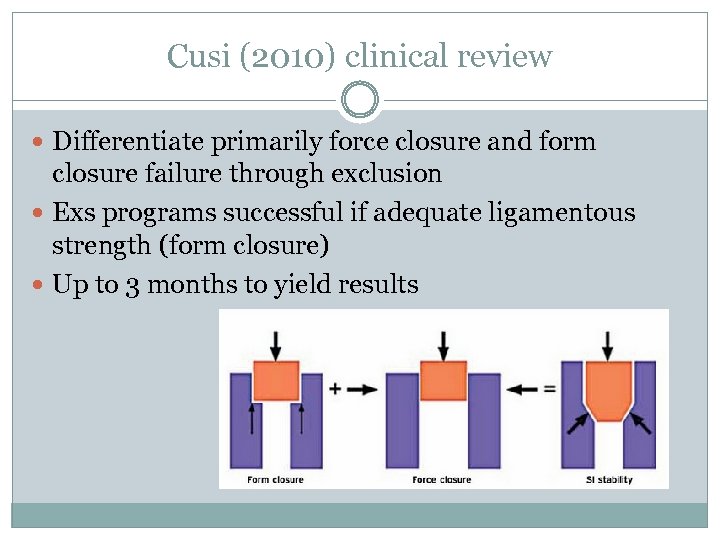 Cusi (2010) clinical review Differentiate primarily force closure and form closure failure through exclusion Exs programs successful if adequate ligamentous strength (form closure) Up to 3 months to yield results
Cusi (2010) clinical review Differentiate primarily force closure and form closure failure through exclusion Exs programs successful if adequate ligamentous strength (form closure) Up to 3 months to yield results
 Stuge et al. (2004) RCT Post partum women with PGP Physio with stabilisation exs vs. Physio alone with basic strengthening/mob exs Exs 30 -60 min, 3 x/week for 18 -20 weeks. 50% reduction in disability, 30 mm reduction in pain VAS scale, improvement in Qo. L at 1 year cf. insignificant changes in control group. Maintained at 2 yr follow-up
Stuge et al. (2004) RCT Post partum women with PGP Physio with stabilisation exs vs. Physio alone with basic strengthening/mob exs Exs 30 -60 min, 3 x/week for 18 -20 weeks. 50% reduction in disability, 30 mm reduction in pain VAS scale, improvement in Qo. L at 1 year cf. insignificant changes in control group. Maintained at 2 yr follow-up
 3 Stages of Exercise Therapy Isolation Train motor control ability Tr. A, pelvic floor +downtrain global mm. compensation Combination Progressively challenge, incorporate activation of global mm. while maintaining control from prev stage. Function Progress to functional activities according to patient needs and goals.
3 Stages of Exercise Therapy Isolation Train motor control ability Tr. A, pelvic floor +downtrain global mm. compensation Combination Progressively challenge, incorporate activation of global mm. while maintaining control from prev stage. Function Progress to functional activities according to patient needs and goals.
 Fail to respond to exs program? Intrinsic factors: Poor design (exs not specific enough) Premature progression through stages Poor compliance Poor exs technique Extrinsic factor: failure of form closure if program was executed correctly.
Fail to respond to exs program? Intrinsic factors: Poor design (exs not specific enough) Premature progression through stages Poor compliance Poor exs technique Extrinsic factor: failure of form closure if program was executed correctly.
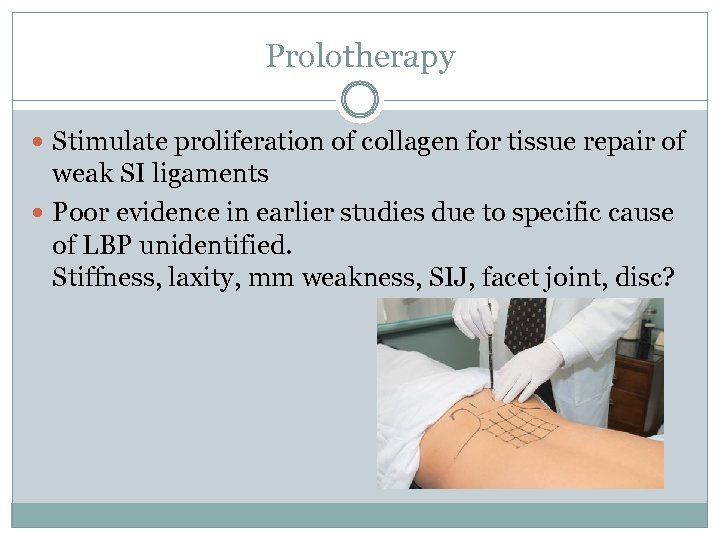 Prolotherapy Stimulate proliferation of collagen for tissue repair of weak SI ligaments Poor evidence in earlier studies due to specific cause of LBP unidentified. Stiffness, laxity, mm weakness, SIJ, facet joint, disc?
Prolotherapy Stimulate proliferation of collagen for tissue repair of weak SI ligaments Poor evidence in earlier studies due to specific cause of LBP unidentified. Stiffness, laxity, mm weakness, SIJ, facet joint, disc?
 Prolotherapy studies Cusi et al. (2008) SIJ Case series 25 patients not responding to exs 3 prolotherapy injections, 6 wks apart into dorsal interosseus lig Significant improvement in clinical exam paramters and functional questionnaires at 3, 12, 24 months. Mitchell et al case series: prolotherapy on SIJ ligaments resulted in 76% of patients satisfied. Kim et al. (2010) RCT: ““Intra-articular prolotherapy provided significant relief of sacroiliac joint pain, and its effects lasted longer than those of steroid injections. ”
Prolotherapy studies Cusi et al. (2008) SIJ Case series 25 patients not responding to exs 3 prolotherapy injections, 6 wks apart into dorsal interosseus lig Significant improvement in clinical exam paramters and functional questionnaires at 3, 12, 24 months. Mitchell et al case series: prolotherapy on SIJ ligaments resulted in 76% of patients satisfied. Kim et al. (2010) RCT: ““Intra-articular prolotherapy provided significant relief of sacroiliac joint pain, and its effects lasted longer than those of steroid injections. ”
 Pelvic Compression Belt Jung et al. (2012) Pelvic compression belt improved hip extension muscle activation in SIJ patients during SLS. SIJ pain group with pelvic belt: sig decrease in biceps fem activation when compared to control +Premotor reaction time for glute max decreased and increased for biceps fem.
Pelvic Compression Belt Jung et al. (2012) Pelvic compression belt improved hip extension muscle activation in SIJ patients during SLS. SIJ pain group with pelvic belt: sig decrease in biceps fem activation when compared to control +Premotor reaction time for glute max decreased and increased for biceps fem.
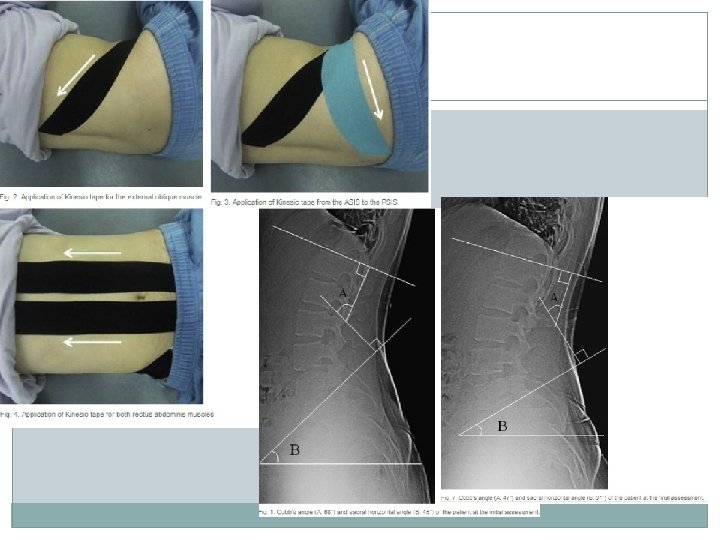
 Posterior pelvic tilt taping: Lee and Yoo (2011) Case report: 20 yr old female swimmer with anterior pelvic tilt and hyperlordosis. Chronic bilateral SIJ pain. PPTT performed 6 x/week. Avg of 9 hr each time for 2 weeks. Cobb's angle (L 1 -S 1) had decreased from 68° to 47° and that the sacral horizontal angle had decreased from 45° to 31°. Reductions in motion asymmetry, provocation test pain and pain on palpation of medial buttock area. No follow up
Posterior pelvic tilt taping: Lee and Yoo (2011) Case report: 20 yr old female swimmer with anterior pelvic tilt and hyperlordosis. Chronic bilateral SIJ pain. PPTT performed 6 x/week. Avg of 9 hr each time for 2 weeks. Cobb's angle (L 1 -S 1) had decreased from 68° to 47° and that the sacral horizontal angle had decreased from 45° to 31°. Reductions in motion asymmetry, provocation test pain and pain on palpation of medial buttock area. No follow up
 Spinal and SIJ HVLA Manipulations Kamali and Shokri (2011): single session HVLA to SIJ vs. HVLA to SIJ and Lumbar spine (rotational) 16 subjects each group, diagnosed with SIJ pain with provocation tests Both groups significant improvement in pain and function immediately, 48 hr and one month post SIJ and lumbar manipulation more effective than SIJ manipulation alone Treat both as closely interrelated
Spinal and SIJ HVLA Manipulations Kamali and Shokri (2011): single session HVLA to SIJ vs. HVLA to SIJ and Lumbar spine (rotational) 16 subjects each group, diagnosed with SIJ pain with provocation tests Both groups significant improvement in pain and function immediately, 48 hr and one month post SIJ and lumbar manipulation more effective than SIJ manipulation alone Treat both as closely interrelated
 Corticosteroid injections Limited evidence Case series report excellent pain relief with duration up to 10 months 77% of 155 patients positive responders over a mean: followup of 44 months, 2. 7 injections, duraction of 9. 3 months
Corticosteroid injections Limited evidence Case series report excellent pain relief with duration up to 10 months 77% of 155 patients positive responders over a mean: followup of 44 months, 2. 7 injections, duraction of 9. 3 months
 Hansen et al. (2012) Sys review on SIJ interventions for pain relief (11 studies) Evidence for cooled radiofrequency neurotomy in managing sacroiliac joint pain is fair. Evidence for effectiveness of intraarticular steroid injections is limited (or poor). Evidence for periarticular injections of local anesthetic and steroid or botulinum toxin is limited (or poor). Evidence for effectiveness of conventional radiofrequency neurotomy is limited (or poor). Evidence for pulsed radiofrequency is limited (or poor).
Hansen et al. (2012) Sys review on SIJ interventions for pain relief (11 studies) Evidence for cooled radiofrequency neurotomy in managing sacroiliac joint pain is fair. Evidence for effectiveness of intraarticular steroid injections is limited (or poor). Evidence for periarticular injections of local anesthetic and steroid or botulinum toxin is limited (or poor). Evidence for effectiveness of conventional radiofrequency neurotomy is limited (or poor). Evidence for pulsed radiofrequency is limited (or poor).
 THE END.
THE END.


