9e58c2ab10a78c244c41a41e19048206.ppt
- Количество слайдов: 60
 Rural Stroke Care for Prehospital Providers Chris Hogness, MD Telehealth Training March 17 th, 2010 Northwest Regional Stroke Network
Rural Stroke Care for Prehospital Providers Chris Hogness, MD Telehealth Training March 17 th, 2010 Northwest Regional Stroke Network
 Welcome n Thank you for joining us! n Format n Introductions
Welcome n Thank you for joining us! n Format n Introductions
 What we will talk about today n n n Evidence behind current stroke therapies ¨ Focus on intravenous thrombolysis Role of EMS in stroke systems of care: ¨ Activation of 911 ¨ Identification of stroke pt in the field ¨ Appropriate pre-hospital care ¨ Transport System planning for improved care
What we will talk about today n n n Evidence behind current stroke therapies ¨ Focus on intravenous thrombolysis Role of EMS in stroke systems of care: ¨ Activation of 911 ¨ Identification of stroke pt in the field ¨ Appropriate pre-hospital care ¨ Transport System planning for improved care
 CASE n Previously healthy 48 yo man n History of migraine HA, last episode 1 yr ago n Possible episodic hypertension remotely, normal blood pressure in recent visit to PCP n Low grade hemoglobin A 1 C elevation: 6. 2 n Normal LDL cholesterol: 100 n No family history of vascular disease
CASE n Previously healthy 48 yo man n History of migraine HA, last episode 1 yr ago n Possible episodic hypertension remotely, normal blood pressure in recent visit to PCP n Low grade hemoglobin A 1 C elevation: 6. 2 n Normal LDL cholesterol: 100 n No family history of vascular disease
 CASE, continued n Experienced episode of weakness, fell at home ¨ Went back to bed Awoke 1 hour later with speech difficulty and left hemiparesis n EMS activated: n ¨ Delay in reaching rural location, paramedics chain up to get to his home
CASE, continued n Experienced episode of weakness, fell at home ¨ Went back to bed Awoke 1 hour later with speech difficulty and left hemiparesis n EMS activated: n ¨ Delay in reaching rural location, paramedics chain up to get to his home
 CASE, continued n Taken to local t-PA capable, critical access hospital Head CT done: no acute change n Phone consultation with neurologist 2 hrs away n Time since last normal 4 ½ hrs n Recommendation for no TPA, not given n Transferred to larger hospital n
CASE, continued n Taken to local t-PA capable, critical access hospital Head CT done: no acute change n Phone consultation with neurologist 2 hrs away n Time since last normal 4 ½ hrs n Recommendation for no TPA, not given n Transferred to larger hospital n
 CASE, continued n Further evaluation: MRA brain: Acute stroke involving posterior division of R MCA n MRA neck: Complete occlusion proximal R internal carotid n F/U CT brain 4 days after event: Interval extension of large R MCA infarct with surrounding edema n Specials: n TEE with bubble: no PFO ¨ Hypercoagulable w/u negative ¨
CASE, continued n Further evaluation: MRA brain: Acute stroke involving posterior division of R MCA n MRA neck: Complete occlusion proximal R internal carotid n F/U CT brain 4 days after event: Interval extension of large R MCA infarct with surrounding edema n Specials: n TEE with bubble: no PFO ¨ Hypercoagulable w/u negative ¨
 Stroke kills and disables many n Most common cause of disability in the world ¨ 1 n person disabled every 45 seconds in US Third leading cause of death in US ¨ 700, 000 n strokes/year in US Washington state: ¨ 26, 612 hosp and 3, 167 (6. 9%) deaths (2005)
Stroke kills and disables many n Most common cause of disability in the world ¨ 1 n person disabled every 45 seconds in US Third leading cause of death in US ¨ 700, 000 n strokes/year in US Washington state: ¨ 26, 612 hosp and 3, 167 (6. 9%) deaths (2005)
 Pathophysiology of stroke Angiographic and autopsy studies reveal approximately 80% of strokes caused by occlusive arterial thrombus
Pathophysiology of stroke Angiographic and autopsy studies reveal approximately 80% of strokes caused by occlusive arterial thrombus
 Brain cells die quickly in stroke n 1. 9 million neurons lost per minute ¨ Initial ischemic penumbra, area of decreased perfusion with neurologic dysfunction which may not be permanent if flow restored n Time window for clinical benefit of opening artery challengingly brief
Brain cells die quickly in stroke n 1. 9 million neurons lost per minute ¨ Initial ischemic penumbra, area of decreased perfusion with neurologic dysfunction which may not be permanent if flow restored n Time window for clinical benefit of opening artery challengingly brief
 Opening the occluded artery Intravenous thrombolytic n Intra-arterial thrombolytic n Mechanical n
Opening the occluded artery Intravenous thrombolytic n Intra-arterial thrombolytic n Mechanical n
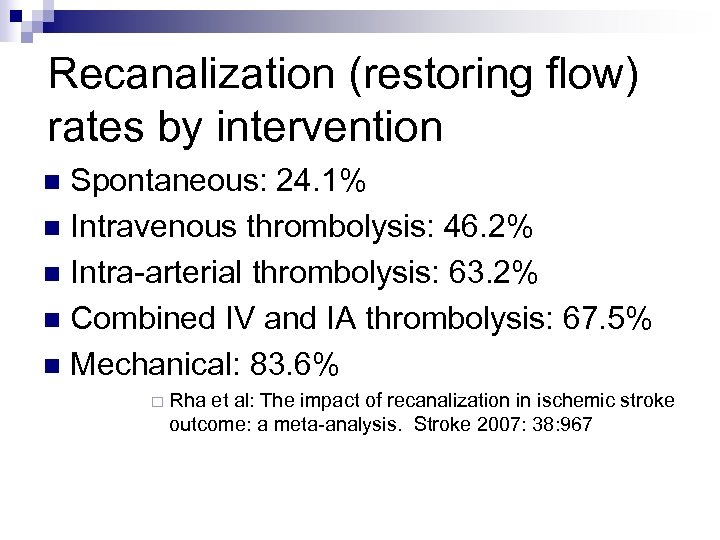 Recanalization (restoring flow) rates by intervention Spontaneous: 24. 1% n Intravenous thrombolysis: 46. 2% n Intra-arterial thrombolysis: 63. 2% n Combined IV and IA thrombolysis: 67. 5% n Mechanical: 83. 6% n ¨ Rha et al: The impact of recanalization in ischemic stroke outcome: a meta-analysis. Stroke 2007: 38: 967
Recanalization (restoring flow) rates by intervention Spontaneous: 24. 1% n Intravenous thrombolysis: 46. 2% n Intra-arterial thrombolysis: 63. 2% n Combined IV and IA thrombolysis: 67. 5% n Mechanical: 83. 6% n ¨ Rha et al: The impact of recanalization in ischemic stroke outcome: a meta-analysis. Stroke 2007: 38: 967
 Recanalization (restoring flow) rates by intervention, update ¨ 1, 122 severe stroke patients at 13 academic centers between 2005 and 2009 ¨ Treated with one or more of: intra-arterial t. PA n intracranial stenting n IV delivery of t. PA in the arm n Merci Retriever for clot removal n Prenumbra aspiration catheter for clot removal n glycoprotein IIb/IIIa antagonists n angioplasty without stenting n
Recanalization (restoring flow) rates by intervention, update ¨ 1, 122 severe stroke patients at 13 academic centers between 2005 and 2009 ¨ Treated with one or more of: intra-arterial t. PA n intracranial stenting n IV delivery of t. PA in the arm n Merci Retriever for clot removal n Prenumbra aspiration catheter for clot removal n glycoprotein IIb/IIIa antagonists n angioplasty without stenting n
 Recanalization update, continued n n n Patients treated with mechanical agents and drugs (n=584) compared to those treated only with mechanical therapy (n=274) or only drug therapy (n=264). Successful recanalization in 68% of all patients Recanalization rate for multimodal therapy patients 74%, no higher incidence of hemorrhage. ¨ Stenting and IA TPA only independent predictors of vessel recanalization during endovascular treatment. ASA International Stroke Conference Feb 2010
Recanalization update, continued n n n Patients treated with mechanical agents and drugs (n=584) compared to those treated only with mechanical therapy (n=274) or only drug therapy (n=264). Successful recanalization in 68% of all patients Recanalization rate for multimodal therapy patients 74%, no higher incidence of hemorrhage. ¨ Stenting and IA TPA only independent predictors of vessel recanalization during endovascular treatment. ASA International Stroke Conference Feb 2010
 Most patient outcome data from intravenous thrombolysis n Intra-arterial, mechanical not randomized with iv thrombolysis: No RCT data comparing disability, death ¨ Improved flow may not correlate with improved outcome depending on technique used (eg distal embolization) ¨ n Exact niche for each modality not determined Intra-arterial lower t. PA volume, role in pts at increased risk of bleeding ¨ Intra-arterial may be more effective for more proximal occlusions ¨
Most patient outcome data from intravenous thrombolysis n Intra-arterial, mechanical not randomized with iv thrombolysis: No RCT data comparing disability, death ¨ Improved flow may not correlate with improved outcome depending on technique used (eg distal embolization) ¨ n Exact niche for each modality not determined Intra-arterial lower t. PA volume, role in pts at increased risk of bleeding ¨ Intra-arterial may be more effective for more proximal occlusions ¨
 Intravenous thrombolysis Multiple randomized controlled trials demonstrate reduced stroke disability n Consensus guidelines recommend: n American Heart Association n American College of Chest Physicians n n Regulatory agencies approve: FDA 1996 n Canada 1999 n European Union 2002 n
Intravenous thrombolysis Multiple randomized controlled trials demonstrate reduced stroke disability n Consensus guidelines recommend: n American Heart Association n American College of Chest Physicians n n Regulatory agencies approve: FDA 1996 n Canada 1999 n European Union 2002 n
 National Institute of Neurologic Disorders and Stroke (NINDS): NEJM 1995 • 624 pts with acute ischemic stroke, treated within 3 hrs of symptoms onset • Randomized to TPA vs placebo • Complete/near complete recovery at 90 days: • 31 -50% TPA vs 20 -35% placebo • Mortality not significantly different • 17% TPA vs 21% placebo • 10 fold increase in brain hemorrhage • 6. 4% TPA vs 0. 5% placebo
National Institute of Neurologic Disorders and Stroke (NINDS): NEJM 1995 • 624 pts with acute ischemic stroke, treated within 3 hrs of symptoms onset • Randomized to TPA vs placebo • Complete/near complete recovery at 90 days: • 31 -50% TPA vs 20 -35% placebo • Mortality not significantly different • 17% TPA vs 21% placebo • 10 fold increase in brain hemorrhage • 6. 4% TPA vs 0. 5% placebo
 Stroke disability scores used in NINDS trial and others n n Modified Rankin scale: functional score ¨ 0 = no symptoms; 5 = severe disability Barthel index: activities of daily living ¨ 0 -100; 100 = complete independence Glasgow outcome scale: function ¨ 1 = good recovery; 5 = death NIH Stroke Scale (NIHSS) ¨ 42 point scale measure of neurologic deficit
Stroke disability scores used in NINDS trial and others n n Modified Rankin scale: functional score ¨ 0 = no symptoms; 5 = severe disability Barthel index: activities of daily living ¨ 0 -100; 100 = complete independence Glasgow outcome scale: function ¨ 1 = good recovery; 5 = death NIH Stroke Scale (NIHSS) ¨ 42 point scale measure of neurologic deficit
 NINDS favorable disability outcomes n n Modified Rankin scale of 0 -1: ¨ 39% t. PA vs 26 % placebo Barthel index of 95 -100: ¨ 50% t. PA vs 38% placebo Glasgow Outcome Scale of 1: ¨ 44% t. PA vs 32% placebo NIHSS 0 -1: ¨ 31% t. PA vs 20% placebo
NINDS favorable disability outcomes n n Modified Rankin scale of 0 -1: ¨ 39% t. PA vs 26 % placebo Barthel index of 95 -100: ¨ 50% t. PA vs 38% placebo Glasgow Outcome Scale of 1: ¨ 44% t. PA vs 32% placebo NIHSS 0 -1: ¨ 31% t. PA vs 20% placebo
 Pooled analysis of 6 t. PA trials n n 2775 patients ¨ NINDS parts 1&2 (3 hr window) ¨ ECASS I and II (6 hr window) ¨ ATLANTIS A (6 hr window) and B (5 hr) Findings: ¨ Benefit dependent on time from onset of symptoms to treatment ¨ Hemorrhage 5. 9% t. PA vs 1. 1% placebo § Lancet 2004: 363: 768 -774
Pooled analysis of 6 t. PA trials n n 2775 patients ¨ NINDS parts 1&2 (3 hr window) ¨ ECASS I and II (6 hr window) ¨ ATLANTIS A (6 hr window) and B (5 hr) Findings: ¨ Benefit dependent on time from onset of symptoms to treatment ¨ Hemorrhage 5. 9% t. PA vs 1. 1% placebo § Lancet 2004: 363: 768 -774
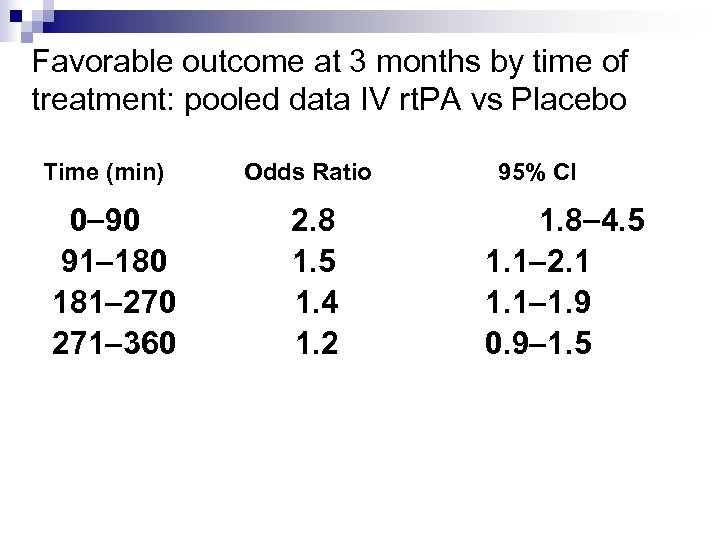 Favorable outcome at 3 months by time of treatment: pooled data IV rt. PA vs Placebo Time (min) 0 90 91 180 181 270 271 360 Odds Ratio 2. 8 1. 5 1. 4 1. 2 95% CI 1. 8 4. 5 1. 1 2. 1 1. 9 0. 9 1. 5
Favorable outcome at 3 months by time of treatment: pooled data IV rt. PA vs Placebo Time (min) 0 90 91 180 181 270 271 360 Odds Ratio 2. 8 1. 5 1. 4 1. 2 95% CI 1. 8 4. 5 1. 1 2. 1 1. 9 0. 9 1. 5
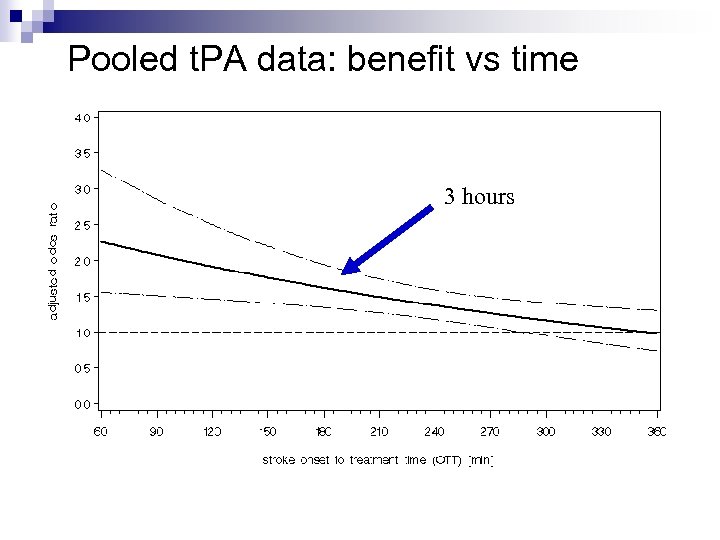 Pooled t. PA data: benefit vs time 3 hours Pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004; 363: 768
Pooled t. PA data: benefit vs time 3 hours Pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004; 363: 768
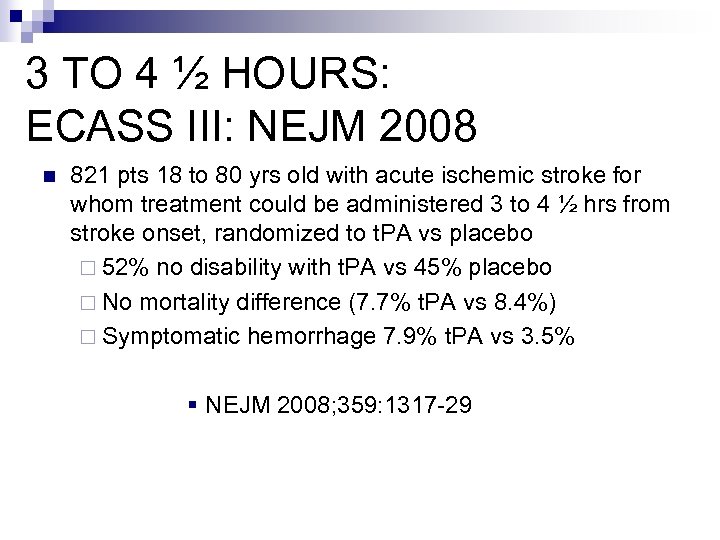 3 TO 4 ½ HOURS: ECASS III: NEJM 2008 n 821 pts 18 to 80 yrs old with acute ischemic stroke for whom treatment could be administered 3 to 4 ½ hrs from stroke onset, randomized to t. PA vs placebo ¨ 52% no disability with t. PA vs 45% placebo ¨ No mortality difference (7. 7% t. PA vs 8. 4%) ¨ Symptomatic hemorrhage 7. 9% t. PA vs 3. 5% § NEJM 2008; 359: 1317 -29
3 TO 4 ½ HOURS: ECASS III: NEJM 2008 n 821 pts 18 to 80 yrs old with acute ischemic stroke for whom treatment could be administered 3 to 4 ½ hrs from stroke onset, randomized to t. PA vs placebo ¨ 52% no disability with t. PA vs 45% placebo ¨ No mortality difference (7. 7% t. PA vs 8. 4%) ¨ Symptomatic hemorrhage 7. 9% t. PA vs 3. 5% § NEJM 2008; 359: 1317 -29
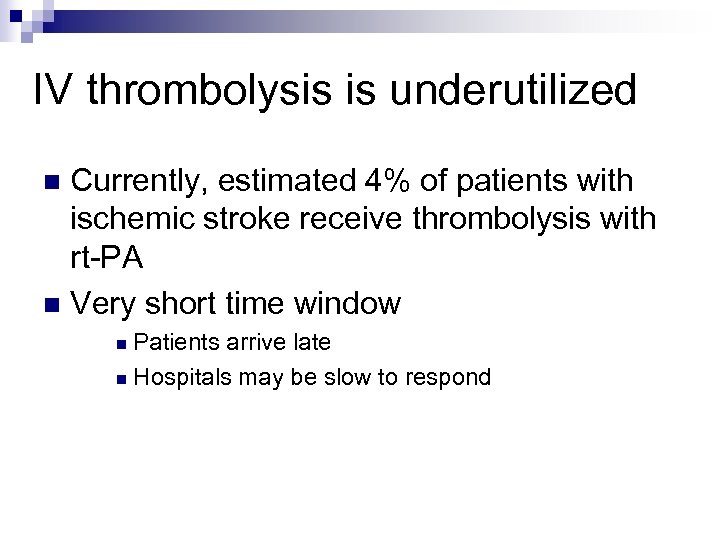 IV thrombolysis is underutilized Currently, estimated 4% of patients with ischemic stroke receive thrombolysis with rt-PA n Very short time window n Patients arrive late n Hospitals may be slow to respond n
IV thrombolysis is underutilized Currently, estimated 4% of patients with ischemic stroke receive thrombolysis with rt-PA n Very short time window n Patients arrive late n Hospitals may be slow to respond n
 How long does it take pts to get to the hospital? n 106, 924 pts treated over 4 year period at 905 “Get-With-the-Guidelines” hospitals for whom time of onset of stroke available ¨ 28. 3% arrived within 60 minutes ¨ 31. 7% 1 -3 hours ¨ 40. 1% > 3 hours § Jeff Saver, Feb 18, 2009, ASA International Stroke Conference
How long does it take pts to get to the hospital? n 106, 924 pts treated over 4 year period at 905 “Get-With-the-Guidelines” hospitals for whom time of onset of stroke available ¨ 28. 3% arrived within 60 minutes ¨ 31. 7% 1 -3 hours ¨ 40. 1% > 3 hours § Jeff Saver, Feb 18, 2009, ASA International Stroke Conference
 How long does it take to begin rt. PA after pt arrives at hospital? •
How long does it take to begin rt. PA after pt arrives at hospital? •
 Goal treatment timeline for doorto-needle Evaluation by physician: 10 min n Stroke expertise contacted: 15 min n Head CT or MRI performed: 25 min n Interpretation of CT/MRI: 45 min n Start of treatment: 60 min n
Goal treatment timeline for doorto-needle Evaluation by physician: 10 min n Stroke expertise contacted: 15 min n Head CT or MRI performed: 25 min n Interpretation of CT/MRI: 45 min n Start of treatment: 60 min n
 Why do patients delay seeking care for acute ischemic stroke? n Painless ¨ Unlike myocardial infarction Cognition may be impaired by the event n Not calling 911 n ¨ 1 st n call to physician associated with delay 911 dispatch may fail to recognize sx or not understand pt due to stroke
Why do patients delay seeking care for acute ischemic stroke? n Painless ¨ Unlike myocardial infarction Cognition may be impaired by the event n Not calling 911 n ¨ 1 st n call to physician associated with delay 911 dispatch may fail to recognize sx or not understand pt due to stroke
 True/False: EMS response times to suspected stroke should be equal to response times for suspected MI
True/False: EMS response times to suspected stroke should be equal to response times for suspected MI
 AHA recommended goals for EMS response time in stroke Dispatch time < 1 minute n Turnout time < 1 minute n Travel time equivalent to trauma or MI calls n
AHA recommended goals for EMS response time in stroke Dispatch time < 1 minute n Turnout time < 1 minute n Travel time equivalent to trauma or MI calls n
 What is the maximum on scene time recommended for EMS personnel prior to transport of the patient with stroke?
What is the maximum on scene time recommended for EMS personnel prior to transport of the patient with stroke?
 Minimize on-scene time Least is best n No more than 10 minutes in assessment n ¨ Some n parts may be done in transit Goal <15 minutes total on-scene time
Minimize on-scene time Least is best n No more than 10 minutes in assessment n ¨ Some n parts may be done in transit Goal <15 minutes total on-scene time
 True / False: EMS personnel should use a validated screening tool in assessing pts for stroke
True / False: EMS personnel should use a validated screening tool in assessing pts for stroke
 EMS stroke assessment tools Cincinnati Prehospital Stroke Scale n Los Angeles Prehospital Stroke Screen n F. A. S. T. n
EMS stroke assessment tools Cincinnati Prehospital Stroke Scale n Los Angeles Prehospital Stroke Screen n F. A. S. T. n
 F. A. S. T. Face n Arm n Speech n Time last normal n n If one component abnormal, 72% probability CVA
F. A. S. T. Face n Arm n Speech n Time last normal n n If one component abnormal, 72% probability CVA
 Name several conditions that can mimic stroke
Name several conditions that can mimic stroke
 Conditions mimicking stroke: Hypoglycemia n Seizure with post-ictal period n Complex migraine n Conversion disorder n Drug ingestion n
Conditions mimicking stroke: Hypoglycemia n Seizure with post-ictal period n Complex migraine n Conversion disorder n Drug ingestion n
 Over-triage Err on the side of over-identification rather than under-identification n AHA: “Initially, EMSS should establish a goal of over-triage of 30% for the prehospital assessment of acute stroke” n Lessons from trauma: if over-triage is not present, under-triage will result n
Over-triage Err on the side of over-identification rather than under-identification n AHA: “Initially, EMSS should establish a goal of over-triage of 30% for the prehospital assessment of acute stroke” n Lessons from trauma: if over-triage is not present, under-triage will result n
 What routine pieces of history should be obtained? TIME LAST NORMAL n Hx diabetes? Use of insulin? n Hypertension? Medications used? n Hx seizure disorder? n
What routine pieces of history should be obtained? TIME LAST NORMAL n Hx diabetes? Use of insulin? n Hypertension? Medications used? n Hx seizure disorder? n
 What piece of history is often not included in prehospital assessments?
What piece of history is often not included in prehospital assessments?
 Time last normal EMS personnel often only medical providers with access to all witnesses n Transporting family/witnesses with patient may help with treatment decisions at the hospital n
Time last normal EMS personnel often only medical providers with access to all witnesses n Transporting family/witnesses with patient may help with treatment decisions at the hospital n
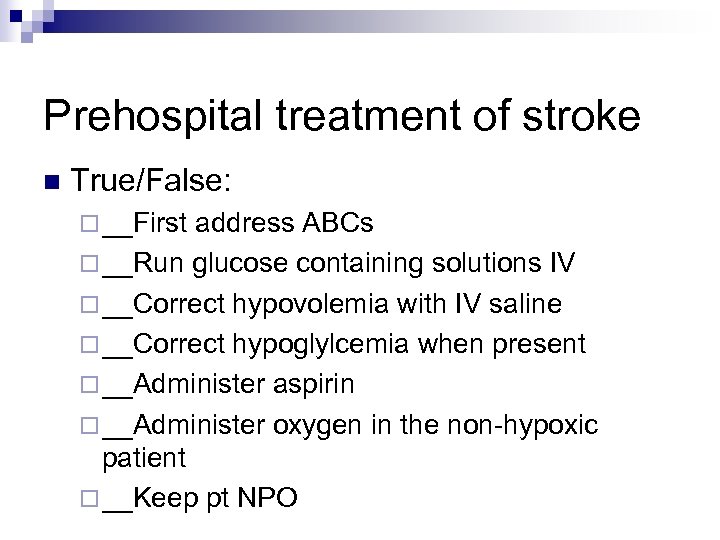 Prehospital treatment of stroke n True/False: ¨ __First address ABCs ¨ __Run glucose containing solutions IV ¨ __Correct hypovolemia with IV saline ¨ __Correct hypoglylcemia when present ¨ __Administer aspirin ¨ __Administer oxygen in the non-hypoxic patient ¨ __Keep pt NPO
Prehospital treatment of stroke n True/False: ¨ __First address ABCs ¨ __Run glucose containing solutions IV ¨ __Correct hypovolemia with IV saline ¨ __Correct hypoglylcemia when present ¨ __Administer aspirin ¨ __Administer oxygen in the non-hypoxic patient ¨ __Keep pt NPO
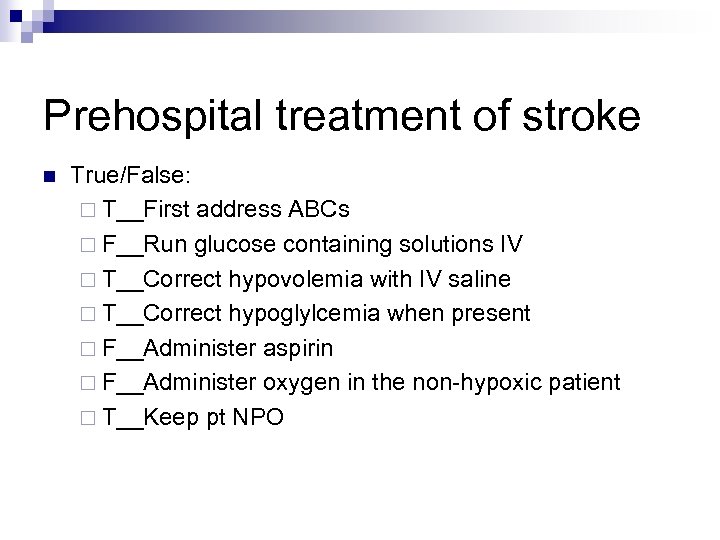 Prehospital treatment of stroke n True/False: ¨ T__First address ABCs ¨ F__Run glucose containing solutions IV ¨ T__Correct hypovolemia with IV saline ¨ T__Correct hypoglylcemia when present ¨ F__Administer aspirin ¨ F__Administer oxygen in the non-hypoxic patient ¨ T__Keep pt NPO
Prehospital treatment of stroke n True/False: ¨ T__First address ABCs ¨ F__Run glucose containing solutions IV ¨ T__Correct hypovolemia with IV saline ¨ T__Correct hypoglylcemia when present ¨ F__Administer aspirin ¨ F__Administer oxygen in the non-hypoxic patient ¨ T__Keep pt NPO
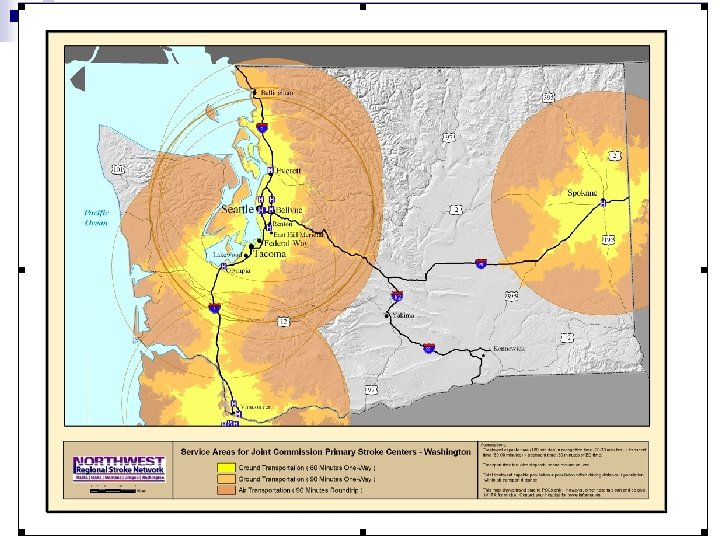
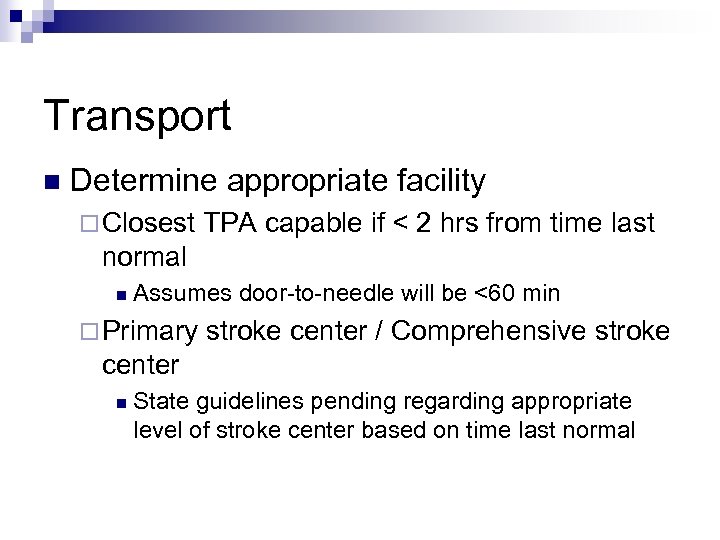 Transport n Determine appropriate facility ¨ Closest TPA capable if < 2 hrs from time last normal n Assumes door-to-needle will be <60 min ¨ Primary stroke center / Comprehensive stroke center n State guidelines pending regarding appropriate level of stroke center based on time last normal
Transport n Determine appropriate facility ¨ Closest TPA capable if < 2 hrs from time last normal n Assumes door-to-needle will be <60 min ¨ Primary stroke center / Comprehensive stroke center n State guidelines pending regarding appropriate level of stroke center based on time last normal
 Transport, cont. n Early hospital notification ¨ Confirm availability of CT ¨ Specify F. A. S. T findings n Consider air transport in remote areas ¨ EMS responders simultaneously call for air transport and prenotify ED at receiving stroke center in some systems
Transport, cont. n Early hospital notification ¨ Confirm availability of CT ¨ Specify F. A. S. T findings n Consider air transport in remote areas ¨ EMS responders simultaneously call for air transport and prenotify ED at receiving stroke center in some systems
 Management en route n Lay patient flat unless airway compromise ¨ Don’t n elevate head greater than 20 degrees IV access ¨ 16 or 18 gage if possible ¨ Avoid glucose containing solutions 2 nd exam/neuro reassess n Perform TPA check list n
Management en route n Lay patient flat unless airway compromise ¨ Don’t n elevate head greater than 20 degrees IV access ¨ 16 or 18 gage if possible ¨ Avoid glucose containing solutions 2 nd exam/neuro reassess n Perform TPA check list n
 What labs need to be sent on stroke TPA treatment candidates? CBC including platelets n Cardiac enzymes n Electrolytes, BUN, creatinine, glucose n PT/INR n PTT n
What labs need to be sent on stroke TPA treatment candidates? CBC including platelets n Cardiac enzymes n Electrolytes, BUN, creatinine, glucose n PT/INR n PTT n
 Name as many contraindications to t. PA as you can
Name as many contraindications to t. PA as you can
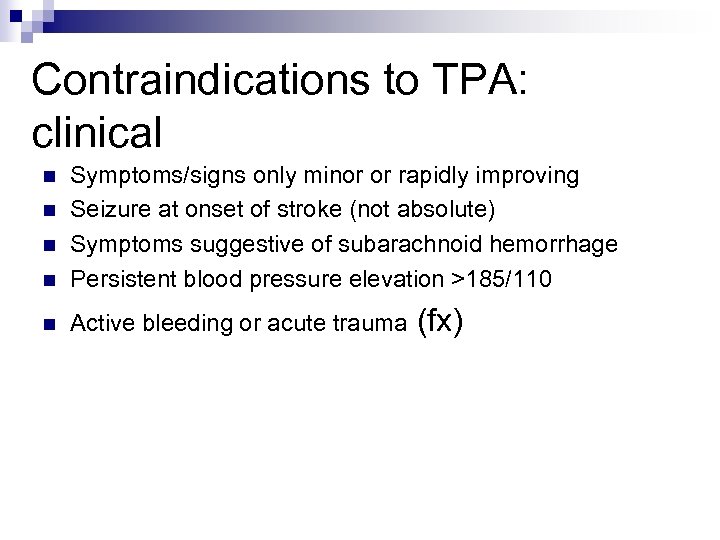 Contraindications to TPA: clinical n Symptoms/signs only minor or rapidly improving Seizure at onset of stroke (not absolute) Symptoms suggestive of subarachnoid hemorrhage Persistent blood pressure elevation >185/110 n Active bleeding or acute trauma n n n (fx)
Contraindications to TPA: clinical n Symptoms/signs only minor or rapidly improving Seizure at onset of stroke (not absolute) Symptoms suggestive of subarachnoid hemorrhage Persistent blood pressure elevation >185/110 n Active bleeding or acute trauma n n n (fx)
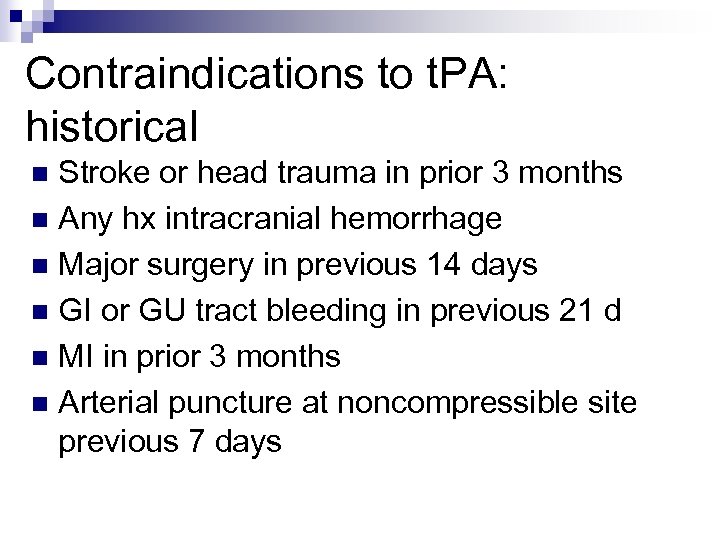 Contraindications to t. PA: historical Stroke or head trauma in prior 3 months n Any hx intracranial hemorrhage n Major surgery in previous 14 days n GI or GU tract bleeding in previous 21 d n MI in prior 3 months n Arterial puncture at noncompressible site previous 7 days n
Contraindications to t. PA: historical Stroke or head trauma in prior 3 months n Any hx intracranial hemorrhage n Major surgery in previous 14 days n GI or GU tract bleeding in previous 21 d n MI in prior 3 months n Arterial puncture at noncompressible site previous 7 days n
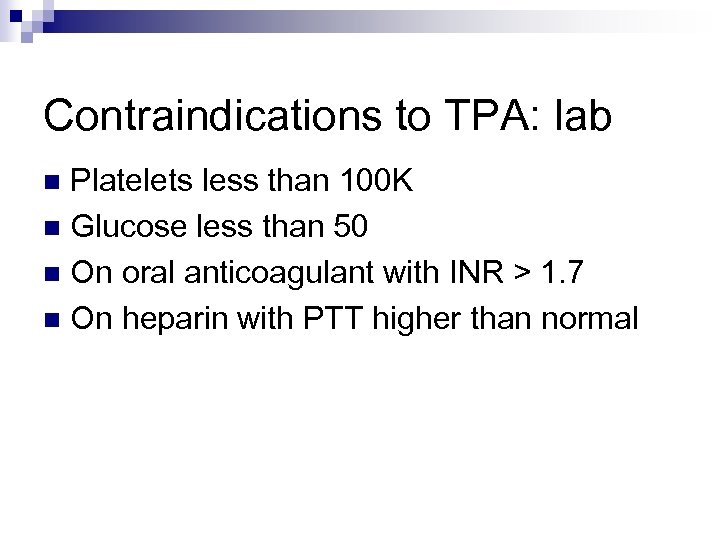 Contraindications to TPA: lab Platelets less than 100 K n Glucose less than 50 n On oral anticoagulant with INR > 1. 7 n On heparin with PTT higher than normal n
Contraindications to TPA: lab Platelets less than 100 K n Glucose less than 50 n On oral anticoagulant with INR > 1. 7 n On heparin with PTT higher than normal n
 Contraindications to TPA: CT Evidence of hemorrhage n Major early infarct signs (diffuse swelling of affected hemisphere, parenchymal hypodensity, and/or effacement of >33% of middle cerebral artery territory) n
Contraindications to TPA: CT Evidence of hemorrhage n Major early infarct signs (diffuse swelling of affected hemisphere, parenchymal hypodensity, and/or effacement of >33% of middle cerebral artery territory) n
 Telemedicine and telephone consultation n Several successful demonstrations published ¨ Technical issues with portable videoconferencing, transmittle of CT scans ¨ Financial issues: reimbursement ¨ Legal issues: liability
Telemedicine and telephone consultation n Several successful demonstrations published ¨ Technical issues with portable videoconferencing, transmittle of CT scans ¨ Financial issues: reimbursement ¨ Legal issues: liability
 Drip and Ship n Starting IV t-PA infusions for acute ischemic stroke at community hospitals prior to transfer to a regional stroke center is feasible and safe ¨ Several n demonstrations published Silva et al, ASA International Stroke Conference, February 2009, others
Drip and Ship n Starting IV t-PA infusions for acute ischemic stroke at community hospitals prior to transfer to a regional stroke center is feasible and safe ¨ Several n demonstrations published Silva et al, ASA International Stroke Conference, February 2009, others
 How often do vital signs need to be checked after the administration of rt-PA?
How often do vital signs need to be checked after the administration of rt-PA?
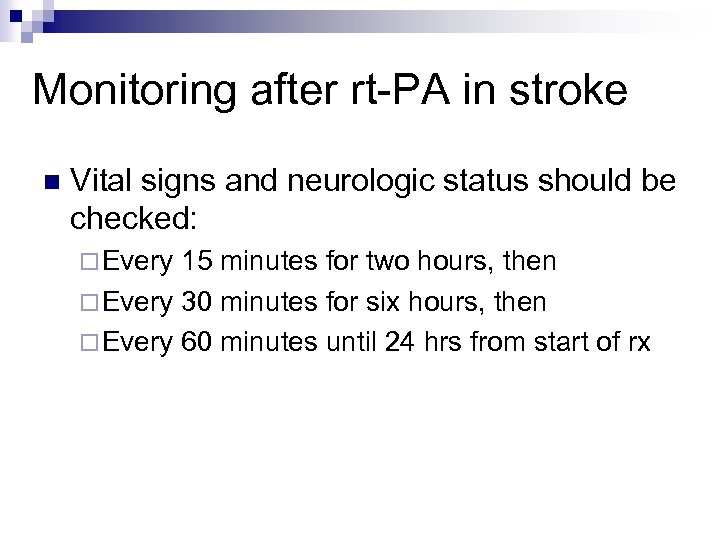 Monitoring after rt-PA in stroke n Vital signs and neurologic status should be checked: ¨ Every 15 minutes for two hours, then ¨ Every 30 minutes for six hours, then ¨ Every 60 minutes until 24 hrs from start of rx
Monitoring after rt-PA in stroke n Vital signs and neurologic status should be checked: ¨ Every 15 minutes for two hours, then ¨ Every 30 minutes for six hours, then ¨ Every 60 minutes until 24 hrs from start of rx
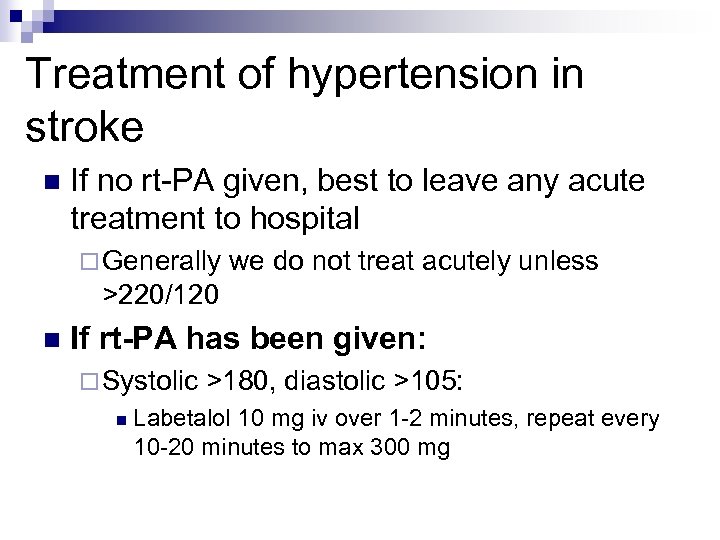 Treatment of hypertension in stroke n If no rt-PA given, best to leave any acute treatment to hospital ¨ Generally we do not treat acutely unless >220/120 n If rt-PA has been given: ¨ Systolic n >180, diastolic >105: Labetalol 10 mg iv over 1 -2 minutes, repeat every 10 -20 minutes to max 300 mg
Treatment of hypertension in stroke n If no rt-PA given, best to leave any acute treatment to hospital ¨ Generally we do not treat acutely unless >220/120 n If rt-PA has been given: ¨ Systolic n >180, diastolic >105: Labetalol 10 mg iv over 1 -2 minutes, repeat every 10 -20 minutes to max 300 mg
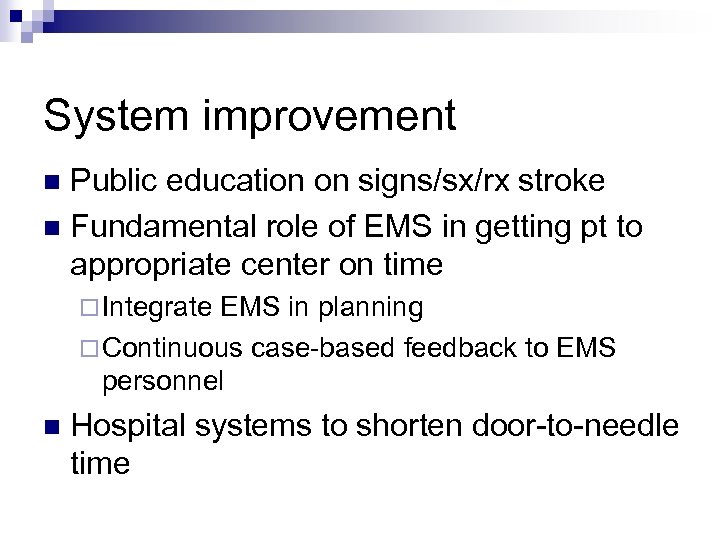 System improvement Public education on signs/sx/rx stroke n Fundamental role of EMS in getting pt to appropriate center on time n ¨ Integrate EMS in planning ¨ Continuous case-based feedback to EMS personnel n Hospital systems to shorten door-to-needle time
System improvement Public education on signs/sx/rx stroke n Fundamental role of EMS in getting pt to appropriate center on time n ¨ Integrate EMS in planning ¨ Continuous case-based feedback to EMS personnel n Hospital systems to shorten door-to-needle time
 Questions? n Q&A n Follow-up questions: ¨ Dr. n Hogness: cchogness@methownet. com Network questions & future trainings: ¨ Coordinator: chara. chamie@doh. wa. gov
Questions? n Q&A n Follow-up questions: ¨ Dr. n Hogness: cchogness@methownet. com Network questions & future trainings: ¨ Coordinator: chara. chamie@doh. wa. gov


