13728b6a35ec41690cf19d055ab0df1b.ppt
- Количество слайдов: 91
 RSPT 2335 Mechanical Ventilation Module E Discontinuation
RSPT 2335 Mechanical Ventilation Module E Discontinuation
 MODULE E Assignments n READ: n Pilbeam’s Mechanical Ventilation n n Chapter 20 & 21 (pp. 402 – 427 & 428 – 452) Egan References: n Chapter 47 (pp. 1199 - 1227)
MODULE E Assignments n READ: n Pilbeam’s Mechanical Ventilation n n Chapter 20 & 21 (pp. 402 – 427 & 428 – 452) Egan References: n Chapter 47 (pp. 1199 - 1227)
 MODULE E Assignments n Review: n n ACCP, AARC, ACCCM - Evidence Based Clinical Practice Guideline: Weaning and Discontinuing Ventilatory Support Homework: n Locate a copy of an actual ventilator weaning protocol at your work or clinical site.
MODULE E Assignments n Review: n n ACCP, AARC, ACCCM - Evidence Based Clinical Practice Guideline: Weaning and Discontinuing Ventilatory Support Homework: n Locate a copy of an actual ventilator weaning protocol at your work or clinical site.
 Optional Videotapes & DVDs n n n AARC PR 2005: Weaning Prolonged Mechanical Ventilation Patients in LTACHs (DVD) AARC PR 2004: Withholding and Withdrawing Life Support in the ICU AARC PR 2003: Weaning the Long Term Ventilator Dependent Patient AARC PR 2002: Transitioning the Ventilator Patient From the Hospital to Home AARC PR 2002: Talking With Patient’s and Families About Death and Dying Passy-Muir Tracheostomy & Ventilation Speaking Valves
Optional Videotapes & DVDs n n n AARC PR 2005: Weaning Prolonged Mechanical Ventilation Patients in LTACHs (DVD) AARC PR 2004: Withholding and Withdrawing Life Support in the ICU AARC PR 2003: Weaning the Long Term Ventilator Dependent Patient AARC PR 2002: Transitioning the Ventilator Patient From the Hospital to Home AARC PR 2002: Talking With Patient’s and Families About Death and Dying Passy-Muir Tracheostomy & Ventilation Speaking Valves
 MODULE E Objectives When you complete this module, you should be able to… n § § § List the different ways to wean from mechanical ventilation and explain which are the most commonly used methods. Explain the 12 guidelines as stated in the ACCP, AARC, ACCCM - Evidence Based Guidelines. Describe how to assess discontinuation potential.
MODULE E Objectives When you complete this module, you should be able to… n § § § List the different ways to wean from mechanical ventilation and explain which are the most commonly used methods. Explain the 12 guidelines as stated in the ACCP, AARC, ACCCM - Evidence Based Guidelines. Describe how to assess discontinuation potential.
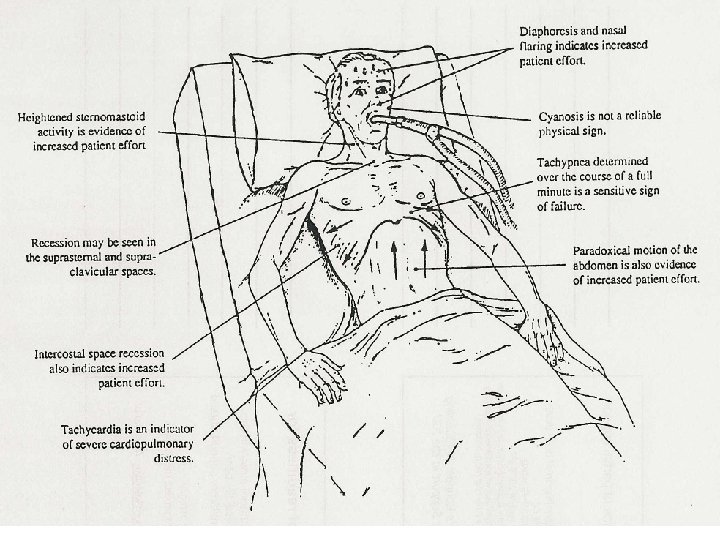
 MODULE E Objectives When you complete this module, you should be able to… n § § § Describe how to do a spontaneous breathing trial. Describe the signs of a patient in distress. Explain how to evaluate the objective and subjective signs of tolerance of a spontaneous breathing trial.
MODULE E Objectives When you complete this module, you should be able to… n § § § Describe how to do a spontaneous breathing trial. Describe the signs of a patient in distress. Explain how to evaluate the objective and subjective signs of tolerance of a spontaneous breathing trial.
 Objectives (continued) When you complete this module, you should be able to… n § § § Explain the process to follow if a patient fails a SBT. Describe the assessment recommended prior to extubation. Explain the present viewpoint on the use of weaning parameters.
Objectives (continued) When you complete this module, you should be able to… n § § § Explain the process to follow if a patient fails a SBT. Describe the assessment recommended prior to extubation. Explain the present viewpoint on the use of weaning parameters.
 Objectives (continued) When you complete this module, you should be able to… n § § § Explain the purpose of weaning protocols and how they work. Explain when tracheotomy should be considered. List the criteria for permanent ventilator dependence.
Objectives (continued) When you complete this module, you should be able to… n § § § Explain the purpose of weaning protocols and how they work. Explain when tracheotomy should be considered. List the criteria for permanent ventilator dependence.
 Objectives (continued) When you complete this module, you should be able to… n § § § Describe how to use a Passy Muir valve on a ventilator dependent patient. Explain the criteria for terminal weaning. List the different types of Advanced Directives.
Objectives (continued) When you complete this module, you should be able to… n § § § Describe how to use a Passy Muir valve on a ventilator dependent patient. Explain the criteria for terminal weaning. List the different types of Advanced Directives.
 Objectives (continued) When you complete this module, you should be able to… n § § § Explain the hierarchy for health care decision making and the role of the Durable Power of Attorney for health care. Explain the “Criteria for Determination of Brain Death. Describe the apnea testing procedure and why it is done.
Objectives (continued) When you complete this module, you should be able to… n § § § Explain the hierarchy for health care decision making and the role of the Durable Power of Attorney for health care. Explain the “Criteria for Determination of Brain Death. Describe the apnea testing procedure and why it is done.
 MODULE E Major Topics 1. 2. 3. Liberation from Ventilation & Weaning Parameters Evidence-Based Guidelines for Weaning and Discontinuing Ventilatory Support End of Life Issues
MODULE E Major Topics 1. 2. 3. Liberation from Ventilation & Weaning Parameters Evidence-Based Guidelines for Weaning and Discontinuing Ventilatory Support End of Life Issues
 Part 1 Liberation & Parameters
Part 1 Liberation & Parameters
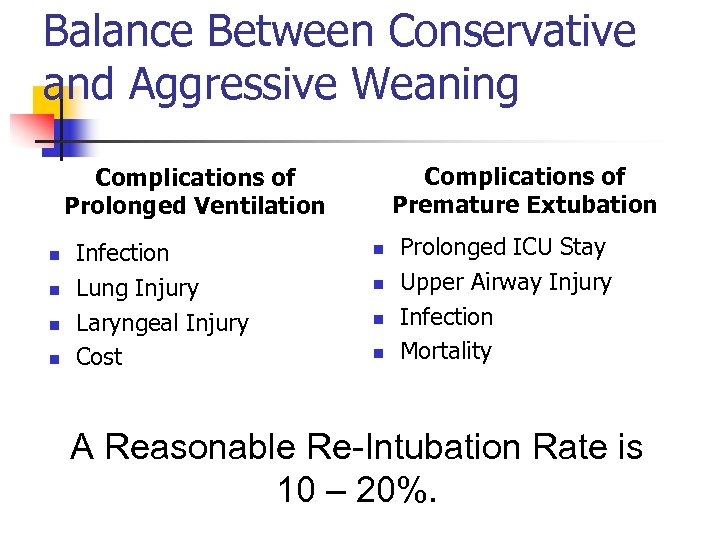 Balance Between Conservative and Aggressive Weaning Complications of Premature Extubation Complications of Prolonged Ventilation n n Infection Lung Injury Laryngeal Injury Cost n n Prolonged ICU Stay Upper Airway Injury Infection Mortality A Reasonable Re-Intubation Rate is 10 – 20%.
Balance Between Conservative and Aggressive Weaning Complications of Premature Extubation Complications of Prolonged Ventilation n n Infection Lung Injury Laryngeal Injury Cost n n Prolonged ICU Stay Upper Airway Injury Infection Mortality A Reasonable Re-Intubation Rate is 10 – 20%.
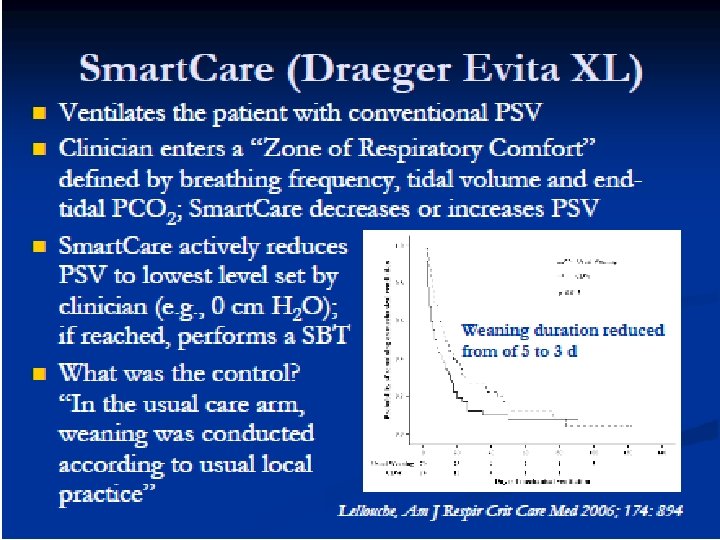
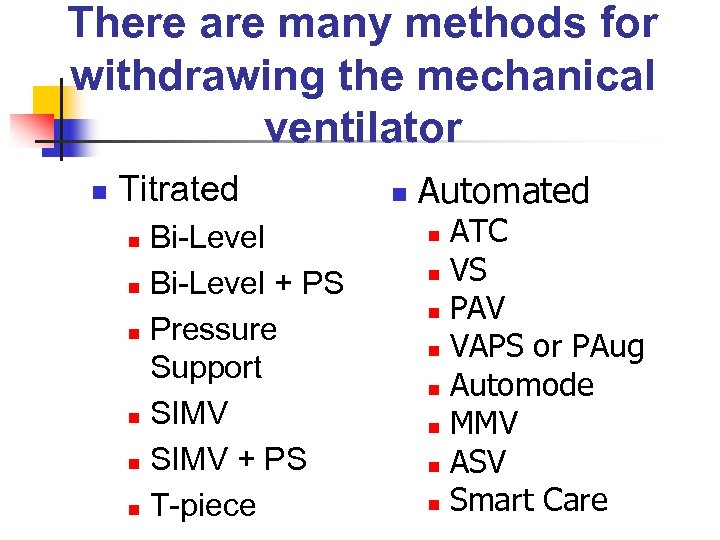 There are many methods for withdrawing the mechanical ventilator n Titrated Bi-Level n Bi-Level + PS n Pressure Support n SIMV + PS n T-piece n n Automated ATC n VS n PAV n VAPS or PAug n Automode n MMV n ASV n Smart Care n
There are many methods for withdrawing the mechanical ventilator n Titrated Bi-Level n Bi-Level + PS n Pressure Support n SIMV + PS n T-piece n n Automated ATC n VS n PAV n VAPS or PAug n Automode n MMV n ASV n Smart Care n
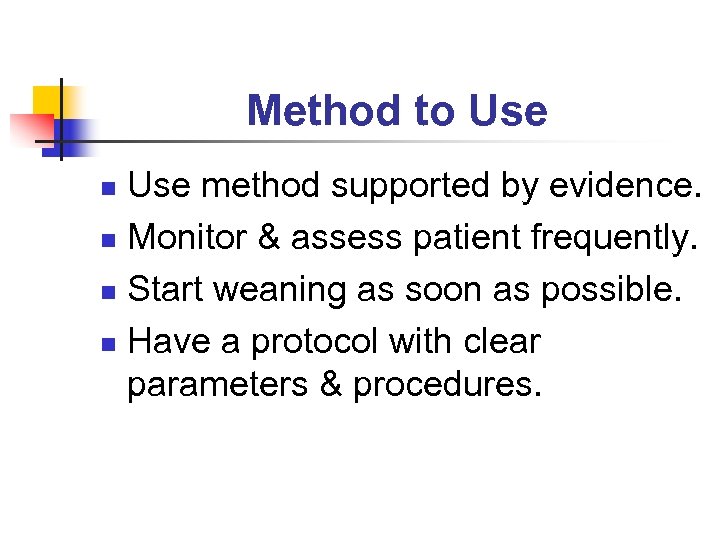 Method to Use method supported by evidence. n Monitor & assess patient frequently. n Start weaning as soon as possible. n Have a protocol with clear parameters & procedures. n
Method to Use method supported by evidence. n Monitor & assess patient frequently. n Start weaning as soon as possible. n Have a protocol with clear parameters & procedures. n
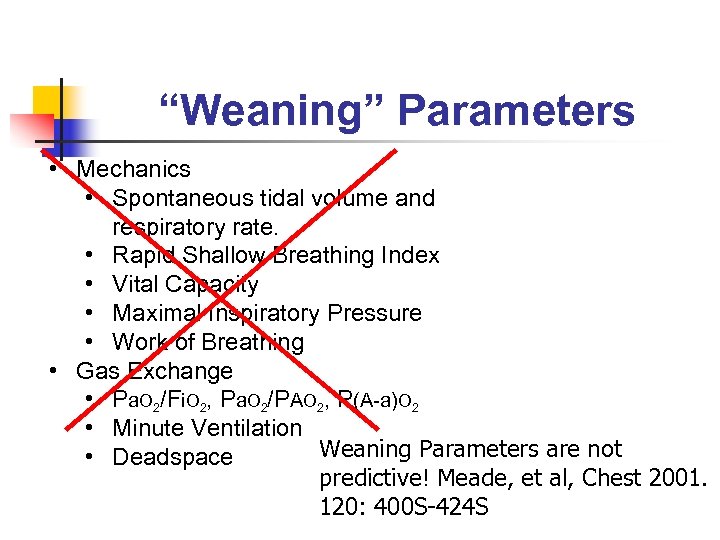 “Weaning” Parameters • Mechanics • Spontaneous tidal volume and respiratory rate. • Rapid Shallow Breathing Index • Vital Capacity • Maximal Inspiratory Pressure • Work of Breathing • Gas Exchange • Pa. O 2/Fi. O 2, Pa. O 2/PAO 2, P(A-a)O 2 • Minute Ventilation Weaning Parameters are not • Deadspace predictive! Meade, et al, Chest 2001. 120: 400 S-424 S
“Weaning” Parameters • Mechanics • Spontaneous tidal volume and respiratory rate. • Rapid Shallow Breathing Index • Vital Capacity • Maximal Inspiratory Pressure • Work of Breathing • Gas Exchange • Pa. O 2/Fi. O 2, Pa. O 2/PAO 2, P(A-a)O 2 • Minute Ventilation Weaning Parameters are not • Deadspace predictive! Meade, et al, Chest 2001. 120: 400 S-424 S
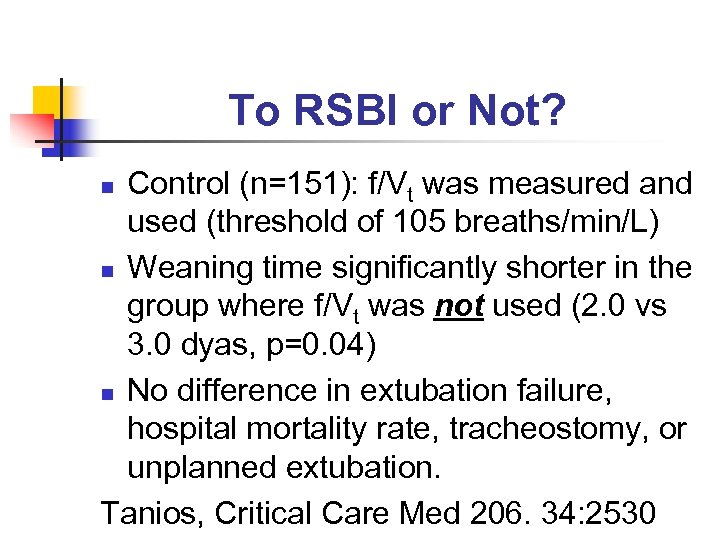 To RSBI or Not? Control (n=151): f/Vt was measured and used (threshold of 105 breaths/min/L) n Weaning time significantly shorter in the group where f/Vt was not used (2. 0 vs 3. 0 dyas, p=0. 04) n No difference in extubation failure, hospital mortality rate, tracheostomy, or unplanned extubation. Tanios, Critical Care Med 206. 34: 2530 n
To RSBI or Not? Control (n=151): f/Vt was measured and used (threshold of 105 breaths/min/L) n Weaning time significantly shorter in the group where f/Vt was not used (2. 0 vs 3. 0 dyas, p=0. 04) n No difference in extubation failure, hospital mortality rate, tracheostomy, or unplanned extubation. Tanios, Critical Care Med 206. 34: 2530 n
 Spontaneous Breath Trials n n n T-piece, PSV (7 cm H 2 O), Tube Compensation equally acceptable for SBT (Estaban et al, Am J Resp Crit Care Med 1997. 156: 459). Spontaneous breathing trial can be applied on ventilator (0/0 SBT) 30 minutes is adequate for spontaneous breathing trial (Esteban et al, Am J Respir Crit Care Med 1999. 159: 512). CPAP with 5 cm H 2 O can produce false positive trial with COPD and CHF. THE BEST WEANING PARAMETER IS A SPONTANEOUS BREATHING TRIAL.
Spontaneous Breath Trials n n n T-piece, PSV (7 cm H 2 O), Tube Compensation equally acceptable for SBT (Estaban et al, Am J Resp Crit Care Med 1997. 156: 459). Spontaneous breathing trial can be applied on ventilator (0/0 SBT) 30 minutes is adequate for spontaneous breathing trial (Esteban et al, Am J Respir Crit Care Med 1999. 159: 512). CPAP with 5 cm H 2 O can produce false positive trial with COPD and CHF. THE BEST WEANING PARAMETER IS A SPONTANEOUS BREATHING TRIAL.
 Weaning Parameters n n See Chart Provided n Wide variation between sources n Study “Pilbeam” column on chart (Table 20 -1 p. 412) Problems with weaning parameters n They are not reproducible or reliable if they are therapist dependent. n VC & MIP n Best parameters are patient driven. n R. S. B. I. n P 0. 1 n Spontaneous rate n Spontaneous tidal volume n Vital signs
Weaning Parameters n n See Chart Provided n Wide variation between sources n Study “Pilbeam” column on chart (Table 20 -1 p. 412) Problems with weaning parameters n They are not reproducible or reliable if they are therapist dependent. n VC & MIP n Best parameters are patient driven. n R. S. B. I. n P 0. 1 n Spontaneous rate n Spontaneous tidal volume n Vital signs
 Occlusion Pressure Measurements P 0. 1 s or P 100 n Occlude airways for first 100 msec and measure pressure. n Index of ventilatory drive. n Fast-twitch vs. slow-twitch fibers of diaphragm. n
Occlusion Pressure Measurements P 0. 1 s or P 100 n Occlude airways for first 100 msec and measure pressure. n Index of ventilatory drive. n Fast-twitch vs. slow-twitch fibers of diaphragm. n
 Pressure-Time Product n n n Comparison of transdiaphragmatic pressure and maximal inspiratory pressure. What percentage of the maximal inspiratory pressure is being used for a “normal” breath. Use of specialized esophageal catheter with two balloons positioned above & the diaphragm (Fig. 10 -25, p. 196).
Pressure-Time Product n n n Comparison of transdiaphragmatic pressure and maximal inspiratory pressure. What percentage of the maximal inspiratory pressure is being used for a “normal” breath. Use of specialized esophageal catheter with two balloons positioned above & the diaphragm (Fig. 10 -25, p. 196).
 Part 2 Evidence-Based Guidelines for Weaning and Discontinuing Ventilatory Support
Part 2 Evidence-Based Guidelines for Weaning and Discontinuing Ventilatory Support
 Reprinted in Respiratory Care 2002; 47(1): 69 -90)
Reprinted in Respiratory Care 2002; 47(1): 69 -90)
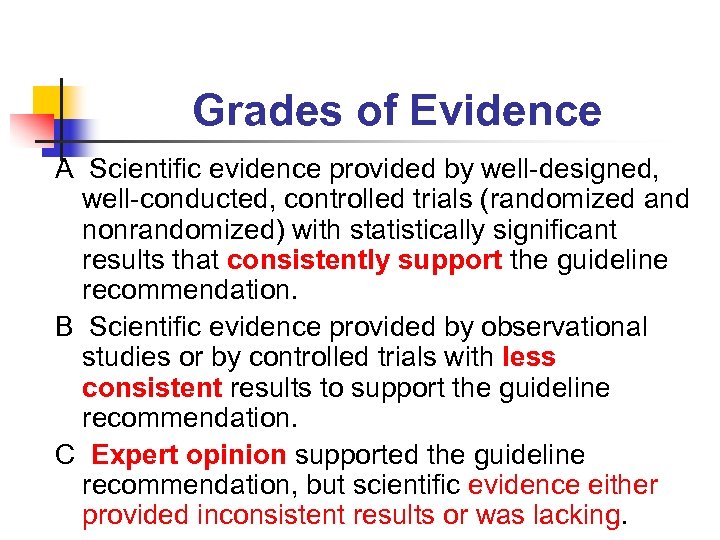 Grades of Evidence A Scientific evidence provided by well-designed, well-conducted, controlled trials (randomized and nonrandomized) with statistically significant results that consistently support the guideline recommendation. B Scientific evidence provided by observational studies or by controlled trials with less consistent results to support the guideline recommendation. C Expert opinion supported the guideline recommendation, but scientific evidence either provided inconsistent results or was lacking.
Grades of Evidence A Scientific evidence provided by well-designed, well-conducted, controlled trials (randomized and nonrandomized) with statistically significant results that consistently support the guideline recommendation. B Scientific evidence provided by observational studies or by controlled trials with less consistent results to support the guideline recommendation. C Expert opinion supported the guideline recommendation, but scientific evidence either provided inconsistent results or was lacking.
 Guideline 1 (Grade B) n n n In patients requiring mechanical ventilation for > 24 hours, a search for all the causes that may be contributing to ventilator dependence should be undertaken. This is particularly true in the patient who has failed attempts at withdrawing the mechanical ventilator. Reversing all possible ventilatory and nonventilatory issues should be an integral part of the ventilator discontinuation process.
Guideline 1 (Grade B) n n n In patients requiring mechanical ventilation for > 24 hours, a search for all the causes that may be contributing to ventilator dependence should be undertaken. This is particularly true in the patient who has failed attempts at withdrawing the mechanical ventilator. Reversing all possible ventilatory and nonventilatory issues should be an integral part of the ventilator discontinuation process.
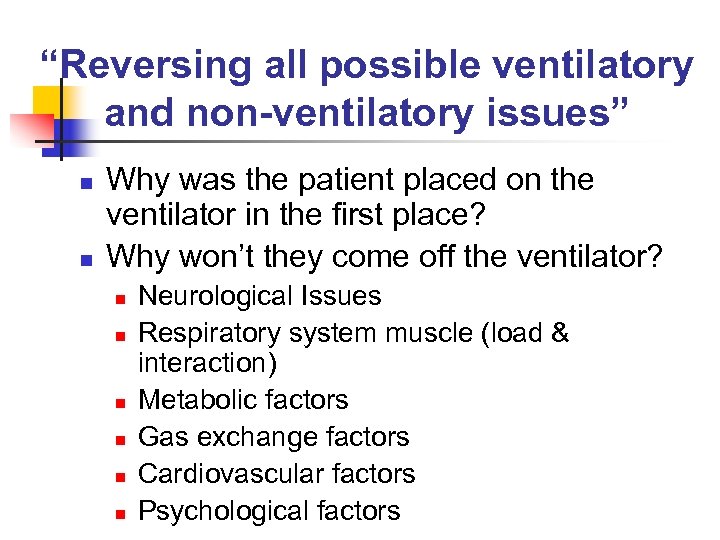 “Reversing all possible ventilatory and non-ventilatory issues” n n Why was the patient placed on the ventilator in the first place? Why won’t they come off the ventilator? n n n Neurological Issues Respiratory system muscle (load & interaction) Metabolic factors Gas exchange factors Cardiovascular factors Psychological factors
“Reversing all possible ventilatory and non-ventilatory issues” n n Why was the patient placed on the ventilator in the first place? Why won’t they come off the ventilator? n n n Neurological Issues Respiratory system muscle (load & interaction) Metabolic factors Gas exchange factors Cardiovascular factors Psychological factors
 Guideline 2 (Grade B) n Patients receiving mechanical ventilation for respiratory failure should undergo a formal assessment of discontinuation potential if the following criteria are satisfied:
Guideline 2 (Grade B) n Patients receiving mechanical ventilation for respiratory failure should undergo a formal assessment of discontinuation potential if the following criteria are satisfied:
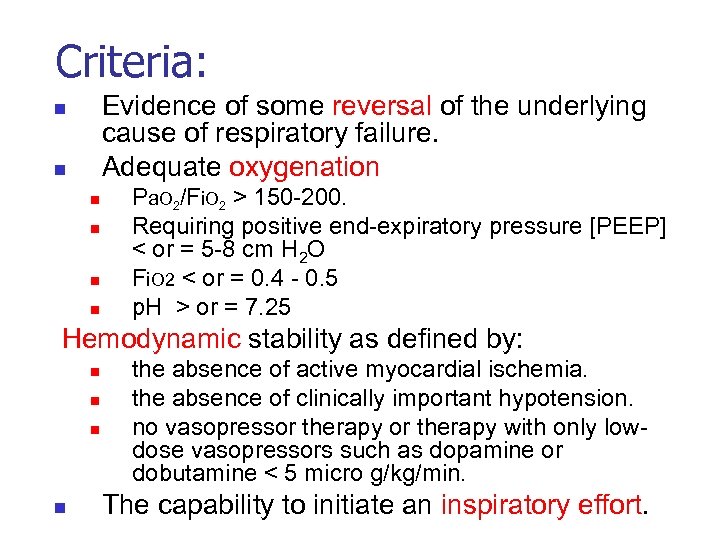 Criteria: Evidence of some reversal of the underlying cause of respiratory failure. Adequate oxygenation n n n Pa. O 2/Fi. O 2 > 150 -200. Requiring positive end-expiratory pressure [PEEP] < or = 5 -8 cm H 2 O Fi. O 2 < or = 0. 4 - 0. 5 p. H > or = 7. 25 Hemodynamic stability as defined by: n n the absence of active myocardial ischemia. the absence of clinically important hypotension. no vasopressor therapy with only lowdose vasopressors such as dopamine or dobutamine < 5 micro g/kg/min. The capability to initiate an inspiratory effort.
Criteria: Evidence of some reversal of the underlying cause of respiratory failure. Adequate oxygenation n n n Pa. O 2/Fi. O 2 > 150 -200. Requiring positive end-expiratory pressure [PEEP] < or = 5 -8 cm H 2 O Fi. O 2 < or = 0. 4 - 0. 5 p. H > or = 7. 25 Hemodynamic stability as defined by: n n the absence of active myocardial ischemia. the absence of clinically important hypotension. no vasopressor therapy with only lowdose vasopressors such as dopamine or dobutamine < 5 micro g/kg/min. The capability to initiate an inspiratory effort.
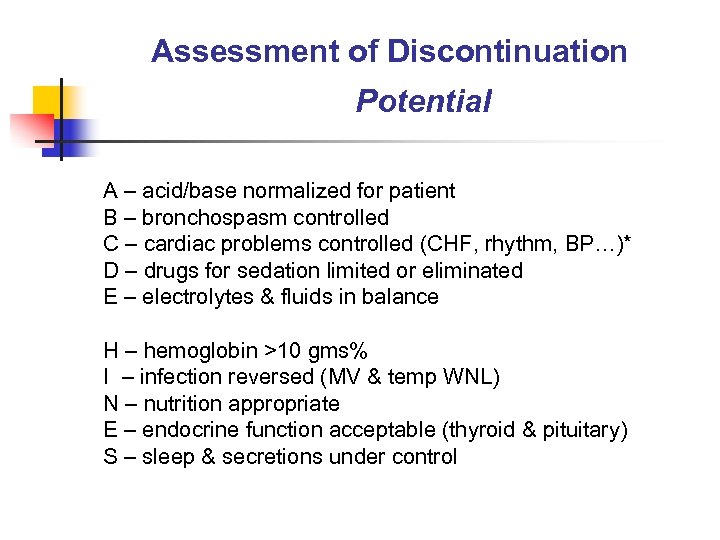 Assessment of Discontinuation Potential A – acid/base normalized for patient B – bronchospasm controlled C – cardiac problems controlled (CHF, rhythm, BP…)* D – drugs for sedation limited or eliminated E – electrolytes & fluids in balance H – hemoglobin >10 gms% I – infection reversed (MV & temp WNL) N – nutrition appropriate E – endocrine function acceptable (thyroid & pituitary) S – sleep & secretions under control
Assessment of Discontinuation Potential A – acid/base normalized for patient B – bronchospasm controlled C – cardiac problems controlled (CHF, rhythm, BP…)* D – drugs for sedation limited or eliminated E – electrolytes & fluids in balance H – hemoglobin >10 gms% I – infection reversed (MV & temp WNL) N – nutrition appropriate E – endocrine function acceptable (thyroid & pituitary) S – sleep & secretions under control
 Guideline 3 (Grade A) n Formal discontinuation assessments for patients receiving mechanical ventilation for respiratory failure should be done during spontaneous breathing rather than while the patient is still receiving substantial ventilatory support. n An initial brief period of spontaneous breathing can be used to assess the capability of continuing onto a formal SBT.
Guideline 3 (Grade A) n Formal discontinuation assessments for patients receiving mechanical ventilation for respiratory failure should be done during spontaneous breathing rather than while the patient is still receiving substantial ventilatory support. n An initial brief period of spontaneous breathing can be used to assess the capability of continuing onto a formal SBT.
 Spontaneous breathing trial (SBT) n Most patients on ventilators do not require formal “weaning”. The tolerance of a formal SBT for 30 – 120 minutes should prompt consideration for permanent ventilator discontinuation. n Studies have shown a 77% weaning success rate with this criteria. n
Spontaneous breathing trial (SBT) n Most patients on ventilators do not require formal “weaning”. The tolerance of a formal SBT for 30 – 120 minutes should prompt consideration for permanent ventilator discontinuation. n Studies have shown a 77% weaning success rate with this criteria. n
 Methods for performing a spontaneous breathing trial (SBT) Low level Pressure Support (5 -7 cm H 2 O) with or without PEEP. n Automated Tube Compensation with or without PEEP. n T-bar (no alarms, more equipment, high Raw). n
Methods for performing a spontaneous breathing trial (SBT) Low level Pressure Support (5 -7 cm H 2 O) with or without PEEP. n Automated Tube Compensation with or without PEEP. n T-bar (no alarms, more equipment, high Raw). n
 Comparison of Weaning Methods n Brochard, Am J Respir Crit Care Med 1994. 150: 896. n n n Patients screened for weaning readiness. T-piece trial for 2 hours; ~75% tolerated and extubated. Greatest success for PSV (worst for SIMV)
Comparison of Weaning Methods n Brochard, Am J Respir Crit Care Med 1994. 150: 896. n n n Patients screened for weaning readiness. T-piece trial for 2 hours; ~75% tolerated and extubated. Greatest success for PSV (worst for SIMV)
 Automatic Tube Compensation: Do We Need It? n n Does not compensate for changes in resistance that occur in vivo; e. g. kinking or secretions. Estaban, Am J Respir Crit Care Med 1997. 156: 459 n n Straus, Am J Respir Crit Care Med 1998; 157: 23 n n PSV or T-piece acceptable for SBTs. Spontaneous breathing through ET tube mimics work of breathing after extubation. Haberthur, Acta Anaesthesiol Scan 2002. 46: 973 n No difference in patient tolerance of SBT between patients randomized to TC, PSV of 5 cm H 2 O or T-piece.
Automatic Tube Compensation: Do We Need It? n n Does not compensate for changes in resistance that occur in vivo; e. g. kinking or secretions. Estaban, Am J Respir Crit Care Med 1997. 156: 459 n n Straus, Am J Respir Crit Care Med 1998; 157: 23 n n PSV or T-piece acceptable for SBTs. Spontaneous breathing through ET tube mimics work of breathing after extubation. Haberthur, Acta Anaesthesiol Scan 2002. 46: 973 n No difference in patient tolerance of SBT between patients randomized to TC, PSV of 5 cm H 2 O or T-piece.
 Formal Discontinuation Assessment Respiratory pattern n Adequacy of gas exchange n Hemodynamic stability n Subjective comfort n
Formal Discontinuation Assessment Respiratory pattern n Adequacy of gas exchange n Hemodynamic stability n Subjective comfort n
 Formal Discontinuation Assessment n n Are respiratory muscles capable of sustaining spontaneous breathing? Ventilatory pattern f 50% n n No increased work of breathing Use of accessory muscles n Thoracoabdominal paradox n
Formal Discontinuation Assessment n n Are respiratory muscles capable of sustaining spontaneous breathing? Ventilatory pattern f 50% n n No increased work of breathing Use of accessory muscles n Thoracoabdominal paradox n
 Assessment of Discontinuation Potential n Are there conditions that can contribute to respiratory muscle fatigue? n n n n Hyperinflation Malnutrition Hypoxemia Acidosis Electrolyte imbalance Endocrine disorders Drugs (paralytics & steroid combos) Neuromuscular problems
Assessment of Discontinuation Potential n Are there conditions that can contribute to respiratory muscle fatigue? n n n n Hyperinflation Malnutrition Hypoxemia Acidosis Electrolyte imbalance Endocrine disorders Drugs (paralytics & steroid combos) Neuromuscular problems
 Objective Measures Indicating Tolerance n Gas exchange n n n Sp. O 2 >/= 85 – 90% Pa. O 2 50 – 60 mm. Hg p. H >/= 7. 32 Pa. CO 2 increase no more than 10 mm. Hg. Hemodynamics n n n HR < 120 – 140 HR change <20% No vasopressors required.
Objective Measures Indicating Tolerance n Gas exchange n n n Sp. O 2 >/= 85 – 90% Pa. O 2 50 – 60 mm. Hg p. H >/= 7. 32 Pa. CO 2 increase no more than 10 mm. Hg. Hemodynamics n n n HR < 120 – 140 HR change <20% No vasopressors required.
 Subjective Measures Indicating Tolerance n Mental state n No somnolence, coma, agitation, anxiety. No onset or worsening discomfort or dyspnea. n No diaphoresis. n
Subjective Measures Indicating Tolerance n Mental state n No somnolence, coma, agitation, anxiety. No onset or worsening discomfort or dyspnea. n No diaphoresis. n
 Guideline 4 (Grade C) n The removal of the artificial airway from a patient who has successfully been discontinued from ventilatory support should be based on assessments of airway patency and the ability of the patient to protect the airway.
Guideline 4 (Grade C) n The removal of the artificial airway from a patient who has successfully been discontinued from ventilatory support should be based on assessments of airway patency and the ability of the patient to protect the airway.
 Reference Material n AARC – Clinical Practice Guideline n Removal of the Endotracheal Tube – 2007 Revision & Update
Reference Material n AARC – Clinical Practice Guideline n Removal of the Endotracheal Tube – 2007 Revision & Update
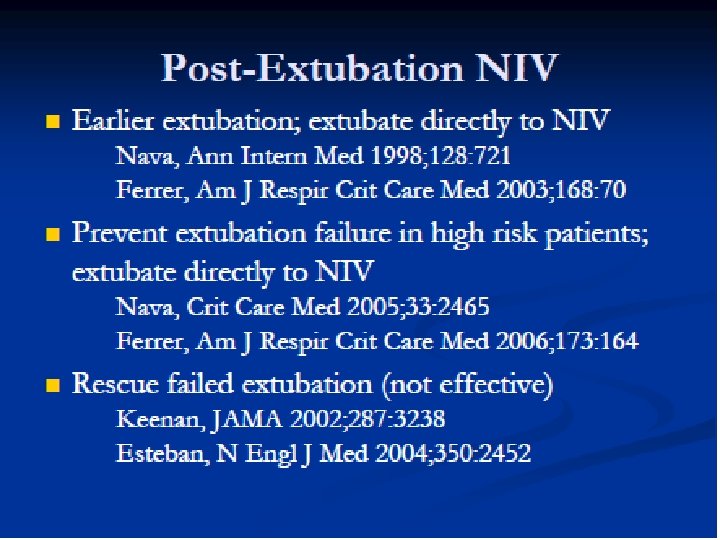
 Extubation n REMEMBER: Weaning from ventilatory support does not mean the patient is ready for extubation. n Assessments of airway patency Review history n Do cuff leak test n n Assessment of ability of the patient to protect the airway Amount of secretions n Ability to cough & gag n Level of consciousness n
Extubation n REMEMBER: Weaning from ventilatory support does not mean the patient is ready for extubation. n Assessments of airway patency Review history n Do cuff leak test n n Assessment of ability of the patient to protect the airway Amount of secretions n Ability to cough & gag n Level of consciousness n
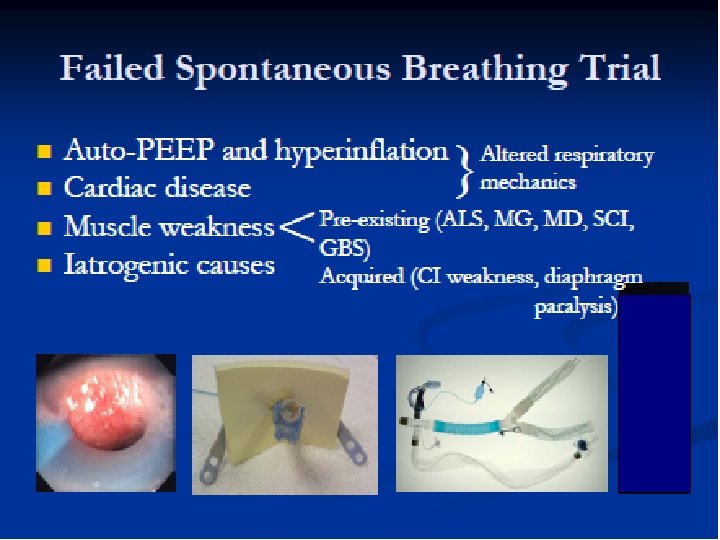
 Guideline 5 (Grade A) Patients receiving mechanical ventilation for respiratory failure who fail an SBT should have the cause for the failed SBT determined. n Once reversible causes for failure are corrected, and if the patient still meets the criteria, subsequent SBTs should be performed every 24 hours. n
Guideline 5 (Grade A) Patients receiving mechanical ventilation for respiratory failure who fail an SBT should have the cause for the failed SBT determined. n Once reversible causes for failure are corrected, and if the patient still meets the criteria, subsequent SBTs should be performed every 24 hours. n
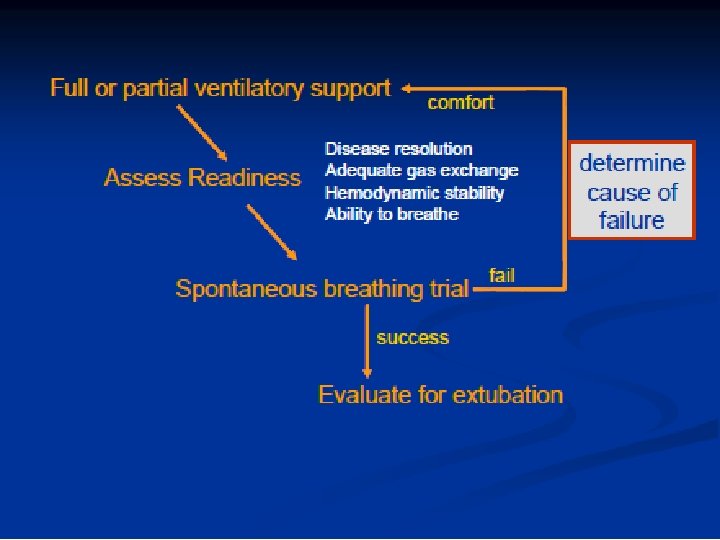
 Guideline 6 (Grade B) n Patients receiving mechanical ventilation for respiratory failure who fail an SBT should receive a stable, non-fatiguing, comfortable form of ventilatory support.
Guideline 6 (Grade B) n Patients receiving mechanical ventilation for respiratory failure who fail an SBT should receive a stable, non-fatiguing, comfortable form of ventilatory support.
 Guideline 7 (Grade A) n Anesthesia/sedation strategies and ventilator management aimed at early extubation should be used in postsurgical patients.
Guideline 7 (Grade A) n Anesthesia/sedation strategies and ventilator management aimed at early extubation should be used in postsurgical patients.
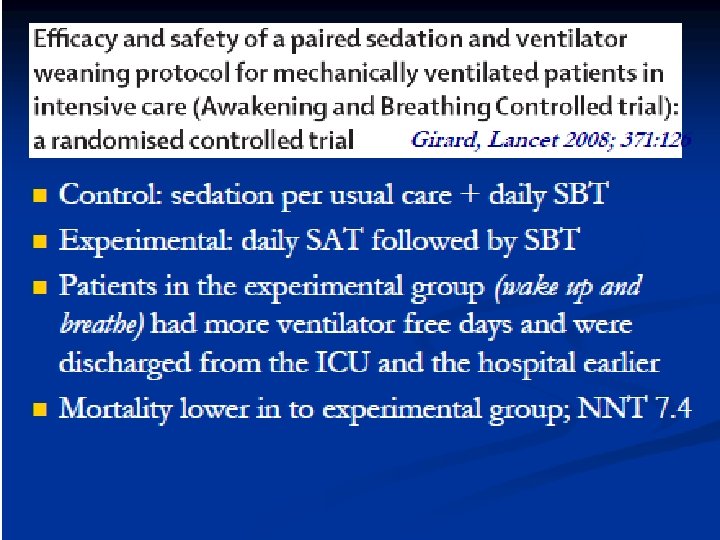
 Guideline 8 (Grade A) Weaning/discontinuation protocols designed for non-physician health care professionals (HCPs) should be developed and implemented by ICUs. n Protocols aimed at optimizing sedation should also be developed and implemented. n
Guideline 8 (Grade A) Weaning/discontinuation protocols designed for non-physician health care professionals (HCPs) should be developed and implemented by ICUs. n Protocols aimed at optimizing sedation should also be developed and implemented. n
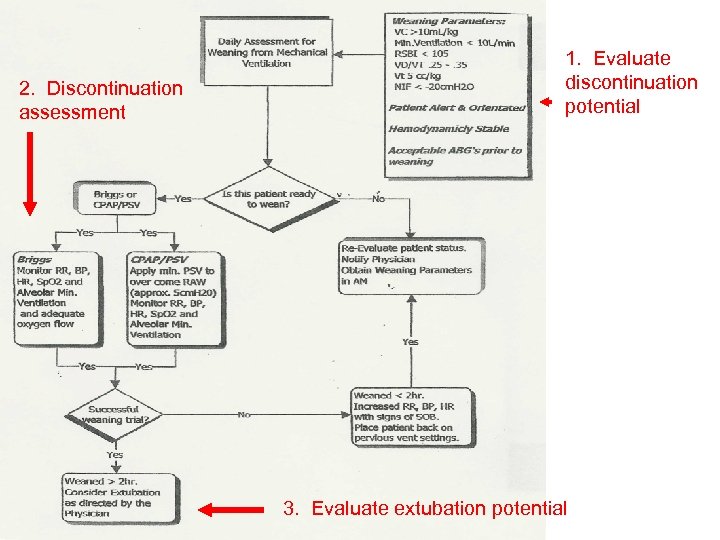 2. Discontinuation assessment 1. Evaluate discontinuation potential 3. Evaluate extubation potential
2. Discontinuation assessment 1. Evaluate discontinuation potential 3. Evaluate extubation potential
 Guideline 9 (Grade B) n n Tracheotomy should be considered after an initial period of stabilization on the ventilator when it becomes apparent that the patient will require prolonged ventilator assistance. Tracheotomy should then be performed when the patient appears likely to gain one or more of the benefits ascribed to the procedure.
Guideline 9 (Grade B) n n Tracheotomy should be considered after an initial period of stabilization on the ventilator when it becomes apparent that the patient will require prolonged ventilator assistance. Tracheotomy should then be performed when the patient appears likely to gain one or more of the benefits ascribed to the procedure.
 Patients who may derive particular benefit from early tracheotomy are the following: n Those requiring high levels of sedation to tolerate translaryngeal tubes. n Those with marginal respiratory mechanics (often manifested as tachypnea) in whom a tracheostomy tube having lower resistance might reduce the risk of muscle overload. n Those who may derive psychological benefit from the ability to eat orally, communicate by articulated speech, and experience enhanced mobility; and n Those in whom enhanced mobility may assist physical therapy efforts.
Patients who may derive particular benefit from early tracheotomy are the following: n Those requiring high levels of sedation to tolerate translaryngeal tubes. n Those with marginal respiratory mechanics (often manifested as tachypnea) in whom a tracheostomy tube having lower resistance might reduce the risk of muscle overload. n Those who may derive psychological benefit from the ability to eat orally, communicate by articulated speech, and experience enhanced mobility; and n Those in whom enhanced mobility may assist physical therapy efforts.
 Guideline 10 (Grade B) n Unless there is evidence for clearly irreversible disease (e. g. , high spinal cord injury or advanced amyotrophic lateral sclerosis), a patient requiring prolonged mechanical ventilatory support for respiratory failure should not be considered permanently ventilator dependent until 3 months of weaning attempts have failed.
Guideline 10 (Grade B) n Unless there is evidence for clearly irreversible disease (e. g. , high spinal cord injury or advanced amyotrophic lateral sclerosis), a patient requiring prolonged mechanical ventilatory support for respiratory failure should not be considered permanently ventilator dependent until 3 months of weaning attempts have failed.
 Permanently Ventilator Dependent Examples: n Irreversible diseases: n n High spinal cord injury Advanced amyotropic lateral sclerosis (ALS) Polio & postpolio sequelae Incurable diseases n n n COPD Kyphoscoliosis Pulmonary Fibrosis
Permanently Ventilator Dependent Examples: n Irreversible diseases: n n High spinal cord injury Advanced amyotropic lateral sclerosis (ALS) Polio & postpolio sequelae Incurable diseases n n n COPD Kyphoscoliosis Pulmonary Fibrosis
 Guideline 11 (Grade C) n Critical-care practitioners should familiarize themselves with facilities in their communities, or units in hospitals they staff, that specialize in managing patients who require prolonged dependence on mechanical ventilation. n n Such familiarization should include reviewing published peer-reviewed data from those units, if available. When medically stable for transfer, patients who have failed ventilator discontinuation attempts in the ICU should be transferred to those facilities that have demonstrated success and safety in accomplishing ventilator discontinuation.
Guideline 11 (Grade C) n Critical-care practitioners should familiarize themselves with facilities in their communities, or units in hospitals they staff, that specialize in managing patients who require prolonged dependence on mechanical ventilation. n n Such familiarization should include reviewing published peer-reviewed data from those units, if available. When medically stable for transfer, patients who have failed ventilator discontinuation attempts in the ICU should be transferred to those facilities that have demonstrated success and safety in accomplishing ventilator discontinuation.
 Guideline 12 (Grade C) n Weaning strategy in the permanent mechanical ventilator patient should be slow-paced and should include gradually lengthening self-breathing trials.
Guideline 12 (Grade C) n Weaning strategy in the permanent mechanical ventilator patient should be slow-paced and should include gradually lengthening self-breathing trials.
 Prolonged Mechanical Ventilator (PMV) patient n Consider use of Passy-Muir Valve Use slow paced trials n Gradually increase self-breathing trials n Often used when partial support ventilation is providing ½ the support needed by the patient n Awake, alert, stable patient able to manage secretions n
Prolonged Mechanical Ventilator (PMV) patient n Consider use of Passy-Muir Valve Use slow paced trials n Gradually increase self-breathing trials n Often used when partial support ventilation is providing ½ the support needed by the patient n Awake, alert, stable patient able to manage secretions n
 Part 3 End of Life Issues
Part 3 End of Life Issues
 Advanced Directives n n Legal documents – written, signed, witnessed and notarized Examples: n n n Living Will - Gives health care providers guidelines regarding the wishes of the patient in the event that the patient is no longer of sound mind and cannot make decisions regarding his care. “Do Not Resuscitate” order (DNR) – Provides guidance when the heart stops or the patient stops breathing. “Chemical Code Only” “Do Not Intubate” “Do Not Shock” “Withhold Nutrition & Hydration” (consult state law)
Advanced Directives n n Legal documents – written, signed, witnessed and notarized Examples: n n n Living Will - Gives health care providers guidelines regarding the wishes of the patient in the event that the patient is no longer of sound mind and cannot make decisions regarding his care. “Do Not Resuscitate” order (DNR) – Provides guidance when the heart stops or the patient stops breathing. “Chemical Code Only” “Do Not Intubate” “Do Not Shock” “Withhold Nutrition & Hydration” (consult state law)
 Durable Power of Attorney (DPA) for Health Care Decisions n n Person designated to make health care decisions for the patient should the patient become incapacitated. If person not designated the law recognizes hierarchy of relationships n n n Parents or legal guardian of minor Durable Power of Attorney Spouse Adult children (all must agree) Parents of patient Adult siblings (all must agree)
Durable Power of Attorney (DPA) for Health Care Decisions n n Person designated to make health care decisions for the patient should the patient become incapacitated. If person not designated the law recognizes hierarchy of relationships n n n Parents or legal guardian of minor Durable Power of Attorney Spouse Adult children (all must agree) Parents of patient Adult siblings (all must agree)
 Sustaining vs. Comfort Care n Terminally ill patients should be made as comfortable as possible (palliative care). n n Observe for agitation and grimacing. Use adequate doses of sedatives & analgesics. n Excessive dosing to hasten death in not allowed (causing apnea or cardiac arrest). n n n Allow open family visitation if possible. Minimize monitoring & alarms. Stop testing (labs, x-rays…).
Sustaining vs. Comfort Care n Terminally ill patients should be made as comfortable as possible (palliative care). n n Observe for agitation and grimacing. Use adequate doses of sedatives & analgesics. n Excessive dosing to hasten death in not allowed (causing apnea or cardiac arrest). n n n Allow open family visitation if possible. Minimize monitoring & alarms. Stop testing (labs, x-rays…).
 End of Life Issues Criteria for Terminal Weaning: 1. 2. Patient’s informed consent. Medical futility (in last 100 cases, treatments were useless). 3. Reduction of pain and suffering.
End of Life Issues Criteria for Terminal Weaning: 1. 2. Patient’s informed consent. Medical futility (in last 100 cases, treatments were useless). 3. Reduction of pain and suffering.
 End of Life Issues n Handouts: Brain Death Criteria n Apnea Testing Procedure n
End of Life Issues n Handouts: Brain Death Criteria n Apnea Testing Procedure n
 End of Life Issues Criteria for Determination of Brain Death: n n n No hypothermia. No purposeful movement to stimulation. Absence of brain stem reflexes. n n n Pupils fixed. No corneal reflex. No cough or gag. Absence of doll’s eyes. No toxins or drug effects. Apnea Testing or Negative Brain Flow Study.
End of Life Issues Criteria for Determination of Brain Death: n n n No hypothermia. No purposeful movement to stimulation. Absence of brain stem reflexes. n n n Pupils fixed. No corneal reflex. No cough or gag. Absence of doll’s eyes. No toxins or drug effects. Apnea Testing or Negative Brain Flow Study.
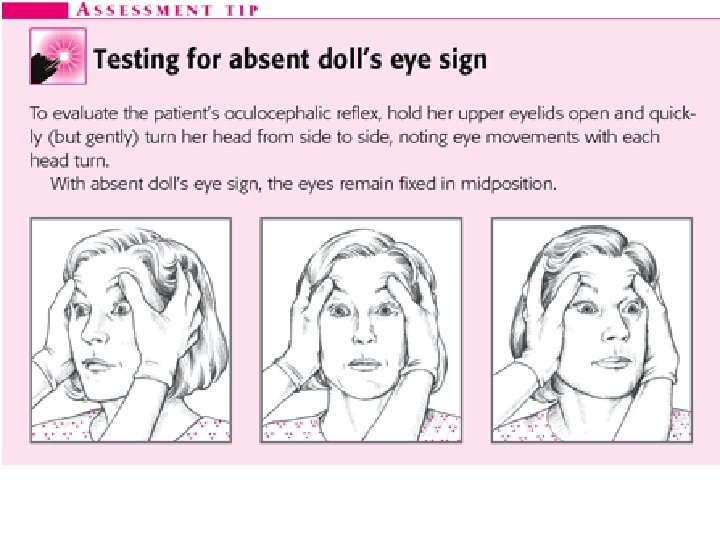
 Doll’s Eye Sign n n An indicator of brain stem dysfunction, the absence of the doll's eye sign is detected by rapid, gentle turning of the patient's head from side to side. The eyes remain fixed in midposition, instead of the normal response of moving laterally toward the side opposite the direction the head is turned.
Doll’s Eye Sign n n An indicator of brain stem dysfunction, the absence of the doll's eye sign is detected by rapid, gentle turning of the patient's head from side to side. The eyes remain fixed in midposition, instead of the normal response of moving laterally toward the side opposite the direction the head is turned.
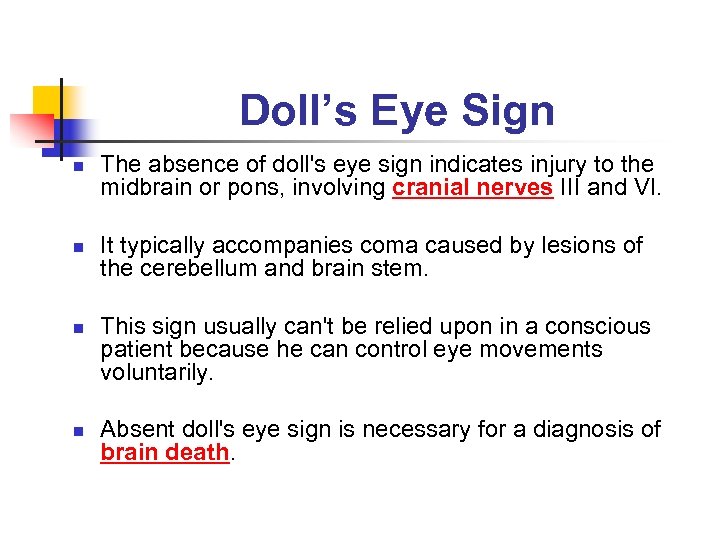 Doll’s Eye Sign n n The absence of doll's eye sign indicates injury to the midbrain or pons, involving cranial nerves III and VI. It typically accompanies coma caused by lesions of the cerebellum and brain stem. This sign usually can't be relied upon in a conscious patient because he can control eye movements voluntarily. Absent doll's eye sign is necessary for a diagnosis of brain death.
Doll’s Eye Sign n n The absence of doll's eye sign indicates injury to the midbrain or pons, involving cranial nerves III and VI. It typically accompanies coma caused by lesions of the cerebellum and brain stem. This sign usually can't be relied upon in a conscious patient because he can control eye movements voluntarily. Absent doll's eye sign is necessary for a diagnosis of brain death.
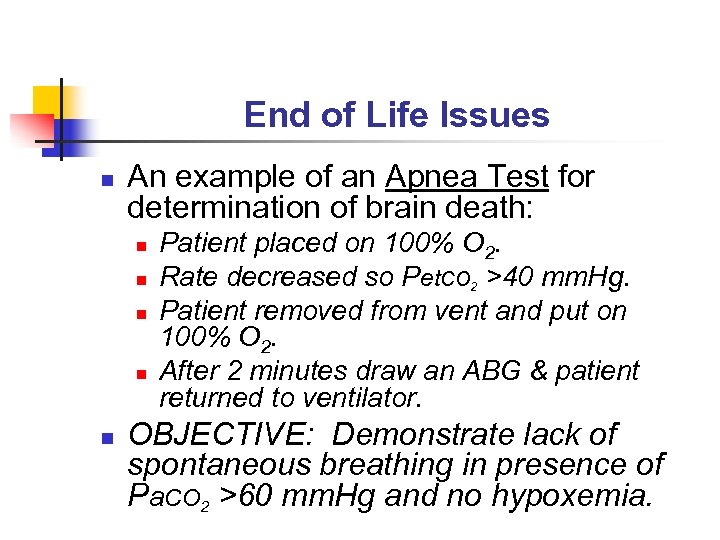 End of Life Issues n An example of an Apnea Test for determination of brain death: n n n Patient placed on 100% O 2. Rate decreased so Pet. CO 2 >40 mm. Hg. Patient removed from vent and put on 100% O 2. After 2 minutes draw an ABG & patient returned to ventilator. OBJECTIVE: Demonstrate lack of spontaneous breathing in presence of Pa. CO 2 >60 mm. Hg and no hypoxemia.
End of Life Issues n An example of an Apnea Test for determination of brain death: n n n Patient placed on 100% O 2. Rate decreased so Pet. CO 2 >40 mm. Hg. Patient removed from vent and put on 100% O 2. After 2 minutes draw an ABG & patient returned to ventilator. OBJECTIVE: Demonstrate lack of spontaneous breathing in presence of Pa. CO 2 >60 mm. Hg and no hypoxemia.
 Protocols n Homework Assignment: n Get a copy of the ventilator weaning protocol from the institution where you work or are doing your clinical rotation.
Protocols n Homework Assignment: n Get a copy of the ventilator weaning protocol from the institution where you work or are doing your clinical rotation.
 LONG-TERM VENTILATION & TRANSPORT
LONG-TERM VENTILATION & TRANSPORT
 Objectives n n n State the goals of mechanical ventilation in an alternate environment. Name the factors used to estimate the cost of home mechanical ventilation. Describe facilities used for long-term mechanical ventilation. Compare the criteria for discharging a child versus discharging an adult who is ventilator dependent. Describe other forms of ventilation for the long-term ventilator dependent patient.
Objectives n n n State the goals of mechanical ventilation in an alternate environment. Name the factors used to estimate the cost of home mechanical ventilation. Describe facilities used for long-term mechanical ventilation. Compare the criteria for discharging a child versus discharging an adult who is ventilator dependent. Describe other forms of ventilation for the long-term ventilator dependent patient.
 Categories of Patients Requiring Long-Term Ventilation n Those recovering from an acute illness. n n Those recovering from a chronic illness. n n n Guillain-Barre COPD Kyphoscoliosis Both have high mortality n n 2 -year mortality of 57%. 5 -year mortality of 66 -97%.
Categories of Patients Requiring Long-Term Ventilation n Those recovering from an acute illness. n n Those recovering from a chronic illness. n n n Guillain-Barre COPD Kyphoscoliosis Both have high mortality n n 2 -year mortality of 57%. 5 -year mortality of 66 -97%.
 Factors Associated with Increase in VAIs n Ventilator-Assisted Individuals n n n Individuals requiring MV for at least 6 hours/day for 21 days or more. (ACCP) Improvements in technology have led to increased survival of critically ill patients. Increased emphasis on reducing costs by transferring patients out early.
Factors Associated with Increase in VAIs n Ventilator-Assisted Individuals n n n Individuals requiring MV for at least 6 hours/day for 21 days or more. (ACCP) Improvements in technology have led to increased survival of critically ill patients. Increased emphasis on reducing costs by transferring patients out early.
 Factors Associated with Increase in VAIs n n NIV is a effective alternative to invasive ventilation. Simpler and more versatile equipment are now available. Increased availability of LTACs and other agencies that allow for ventilation in the home or other SNFs. Example: Christopher Reeves
Factors Associated with Increase in VAIs n n NIV is a effective alternative to invasive ventilation. Simpler and more versatile equipment are now available. Increased availability of LTACs and other agencies that allow for ventilation in the home or other SNFs. Example: Christopher Reeves
 Goals of LTMV Enhancing the individual’s living potential. n Improving physical and physiological level of function. n Reducing mortality. n Reducing hospitalizations. n Extending life. n Providing cost-effective care. n
Goals of LTMV Enhancing the individual’s living potential. n Improving physical and physiological level of function. n Reducing mortality. n Reducing hospitalizations. n Extending life. n Providing cost-effective care. n
 Sites for LTMV n Acute-Care Sites n n Intermediate-Care Sites n n ICU or specialized respiratory-care units. General Medical-Surgical floors. LTACs Sub-Acute Units Long-term care hospitals Rehabilitation Hospitals Long-Term Care Sites n n SNFs Single-Family homes
Sites for LTMV n Acute-Care Sites n n Intermediate-Care Sites n n ICU or specialized respiratory-care units. General Medical-Surgical floors. LTACs Sub-Acute Units Long-term care hospitals Rehabilitation Hospitals Long-Term Care Sites n n SNFs Single-Family homes
 Patient Selection for LTMV n Disease Process & Clinical Stability Acute illness/ARF who aren’t responding to conventional liberation techniques. n Chronic disorders who need support only during certain times of the day. n Need for continuous support. n CVA n Diaphragmatic paralysis Box 21 -2 pg. 429 n
Patient Selection for LTMV n Disease Process & Clinical Stability Acute illness/ARF who aren’t responding to conventional liberation techniques. n Chronic disorders who need support only during certain times of the day. n Need for continuous support. n CVA n Diaphragmatic paralysis Box 21 -2 pg. 429 n
 Patient Selection for LTMV n Psychosocial Factors Prior to discharge. n Family awareness and preparedness. n Psychological evaluation. n Other support systems. n n Respite Care
Patient Selection for LTMV n Psychosocial Factors Prior to discharge. n Family awareness and preparedness. n Psychological evaluation. n Other support systems. n n Respite Care
 Patient Selection for LTMV n Financial Considerations High cost regardless of site. n Multiple factors: n Diagnosis. n Level of acuity. n Need for rehabilitation services. n Need for monitoring. n Oxygen & medications. n
Patient Selection for LTMV n Financial Considerations High cost regardless of site. n Multiple factors: n Diagnosis. n Level of acuity. n Need for rehabilitation services. n Need for monitoring. n Oxygen & medications. n
 Preparation for Discharge Assessment n Education n Training n Plan of Care n
Preparation for Discharge Assessment n Education n Training n Plan of Care n
 Preparation for Discharge n Multi-disciplinary n n n n n Primary Care Physician Pulmonologist Nurse RT Social Worker/Discharge Planner PT OT Speech Pathologist Dietician DME
Preparation for Discharge n Multi-disciplinary n n n n n Primary Care Physician Pulmonologist Nurse RT Social Worker/Discharge Planner PT OT Speech Pathologist Dietician DME
 Geographic & Home Assessment Proximity to home care services. n Modifications to Home. n Mapping of electrical circuits. (Box 21 -4, pg. 433) n
Geographic & Home Assessment Proximity to home care services. n Modifications to Home. n Mapping of electrical circuits. (Box 21 -4, pg. 433) n
 Training n Family Education Detailed, written instructions. n Equipment & troubleshooting. n Disinfection. n Status change recognition. n Return demonstration. n
Training n Family Education Detailed, written instructions. n Equipment & troubleshooting. n Disinfection. n Status change recognition. n Return demonstration. n
 Follow-Up Especially important in infants & children because of changes due to growth and development. n Adequate nutrition. n Family/Social issues. n
Follow-Up Especially important in infants & children because of changes due to growth and development. n Adequate nutrition. n Family/Social issues. n
 Alternatives to Invasive Mechanical Ventilation in the Home n n Non-invasive Positive Pressure Negative-Pressure Ventilation n n n Iron lung Chest Cuirass Body Suit Rocking Bed Pneumobelt Diaphragmatic Pacing
Alternatives to Invasive Mechanical Ventilation in the Home n n Non-invasive Positive Pressure Negative-Pressure Ventilation n n n Iron lung Chest Cuirass Body Suit Rocking Bed Pneumobelt Diaphragmatic Pacing
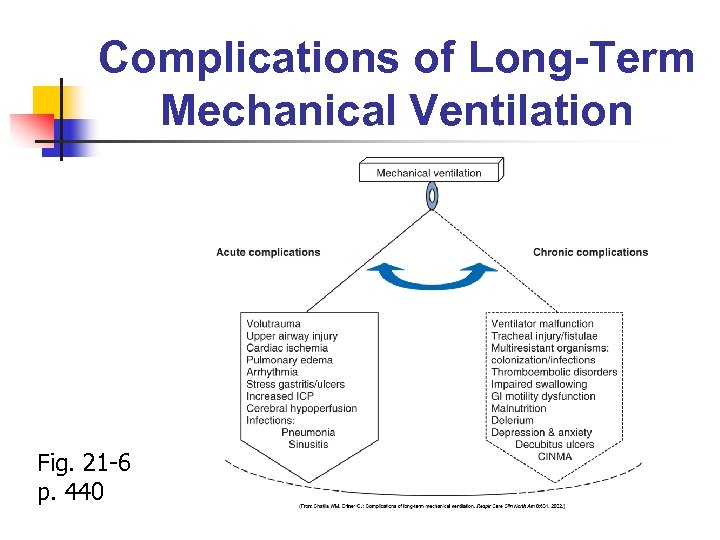 Complications of Long-Term Mechanical Ventilation Fig. 21 -6 p. 440
Complications of Long-Term Mechanical Ventilation Fig. 21 -6 p. 440
 Transport n n Necessity Monitoring Evaluation of Transport Team Transport Ventilator n n n MRD Critical Care Ventilator Transport Ventilator n n LTV Dräger
Transport n n Necessity Monitoring Evaluation of Transport Team Transport Ventilator n n n MRD Critical Care Ventilator Transport Ventilator n n LTV Dräger


