809126f22597e4d38129813a7e167429.ppt
- Количество слайдов: 42
 Rhode Island Long Term Care Mutual Aid Plan (LTC-MAP) Leadership Education
Rhode Island Long Term Care Mutual Aid Plan (LTC-MAP) Leadership Education
 What Led to Mutual Aid in New England: Learning from experiences in: • • • NY State – 1 st Plan (began in 1983) 2001 Tropical Storm Alison (Houston) 2001 9/11 2005 Hurricanes Katrina / Rita Massachusetts Disasters (1 st New England State) • • May 2006 Flooding (Mother’s Day Storm) November 2006 Chemical Explosion (Danvers) 2008 Ice Storm in Central & Western MA
What Led to Mutual Aid in New England: Learning from experiences in: • • • NY State – 1 st Plan (began in 1983) 2001 Tropical Storm Alison (Houston) 2001 9/11 2005 Hurricanes Katrina / Rita Massachusetts Disasters (1 st New England State) • • May 2006 Flooding (Mother’s Day Storm) November 2006 Chemical Explosion (Danvers) 2008 Ice Storm in Central & Western MA
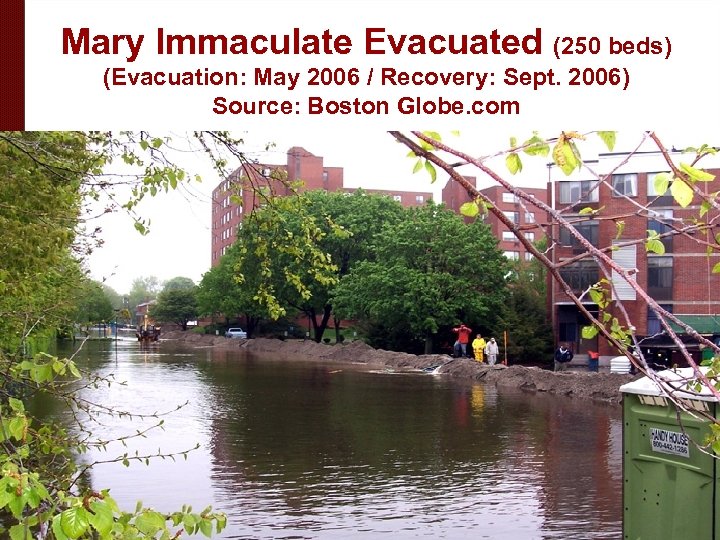 Mary Immaculate Evacuated (250 beds) (Evacuation: May 2006 / Recovery: Sept. 2006) Source: Boston Globe. com
Mary Immaculate Evacuated (250 beds) (Evacuation: May 2006 / Recovery: Sept. 2006) Source: Boston Globe. com
 Other Incidents where Mutual Aid Plans were Activated § § § § Aug/Sept 2011 - Tropical Storm Irene/Lee Flooding Oct/Nov 2011 - “Halloween Storm” - Snowstorm/ Power Failure July 2012 – MA Nursing Home Generator Failure Oct/Nov 2012 - Superstorm Sandy Jan 2013 Influenza Event – Boston & Hartford, CT Activations for Hospital Resident Decompression Feb 2013 – Blizzard (NEMO) Jan 2014 – Snowstorm
Other Incidents where Mutual Aid Plans were Activated § § § § Aug/Sept 2011 - Tropical Storm Irene/Lee Flooding Oct/Nov 2011 - “Halloween Storm” - Snowstorm/ Power Failure July 2012 – MA Nursing Home Generator Failure Oct/Nov 2012 - Superstorm Sandy Jan 2013 Influenza Event – Boston & Hartford, CT Activations for Hospital Resident Decompression Feb 2013 – Blizzard (NEMO) Jan 2014 – Snowstorm
 OVERVIEW of the RI LTC-MAP
OVERVIEW of the RI LTC-MAP
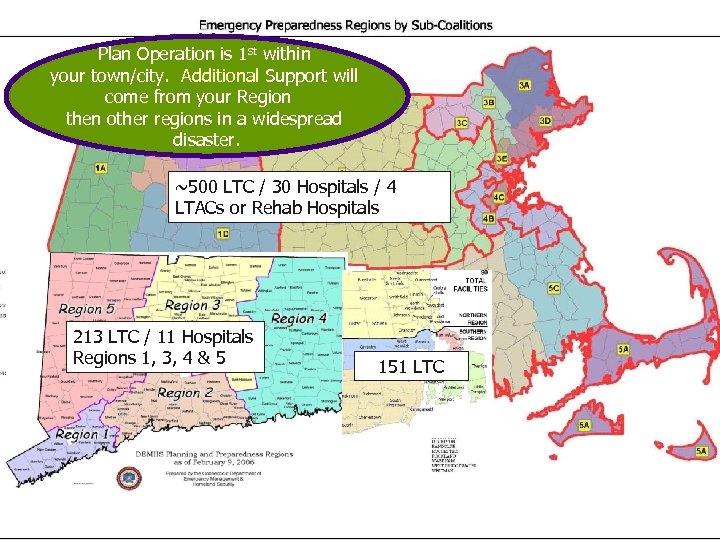 Plan Operation is 1 st within your town/city. Additional Support will come from your Region then other regions in a widespread disaster. ~500 LTC / 30 Hospitals / 4 LTACs or Rehab Hospitals 213 LTC / 11 Hospitals Regions 1, 3, 4 & 5 151 LTC
Plan Operation is 1 st within your town/city. Additional Support will come from your Region then other regions in a widespread disaster. ~500 LTC / 30 Hospitals / 4 LTACs or Rehab Hospitals 213 LTC / 11 Hospitals Regions 1, 3, 4 & 5 151 LTC
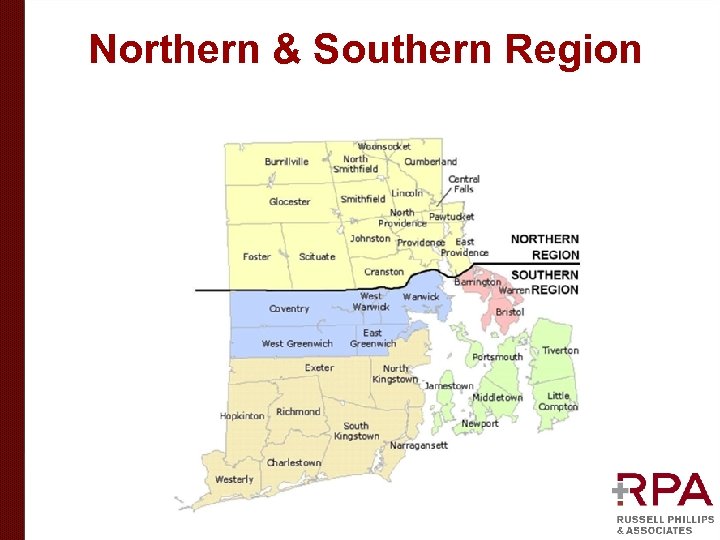 Northern & Southern Region
Northern & Southern Region
 The Basics • • Identify needs and provide supplies/ equipment/pharmaceuticals as necessary Assist with transportation of supplies / staff / equipment / evacuated residents Provide staffing support (whether a facility is evacuating or isolated) Place and support the care of evacuated residents (continuity of care / surge locations)
The Basics • • Identify needs and provide supplies/ equipment/pharmaceuticals as necessary Assist with transportation of supplies / staff / equipment / evacuated residents Provide staffing support (whether a facility is evacuating or isolated) Place and support the care of evacuated residents (continuity of care / surge locations)
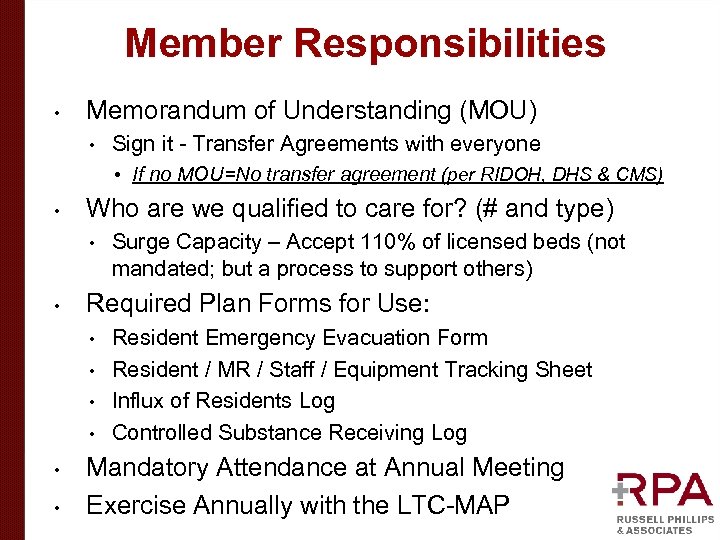 Member Responsibilities • Memorandum of Understanding (MOU) • Sign it - Transfer Agreements with everyone • If no MOU=No transfer agreement (per RIDOH, DHS & CMS) • Who are we qualified to care for? (# and type) • • Surge Capacity – Accept 110% of licensed beds (not mandated; but a process to support others) Required Plan Forms for Use: Resident Emergency Evacuation Form • Resident / MR / Staff / Equipment Tracking Sheet • Influx of Residents Log • Controlled Substance Receiving Log • • • Mandatory Attendance at Annual Meeting Exercise Annually with the LTC-MAP
Member Responsibilities • Memorandum of Understanding (MOU) • Sign it - Transfer Agreements with everyone • If no MOU=No transfer agreement (per RIDOH, DHS & CMS) • Who are we qualified to care for? (# and type) • • Surge Capacity – Accept 110% of licensed beds (not mandated; but a process to support others) Required Plan Forms for Use: Resident Emergency Evacuation Form • Resident / MR / Staff / Equipment Tracking Sheet • Influx of Residents Log • Controlled Substance Receiving Log • • • Mandatory Attendance at Annual Meeting Exercise Annually with the LTC-MAP
 Memorandum of Understanding (MOU) (Located in Section 8 of the plan) • • The MOU is a “voluntary agreement” among members By signing the (MOU) all facilities agree to their intent to abide by the terms in the event of a disaster. The terms are to be incorporated into the facility’s Emergency Management Plans and Emergency Operations Plans PUSH IS FOR A SUMMER OF 2014 MOU SIGNATURE AND RETURNED TO Alysia Mihalakos, Interim Chief of CEPR, Rhode Island Department of Health (RIDOH): alysia. mihalakos@health. ri. gov
Memorandum of Understanding (MOU) (Located in Section 8 of the plan) • • The MOU is a “voluntary agreement” among members By signing the (MOU) all facilities agree to their intent to abide by the terms in the event of a disaster. The terms are to be incorporated into the facility’s Emergency Management Plans and Emergency Operations Plans PUSH IS FOR A SUMMER OF 2014 MOU SIGNATURE AND RETURNED TO Alysia Mihalakos, Interim Chief of CEPR, Rhode Island Department of Health (RIDOH): alysia. mihalakos@health. ri. gov
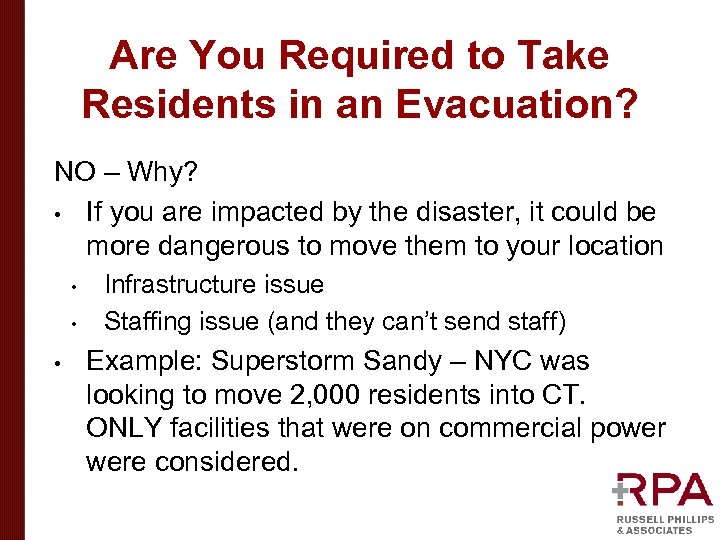 Are You Required to Take Residents in an Evacuation? NO – Why? • If you are impacted by the disaster, it could be more dangerous to move them to your location • • • Infrastructure issue Staffing issue (and they can’t send staff) Example: Superstorm Sandy – NYC was looking to move 2, 000 residents into CT. ONLY facilities that were on commercial power were considered.
Are You Required to Take Residents in an Evacuation? NO – Why? • If you are impacted by the disaster, it could be more dangerous to move them to your location • • • Infrastructure issue Staffing issue (and they can’t send staff) Example: Superstorm Sandy – NYC was looking to move 2, 000 residents into CT. ONLY facilities that were on commercial power were considered.
 Responsibility for Care • Resident Accepting Facility (RAF) receives the resident: • • Do not admit (being reviewed with DHS) Under the care of the RAF Return the resident to the facility or origin after completion of the disaster Ethical standpoint – no marketing efforts to the residents and their families
Responsibility for Care • Resident Accepting Facility (RAF) receives the resident: • • Do not admit (being reviewed with DHS) Under the care of the RAF Return the resident to the facility or origin after completion of the disaster Ethical standpoint – no marketing efforts to the residents and their families
 Reimbursement Approach Disaster Struck Facility • • Can the facility reopen within 30 days? IF YES – The resident is never discharged and they are “sheltered” at the RAF IF NO – The resident is discharged and permanent placement will be addressed Process of not admitting (“sheltering”) – enables surge to 110% of licensed beds to take place (waiver) RIDOH & CMS will support this process
Reimbursement Approach Disaster Struck Facility • • Can the facility reopen within 30 days? IF YES – The resident is never discharged and they are “sheltered” at the RAF IF NO – The resident is discharged and permanent placement will be addressed Process of not admitting (“sheltering”) – enables surge to 110% of licensed beds to take place (waiver) RIDOH & CMS will support this process
 Reimbursement Approach • Disaster Struck Facility • • Paid by CMS (Medicare), DHS (Medicaid) or private pay RAF is paid by DSF at DSF rate • • If 100% of services provided by RAF, 100% of payment If staff, equipment and meds come from DSF, amicable division (incremental labor costs & consumables) If exceeding licensed beds, amicable division Mediation or Arbitration (called out in MOU)
Reimbursement Approach • Disaster Struck Facility • • Paid by CMS (Medicare), DHS (Medicaid) or private pay RAF is paid by DSF at DSF rate • • If 100% of services provided by RAF, 100% of payment If staff, equipment and meds come from DSF, amicable division (incremental labor costs & consumables) If exceeding licensed beds, amicable division Mediation or Arbitration (called out in MOU)
 Facilities Still Must Be Ready Internally What we need to have internally: • • Have an Incident Command System (Nursing Home Incident Command System – NHICS) Full Building Evacuation Plan • • • Get residents to the sidewalk Influx of Residents (Census Reduction / Surge Capacity Plan) Resources & Assets for 96 hours • Self-sustainability
Facilities Still Must Be Ready Internally What we need to have internally: • • Have an Incident Command System (Nursing Home Incident Command System – NHICS) Full Building Evacuation Plan • • • Get residents to the sidewalk Influx of Residents (Census Reduction / Surge Capacity Plan) Resources & Assets for 96 hours • Self-sustainability
 Disaster Struck Facility
Disaster Struck Facility
 Shelter-in-Place / Evacuating Disaster Struck Facility (when speaking with RIDOH and Local Emergency Manager or 911) • Size-up the Situation • • Resource & Assets needs to stay operational Failure of infrastructure to remain in the facility Who – Your contact name and phone number Where – Facility Name, Address and Town/City What – What is the issue? When – Window of time the resources will be required in / How long until the evacuation must commence Why – Reason
Shelter-in-Place / Evacuating Disaster Struck Facility (when speaking with RIDOH and Local Emergency Manager or 911) • Size-up the Situation • • Resource & Assets needs to stay operational Failure of infrastructure to remain in the facility Who – Your contact name and phone number Where – Facility Name, Address and Town/City What – What is the issue? When – Window of time the resources will be required in / How long until the evacuation must commence Why – Reason
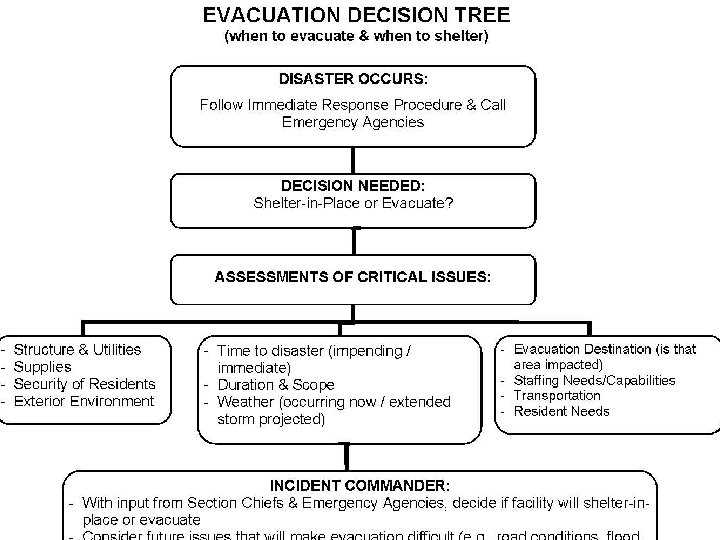 Shelter-in-Place / Evacuating
Shelter-in-Place / Evacuating
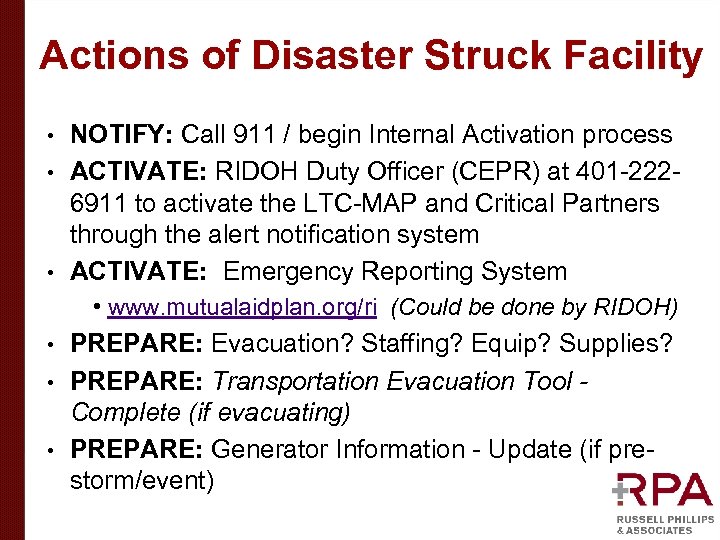 Actions of Disaster Struck Facility NOTIFY: Call 911 / begin Internal Activation process • ACTIVATE: RIDOH Duty Officer (CEPR) at 401 -2226911 to activate the LTC-MAP and Critical Partners through the alert notification system • ACTIVATE: Emergency Reporting System • • www. mutualaidplan. org/ri (Could be done by RIDOH) PREPARE: Evacuation? Staffing? Equip? Supplies? • PREPARE: Transportation Evacuation Tool Complete (if evacuating) • PREPARE: Generator Information - Update (if prestorm/event) •
Actions of Disaster Struck Facility NOTIFY: Call 911 / begin Internal Activation process • ACTIVATE: RIDOH Duty Officer (CEPR) at 401 -2226911 to activate the LTC-MAP and Critical Partners through the alert notification system • ACTIVATE: Emergency Reporting System • • www. mutualaidplan. org/ri (Could be done by RIDOH) PREPARE: Evacuation? Staffing? Equip? Supplies? • PREPARE: Transportation Evacuation Tool Complete (if evacuating) • PREPARE: Generator Information - Update (if prestorm/event) •
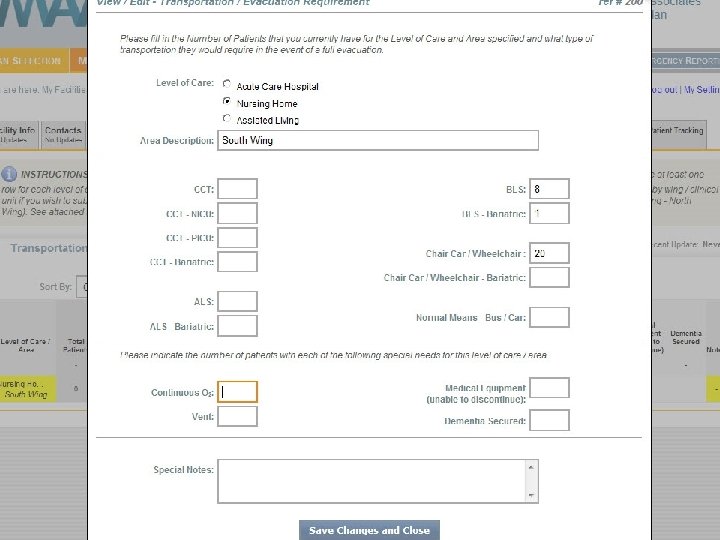
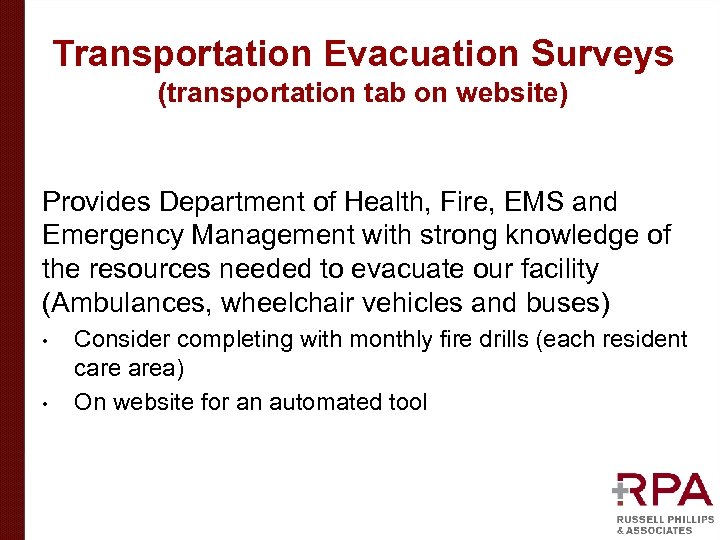 Transportation Evacuation Surveys (transportation tab on website) Provides Department of Health, Fire, EMS and Emergency Management with strong knowledge of the resources needed to evacuate our facility (Ambulances, wheelchair vehicles and buses) • • Consider completing with monthly fire drills (each resident care area) On website for an automated tool
Transportation Evacuation Surveys (transportation tab on website) Provides Department of Health, Fire, EMS and Emergency Management with strong knowledge of the resources needed to evacuate our facility (Ambulances, wheelchair vehicles and buses) • • Consider completing with monthly fire drills (each resident care area) On website for an automated tool

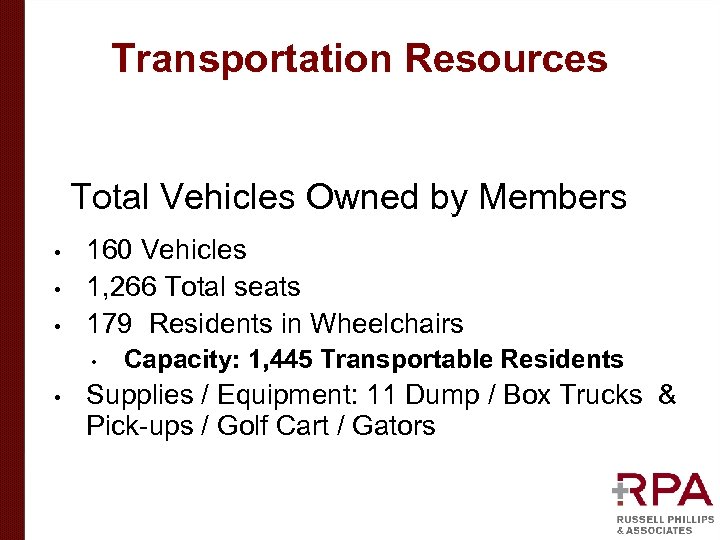 Transportation Resources • • • Total Vehicles Owned by Members 160 Vehicles 1, 266 Total seats 179 Residents in Wheelchairs • • Capacity: 1, 445 Transportable Residents Supplies / Equipment: 11 Dump / Box Trucks & Pick-ups / Golf Cart / Gators
Transportation Resources • • • Total Vehicles Owned by Members 160 Vehicles 1, 266 Total seats 179 Residents in Wheelchairs • • Capacity: 1, 445 Transportable Residents Supplies / Equipment: 11 Dump / Box Trucks & Pick-ups / Golf Cart / Gators
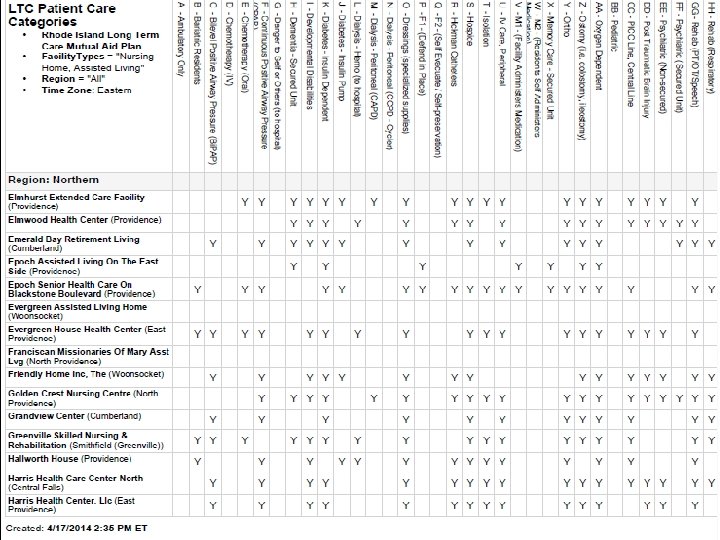
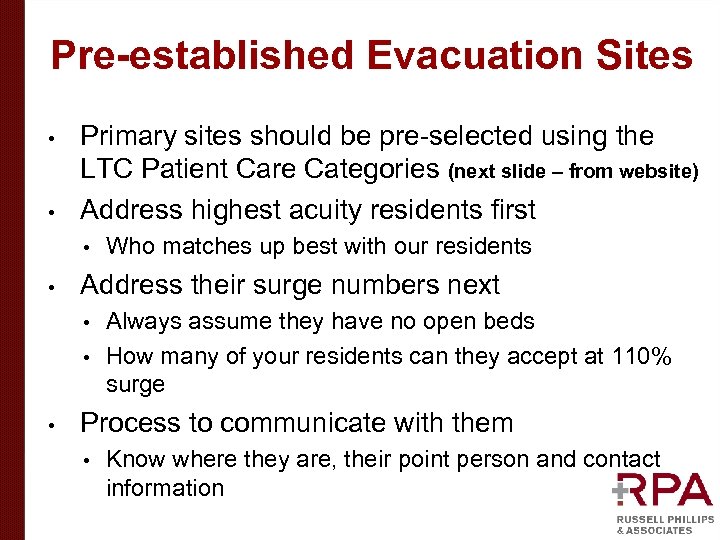 Pre-established Evacuation Sites • • Primary sites should be pre-selected using the LTC Patient Care Categories (next slide – from website) Address highest acuity residents first • • Who matches up best with our residents Address their surge numbers next Always assume they have no open beds • How many of your residents can they accept at 110% surge • • Process to communicate with them • Know where they are, their point person and contact information
Pre-established Evacuation Sites • • Primary sites should be pre-selected using the LTC Patient Care Categories (next slide – from website) Address highest acuity residents first • • Who matches up best with our residents Address their surge numbers next Always assume they have no open beds • How many of your residents can they accept at 110% surge • • Process to communicate with them • Know where they are, their point person and contact information
 25
25
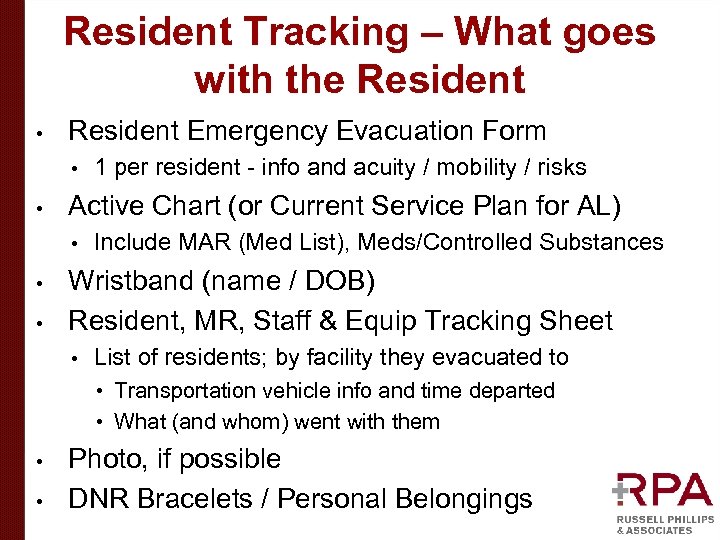 Resident Tracking – What goes with the Resident • Resident Emergency Evacuation Form • • Active Chart (or Current Service Plan for AL) • • • 1 per resident - info and acuity / mobility / risks Include MAR (Med List), Meds/Controlled Substances Wristband (name / DOB) Resident, MR, Staff & Equip Tracking Sheet • List of residents; by facility they evacuated to • Transportation vehicle info and time departed • What (and whom) went with them • • Photo, if possible DNR Bracelets / Personal Belongings
Resident Tracking – What goes with the Resident • Resident Emergency Evacuation Form • • Active Chart (or Current Service Plan for AL) • • • 1 per resident - info and acuity / mobility / risks Include MAR (Med List), Meds/Controlled Substances Wristband (name / DOB) Resident, MR, Staff & Equip Tracking Sheet • List of residents; by facility they evacuated to • Transportation vehicle info and time departed • What (and whom) went with them • • Photo, if possible DNR Bracelets / Personal Belongings
 Resident Accepting Facilities/Lenders
Resident Accepting Facilities/Lenders
 Actions of Resident Accepting Facilities/Lenders • Prepare to receive residents • • • Open beds vs. Surge Area Complete Emergency Reporting Complete the Influx of Resident Log - residents arrive Confirm with DSF or LTC Group Responders that the residents are received – “CLOSE THE LOOP” Start a new chart for resident Notify RIDOH and your local AHJ about activating a Surge Plan (Influx / Surge Guidelines) If Lender: Prepare to provide Resources/Assets
Actions of Resident Accepting Facilities/Lenders • Prepare to receive residents • • • Open beds vs. Surge Area Complete Emergency Reporting Complete the Influx of Resident Log - residents arrive Confirm with DSF or LTC Group Responders that the residents are received – “CLOSE THE LOOP” Start a new chart for resident Notify RIDOH and your local AHJ about activating a Surge Plan (Influx / Surge Guidelines) If Lender: Prepare to provide Resources/Assets
 What happens at 2: 00 AM? Anyone who might answer the phone: Basic knowledge that RI LTC-MAP exists (there is a plan) • Get the name of the person calling, facility, contact number and issue or request • OR – Listen to the automated message and take down directions for what it tells you to do • Inform the Nursing Supervisor ASAP • Nursing Supervisor – Scope will determine actions • • • Immediate analysis of open beds – M / F / Either Activate internal emergency notification tree Complete Emergency Reporting- www. mutualaidplan. org/ri Evacuation? Prepare to receiving incoming residents Resource & Asset Request: Prepare to provide staff, equipment, supplies or transportation
What happens at 2: 00 AM? Anyone who might answer the phone: Basic knowledge that RI LTC-MAP exists (there is a plan) • Get the name of the person calling, facility, contact number and issue or request • OR – Listen to the automated message and take down directions for what it tells you to do • Inform the Nursing Supervisor ASAP • Nursing Supervisor – Scope will determine actions • • • Immediate analysis of open beds – M / F / Either Activate internal emergency notification tree Complete Emergency Reporting- www. mutualaidplan. org/ri Evacuation? Prepare to receiving incoming residents Resource & Asset Request: Prepare to provide staff, equipment, supplies or transportation
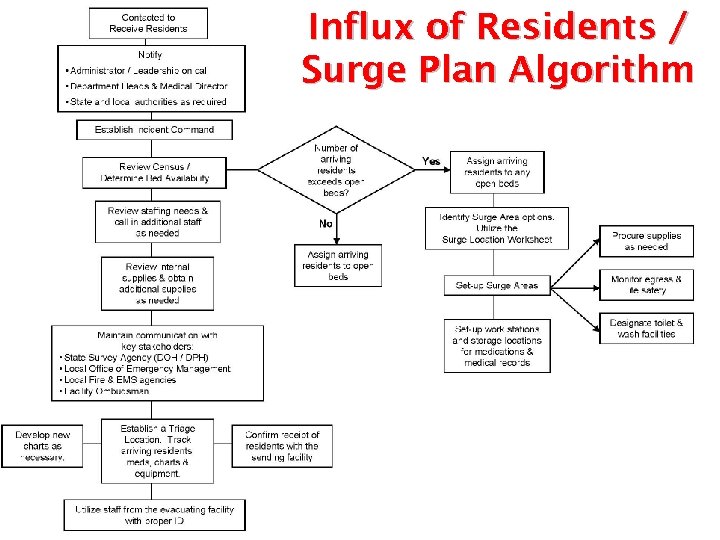 Influx of Residents / Surge Plan Algorithm
Influx of Residents / Surge Plan Algorithm
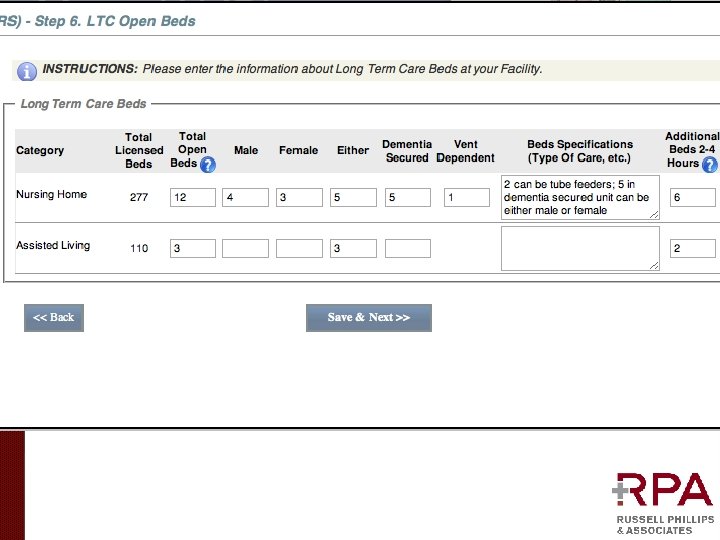
 RI LTC-MAP Website (all tabs are specific to our facility based on data we enter)
RI LTC-MAP Website (all tabs are specific to our facility based on data we enter)

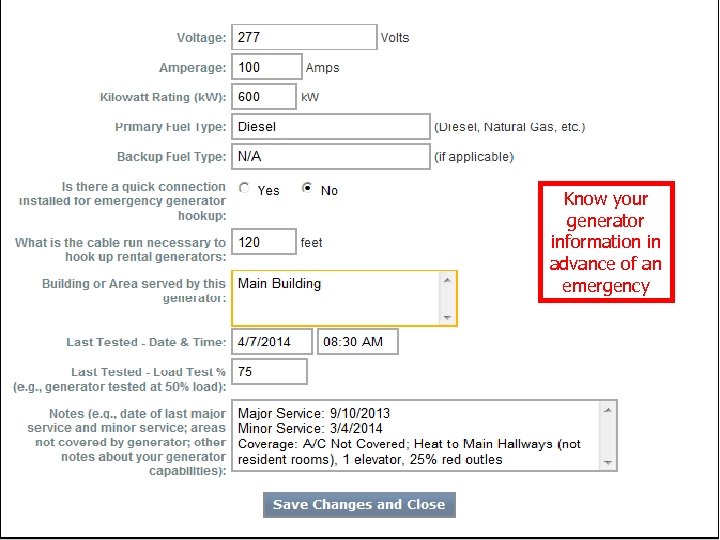 Know your generator information in advance of an emergency
Know your generator information in advance of an emergency
 Emergency Reporting Designated Facility Leadership or Nursing Supervisor (complete for LTC -MAP when requested)
Emergency Reporting Designated Facility Leadership or Nursing Supervisor (complete for LTC -MAP when requested)
 Internal Situation-Status Report & Emergency Reporting: What You Should Know (and WHY) HANDOUT Operational Issues at your facility (other plan members) • Open Beds • Available Transportation for • • Resident Transportation • Movement of Supplies and Equipment Resources & Assets (needed) • Resources & Assets (you could provide) • • Equipment • Supplies • Staffing
Internal Situation-Status Report & Emergency Reporting: What You Should Know (and WHY) HANDOUT Operational Issues at your facility (other plan members) • Open Beds • Available Transportation for • • Resident Transportation • Movement of Supplies and Equipment Resources & Assets (needed) • Resources & Assets (you could provide) • • Equipment • Supplies • Staffing


 RIDOH Department Operations Center (DOC) LTC Group Responders
RIDOH Department Operations Center (DOC) LTC Group Responders
 RIDOH Department Operations Center (LTC Group Responders)
RIDOH Department Operations Center (LTC Group Responders)
 Function of the LTC Group Responders “Air Traffic Control” • • • Staffed by RIDOH & volunteers from the LTC-MAP Assist with resident placement Support resident tracking - “Close the loop” Assist with obtaining staff, supplies and equipment Assist with transportation of residents, staff, supplies and equipment Support interaction with local and state agencies ENSURE ALL MEMBERS ARE ACCOUNTED FOR
Function of the LTC Group Responders “Air Traffic Control” • • • Staffed by RIDOH & volunteers from the LTC-MAP Assist with resident placement Support resident tracking - “Close the loop” Assist with obtaining staff, supplies and equipment Assist with transportation of residents, staff, supplies and equipment Support interaction with local and state agencies ENSURE ALL MEMBERS ARE ACCOUNTED FOR
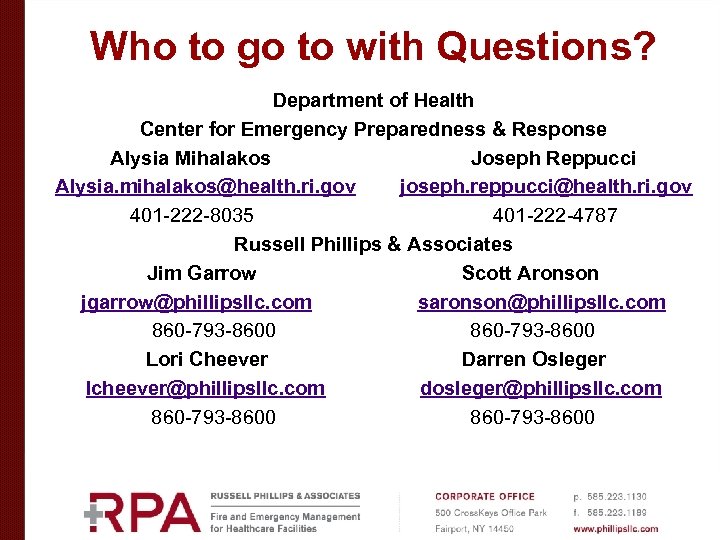 Who to go to with Questions? Department of Health Center for Emergency Preparedness & Response Alysia Mihalakos Joseph Reppucci Alysia. mihalakos@health. ri. gov joseph. reppucci@health. ri. gov 401 -222 -8035 401 -222 -4787 Russell Phillips & Associates Jim Garrow Scott Aronson jgarrow@phillipsllc. com saronson@phillipsllc. com 860 -793 -8600 Lori Cheever Darren Osleger lcheever@phillipsllc. com dosleger@phillipsllc. com David Hood Scott Aronson dhood@phillipsllc. com saronson@phillipsllc. com 860 -793 -8600
Who to go to with Questions? Department of Health Center for Emergency Preparedness & Response Alysia Mihalakos Joseph Reppucci Alysia. mihalakos@health. ri. gov joseph. reppucci@health. ri. gov 401 -222 -8035 401 -222 -4787 Russell Phillips & Associates Jim Garrow Scott Aronson jgarrow@phillipsllc. com saronson@phillipsllc. com 860 -793 -8600 Lori Cheever Darren Osleger lcheever@phillipsllc. com dosleger@phillipsllc. com David Hood Scott Aronson dhood@phillipsllc. com saronson@phillipsllc. com 860 -793 -8600


