romatoid arthrites introduction.pptx
- Количество слайдов: 27

 Rheumatoid arthritis
Rheumatoid arthritis
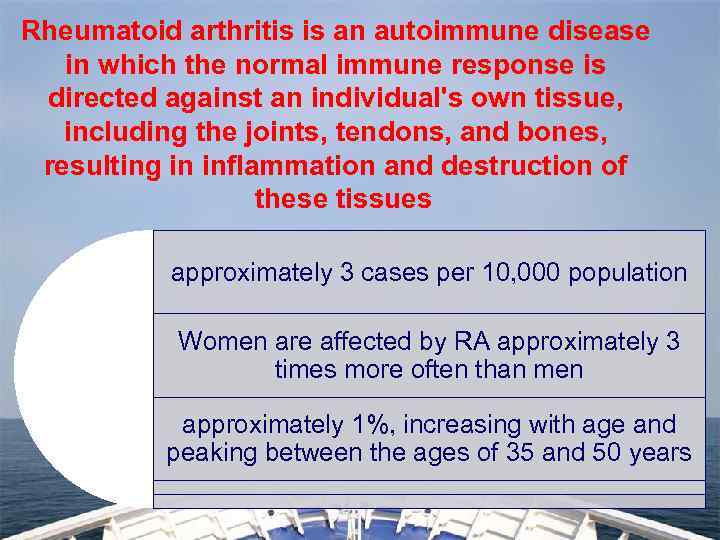 Rheumatoid arthritis is an autoimmune disease in which the normal immune response is directed against an individual's own tissue, including the joints, tendons, and bones, resulting in inflammation and destruction of these tissues approximately 3 cases per 10, 000 population Women are affected by RA approximately 3 times more often than men approximately 1%, increasing with age and peaking between the ages of 35 and 50 years
Rheumatoid arthritis is an autoimmune disease in which the normal immune response is directed against an individual's own tissue, including the joints, tendons, and bones, resulting in inflammation and destruction of these tissues approximately 3 cases per 10, 000 population Women are affected by RA approximately 3 times more often than men approximately 1%, increasing with age and peaking between the ages of 35 and 50 years
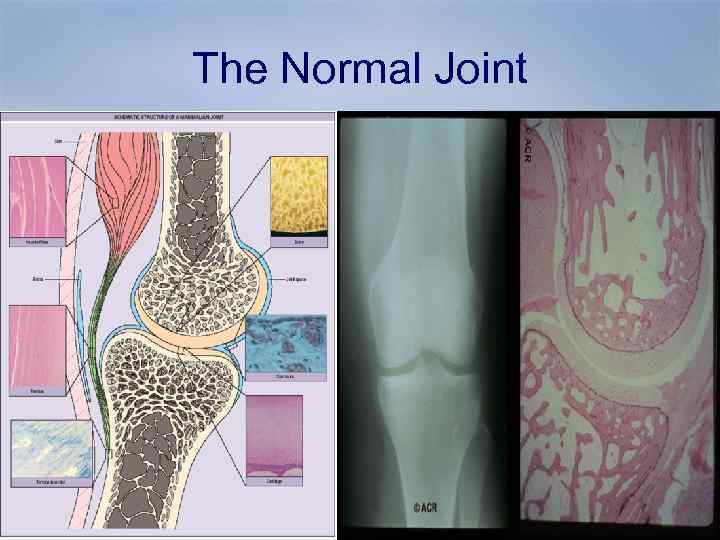 The Normal Joint
The Normal Joint
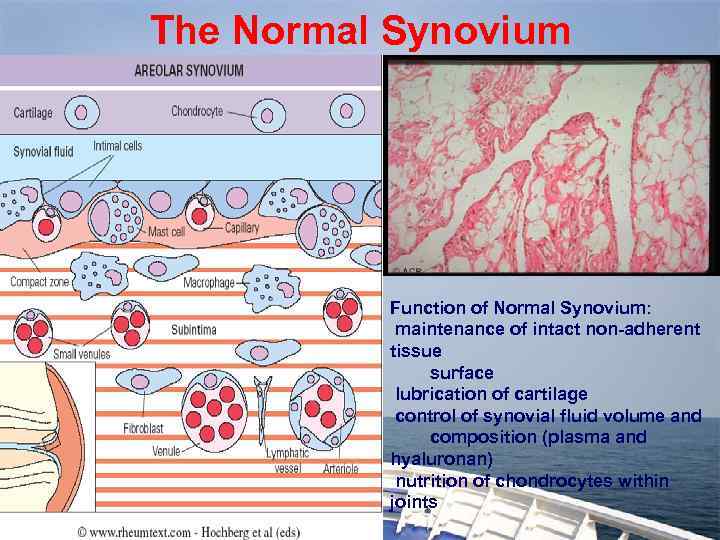 The Normal Synovium Function of Normal Synovium: maintenance of intact non-adherent tissue surface lubrication of cartilage control of synovial fluid volume and composition (plasma and hyaluronan) nutrition of chondrocytes within joints
The Normal Synovium Function of Normal Synovium: maintenance of intact non-adherent tissue surface lubrication of cartilage control of synovial fluid volume and composition (plasma and hyaluronan) nutrition of chondrocytes within joints
 Symptoms Of RA • General symptoms • Fever • • Weakness • Fatigue And Tiredness • Loss Of Appetite Numbness
Symptoms Of RA • General symptoms • Fever • • Weakness • Fatigue And Tiredness • Loss Of Appetite Numbness
 Signs Of RA Joint Deformity Sign Joint swelling Joint Dislocation. Ulnar Deviation
Signs Of RA Joint Deformity Sign Joint swelling Joint Dislocation. Ulnar Deviation
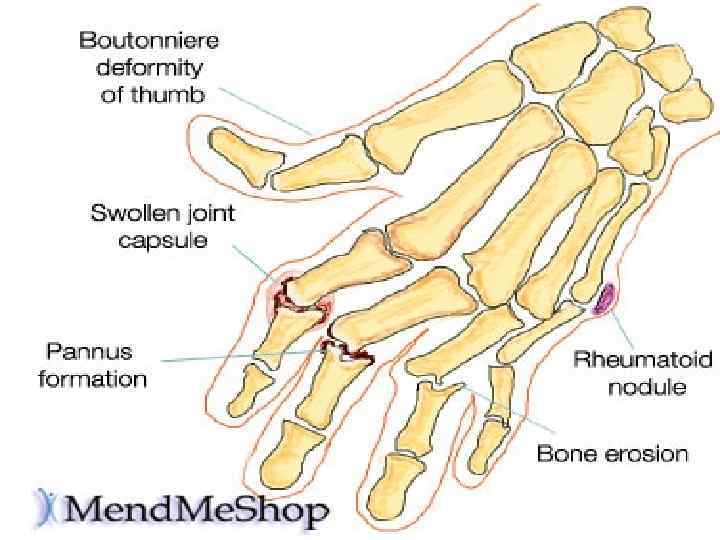
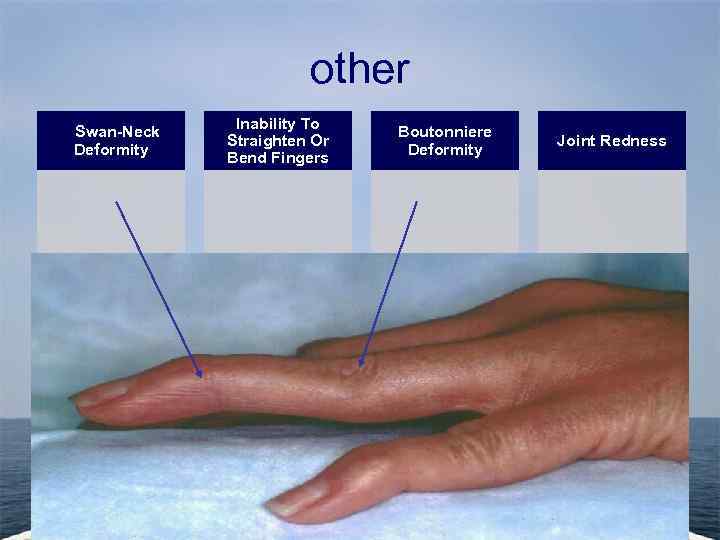 other Swan-Neck Deformity Inability To Straighten Or Bend Fingers Boutonniere Deformity Joint Redness
other Swan-Neck Deformity Inability To Straighten Or Bend Fingers Boutonniere Deformity Joint Redness
 Rheumatoid arthritis small joints of hands and feet affected first, larger joints later
Rheumatoid arthritis small joints of hands and feet affected first, larger joints later
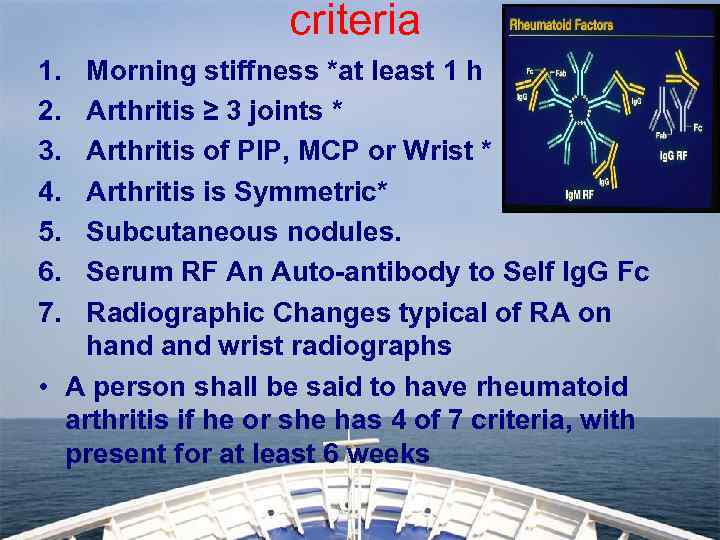 criteria 1. 2. 3. 4. 5. 6. 7. Morning stiffness *at least 1 h Arthritis ≥ 3 joints * Arthritis of PIP, MCP or Wrist * Arthritis is Symmetric* Subcutaneous nodules. Serum RF An Auto-antibody to Self Ig. G Fc Radiographic Changes typical of RA on hand wrist radiographs • A person shall be said to have rheumatoid arthritis if he or she has 4 of 7 criteria, with present for at least 6 weeks
criteria 1. 2. 3. 4. 5. 6. 7. Morning stiffness *at least 1 h Arthritis ≥ 3 joints * Arthritis of PIP, MCP or Wrist * Arthritis is Symmetric* Subcutaneous nodules. Serum RF An Auto-antibody to Self Ig. G Fc Radiographic Changes typical of RA on hand wrist radiographs • A person shall be said to have rheumatoid arthritis if he or she has 4 of 7 criteria, with present for at least 6 weeks
 Effects on organ systems • • • RA affects several organ systems, as follows: Cutaneous Cardiac Pulmonary Renal Gastrointestinal (GI) Vascular Hematologic Neurologic Ocular
Effects on organ systems • • • RA affects several organ systems, as follows: Cutaneous Cardiac Pulmonary Renal Gastrointestinal (GI) Vascular Hematologic Neurologic Ocular

 What causes rheumatoid arthritis? • The cause of RA is not known. Yet, new research is giving us a better idea of what makes the immune system attack the body and create inflammation. In RA, the focus of the inflammation is in the synovium, the tissue that lines the joint. Immune cells release inflammation-causing chemicals. These chemicals can damage cartilage (the tissue that cushions between joints) and bone. • Other things likely play a role in RA as well. For instance, genes make some people more prone to getting RA. that affect the immune system may
What causes rheumatoid arthritis? • The cause of RA is not known. Yet, new research is giving us a better idea of what makes the immune system attack the body and create inflammation. In RA, the focus of the inflammation is in the synovium, the tissue that lines the joint. Immune cells release inflammation-causing chemicals. These chemicals can damage cartilage (the tissue that cushions between joints) and bone. • Other things likely play a role in RA as well. For instance, genes make some people more prone to getting RA. that affect the immune system may
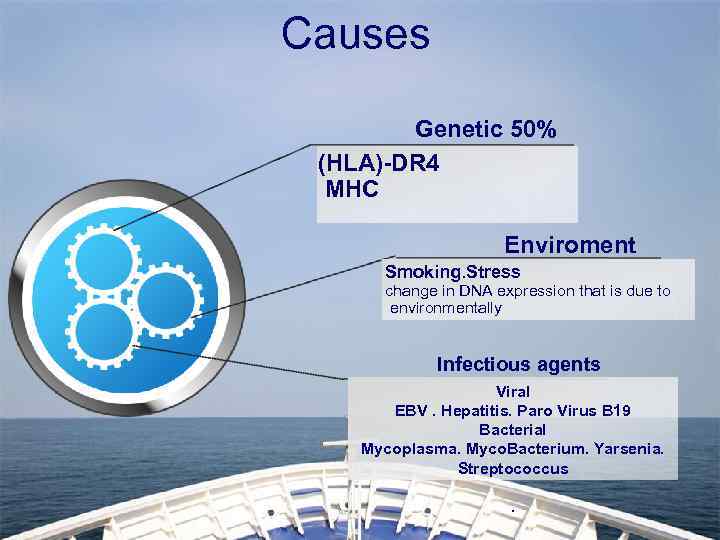 Causes Genetic 50% (HLA)-DR 4 MHC Enviroment Smoking. Stress change in DNA expression that is due to environmentally Infectious agents Viral EBV. Hepatitis. Paro Virus B 19 Bacterial Mycoplasma. Myco. Bacterium. Yarsenia. Streptococcus.
Causes Genetic 50% (HLA)-DR 4 MHC Enviroment Smoking. Stress change in DNA expression that is due to environmentally Infectious agents Viral EBV. Hepatitis. Paro Virus B 19 Bacterial Mycoplasma. Myco. Bacterium. Yarsenia. Streptococcus.
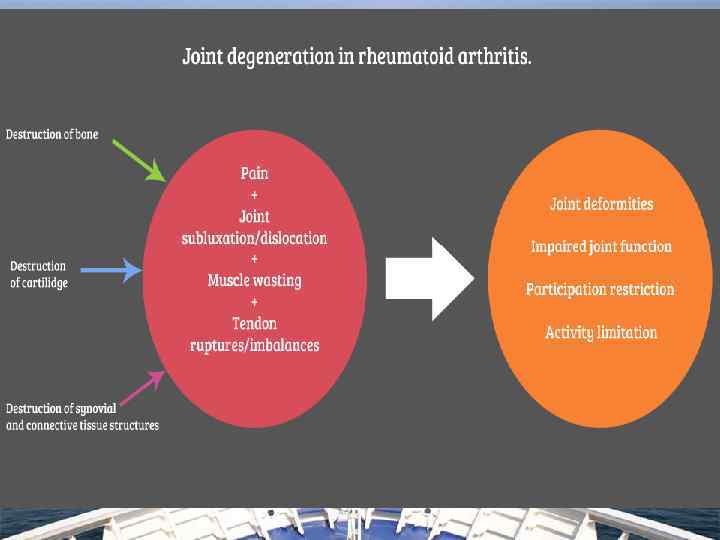
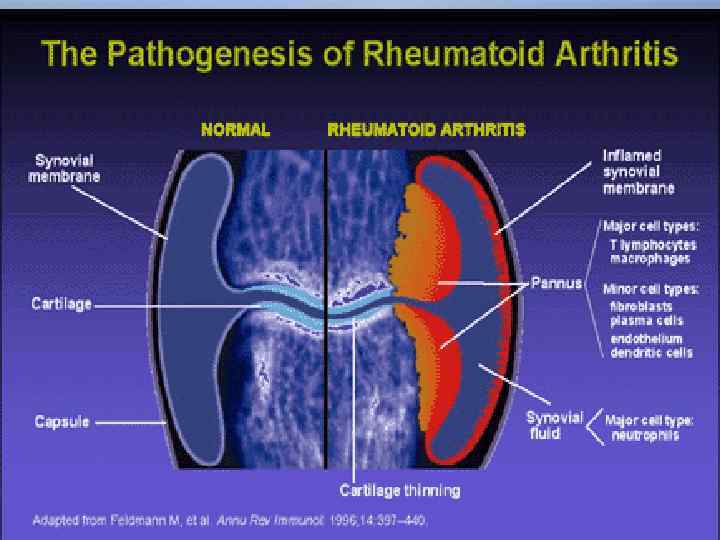
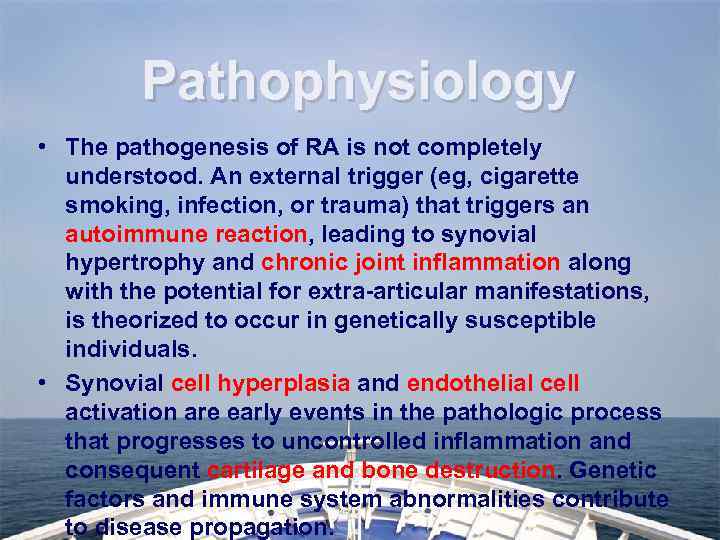 Pathophysiology • The pathogenesis of RA is not completely understood. An external trigger (eg, cigarette smoking, infection, or trauma) that triggers an autoimmune reaction, leading to synovial hypertrophy and chronic joint inflammation along with the potential for extra-articular manifestations, is theorized to occur in genetically susceptible individuals. • Synovial cell hyperplasia and endothelial cell activation are early events in the pathologic process that progresses to uncontrolled inflammation and consequent cartilage and bone destruction. Genetic factors and immune system abnormalities contribute to disease propagation.
Pathophysiology • The pathogenesis of RA is not completely understood. An external trigger (eg, cigarette smoking, infection, or trauma) that triggers an autoimmune reaction, leading to synovial hypertrophy and chronic joint inflammation along with the potential for extra-articular manifestations, is theorized to occur in genetically susceptible individuals. • Synovial cell hyperplasia and endothelial cell activation are early events in the pathologic process that progresses to uncontrolled inflammation and consequent cartilage and bone destruction. Genetic factors and immune system abnormalities contribute to disease propagation.
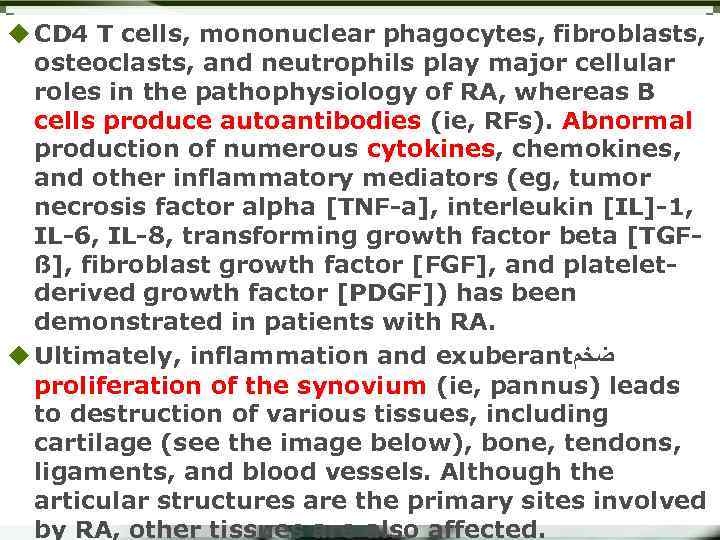 u CD 4 T cells, mononuclear phagocytes, fibroblasts, osteoclasts, and neutrophils play major cellular roles in the pathophysiology of RA, whereas B cells produce autoantibodies (ie, RFs). Abnormal production of numerous cytokines, chemokines, and other inflammatory mediators (eg, tumor necrosis factor alpha [TNF-a], interleukin [IL]-1, IL-6, IL-8, transforming growth factor beta [TGFß], fibroblast growth factor [FGF], and plateletderived growth factor [PDGF]) has been demonstrated in patients with RA. u Ultimately, inflammation and exuberant ﺿﺨﻢ proliferation of the synovium (ie, pannus) leads to destruction of various tissues, including cartilage (see the image below), bone, tendons, ligaments, and blood vessels. Although the articular structures are the primary sites involved by RA, other tissues are also affected.
u CD 4 T cells, mononuclear phagocytes, fibroblasts, osteoclasts, and neutrophils play major cellular roles in the pathophysiology of RA, whereas B cells produce autoantibodies (ie, RFs). Abnormal production of numerous cytokines, chemokines, and other inflammatory mediators (eg, tumor necrosis factor alpha [TNF-a], interleukin [IL]-1, IL-6, IL-8, transforming growth factor beta [TGFß], fibroblast growth factor [FGF], and plateletderived growth factor [PDGF]) has been demonstrated in patients with RA. u Ultimately, inflammation and exuberant ﺿﺨﻢ proliferation of the synovium (ie, pannus) leads to destruction of various tissues, including cartilage (see the image below), bone, tendons, ligaments, and blood vessels. Although the articular structures are the primary sites involved by RA, other tissues are also affected.
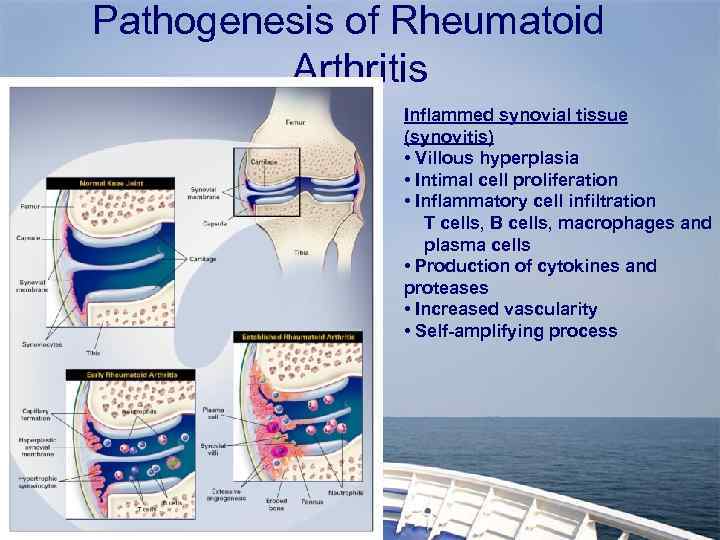 Pathogenesis of Rheumatoid Arthritis Inflammed synovial tissue (synovitis) • Villous hyperplasia • Intimal cell proliferation • Inflammatory cell infiltration T cells, B cells, macrophages and plasma cells • Production of cytokines and proteases • Increased vascularity • Self-amplifying process
Pathogenesis of Rheumatoid Arthritis Inflammed synovial tissue (synovitis) • Villous hyperplasia • Intimal cell proliferation • Inflammatory cell infiltration T cells, B cells, macrophages and plasma cells • Production of cytokines and proteases • Increased vascularity • Self-amplifying process
 This gross photo shows destruction of the cartilage and erosion of the underlying bone with pannus from a patient with rheumatoid arthritis.
This gross photo shows destruction of the cartilage and erosion of the underlying bone with pannus from a patient with rheumatoid arthritis.

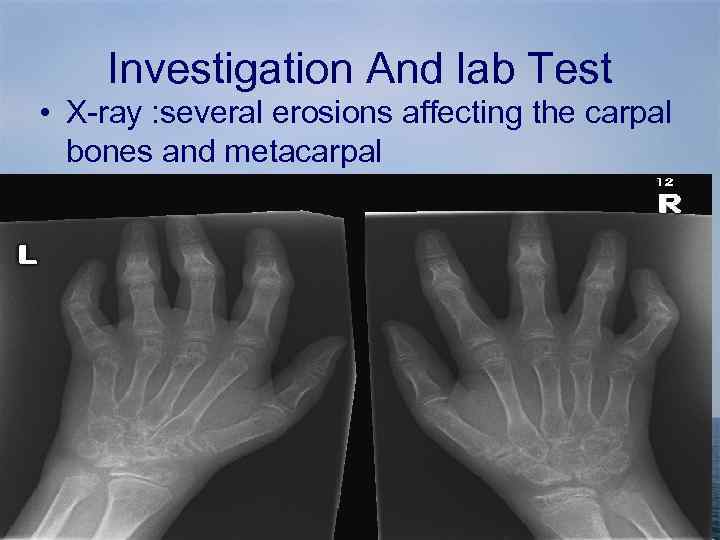 Investigation And lab Test • X-ray : several erosions affecting the carpal bones and metacarpal
Investigation And lab Test • X-ray : several erosions affecting the carpal bones and metacarpal
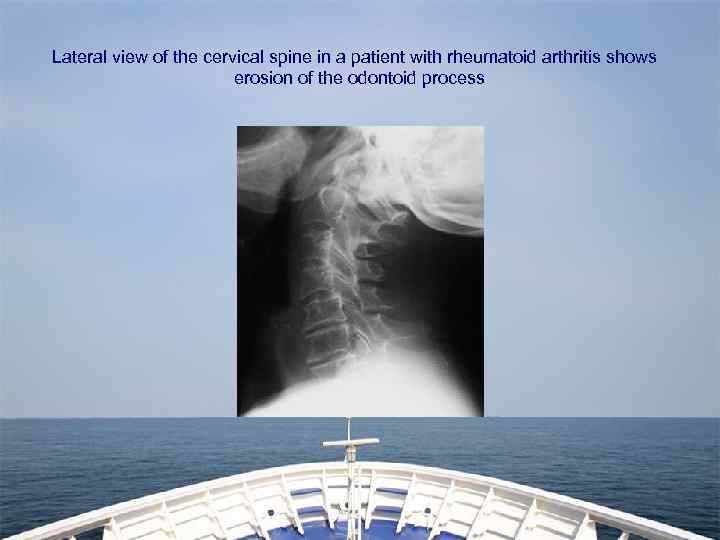 Lateral view of the cervical spine in a patient with rheumatoid arthritis shows erosion of the odontoid process
Lateral view of the cervical spine in a patient with rheumatoid arthritis shows erosion of the odontoid process
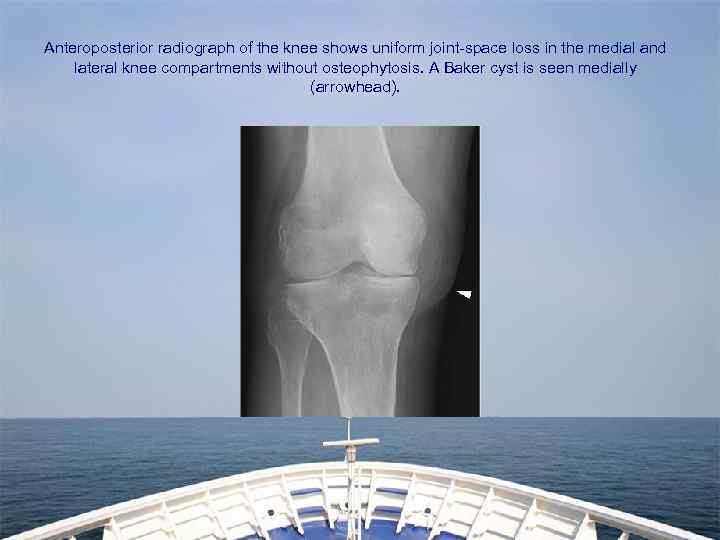 Anteroposterior radiograph of the knee shows uniform joint-space loss in the medial and lateral knee compartments without osteophytosis. A Baker cyst is seen medially (arrowhead).
Anteroposterior radiograph of the knee shows uniform joint-space loss in the medial and lateral knee compartments without osteophytosis. A Baker cyst is seen medially (arrowhead).
 • MRI And CAT scan • Blood Examination Erythrocyte sedimentation rate (ESR) C-reactive protein (CRP) level Complete blood count (CBC) Rheumatoid factor (RF) assay Antinuclear antibody (ANA) assay • Urine Analysis Test • • •
• MRI And CAT scan • Blood Examination Erythrocyte sedimentation rate (ESR) C-reactive protein (CRP) level Complete blood count (CBC) Rheumatoid factor (RF) assay Antinuclear antibody (ANA) assay • Urine Analysis Test • • •
 The Sun is Rising for Patients with Rheumatic Diseases: The Future is Bright
The Sun is Rising for Patients with Rheumatic Diseases: The Future is Bright


