5cacb0099868f06723c3f11fd3e5cbef.ppt
- Количество слайдов: 25
Rheumatoid arthritis in the brain- a diagnosis of exclusion Dr Suzanne O’Leary Sp. R Neuroradiology Frenchay Hospital Bristol UK
Bristol case • 59 year old female patient • Known diagnosis of Rheumatoid arthritis • RA affecting joints only. Inactive at time of this presentation • Otherwise well • No previous neurological condition
Presentation • Severe headache that had persisted for 2 weeks • Headache had been sudden in onset and very severe. • Initially a diagnosis of SAH was considered
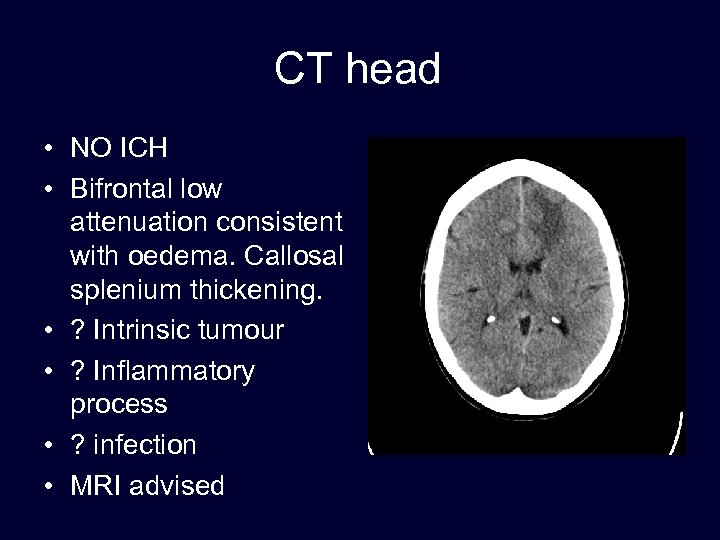
CT head • NO ICH • Bifrontal low attenuation consistent with oedema. Callosal splenium thickening. • ? Intrinsic tumour • ? Inflammatory process • ? infection • MRI advised
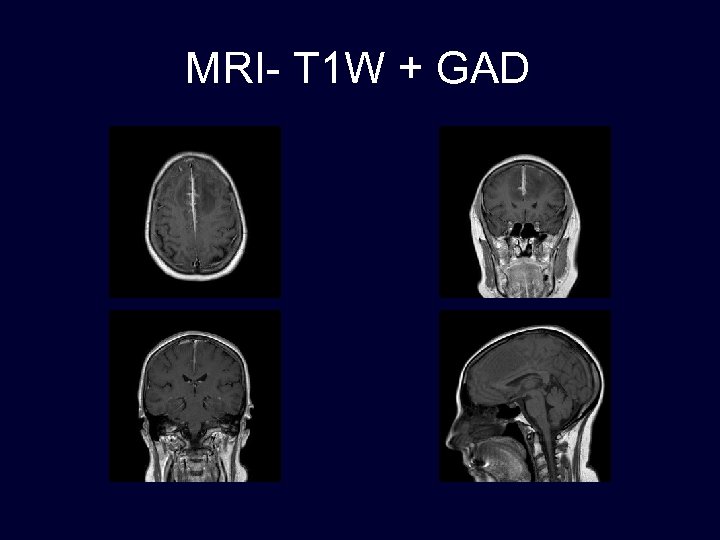
Deterioration • Patient becoming increasingly confused and absent episodes. • Acyclovir started • ECG, CXR, FBC, MSU normal. • No evidence of infection. • ESR elevated • ANA positive • Rh. F positive
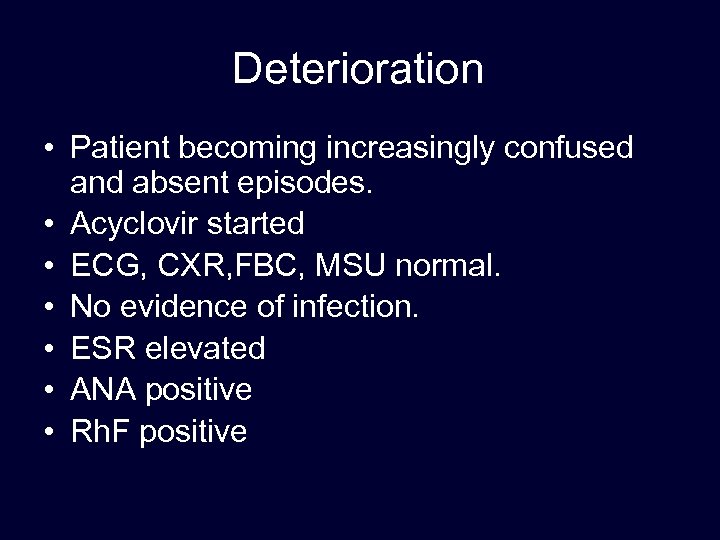
MRI FLAIR T 1 W DWI T 2 W
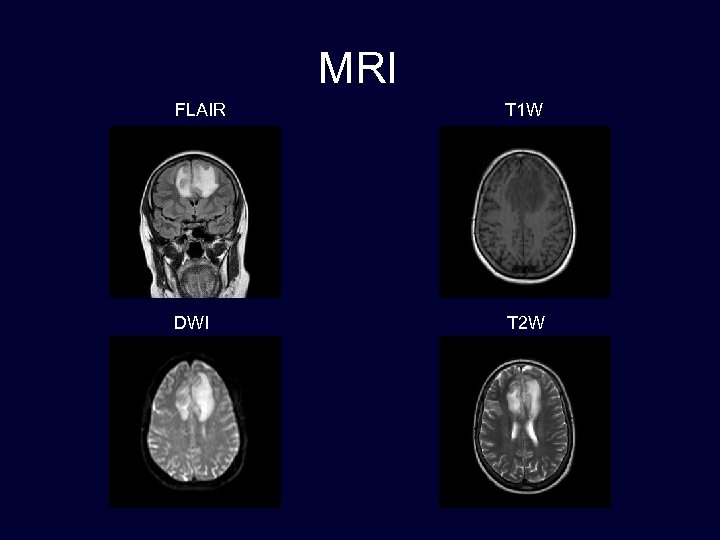
MRI- T 1 W + GAD
MRI findings • Post contrast images show leptomeningeal enhancement either side of the falx in the anterior interhemispheric fissure, with enhancement of the dura over the falx at this site. There is reactive oedema in the adjacent anteromedial frontal lobes. • Appearances are unusual but clearly demonstrate a meningeal process which may be inflammatory, reactive or malignant. Is there any abnormality on lumbar puncture?
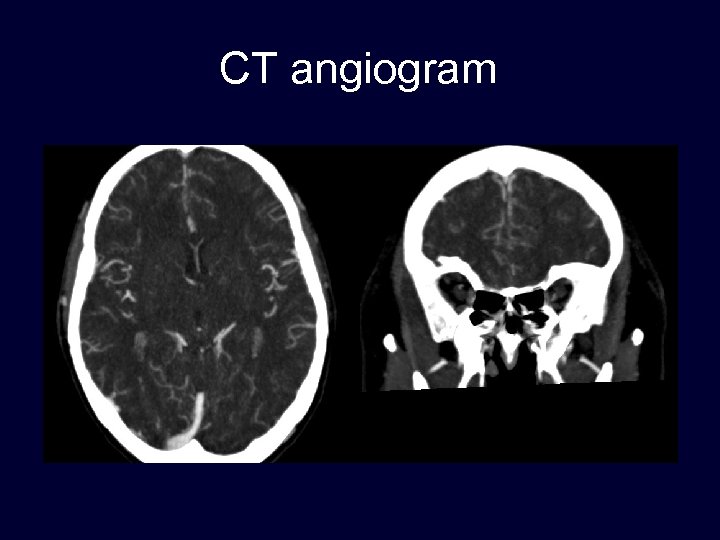
CT angiogram
CTA • The medial frontal lobes demonstrate paucity of vessels. • The vessels that are visible are irregular in outline. 10
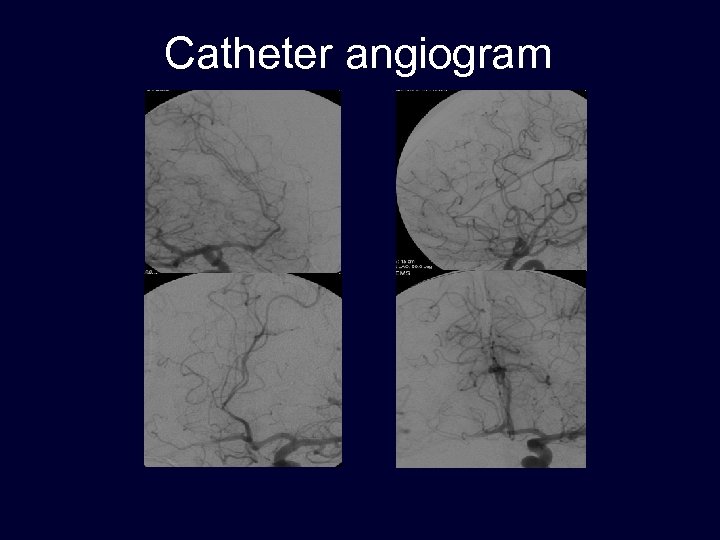
Catheter angiogram
Catheter angiogram findings • There is abnormality in the vasculature supplying the medial frontal lobes bilaterally where there is slight reduction in vascularity and evidence of vascular irregularity including general stenosis with pruning and beading in places. There is no arteriovenous shunting. There does not appear to be involvement of any of the more proximal vessels. No other territories appear to be involved. • The abnormal vasculature corresponds to the abnormality on the CT and MRI. This raises the possibility of a vasculitic process accounting for the changes on the CT and in the anterior cerebral artery distribution predominantly callosal marginal.
Lumbar puncture • • Lymphocytosis Protein increase Glucose reduced Gram stain, ZN stain, India ink, mycobacterium and fungal cultures were negative. • Treated with Acyclovir on admission
Brain biopsy- Rheumatoid meningitis and vasculitis • Fibrinoid necrosis • Surrounded by histiocytes • Dense infiltrate of plasma cells within the subarachnoid space • Vasculitis of the leptomeninges and underlying cortex • Staining for bacteria, acid-fast bacillii, fungi and spirochetes was negative.
Diagnosis • Definite diagnosis of Rheumatoid meningitis and vasculitis made • Patient started on steroids and immunosuppressants • Clinical improvement within days • Discharged home after 7 days.
Rheumatoid Arthritis • Systemic inflammatory disorder, usually affecting the joints. • Extra-articular sites affected, including skin, lungs, eyes and blood vessels. • Blood vessels are involved, it is medium and small vessels of the skin and peripheral nervous system which are more commonly affected. • There are case reports of it affecting the brain, causing a cerebral vasculitis and rarely causes meningitis or pachymeningitis. • The neurological sequelae of RA cause death in 18. 6% of cases. • This is often a diagnosis of exclusion, and brain biopsy may be required.
Rheumatoid arthritis and the brain • • • Nervous system involvement with RA is uncommon. Neurologic complications are usually due to mass effect on the spinal cord or peripheral nerves from synovitis, pannus formation or subluxation Direct involvement of the CNS includes pachymeningitis, leptomeningitis and vasculitis. Rarer complications include organic brain syndrome and progressive multifocal leukoencephalopathy. CNS involvement can occur without typical extracranial patterns of RA. Neurologic symptoms of rheumatoid meningitis include cranial nerve dysfunction, seizure, mental status change, and hemiparesis or paraparesis. CSF analysis are usually abnormal, with an elevated protein level, occasional pleocytosis and a low glucose level. The diagnosis is one of exclusion, and all other causes of leptomeningitis and pachymeningitis must be considered Diagnosis is aided by a clinical diagnosis of RA, positive serologic results for rheumatoid factors, and the pathologic visualization of rheumatoid nodules.
Leptomeningitis/ Pachymeningitis • Lepto/Pachymeningitis contains a nonspecific infiltrate of mononuclear cells, particularly plasma cells. Less frequently seen areas of necrosis and multinucleated giant cells. Although they may be present in 60% of cases, rheumatic nodules often do not cause symptoms. The presence of epithelioid granulomas typically in the cranial meninges or choroid plexus confirms the diagnosis of rheumatoid meningitis but is not a specific finding. • CNS symptoms can be caused by a CNS vasculitis due to a lymphoplasmacytic infiltrate in the vessel walls. This involves both parenchymal and meningeal vessels. Large vessels, such as the middle cerebral artery, are usually spared.
Leptomeningitis/ Pachymeningitis • Infection-TB, fungal, cysticercosis, pyogenic • Tumour- lymphoma, leukaemia, carcinomatosis, meningioma • Inflammation- sarcoid, Whipples, Behcets, Sjogrens, Wegners, Temporal arteritis, RA • Idiopathic pachymeningitis • Intracerebral hypotension. 19
Conclusion • Rare complication of RA • Need to exclude all other causes of lepto/pachymeningitis. • Brain biopsy may be necessary • Poor prognosis- 6 months 20
References • 1. Jones SE, Belsley NA, Mcloud TC, Mullins ME. Rheumatoid Meningitis: Radiologic and Pathologic correlation. AJR 2006; 186: 1181 -1183. • 2. Tan HJ, Raymond AA, Phadke PP, Rozman Z. Rheumatoid pachymeningitis. Singapore Med J 2004; 45(7): 337 • 3. Agildere AM, Tutar NU, Yucel E, Coskun M. Case report. Pachymeningitis and optic neuritis in rheumatoid arthritis: MRI findings. BR J Radiol 1999; 72: 404 -7 • 4. William TC, Drew JM, Rizzo M, Ryals TJ, Sato Y, Bell WE. Evaluation of pachymeningitis by contrast-enhanced MR imaging in a patient with rheumatoid disease. AM J Neuroradiol 1990: 11: 1247 -8. 21
Thank you 22 22

23

24

25
5cacb0099868f06723c3f11fd3e5cbef.ppt