Rheumatoid Arthritis DOM MR Week of 9/8/2008 Rozina




370-dommr_rheumatoid_arthritis.ppt
- Количество слайдов: 60
 Rheumatoid Arthritis DOM MR Week of 9/8/2008 Rozina Mithani
Rheumatoid Arthritis DOM MR Week of 9/8/2008 Rozina Mithani
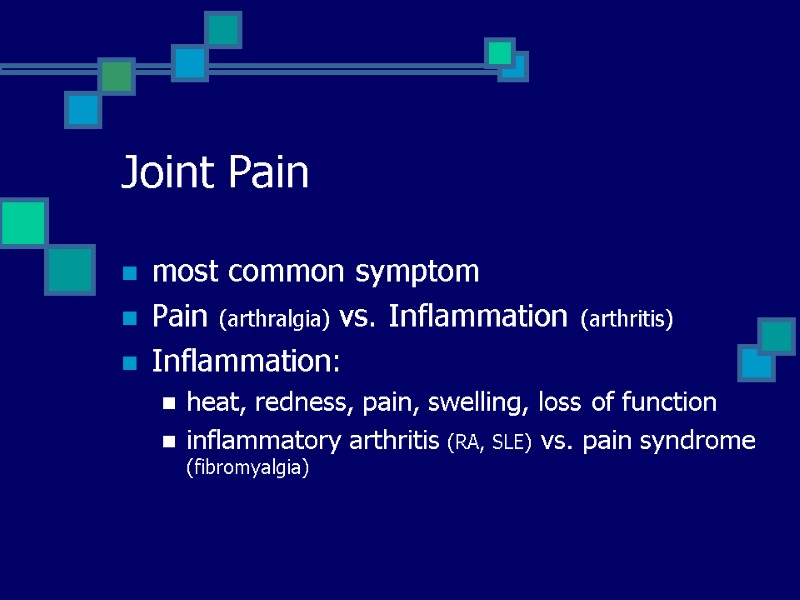
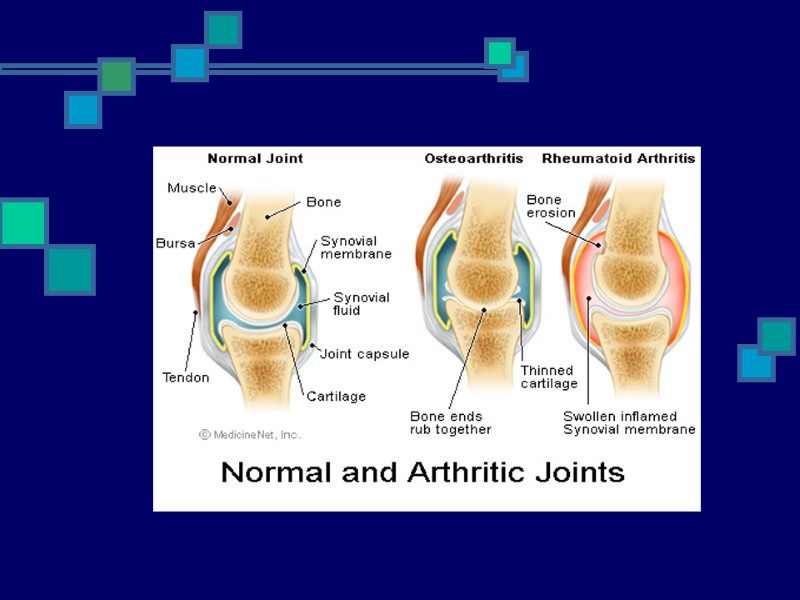
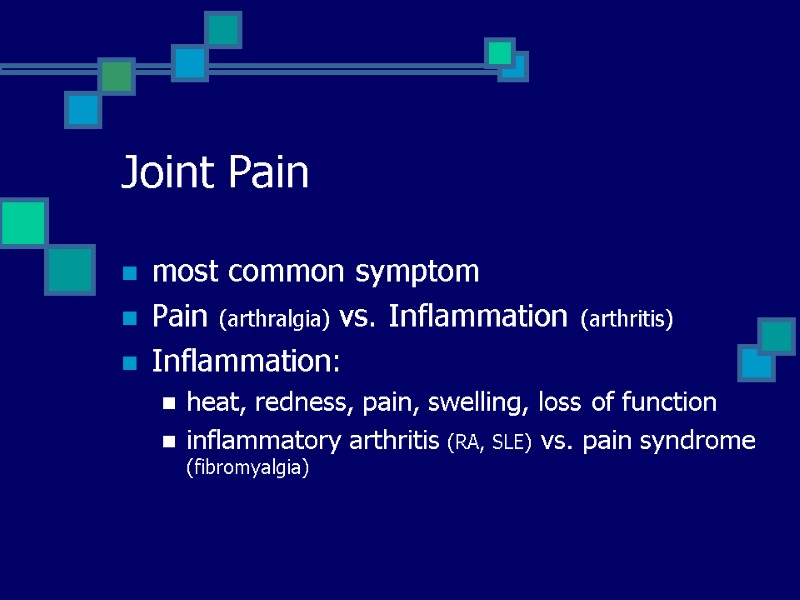 Joint Pain most common symptom Pain (arthralgia) vs. Inflammation (arthritis) Inflammation: heat, redness, pain, swelling, loss of function inflammatory arthritis (RA, SLE) vs. pain syndrome (fibromyalgia)
Joint Pain most common symptom Pain (arthralgia) vs. Inflammation (arthritis) Inflammation: heat, redness, pain, swelling, loss of function inflammatory arthritis (RA, SLE) vs. pain syndrome (fibromyalgia)
 Number of Joints Affected Inflammatory vs. Non-Inflammatory
Number of Joints Affected Inflammatory vs. Non-Inflammatory
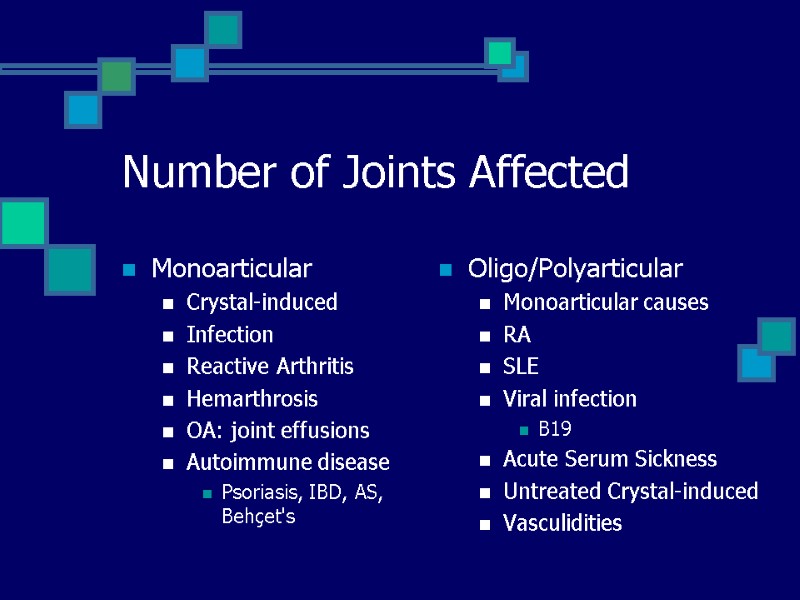
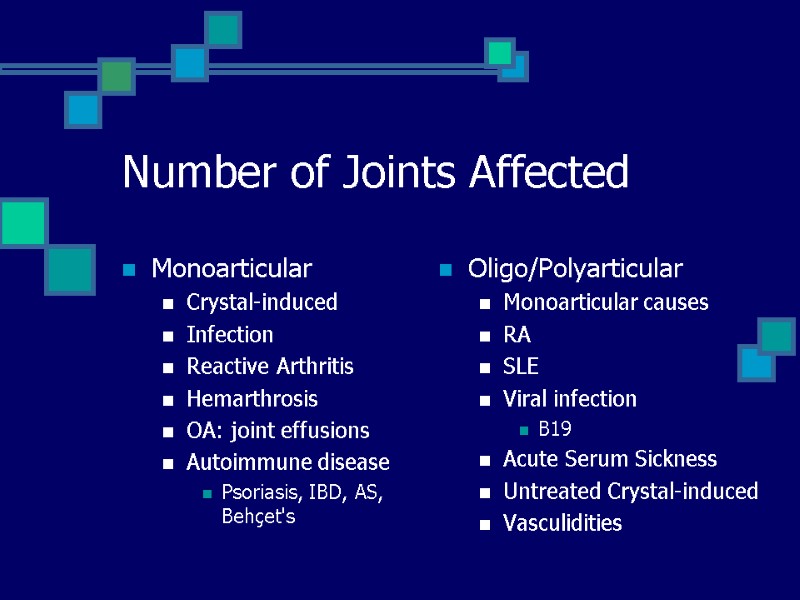 Number of Joints Affected Monoarticular Crystal-induced Infection Reactive Arthritis Hemarthrosis OA: joint effusions Autoimmune disease Psoriasis, IBD, AS, Behçet's Oligo/Polyarticular Monoarticular causes RA SLE Viral infection B19 Acute Serum Sickness Untreated Crystal-induced Vasculidities
Number of Joints Affected Monoarticular Crystal-induced Infection Reactive Arthritis Hemarthrosis OA: joint effusions Autoimmune disease Psoriasis, IBD, AS, Behçet's Oligo/Polyarticular Monoarticular causes RA SLE Viral infection B19 Acute Serum Sickness Untreated Crystal-induced Vasculidities
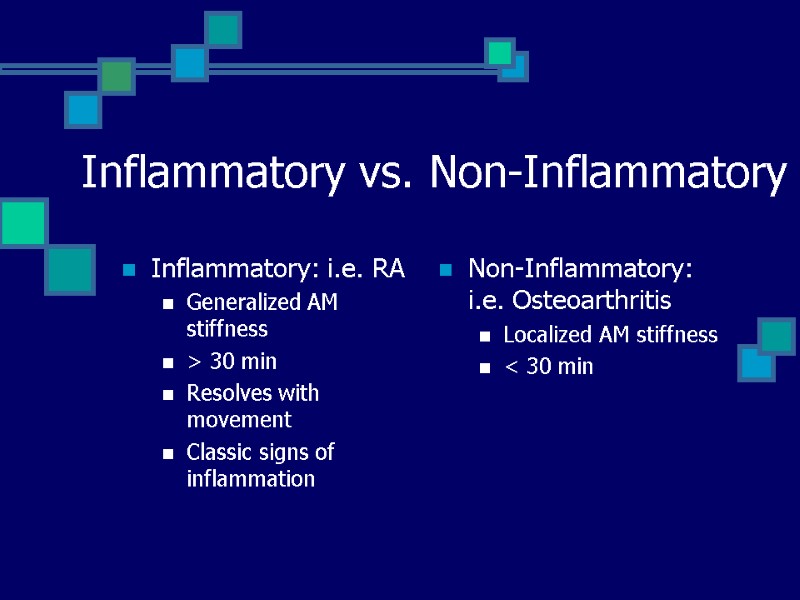
 Inflammatory vs. Non-Inflammatory Inflammatory: i.e. RA Generalized AM stiffness > 30 min Resolves with movement Classic signs of inflammation Non-Inflammatory: i.e. Osteoarthritis Localized AM stiffness < 30 min
Inflammatory vs. Non-Inflammatory Inflammatory: i.e. RA Generalized AM stiffness > 30 min Resolves with movement Classic signs of inflammation Non-Inflammatory: i.e. Osteoarthritis Localized AM stiffness < 30 min
 Arthrocentesis Confirm diagnoses Differentiate between inflammatory & noninflammatory Therapeutic/Adjunct to Antibiotics Labs: cell count w/diff crystal analysis Gram stain & Culture WBC >2000/µL indicates inflammatory arthritis Arthroscopy Evaluate ligamentous & cartilaginous integrity Biopsy Infectioun: aspirate thick or loculated fluid
Arthrocentesis Confirm diagnoses Differentiate between inflammatory & noninflammatory Therapeutic/Adjunct to Antibiotics Labs: cell count w/diff crystal analysis Gram stain & Culture WBC >2000/µL indicates inflammatory arthritis Arthroscopy Evaluate ligamentous & cartilaginous integrity Biopsy Infectioun: aspirate thick or loculated fluid
 Rheumatoid Arthritis
Rheumatoid Arthritis
 RA Systemic inflammatory autoimmune disorder ~1% of population Onset: 52 years 40-70 years of age <60 - 3-5:1 female predominance
RA Systemic inflammatory autoimmune disorder ~1% of population Onset: 52 years 40-70 years of age <60 - 3-5:1 female predominance
 Genetics Increased incidence among Pima & Chippewa Native American tribes (5%) Genetic & Environmental HLA-DRB1*0401 & HLA-DRB1*0404 Increased risk Increased joint damage Increased joint surgery
Genetics Increased incidence among Pima & Chippewa Native American tribes (5%) Genetic & Environmental HLA-DRB1*0401 & HLA-DRB1*0404 Increased risk Increased joint damage Increased joint surgery
 Pathophysiology
Pathophysiology
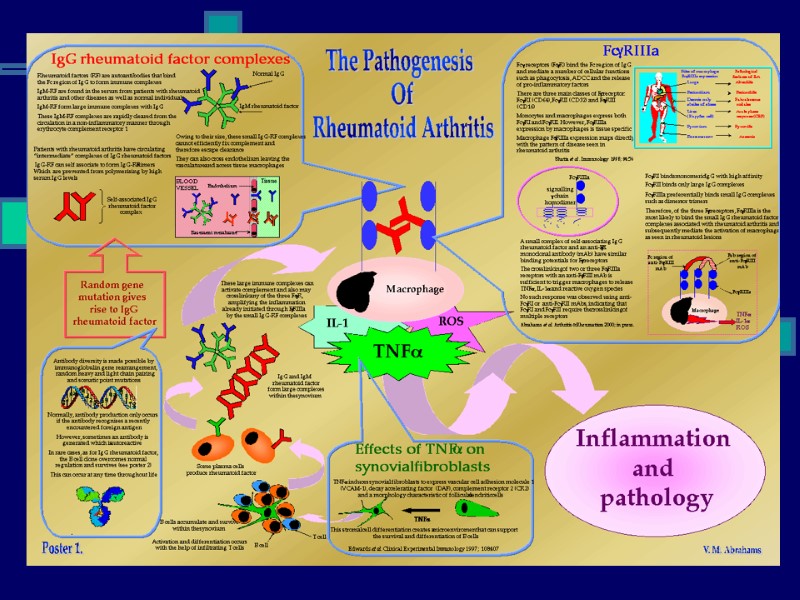
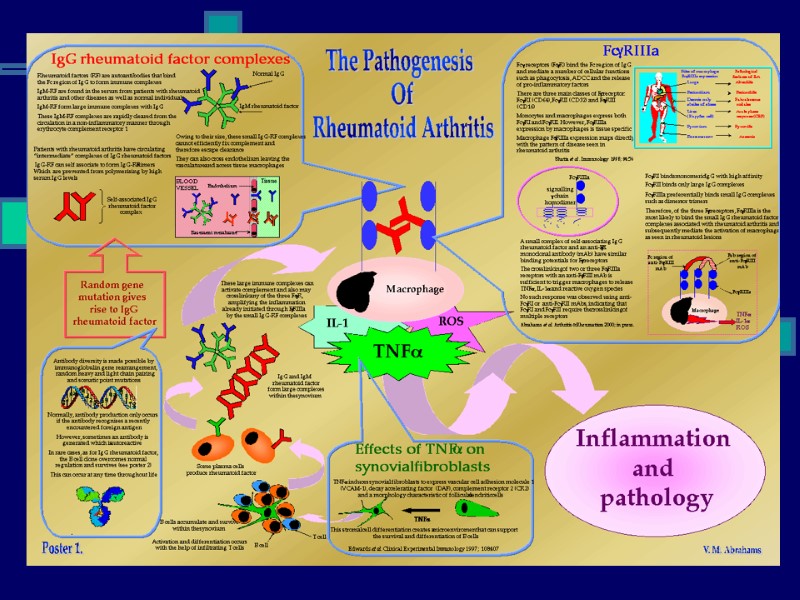
 Immunology Macrophages: Produce cytokines Cytokines (TNF-α) cause systemic features Release chemokines recruit PMNs into synovial fluid/membrane TNF-α & IL-1: Proliferation of T cells Activation of B cells Initiates proinflammatory/joint-damaging processes TH-1 cells: Mediate disease processes Activate B cells B cells: Release cytokines Plasma cells that produce Ab Osteoclasts: Bone erosion Juxta-articular & Systemic osteoporosis
Immunology Macrophages: Produce cytokines Cytokines (TNF-α) cause systemic features Release chemokines recruit PMNs into synovial fluid/membrane TNF-α & IL-1: Proliferation of T cells Activation of B cells Initiates proinflammatory/joint-damaging processes TH-1 cells: Mediate disease processes Activate B cells B cells: Release cytokines Plasma cells that produce Ab Osteoclasts: Bone erosion Juxta-articular & Systemic osteoporosis
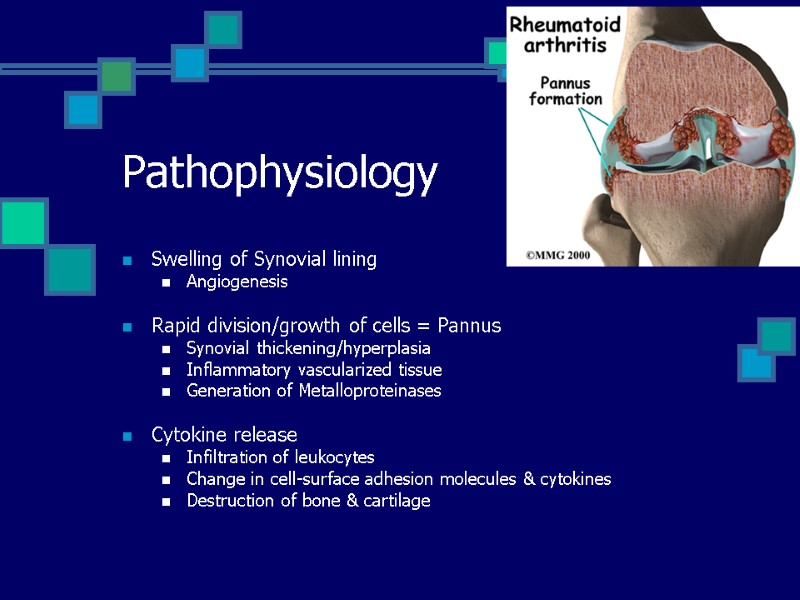
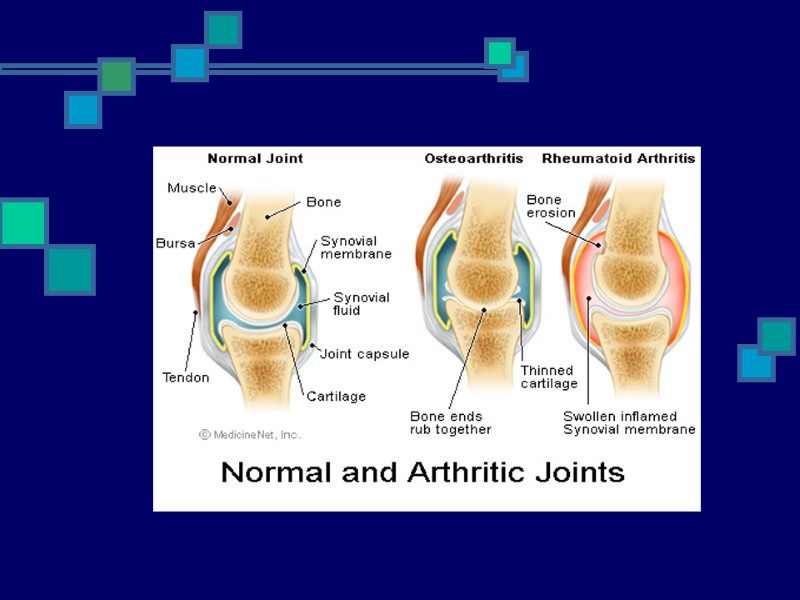
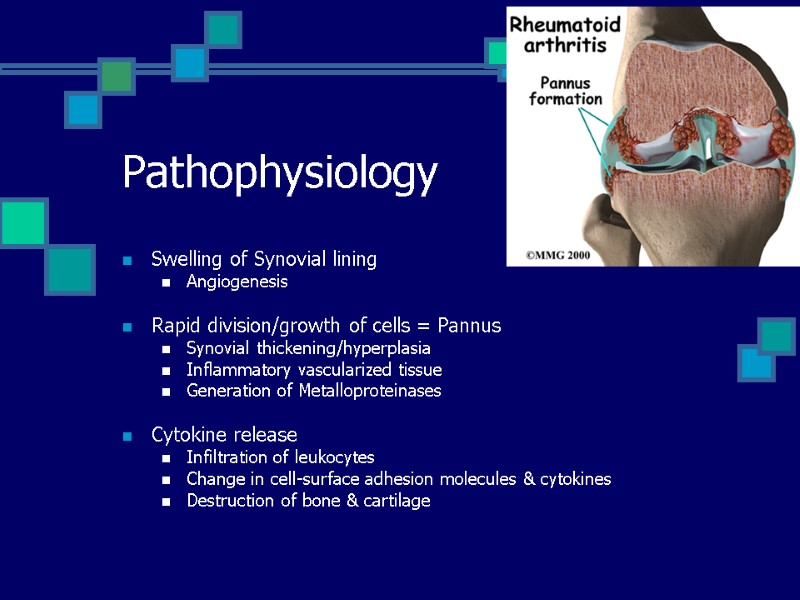 Pathophysiology Swelling of Synovial lining Angiogenesis Rapid division/growth of cells = Pannus Synovial thickening/hyperplasia Inflammatory vascularized tissue Generation of Metalloproteinases Cytokine release Infiltration of leukocytes Change in cell-surface adhesion molecules & cytokines Destruction of bone & cartilage
Pathophysiology Swelling of Synovial lining Angiogenesis Rapid division/growth of cells = Pannus Synovial thickening/hyperplasia Inflammatory vascularized tissue Generation of Metalloproteinases Cytokine release Infiltration of leukocytes Change in cell-surface adhesion molecules & cytokines Destruction of bone & cartilage
 Bottom Line Proliferation Destruction of joints Disability
Bottom Line Proliferation Destruction of joints Disability
 Disease Trigger Subclinical vs. Viral trigger Lab manifestations up to 10 yrs before clinical RF & anti-CCP (anti–cyclic citrullinated peptide) Ab Increased CRP subclinical inflammatory disease ADLs: > 50% of pts stop working w/i 5-10 years of disease onset ~ 80% disabled to some degree > 20 years Life expectancy: decreased by 3-18 years
Disease Trigger Subclinical vs. Viral trigger Lab manifestations up to 10 yrs before clinical RF & anti-CCP (anti–cyclic citrullinated peptide) Ab Increased CRP subclinical inflammatory disease ADLs: > 50% of pts stop working w/i 5-10 years of disease onset ~ 80% disabled to some degree > 20 years Life expectancy: decreased by 3-18 years
 Clinical Presentation Gradual onset Stiffness & Swelling Intermittent or Migratory involvement Extraarticular manifestations Myalgia, fatigue, low-grade fever, wt loss, depression
Clinical Presentation Gradual onset Stiffness & Swelling Intermittent or Migratory involvement Extraarticular manifestations Myalgia, fatigue, low-grade fever, wt loss, depression
 Stiffness & Swelling Pain with pressure to joint Pain with movement of joint Swelling due to hypertrophy Effusion Heat Redness
Stiffness & Swelling Pain with pressure to joint Pain with movement of joint Swelling due to hypertrophy Effusion Heat Redness
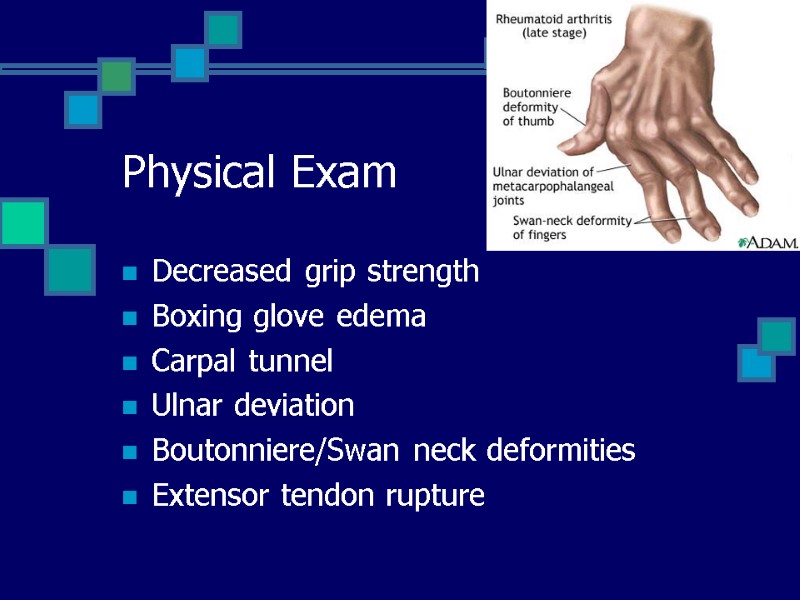
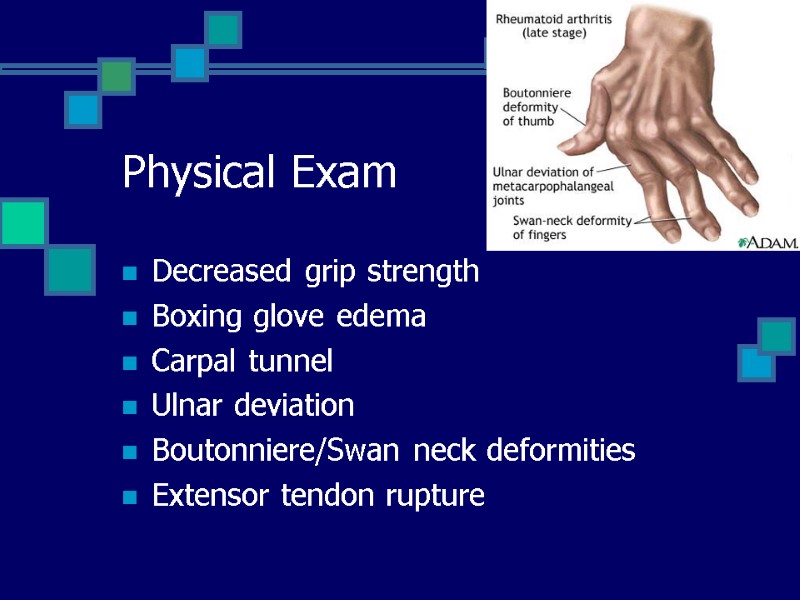 Physical Exam Decreased grip strength Boxing glove edema Carpal tunnel Ulnar deviation Boutonniere/Swan neck deformities Extensor tendon rupture
Physical Exam Decreased grip strength Boxing glove edema Carpal tunnel Ulnar deviation Boutonniere/Swan neck deformities Extensor tendon rupture
 Extraarticular Involvement Anemia Rheumatoid nodules Pleuropericarditis Neuropathy Episcleritis, Scleritis Splenomegaly Sjogren’s Vasculitis
Extraarticular Involvement Anemia Rheumatoid nodules Pleuropericarditis Neuropathy Episcleritis, Scleritis Splenomegaly Sjogren’s Vasculitis
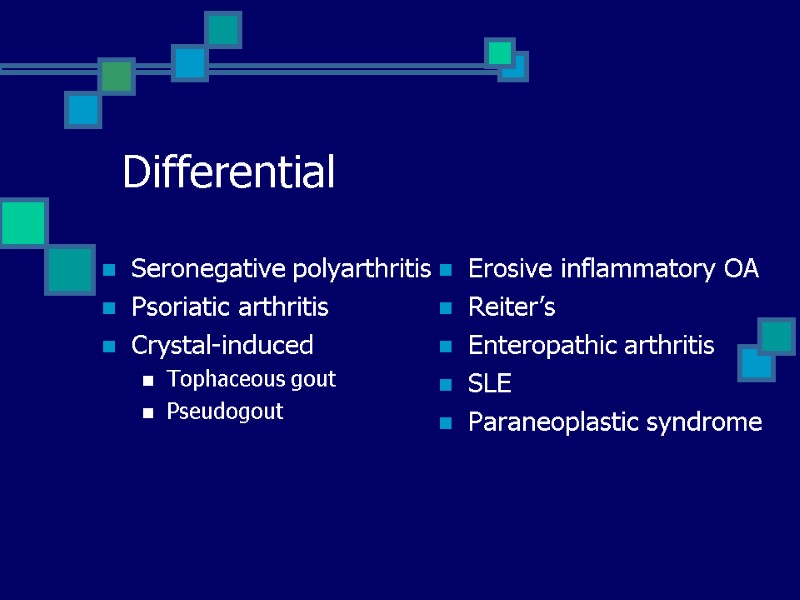 Differential Seronegative polyarthritis Psoriatic arthritis Crystal-induced Tophaceous gout Pseudogout Erosive inflammatory OA Reiter’s Enteropathic arthritis SLE Paraneoplastic syndrome
Differential Seronegative polyarthritis Psoriatic arthritis Crystal-induced Tophaceous gout Pseudogout Erosive inflammatory OA Reiter’s Enteropathic arthritis SLE Paraneoplastic syndrome
 Diagnostic Criteria
Diagnostic Criteria
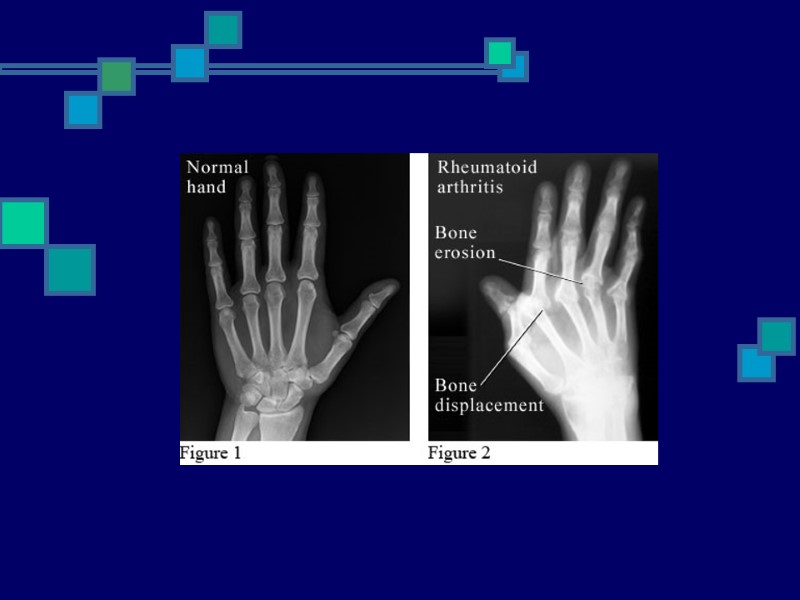
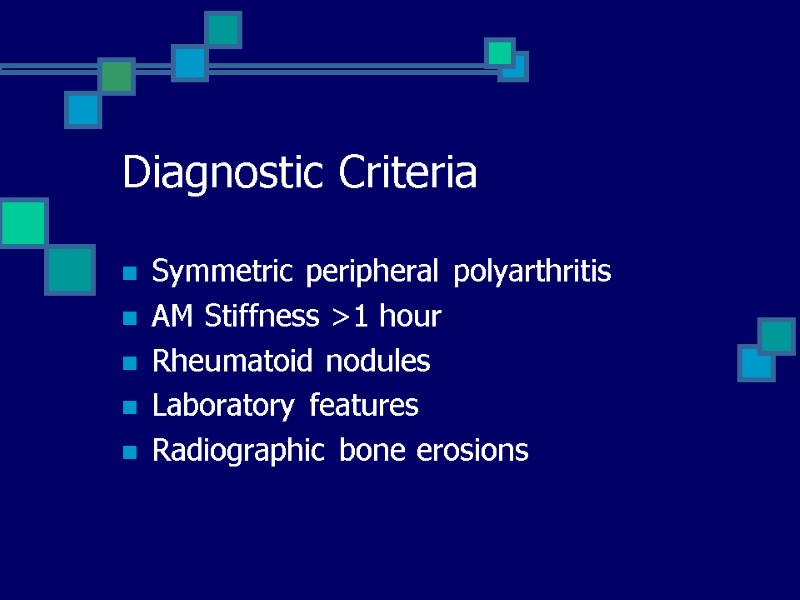 Diagnostic Criteria Symmetric peripheral polyarthritis AM Stiffness >1 hour Rheumatoid nodules Laboratory features Radiographic bone erosions
Diagnostic Criteria Symmetric peripheral polyarthritis AM Stiffness >1 hour Rheumatoid nodules Laboratory features Radiographic bone erosions
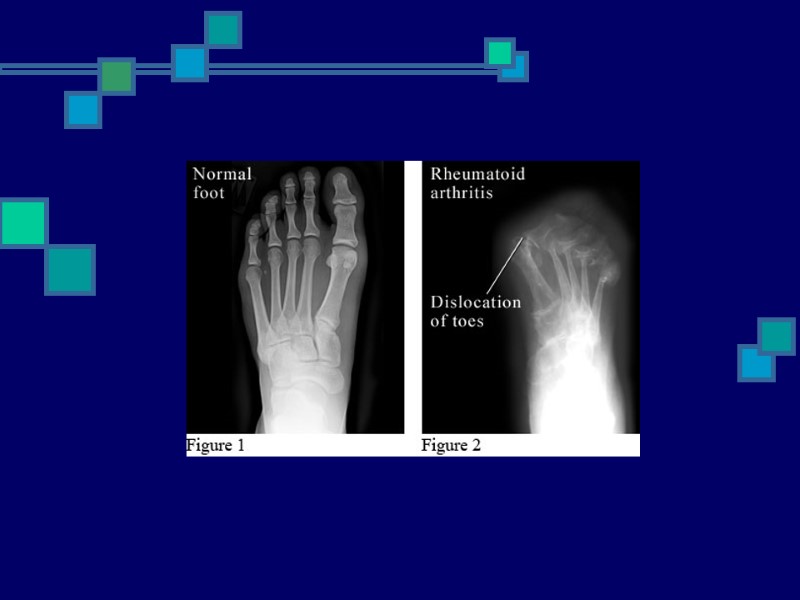
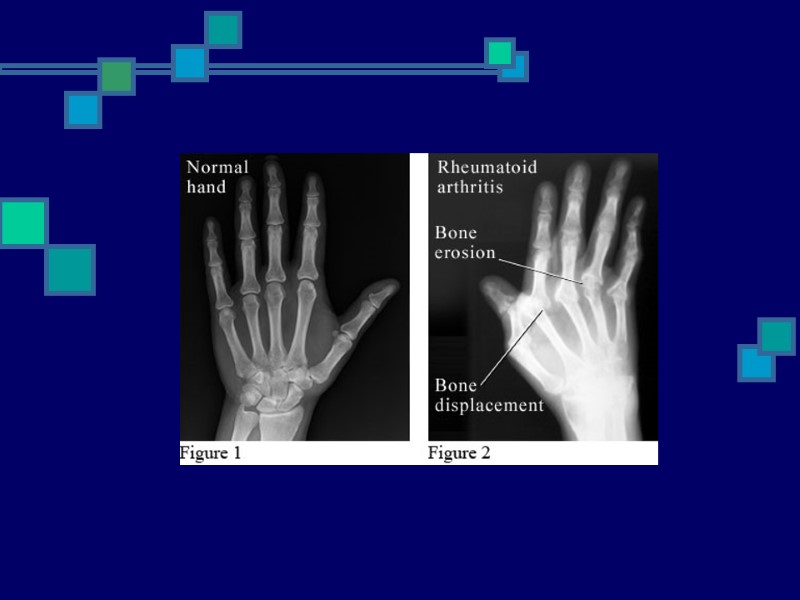
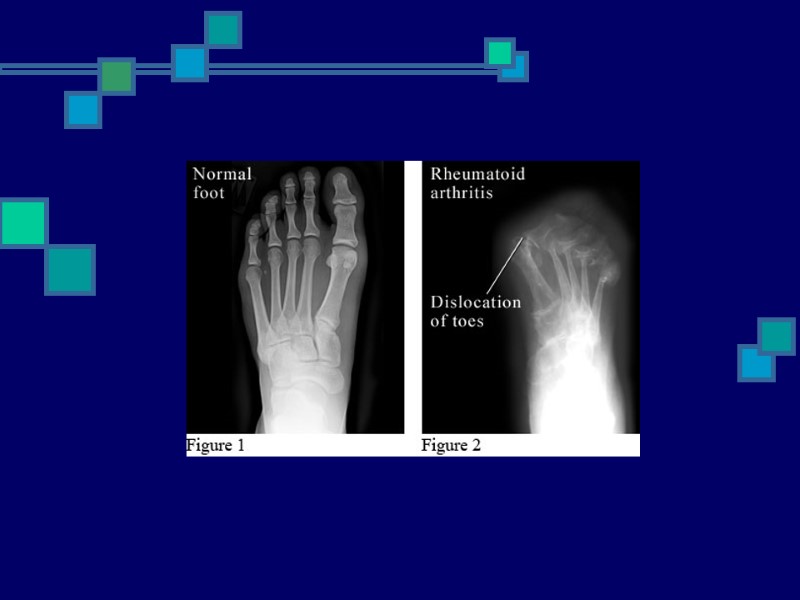
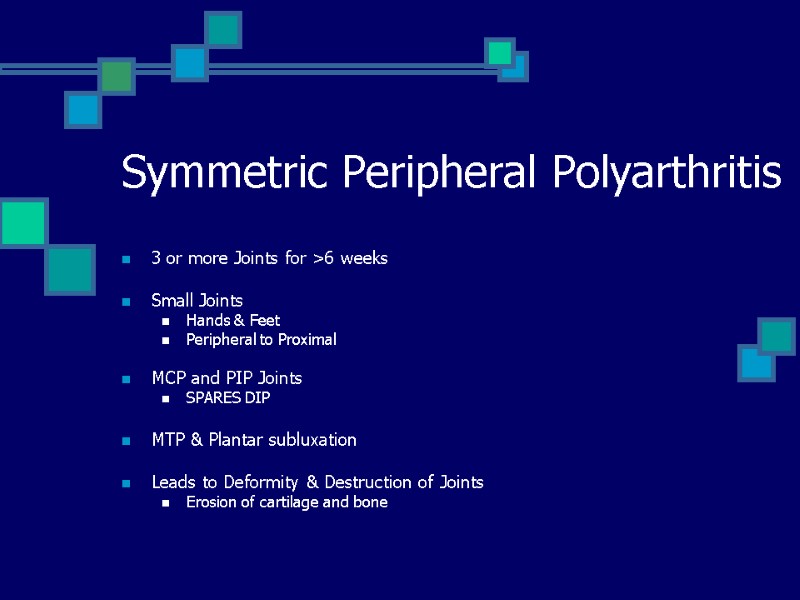 Symmetric Peripheral Polyarthritis 3 or more Joints for >6 weeks Small Joints Hands & Feet Peripheral to Proximal MCP and PIP Joints SPARES DIP MTP & Plantar subluxation Leads to Deformity & Destruction of Joints Erosion of cartilage and bone
Symmetric Peripheral Polyarthritis 3 or more Joints for >6 weeks Small Joints Hands & Feet Peripheral to Proximal MCP and PIP Joints SPARES DIP MTP & Plantar subluxation Leads to Deformity & Destruction of Joints Erosion of cartilage and bone
 Stiffness AM or after Prolonged Inactivity Bilateral In/Around Joints > 1 hours Reflects severe joint inflammation Better with movement Present >6 weeks
Stiffness AM or after Prolonged Inactivity Bilateral In/Around Joints > 1 hours Reflects severe joint inflammation Better with movement Present >6 weeks
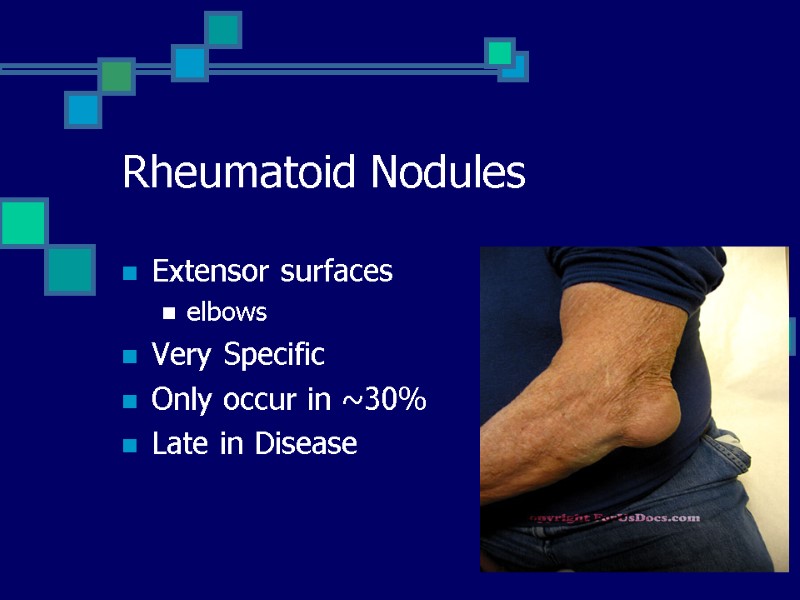
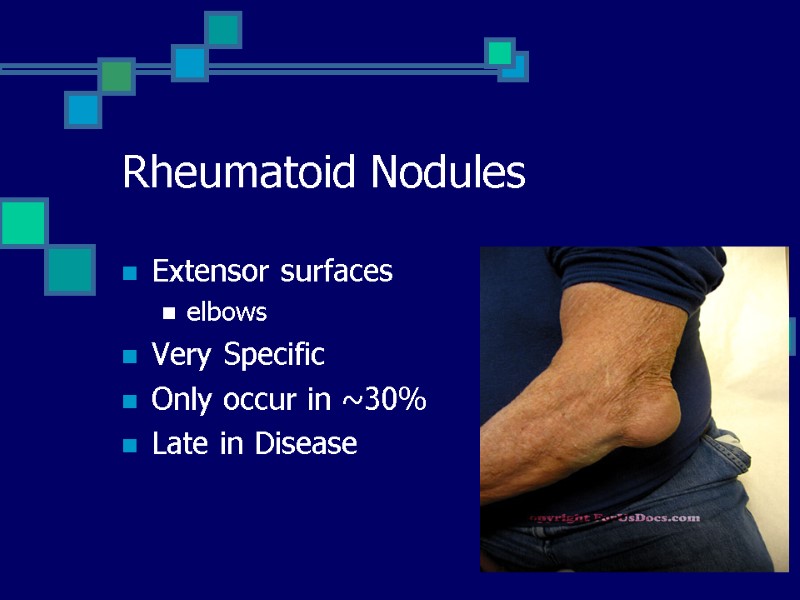 Rheumatoid Nodules Extensor surfaces elbows Very Specific Only occur in ~30% Late in Disease
Rheumatoid Nodules Extensor surfaces elbows Very Specific Only occur in ~30% Late in Disease
 Laboratory Features RF 70-80% of pts Overlap with HCV/Cryoglobulinemia Anti-Cyclic Citrulline Peptide (anti-CCP) Rare overlap with HCV Acute Phase reactants ESR, CRP monitoring disease activity
Laboratory Features RF 70-80% of pts Overlap with HCV/Cryoglobulinemia Anti-Cyclic Citrulline Peptide (anti-CCP) Rare overlap with HCV Acute Phase reactants ESR, CRP monitoring disease activity
 Rheumatoid Factor IgM against IgG IgM+ pts: more severe disease & poorer outcome Non-specific SLE, Sjögren's, Sarcoidosis, Chronic infections
Rheumatoid Factor IgM against IgG IgM+ pts: more severe disease & poorer outcome Non-specific SLE, Sjögren's, Sarcoidosis, Chronic infections
 Anti-CCP IgG against synovial membrane peptides damaged via inflammation Value in IgM-RF negative Sensitivity (65%) & Specificity (95%) Predictive of Erosive Disease Disease severity Radiologic progression Poor functional outcomes
Anti-CCP IgG against synovial membrane peptides damaged via inflammation Value in IgM-RF negative Sensitivity (65%) & Specificity (95%) Predictive of Erosive Disease Disease severity Radiologic progression Poor functional outcomes
 Other Lab Abnormalities AOCD Thrombocytosis Leukocytosis ANA 30-40% Inflammatory synovial fluid Hypoalbuminemia
Other Lab Abnormalities AOCD Thrombocytosis Leukocytosis ANA 30-40% Inflammatory synovial fluid Hypoalbuminemia
 Radiology Evaluate disease activity & joint damage Bony decalcification Baseline AP views Initiation of DMARDs
Radiology Evaluate disease activity & joint damage Bony decalcification Baseline AP views Initiation of DMARDs
 Radiological Studies Plain Films Bilateral hands & feet Only 25% of lesions Less expensive Through bone cortex around joint margins Color Doppler U/S & MRI Early signs of damage i.e. Erosions Bone Edema - even with normal findings on radiography
Radiological Studies Plain Films Bilateral hands & feet Only 25% of lesions Less expensive Through bone cortex around joint margins Color Doppler U/S & MRI Early signs of damage i.e. Erosions Bone Edema - even with normal findings on radiography
 Disease Severity
Disease Severity
 Arthralgias >3 inflamed joints Mild functional limitation Minimally elevated ESR & CRP No erosions/cartilage loss No extraarticular disease i.e. anemia Mild Disease
Arthralgias >3 inflamed joints Mild functional limitation Minimally elevated ESR & CRP No erosions/cartilage loss No extraarticular disease i.e. anemia Mild Disease
 Moderate Disease 6-20 Inflamed joints Moderate functional limitation Elevated ESR/CRP Radiographic evidence of inflammation No extraarticular disease
Moderate Disease 6-20 Inflamed joints Moderate functional limitation Elevated ESR/CRP Radiographic evidence of inflammation No extraarticular disease
 Severe Disease >20 persistently inflamed joints Rapid decline in functional capacity Radiographic evidence of rapid progession of bony erosions & loss of cartilage Extraarticular disease: AOCD, Hypoalbuminemia
Severe Disease >20 persistently inflamed joints Rapid decline in functional capacity Radiographic evidence of rapid progession of bony erosions & loss of cartilage Extraarticular disease: AOCD, Hypoalbuminemia
 Prognostic Features RF & Anti-CCP antibodies Early development of multiple inflamed joints and joint erosions Severe functional limitation Female HLA epitope presence Lower socioeconomic status & Less education Persistent joint inflammation for >12 weeks
Prognostic Features RF & Anti-CCP antibodies Early development of multiple inflamed joints and joint erosions Severe functional limitation Female HLA epitope presence Lower socioeconomic status & Less education Persistent joint inflammation for >12 weeks
 CV Disease Leading cause of death ~50% 2x more likely to develop MI chronic, inflammatory vascular burden premature atherosclerosis MTX: elevated homocysteine levels Control inflammatory process = Decreased atherosclerosis/morbidity Lipid screening & treatment Control of obesity, Hyperhomocystinemia, DM, HTN ASA
CV Disease Leading cause of death ~50% 2x more likely to develop MI chronic, inflammatory vascular burden premature atherosclerosis MTX: elevated homocysteine levels Control inflammatory process = Decreased atherosclerosis/morbidity Lipid screening & treatment Control of obesity, Hyperhomocystinemia, DM, HTN ASA
 Other diseases 70% more likely to have a stroke 70% higher risk for developing infection 44x more likely to develop NHL
Other diseases 70% more likely to have a stroke 70% higher risk for developing infection 44x more likely to develop NHL
 Staging Early <3 months Established/Persistent 6-12 months End-stage Significant joint destruction Functional disability
Staging Early <3 months Established/Persistent 6-12 months End-stage Significant joint destruction Functional disability
 Management Early and aggressive disease control Rheumatologist Referral Early/Undiagnosed: NSAIDs, short course Corticosteroids Late/Uncontrolled: DMARD therapy depends on the presence or absence of joint damage, functional limitation, presence of predictive factors for poorer prognosis Goals achieve NED & inflammation no treatment to resolve erosions once they occur
Management Early and aggressive disease control Rheumatologist Referral Early/Undiagnosed: NSAIDs, short course Corticosteroids Late/Uncontrolled: DMARD therapy depends on the presence or absence of joint damage, functional limitation, presence of predictive factors for poorer prognosis Goals achieve NED & inflammation no treatment to resolve erosions once they occur
 Treatment Strategies
Treatment Strategies
 Therapy Non-Pharmacologic: Referral to PT/OT Evaluate ADLs Assistive devices/splints Weight loss Smoking cessation Pharmacologic: Anti-inflammatory Interrupt progression Development of erosions Joint space narrowing
Therapy Non-Pharmacologic: Referral to PT/OT Evaluate ADLs Assistive devices/splints Weight loss Smoking cessation Pharmacologic: Anti-inflammatory Interrupt progression Development of erosions Joint space narrowing
 Pharmacologic Therapy Analgesics NSAIDs Glucocorticoids SAARD/DMARD Anticytokine therapy
Pharmacologic Therapy Analgesics NSAIDs Glucocorticoids SAARD/DMARD Anticytokine therapy
 Analgesics Topical Capsaicin Diclofenac Oral Tylenol Opiods
Analgesics Topical Capsaicin Diclofenac Oral Tylenol Opiods
 NSAIDs Analgesic, Antipyretic, Anti-inflammatory Don’t alter disease progression Ineffective in Erosive disease GI/Ulcers Hepatotoxicity Nephrotoxicity AIN Bleeding – antiplatelet Rash Aseptic meningitis
NSAIDs Analgesic, Antipyretic, Anti-inflammatory Don’t alter disease progression Ineffective in Erosive disease GI/Ulcers Hepatotoxicity Nephrotoxicity AIN Bleeding – antiplatelet Rash Aseptic meningitis
 Corticosteroids Decrease cytokines Slow Joint Inflammation Insomnia Emotional lability Fluid retention Weight gain HTN Hyperglycemia Osteoporosis Bisphosphonates: >5mg/d for >3months Cataracts Avascular necrosis Myopathy Psychosis
Corticosteroids Decrease cytokines Slow Joint Inflammation Insomnia Emotional lability Fluid retention Weight gain HTN Hyperglycemia Osteoporosis Bisphosphonates: >5mg/d for >3months Cataracts Avascular necrosis Myopathy Psychosis
 Disease modification SAARD – slow acting antirheumatic drugs DMARD – disease modifying antirheumatic drugs
Disease modification SAARD – slow acting antirheumatic drugs DMARD – disease modifying antirheumatic drugs
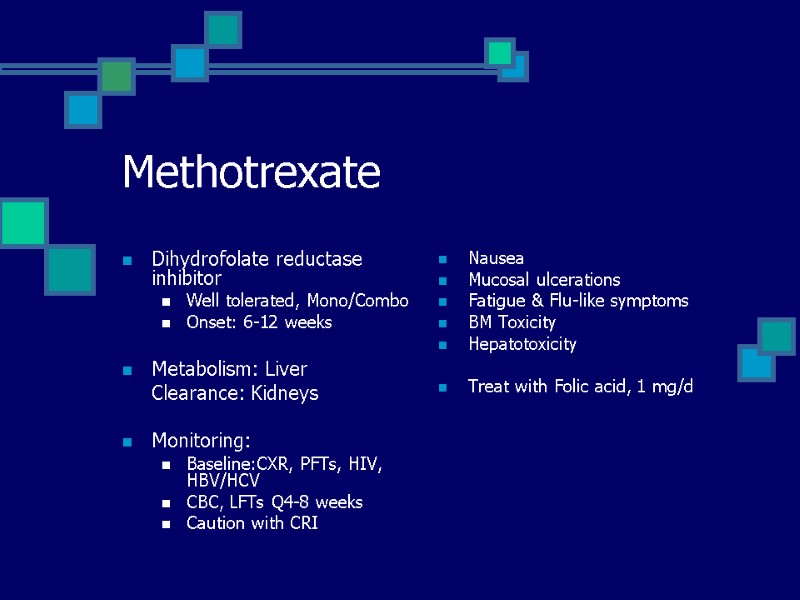
 Methotrexate Dihydrofolate reductase inhibitor Well tolerated, Mono/Combo Onset: 6-12 weeks Metabolism: Liver Clearance: Kidneys Monitoring: Baseline:CXR, PFTs, HIV, HBV/HCV CBC, LFTs Q4-8 weeks Caution with CRI Nausea Mucosal ulcerations Fatigue & Flu-like symptoms BM Toxicity Hepatotoxicity Treat with Folic acid, 1 mg/d
Methotrexate Dihydrofolate reductase inhibitor Well tolerated, Mono/Combo Onset: 6-12 weeks Metabolism: Liver Clearance: Kidneys Monitoring: Baseline:CXR, PFTs, HIV, HBV/HCV CBC, LFTs Q4-8 weeks Caution with CRI Nausea Mucosal ulcerations Fatigue & Flu-like symptoms BM Toxicity Hepatotoxicity Treat with Folic acid, 1 mg/d
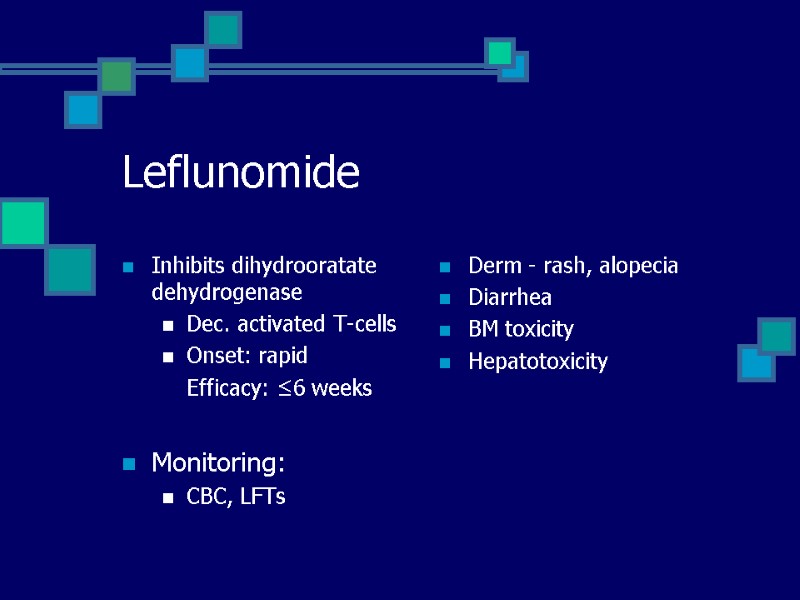
 Leflunomide Inhibits dihydrooratate dehydrogenase Dec. activated T-cells Onset: rapid Efficacy: ≤6 weeks Monitoring: CBC, LFTs Derm - rash, alopecia Diarrhea BM toxicity Hepatotoxicity
Leflunomide Inhibits dihydrooratate dehydrogenase Dec. activated T-cells Onset: rapid Efficacy: ≤6 weeks Monitoring: CBC, LFTs Derm - rash, alopecia Diarrhea BM toxicity Hepatotoxicity
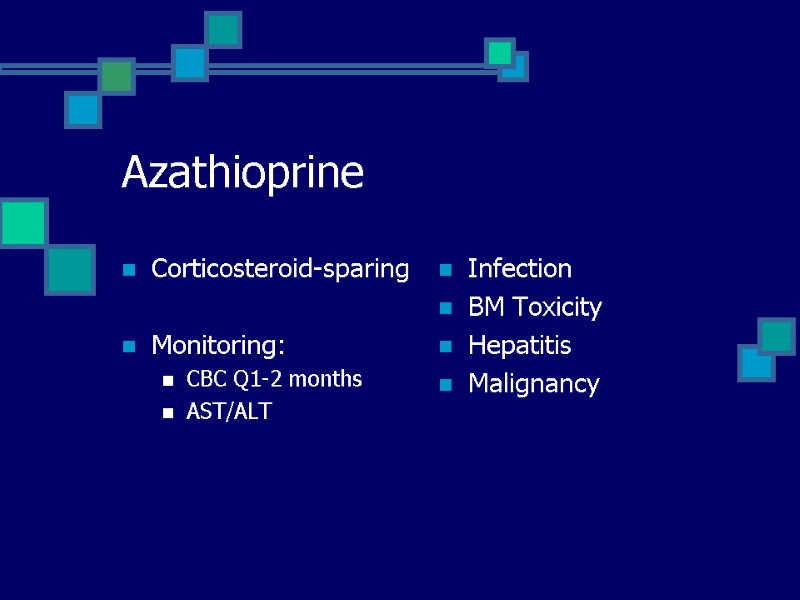
 Azathioprine Corticosteroid-sparing Monitoring: CBC Q1-2 months AST/ALT Infection BM Toxicity Hepatitis Malignancy
Azathioprine Corticosteroid-sparing Monitoring: CBC Q1-2 months AST/ALT Infection BM Toxicity Hepatitis Malignancy
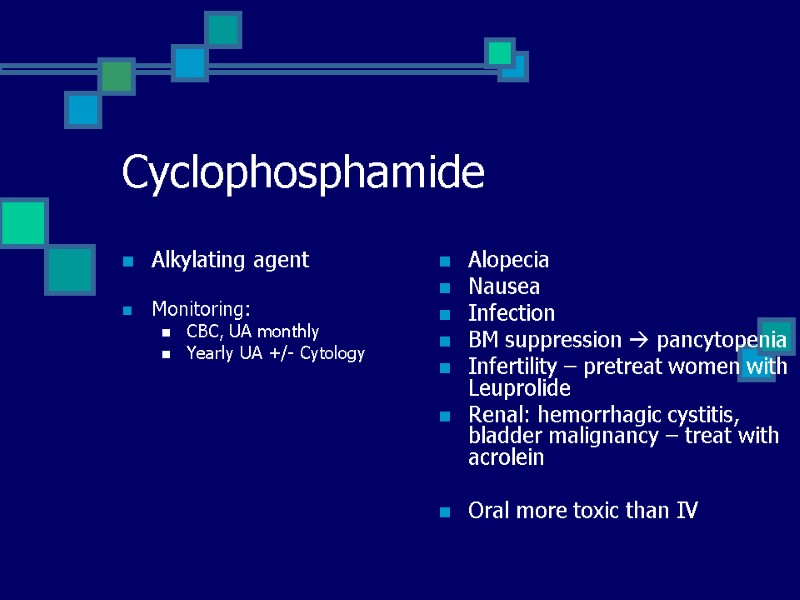
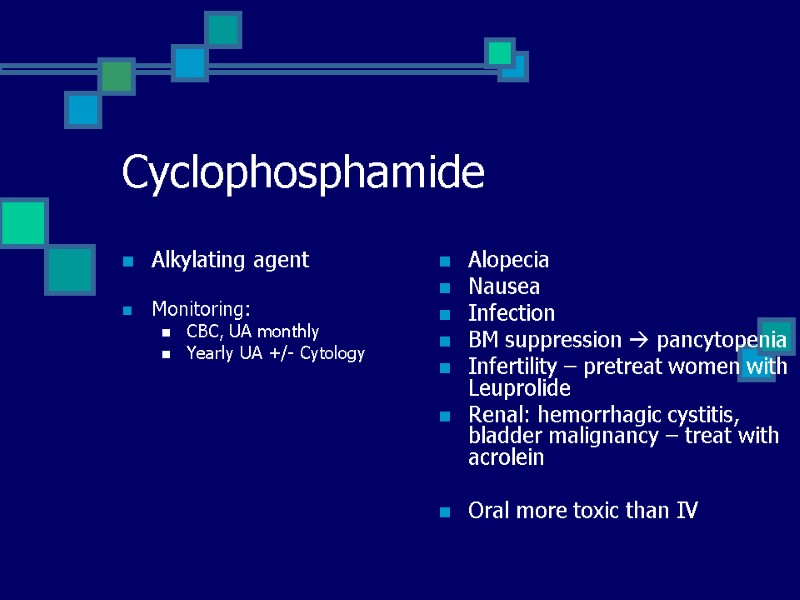 Cyclophosphamide Alkylating agent Monitoring: CBC, UA monthly Yearly UA +/- Cytology Alopecia Nausea Infection BM suppression pancytopenia Infertility – pretreat women with Leuprolide Renal: hemorrhagic cystitis, bladder malignancy – treat with acrolein Oral more toxic than IV
Cyclophosphamide Alkylating agent Monitoring: CBC, UA monthly Yearly UA +/- Cytology Alopecia Nausea Infection BM suppression pancytopenia Infertility – pretreat women with Leuprolide Renal: hemorrhagic cystitis, bladder malignancy – treat with acrolein Oral more toxic than IV
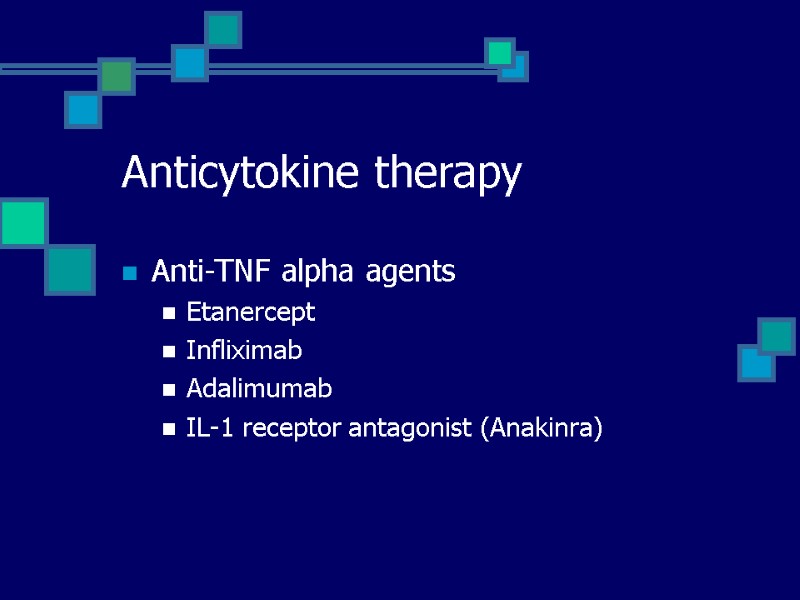 Anticytokine therapy Anti-TNF alpha agents Etanercept Infliximab Adalimumab IL-1 receptor antagonist (Anakinra)
Anticytokine therapy Anti-TNF alpha agents Etanercept Infliximab Adalimumab IL-1 receptor antagonist (Anakinra)
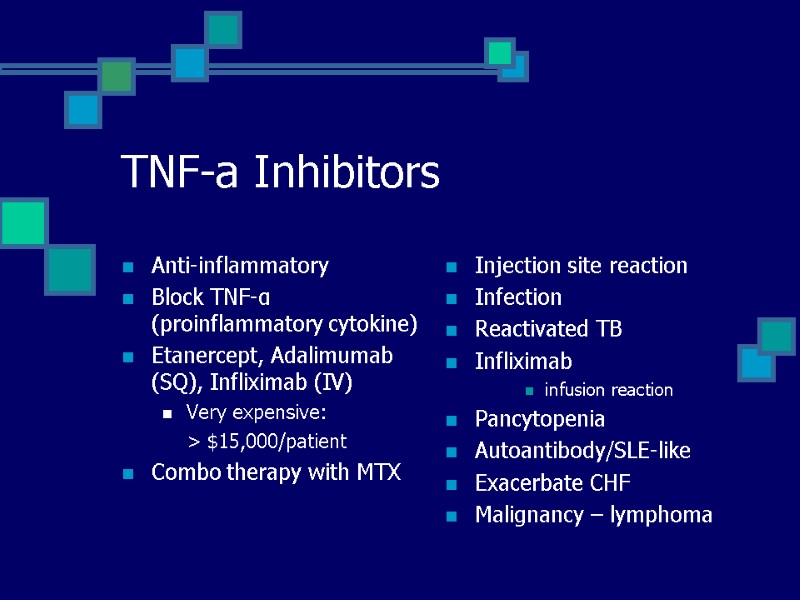
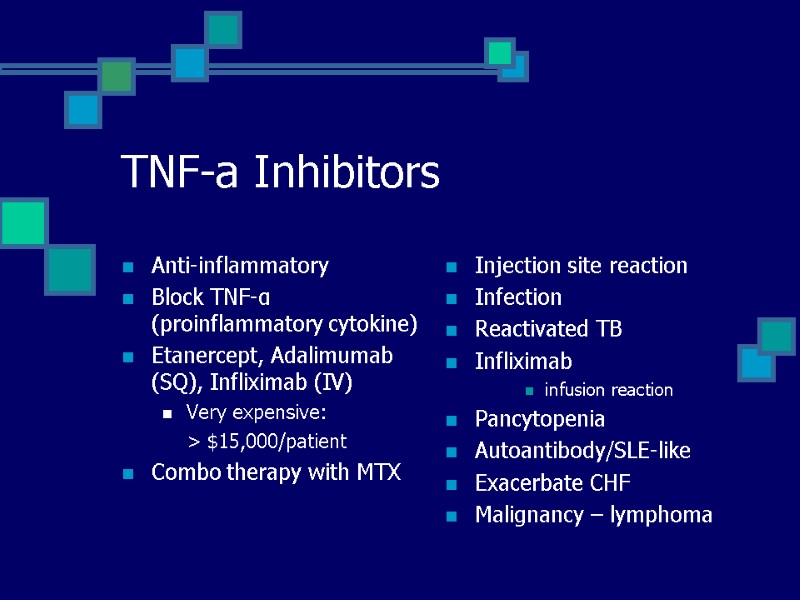 TNF-a Inhibitors Anti-inflammatory Block TNF-α (proinflammatory cytokine) Etanercept, Adalimumab (SQ), Infliximab (IV) Very expensive: > $15,000/patient Combo therapy with MTX Injection site reaction Infection Reactivated TB Infliximab infusion reaction Pancytopenia Autoantibody/SLE-like Exacerbate CHF Malignancy – lymphoma
TNF-a Inhibitors Anti-inflammatory Block TNF-α (proinflammatory cytokine) Etanercept, Adalimumab (SQ), Infliximab (IV) Very expensive: > $15,000/patient Combo therapy with MTX Injection site reaction Infection Reactivated TB Infliximab infusion reaction Pancytopenia Autoantibody/SLE-like Exacerbate CHF Malignancy – lymphoma
 More aggressive approach Combo therapy Adjunctive therapy: TNF-α antagonist
More aggressive approach Combo therapy Adjunctive therapy: TNF-α antagonist
 Disease Course Long Remission 10% Intermittent Disease 15-30% Progressive Disease
Disease Course Long Remission 10% Intermittent Disease 15-30% Progressive Disease
 Summary Approach to Arthritis Number of Joints Affected Inflammatory vs. Non-Inflammatory Rheumatoid Arthritis Diagnostic Criteria Pathophysiology Therapeutic Approach Disease Severity and Course
Summary Approach to Arthritis Number of Joints Affected Inflammatory vs. Non-Inflammatory Rheumatoid Arthritis Diagnostic Criteria Pathophysiology Therapeutic Approach Disease Severity and Course
 Questions?
Questions?

