2094d8fa32f9f035880b52ec8854b8bc.ppt
- Количество слайдов: 73
RETRAINING OBSTRUCTIVE PULMONARY DISEASE SUBJECTS: From theory to practice Alain VARRAY Diplôme Européen Universitaire en Activités Physiques Adaptées
From To…
COPD Chronic Obstructive Pulmonary Disease l l l Permanent and irreversible bronchial obstruction chronic hypoxemia In 2020: probably 3 rd cause of mortality in the world From a clinical point of view: ð Main symptom: dyspnea ð Very poor respiratory function (permanent) ð obvious and high exercise intolerance
Physical Activity and COPD: not evident at all ! l 2 main hurdles : ð PA Ø ð PA increased breathlessness to be avoided in dyspneic individuals does not change respiratory function so, PA considered difficult and useless or even non relevant
Major changes l In ten years, many works have improved our understanding of the COPD/exercise interface : ð ð Exercise tolerance is not only linked to COPD severity COPD muscle shows important abnormalities Ø Quantitative Ø Qualitative Ø Functional aspect (low muscle mass) aspect (muscle structure) consequences Ø Metabolic aspect: the muscle impairments are not linked with insufficient O 2 delivery 2001 AJRCCM editorial : COPD as a muscle disease
WHAT IS THE CONSEQUENCE ? Reminder of reasons in favor of PA avoidance Poor exercise tolerance due to pulmonary function impossible to improve it (chronic disease) exercise induces dyspnea worsening New evidences in favor of APA : Alteration of muscle function early dyspnea PA can be used to improve muscle function for the same disease severity improve exercise tolerance is possible, so better quality of life
The main key… To prove that muscle impairment is responsible for early dyspnea
COPD MUSCLE STRUCTURE l l l Less fat free mass Loss of maximal force Predictive of peak V'O 2 ________ Baarends et al. Eur Respir J, 1997, 10 : 2807 -13.
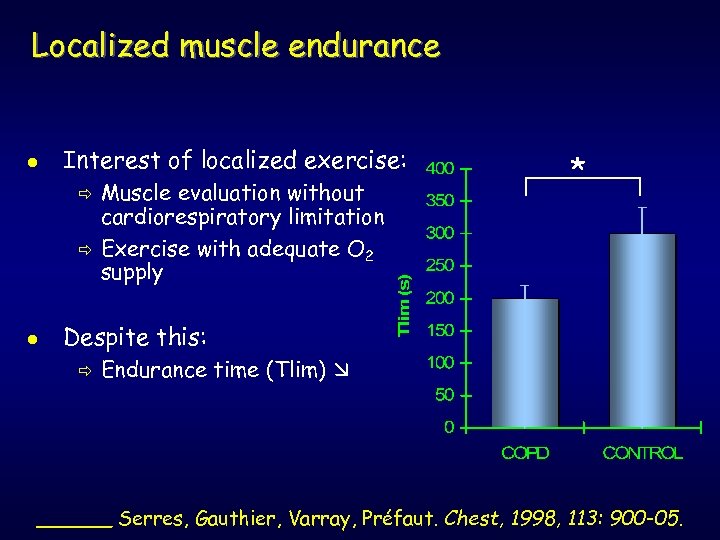
Localized muscle endurance l Interest of localized exercise: ð ð l Muscle evaluation without cardiorespiratory limitation Exercise with adequate O 2 supply * Despite this: ð Endurance time (Tlim) ______ Serres, Gauthier, Varray, Préfaut. Chest, 1998, 113: 900 -05.
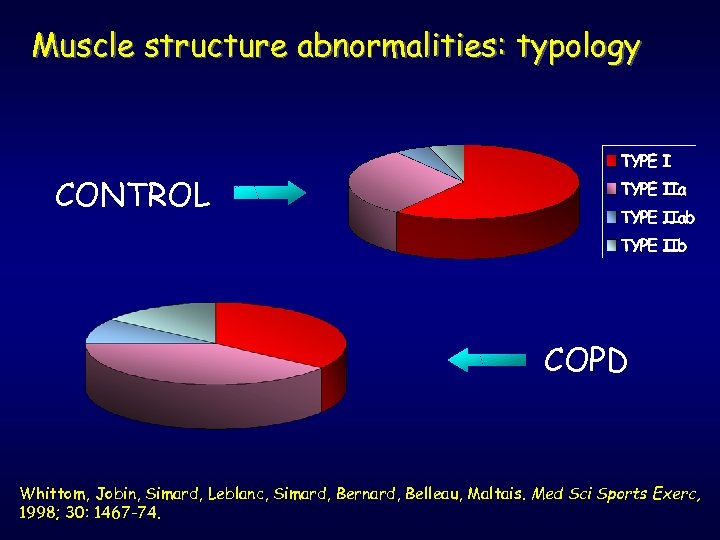
Muscle structure abnormalities: typology CONTROL COPD Whittom, Jobin, Simard, Leblanc, Simard, Bernard, Belleau, Maltais. Med Sci Sports Exerc, 1998; 30: 1467 -74.
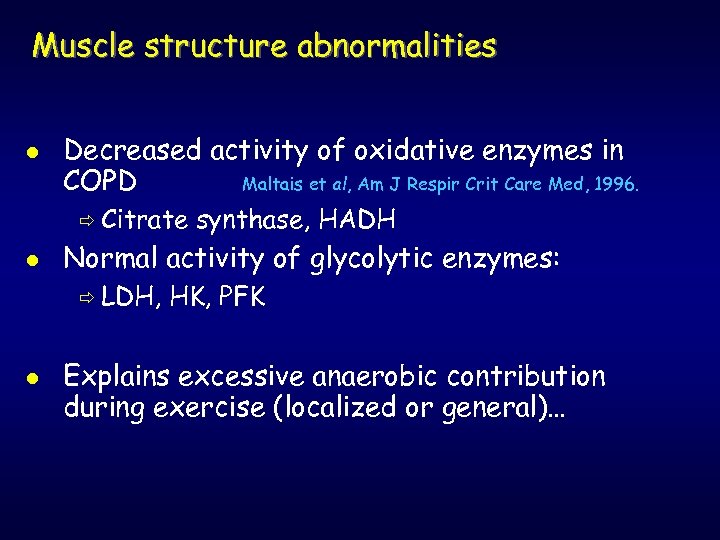
Muscle structure abnormalities l Decreased activity of oxidative enzymes in COPD Maltais et al, Am J Respir Crit Care Med, 1996. ð Citrate l Normal activity of glycolytic enzymes: ð LDH, l synthase, HADH HK, PFK Explains excessive anaerobic contribution during exercise (localized or general)…
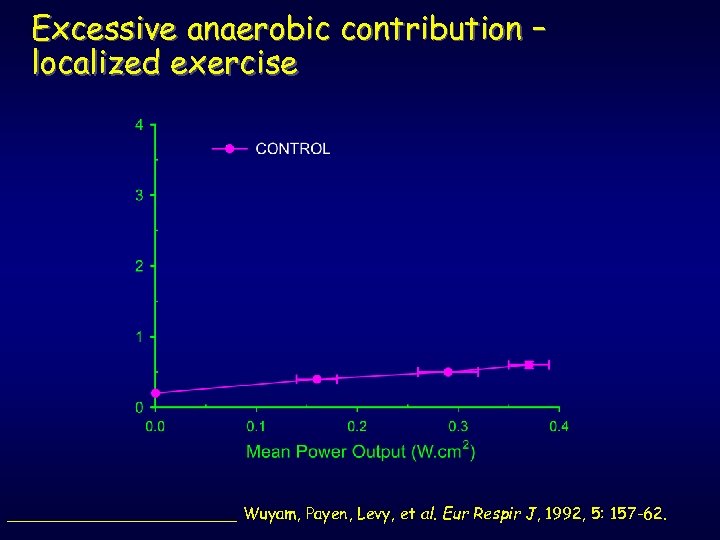
Excessive anaerobic contribution – localized exercise ____________ Wuyam, Payen, Levy, et al. Eur Respir J, 1992, 5: 157 -62.
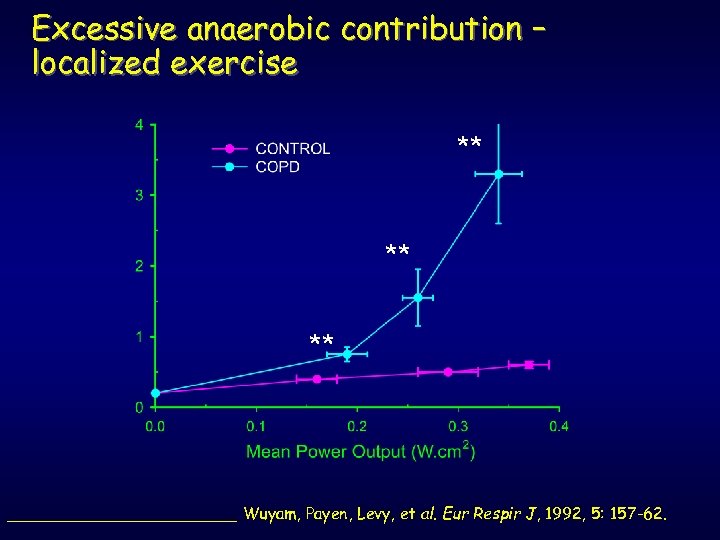
Excessive anaerobic contribution – localized exercise ** ** ** ____________ Wuyam, Payen, Levy, et al. Eur Respir J, 1992, 5: 157 -62.
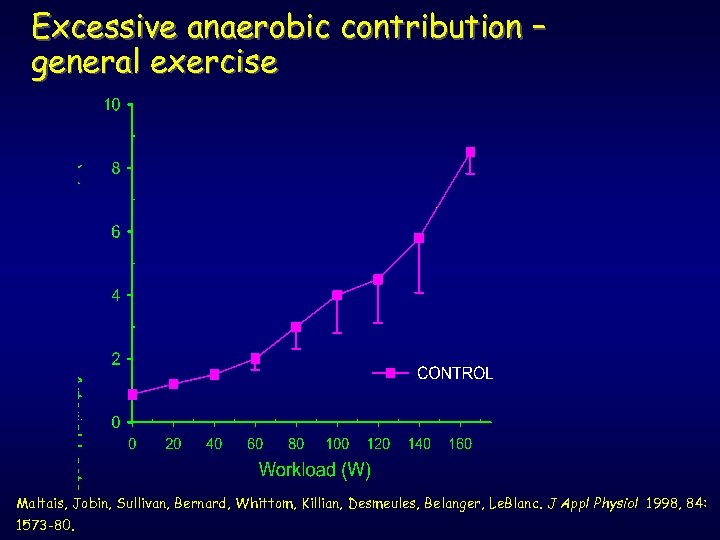
Excessive anaerobic contribution – general exercise Maltais, Jobin, Sullivan, Bernard, Whittom, Killian, Desmeules, Belanger, Le. Blanc. J Appl Physiol 1998, 84: 1573 -80.
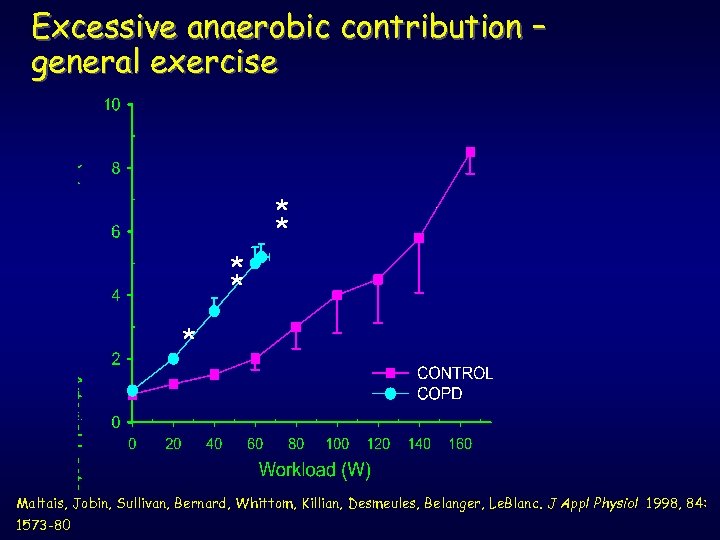
Excessive anaerobic contribution – general exercise * * * Maltais, Jobin, Sullivan, Bernard, Whittom, Killian, Desmeules, Belanger, Le. Blanc. J Appl Physiol 1998, 84: 1573 -80
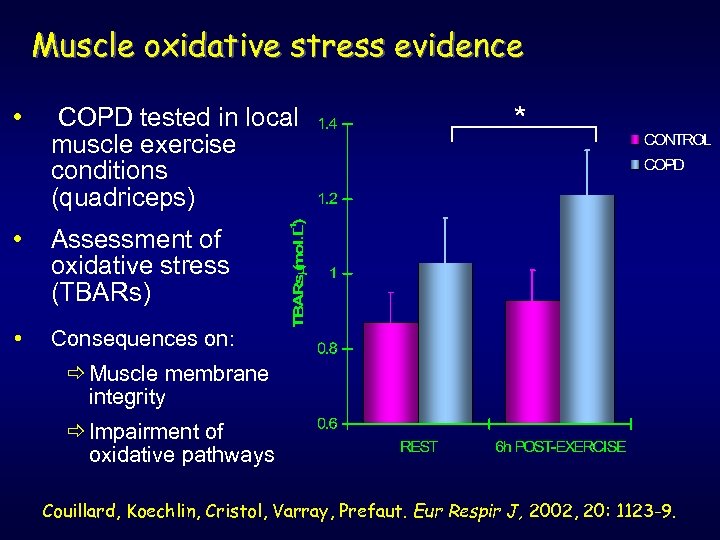
Muscle oxidative stress evidence • COPD tested in local muscle exercise conditions (quadriceps) • Assessment of oxidative stress (TBARs) • * Consequences on: ð Muscle membrane integrity ð Impairment of oxidative pathways Couillard, Koechlin, Cristol, Varray, Prefaut. Eur Respir J, 2002, 20: 1123 -9.
Muscle impairment occurs before any problem in O 2 supply Gosselin, Poulain, Ramonatxo, Ceugniet, Préfaut, Varray. Muscle & Nerve, 2003, 27: 170 -9.
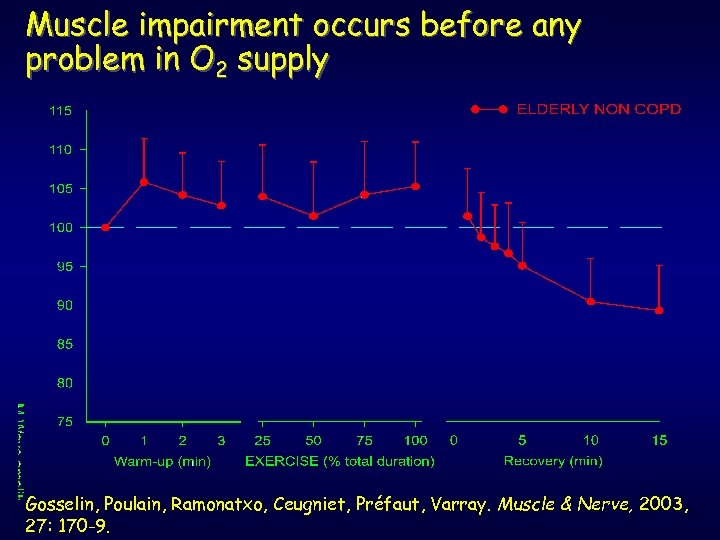
Muscle impairment occurs before any problem in O 2 supply Gosselin, Poulain, Ramonatxo, Ceugniet, Préfaut, Varray. Muscle & Nerve, 2003, 27: 170 -9.
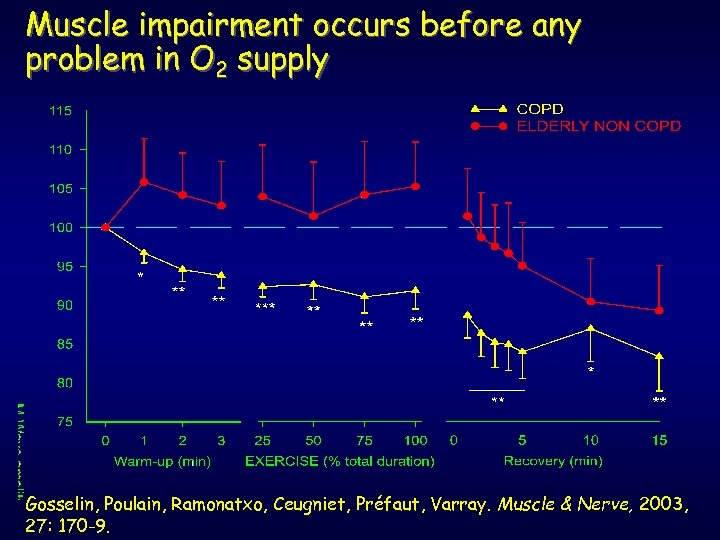
Muscle impairment occurs before any problem in O 2 supply Gosselin, Poulain, Ramonatxo, Ceugniet, Préfaut, Varray. Muscle & Nerve, 2003, 27: 170 -9.
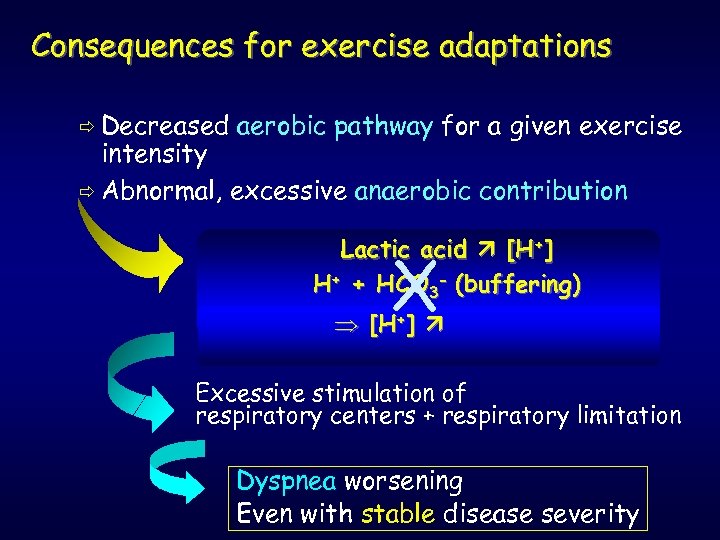
Consequences for exercise adaptations ð Decreased aerobic pathway for a given exercise intensity ð Abnormal, excessive anaerobic contribution Lactic acid [H+] H+ + HCO 3 - (buffering) CO 2 ] [H+ production X Excessive stimulation of respiratory centers + respiratory limitation Dyspnea worsening Even with stable disease severity
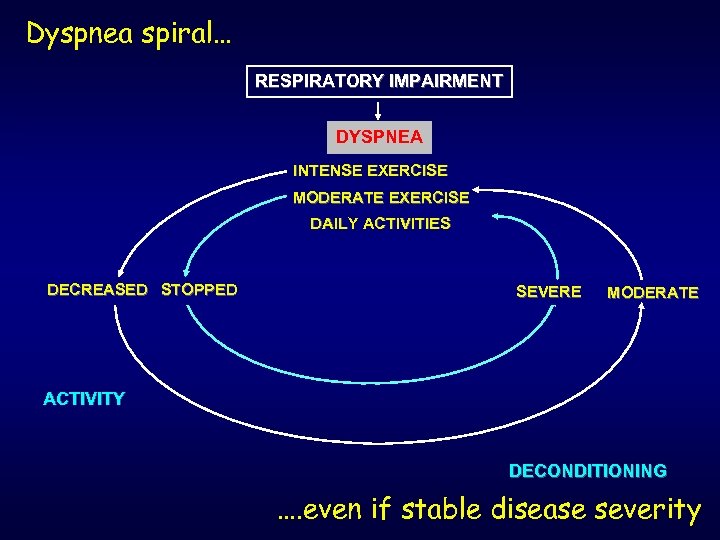
Dyspnea spiral… RESPIRATORY IMPAIRMENT DYSPNEA INTENSE EXERCISE MODERATE EXERCISE DAILY ACTIVITIES DECREASED STOPPED SEVERE MODERATE ACTIVITY DECONDITIONING …. even if stable disease severity
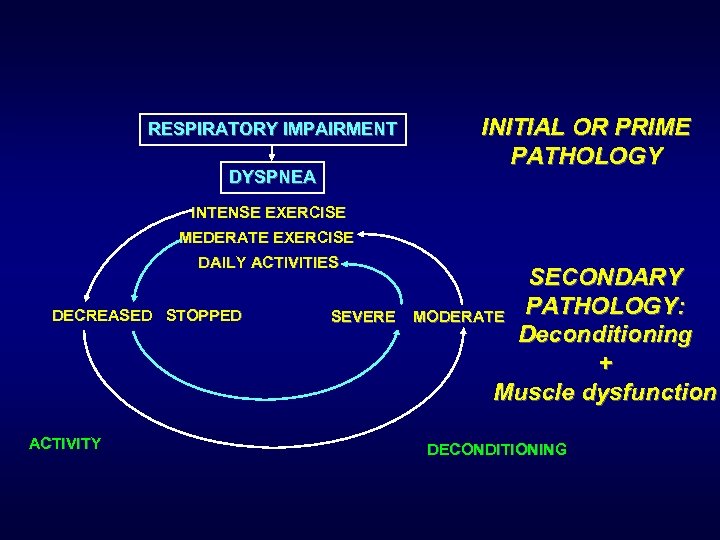
RESPIRATORY IMPAIRMENT DYSPNEA INITIAL OR PRIME PATHOLOGY INTENSE EXERCISE MEDERATE EXERCISE DAILY ACTIVITIES DECREASED STOPPED ACTIVITY SEVERE SECONDARY PATHOLOGY: MODERATE Deconditioning + Muscle dysfunction DECONDITIONING
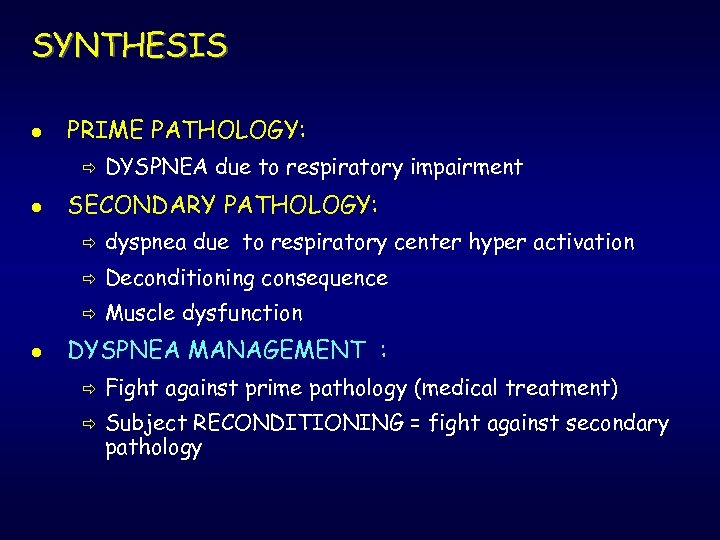
SYNTHESIS l PRIME PATHOLOGY: ð l DYSPNEA due to respiratory impairment SECONDARY PATHOLOGY: ð ð Deconditioning consequence ð l dyspnea due to respiratory center hyper activation Muscle dysfunction DYSPNEA MANAGEMENT : ð ð Fight against prime pathology (medical treatment) Subject RECONDITIONING = fight against secondary pathology
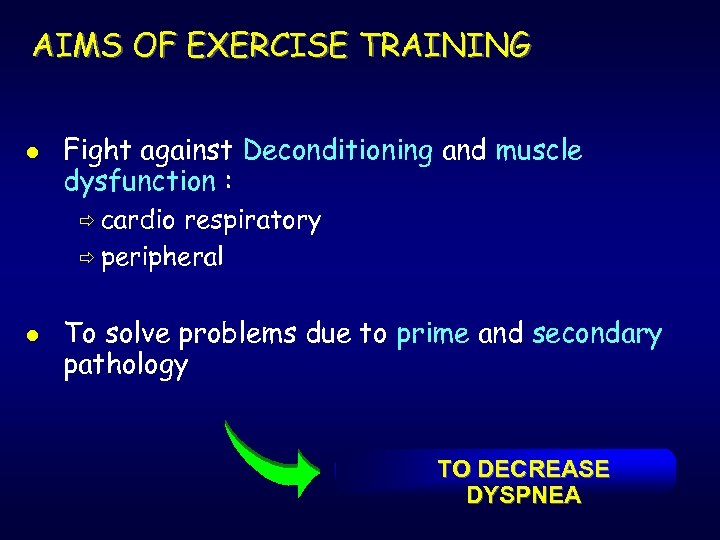
AIMS OF EXERCISE TRAINING l Fight against Deconditioning and muscle dysfunction : ð cardio respiratory ð peripheral l To solve problems due to prime and secondary pathology TO DECREASE DYSPNEA
A. P. A. JUSTIFICATION l PRIME PATHOLOGY: ð Medical and paramedical management ð Treatment stabilisation and optimization l SECONDARY PATHOLOGY : ð EPSA teacher directly concerned ð Work on relationship between Metabolic effects physical practice and Ø Health increase Ø ð Decreased dyspnea so increased quality of life
BASIC KNOWLEDGE NEEDED TO OPTIMIZE A. P. A. l Good adaptation of exercise testing ð Methodological basis of individualization ð Exercise tests too often done incorrectly l l dyspnea measurement (diagnosis and evaluation) Optimal training intensity Field test development Retraining follow-up
ADAPTED EXERCISE TESTING l Basic principle : ð Individualize l on standardized basis Main principles: ð Continuous test ð Progressively increased ð Step duration = 1 min ð Total test duration = about 10 min after warmup so imperative individualization of load increment
WHY INDIVIDUALIZATION ? l l l Initially, exercise inadaptation are proportional to pathology severity Most of the time : exercise testing too short impossible ventilatory threshold assessment No maximal exercise test (RER<1. 10) Bad interpretation of subject ability to perform exercise and training programing
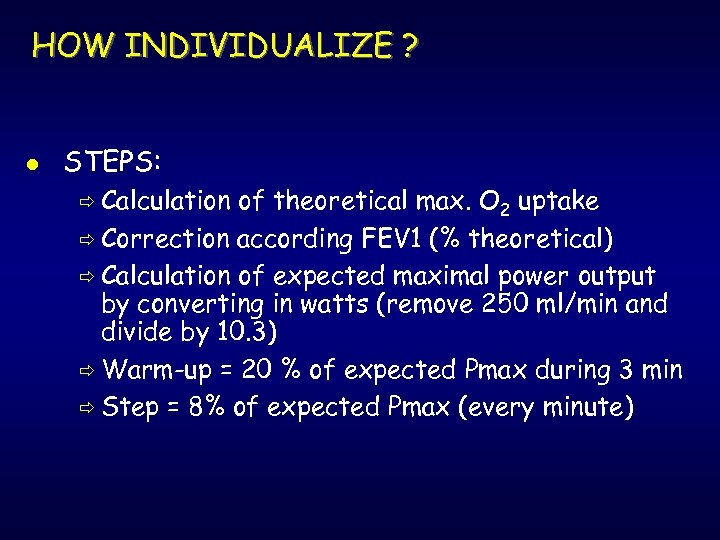
HOW INDIVIDUALIZE ? l STEPS: ð Calculation of theoretical max. O 2 uptake ð Correction according FEV 1 (% theoretical) ð Calculation of expected maximal power output by converting in watts (remove 250 ml/min and divide by 10. 3) ð Warm-up = 20 % of expected Pmax during 3 min ð Step = 8% of expected Pmax (every minute)
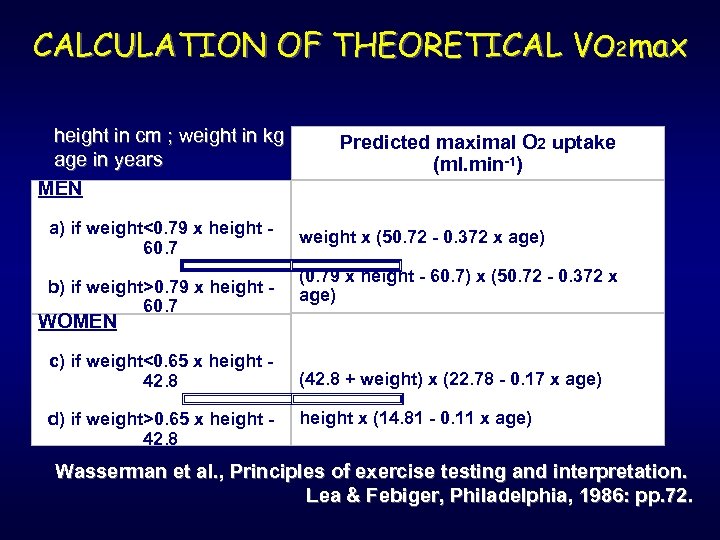
CALCULATION OF THEORETICAL VO 2 max height in cm ; weight in kg age in years MEN a) if weight<0. 79 x height 60. 7 b) if weight>0. 79 x height 60. 7 Predicted maximal O 2 uptake (ml. min-1) weight x (50. 72 - 0. 372 x age) (0. 79 x height - 60. 7) x (50. 72 - 0. 372 x age) WOMEN c) if weight<0. 65 x height 42. 8 d) if weight>0. 65 x height 42. 8 (42. 8 + weight) x (22. 78 - 0. 17 x age) height x (14. 81 - 0. 11 x age) Wasserman et al. , Principles of exercise testing and interpretation. Lea & Febiger, Philadelphia, 1986: pp. 72.
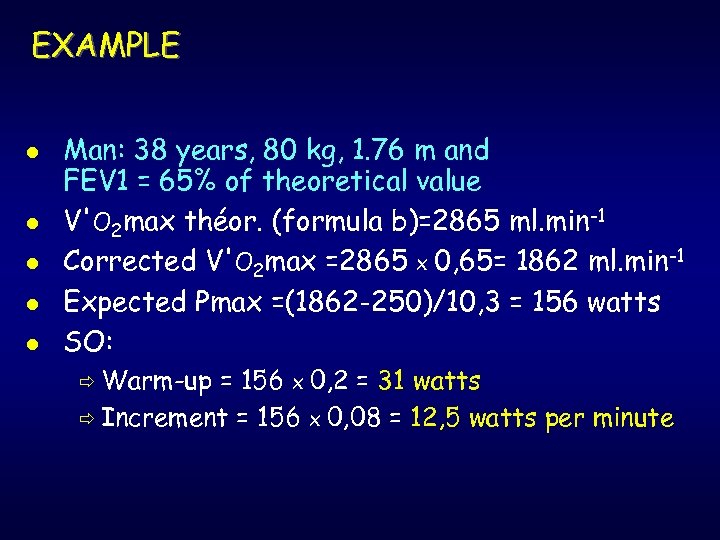
EXAMPLE l l l Man: 38 years, 80 kg, 1. 76 m and FEV 1 = 65% of theoretical value V'O 2 max théor. (formula b)=2865 ml. min-1 Corrected V'O 2 max =2865 x 0, 65= 1862 ml. min-1 Expected Pmax =(1862 -250)/10, 3 = 156 watts SO: ð Warm-up = 156 x 0, 2 = 31 watts ð Increment = 156 x 0, 08 = 12, 5 watts per minute
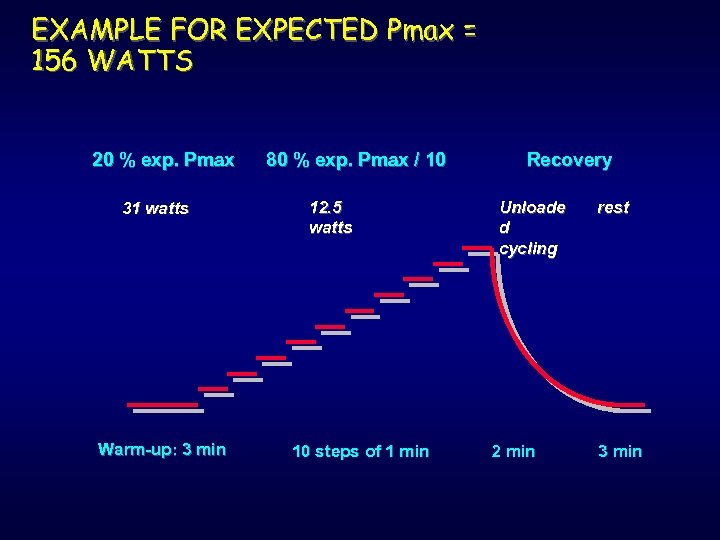
EXAMPLE FOR EXPECTED Pmax = 156 WATTS 20 % exp. Pmax 31 watts Warm-up: 3 min 80 % exp. Pmax / 10 12. 5 watts 10 steps of 1 min Recovery Unloade d cycling 2 min rest 3 min
MEASUREMENT OF VENTILATORY THRESHOLD l DURING INCREMENTAL EXERCISE/ ð Recording V’O 2 and V’CO 2 (breath-by-breath) ð Averaging every 10 seconds ð Computation of V’O 2 / V’CO 2 relationship Ventilatory threshold = breakdown of linearity
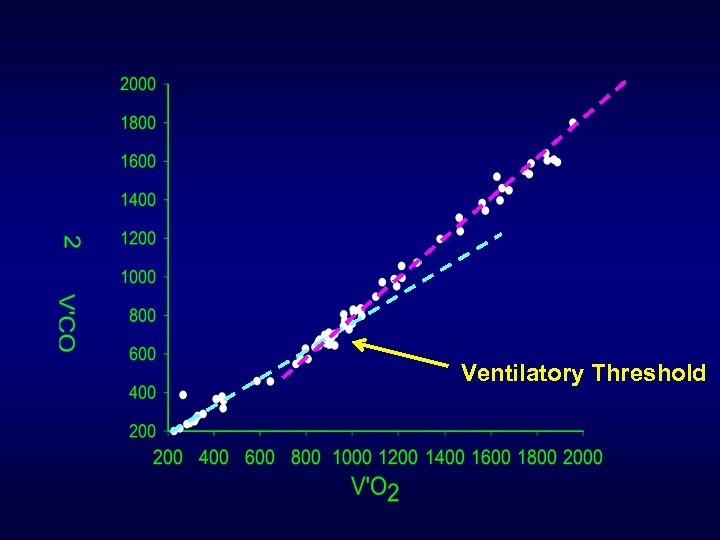
Ventilatory Threshold
Interest of individualization at ventilatory threshold l l l l directly function of aerobic physical fitness Individualization / real capacities Before excessive hyperventilation Very well tolerated (no or few dyspnea) Efficient to induce training effects Easy learning of individualized practice Usable in current life If impossible to measure dyspnea threshold
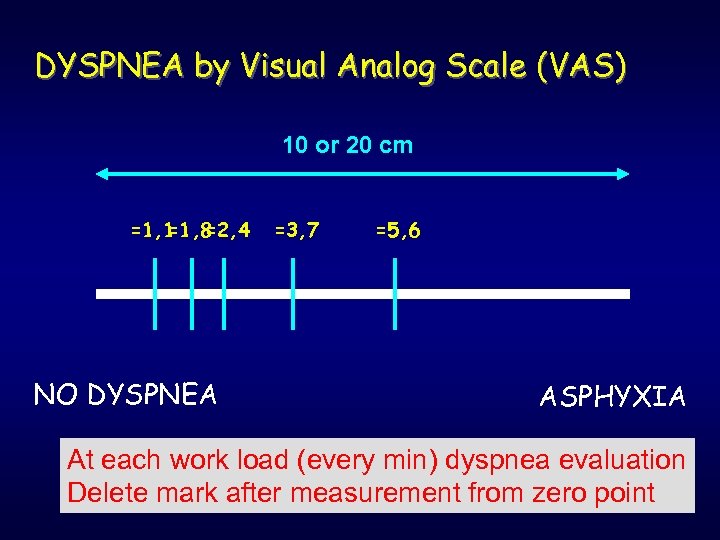
DYSPNEA by Visual Analog Scale (VAS) 10 or 20 cm =1, 1 =2, 4 =1, 8 NO DYSPNEA =3, 7 =5, 6 ASPHYXIA At each work load (every min) dyspnea evaluation Delete mark after measurement from zero point
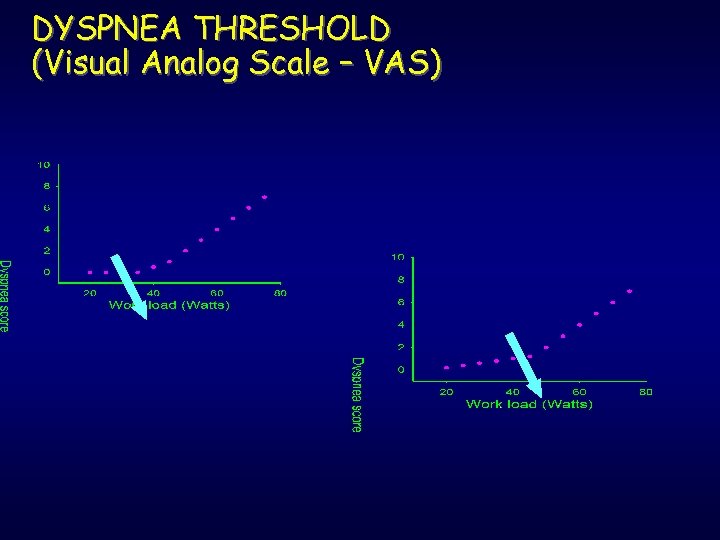
DYSPNEA THRESHOLD (Visual Analog Scale – VAS)

OPTIMIZATION. . . RETRAINING DEVELOPMENT USEFULNESS OF FIELD TESTS
RATIONALE l Disadvantage of individualized training : ð Regular l cardio respiratory evaluation => cost Solution : ð Adapted l field test One of the most popular : ð 6 or 12 min walking test
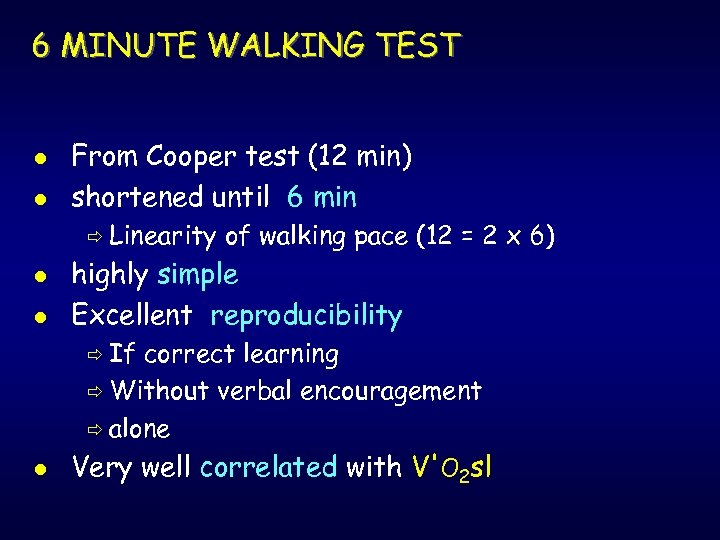
6 MINUTE WALKING TEST l l From Cooper test (12 min) shortened until 6 min ð Linearity l l of walking pace (12 = 2 x 6) highly simple Excellent reproducibility ð If correct learning ð Without verbal encouragement ð alone l Very well correlated with V'O 2 sl
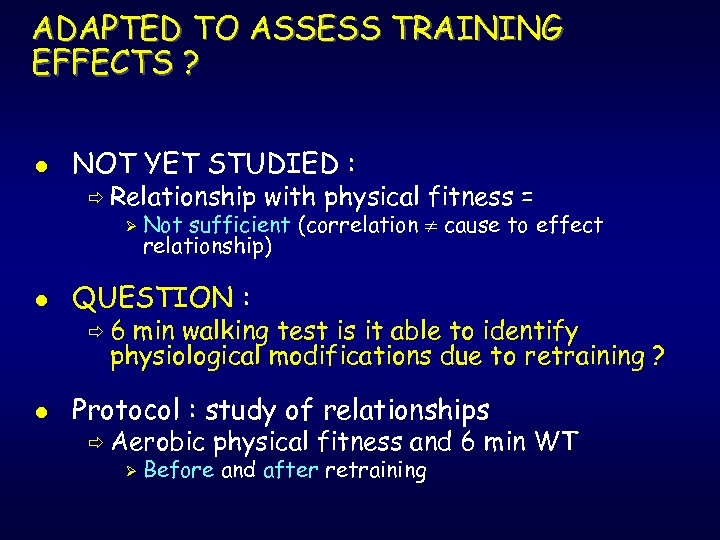
ADAPTED TO ASSESS TRAINING EFFECTS ? l NOT YET STUDIED : ð Relationship Ø with physical fitness = Not sufficient (correlation cause to effect relationship) l QUESTION : l Protocol : study of relationships ð 6 min walking test is it able to identify physiological modifications due to retraining ? ð Aerobic Ø physical fitness and 6 min WT Before and after retraining
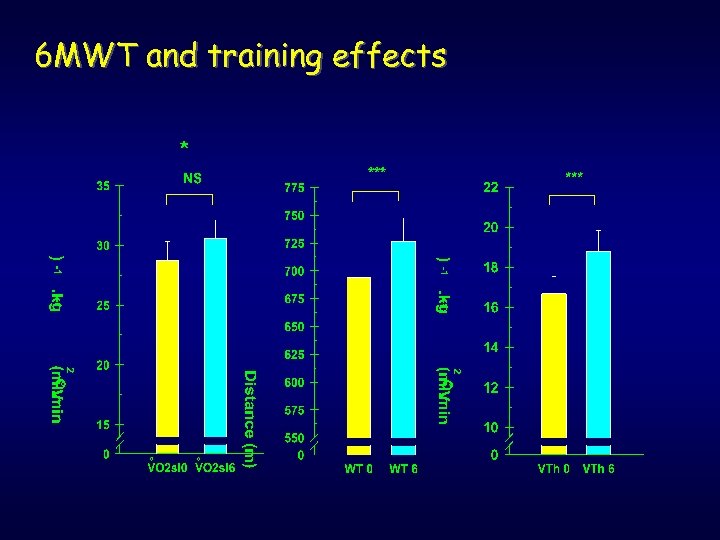
6 MWT and training effects *
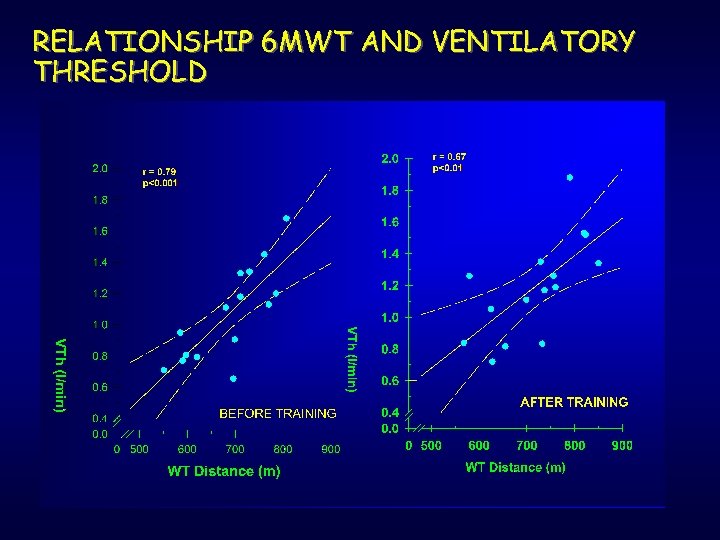
RELATIONSHIP 6 MWT AND VENTILATORY THRESHOLD
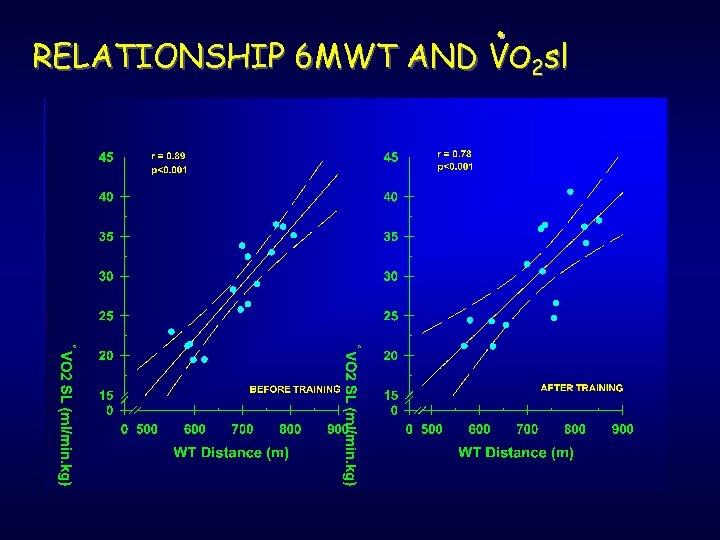
RELATIONSHIP 6 MWT AND VO 2 sl
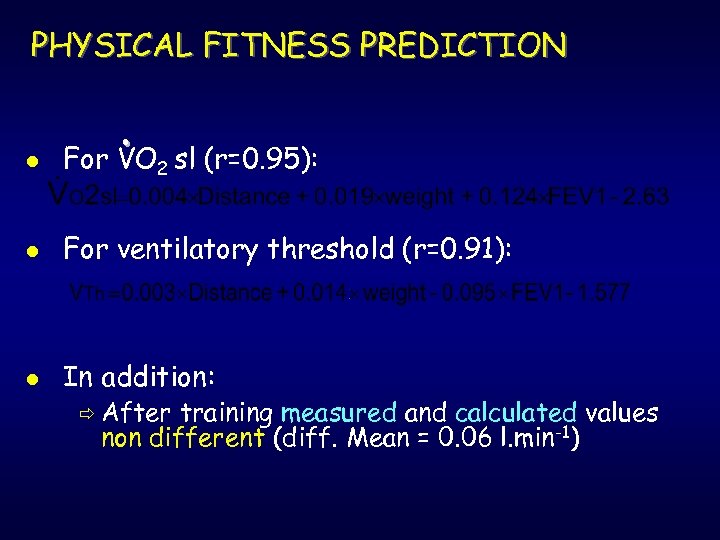
PHYSICAL FITNESS PREDICTION l For VO 2 sl (r=0. 95): l For ventilatory threshold (r=0. 91): l In addition: ð After training measured and calculated values non different (diff. Mean = 0. 06 l. min-1)
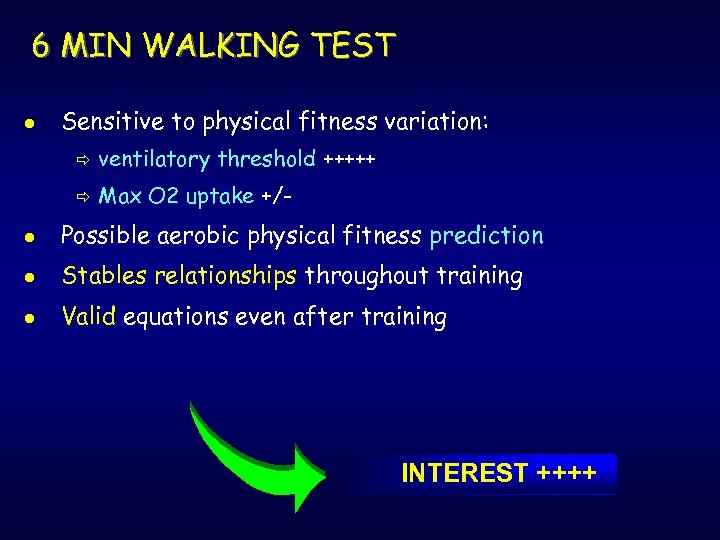
6 MIN WALKING TEST l Sensitive to physical fitness variation: ð ventilatory threshold +++++ ð Max O 2 uptake +/- l Possible aerobic physical fitness prediction l Stables relationships throughout training l Valid equations even after training INTEREST ++++
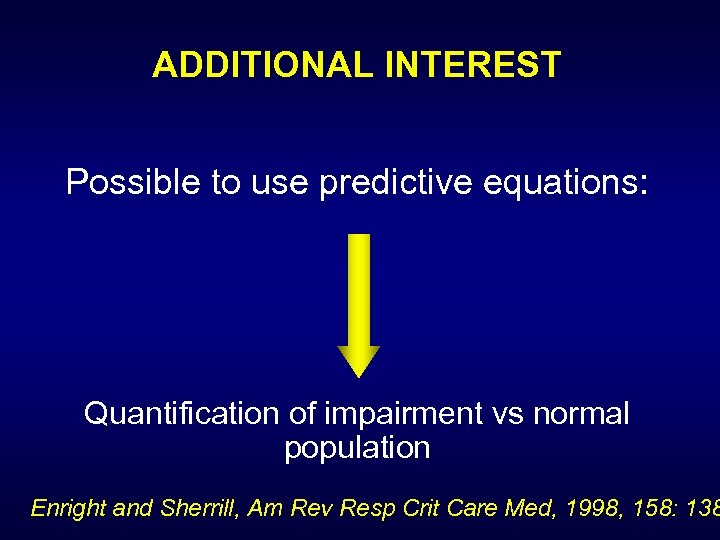
ADDITIONAL INTEREST Possible to use predictive equations: Quantification of impairment vs normal population Enright and Sherrill, Am Rev Resp Crit Care Med, 1998, 158: 138
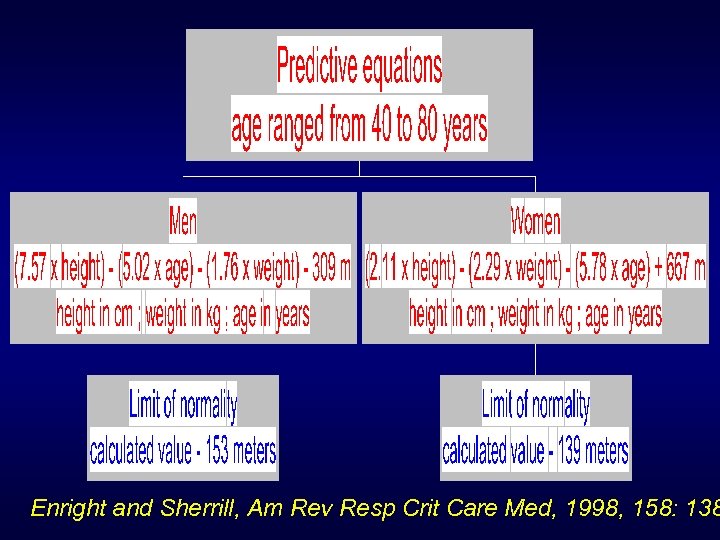
Enright and Sherrill, Am Rev Resp Crit Care Med, 1998, 158: 138
OPTIMIZATION WHICH INTENSITIES ?
STATE OF THE ART l Works of literature : ð No l consensus Most of the time : ð Training intensities based on % reserve heart rate [ HRrest + (HRmax - HRrest) % ] l Interest : ð Simplicity of realization
PROBLEM : NEED TO CERTIFY EFFECTIVENESS OF RESULTS l Relevance ? ? ? ð No consideration of cardio respiratory fitness ð standardization is in opposition to individualization l QUESTION : ð Which method lead to best results ?
-- INTEREST -l Stays in specialized centers : ð More l and more shortened SO : ð High need to be as efficient as possible ð That is Obtain best results every time Ø In a minimum amount of time Ø
PROTOCOL l 2 groups studied : ð Trained Ø Ø at the same absolute HR, but : 1 gpe at ventilatory threshold (individualization) 1 gpe at 50% of reserve HR (standardtion )training at the same frequency and duration ð Blind final evaluation
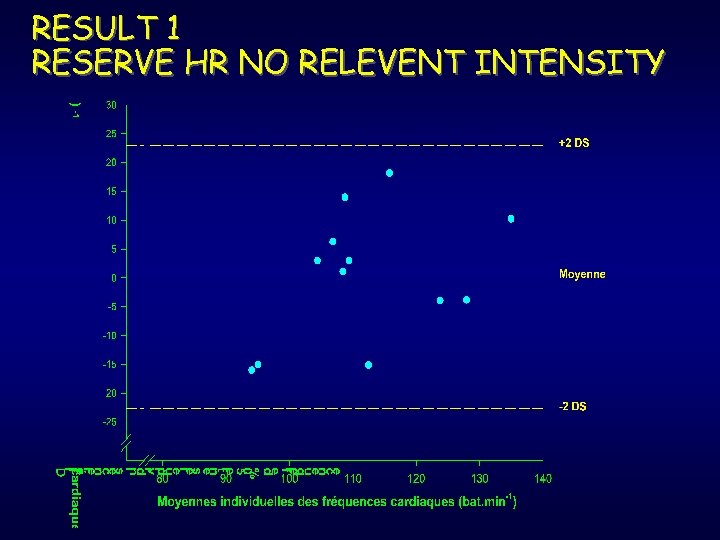
RESULT 1 RESERVE HR NO RELEVENT INTENSITY
CONCLUSION l Reserve HR : ð Random results ð Under- or over-estimation of efficient intensities Another reserve HR % choice cannot be a solution to improve this technique
GENERAL RESULTS l Exercise adaptations : ð ð l Enhancement of quality of life : ð ð l Better exercise tolerance : dyspnea decrease Restoration on self confidence General well-being, emotional state (Ojanen et al, 1993) durable effect (Dekhuijzen et al. , 1990) Improvement of psychological state : ð ð Never linked with resting pulmonary function Always related to possible physical activity amount linked to functional state
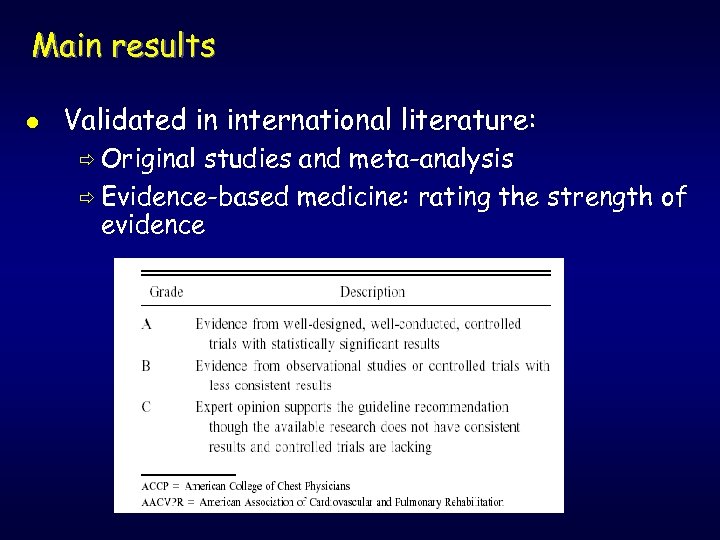
Main results l Validated in international literature: ð Original studies and meta-analysis ð Evidence-based medicine: rating the strength of evidence
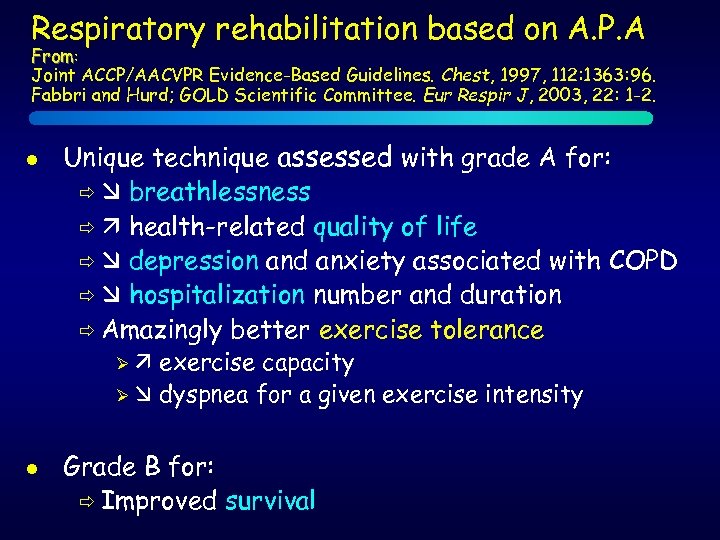
Respiratory rehabilitation based on A. P. A From: Joint ACCP/AACVPR Evidence-Based Guidelines. Chest, 1997, 112: 1363: 96. Fabbri and Hurd; GOLD Scientific Committee. Eur Respir J, 2003, 22: 1 -2. l Unique technique assessed with grade A for: ð breathlessness ð health-related quality of life ð depression and anxiety associated with COPD ð hospitalization number and duration ð Amazingly better exercise tolerance exercise capacity Ø dyspnea for a given exercise intensity Ø l Grade B for: ð Improved survival
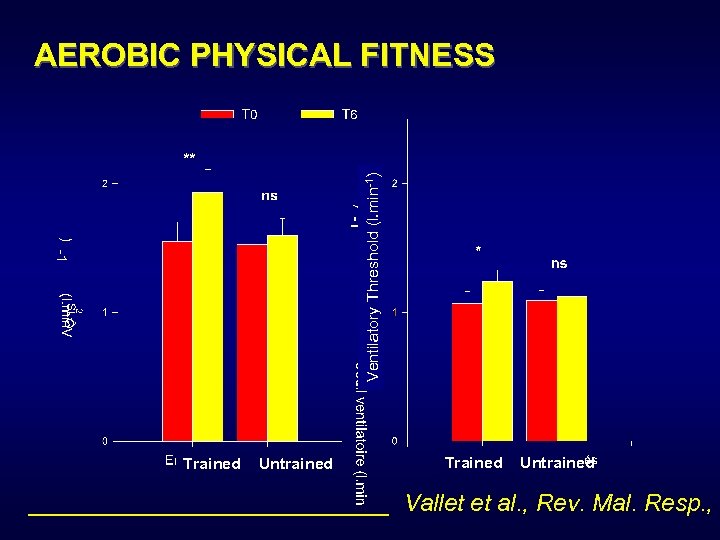
Ventilatory Threshold (l. min-1) AEROBIC PHYSICAL FITNESS Trained Untrained ______________ Vallet et al. , Rev. Mal. Resp. , 1
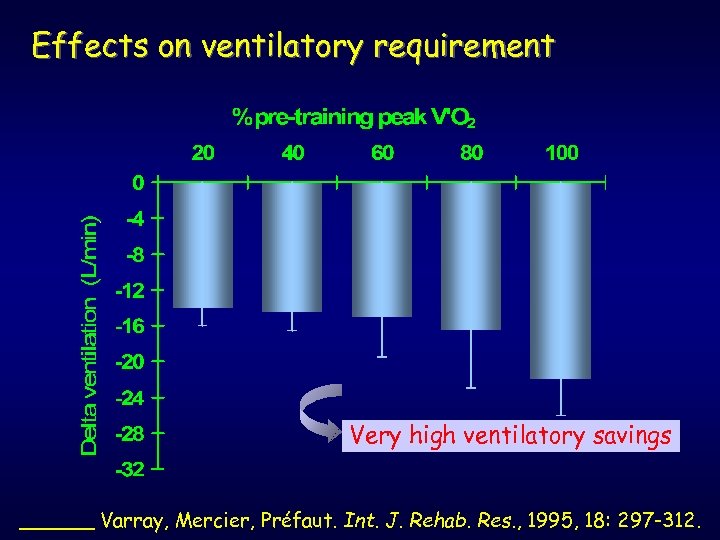
Effects on ventilatory requirement Very high ventilatory savings ______ Varray, Mercier, Préfaut. Int. J. Rehab. Res. , 1995, 18: 297 -312.
VENTILATORY REQUIREMENT l Ventilation decrease for a given exercise intensity: ð Increased ventilatory comfort for any exercise intensity ð Decreased respiratory cost (dyspnea ) ð SO: more O 2 for exercising muscles : Exercise capacity increased Ø Better exercise efficiency Ø
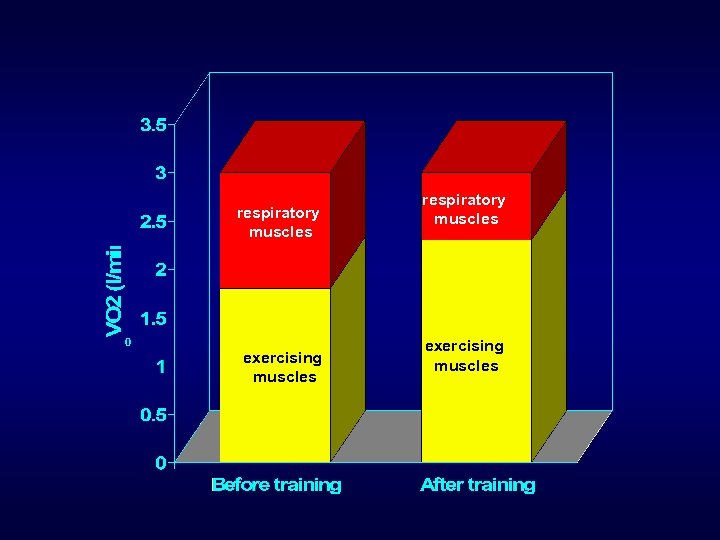
respiratory muscles o exercising muscles respiratory muscles exercising muscles
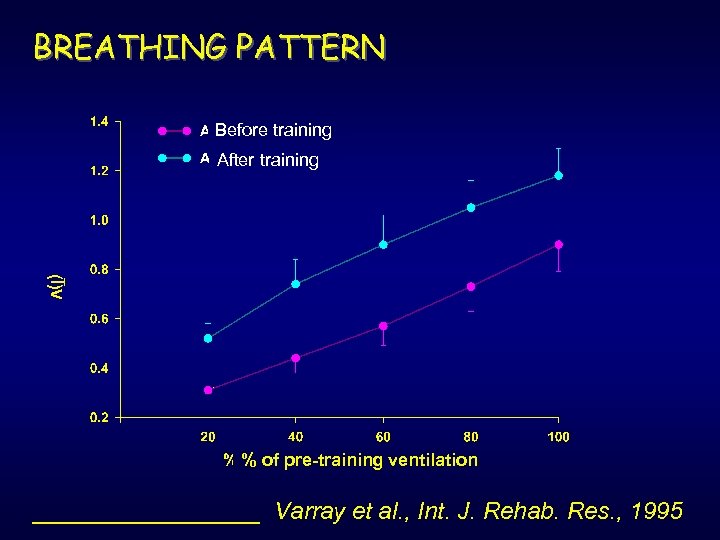
BREATHING PATTERN Before training After training % of pre-training ventilation _________ Varray et al. , Int. J. Rehab. Res. , 1995
BREATHING PATTERN MODIFICATION • VT always higher for a given ventilation : ü Better alveolar ventilation ü Airways turbulences decrease for a given obstruction level ü Explanation of the effects on dynamic hyperinflation ü Dyspnea decrease during exercise (lower fb) ü Reduced ventilatory cost
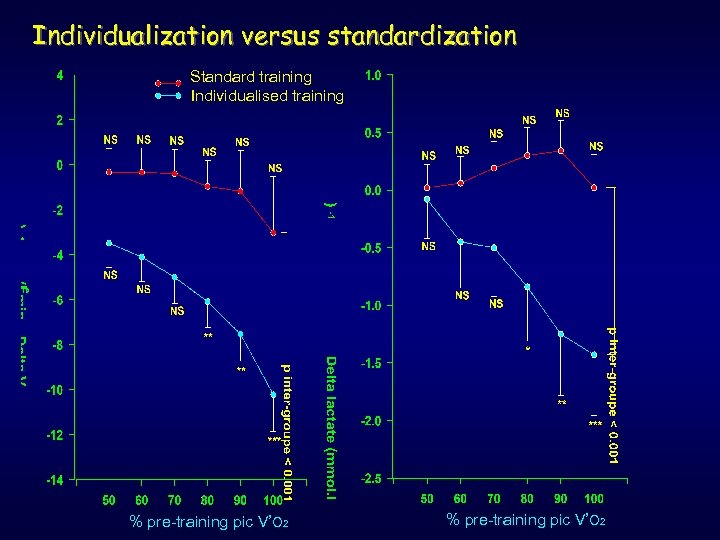
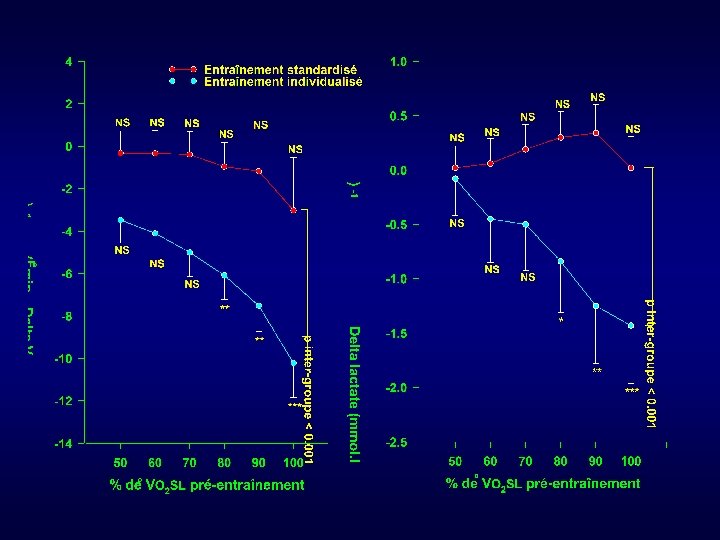
Individualization versus standardization Standard training Individualised training % pre-training pic V’O 2
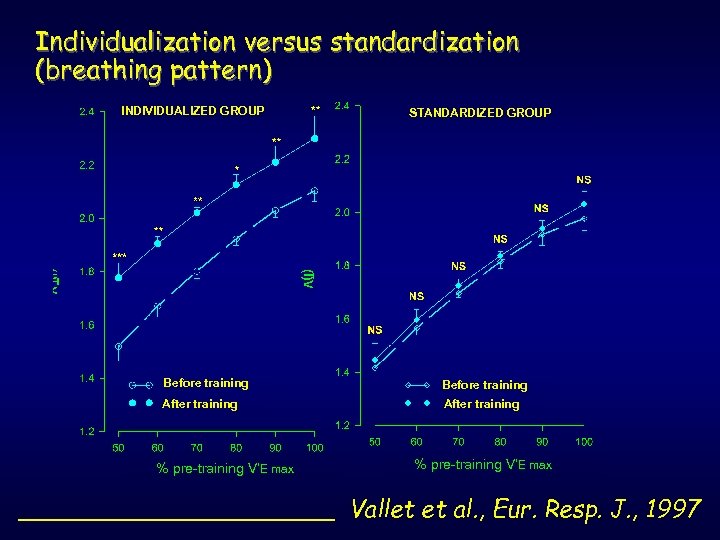
Individualization versus standardization (breathing pattern) INDIVIDUALIZED GROUP STANDARDIZED GROUP Before training After training % pre-training V’E max ___________ Vallet et al. , Eur. Resp. J. , 1997
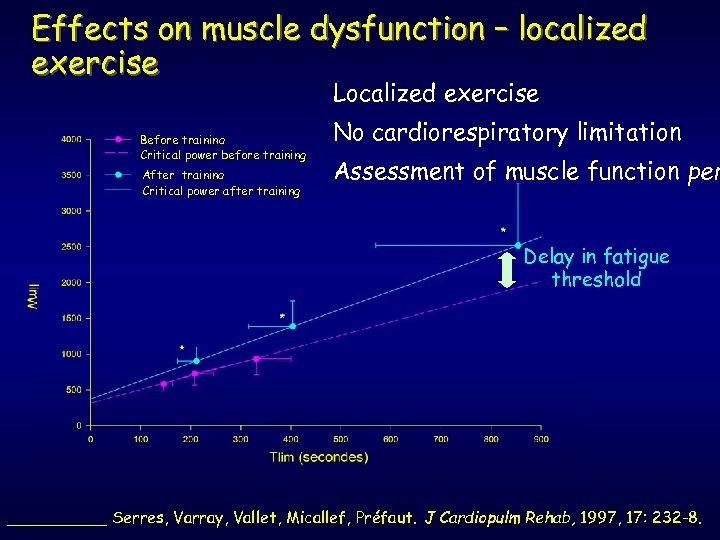
Effects on muscle dysfunction – localized exercise Localized exercise Before training Critical power before training After training Critical power after training No cardiorespiratory limitation Assessment of muscle function per Delay in fatigue threshold _____ Serres, Varray, Vallet, Micallef, Préfaut. J Cardiopulm Rehab, 1997, 17: 232 -8.
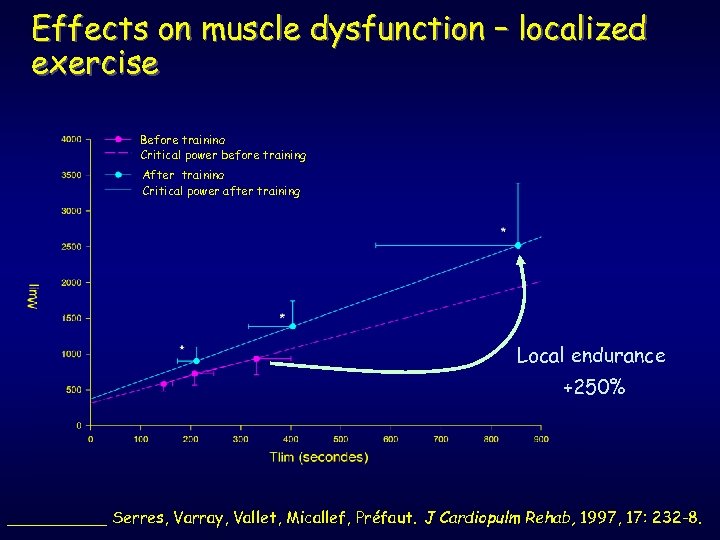
Effects on muscle dysfunction – localized exercise Before training Critical power before training After training Critical power after training Local endurance +250% _____ Serres, Varray, Vallet, Micallef, Préfaut. J Cardiopulm Rehab, 1997, 17: 232 -8.
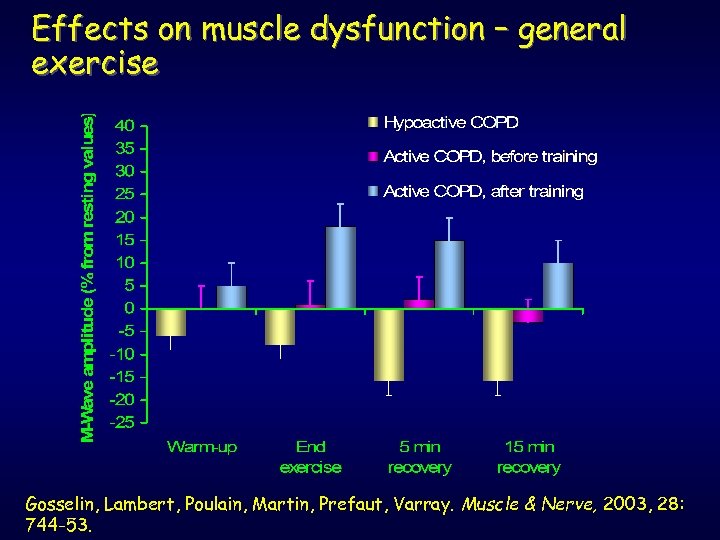
Effects on muscle dysfunction – general exercise Gosselin, Lambert, Poulain, Martin, Prefaut, Varray. Muscle & Nerve, 2003, 28: 744 -53.
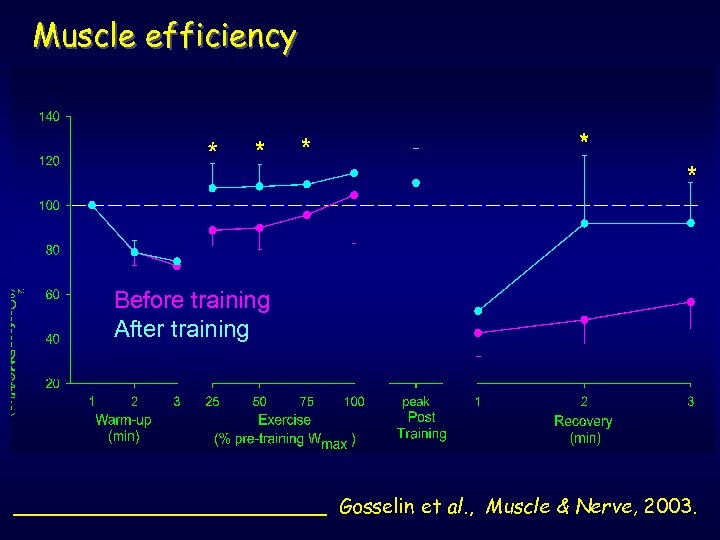
Muscle efficiency Before training After training _____________ Gosselin et al. , Muscle & Nerve, 2003.

COST/EFFECTIVENESS RELATIONSHIPS Sneider, J. Cardio GROUP 1 Treatment : -pulm. Rehab. , medical 1988 n = 50 GROUPE 2 GROUPE 3 Treatment: Médical + Education n = 50 Respiratory Rehabilitation n = 50 5 years PRE-R. R. 4. 24* / 1069** 2. 34* / 586** 3. 2* / 801** 5 years POST-R. R. 6. 28* / 1570** 3. 78* / 946** 1. 67* / 417** + 430 000 $ - 458 000 $ EVOLUTION COST / 5 years (1193$/day) + 600 000 $ * : hospitalization days /patient/year l ** : total hospitalization days during 5 years + work of Trautner (Eur. Resp. J. , 1993) - asthma and health management : ð For 1 DM (cost), 5 DM saved for public health economy
2094d8fa32f9f035880b52ec8854b8bc.ppt