64afd592da4b37bb99cd9e99ab88370d.ppt
- Количество слайдов: 116
 Responding to Mental Health Issues Within Drug & Alcohol Treatment Clinician’s Training Package These training resources were funded by Drug Strategy Branch, Australian Government Department of Health and Ageing through the National Comorbidity Initiative
Responding to Mental Health Issues Within Drug & Alcohol Treatment Clinician’s Training Package These training resources were funded by Drug Strategy Branch, Australian Government Department of Health and Ageing through the National Comorbidity Initiative
 Exercise 1: Who Here Do You Think… • • Loves The Simpsons? Can change a flat tyre? Exceeds the speed limit? Snores? Is kind to dogs? Would tell you that you have bad breath? Is trustworthy?
Exercise 1: Who Here Do You Think… • • Loves The Simpsons? Can change a flat tyre? Exceeds the speed limit? Snores? Is kind to dogs? Would tell you that you have bad breath? Is trustworthy?
 Exercise 2: How Are You Thinking-Feeling-Doing? • What are your THOUGHTS about working with clients with comorbidity? • What are your FEELINGS about this training? • Notice how you BEHAVE when I say we have 2 days to get this on board?
Exercise 2: How Are You Thinking-Feeling-Doing? • What are your THOUGHTS about working with clients with comorbidity? • What are your FEELINGS about this training? • Notice how you BEHAVE when I say we have 2 days to get this on board?
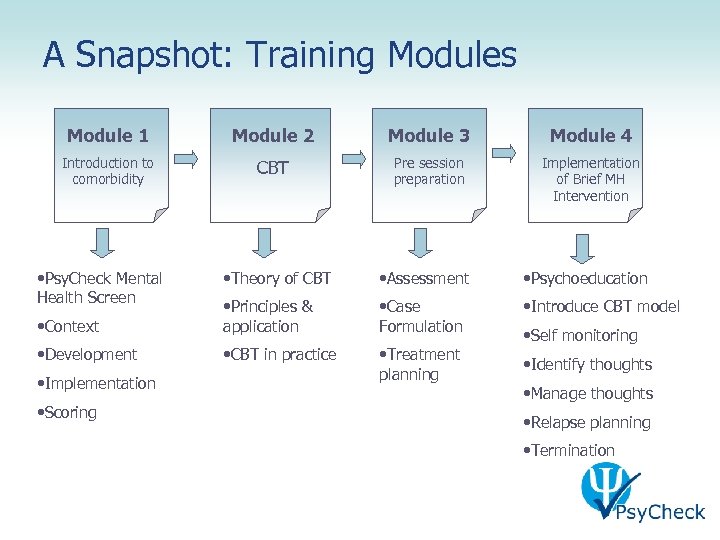 A Snapshot: Training Modules Module 1 Module 2 Module 3 Module 4 Introduction to comorbidity CBT Pre session preparation Implementation of Brief MH Intervention • Psy. Check Mental Health Screen • Theory of CBT • Assessment • Psychoeducation • Context • Principles & application • Case Formulation • Introduce CBT model • Development • CBT in practice • Treatment • Identify thoughts planning • Manage thoughts • Implementation • Scoring • Self monitoring • Relapse planning • Termination
A Snapshot: Training Modules Module 1 Module 2 Module 3 Module 4 Introduction to comorbidity CBT Pre session preparation Implementation of Brief MH Intervention • Psy. Check Mental Health Screen • Theory of CBT • Assessment • Psychoeducation • Context • Principles & application • Case Formulation • Introduce CBT model • Development • CBT in practice • Treatment • Identify thoughts planning • Manage thoughts • Implementation • Scoring • Self monitoring • Relapse planning • Termination
 Module 1 Introduction to Comorbidity & Psy. Check Mental Health Screen
Module 1 Introduction to Comorbidity & Psy. Check Mental Health Screen
 • To provide a context for the Psy. Check Screening Tool • To understand the development and psychometric properties of Psy. Check • To gain skills in implementation, scoring and interpretation of Psy. Check Module 1 Aims of Module 1
• To provide a context for the Psy. Check Screening Tool • To understand the development and psychometric properties of Psy. Check • To gain skills in implementation, scoring and interpretation of Psy. Check Module 1 Aims of Module 1
 • Introduction to Comorbidity • Development of Psy. Check • Psychometric properties of the Psy. Check Screening Tool • Negotiating the Users Guide • Administering the Psy. Check Screening Tool • Mental Health Screen • Suicide/Self-Harm Risk Assessment • Self Reporting Questionnaire Tool • Interpreting the Psy. Check Screening Module 1 Overview of Components of Module 1
• Introduction to Comorbidity • Development of Psy. Check • Psychometric properties of the Psy. Check Screening Tool • Negotiating the Users Guide • Administering the Psy. Check Screening Tool • Mental Health Screen • Suicide/Self-Harm Risk Assessment • Self Reporting Questionnaire Tool • Interpreting the Psy. Check Screening Module 1 Overview of Components of Module 1
 • Up to a third of mental health clients have an AOD problem • May be referred in to AOD services • Up to 80% of AOD clients also have a cooccurring mental health problem • Many more may have subclinical symptoms • Rule rather than the exception in treatment settings Module 1 Introduction to Comorbidity
• Up to a third of mental health clients have an AOD problem • May be referred in to AOD services • Up to 80% of AOD clients also have a cooccurring mental health problem • Many more may have subclinical symptoms • Rule rather than the exception in treatment settings Module 1 Introduction to Comorbidity
 • Those that have comorbid AOD and mental health problems have • • Poorer prognosis Higher risk of harm Greater likelihood of relapse to both disorders Greater use of health services Module 1 Introduction to Comorbidity
• Those that have comorbid AOD and mental health problems have • • Poorer prognosis Higher risk of harm Greater likelihood of relapse to both disorders Greater use of health services Module 1 Introduction to Comorbidity
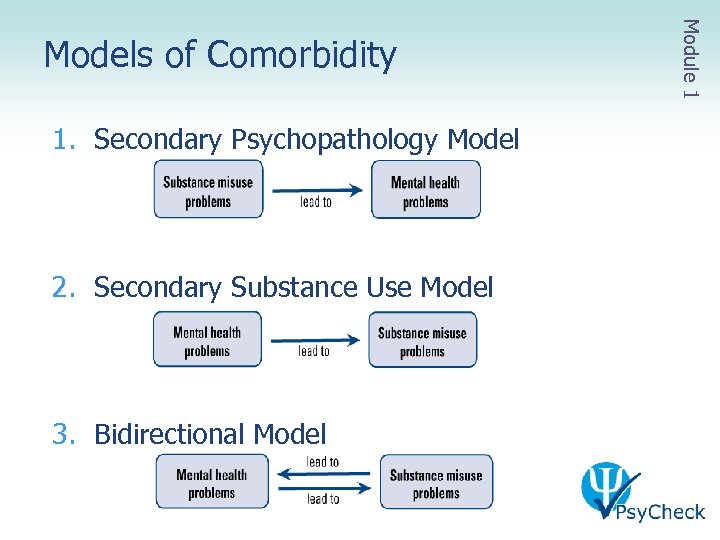 1. Secondary Psychopathology Model 2. Secondary Substance Use Model 3. Bidirectional Model Module 1 Models of Comorbidity
1. Secondary Psychopathology Model 2. Secondary Substance Use Model 3. Bidirectional Model Module 1 Models of Comorbidity
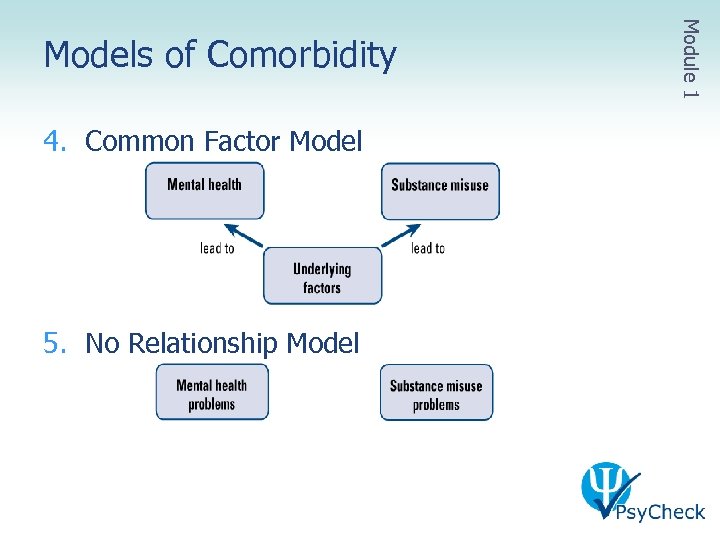 4. Common Factor Model 5. No Relationship Model Module 1 Models of Comorbidity
4. Common Factor Model 5. No Relationship Model Module 1 Models of Comorbidity
 • Comorbidity is the norm • In both mental health and alcohol and drug services BUT • Client group is very different in each service Module 1 Comorbidity in Practice
• Comorbidity is the norm • In both mental health and alcohol and drug services BUT • Client group is very different in each service Module 1 Comorbidity in Practice
 • In Mental Health Services • Mostly psychotic disorders with range of alcohol and other drug issues • In Alcohol and Drug Services • Mostly high prevalence disorders: anxiety and depression • Often not able to refer to Mental Health Services • Often have subclinical symptoms: often go undetected Module 1 Comorbidity in Practice
• In Mental Health Services • Mostly psychotic disorders with range of alcohol and other drug issues • In Alcohol and Drug Services • Mostly high prevalence disorders: anxiety and depression • Often not able to refer to Mental Health Services • Often have subclinical symptoms: often go undetected Module 1 Comorbidity in Practice
 • Sequential • Treat one problem first • Parallel • Simultaneous treatment in different service provider • Integrated treatment by same service provider • Best empirical support • Client and clinician preference Module 1 Treatment for Comorbidity
• Sequential • Treat one problem first • Parallel • Simultaneous treatment in different service provider • Integrated treatment by same service provider • Best empirical support • Client and clinician preference Module 1 Treatment for Comorbidity
 • Many AOD clinicians report training is • Concentrated on acute low prevalence disorders • Focused on relationship building with Mental Health Services Module 1 Comorbidity Training
• Many AOD clinicians report training is • Concentrated on acute low prevalence disorders • Focused on relationship building with Mental Health Services Module 1 Comorbidity Training
 • Designed for AOD clinicians with little or no experience in mental health interventions • But can still be used by experienced clinicians • Focused on the disorders most commonly encountered in AOD Services • Anxiety, depression, some somatic symptoms • Offers a screening tool and articulated intervention • Offers options for training and support through clinical supervision Module 1 Psy. Check Developed to Address Gaps
• Designed for AOD clinicians with little or no experience in mental health interventions • But can still be used by experienced clinicians • Focused on the disorders most commonly encountered in AOD Services • Anxiety, depression, some somatic symptoms • Offers a screening tool and articulated intervention • Offers options for training and support through clinical supervision Module 1 Psy. Check Developed to Address Gaps
 • Screening and intervention for anxiety and depression among AOD clients • Brief screening • 4 session intervention • Youth modifications • Extension material • Accompanying resources • Psy. Check Screening Tool User’s Guide • Psy. Check Clinical Treatment Guidelines Module 1 Psy. Check Overview
• Screening and intervention for anxiety and depression among AOD clients • Brief screening • 4 session intervention • Youth modifications • Extension material • Accompanying resources • Psy. Check Screening Tool User’s Guide • Psy. Check Clinical Treatment Guidelines Module 1 Psy. Check Overview
 • Comprehensive capacity building • 4 module workshop • Clinical supervision • Part of a whole organisation approach to improving comorbidity services for our clients • Managers resources (Implementation Guidelines) • Clinical supervisors resources (Training and Clinical Supervision Guidelines) Module 1 Psy. Check Overview
• Comprehensive capacity building • 4 module workshop • Clinical supervision • Part of a whole organisation approach to improving comorbidity services for our clients • Managers resources (Implementation Guidelines) • Clinical supervisors resources (Training and Clinical Supervision Guidelines) Module 1 Psy. Check Overview
 • Psy. Check Screening Tool scientifically validated • A general mental health screen, including history of treatment • A suicide/self harm risk assessment • The Self Reporting Questionnaire (SRQ) • World Health Organization instrument • Assesses current symptoms of anxiety, depression and somatic disorders Module 1 Psy. Check Screening Tool
• Psy. Check Screening Tool scientifically validated • A general mental health screen, including history of treatment • A suicide/self harm risk assessment • The Self Reporting Questionnaire (SRQ) • World Health Organization instrument • Assesses current symptoms of anxiety, depression and somatic disorders Module 1 Psy. Check Screening Tool
 • Evidence based: drawn from empirically supported treatment • Intervention is designed to be integrated into routine AOD practice • CBT principles used in both AOD and mental health • Best practice in both sectors • Easily integrated • Easily manualised • Focus on scientist-practitioner approach • Hypothesis testing • Reflective practice Module 1 Psy. Check Intervention
• Evidence based: drawn from empirically supported treatment • Intervention is designed to be integrated into routine AOD practice • CBT principles used in both AOD and mental health • Best practice in both sectors • Easily integrated • Easily manualised • Focus on scientist-practitioner approach • Hypothesis testing • Reflective practice Module 1 Psy. Check Intervention
 • 120 newly engaged AOD clients • Psy. Check Screening Tool compared to General Health Questionnaire (GHQ) • Both compared to a diagnostic instrument (CIDI) • Results • SRQ superior to GHQ in predicting anxiety and depressive disorder • Cut-off identified that indicates presence of disorder • General mental health screen good indicator of psychosis Module 1 Psychometric Properties
• 120 newly engaged AOD clients • Psy. Check Screening Tool compared to General Health Questionnaire (GHQ) • Both compared to a diagnostic instrument (CIDI) • Results • SRQ superior to GHQ in predicting anxiety and depressive disorder • Cut-off identified that indicates presence of disorder • General mental health screen good indicator of psychosis Module 1 Psychometric Properties
 • About the Psy. Check Screening Tool • Statistical properties • Decision tree • Administration and scoring • General mental health screen • Suicide risk/self harm assessment • Self Reporting Questionnaire • Psy. Check Screening Tool • Sample contingency plan Module 1 Negotiating the Psy. Check User’s Guide
• About the Psy. Check Screening Tool • Statistical properties • Decision tree • Administration and scoring • General mental health screen • Suicide risk/self harm assessment • Self Reporting Questionnaire • Psy. Check Screening Tool • Sample contingency plan Module 1 Negotiating the Psy. Check User’s Guide
 • Designed for routine screening (all clients) • Administer the whole SRQ • Other parts only if information not already collected • Suicidality monitored over time • Suicide assessment a framework not a checklist • Clinical judgement is required • Assess risk of harm to others in same way Module 1 Administering the Screening Tool
• Designed for routine screening (all clients) • Administer the whole SRQ • Other parts only if information not already collected • Suicidality monitored over time • Suicide assessment a framework not a checklist • Clinical judgement is required • Assess risk of harm to others in same way Module 1 Administering the Screening Tool
 • Work in groups of 3 • Select a celebrity square • One person plays the celebrity • 2 clinicians assist each other in administering the Psy. Check Screening Tool • Group Discussion Module 1 Exercise 3: Celebrity Squares
• Work in groups of 3 • Select a celebrity square • One person plays the celebrity • 2 clinicians assist each other in administering the Psy. Check Screening Tool • Group Discussion Module 1 Exercise 3: Celebrity Squares
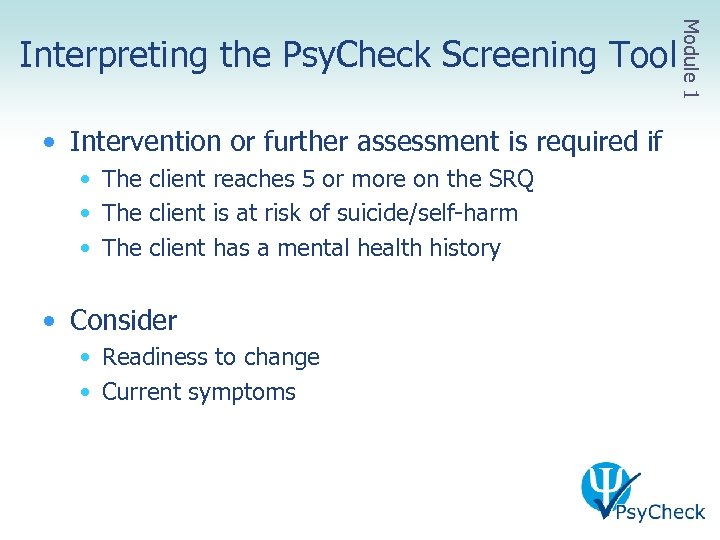 Module 1 Interpreting the Psy. Check Screening Tool • Intervention or further assessment is required if • The client reaches 5 or more on the SRQ • The client is at risk of suicide/self-harm • The client has a mental health history • Consider • Readiness to change • Current symptoms
Module 1 Interpreting the Psy. Check Screening Tool • Intervention or further assessment is required if • The client reaches 5 or more on the SRQ • The client is at risk of suicide/self-harm • The client has a mental health history • Consider • Readiness to change • Current symptoms
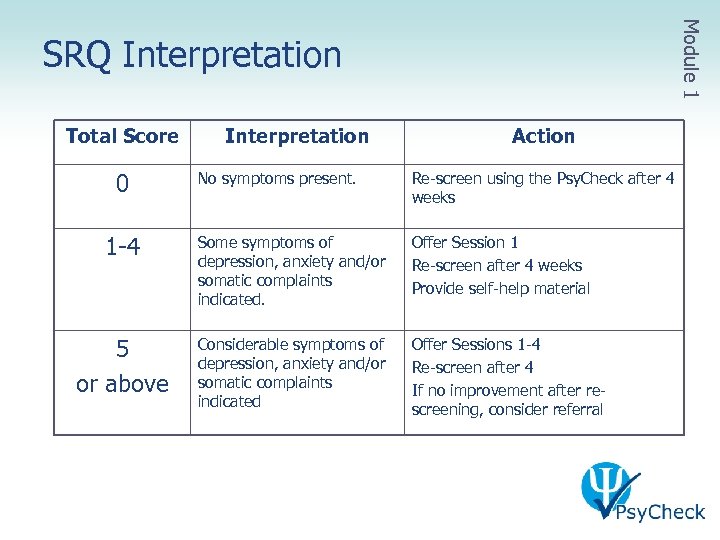 Module 1 SRQ Interpretation Total Score 0 Interpretation Action No symptoms present. Re-screen using the Psy. Check after 4 weeks 1 -4 Some symptoms of depression, anxiety and/or somatic complaints indicated. Offer Session 1 Re-screen after 4 weeks Provide self-help material 5 or above Considerable symptoms of depression, anxiety and/or somatic complaints indicated Offer Sessions 1 -4 Re-screen after 4 If no improvement after rescreening, consider referral
Module 1 SRQ Interpretation Total Score 0 Interpretation Action No symptoms present. Re-screen using the Psy. Check after 4 weeks 1 -4 Some symptoms of depression, anxiety and/or somatic complaints indicated. Offer Session 1 Re-screen after 4 weeks Provide self-help material 5 or above Considerable symptoms of depression, anxiety and/or somatic complaints indicated Offer Sessions 1 -4 Re-screen after 4 If no improvement after rescreening, consider referral
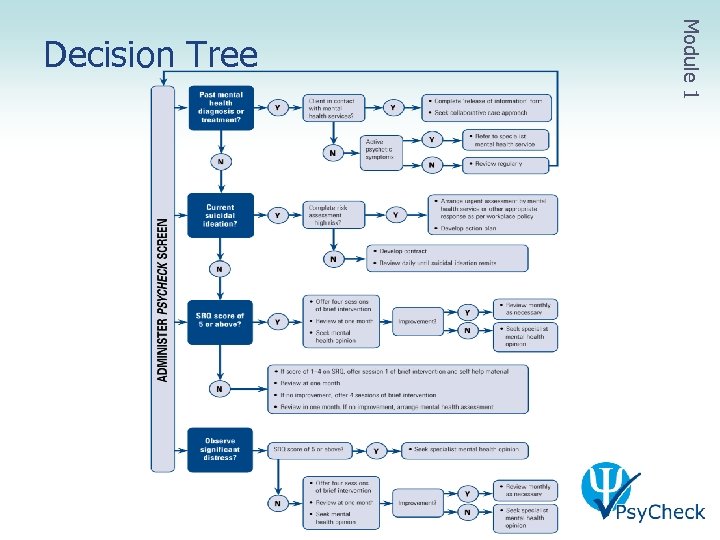 Module 1 Decision Tree
Module 1 Decision Tree
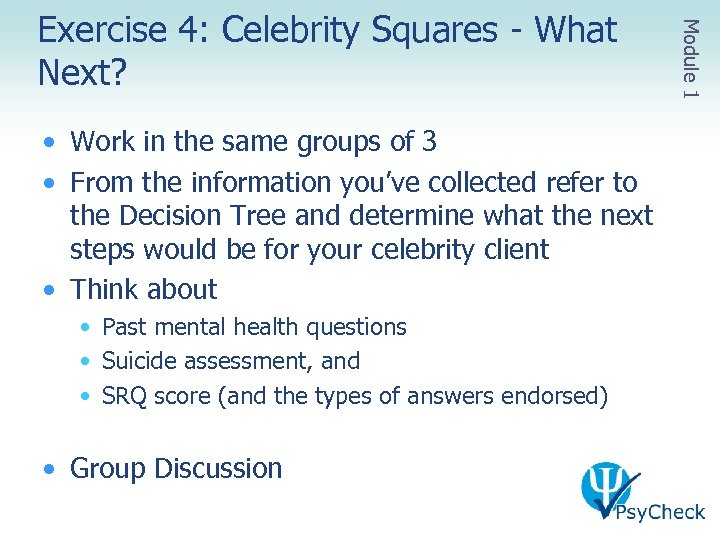 • Work in the same groups of 3 • From the information you’ve collected refer to the Decision Tree and determine what the next steps would be for your celebrity client • Think about • Past mental health questions • Suicide assessment, and • SRQ score (and the types of answers endorsed) • Group Discussion Module 1 Exercise 4: Celebrity Squares - What Next?
• Work in the same groups of 3 • From the information you’ve collected refer to the Decision Tree and determine what the next steps would be for your celebrity client • Think about • Past mental health questions • Suicide assessment, and • SRQ score (and the types of answers endorsed) • Group Discussion Module 1 Exercise 4: Celebrity Squares - What Next?
 I’m never going to get this I may as well give up now I’m useless Module 1 What’s on Your Mind – Is It This…?
I’m never going to get this I may as well give up now I’m useless Module 1 What’s on Your Mind – Is It This…?
 Module 1 Or This …? I’m getting some of this If I hang in it will fall into place I feel confident I will get it
Module 1 Or This …? I’m getting some of this If I hang in it will fall into place I feel confident I will get it
 Module 1 Or Maybe This …? This is too easy… What if I get bored… I’ll think about how I can use it in my practice
Module 1 Or Maybe This …? This is too easy… What if I get bored… I’ll think about how I can use it in my practice
 Module 2 Cognitive Behaviour Therapy
Module 2 Cognitive Behaviour Therapy
 • To understand theory of CBT • To understand the principles of application underpinning the Psy. Check intervention • To understand of the practice of CBT Module 2 Aims: Module 2
• To understand theory of CBT • To understand the principles of application underpinning the Psy. Check intervention • To understand of the practice of CBT Module 2 Aims: Module 2
 • Introduction to CBT • Theoretical underpinnings • CBT Model • Evidenced based practice • CBT in practice • Standard sessions • Self-monitoring Module 2 Overview: Module 2
• Introduction to CBT • Theoretical underpinnings • CBT Model • Evidenced based practice • CBT in practice • Standard sessions • Self-monitoring Module 2 Overview: Module 2
 Module 2 Exercise 5: What Works for You? • Working individually complete the worksheet, identifying which models you have an affinity with • Then circle the main model you work with • Now find someone else in the room that uses a DIFFERENT model to the one you typically work with and discuss with your partner • Why you use this model/strategies you do? • How you know it’s working ? • Group discussion
Module 2 Exercise 5: What Works for You? • Working individually complete the worksheet, identifying which models you have an affinity with • Then circle the main model you work with • Now find someone else in the room that uses a DIFFERENT model to the one you typically work with and discuss with your partner • Why you use this model/strategies you do? • How you know it’s working ? • Group discussion
 • There is emerging evidence that a single theory planned approach is more effective than an ad hoc one • Most effective to have a single framework or philosophy about treatment and incorporate a range of techniques and strategies that fit with your philosophy Cognitive Behavioural Approach Module 2 Planned Approach
• There is emerging evidence that a single theory planned approach is more effective than an ad hoc one • Most effective to have a single framework or philosophy about treatment and incorporate a range of techniques and strategies that fit with your philosophy Cognitive Behavioural Approach Module 2 Planned Approach
 Module 2 Evidenced Based Practice • Best evidence for CBT compared to other types of therapies • Most high level research (RCTs) and the most positive research • Effective for a wide range of mental health problems including AOD, anxiety and depression BUT Whatever framework you use, you can create your own evidence through measuring individual outcomes – CBT emphasises this
Module 2 Evidenced Based Practice • Best evidence for CBT compared to other types of therapies • Most high level research (RCTs) and the most positive research • Effective for a wide range of mental health problems including AOD, anxiety and depression BUT Whatever framework you use, you can create your own evidence through measuring individual outcomes – CBT emphasises this
 • Umbrella term for a range of therapies with a cognitive and/or behavioural focus • Therapy examples • • • Cognitive Therapy (Aaron Beck) Relapse Prevention (G. Alan Marlatt) Coping Skills Therapy (Peter Monti) Mindfulness Therapy (Mark Williams) Schema Therapy (Jeff Young) Dialectical Behaviour Therapy (Marsha Linehan) Module 2 What is CBT? • Strategy examples • • • Problem Solving Goal Setting Cue Exposure Therapy Thought stopping Urge surfing Activity scheduling…
• Umbrella term for a range of therapies with a cognitive and/or behavioural focus • Therapy examples • • • Cognitive Therapy (Aaron Beck) Relapse Prevention (G. Alan Marlatt) Coping Skills Therapy (Peter Monti) Mindfulness Therapy (Mark Williams) Schema Therapy (Jeff Young) Dialectical Behaviour Therapy (Marsha Linehan) Module 2 What is CBT? • Strategy examples • • • Problem Solving Goal Setting Cue Exposure Therapy Thought stopping Urge surfing Activity scheduling…
 • Solution-Focused Therapy • An understanding of the past and cause of problem not necessary for resolution of the problem • Change occurs as a result of a focus on the future without the problem • Narrative Therapy • Focus is on meaning, narrative and power • Talking about the influence of problems enables talk about their defeat via the new stories Module 2 In Comparison…
• Solution-Focused Therapy • An understanding of the past and cause of problem not necessary for resolution of the problem • Change occurs as a result of a focus on the future without the problem • Narrative Therapy • Focus is on meaning, narrative and power • Talking about the influence of problems enables talk about their defeat via the new stories Module 2 In Comparison…
 • Gestalt Therapy • Focus is on the present rather than past or future • Central aim is awareness-raising and creating conditions to de-construct dysfunctional fixed or habitual patterns of interaction • Change occurs through understanding and acceptance of what is • Psychodynamic Therapy • Focus is on initial underlying causes • Understanding and having insight into the problem leads to change • Therapeutic relationship is the key to change Module 2 In Comparison…
• Gestalt Therapy • Focus is on the present rather than past or future • Central aim is awareness-raising and creating conditions to de-construct dysfunctional fixed or habitual patterns of interaction • Change occurs through understanding and acceptance of what is • Psychodynamic Therapy • Focus is on initial underlying causes • Understanding and having insight into the problem leads to change • Therapeutic relationship is the key to change Module 2 In Comparison…
 • ‘Self-help’ oriented • Clinician provides tools and framework for change • Client’s responsibility to create and maintain change • Skills oriented • Attention to therapeutic process vital but not sufficient in itself for change to occur • Structured but not inflexible • Clinical judgement necessary Module 2 What is CBT?
• ‘Self-help’ oriented • Clinician provides tools and framework for change • Client’s responsibility to create and maintain change • Skills oriented • Attention to therapeutic process vital but not sufficient in itself for change to occur • Structured but not inflexible • Clinical judgement necessary Module 2 What is CBT?
 CBT… • is based on an ever-evolving formulation of the client in cognitive terms • requires a sound therapeutic alliance • emphasises collaboration and active participation • is goal oriented and problem focused • initially emphasises the present Module 2 CBT Principles
CBT… • is based on an ever-evolving formulation of the client in cognitive terms • requires a sound therapeutic alliance • emphasises collaboration and active participation • is goal oriented and problem focused • initially emphasises the present Module 2 CBT Principles
 CBT… • is educative, aims to teach the client to be their own therapist, and emphasises relapse prevention • is time limited • sessions are structured • teaches clients to identify, evaluate and respond to their dysfunctional thoughts and beliefs • uses a variety of techniques to change thinking, mood and behaviour Module 2 CBT Principles
CBT… • is educative, aims to teach the client to be their own therapist, and emphasises relapse prevention • is time limited • sessions are structured • teaches clients to identify, evaluate and respond to their dysfunctional thoughts and beliefs • uses a variety of techniques to change thinking, mood and behaviour Module 2 CBT Principles
 • From the cards you have been given, keep the ones that represent the way you work (in the majority) and trade unwanted cards for wanted cards with other participants • Either • Line up on the cognitive/behavioural continuum to show whether you work more in a cognitive or behavioral approach, or • Place your cards on the grid (cognitive/behavioural vs skills/process) • Group discussion • Why did you put your card or yourself where you did? • Did the cards fall in a pattern? Module 2 Exercise 6: Mix ‘n’ Match
• From the cards you have been given, keep the ones that represent the way you work (in the majority) and trade unwanted cards for wanted cards with other participants • Either • Line up on the cognitive/behavioural continuum to show whether you work more in a cognitive or behavioral approach, or • Place your cards on the grid (cognitive/behavioural vs skills/process) • Group discussion • Why did you put your card or yourself where you did? • Did the cards fall in a pattern? Module 2 Exercise 6: Mix ‘n’ Match
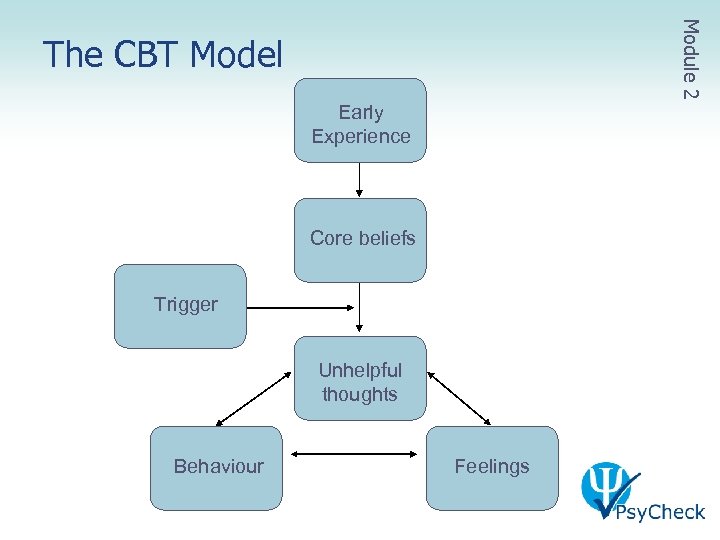 Module 2 The CBT Model Early Experience Core beliefs Trigger Unhelpful thoughts Behaviour Feelings
Module 2 The CBT Model Early Experience Core beliefs Trigger Unhelpful thoughts Behaviour Feelings
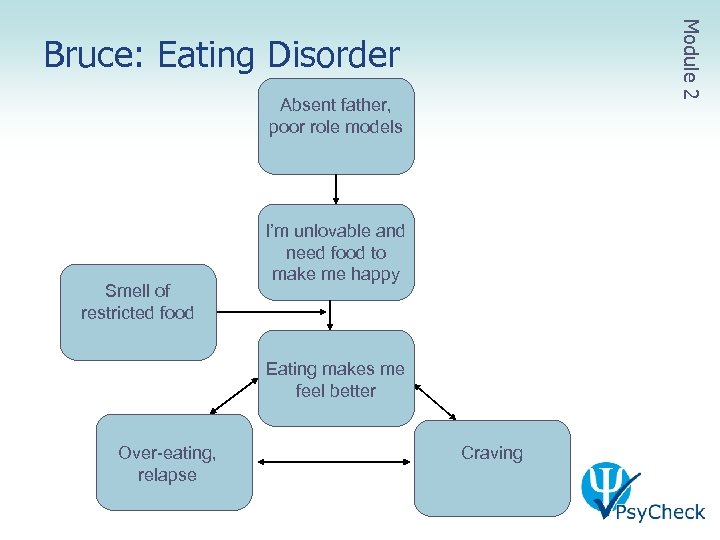 Module 2 Bruce: Eating Disorder Absent father, poor role models Smell of restricted food I’m unlovable and need food to make me happy Eating makes me feel better Over-eating, relapse Craving
Module 2 Bruce: Eating Disorder Absent father, poor role models Smell of restricted food I’m unlovable and need food to make me happy Eating makes me feel better Over-eating, relapse Craving
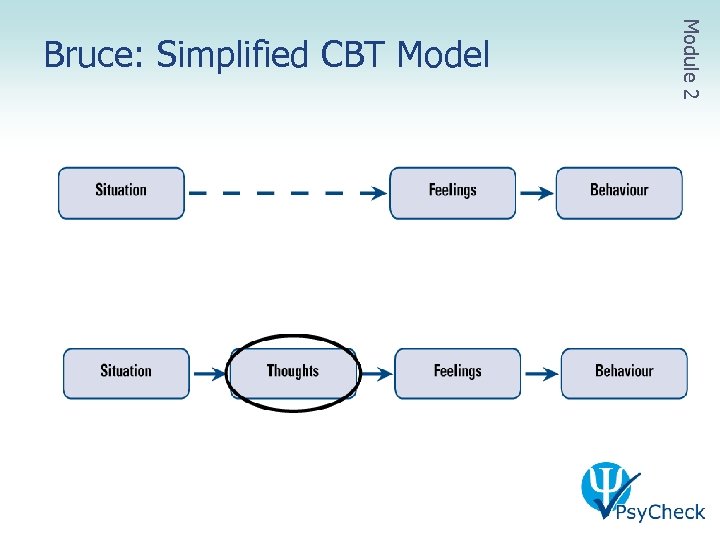 Module 2 Bruce: Simplified CBT Model
Module 2 Bruce: Simplified CBT Model
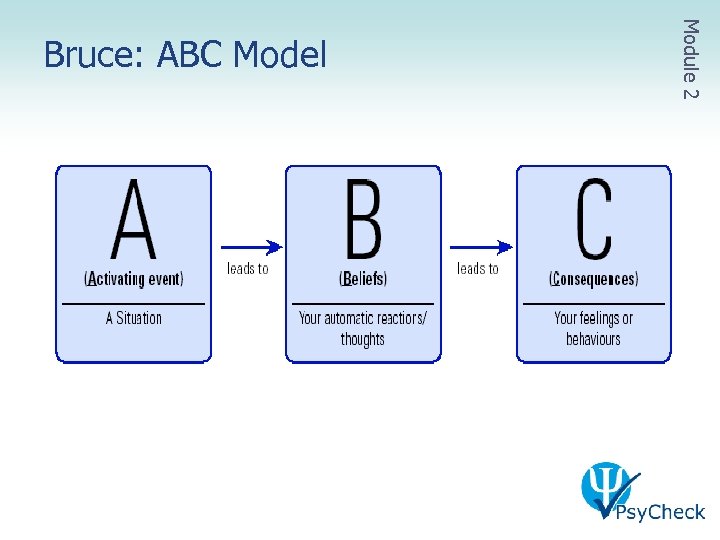 Module 2 Bruce: ABC Model
Module 2 Bruce: ABC Model
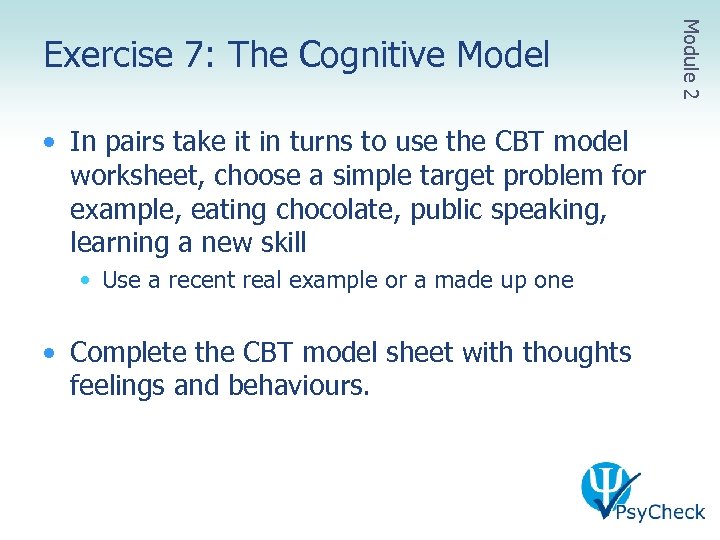 • In pairs take it in turns to use the CBT model worksheet, choose a simple target problem for example, eating chocolate, public speaking, learning a new skill • Use a recent real example or a made up one • Complete the CBT model sheet with thoughts feelings and behaviours. Module 2 Exercise 7: The Cognitive Model
• In pairs take it in turns to use the CBT model worksheet, choose a simple target problem for example, eating chocolate, public speaking, learning a new skill • Use a recent real example or a made up one • Complete the CBT model sheet with thoughts feelings and behaviours. Module 2 Exercise 7: The Cognitive Model
 • I: Review and feedback from last session • II: Information and practice of session topic • III: Summary and feedback from this session Module 2 Typical Session Format
• I: Review and feedback from last session • II: Information and practice of session topic • III: Summary and feedback from this session Module 2 Typical Session Format
 • Check-in past week, mood/drug use, homework • ‘What’s been happening this week? ’ • ‘How’s your [mood] been this week? ’ • ‘How did you go with your homework? ’ • Bridge from previous session • ‘Remember last week we talked about [x]… did you have any more thoughts about it? ’ • ‘Were you able to get any practice of [skill]’ Module 2 CBT in Practice I: Review and Feedback
• Check-in past week, mood/drug use, homework • ‘What’s been happening this week? ’ • ‘How’s your [mood] been this week? ’ • ‘How did you go with your homework? ’ • Bridge from previous session • ‘Remember last week we talked about [x]… did you have any more thoughts about it? ’ • ‘Were you able to get any practice of [skill]’ Module 2 CBT in Practice I: Review and Feedback
![• Information about skill • ‘last week we talked about [identifying thoughts] this • Information about skill • ‘last week we talked about [identifying thoughts] this](https://present5.com/presentation/64afd592da4b37bb99cd9e99ab88370d/image-52.jpg) • Information about skill • ‘last week we talked about [identifying thoughts] this week I thought we’d talk about how to manage those thoughts…’ • ‘Remember the cognitive model…the way I like to think about it is…’ • Practice of skill in session • ‘let’s try to do this together…’ [use whiteboard] Module 2 CBT in Practice II: Info & Practice
• Information about skill • ‘last week we talked about [identifying thoughts] this week I thought we’d talk about how to manage those thoughts…’ • ‘Remember the cognitive model…the way I like to think about it is…’ • Practice of skill in session • ‘let’s try to do this together…’ [use whiteboard] Module 2 CBT in Practice II: Info & Practice
 • Summary and feedback • ‘so what we talked about today was…’ • ‘how does that fit with you…? ’ • Set homework tasks • ‘it’s really important to practice these things between sessions so they become second nature… what do you think you could do that would help you remember what we did? ’ Module 2 CBT in Practice III: Summary & Feedback
• Summary and feedback • ‘so what we talked about today was…’ • ‘how does that fit with you…? ’ • Set homework tasks • ‘it’s really important to practice these things between sessions so they become second nature… what do you think you could do that would help you remember what we did? ’ Module 2 CBT in Practice III: Summary & Feedback
 • A. Watch video demonstration of basic elements of a session • Discussion about the elements as a group • B. Practice the elements in pairs • Feedback to each other good aspects and an area for improvement Module 2 Exercise 8: CBT Demonstration I
• A. Watch video demonstration of basic elements of a session • Discussion about the elements as a group • B. Practice the elements in pairs • Feedback to each other good aspects and an area for improvement Module 2 Exercise 8: CBT Demonstration I
 • Interventions are applied from the least to most intensive • Each step is incremental based on the client's response to the previous one • A stepped care approach can add flexibility to treatment and improve outcomes • CBT (and Psy. Check) facilitates the stepped care approach Module 2 Stepped Care Approach
• Interventions are applied from the least to most intensive • Each step is incremental based on the client's response to the previous one • A stepped care approach can add flexibility to treatment and improve outcomes • CBT (and Psy. Check) facilitates the stepped care approach Module 2 Stepped Care Approach
 • Therapeutic alliance vital • Basis of ALL therapy • Requires good counselling skills • Necessary but not sufficient condition for change • Collaboration and active participation by client and clinician essential • Requires good active and empathetic listening skills • CBT builds therapeutic alliance through collaboration and encouraging client involvement in their own therapy Module 2 Therapeutic Relationship
• Therapeutic alliance vital • Basis of ALL therapy • Requires good counselling skills • Necessary but not sufficient condition for change • Collaboration and active participation by client and clinician essential • Requires good active and empathetic listening skills • CBT builds therapeutic alliance through collaboration and encouraging client involvement in their own therapy Module 2 Therapeutic Relationship
 • Clinical judgement is required, even though therapy is manualised • Use Psy. Check as guidelines – follow steps only as closely as you need to • Use flexibly with extension material to tailor to client’s needs • Consider existing clinical practices and pathways Module 2 Clinical Judgement
• Clinical judgement is required, even though therapy is manualised • Use Psy. Check as guidelines – follow steps only as closely as you need to • Use flexibly with extension material to tailor to client’s needs • Consider existing clinical practices and pathways Module 2 Clinical Judgement
 • Psy. Check designed to be integrated into routine AOD treatment • Techniques are deliberately similar to those in AOD treatment • Emphasise to the client the link between AOD use and mental health problems • Consider ways in which you can integrate into what you already do Module 2 Integrated Treatment
• Psy. Check designed to be integrated into routine AOD treatment • Techniques are deliberately similar to those in AOD treatment • Emphasise to the client the link between AOD use and mental health problems • Consider ways in which you can integrate into what you already do Module 2 Integrated Treatment
 • In small groups (3 -4) discuss how therapeutic processes can be used in CBT • What makes a good therapeutic alliance - list as many elements as you can? • What could happen if you don’t have a good therapeutic alliance? Think about the client, the practitioner and therapy relationship • Group discussion Module 2 Exercise 9: Therapeutic Process
• In small groups (3 -4) discuss how therapeutic processes can be used in CBT • What makes a good therapeutic alliance - list as many elements as you can? • What could happen if you don’t have a good therapeutic alliance? Think about the client, the practitioner and therapy relationship • Group discussion Module 2 Exercise 9: Therapeutic Process
 What have we learned so far…. . ? Module 2 Let’s Take a Breather…
What have we learned so far…. . ? Module 2 Let’s Take a Breather…
 What brief practice at home would assist you to consolidate the knowledge you gained in this module? • eg. Use the CBT model on your self • eg. Further reading about CBT • eg. Practice explain the CBT model to a client/colleague Next session you will be asked to share your experience of self practice if you are willing, (but not of the actual target problem itself if you used yourself as a client) Module 2 Homework
What brief practice at home would assist you to consolidate the knowledge you gained in this module? • eg. Use the CBT model on your self • eg. Further reading about CBT • eg. Practice explain the CBT model to a client/colleague Next session you will be asked to share your experience of self practice if you are willing, (but not of the actual target problem itself if you used yourself as a client) Module 2 Homework
 Module 3 Pre-Session Preparation: Assessment, Formulation and Treatment Planning
Module 3 Pre-Session Preparation: Assessment, Formulation and Treatment Planning
 • What did we do last time? • What is your feedback about what we covered? • Homework feedback • Challenges in completing the homework? • What was the effect of self-practice? • Next step…? Module 3 Before We Start…
• What did we do last time? • What is your feedback about what we covered? • Homework feedback • Challenges in completing the homework? • What was the effect of self-practice? • Next step…? Module 3 Before We Start…
 • Work in groups of 3, you have just interviewed your celebrity. Write a few lines using the following criteria as if you were writing for a trash magazine • • • Their current problem Their presenting mood/feelings Thoughts Behaviour What’s driving the behaviour Consequences of behaviour • Present to the large group Module 3 Exercise 10: The Young and The Restless
• Work in groups of 3, you have just interviewed your celebrity. Write a few lines using the following criteria as if you were writing for a trash magazine • • • Their current problem Their presenting mood/feelings Thoughts Behaviour What’s driving the behaviour Consequences of behaviour • Present to the large group Module 3 Exercise 10: The Young and The Restless
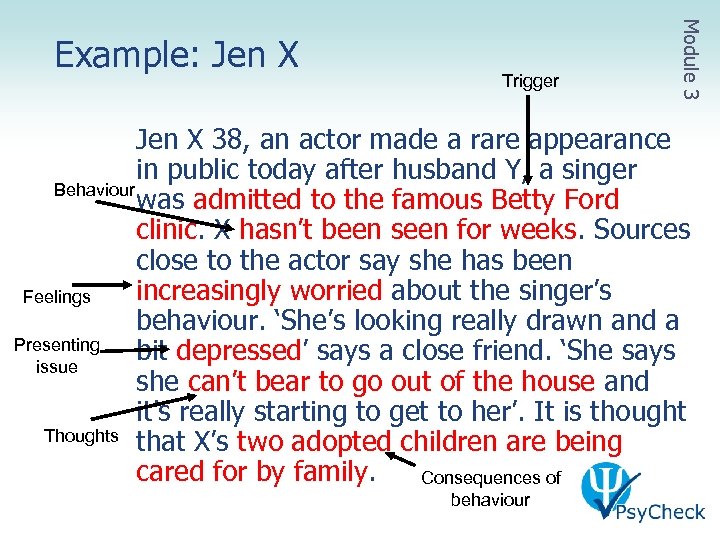 Trigger Module 3 Example: Jen X 38, an actor made a rare appearance in public today after husband Y, a singer Behaviour was admitted to the famous Betty Ford clinic. X hasn’t been seen for weeks. Sources close to the actor say she has been increasingly worried about the singer’s Feelings behaviour. ‘She’s looking really drawn and a Presenting bit depressed’ says a close friend. ‘She says issue she can’t bear to go out of the house and it’s really starting to get to her’. It is thought Thoughts that X’s two adopted children are being cared for by family. Consequences of behaviour
Trigger Module 3 Example: Jen X 38, an actor made a rare appearance in public today after husband Y, a singer Behaviour was admitted to the famous Betty Ford clinic. X hasn’t been seen for weeks. Sources close to the actor say she has been increasingly worried about the singer’s Feelings behaviour. ‘She’s looking really drawn and a Presenting bit depressed’ says a close friend. ‘She says issue she can’t bear to go out of the house and it’s really starting to get to her’. It is thought Thoughts that X’s two adopted children are being cared for by family. Consequences of behaviour
 • To understand how to screen for mental health issues and prepare feedback • To understand how to undertake a cognitive behavioural assessment • To understand how to collect sufficient information to develop a cognitive behavioural formulation Module 3 Aims: Module 3
• To understand how to screen for mental health issues and prepare feedback • To understand how to undertake a cognitive behavioural assessment • To understand how to collect sufficient information to develop a cognitive behavioural formulation Module 3 Aims: Module 3
 • Negotiating the Psy. Check Intervention & Clinical Treatment Guidelines • Undertake screening and preparing feedback • Undertake a cognitive behavioural assessment • Prepare a preliminary case formulation Module 3 Overview: Module 3
• Negotiating the Psy. Check Intervention & Clinical Treatment Guidelines • Undertake screening and preparing feedback • Undertake a cognitive behavioural assessment • Prepare a preliminary case formulation Module 3 Overview: Module 3
 • Designed for a range of experience and background • Manualised for new clinicians • Use flexibly for experienced clinicians • Use with • Introduction to Psy. Check package • Psy. Check Screening Tool and User’s Guide Module 3 Negotiating the Psy. Check Clinical Treatment Guidelines
• Designed for a range of experience and background • Manualised for new clinicians • Use flexibly for experienced clinicians • Use with • Introduction to Psy. Check package • Psy. Check Screening Tool and User’s Guide Module 3 Negotiating the Psy. Check Clinical Treatment Guidelines
 • Three sections • Principles of intervention • Practice Guidelines • Extension material • Worksheets • Modifications for young people Module 3 Negotiating the Psy. Check Clinical Treatment Guidelines
• Three sections • Principles of intervention • Practice Guidelines • Extension material • Worksheets • Modifications for young people Module 3 Negotiating the Psy. Check Clinical Treatment Guidelines
 • Pre-session preparation: Reflection • • Prepare feedback from the Psy. Check Screening Tool Cognitive behavioural assessment Cognitive behavioural formulation Treatment planning • Psy. Check intervention • • Session 1: Introduction Session 2: Identifying unhelpful thoughts Session 3: Managing unhelpful thoughts Session 4: Relapse prevention Module 3 Practice Guidelines
• Pre-session preparation: Reflection • • Prepare feedback from the Psy. Check Screening Tool Cognitive behavioural assessment Cognitive behavioural formulation Treatment planning • Psy. Check intervention • • Session 1: Introduction Session 2: Identifying unhelpful thoughts Session 3: Managing unhelpful thoughts Session 4: Relapse prevention Module 3 Practice Guidelines
 • Psy. Check screening • Snapshot of potential need • Feedback • Results of Psy. Check Screening Tool • Any other information gathered Module 3 Screening in Context
• Psy. Check screening • Snapshot of potential need • Feedback • Results of Psy. Check Screening Tool • Any other information gathered Module 3 Screening in Context
 • Also known as ‘functional’ assessment • Occurs during an assessment session and continues through therapy • Functional vs structural/diagnostic analysis • Drivers vs descriptors of behaviour/problem Module 3 Cognitive Behavioural Assessment
• Also known as ‘functional’ assessment • Occurs during an assessment session and continues through therapy • Functional vs structural/diagnostic analysis • Drivers vs descriptors of behaviour/problem Module 3 Cognitive Behavioural Assessment
 • • Presenting issues Pattern (onset and course) Predisposing factors Precipitating factors Perpetuating factors Protective factors Prognosis Other factors Module 3 Cognitive Behavioural Assessment: 7 Ps
• • Presenting issues Pattern (onset and course) Predisposing factors Precipitating factors Perpetuating factors Protective factors Prognosis Other factors Module 3 Cognitive Behavioural Assessment: 7 Ps
 Bruce • Discussion • Identify elements of the functional assessment for Bruce Module 3 Exercise 11: Something Fishy
Bruce • Discussion • Identify elements of the functional assessment for Bruce Module 3 Exercise 11: Something Fishy
 • Case formulation is • Theory driven • An interpretation - more than a case summary or summary of presenting problems • A working hypothesis to be reviewed • Dynamic - as new information comes to hand, your formulation is reviewed, added to, changed • The case formulation puts the 7 Ps into a context • Always present it to your client and ask for their response Module 3 CBT Case Formulation
• Case formulation is • Theory driven • An interpretation - more than a case summary or summary of presenting problems • A working hypothesis to be reviewed • Dynamic - as new information comes to hand, your formulation is reviewed, added to, changed • The case formulation puts the 7 Ps into a context • Always present it to your client and ask for their response Module 3 CBT Case Formulation
 • • • Clarifying hypotheses and questions Understanding the overall picture Prioritising issues and problems Planning treatment strategies Predicting responses to interventions Identifying barriers to progress Module 3 The Purpose of Case Formulation
• • • Clarifying hypotheses and questions Understanding the overall picture Prioritising issues and problems Planning treatment strategies Predicting responses to interventions Identifying barriers to progress Module 3 The Purpose of Case Formulation
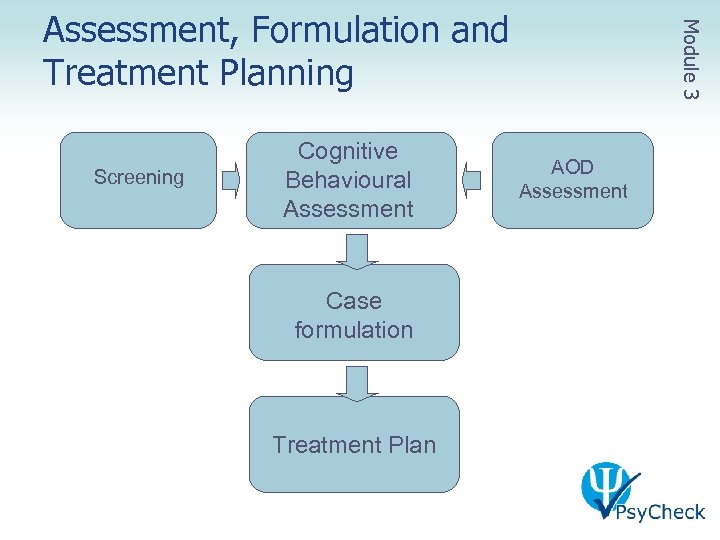 Screening Cognitive Behavioural Assessment Case formulation Treatment Plan AOD Assessment Module 3 Assessment, Formulation and Treatment Planning
Screening Cognitive Behavioural Assessment Case formulation Treatment Plan AOD Assessment Module 3 Assessment, Formulation and Treatment Planning
 • Identify the components of formulation as a group • In small groups, use the information from the earlier exercise, Something Fishy • Write a formal formulation from this information • Use the formal formulation to ‘translate’ this into language suitable for a client • Group discussion Module 3 Exercise 12: Fishy Formulation
• Identify the components of formulation as a group • In small groups, use the information from the earlier exercise, Something Fishy • Write a formal formulation from this information • Use the formal formulation to ‘translate’ this into language suitable for a client • Group discussion Module 3 Exercise 12: Fishy Formulation
 • Return to your small groups, use the previous case formulation and develop the treatment plan for Bruce including: • Immediate strategies • Longer term strategies • Referral options • One person in your group to role play Bruce and share presenting the formulation and treatment plan to him • Think about the stage of change, insight and the way you present it to him. Notice how he responds. Module 3 Exercise 13: Gummy Shark
• Return to your small groups, use the previous case formulation and develop the treatment plan for Bruce including: • Immediate strategies • Longer term strategies • Referral options • One person in your group to role play Bruce and share presenting the formulation and treatment plan to him • Think about the stage of change, insight and the way you present it to him. Notice how he responds. Module 3 Exercise 13: Gummy Shark
 Let’s go back over what we’ve done so far… Module 3 Checking in Again…
Let’s go back over what we’ve done so far… Module 3 Checking in Again…
 Module 4 Implementation of Brief Mental Health Intervention
Module 4 Implementation of Brief Mental Health Intervention
 • Write down your immediate response to the following • • • Standing in a long line at the supermarket A heavily tattooed woman Someone throwing a cigarette out of a car Running late The beach Case formulation Module 4 Exercise 14: First Response
• Write down your immediate response to the following • • • Standing in a long line at the supermarket A heavily tattooed woman Someone throwing a cigarette out of a car Running late The beach Case formulation Module 4 Exercise 14: First Response
 • Understand cognitive behavioural practice to undertake the Psy. Check Intervention Module 4 Aims: Module 4
• Understand cognitive behavioural practice to undertake the Psy. Check Intervention Module 4 Aims: Module 4
 • Negotiating the step-by-step guide to the 4 session Psy. Check Intervention • Session 1: Psychoeducation • Session 2: Identifying unhelpful thoughts • Session 3: Managing unhelpful thoughts • Session 4: Relapse prevention Module 4 Overview: Module 4
• Negotiating the step-by-step guide to the 4 session Psy. Check Intervention • Session 1: Psychoeducation • Session 2: Identifying unhelpful thoughts • Session 3: Managing unhelpful thoughts • Session 4: Relapse prevention Module 4 Overview: Module 4
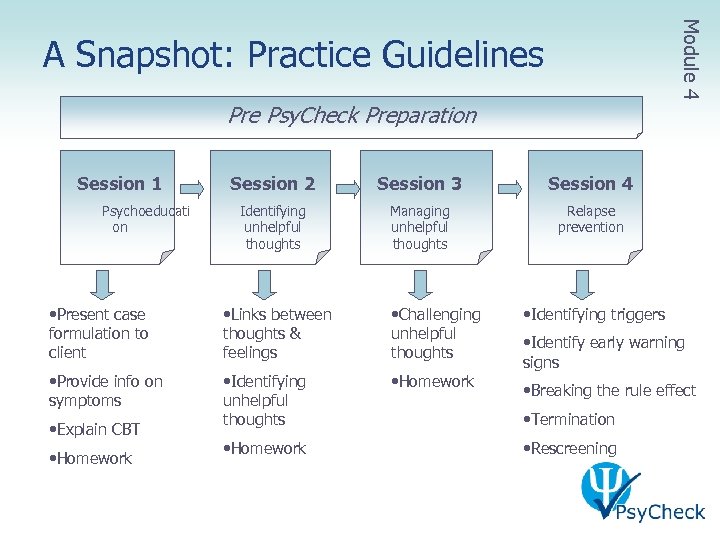 Module 4 A Snapshot: Practice Guidelines Pre Psy. Check Preparation Session 1 Psychoeducati on Session 2 Session 3 Session 4 Identifying unhelpful thoughts Managing unhelpful thoughts Relapse prevention • Present case formulation to client • Links between thoughts & feelings • Challenging unhelpful thoughts • Provide info on symptoms • Identifying unhelpful thoughts • Homework • Explain CBT • Homework • Identifying triggers • Identify early warning signs • Breaking the rule effect • Termination • Rescreening
Module 4 A Snapshot: Practice Guidelines Pre Psy. Check Preparation Session 1 Psychoeducati on Session 2 Session 3 Session 4 Identifying unhelpful thoughts Managing unhelpful thoughts Relapse prevention • Present case formulation to client • Links between thoughts & feelings • Challenging unhelpful thoughts • Provide info on symptoms • Identifying unhelpful thoughts • Homework • Explain CBT • Homework • Identifying triggers • Identify early warning signs • Breaking the rule effect • Termination • Rescreening
 Module 4 Session 1 Presenting the Case Formulation and Beginning Psychoeducation and Self Monitoring
Module 4 Session 1 Presenting the Case Formulation and Beginning Psychoeducation and Self Monitoring
 • Psychoeducation can be about: • Current symptoms • What’s going on for the client (formulation) • CBT model Module 4 Session 1: Psychoeducation
• Psychoeducation can be about: • Current symptoms • What’s going on for the client (formulation) • CBT model Module 4 Session 1: Psychoeducation
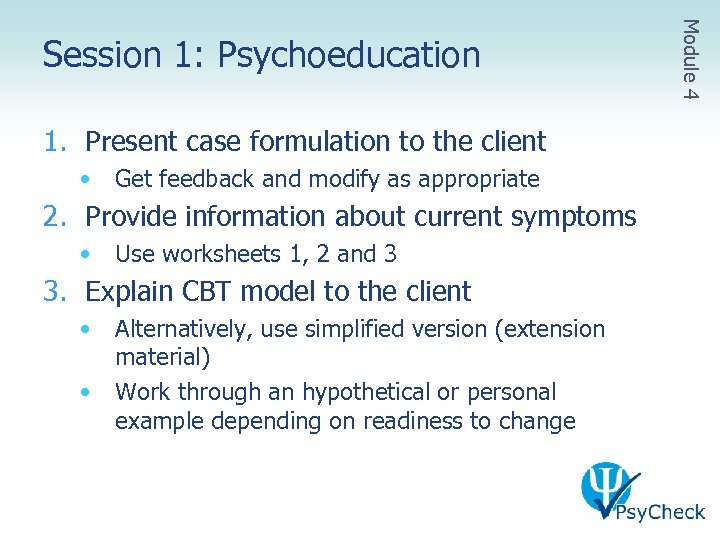 1. Present case formulation to the client • Get feedback and modify as appropriate 2. Provide information about current symptoms • Use worksheets 1, 2 and 3 3. Explain CBT model to the client • • Alternatively, use simplified version (extension material) Work through an hypothetical or personal example depending on readiness to change Module 4 Session 1: Psychoeducation
1. Present case formulation to the client • Get feedback and modify as appropriate 2. Provide information about current symptoms • Use worksheets 1, 2 and 3 3. Explain CBT model to the client • • Alternatively, use simplified version (extension material) Work through an hypothetical or personal example depending on readiness to change Module 4 Session 1: Psychoeducation
 • Link the formulation and treatment • Explain in detail how they are linked using personal examples • Develop a treatment plan with the client • Identify areas for intervention and priorities based on the formulation • Emphasise revisiting both formulation and treatment plan regularly • Finalise and record treatment plan • Give client a copy Module 4 Session 1: Treatment Planning
• Link the formulation and treatment • Explain in detail how they are linked using personal examples • Develop a treatment plan with the client • Identify areas for intervention and priorities based on the formulation • Emphasise revisiting both formulation and treatment plan regularly • Finalise and record treatment plan • Give client a copy Module 4 Session 1: Treatment Planning
 • Use Worksheet 4: Self monitoring • Explain the role of self monitoring • A temporary tool until it becomes automatic • Explain the process of self monitoring • Work through example with client • Give client a copy to take home Module 4 Session 1: Introduce Self-Monitoring
• Use Worksheet 4: Self monitoring • Explain the role of self monitoring • A temporary tool until it becomes automatic • Explain the process of self monitoring • Work through example with client • Give client a copy to take home Module 4 Session 1: Introduce Self-Monitoring
 • Large group discussion • What assists clients to understand self monitoring? • What can clinicians do to get in the way of effective self monitoring? • How do you know if you are being effective or obstructive? Module 4 Exercise 15: Self Monitoring
• Large group discussion • What assists clients to understand self monitoring? • What can clinicians do to get in the way of effective self monitoring? • How do you know if you are being effective or obstructive? Module 4 Exercise 15: Self Monitoring
 • Summarise content and ask for feedback from the client • Emphasise the importance of take home tasks • Set homework – Self Monitoring • Identify any difficulties with content • Identify easiest method • Immediate recording, once a day etc • Emphasise importance • Prepare for next step • Outline next session topic • Organise next appointment or discharge Module 4 Session 1: Session Summary
• Summarise content and ask for feedback from the client • Emphasise the importance of take home tasks • Set homework – Self Monitoring • Identify any difficulties with content • Identify easiest method • Immediate recording, once a day etc • Emphasise importance • Prepare for next step • Outline next session topic • Organise next appointment or discharge Module 4 Session 1: Session Summary
 • Simplified explanation of the CBT model • Alternative explanation of CBT model: ABCs Module 4 Session 1: Extension Material
• Simplified explanation of the CBT model • Alternative explanation of CBT model: ABCs Module 4 Session 1: Extension Material
 • Work in groups of 3 • One person plays the client, one the practitioner and one the observer • Use the celebrity’s Psy. Check Screen and other information you have gathered to inform this session • Together develop a formulation for your celebrity and the practitioner then explains it to the client; integrate any other psychoeducation material that the client would benefit from • Group discussion Module 4 Exercise 16: Please Explain…
• Work in groups of 3 • One person plays the client, one the practitioner and one the observer • Use the celebrity’s Psy. Check Screen and other information you have gathered to inform this session • Together develop a formulation for your celebrity and the practitioner then explains it to the client; integrate any other psychoeducation material that the client would benefit from • Group discussion Module 4 Exercise 16: Please Explain…
 Module 4 Session 2 Identifying Unhelpful Thoughts
Module 4 Session 2 Identifying Unhelpful Thoughts
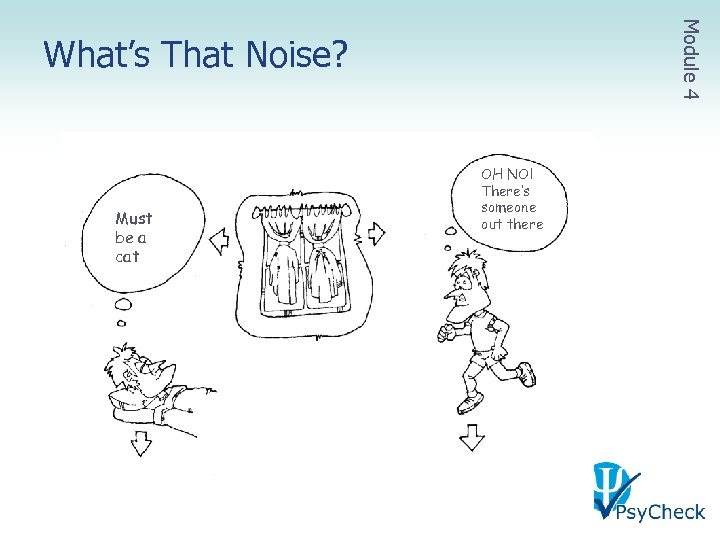 Module 4 What’s That Noise? Must be a cat OH NO! There’s someone out there
Module 4 What’s That Noise? Must be a cat OH NO! There’s someone out there
 • • Use the Unhelpful Thoughts Worksheet What are your thoughts? • • • Are you a black and white thinker? Do you jump to negative conclusions? Do you catastrophise? Are you a personaliser? Are you a should/ought person? • How do you manage these unhelpful thoughts • Group discussion Module 4 Exercise 17: Spot the Unhelpful Thought
• • Use the Unhelpful Thoughts Worksheet What are your thoughts? • • • Are you a black and white thinker? Do you jump to negative conclusions? Do you catastrophise? Are you a personaliser? Are you a should/ought person? • How do you manage these unhelpful thoughts • Group discussion Module 4 Exercise 17: Spot the Unhelpful Thought
 • Client didn’t understand the task • More explanation AND practice • Task was too difficult • Simplify • Task was too time-consuming • Do in stages or in parts • Do on some days • Readiness to change • Motivational approach Module 4 Homework Non-Completion
• Client didn’t understand the task • More explanation AND practice • Task was too difficult • Simplify • Task was too time-consuming • Do in stages or in parts • Do on some days • Readiness to change • Motivational approach Module 4 Homework Non-Completion
 • Reiterate the CBT model • Explain negative bias/interpretation • Use monitoring to identify areas of (mis)interpretation of events • Make personal link between thoughts and feelings and behaviours Module 4 Session 2: Information
• Reiterate the CBT model • Explain negative bias/interpretation • Use monitoring to identify areas of (mis)interpretation of events • Make personal link between thoughts and feelings and behaviours Module 4 Session 2: Information
 • Identify unhelpful thoughts • Use self monitoring sheets as examples • The aim is to raise awareness about when unhelpful thoughts occur • Focus is on catching thoughts as they occur rather than allowing them to create negative mood • Label unhelpful thoughts • Use Worksheet 5 Module 4 Session 2: Practice
• Identify unhelpful thoughts • Use self monitoring sheets as examples • The aim is to raise awareness about when unhelpful thoughts occur • Focus is on catching thoughts as they occur rather than allowing them to create negative mood • Label unhelpful thoughts • Use Worksheet 5 Module 4 Session 2: Practice
 • Behavioural activation • Very important especially for depression when people often withdraw and lose interest in usual activities • Focus both on pleasant activities and usual daily activities (showering, washing up) • Guidelines for better sleep • Especially important for those with anxiety and depression who often have difficulty sleeping • Relaxation • Helpful for anxiety and depression Module 4 Session 2: Extension Material
• Behavioural activation • Very important especially for depression when people often withdraw and lose interest in usual activities • Focus both on pleasant activities and usual daily activities (showering, washing up) • Guidelines for better sleep • Especially important for those with anxiety and depression who often have difficulty sleeping • Relaxation • Helpful for anxiety and depression Module 4 Session 2: Extension Material
 • Watch the video of Richard and Lynn discussing the thinking-feeling-doing cycle • In small groups, one person plays the celebrity while the others explain the thinking-feelingdoing cycle using the celebrity’s information that you have gathered previously and to identify some of their unhelpful thinking • Group discussion Module 4 Exercise 18: CBT Demonstration II
• Watch the video of Richard and Lynn discussing the thinking-feeling-doing cycle • In small groups, one person plays the celebrity while the others explain the thinking-feelingdoing cycle using the celebrity’s information that you have gathered previously and to identify some of their unhelpful thinking • Group discussion Module 4 Exercise 18: CBT Demonstration II
 Module 4 Session 3 Managing Unhelpful Thoughts
Module 4 Session 3 Managing Unhelpful Thoughts
 • How to challenge unhelpful thoughts • Go through Worksheet 6 with examples • Two main strategies for challenging thoughts: • Is this a misinterpretation? • Is there another way to think about this? • If not, is it helpful to think this way? • Even if it is true perhaps it doesn’t help me if I think this way Module 4 Session 3: Information
• How to challenge unhelpful thoughts • Go through Worksheet 6 with examples • Two main strategies for challenging thoughts: • Is this a misinterpretation? • Is there another way to think about this? • If not, is it helpful to think this way? • Even if it is true perhaps it doesn’t help me if I think this way Module 4 Session 3: Information
 • Practice challenge unhelpful thoughts • Use monitoring sheets completed for homework • Assist client to practice the process from monitoring sheet • Use Worksheet 6 as a reference Module 4 Session 3: Practice
• Practice challenge unhelpful thoughts • Use monitoring sheets completed for homework • Assist client to practice the process from monitoring sheet • Use Worksheet 6 as a reference Module 4 Session 3: Practice
 • Communication skills • Assertive communication skills are important for those who are anxious in social situations and for those who are depressed and have withdrawn from public Module 4 Session 3: Extension Material
• Communication skills • Assertive communication skills are important for those who are anxious in social situations and for those who are depressed and have withdrawn from public Module 4 Session 3: Extension Material
 • Work in groups of 3 • One person plays the client, one the practitioner and one the observer • Use the celebrity’s previous CBT model to assist • Help the celebrity identify and challenge one of their unhelpful thoughts • Use Worksheet 4 & 7 to assist you • Group discussion Module 4 Exercise 19: Celebrity Challenge
• Work in groups of 3 • One person plays the client, one the practitioner and one the observer • Use the celebrity’s previous CBT model to assist • Help the celebrity identify and challenge one of their unhelpful thoughts • Use Worksheet 4 & 7 to assist you • Group discussion Module 4 Exercise 19: Celebrity Challenge
 Module 4 Session 4 Preventing Relapse
Module 4 Session 4 Preventing Relapse
 • Discuss triggers and early warning signs • Use Worksheet 8 to explain the ‘breaking the rule effect’ • Use Worksheet 9 to emphasise looking after yourself Module 4 Session 4: Information
• Discuss triggers and early warning signs • Use Worksheet 8 to explain the ‘breaking the rule effect’ • Use Worksheet 9 to emphasise looking after yourself Module 4 Session 4: Information
 • Develop a relapse prevention plan • Explore ways the client can regulate thoughts and feelings • Emphasise the need for additional skills and supports • Remind the client to self-reward • Encourage the client to take care of themself Module 4 Session 4: Practice
• Develop a relapse prevention plan • Explore ways the client can regulate thoughts and feelings • Emphasise the need for additional skills and supports • Remind the client to self-reward • Encourage the client to take care of themself Module 4 Session 4: Practice
 • Summarise content of sessions 1 -4 and ask for feedback from the client • Reinforce gains and effort • Re-emphasise the importance of continued practice • Reminder about tasks to continue with • If continuing AOD treatment check homework in subsequent sessions • Prepare for next step • Manage concerns using a motivational approach • Consider and discuss referral options • Boosters/continued intervention Module 4 Session 4: Termination
• Summarise content of sessions 1 -4 and ask for feedback from the client • Reinforce gains and effort • Re-emphasise the importance of continued practice • Reminder about tasks to continue with • If continuing AOD treatment check homework in subsequent sessions • Prepare for next step • Manage concerns using a motivational approach • Consider and discuss referral options • Boosters/continued intervention Module 4 Session 4: Termination
 • Problem solving • Seemingly irrelevant decisions Module 4 Session 4: Extension Material
• Problem solving • Seemingly irrelevant decisions Module 4 Session 4: Extension Material
 • Work in groups of 3 • One person plays the celebrity client, one the practitioner and one the observer – swap roles from last exercise • Summarise for the client and develop a relapse prevention plan • Group discussion Module 4 Exercise 20: Celebrity Survivor
• Work in groups of 3 • One person plays the celebrity client, one the practitioner and one the observer – swap roles from last exercise • Summarise for the client and develop a relapse prevention plan • Group discussion Module 4 Exercise 20: Celebrity Survivor
 • Rescreening has benefits for both the clients and clinician: • Monitoring client progress with the client can assist to build the client’s self efficacy as they see themselves improving • Clinicians can monitor and reflect on their own practice using objective ‘data’ • Clinicians can reorient therapy if no improvement and reflect on potential gaps in treatment Module 4 Rescreening
• Rescreening has benefits for both the clients and clinician: • Monitoring client progress with the client can assist to build the client’s self efficacy as they see themselves improving • Clinicians can monitor and reflect on their own practice using objective ‘data’ • Clinicians can reorient therapy if no improvement and reflect on potential gaps in treatment Module 4 Rescreening
 • Optimal supervision: • • A single consistent supervisor to build a relationship Weekly or fortnightly supervision preferable Individual supervision as a minimum Group and/or peer supervision as an adjunct Module 4 Support: Clinical Supervision
• Optimal supervision: • • A single consistent supervisor to build a relationship Weekly or fortnightly supervision preferable Individual supervision as a minimum Group and/or peer supervision as an adjunct Module 4 Support: Clinical Supervision
 • What aspects of the training do you feel comfortable with? • What areas will you need to work on? • What will you do differently in your practice • In the next few weeks? • In the next year? Module 4 Lights… Camera… ACTION…
• What aspects of the training do you feel comfortable with? • What areas will you need to work on? • What will you do differently in your practice • In the next few weeks? • In the next year? Module 4 Lights… Camera… ACTION…


