Respiratory Tract Disorders.ppt
- Количество слайдов: 74
 Respiratory Tract Disorders Dr. OWIS khater
Respiratory Tract Disorders Dr. OWIS khater
 Congenital disorders of the nose Most newborn are obligatory nasal breathers Nasal congestion is common in the first year of life…. 1. narrow nasal airway 2. Enlarged adenoids 3. Maternal estrogenic stimuli 4. Viral or bacterial infections The nasal airway double in size in the first 6 months of life.
Congenital disorders of the nose Most newborn are obligatory nasal breathers Nasal congestion is common in the first year of life…. 1. narrow nasal airway 2. Enlarged adenoids 3. Maternal estrogenic stimuli 4. Viral or bacterial infections The nasal airway double in size in the first 6 months of life.
 Choanal Atresia. It is the most common congenital anomalies of e 00 live births lateral or bilateral. bony(90%) or membranous(10%). most cases are combination of bony and mbranous. 50 -70% with other congenital anomalies (CHARGE syndrome)
Choanal Atresia. It is the most common congenital anomalies of e 00 live births lateral or bilateral. bony(90%) or membranous(10%). most cases are combination of bony and mbranous. 50 -70% with other congenital anomalies (CHARGE syndrome)
 CHAr. Ge Syndrome oloboma…. . H=heart disease. A=atresia choanae. . R=retarded growth lies or both. G=genital anomalies or hypogonadism or . E=ear anomalies or deafness or both 10 -20%of patients with choanal atresia have the CHARGE syndrome
CHAr. Ge Syndrome oloboma…. . H=heart disease. A=atresia choanae. . R=retarded growth lies or both. G=genital anomalies or hypogonadism or . E=ear anomalies or deafness or both 10 -20%of patients with choanal atresia have the CHARGE syndrome
 Clinical signs Unilateral. . . . asymptom atic, nasal obstruction, nasal discharge. . . bilateral………. cyanosis which relieve with ng and increase with feeding Diagnosis……inability to pass a firm catheter through each nostril 3 -4 cm n CT
Clinical signs Unilateral. . . . asymptom atic, nasal obstruction, nasal discharge. . . bilateral………. cyanosis which relieve with ng and increase with feeding Diagnosis……inability to pass a firm catheter through each nostril 3 -4 cm n CT
 e for feeding Mitomycin C(prevent formation of granulatio enosis)
e for feeding Mitomycin C(prevent formation of granulatio enosis)
 Congenital midline nasal masses Dermoids (have adimple or pit at the dorsum Of the nose , sometimes with hair) s. . ) Encephaloceles (soft mass enlarge with …… va lva) Congenital nasolacrimal duct obstruction asal polyps and tumors (rare at birth)
Congenital midline nasal masses Dermoids (have adimple or pit at the dorsum Of the nose , sometimes with hair) s. . ) Encephaloceles (soft mass enlarge with …… va lva) Congenital nasolacrimal duct obstruction asal polyps and tumors (rare at birth)
 Nasal foreign body Unilateral obstruction, history of insertion of foreign body, mucopurulent nasal dischrge, foul nasal ng known as bromhidrosis Complications…. 1. infection. 2. septal perforation. . 3. tetanus. . 4. toxic shock syndrome
Nasal foreign body Unilateral obstruction, history of insertion of foreign body, mucopurulent nasal dischrge, foul nasal ng known as bromhidrosis Complications…. 1. infection. 2. septal perforation. . 3. tetanus. . 4. toxic shock syndrome
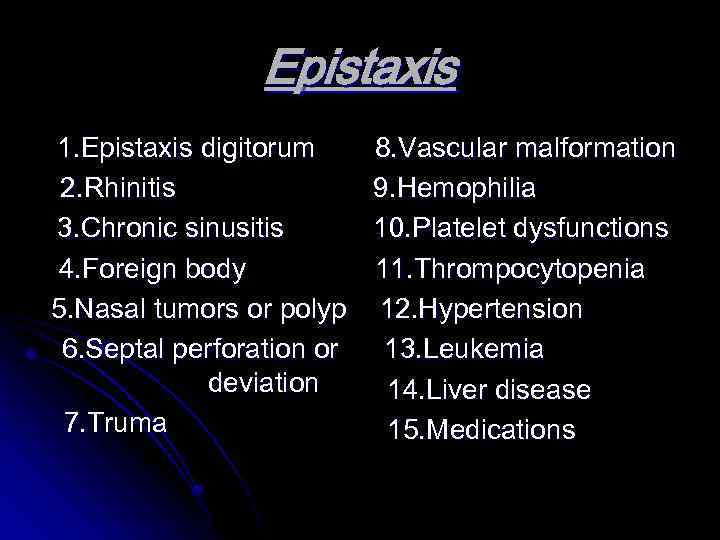 Epistaxis 1. Epistaxis digitorum 2. Rhinitis 3. Chronic sinusitis 4. Foreign body 5. Nasal tumors or polyp 6. Septal perforation or deviation 7. Truma 8. Vascular malformation 9. Hemophilia 10. Platelet dysfunctions 11. Thrompocytopenia 12. Hypertension 13. Leukemia 14. Liver disease 15. Medications
Epistaxis 1. Epistaxis digitorum 2. Rhinitis 3. Chronic sinusitis 4. Foreign body 5. Nasal tumors or polyp 6. Septal perforation or deviation 7. Truma 8. Vascular malformation 9. Hemophilia 10. Platelet dysfunctions 11. Thrompocytopenia 12. Hypertension 13. Leukemia 14. Liver disease 15. Medications
 Profuse unilateral epistaxis with nasal mass in adolescent boy. . Think of Juvenile nasal angiofibroma
Profuse unilateral epistaxis with nasal mass in adolescent boy. . Think of Juvenile nasal angiofibroma
 sa ) Nasal polyps Benign pedunculated tumor (chronically inflamed nasal . cystic fibrosis is the most common childhood cause of nasal polyposis(30%). chronic sinusitis and allergic rhinitis. Samter triad …nasal polyps , aspirin sensitivity and asthma. . hyponasal speech and mouth breathing. rhinoscopy and CTscan of the midface. Nasal steroid …surgical removal(complete nasal obstruction , uncontrolled rhinorrhea and nose deformity.
sa ) Nasal polyps Benign pedunculated tumor (chronically inflamed nasal . cystic fibrosis is the most common childhood cause of nasal polyposis(30%). chronic sinusitis and allergic rhinitis. Samter triad …nasal polyps , aspirin sensitivity and asthma. . hyponasal speech and mouth breathing. rhinoscopy and CTscan of the midface. Nasal steroid …surgical removal(complete nasal obstruction , uncontrolled rhinorrhea and nose deformity.
 Common cold Rhinosinusitis . most common cause are rhinoviruses have an average of 6 -8 colds per year of children have at least 12 infections per year. infections with rhinoviruses and adenoviruses result in the development of serotype specific protective immunity. . but infections with parainfluenza viruses and SV does not developing protective immunity. influenza is responsible for only a small proportions of all
Common cold Rhinosinusitis . most common cause are rhinoviruses have an average of 6 -8 colds per year of children have at least 12 infections per year. infections with rhinoviruses and adenoviruses result in the development of serotype specific protective immunity. . but infections with parainfluenza viruses and SV does not developing protective immunity. influenza is responsible for only a small proportions of all
 . Influenza viruses , RSV and adenoviruses are more likely to be associated with fever and other constitutional mptoms than rhinoviruses or coronaviruses . change in the color or consistency of the secretion does ate sinusitis or bacterial superinfection. polymorphonucler leukocytes in nasal secretion is characteristic of uncomplicated cold and dose not cterial superinfection
. Influenza viruses , RSV and adenoviruses are more likely to be associated with fever and other constitutional mptoms than rhinoviruses or coronaviruses . change in the color or consistency of the secretion does ate sinusitis or bacterial superinfection. polymorphonucler leukocytes in nasal secretion is characteristic of uncomplicated cold and dose not cterial superinfection
 c in common cold treatment Aspirin should not be used in children with respiratory infections because the risk of Reye syndrome Complications of common cold……. 1. Otitis media (the most common) 2. Sinusitis (facial pain and swelling ) 3. Exacerbation of asthma
c in common cold treatment Aspirin should not be used in children with respiratory infections because the risk of Reye syndrome Complications of common cold……. 1. Otitis media (the most common) 2. Sinusitis (facial pain and swelling ) 3. Exacerbation of asthma
 Sinusitis Both ethmoidal and maxillary sinuses are present at birth. only the ethmoidal sinuses are pneumatized at. maxillary sinuses are pneumatized at age of 4 t by age of 5 years. frontal sinuses begin development at age 7 -8 year and completely developed at adolescence
Sinusitis Both ethmoidal and maxillary sinuses are present at birth. only the ethmoidal sinuses are pneumatized at. maxillary sinuses are pneumatized at age of 4 t by age of 5 years. frontal sinuses begin development at age 7 -8 year and completely developed at adolescence
 sitis ……. . streptococcus pneumoniae 30%. nontypable Haemophilus influenzae 20% arrhalis 20%
sitis ……. . streptococcus pneumoniae 30%. nontypable Haemophilus influenzae 20% arrhalis 20%
 . acute bacterial sinusitis can occur at any age. predisposing factors ……………. . 1. Viral URTI 2. allergic rhinitis Cigarette smoke exposure 4. Immune deficiencies 5. cystic fibrosis. Ciliary dysfunctions 7. GERD Cleft palate 9. nasal polyps 10. Foreign body 11. immunosuppression
. acute bacterial sinusitis can occur at any age. predisposing factors ……………. . 1. Viral URTI 2. allergic rhinitis Cigarette smoke exposure 4. Immune deficiencies 5. cystic fibrosis. Ciliary dysfunctions 7. GERD Cleft palate 9. nasal polyps 10. Foreign body 11. immunosuppression
 Symptoms . nasal congestion. purulent nasal discharge ever. cough. halitosis. hyposmia. periorbital edema. Headache. facial pain. maxillary tooth discomfort increase with ation (opaque)
Symptoms . nasal congestion. purulent nasal discharge ever. cough. halitosis. hyposmia. periorbital edema. Headache. facial pain. maxillary tooth discomfort increase with ation (opaque)
 Diagnosis History …. . . persistent symptoms of URTI for more than 10 -14 days without improvement. chronic sinusitis have history of persistent respiratory symptoms for more than 3 months ate for culture doscopy
Diagnosis History …. . . persistent symptoms of URTI for more than 10 -14 days without improvement. chronic sinusitis have history of persistent respiratory symptoms for more than 3 months ate for culture doscopy
 Treatment 50 -60%of cases recover without antimicrobial . amoxicillin. Amoxi –clav. azithromycin. Clarithromycin. trimethoprim-sulfamethoxazole evofloxacin. ceftriaxone. for 7 days after resolution of symptoms. . antihistamines , decongestant and mucolytics are
Treatment 50 -60%of cases recover without antimicrobial . amoxicillin. Amoxi –clav. azithromycin. Clarithromycin. trimethoprim-sulfamethoxazole evofloxacin. ceftriaxone. for 7 days after resolution of symptoms. . antihistamines , decongestant and mucolytics are
 Complications of sinusitis 1. Orbital complications …………. . . periorbital and orbital cellulitis 2. Intracranial complications ………………. . . epidural abscess. meningitis. brain abscess. subdural empyema. cavernous sinus thrombosis. Pott puffy tumor (osteomyelitis of the frontal bone). Mucocele in the frontal sinuses
Complications of sinusitis 1. Orbital complications …………. . . periorbital and orbital cellulitis 2. Intracranial complications ………………. . . epidural abscess. meningitis. brain abscess. subdural empyema. cavernous sinus thrombosis. Pott puffy tumor (osteomyelitis of the frontal bone). Mucocele in the frontal sinuses
 Acute Pharyngitis Most common cause is viral (adenoviruses, rhinoviruses and RSV). Streptococcus pharyngitis is uncommon before 2 -3 year of age (GABHS). GABHS leads to Scarlet fever which due to exotoxins . viral cause associated with conjunctivitis , coryza hoarseness and cough. . Herpangina caused by coxsackievirus and lead to ulcer in ononucleosis mononucleosis caused by EBV
Acute Pharyngitis Most common cause is viral (adenoviruses, rhinoviruses and RSV). Streptococcus pharyngitis is uncommon before 2 -3 year of age (GABHS). GABHS leads to Scarlet fever which due to exotoxins . viral cause associated with conjunctivitis , coryza hoarseness and cough. . Herpangina caused by coxsackievirus and lead to ulcer in ononucleosis mononucleosis caused by EBV
 Lemierre syndrome. it is a serious complication of Fusobacterium necrophorum pharyngitis >>>septic thrombophlebitis of the internal jugular veins with septic pulmonary embolism which lead to hypoxia and pulmonary infiltration with plural
Lemierre syndrome. it is a serious complication of Fusobacterium necrophorum pharyngitis >>>septic thrombophlebitis of the internal jugular veins with septic pulmonary embolism which lead to hypoxia and pulmonary infiltration with plural
 e benefit of treatment to prevent rheumatic fever Treatment …. . benzathine-procaine penicillin. erythromycin , azithromycin , clarithromycin or Prolonged pharyngitis more than 1 -2 weeks recurrent fever syndrome. tonsillectomy (> 7 episodes in the last year or more than 5 episodes in the preceding 2 years)
e benefit of treatment to prevent rheumatic fever Treatment …. . benzathine-procaine penicillin. erythromycin , azithromycin , clarithromycin or Prolonged pharyngitis more than 1 -2 weeks recurrent fever syndrome. tonsillectomy (> 7 episodes in the last year or more than 5 episodes in the preceding 2 years)
 Complications ear infections rapharyngeal abscess e rheumatic fever 4. Poststreptococcus glomerulonephritis
Complications ear infections rapharyngeal abscess e rheumatic fever 4. Poststreptococcus glomerulonephritis
 Retropharyngeal Abscess most common before 3 -4 year of age n in male Less common after 5 year of age (involution of retropharyngeal nodes ). differential diagnosis …. acute epiglottitis , foreign body aspiration , meningitis , lymphoma , hematoma and yelitis Lateral soft tissue neck x-ray and CT with contrast treatment 3 rd generation cephalosporin and ampicillin or clindamycin…. . repiratory distress >>>drainage
Retropharyngeal Abscess most common before 3 -4 year of age n in male Less common after 5 year of age (involution of retropharyngeal nodes ). differential diagnosis …. acute epiglottitis , foreign body aspiration , meningitis , lymphoma , hematoma and yelitis Lateral soft tissue neck x-ray and CT with contrast treatment 3 rd generation cephalosporin and ampicillin or clindamycin…. . repiratory distress >>>drainage
 Indications for tonsillectomy 1. Recurrent pharyngitis (7 episodes in the past year , 5 in each of the last 2 years or 3 the past 3 years. Marked 2. Marked adeno-tonsillar hypertrophy ors ea nea. it dose not help with preventing acute or chronic sinusitis or otitis media
Indications for tonsillectomy 1. Recurrent pharyngitis (7 episodes in the past year , 5 in each of the last 2 years or 3 the past 3 years. Marked 2. Marked adeno-tonsillar hypertrophy ors ea nea. it dose not help with preventing acute or chronic sinusitis or otitis media
 Indications for adenoidectomy 1. Persistent mouth breathing 2. Repeated or chronic otitis media 3. Hyponasal speech 4. Adenoid facies 5. Recurrent nasopharyngitis. do not perform tonsillectomy for these above problems
Indications for adenoidectomy 1. Persistent mouth breathing 2. Repeated or chronic otitis media 3. Hyponasal speech 4. Adenoid facies 5. Recurrent nasopharyngitis. do not perform tonsillectomy for these above problems
 Adenotonsillectomy bstruction ep disorders e to thrive. craniofacial abnormalities. speech abnormalities lmonale ulmonale
Adenotonsillectomy bstruction ep disorders e to thrive. craniofacial abnormalities. speech abnormalities lmonale ulmonale
 Croup Cricoid cartilage just below the vocal cord and defines the narrowest portion of the upper airway in children < 10 year of age. stridor (high pitched respiratory sound , which is usually inspiratory but can be biphasic and is produced by turbulent air flow , it is a sign of upper airway obstruction. laryngeotracheobronchitis or recurrent (spasmodic) croup.
Croup Cricoid cartilage just below the vocal cord and defines the narrowest portion of the upper airway in children < 10 year of age. stridor (high pitched respiratory sound , which is usually inspiratory but can be biphasic and is produced by turbulent air flow , it is a sign of upper airway obstruction. laryngeotracheobronchitis or recurrent (spasmodic) croup.
 Croup a viruses 75% viruses, RSV and measles nth -5 year of age (2 year of age ) n boys. 15% with positive family history of croup. barking cough , hoarseness and inspiratory stridor (more vated by agitation and crying) ent looks not seriously ill. . croup is a disease of upper airway and the alveolar gas normal
Croup a viruses 75% viruses, RSV and measles nth -5 year of age (2 year of age ) n boys. 15% with positive family history of croup. barking cough , hoarseness and inspiratory stridor (more vated by agitation and crying) ent looks not seriously ill. . croup is a disease of upper airway and the alveolar gas normal
 . neck x-ray …show subglottic narrowing sign). steeple sign may be absent in patient with croup and may be present in normal child. . the radiographic signs does not correlate everity
. neck x-ray …show subglottic narrowing sign). steeple sign may be absent in patient with croup and may be present in normal child. . the radiographic signs does not correlate everity
 Differential diagnosis of upper airway obstruction epiglotitis smodic croup cterial tracheitis thric croup sles croup eign body 8. Retropharyngeal or peritonsillar abscess 9. Extrensic compression 10. Intraluminal obstruction Angioedema 12. Post intubation 13. Hypocalcemic tetany 14. Vocal cord dysfunction
Differential diagnosis of upper airway obstruction epiglotitis smodic croup cterial tracheitis thric croup sles croup eign body 8. Retropharyngeal or peritonsillar abscess 9. Extrensic compression 10. Intraluminal obstruction Angioedema 12. Post intubation 13. Hypocalcemic tetany 14. Vocal cord dysfunction
 Acute Epiglottitis e is H. influenzae type b dition. high fever , sore throat , dyspnia and progressing repiratory obstruction arance Tripoid position =sitting upright and leaning forward with the chin up and mouth open with drooling of saliva and hyperextended neck. stridor is a late sign and suggest near complete airway obstruction while barking cough is rare. keep the patient calm and do not try mouth examination ur cur with acute airway obstruction >>>>thumb sign. generally patient with acute epiglottitis is intubated for 2 -3 days
Acute Epiglottitis e is H. influenzae type b dition. high fever , sore throat , dyspnia and progressing repiratory obstruction arance Tripoid position =sitting upright and leaning forward with the chin up and mouth open with drooling of saliva and hyperextended neck. stridor is a late sign and suggest near complete airway obstruction while barking cough is rare. keep the patient calm and do not try mouth examination ur cur with acute airway obstruction >>>>thumb sign. generally patient with acute epiglottitis is intubated for 2 -3 days
 Spasmodic croup. in children 1 -3 year of age. no history of fever or family history. the cause is viral in same cases but allergic or psychological factors may be important in others. more at evening or night time. barking metallic cough with noisy breathing
Spasmodic croup. in children 1 -3 year of age. no history of fever or family history. the cause is viral in same cases but allergic or psychological factors may be important in others. more at evening or night time. barking metallic cough with noisy breathing
 Treatment for child with croup. airway management and treatment of hypoxia. keep the patient quite. . racemic epinephrine nebulizer (stridor at rest , possible need for intubation and hypoxia ) Oral or intramuscular steroids (dexamethasone 0. 6 mg /kg). antibiotics are not indicated for viral croup
Treatment for child with croup. airway management and treatment of hypoxia. keep the patient quite. . racemic epinephrine nebulizer (stridor at rest , possible need for intubation and hypoxia ) Oral or intramuscular steroids (dexamethasone 0. 6 mg /kg). antibiotics are not indicated for viral croup
 Indications of admission in patient with croup 1. Progressive stridor 2. Sever stridor at rest 3. Respiratory distress 4. Hypoxia 5. Cyanosis 6. Depressed mental status 7. Poor oral intake 8. The need for reliable observation
Indications of admission in patient with croup 1. Progressive stridor 2. Sever stridor at rest 3. Respiratory distress 4. Hypoxia 5. Cyanosis 6. Depressed mental status 7. Poor oral intake 8. The need for reliable observation
 Treatment of acute epiglottitis Treat the patient in ICU or theater. artificial airway for all patient. oxygen. blood culture and CSF culture. ceftriaxon, cefotaxime or meropenum(7 -10 days). chemoprophylaxis for household member(rifampin 20 mg/kg once daily for 4 days). racemic epinephrine with dexamethasone 0. 5 mg/kg q 6 hours may used in treatment of croup associated with extubation
Treatment of acute epiglottitis Treat the patient in ICU or theater. artificial airway for all patient. oxygen. blood culture and CSF culture. ceftriaxon, cefotaxime or meropenum(7 -10 days). chemoprophylaxis for household member(rifampin 20 mg/kg once daily for 4 days). racemic epinephrine with dexamethasone 0. 5 mg/kg q 6 hours may used in treatment of croup associated with extubation
 Bacterial tracheitis. life threatening. Staph aureus (the most common). Maroxella catarrhalis , anaerobes, nontypable H. influenzae. 5 -7 year of age. M=F. High fever, toxic , respiratory distress, no drooling and no dysphagia. Pseudomembrane. Consider intubation and antibiotics(vancomycin). Complicated by toxic shock syndrome. Chest show bilateral infiltrations
Bacterial tracheitis. life threatening. Staph aureus (the most common). Maroxella catarrhalis , anaerobes, nontypable H. influenzae. 5 -7 year of age. M=F. High fever, toxic , respiratory distress, no drooling and no dysphagia. Pseudomembrane. Consider intubation and antibiotics(vancomycin). Complicated by toxic shock syndrome. Chest show bilateral infiltrations
 Laryngomalacia It is the most common cause of stridor in infant and children. Appear within the first 2 weeks of life. Increase in severity up to 6 months Associated with laryngopharyngeal reflux Confirmed by laryngoscopy. . Observe and most cases are improve. Surgical correction indicated in( apparent life threatening event , cor pulmonale , cyanosis, failure to thrive )
Laryngomalacia It is the most common cause of stridor in infant and children. Appear within the first 2 weeks of life. Increase in severity up to 6 months Associated with laryngopharyngeal reflux Confirmed by laryngoscopy. . Observe and most cases are improve. Surgical correction indicated in( apparent life threatening event , cor pulmonale , cyanosis, failure to thrive )
 Congenital subglottic stenosis is the 2 nd most common cause of stridor in infants and children. Vocal cord paralysis is the 3 rd most common congenital cause of stridor in infants and children (associated with neurological and cardiac anomalies >>diagnosed by awake flexible laryngoscopy >>usually resolves spontaneously )
Congenital subglottic stenosis is the 2 nd most common cause of stridor in infants and children. Vocal cord paralysis is the 3 rd most common congenital cause of stridor in infants and children (associated with neurological and cardiac anomalies >>diagnosed by awake flexible laryngoscopy >>usually resolves spontaneously )
 Foreign bodies of the airway Common in children<3 year of age. nuts, apple , popcorn, watermelon seeds, small toys. three stages … 1. initial event(coughing, chocking, gagging) 2. Asymptomatic interval 3. complications(obstruction, erosions, infe). history is the most important factor in determining the need for broncoscopy
Foreign bodies of the airway Common in children<3 year of age. nuts, apple , popcorn, watermelon seeds, small toys. three stages … 1. initial event(coughing, chocking, gagging) 2. Asymptomatic interval 3. complications(obstruction, erosions, infe). history is the most important factor in determining the need for broncoscopy
 Laryngeal foreign body>Heimlich Maneuver. bronchial foreign body>>obstructive emphysema >>air trapping >shift of mediastinum>>atelactesis(late sign)…more in the right side (60%)
Laryngeal foreign body>Heimlich Maneuver. bronchial foreign body>>obstructive emphysema >>air trapping >shift of mediastinum>>atelactesis(late sign)…more in the right side (60%)
 Bronchomalacia and tracheomalacia Insufficient cartilage to maintain airway patency. It is common cause of persistent wheezing in infancy. primary or 2 ry (external compression. . vascular ring ). may associated with laryngomalacia (laryngotrachobronchomalacia). bronchdilators can worsen a case of bronchomalacia or tracheomalacia(ipratrpoium may help)
Bronchomalacia and tracheomalacia Insufficient cartilage to maintain airway patency. It is common cause of persistent wheezing in infancy. primary or 2 ry (external compression. . vascular ring ). may associated with laryngomalacia (laryngotrachobronchomalacia). bronchdilators can worsen a case of bronchomalacia or tracheomalacia(ipratrpoium may help)
 Bronchiolitis Viral disease(RSV in >50% f cases) Other agent ( parainfluenza, adenovirus and mycoplasma) Human bocavirus and human metapneumovirus(co –infection with RSV). no evidence for bacterial cause for bronchiolitis. more common in boys. more in bottle feed infant. more in infant for young mother and smoker mother during pregnancy
Bronchiolitis Viral disease(RSV in >50% f cases) Other agent ( parainfluenza, adenovirus and mycoplasma) Human bocavirus and human metapneumovirus(co –infection with RSV). no evidence for bacterial cause for bronchiolitis. more common in boys. more in bottle feed infant. more in infant for young mother and smoker mother during pregnancy
 RSV lead to immune complex response with eosinophils release of ( eosinophil cationic proteine ) which is cytotoxic for airway epithelium. bronchiolar obstruction with edema , mucus, and cellular debris >>air trapping >>overinflation>>>with time >>atelectasis. wheezes , retraction , tachypnia and hypoxemia
RSV lead to immune complex response with eosinophils release of ( eosinophil cationic proteine ) which is cytotoxic for airway epithelium. bronchiolar obstruction with edema , mucus, and cellular debris >>air trapping >>overinflation>>>with time >>atelectasis. wheezes , retraction , tachypnia and hypoxemia
 Lack of audible wheezing with presence of other signs of respiratory distress is not reassuring (complete airway obstruction ). the patient may develop fever or hypothermia. apnea may be more prominent in very young premature infant (< 2 month old). The degree of tachypnea does not correlate with the degree of hypoxemia or hypercarbia CBC are usually normal
Lack of audible wheezing with presence of other signs of respiratory distress is not reassuring (complete airway obstruction ). the patient may develop fever or hypothermia. apnea may be more prominent in very young premature infant (< 2 month old). The degree of tachypnea does not correlate with the degree of hypoxemia or hypercarbia CBC are usually normal
 Treatment of bronchiolitis Mainly supportive. humidified oxygen (nasal cannula can reduce the need for intubation ). extended neck. feed through NGT or IVF Frequent suctioning of nasal and oral secretion. bronchodilator. corticosteroids are not recommended. No need for antibiotics. hypertonic saline nebulizer
Treatment of bronchiolitis Mainly supportive. humidified oxygen (nasal cannula can reduce the need for intubation ). extended neck. feed through NGT or IVF Frequent suctioning of nasal and oral secretion. bronchodilator. corticosteroids are not recommended. No need for antibiotics. hypertonic saline nebulizer
 Indications for admission 1. Hypoxia ( oxygen sat< 93%) 2. Inability to take oral feeding 3. Extreme tachypnea 4. Risk for sever disease. age <3 months. preterm birth. comorbidity (cardiovascular, pulmonary, immunological )
Indications for admission 1. Hypoxia ( oxygen sat< 93%) 2. Inability to take oral feeding 3. Extreme tachypnea 4. Risk for sever disease. age <3 months. preterm birth. comorbidity (cardiovascular, pulmonary, immunological )
 Ribavirin (aerosol antiviral agent ) may used in patient with 1. congenital heart disease 2. chronic lung disease 3. prematurity. RSV immunoglobulin had no rule during the acute episodes. RSV IVIG and palivizumab (monoclonal antibody to the RSV protein f) may reduce the severity and the incidence of acute bronchiolitis in these patients. mortality rate <1%(apnea , respiratory arrest , sever dehydration)
Ribavirin (aerosol antiviral agent ) may used in patient with 1. congenital heart disease 2. chronic lung disease 3. prematurity. RSV immunoglobulin had no rule during the acute episodes. RSV IVIG and palivizumab (monoclonal antibody to the RSV protein f) may reduce the severity and the incidence of acute bronchiolitis in these patients. mortality rate <1%(apnea , respiratory arrest , sever dehydration)
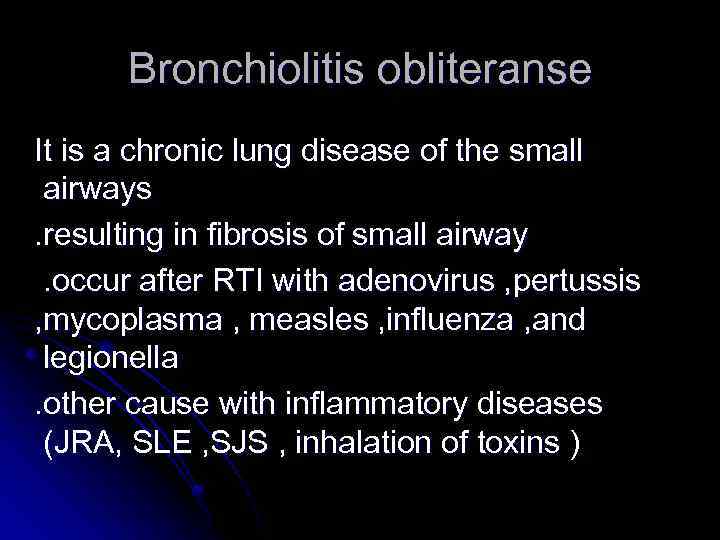 Bronchiolitis obliteranse It is a chronic lung disease of the small airways. resulting in fibrosis of small airway. occur after RTI with adenovirus , pertussis , mycoplasma , measles , influenza , and legionella. other cause with inflammatory diseases (JRA, SLE , SJS , inhalation of toxins )
Bronchiolitis obliteranse It is a chronic lung disease of the small airways. resulting in fibrosis of small airway. occur after RTI with adenovirus , pertussis , mycoplasma , measles , influenza , and legionella. other cause with inflammatory diseases (JRA, SLE , SJS , inhalation of toxins )
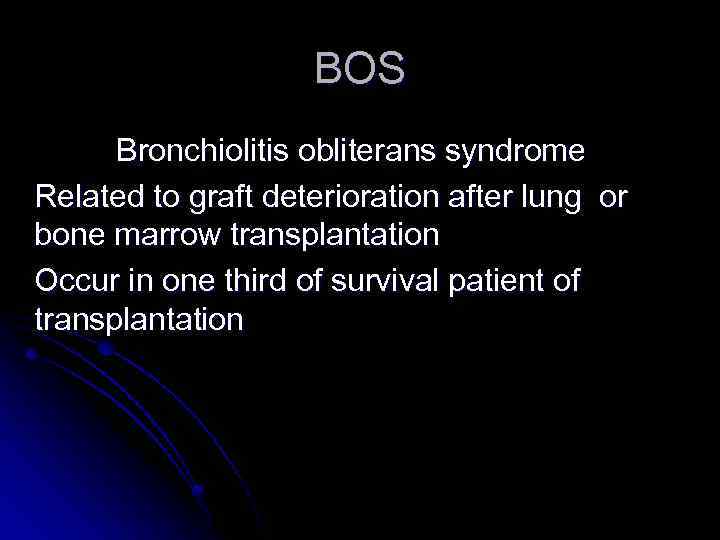 BOS Bronchiolitis obliterans syndrome Related to graft deterioration after lung or bone marrow transplantation Occur in one third of survival patient of transplantation
BOS Bronchiolitis obliterans syndrome Related to graft deterioration after lung or bone marrow transplantation Occur in one third of survival patient of transplantation
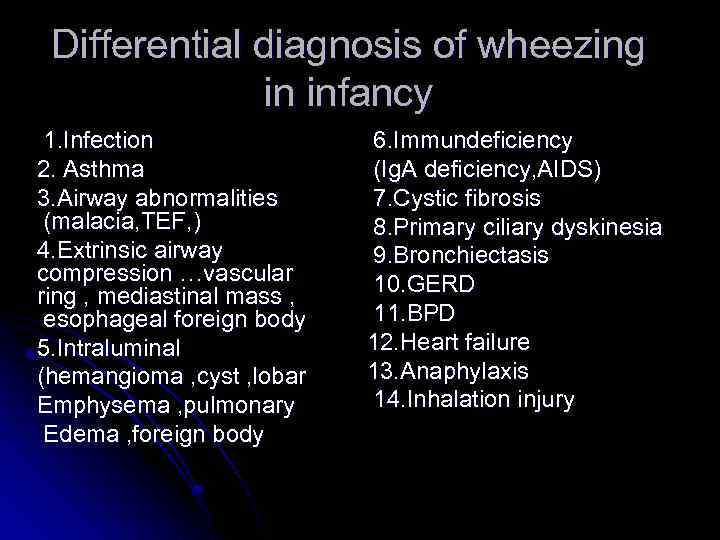 Differential diagnosis of wheezing in infancy 1. Infection 2. Asthma 3. Airway abnormalities (malacia, TEF, ) 4. Extrinsic airway compression …vascular ring , mediastinal mass , esophageal foreign body 5. Intraluminal (hemangioma , cyst , lobar Emphysema , pulmonary Edema , foreign body 6. Immundeficiency (Ig. A deficiency, AIDS) 7. Cystic fibrosis 8. Primary ciliary dyskinesia 9. Bronchiectasis 10. GERD 11. BPD 12. Heart failure 13. Anaphylaxis 14. Inhalation injury
Differential diagnosis of wheezing in infancy 1. Infection 2. Asthma 3. Airway abnormalities (malacia, TEF, ) 4. Extrinsic airway compression …vascular ring , mediastinal mass , esophageal foreign body 5. Intraluminal (hemangioma , cyst , lobar Emphysema , pulmonary Edema , foreign body 6. Immundeficiency (Ig. A deficiency, AIDS) 7. Cystic fibrosis 8. Primary ciliary dyskinesia 9. Bronchiectasis 10. GERD 11. BPD 12. Heart failure 13. Anaphylaxis 14. Inhalation injury
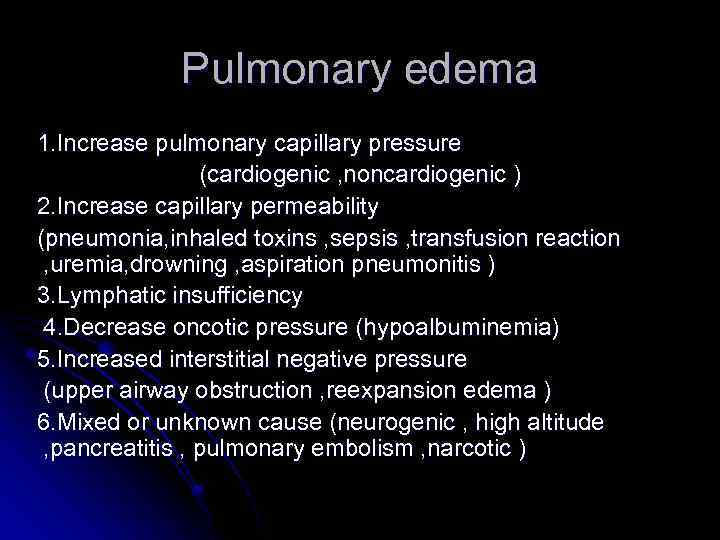 Pulmonary edema 1. Increase pulmonary capillary pressure (cardiogenic , noncardiogenic ) 2. Increase capillary permeability (pneumonia, inhaled toxins , sepsis , transfusion reaction , uremia, drowning , aspiration pneumonitis ) 3. Lymphatic insufficiency 4. Decrease oncotic pressure (hypoalbuminemia) 5. Increased interstitial negative pressure (upper airway obstruction , reexpansion edema ) 6. Mixed or unknown cause (neurogenic , high altitude , pancreatitis , pulmonary embolism , narcotic )
Pulmonary edema 1. Increase pulmonary capillary pressure (cardiogenic , noncardiogenic ) 2. Increase capillary permeability (pneumonia, inhaled toxins , sepsis , transfusion reaction , uremia, drowning , aspiration pneumonitis ) 3. Lymphatic insufficiency 4. Decrease oncotic pressure (hypoalbuminemia) 5. Increased interstitial negative pressure (upper airway obstruction , reexpansion edema ) 6. Mixed or unknown cause (neurogenic , high altitude , pancreatitis , pulmonary embolism , narcotic )
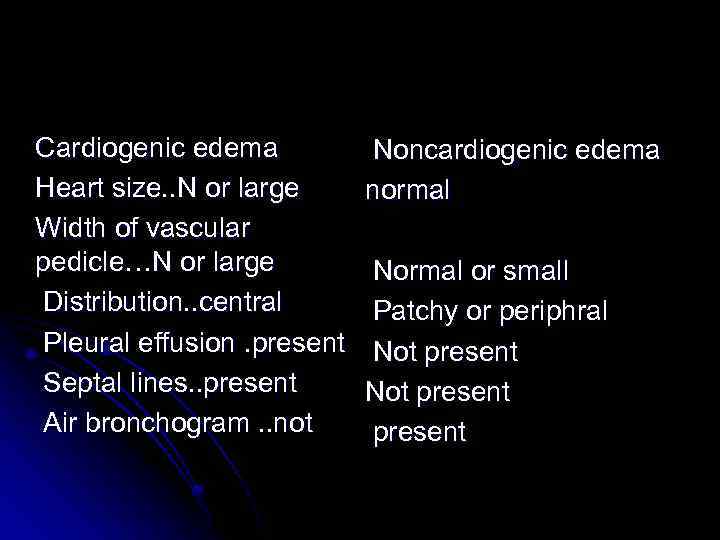 Cardiogenic edema Heart size. . N or large Width of vascular pedicle…N or large Distribution. . central Pleural effusion. present Septal lines. . present Air bronchogram. . not Noncardiogenic edema normal Normal or small Patchy or periphral Not present
Cardiogenic edema Heart size. . N or large Width of vascular pedicle…N or large Distribution. . central Pleural effusion. present Septal lines. . present Air bronchogram. . not Noncardiogenic edema normal Normal or small Patchy or periphral Not present
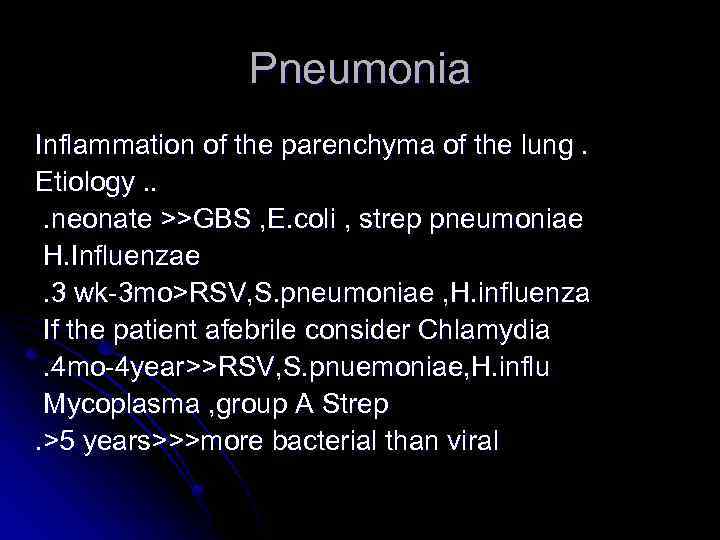 Pneumonia Inflammation of the parenchyma of the lung. Etiology. . . neonate >>GBS , E. coli , strep pneumoniae H. Influenzae. 3 wk-3 mo>RSV, S. pneumoniae , H. influenza If the patient afebrile consider Chlamydia. 4 mo-4 year>>RSV, S. pnuemoniae, H. influ Mycoplasma , group A Strep. >5 years>>>more bacterial than viral
Pneumonia Inflammation of the parenchyma of the lung. Etiology. . . neonate >>GBS , E. coli , strep pneumoniae H. Influenzae. 3 wk-3 mo>RSV, S. pneumoniae , H. influenza If the patient afebrile consider Chlamydia. 4 mo-4 year>>RSV, S. pnuemoniae, H. influ Mycoplasma , group A Strep. >5 years>>>more bacterial than viral
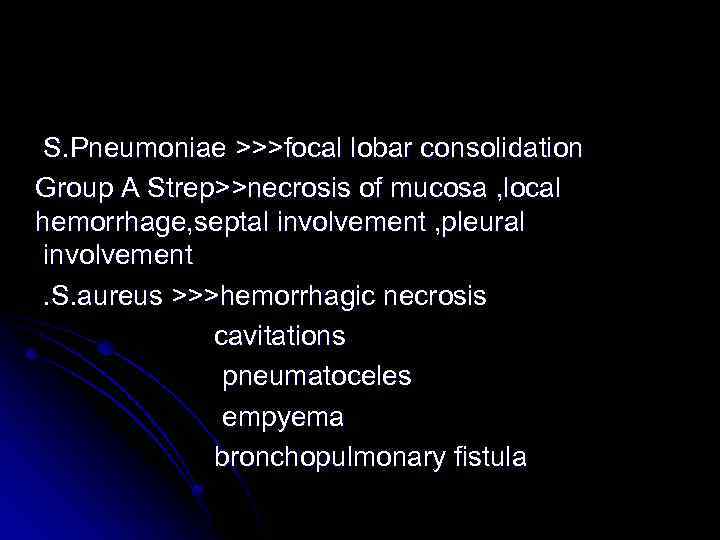 S. Pneumoniae >>>focal lobar consolidation Group A Strep>>necrosis of mucosa , local hemorrhage, septal involvement , pleural involvement. S. aureus >>>hemorrhagic necrosis cavitations pneumatoceles empyema bronchopulmonary fistula
S. Pneumoniae >>>focal lobar consolidation Group A Strep>>necrosis of mucosa , local hemorrhage, septal involvement , pleural involvement. S. aureus >>>hemorrhagic necrosis cavitations pneumatoceles empyema bronchopulmonary fistula
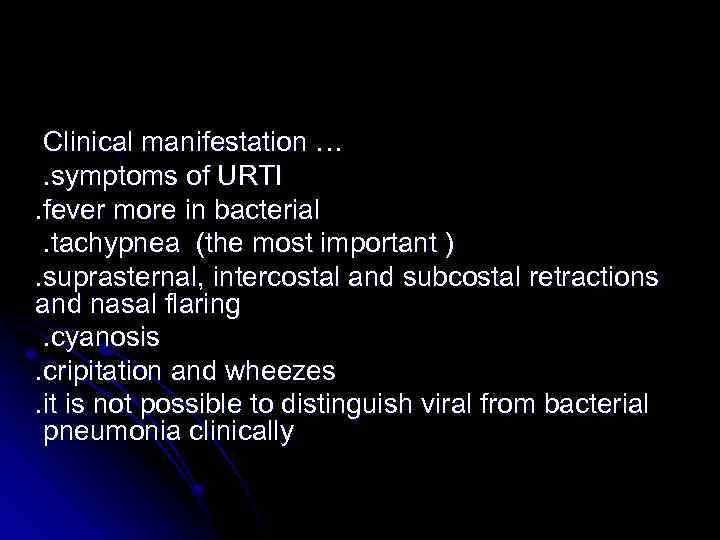 Clinical manifestation …. symptoms of URTI. fever more in bacterial. tachypnea (the most important ). suprasternal, intercostal and subcostal retractions and nasal flaring. cyanosis. cripitation and wheezes. it is not possible to distinguish viral from bacterial pneumonia clinically
Clinical manifestation …. symptoms of URTI. fever more in bacterial. tachypnea (the most important ). suprasternal, intercostal and subcostal retractions and nasal flaring. cyanosis. cripitation and wheezes. it is not possible to distinguish viral from bacterial pneumonia clinically
 Diagnosis…. History. . , examination , investigations. CXR…. viral>>hyperinflation, bilateral infiltration …. . bacterial>> lobar consolidation +-pleural effusion (the radiographic appearance alone is not diagnostic ). CBC …WBC not < 20000 in viral cause and mainly lymphocytic …WBC. . 15000 -40000 in bacterial cause and mainly granulocytes. ESR and CRP are high. blood culture results are positive only in 10% of children with pneumococcal pneumonia
Diagnosis…. History. . , examination , investigations. CXR…. viral>>hyperinflation, bilateral infiltration …. . bacterial>> lobar consolidation +-pleural effusion (the radiographic appearance alone is not diagnostic ). CBC …WBC not < 20000 in viral cause and mainly lymphocytic …WBC. . 15000 -40000 in bacterial cause and mainly granulocytes. ESR and CRP are high. blood culture results are positive only in 10% of children with pneumococcal pneumonia
 Indications for admission in pneumonia 1. Age <6 months 2. Toxic appearance 3. Moderate to sever respiratory distress 4. Requirement for supplemental oxygen 5. Dehydration 6. Vomiting and intolerance of oral treatment 7. No response for oral antibiotics 8. Immunocompromised patient 9. Multiple lobes involvement 10. Sicle cell anemia with acute chest syndrome
Indications for admission in pneumonia 1. Age <6 months 2. Toxic appearance 3. Moderate to sever respiratory distress 4. Requirement for supplemental oxygen 5. Dehydration 6. Vomiting and intolerance of oral treatment 7. No response for oral antibiotics 8. Immunocompromised patient 9. Multiple lobes involvement 10. Sicle cell anemia with acute chest syndrome
 Differential diagnosis of recurrent pneumonia (tow or more episodes in single year …or. . Three or more episodes ever with radiographic clearing between occurrence)
Differential diagnosis of recurrent pneumonia (tow or more episodes in single year …or. . Three or more episodes ever with radiographic clearing between occurrence)
 Recurrent pneumonia 1. Cystic fibrosis 2. Sickle cell disease 3. Immundeficiency 4. Immotile cilia syndrome 5. Kartagener syndrome 6. Lobar emphysema 7. Pulmonary sequestration 8. GERD 9. Foreign body 10. TEF (H type ) 11. Recurrent aspiration (oropharyngeal incoordination) 12. bronchiectasis
Recurrent pneumonia 1. Cystic fibrosis 2. Sickle cell disease 3. Immundeficiency 4. Immotile cilia syndrome 5. Kartagener syndrome 6. Lobar emphysema 7. Pulmonary sequestration 8. GERD 9. Foreign body 10. TEF (H type ) 11. Recurrent aspiration (oropharyngeal incoordination) 12. bronchiectasis
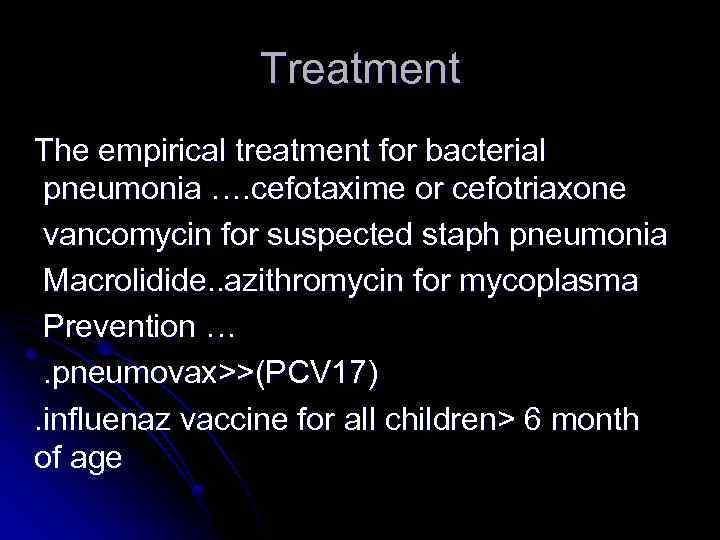 Treatment The empirical treatment for bacterial pneumonia …. cefotaxime or cefotriaxone vancomycin for suspected staph pneumonia Macrolidide. . azithromycin for mycoplasma Prevention …. pneumovax>>(PCV 17). influenaz vaccine for all children> 6 month of age
Treatment The empirical treatment for bacterial pneumonia …. cefotaxime or cefotriaxone vancomycin for suspected staph pneumonia Macrolidide. . azithromycin for mycoplasma Prevention …. pneumovax>>(PCV 17). influenaz vaccine for all children> 6 month of age
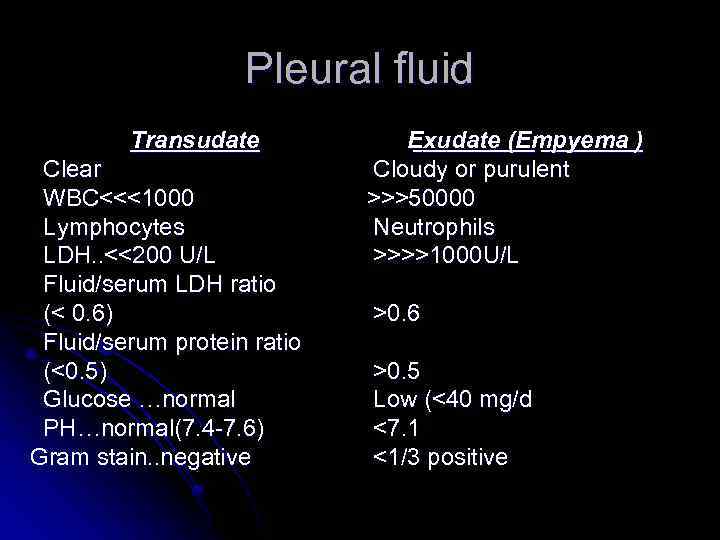 Pleural fluid Transudate Clear WBC<<<1000 Lymphocytes LDH. . <<200 U/L Fluid/serum LDH ratio (< 0. 6) Fluid/serum protein ratio (<0. 5) Glucose …normal PH…normal(7. 4 -7. 6) Gram stain. . negative Exudate (Empyema ) Cloudy or purulent >>>50000 Neutrophils >>>>1000 U/L >0. 6 >0. 5 Low (<40 mg/d <7. 1 <1/3 positive
Pleural fluid Transudate Clear WBC<<<1000 Lymphocytes LDH. . <<200 U/L Fluid/serum LDH ratio (< 0. 6) Fluid/serum protein ratio (<0. 5) Glucose …normal PH…normal(7. 4 -7. 6) Gram stain. . negative Exudate (Empyema ) Cloudy or purulent >>>50000 Neutrophils >>>>1000 U/L >0. 6 >0. 5 Low (<40 mg/d <7. 1 <1/3 positive
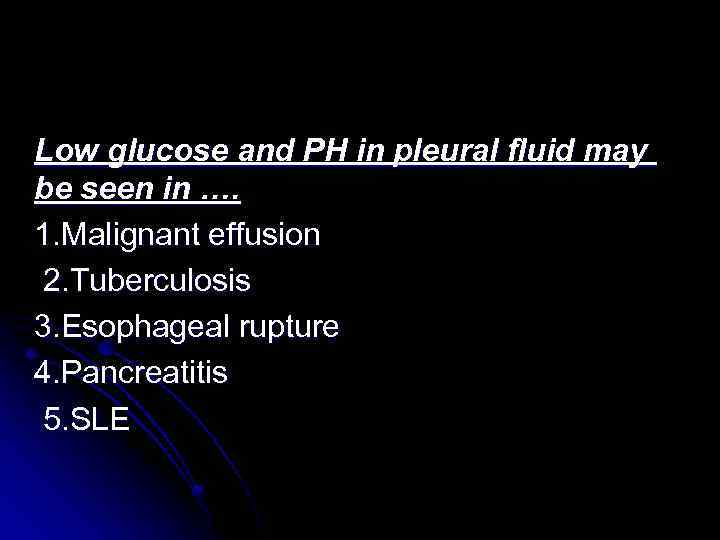 Low glucose and PH in pleural fluid may be seen in …. 1. Malignant effusion 2. Tuberculosis 3. Esophageal rupture 4. Pancreatitis 5. SLE
Low glucose and PH in pleural fluid may be seen in …. 1. Malignant effusion 2. Tuberculosis 3. Esophageal rupture 4. Pancreatitis 5. SLE
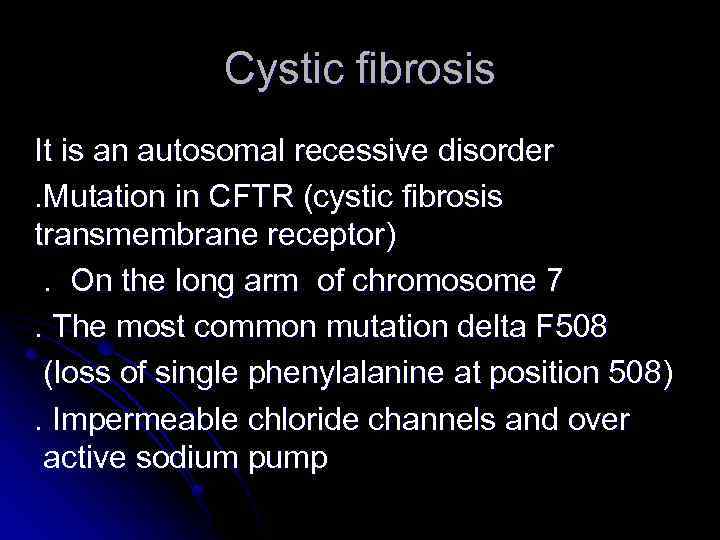 Cystic fibrosis It is an autosomal recessive disorder. Mutation in CFTR (cystic fibrosis transmembrane receptor). On the long arm of chromosome 7. The most common mutation delta F 508 (loss of single phenylalanine at position 508). Impermeable chloride channels and over active sodium pump
Cystic fibrosis It is an autosomal recessive disorder. Mutation in CFTR (cystic fibrosis transmembrane receptor). On the long arm of chromosome 7. The most common mutation delta F 508 (loss of single phenylalanine at position 508). Impermeable chloride channels and over active sodium pump
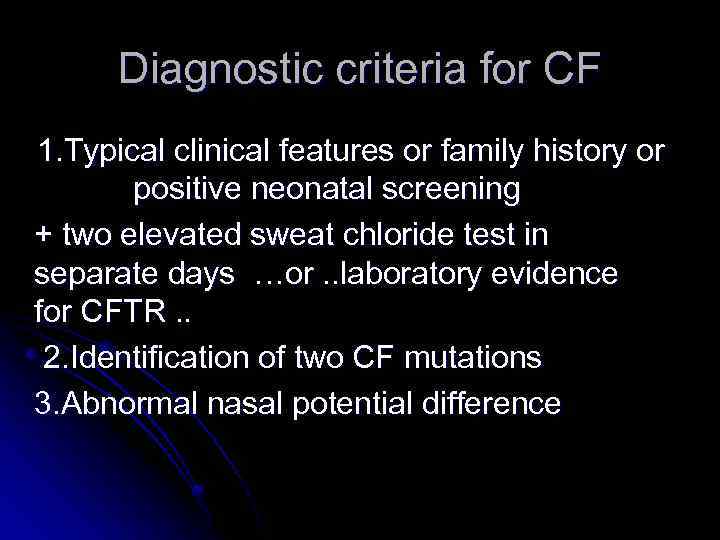 Diagnostic criteria for CF 1. Typical clinical features or family history or positive neonatal screening + two elevated sweat chloride test in separate days …or. . laboratory evidence for CFTR. . 2. Identification of two CF mutations 3. Abnormal nasal potential difference
Diagnostic criteria for CF 1. Typical clinical features or family history or positive neonatal screening + two elevated sweat chloride test in separate days …or. . laboratory evidence for CFTR. . 2. Identification of two CF mutations 3. Abnormal nasal potential difference
 Reasons to think about CF. meconium ileus. rectal prolapse. prolonged neonatal jaundice. chronic diarrhea. steatorrhea. nasal polyps. pansinusitis. chronic cough. recurrent wheezing. staph pneumonia . pseudomonas in throat. clubbing. family history. failure to thrive. salty baby. male infertility
Reasons to think about CF. meconium ileus. rectal prolapse. prolonged neonatal jaundice. chronic diarrhea. steatorrhea. nasal polyps. pansinusitis. chronic cough. recurrent wheezing. staph pneumonia . pseudomonas in throat. clubbing. family history. failure to thrive. salty baby. male infertility
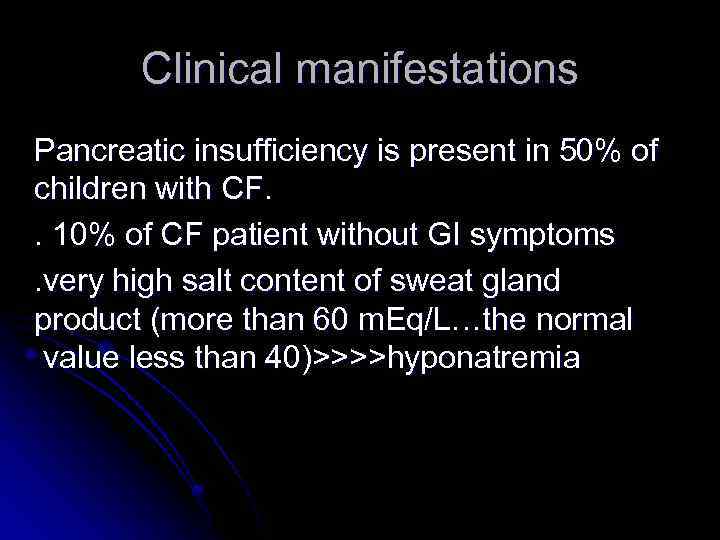 Clinical manifestations Pancreatic insufficiency is present in 50% of children with CF. . 10% of CF patient without GI symptoms. very high salt content of sweat gland product (more than 60 m. Eq/L…the normal value less than 40)>>>>hyponatremia
Clinical manifestations Pancreatic insufficiency is present in 50% of children with CF. . 10% of CF patient without GI symptoms. very high salt content of sweat gland product (more than 60 m. Eq/L…the normal value less than 40)>>>>hyponatremia
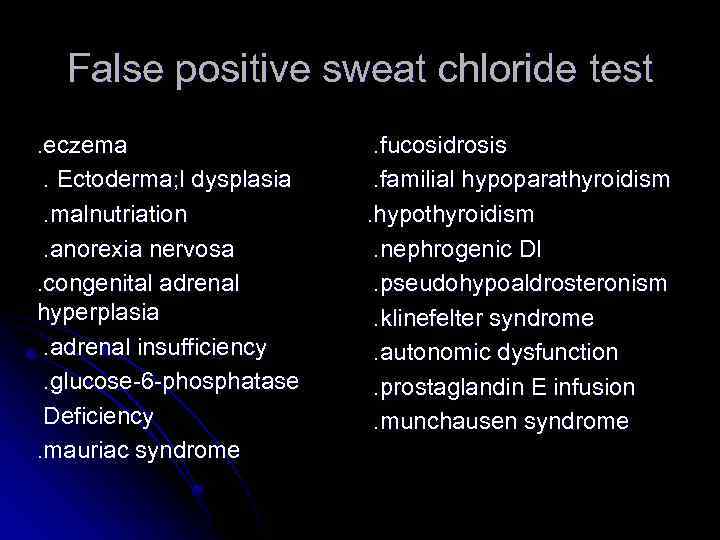 False positive sweat chloride test. eczema. Ectoderma; l dysplasia. malnutriation. anorexia nervosa. congenital adrenal hyperplasia. adrenal insufficiency. glucose-6 -phosphatase Deficiency. mauriac syndrome . fucosidrosis. familial hypoparathyroidism. hypothyroidism. nephrogenic DI. pseudohypoaldrosteronism. klinefelter syndrome. autonomic dysfunction. prostaglandin E infusion. munchausen syndrome
False positive sweat chloride test. eczema. Ectoderma; l dysplasia. malnutriation. anorexia nervosa. congenital adrenal hyperplasia. adrenal insufficiency. glucose-6 -phosphatase Deficiency. mauriac syndrome . fucosidrosis. familial hypoparathyroidism. hypothyroidism. nephrogenic DI. pseudohypoaldrosteronism. klinefelter syndrome. autonomic dysfunction. prostaglandin E infusion. munchausen syndrome
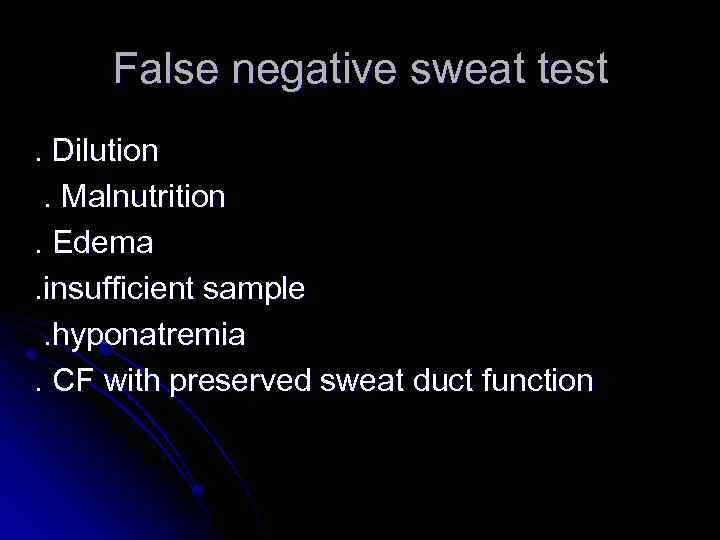 False negative sweat test. Dilution. Malnutrition. Edema. insufficient sample. hyponatremia. CF with preserved sweat duct function
False negative sweat test. Dilution. Malnutrition. Edema. insufficient sample. hyponatremia. CF with preserved sweat duct function
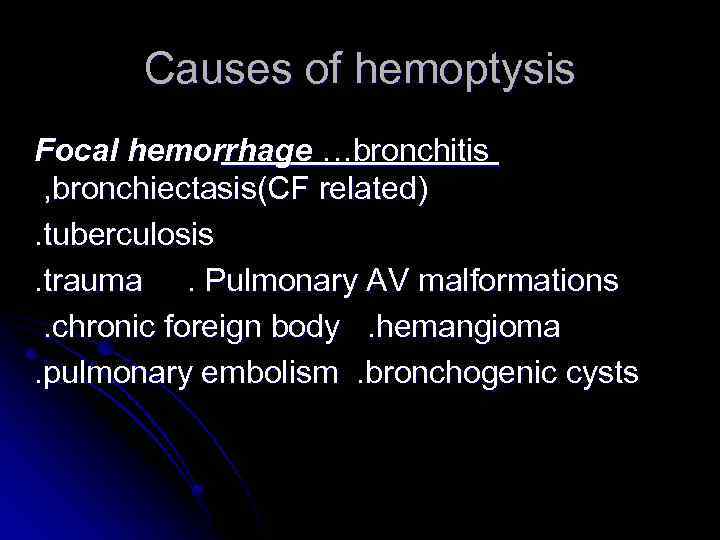 Causes of hemoptysis Focal hemorrhage …bronchitis , bronchiectasis(CF related). tuberculosis. trauma. Pulmonary AV malformations. chronic foreign body. hemangioma. pulmonary embolism. bronchogenic cysts
Causes of hemoptysis Focal hemorrhage …bronchitis , bronchiectasis(CF related). tuberculosis. trauma. Pulmonary AV malformations. chronic foreign body. hemangioma. pulmonary embolism. bronchogenic cysts
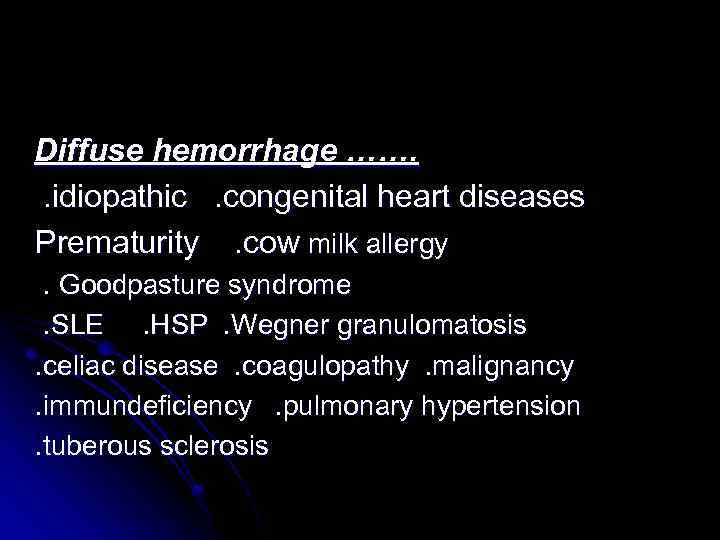 Diffuse hemorrhage ……. . idiopathic. congenital heart diseases Prematurity. cow milk allergy. Goodpasture syndrome. SLE. HSP. Wegner granulomatosis. celiac disease. coagulopathy. malignancy. immundeficiency. pulmonary hypertension. tuberous sclerosis
Diffuse hemorrhage ……. . idiopathic. congenital heart diseases Prematurity. cow milk allergy. Goodpasture syndrome. SLE. HSP. Wegner granulomatosis. celiac disease. coagulopathy. malignancy. immundeficiency. pulmonary hypertension. tuberous sclerosis
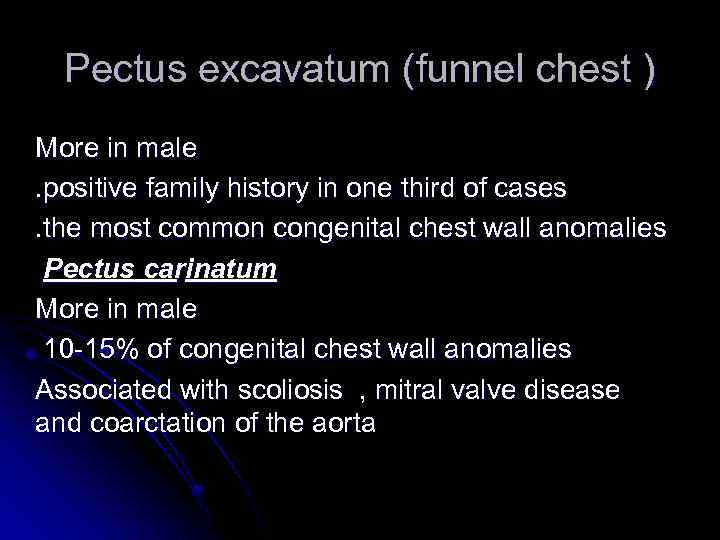 Pectus excavatum (funnel chest ) More in male. positive family history in one third of cases. the most common congenital chest wall anomalies Pectus carinatum More in male 10 -15% of congenital chest wall anomalies Associated with scoliosis , mitral valve disease and coarctation of the aorta
Pectus excavatum (funnel chest ) More in male. positive family history in one third of cases. the most common congenital chest wall anomalies Pectus carinatum More in male 10 -15% of congenital chest wall anomalies Associated with scoliosis , mitral valve disease and coarctation of the aorta


