96189c97aad3d5a36ad51e6047700c51.ppt
- Количество слайдов: 64
Respiratory System Learning Objectives: To study the pathophysiology of ; v Pneumonia v COPD By; Mrs. Deepa K. Ingawale (Mandlik) Department of Pharmacology SIPS, Lonavala
PNEUMONIA
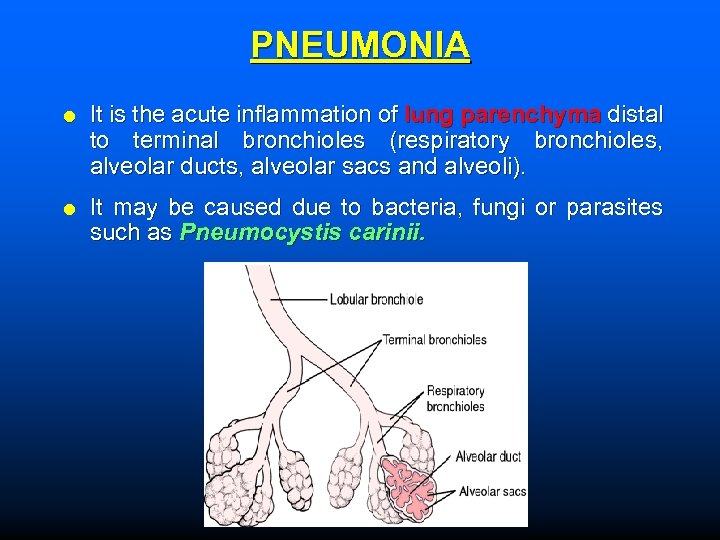
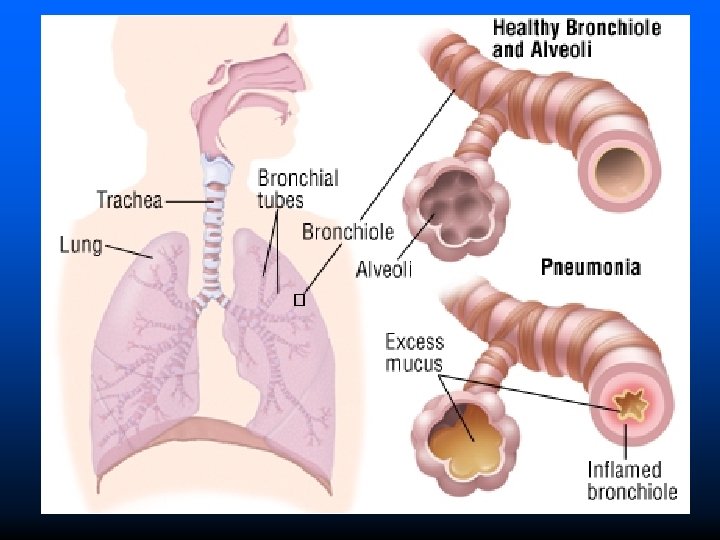
PNEUMONIA It is the acute inflammation of lung parenchyma distal to terminal bronchioles (respiratory bronchioles, alveolar ducts, alveolar sacs and alveoli). It may be caused due to bacteria, fungi or parasites such as Pneumocystis carinii.
Route of entry of microorganism The m. o. enters the lungs by any one of the four routes. Inhalation: Inhalation of microbes present in the air Aspiration: Aspiration of organism from the pharynx Hematogenous: Infection is passes from blood stream Direct spread: Entry of m. o. from adjacent site of infection.
Risk factors Problems in swallowing: People who have problems of swallowing or are bedridden can easily develop pneumonia. Age: Infants from 0 to 2 years & older people above 65 years are at high risk of pneumonia. Weakened immune system: People taking medications such as steroid anti-cancer drugs that weaken the immune system & people with HIV, AIDS, or cancer are susceptible to pneumonia. Drug abuse: Excessive alcohol consumption & smoking Certain medical conditions: Asthma, diabetes and HF raise the risks of pneumonia.

Classification Etiological classification Anatomical classification Pathological classification
Etiological Classification Bacterial pneumonia: Lobar pneumonia: It is an acute bacterial infection of a part of lobe, the entire lobe or even two lobes lungs. The causative m. o. are as follows; Pneumococcal pneumonia Staphylococcal pneumonia Streptococcal pneumonia Haemophilus influenzae Klebsiella pneumonia Escherichia coli
Etiological Classification Bronchopneumonia (Lobular pneumonia): It is an infection of terminal bronchioles that extends into surrounding alveoli results in patchy consolidation of lungs. The causative m. o. are as follows; Pneumococcal pneumonia Staphylococcal pneumonia Streptococcal pneumonia Haemophilus influenzae Klebsiella pneumonia Pseudomonas aeruginosa
Etiological Classification Viral and mycoplasmal pneumonia: It is characterised by patchy inflammatory changes of the lungs. The causative m. o. are as follows; Respiratory syncytial viruses (RSV) Mycoplasma pneumonia Influenza virus Para influenza virus Adenovirus Rhinovirus Cytomegalovirus
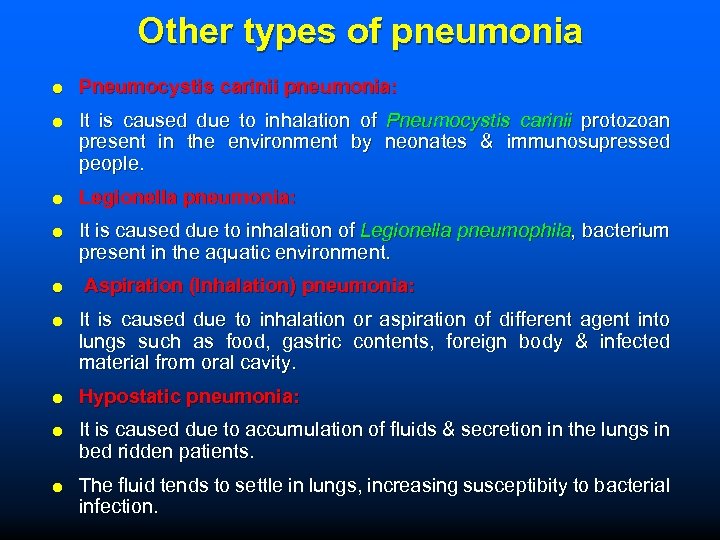
Other types of pneumonia Pneumocystis carinii pneumonia: It is caused due to inhalation of Pneumocystis carinii protozoan present in the environment by neonates & immunosupressed people. Legionella pneumonia: It is caused due to inhalation of Legionella pneumophila, bacterium present in the aquatic environment. Aspiration (Inhalation) pneumonia: It is caused due to inhalation or aspiration of different agent into lungs such as food, gastric contents, foreign body & infected material from oral cavity. Hypostatic pneumonia: It is caused due to accumulation of fluids & secretion in the lungs in bed ridden patients. The fluid tends to settle in lungs, increasing susceptibity to bacterial infection.
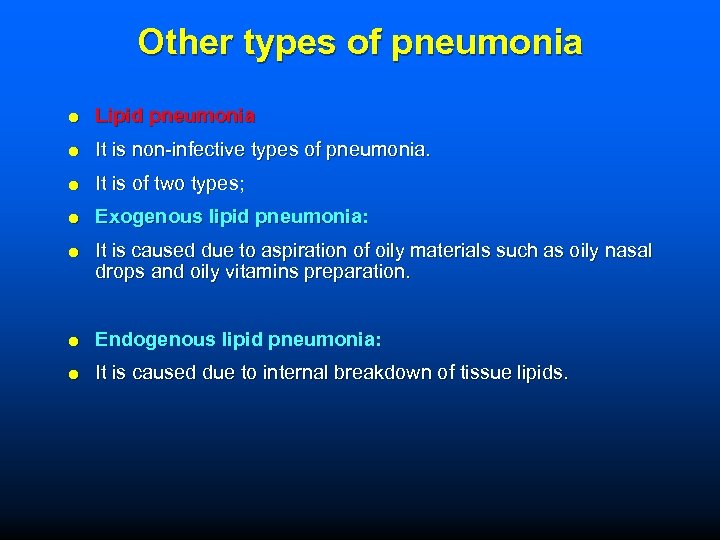
Other types of pneumonia Lipid pneumonia It is non-infective types of pneumonia. It is of two types; Exogenous lipid pneumonia: It is caused due to aspiration of oily materials such as oily nasal drops and oily vitamins preparation. Endogenous lipid pneumonia: It is caused due to internal breakdown of tissue lipids.
Anatomical Classification Lobar pneumonia Bronchopneumonia (Lobular pneumonia) Interstitial pneumonia
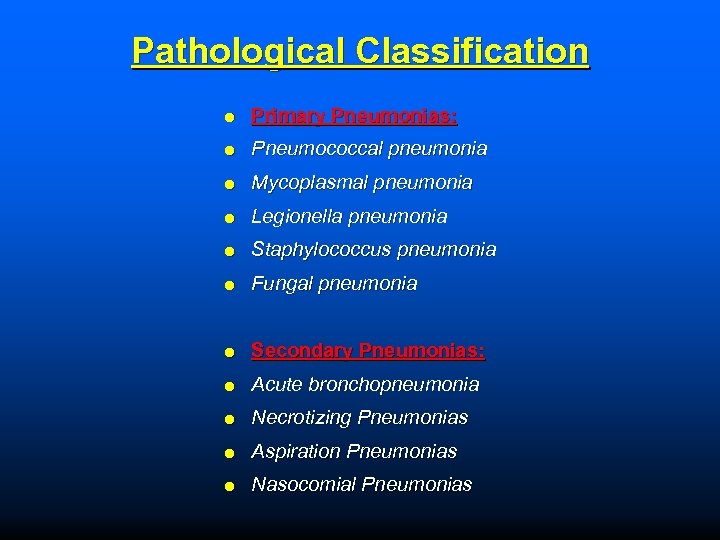
Pathological Classification Primary Pneumonias: Pneumococcal pneumonia Mycoplasmal pneumonia Legionella pneumonia Staphylococcus pneumonia Fungal pneumonia Secondary Pneumonias: Acute bronchopneumonia Necrotizing Pneumonias Aspiration Pneumonias Nasocomial Pneumonias
Symptoms Chest pain Shaking chills High fever (103 °F or higher) Fever Dry cough Muscle aches Nausea/vomiting Rapid heartbeat Difficulty breathing Skin with bluish tone (from lack of oxygen) Blood in sputum
Pathogenesis Pneumonia infection frequently starts at upper respiratory tract infection that moves into the lower respiratory tract. Bacterial Pneumonia: Bacteria enter the lungs by any of 4 routes. Once the bacteria are present in the lungs, it may invade the surrounding cells & alveoli, where the macrophages & neutrophils inactivate the bacteria. The neutrophils also release cytokines, causing a activation of immune system. This leads to fever, chills & fatigue. The neutrophils, bacteria, and fluid from surrounding blood vessels fill the alveoli, resulting in patchy consolidation of lung.
Pathogenesis Viral Pneumonia: The viruses may reach the lung in a number of different routes. RSV enters the lungs when people touch contaminated objects. Other viral infections occur after inhalation of contaminated airborne droplets by mouth or nose. The virus present in the lungs, invade the cells of airways, alveoli, or lung parenchyma. Some viruses such as measles and herpes simplex may reach the lungs via blood. The invasion of viruses in lungs may lead to varying degrees of cell death. Primarily the WBCs are responsible for causing lung parenchymal inflammation.
Diagnosis Physical Examination: Crackling & wheezing sounds in chest during inhalation of air are signs of pneumonia. Chest X-ray: Used to determine the infection of lungs. Blood tests: These tests are used to observe the infection of blood stream. Chest computed tomography (CT scan): This test provides a clear & precise picture of chest & lungs.
Diagnosis Sputum test: Examines the sputum to detect the type of pneumonia. Pleural fluid test: Examination of pleural fluid identifies the origin of pneumonia (bacterial or viral origin). Pulse oximetry: This test measures the level of oxygen in blood. Pneumonia can hampers the normal oxygenation of blood. Bronchoscopy: Flexible tube with camera at the other end is inserted through nose or mouth into airways that provides a video image of the airways. It also detects the degree of blockage in airways.
Treatment The type of treatment depends on the type of pneumonia and its severity. Bacterial Pneumonia Antibiotics are used to treat this type of pneumonia. Penicillin-G, Erythromycin, Azithromycin, Roxythromycin, Ciprofloxacin, Sparfloxacin, Cephalosporins, Gentamycin and Amphotericin Viral Pneumonia Antiviral drugs are used for the treatment of viral pneumonia.
Prevention Drink plenty of fluids to help loosen secretions. Avoid alcohol drinking & smoking. Regular chest physiotherapy. Clear the secretions. Inject pneumococcal vaccine to avoid infection of pneumonia.
CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD) Also known as chronic obstructive lung disease (COLD) or chronic obstructive airway disease (COAD). There is chronic, partial or complete obstruction to the airflow from trachea to smallest airways resulting in functional disability of lungs. It includes; v Chronic bronchitis v Emphysema v Asthma v Bronchitectasis
CHRONIC BRONCHITIS It is defined as persistent cough with expectoration for at least 3 months of the year for two or more consecutive years. Condition is more common in middle aged males than in females. Approximately 20 % of adult men & 5 % of adult women have chronic bronchitis.
Etiology Smoking: Heavy cigarette smokers have 4 to 10 times higher chance of chronic bronchitis. Atmospheric pollution: Sulfur dioxide, nitrogen dioxide, dust & toxic fumes. Occupation: Workers engaged in Cotton mills & Plastic factories are exposed to various organic & inorganic dusts and chemicals. Infection: Bacterial, viral & mycoplasmal infections are secondary factors Familial & genetic factors: Familial & genetic factors are also responsible. Non-smokers family members are exposed to cigarette smoke (passive smokers) & hence have increased levels of CO
Symptoms Persistent Cough that produces mucus (sputum) Shortness of breath aggravated by exertion Frequent respiratory infections Wheezing sound Hypoxia & cyanosis Fatigue Chest discomfort Slight fever & chills
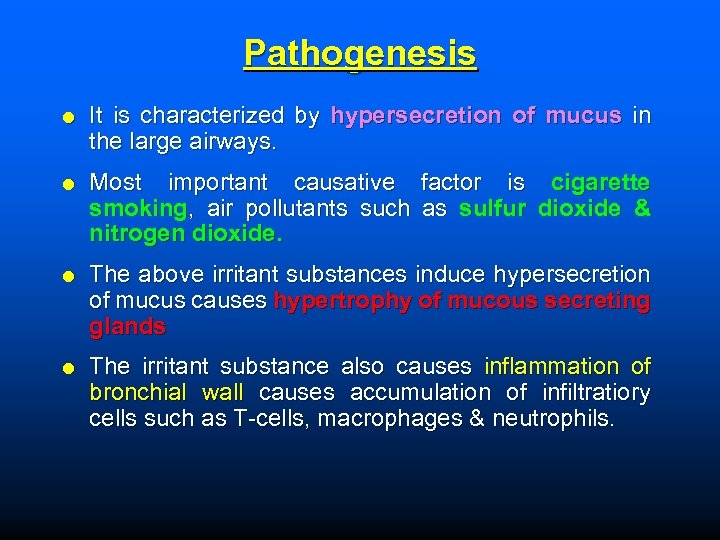
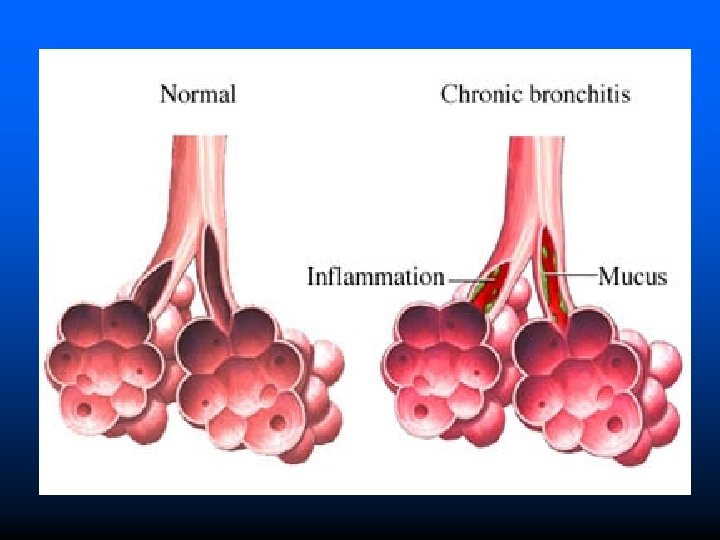
Pathogenesis It is characterized by hypersecretion of mucus in the large airways. Most important causative factor is cigarette smoking, air pollutants such as sulfur dioxide & nitrogen dioxide. The above irritant substances induce hypersecretion of mucus causes hypertrophy of mucous secreting glands The irritant substance also causes inflammation of bronchial wall causes accumulation of infiltratiory cells such as T-cells, macrophages & neutrophils.
Diagnosis Pulmonary function tests: Measures the functional ability of lungs. Pulse oximetry test: Measure oxygen level in blood Chest X-ray: It includes examination of chest & lungs Determination of Complete blood count (CBC) Exercise testing CT scan: It uses x-rays to create clear pictures of chest
Treatment Cessation of smoking & exposure to irritant substances Bronchodilators to dilate the airways Expectorant to loosen the mucus Anti-inflammatories to relieve airway inflammation & reduces mucus secretion Antibiotic treatment for respiratory infections Oxygen therapy
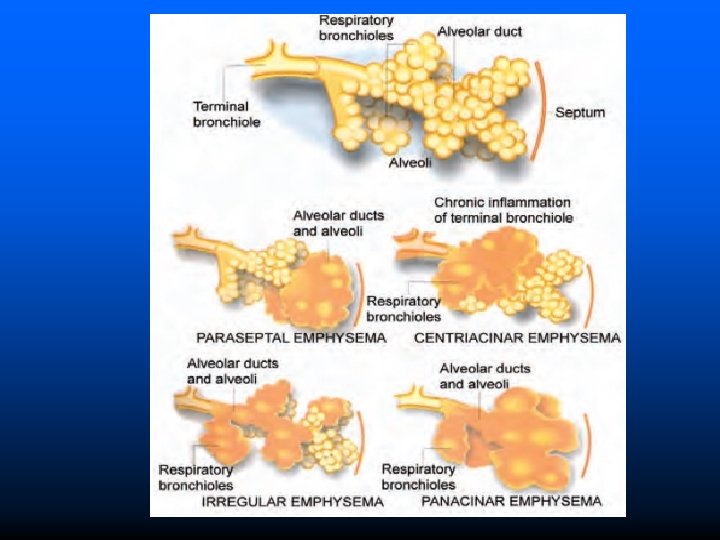
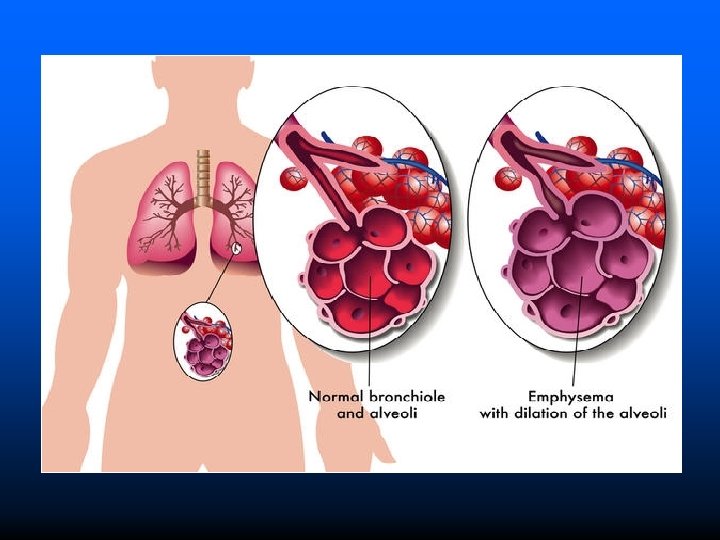
EMPHYSEMA It is a respiratory disease characterised by destruction & permanent enlargement of terminal bronchioles and alveolar sacs. Classified into 5 types depending on portion of acinus involved. Centri-acinar Emphysema (Centrilobular Emphysema): Common type It is characterised initial involvement of acinus Pana-acinar Emphysema (Panlobular Emphysema): Uniform enlargement of acinus from respiratory bronchiole to the alveoli.
Types Para-septal Emphysema (Distal-acinar Emphysema): Distal part of acius is affected while the proximal part is normal. Irregular Emphysema (Para-cicatricial Emphysema): Involvement of aciuns is irregular i. e. any portion of acinus is affected with fibrosis. Mixed Emphysema (Unclassified Emphysema): Same lung shows more than one types of emphysema.
Etiology Tobacco and Smoking Air pollutant Occupational exposure to fumes & smokes Infection Familial history Genetic history
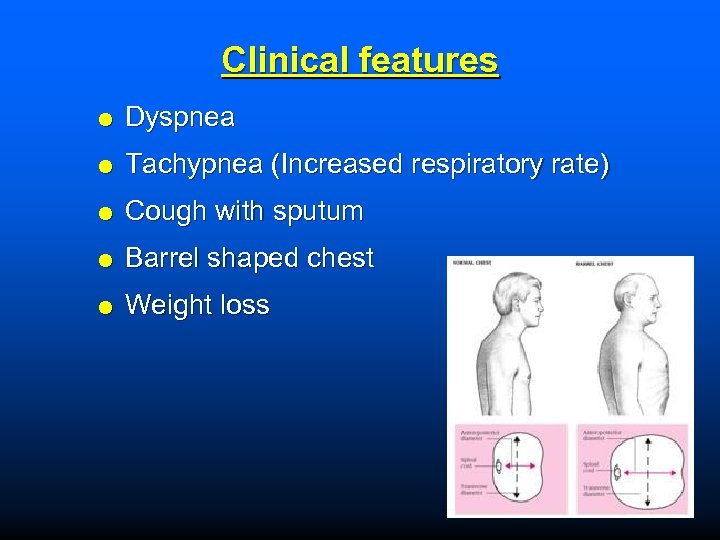
Clinical features Dyspnea Tachypnea (Increased respiratory rate) Cough with sputum Barrel shaped chest Weight loss
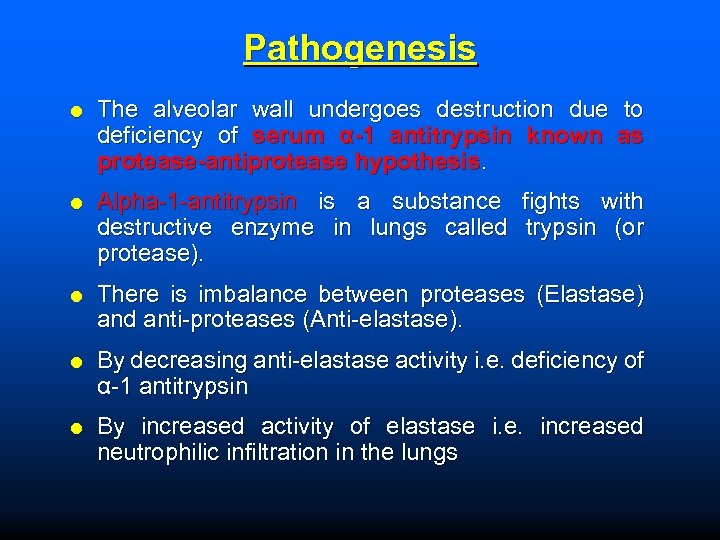
Pathogenesis The alveolar wall undergoes destruction due to deficiency of serum α-1 antitrypsin known as protease-antiprotease hypothesis. Alpha-1 -antitrypsin is a substance fights with destructive enzyme in lungs called trypsin (or protease). There is imbalance between proteases (Elastase) and anti-proteases (Anti-elastase). By decreasing anti-elastase activity i. e. deficiency of α-1 antitrypsin By increased activity of elastase i. e. increased neutrophilic infiltration in the lungs
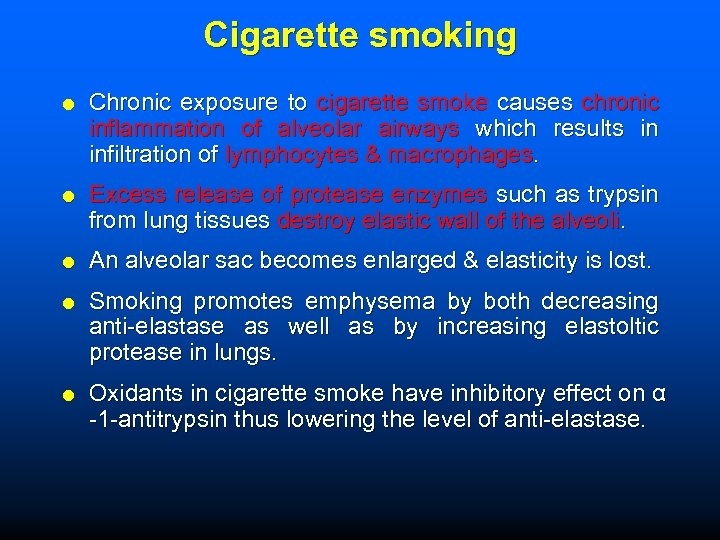
Cigarette smoking Chronic exposure to cigarette smoke causes chronic inflammation of alveolar airways which results in infiltration of lymphocytes & macrophages. Excess release of protease enzymes such as trypsin from lung tissues destroy elastic wall of the alveoli. An alveolar sac becomes enlarged & elasticity is lost. Smoking promotes emphysema by both decreasing anti-elastase as well as by increasing elastoltic protease in lungs. Oxidants in cigarette smoke have inhibitory effect on α -1 -antitrypsin thus lowering the level of anti-elastase.
Diagnosis Physical examination: Doctor will observe following signs; Increased chest size (barrel chest), Decreased breath sounds through stethoscope, Low oxygen levels in blood (Hypoxemia), High levels of carbon dioxide in blood (Hypercarbia), Blue-tinged lips (Cyanosis) & Malnutrition Pulmonary function tests: These measures functional ability of lungs. Chest X-ray examination: Chest X-ray may show abnormally of lungs.
Diagnosis Computed tomography: A CT scan shows small air pockets throughout the lung. Oximetry: Measures the amount of oxygen in the blood. Arterial blood gases: Blood tests are done to measures the levels of oxygen & carbon dioxide in bloodstream. Complete blood count: The red blood cell & white blood cell count may rises.
Prevention Avoid air pollution Don't smoke Avoid passive smoke Avoid high altitudes Avoid allergic "triggers" that can aggravate emphysema if asthma coexists Wash hands & brush teeth to avoid infections Drink plenty of fluids to reduce accumulation of thick mucus in air passages
Treatments Inhaled bronchodilators: Short acting (Albuterol) or long acting (Formoterol, Salmeterol) inhaled bronchodilators open the airways. Inhaled corticosteroids: Inhaled corticosteroids such as fluticasone or beclomethasone may reduce inflammation in the airways. Antibiotics: Used to treat lung infection if any. Purified human α 1 -antitrypsin: It is used for treatment of emphysema due to alpha-1 -antitrypsin deficiency. Besides medications, other treatments include:
Treatments Oxygen therapy: People with severe emphysema and low oxygen in blood can require long-term oxygen therapy. Pulmonary rehabilitation: It is an intensive program that combines exercise, nutrition, counseling and medication management. Lung volume reduction surgery: Surgical removal of affected lungs areas can improve the function of lung. This can improve breathing & quality of life. Vaccinations against influenza & pneumonia: The vaccination doesn’t treat the emphysema but may prevent the lungs from respiratory infections.
BRONCHIECTASIS It is defined as abnormal & irreversible dilation of bronchi & bronchioles (greater than 2 mm in diameter) due to inflammation of airways & bronchioles.
Etiology Bronchial obstruction: Common cause are tumors, foreign bodies, mucus plugs & compression by enlarged lymph nodes Congenital or hereditary causes: Necrotizing pneumonia: The staphylococcus aureus or Klebsiella pneumoniae species may predispose to bronchiectasis.
Clinical features Chronic cough with foul smelling sputum Bloody sputum Dyspnea Shortness of breath Wheezing Fever
Pathogenesis Two main processes are involved in inflammatory destructive process of bronchial walls. Endo-bronchial obstruction: The common cause is foreign body, neoplastic growth or enlarged lymph nodes impairs with the clearance of secretion, providing a good atmosphere for the growth of infective micro-organism. The inflammation of bronchial wall distend the airways causing irreversible dilation of bronchial airways. Infection: The infection is secondary cause of obstruction & promotes bacterial growth in necrotizing pneumonia.
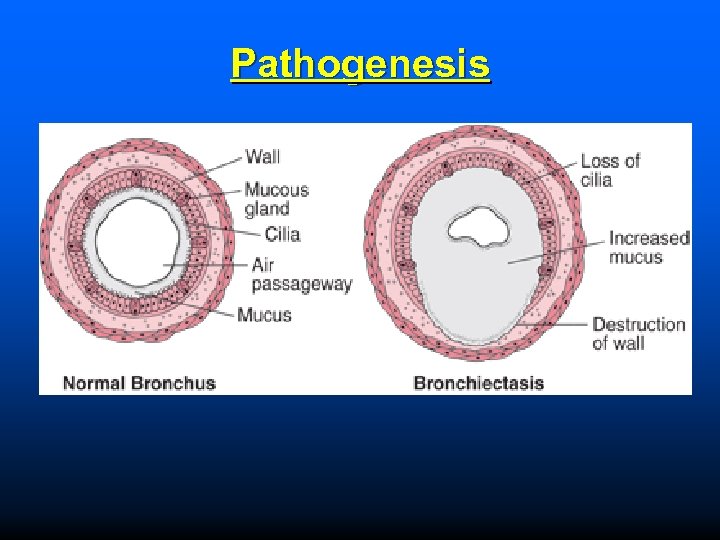
Pathogenesis
Diagnosis Chest X Ray: This test creates clear pictures of chest. It can show areas of abnormal lung & thickened, irregular airway walls. Chest CT Scan: It creates precise pictures of lungs. It shows the area of lung damage. Blood tests: It can detect any infection & increase the amount of white blood cells.
Diagnosis Sputum culture: It can detect the presence of bacteria or fungi in sputum. Lung function tests: It measure the quantity of air inhaled & exhaled during respiration. Bronchoscopy: It is a small flexible tube provides a video image of the airways. It also detects the degree of blockage in airways.
Treatment The goals of treatment are; Treat any underlying conditions and lung infections. Removal of mucus from lungs. Maintaining good hydration therapy in order to remove mucus. Prevent complications. Antibiotics: Antibiotics are used for treatment of repeated lung infections. Oral antibiotics are used to treat these infections. E. g. Amoxicillin, Tetracycline, Trimethoprimsulfamethoxazole, Azithromycin & Clarithromycin. Chest physical therapy (CPT): This technique involves massage of chest & back with hands or device which helps to loosen the mucus from lungs.
Treatment Inhaled bronchodilators: The use of short acting (Albuterol) or long acting (Formoterol, Salmeterol) inhaled bronchodilators may relax and open the airways. Inhaled corticosteroids: The use of inhaled corticosteroids such as fluticasone or beclomethasone may reduce inflammation in the airways. Expectorants & mucus-thinning medicines: They helps to loosen the mucus in lungs such as acetylcysteine. Hydration: Drinking plenty of water helps to prevent the airway mucus from becoming thick & sticky. Oxygen therapy: It can helps to raise the low blood oxygen levels.
Prevention Avoid air pollution Drink plenty of fluids to reduce the mucus in air passages Avoiding entry of toxic fumes, gases, smoke, & other harmful substances in to lungs Prevent the lung from infections Childhood vaccines for measles & whooping cough prevent chances of infections
Bronchial Asthma It is airways disease characterized by increased responsiveness of bronchial tree to a variety of stimuli resulting in chronic inflammation and reversible bronchospasm of airway passages. It occurs at all stages but 50% of cases develop before the age of 10 years. Types of asthma: Depending on the etiological factors; Classified into 3 types. v Extrinsic asthma (Atopic or allergic) v Intrinsic asthma (Non-atopic or idiosyncratic) v Mixed type asthma
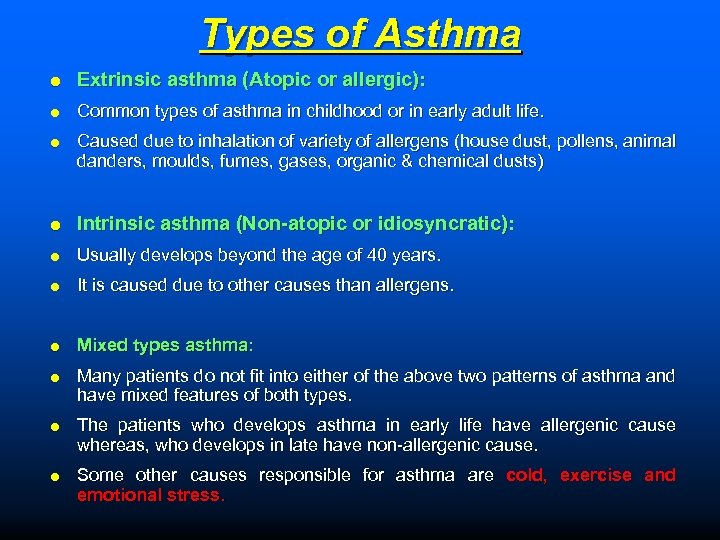
Types of Asthma Extrinsic asthma (Atopic or allergic): Common types of asthma in childhood or in early adult life. Caused due to inhalation of variety of allergens (house dust, pollens, animal danders, moulds, fumes, gases, organic & chemical dusts) Intrinsic asthma (Non-atopic or idiosyncratic): Usually develops beyond the age of 40 years. It is caused due to other causes than allergens. Mixed types asthma: Many patients do not fit into either of the above two patterns of asthma and have mixed features of both types. The patients who develops asthma in early life have allergenic cause whereas, who develops in late have non-allergenic cause. Some other causes responsible for asthma are cold, exercise and emotional stress.
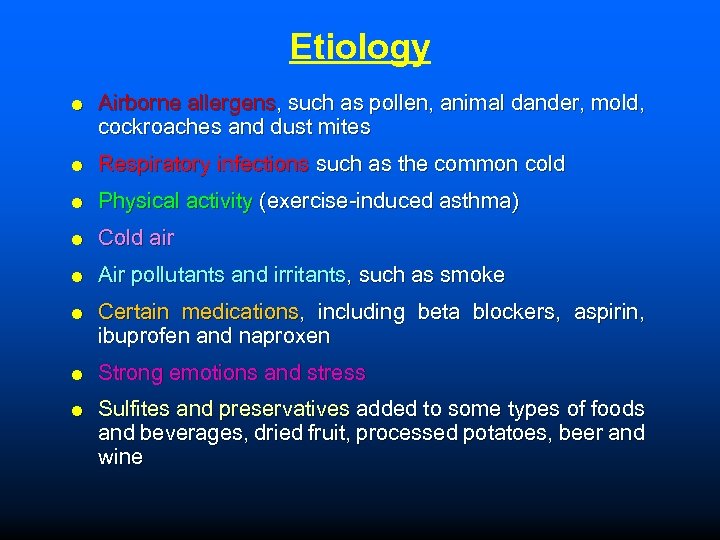
Etiology Airborne allergens, such as pollen, animal dander, mold, cockroaches and dust mites Respiratory infections such as the common cold Physical activity (exercise-induced asthma) Cold air Air pollutants and irritants, such as smoke Certain medications, including beta blockers, aspirin, ibuprofen and naproxen Strong emotions and stress Sulfites and preservatives added to some types of foods and beverages, dried fruit, processed potatoes, beer and wine
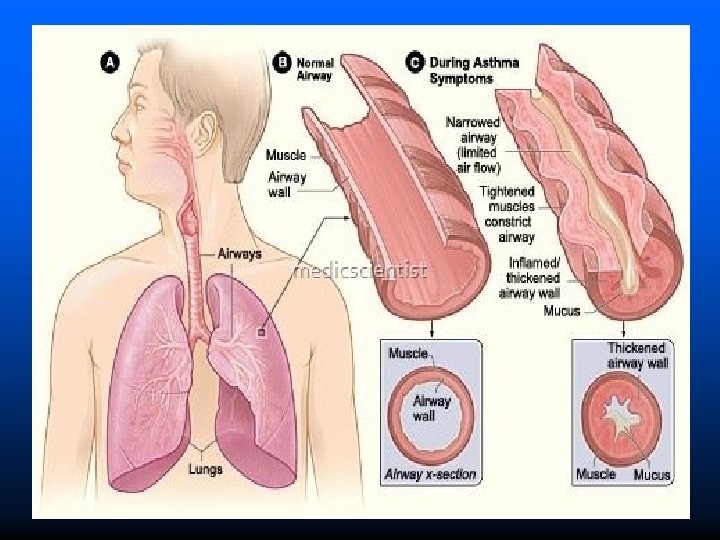
Clinical features Shortness of breath Chest tightness or pain Itching on chest Trouble in sleeping caused by shortness of breath, coughing or wheezing Wheezing sound during expiration Excess mucus production
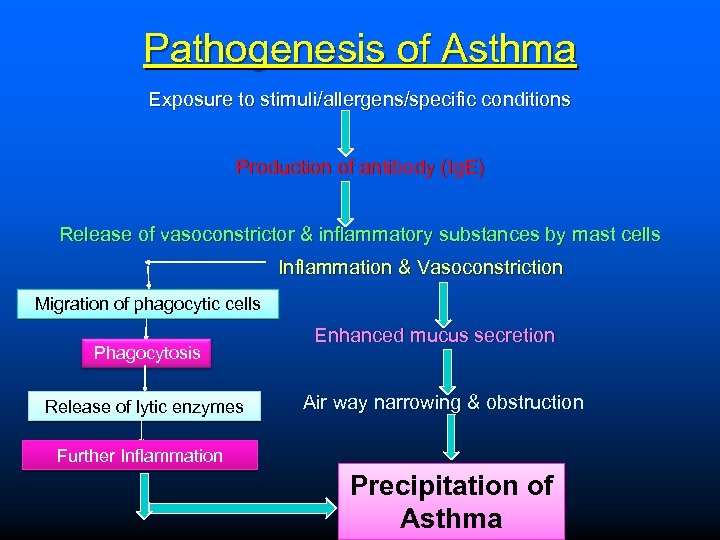
Pathogenesis of Asthma Exposure to stimuli/allergens/specific conditions Production of antibody (Ig. E) Release of vasoconstrictor & inflammatory substances by mast cells Inflammation & Vasoconstriction Migration of phagocytic cells Enhanced mucus secretion Phagocytosis Air way narrowing & obstruction Release of lytic enzymes Further Inflammation Precipitation of Asthma
Pathogenesis Exposure to various types of allergens causes hypersensitivity reaction. Type-I It includes acute immediate response and late phase response. Acute immediate response: It occurs by production of Ig. E immunoglobulins by mast cells. The mast cell on degranulation causes release of variety of chemical mediators such as HT, LT, PG, BK, PAF and chemotactic factors for eosinophils & neutrophils. The above released mediator causes bronchoconstriction, edema, mucus hypersecretion & accumulation of eosinophils and neutrophils at the site of inflammation.
Pathogenesis Late phase response: Late phase response manifests the inflammatory response. The primary mediators of inflammation are WBCs (eosinophils) that stimulate mast cell degranulation & releases substances that attract other WBCs to the area. Later on infiltration of other white cells such as neutrophils and lymphocytes to the site of inflammation contributes to overall inflammatory responses.
Diagnosis Physical examination: Doctor will examine nose, throat & upper airways. Wheezing sound is main signs. Spirometry test: This involves taking a deep breath & exhaling as fast as you can by using spirometer. Challenge test: If the spirometer results are normal, try to trigger the asthma symptoms by inhaling Methacholine that causes airways narrowing and spirometry test is repeated. If the spirometry measurements remain normal, it is said that the person is not having asthma. Allergy test: Skin testing or a blood test can be used to confirm whether asthma is associated with specific allergies, such as dust mites, pollen or foods.
Diagnosis Exhaled nitric oxide test: Patient breathe into a tube connected to a machine that measures the amount of NO 2 gas in breath. NO 2 gas is produced by body normally, but high levels in breath indicate inflammation of airways. Mucus sample test: The sample of mucus is tested for airways inflammation, viral & bacterial infection. Laboratory investigation test: Chest X-ray examination: To check chest infection & severity of lung pathology Blood examination: Leukocytosis is common in respiratory infection. Sputum examination: To check respiratory infection.
Treatments Bronchodilators: E. g. Albuterol, Salbutamol & Terbutaline These drugs dilates the bronchioles but do not prevent inflammatory response. Xanthine drugs: E. g. Theophylline These drugs cause bronchodilation and inhibit late phase of asthma. Administered alone or in combination with β 2 receptor agonist for better effects. Anti-inflammatory drugs (Corticosteroids): E. g. Prednisolone, Methylprednisolone, Hydrocortisone, Beclomethasone These drugs inhibit the inflammatory responses of asthma. Cromolyn sodium: It is an anti-inflammatory agent that inhibits the releases of inflammatory mediators from mast cells. Leukotriene modifiers: E. g. Zafirlukast It blocks the synthesis of the key inflammatory mediators LT.
Prevention Dust free house Avoidance of triggers and allergens. Improved ventilation of living spaces Use of air conditioning Avoid extreme exposure to cold condition Medication before heavy exertion and exercise Intake of selective food material
96189c97aad3d5a36ad51e6047700c51.ppt