39f86e07d35fa5041ba45b901322e6f3.ppt
- Количество слайдов: 52
 RESPIRATORY SYSTEM ASSESSMENT
RESPIRATORY SYSTEM ASSESSMENT
 PYRAMID POINTS • Respiratory assessment techniques • Risk factors related to respiratory disorders • Preprocedure and postprocedure client instructions for diagnostic tests • Monitoring for complications following diagnostic procedures • Mantoux skin test • Obtaining arterial blood gases • Performing pulse oximetry
PYRAMID POINTS • Respiratory assessment techniques • Risk factors related to respiratory disorders • Preprocedure and postprocedure client instructions for diagnostic tests • Monitoring for complications following diagnostic procedures • Mantoux skin test • Obtaining arterial blood gases • Performing pulse oximetry
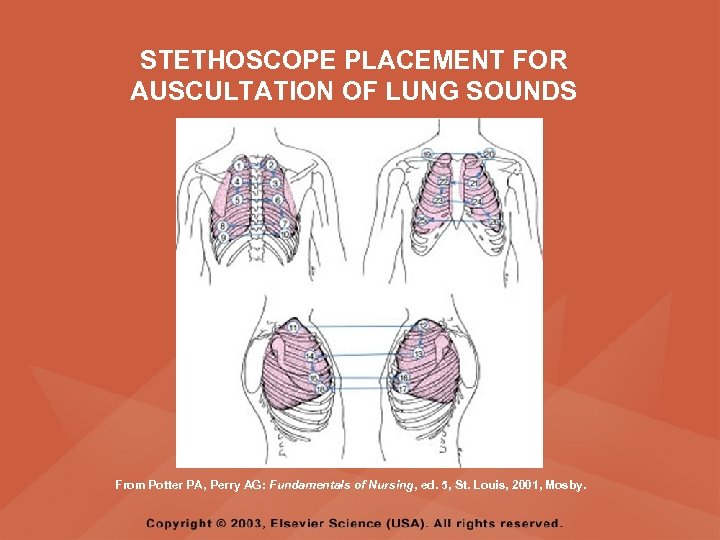 STETHOSCOPE PLACEMENT FOR AUSCULTATION OF LUNG SOUNDS From Potter PA, Perry AG: Fundamentals of Nursing, ed. 5, St. Louis, 2001, Mosby.
STETHOSCOPE PLACEMENT FOR AUSCULTATION OF LUNG SOUNDS From Potter PA, Perry AG: Fundamentals of Nursing, ed. 5, St. Louis, 2001, Mosby.
 RISK FACTORS FOR RESPIRATORY DISORDERS • • • Smoking or use of chewing tobacco Allergies Frequent respiratory illnesses Chest injury Surgery Exposure to chemicals and environmental pollutants • Crowded living conditions • Family history of infectious disease • Geographic residence and travel to foreign countries
RISK FACTORS FOR RESPIRATORY DISORDERS • • • Smoking or use of chewing tobacco Allergies Frequent respiratory illnesses Chest injury Surgery Exposure to chemicals and environmental pollutants • Crowded living conditions • Family history of infectious disease • Geographic residence and travel to foreign countries
 CHEST X-RAY (CXR) FILM (RADIOGRAPH) • DESCRIPTION – Provides information regarding the anatomic location and appearance of the lungs
CHEST X-RAY (CXR) FILM (RADIOGRAPH) • DESCRIPTION – Provides information regarding the anatomic location and appearance of the lungs
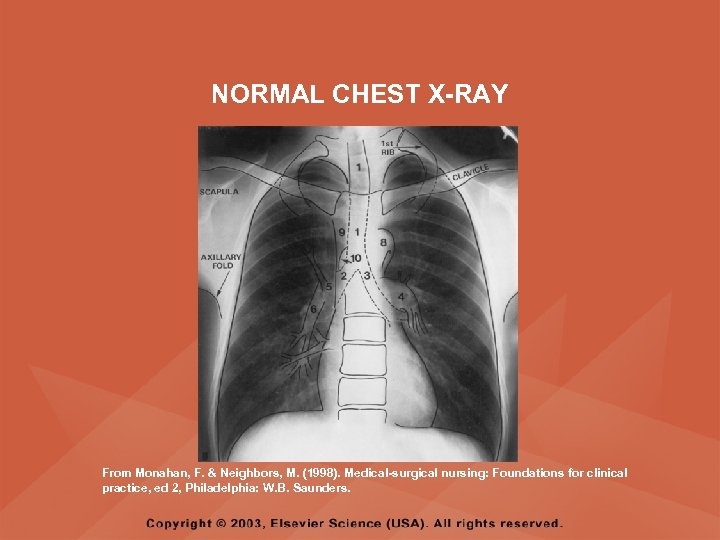 NORMAL CHEST X-RAY From Monahan, F. & Neighbors, M. (1998). Medical-surgical nursing: Foundations for clinical practice, ed 2, Philadelphia: W. B. Saunders.
NORMAL CHEST X-RAY From Monahan, F. & Neighbors, M. (1998). Medical-surgical nursing: Foundations for clinical practice, ed 2, Philadelphia: W. B. Saunders.
 CHEST X-RAY (CXR) FILM (RADIOGRAPH) • PREPROCEDURE – Remove all jewelry and other metal objects from the chest area – Assess the client’s ability to inhale and hold breath – Question females regarding pregnancy or the possibility of pregnancy • POSTPROCEDURE – Assist the client to dress
CHEST X-RAY (CXR) FILM (RADIOGRAPH) • PREPROCEDURE – Remove all jewelry and other metal objects from the chest area – Assess the client’s ability to inhale and hold breath – Question females regarding pregnancy or the possibility of pregnancy • POSTPROCEDURE – Assist the client to dress
 SPUTUM SPECIMEN • DESCRIPTION – A specimen obtained by expectoration or tracheal suctioning to assist in the identification of organisms or abnormal cells
SPUTUM SPECIMEN • DESCRIPTION – A specimen obtained by expectoration or tracheal suctioning to assist in the identification of organisms or abnormal cells
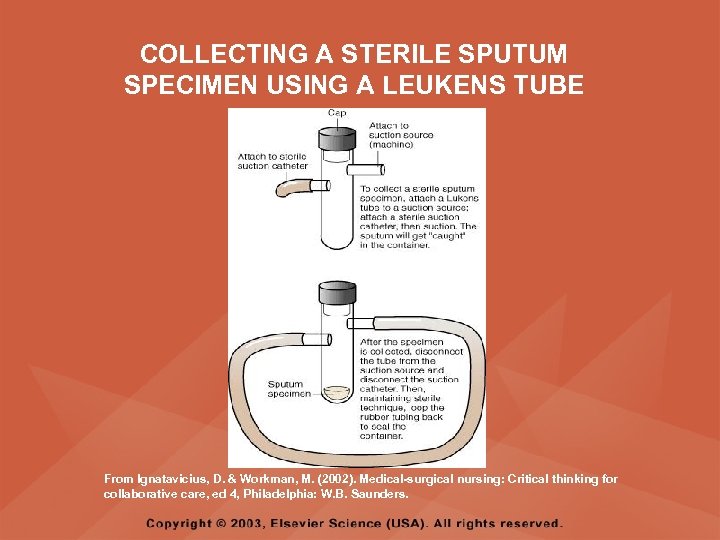 COLLECTING A STERILE SPUTUM SPECIMEN USING A LEUKENS TUBE From Ignatavicius, D. & Workman, M. (2002). Medical-surgical nursing: Critical thinking for collaborative care, ed 4, Philadelphia: W. B. Saunders.
COLLECTING A STERILE SPUTUM SPECIMEN USING A LEUKENS TUBE From Ignatavicius, D. & Workman, M. (2002). Medical-surgical nursing: Critical thinking for collaborative care, ed 4, Philadelphia: W. B. Saunders.
 SPUTUM SPECIMEN • PREPROCEDURE – Determine specific purpose of collection and check with institutional policy for appropriate collection of specimen – Obtain an early morning sterile specimen from suctioning or expectoration after a respiratory treatment, if a treatment is prescribed – Obtain 15 ml of sputum
SPUTUM SPECIMEN • PREPROCEDURE – Determine specific purpose of collection and check with institutional policy for appropriate collection of specimen – Obtain an early morning sterile specimen from suctioning or expectoration after a respiratory treatment, if a treatment is prescribed – Obtain 15 ml of sputum
 SPUTUM SPECIMEN • PREPROCEDURE – Instruct the client to rinse the mouth with water prior to collection – Instruct the client to take several deep breaths and then cough deeply to obtain sputum – Always collect the specimen before starting antibiotics
SPUTUM SPECIMEN • PREPROCEDURE – Instruct the client to rinse the mouth with water prior to collection – Instruct the client to take several deep breaths and then cough deeply to obtain sputum – Always collect the specimen before starting antibiotics
 SPUTUM SPECIMEN • POSTPROCEDURE – If a culture of sputum is prescribed, transport specimen to laboratory immediately – Assist the client with mouth care
SPUTUM SPECIMEN • POSTPROCEDURE – If a culture of sputum is prescribed, transport specimen to laboratory immediately – Assist the client with mouth care
 BRONCHOSCOPY • DESCRIPTION – Direct visual examination of the larynx, trachea, and bronchi with a fiberoptic bronchoscope
BRONCHOSCOPY • DESCRIPTION – Direct visual examination of the larynx, trachea, and bronchi with a fiberoptic bronchoscope
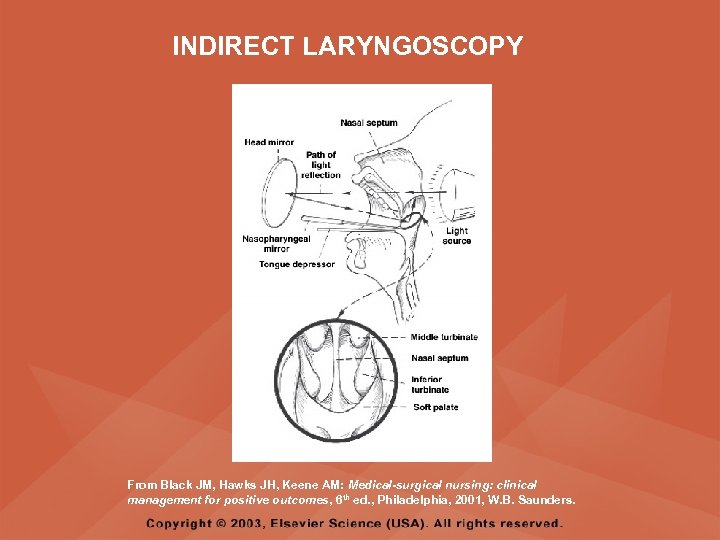 INDIRECT LARYNGOSCOPY From Black JM, Hawks JH, Keene AM: Medical-surgical nursing: clinical management for positive outcomes, 6 th ed. , Philadelphia, 2001, W. B. Saunders.
INDIRECT LARYNGOSCOPY From Black JM, Hawks JH, Keene AM: Medical-surgical nursing: clinical management for positive outcomes, 6 th ed. , Philadelphia, 2001, W. B. Saunders.
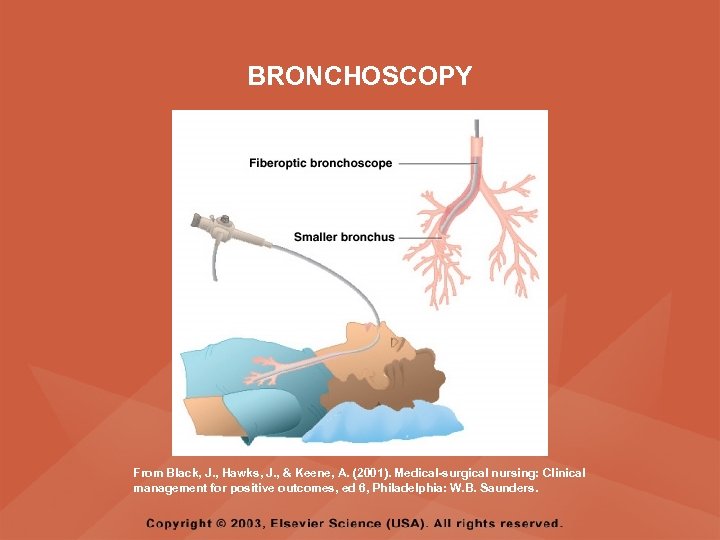 BRONCHOSCOPY From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
BRONCHOSCOPY From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
 BRONCHOSCOPY • PREPROCEDURE – Obtain informed consent – NPO from midnight prior to the procedure – Obtain vital signs – Assess the results of coagulation studies – Remove dentures or eyeglasses – Prepare suction equipment – Administer medication for sedation as prescribed – Have emergency resuscitation equipment readily available
BRONCHOSCOPY • PREPROCEDURE – Obtain informed consent – NPO from midnight prior to the procedure – Obtain vital signs – Assess the results of coagulation studies – Remove dentures or eyeglasses – Prepare suction equipment – Administer medication for sedation as prescribed – Have emergency resuscitation equipment readily available
 BRONCHOSCOPY • POSTPROCEDURE – Monitor vital signs – Maintain semi-Fowler's position – Assess for the return of the gag reflex – Maintain NPO status until gag reflex returns – Have an emesis basin readily available for client to expectorate sputum – Monitor for bloody sputum
BRONCHOSCOPY • POSTPROCEDURE – Monitor vital signs – Maintain semi-Fowler's position – Assess for the return of the gag reflex – Maintain NPO status until gag reflex returns – Have an emesis basin readily available for client to expectorate sputum – Monitor for bloody sputum
 BRONCHOSCOPY • POSTPROCEDURE – Monitor respiratory status, particularly if sedation was administered – Monitor for complications, such as bronchospasm, bronchial perforation indicated by facial or neck crepitus, dysrhythmias, fever, bacteremia, hemorrhage, hypoxemia, and pneumothorax – Notify the physician if fever, difficulty breathing, or other signs of complications occur following the procedure
BRONCHOSCOPY • POSTPROCEDURE – Monitor respiratory status, particularly if sedation was administered – Monitor for complications, such as bronchospasm, bronchial perforation indicated by facial or neck crepitus, dysrhythmias, fever, bacteremia, hemorrhage, hypoxemia, and pneumothorax – Notify the physician if fever, difficulty breathing, or other signs of complications occur following the procedure
 PULMONARY ANGIOGRAPHY • DESCRIPTION – An invasive fluoroscopic procedure in which a catheter inserted through the antecubital or femoral vein into the pulmonary artery or one of its branches – Involves an injection of iodine, radiopaque, or contrast material
PULMONARY ANGIOGRAPHY • DESCRIPTION – An invasive fluoroscopic procedure in which a catheter inserted through the antecubital or femoral vein into the pulmonary artery or one of its branches – Involves an injection of iodine, radiopaque, or contrast material
 PULMONARY ANGIOGRAPHY • PREPROCEDURE – Obtain informed consent – Assess for allergies to iodine, seafood, or other radiopaque dyes – Maintain NPO status for 8 hours prior to the procedure – Monitor vital signs – Assess results of coagulation studies – Establish an IV access
PULMONARY ANGIOGRAPHY • PREPROCEDURE – Obtain informed consent – Assess for allergies to iodine, seafood, or other radiopaque dyes – Maintain NPO status for 8 hours prior to the procedure – Monitor vital signs – Assess results of coagulation studies – Establish an IV access
 PULMONARY ANGIOGRAPHY • PREPROCEDURE – Administer sedation as prescribed – Instruct the client that he or she must lie still during the procedure – Instruct the client that he or she may feel an urge to cough, flushing, nausea, or a salty taste following injection of the dye – Have emergency resuscitation equipment available
PULMONARY ANGIOGRAPHY • PREPROCEDURE – Administer sedation as prescribed – Instruct the client that he or she must lie still during the procedure – Instruct the client that he or she may feel an urge to cough, flushing, nausea, or a salty taste following injection of the dye – Have emergency resuscitation equipment available
 PULMONARY ANGIOGRAPHY • POSTPROCEDURE – Monitor vital signs – Avoid taking blood pressures in the extremity used for the injection for 24 hours – Monitor peripheral neurovascular status – Assess insertion site for bleeding – Monitor for delayed reaction to the dye
PULMONARY ANGIOGRAPHY • POSTPROCEDURE – Monitor vital signs – Avoid taking blood pressures in the extremity used for the injection for 24 hours – Monitor peripheral neurovascular status – Assess insertion site for bleeding – Monitor for delayed reaction to the dye
 THORACENTESIS • DESCRIPTION – Removal of fluid or air from the pleural space via a transthoracic aspiration • PREPROCEDURE – Obtain consent – Obtain vital signs – Prepare the client for ultrasound or chest radiograph if prescribed prior to procedure – Assess results of coagulation studies
THORACENTESIS • DESCRIPTION – Removal of fluid or air from the pleural space via a transthoracic aspiration • PREPROCEDURE – Obtain consent – Obtain vital signs – Prepare the client for ultrasound or chest radiograph if prescribed prior to procedure – Assess results of coagulation studies
 THORACENTESIS • DURING THE PROCEDURE – The client is positioned sitting upright, with the arms and head supported by a table at the bedside during the procedure – If the client cannot sit up, the client is placed lying in bed on the unaffected side with the head of the bed elevated 45 degrees – Inform the client not to cough, breathe deeply, or move during the procedure
THORACENTESIS • DURING THE PROCEDURE – The client is positioned sitting upright, with the arms and head supported by a table at the bedside during the procedure – If the client cannot sit up, the client is placed lying in bed on the unaffected side with the head of the bed elevated 45 degrees – Inform the client not to cough, breathe deeply, or move during the procedure
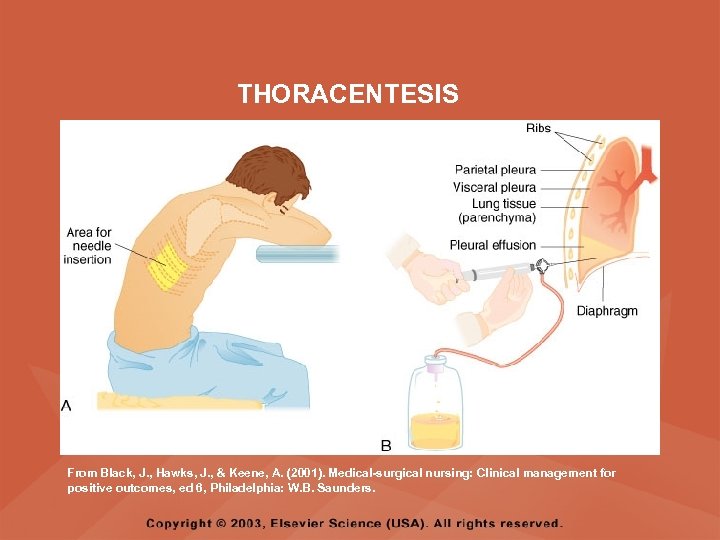 THORACENTESIS From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
THORACENTESIS From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
 THORACENTESIS • POSTPROCEDURE – Monitor vital signs – Monitor respiratory status – Apply a pressure dressing and assess the puncture site for bleeding and crepitus – Monitor for signs of pneumothorax, air embolism, and pulmonary edema
THORACENTESIS • POSTPROCEDURE – Monitor vital signs – Monitor respiratory status – Apply a pressure dressing and assess the puncture site for bleeding and crepitus – Monitor for signs of pneumothorax, air embolism, and pulmonary edema
 PULMONARY FUNCTION TEST (PFT) • DESCRIPTION – Includes a number of different tests used to evaluate lung mechanics, gas exchange, and acid-base disturbance through spirometric measurements, lung volumes, and arterial blood gases
PULMONARY FUNCTION TEST (PFT) • DESCRIPTION – Includes a number of different tests used to evaluate lung mechanics, gas exchange, and acid-base disturbance through spirometric measurements, lung volumes, and arterial blood gases
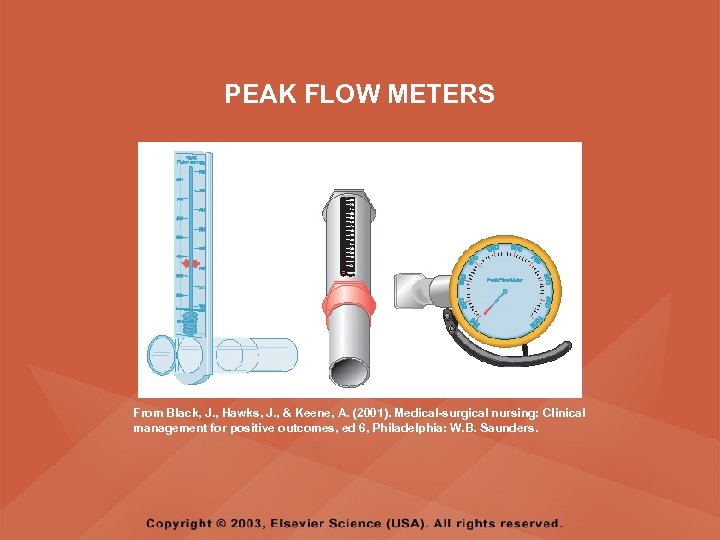 PEAK FLOW METERS From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
PEAK FLOW METERS From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
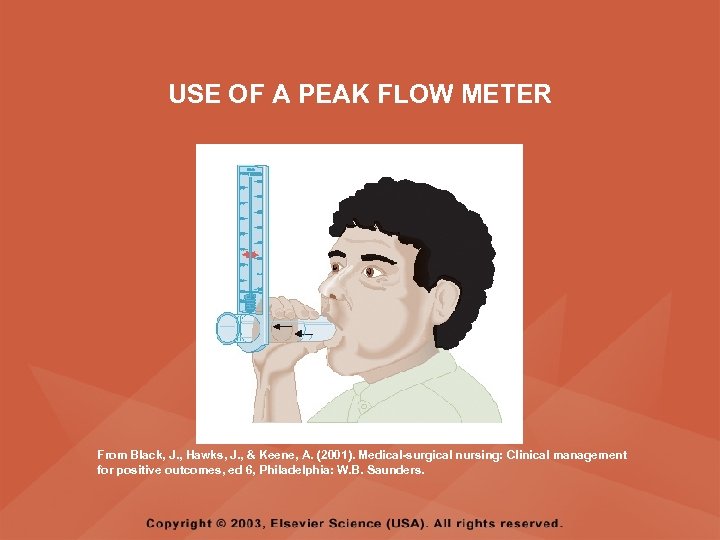 USE OF A PEAK FLOW METER From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
USE OF A PEAK FLOW METER From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
 SPIROMETER From Wilson SF, Thompson JM: Respiratory Disorders, St. Louis, 1990, Mosby.
SPIROMETER From Wilson SF, Thompson JM: Respiratory Disorders, St. Louis, 1990, Mosby.
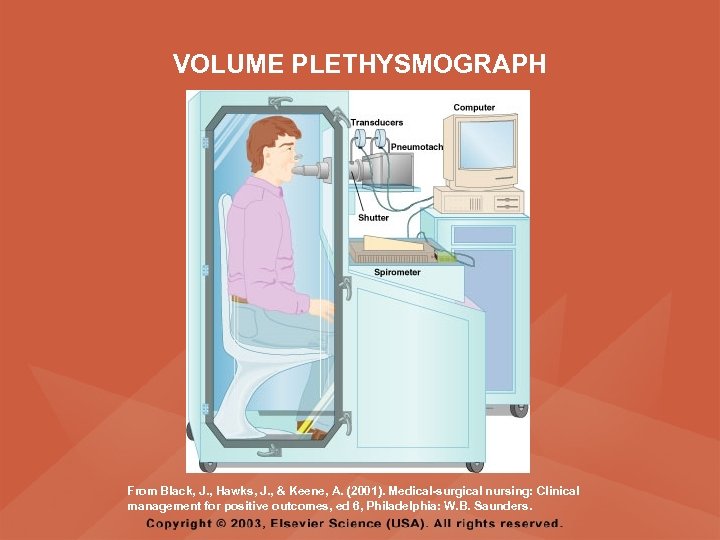 VOLUME PLETHYSMOGRAPH From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
VOLUME PLETHYSMOGRAPH From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
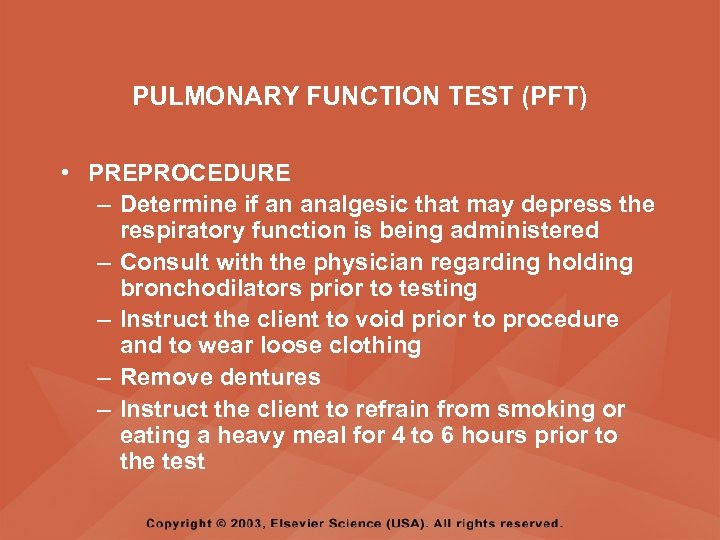 PULMONARY FUNCTION TEST (PFT) • PREPROCEDURE – Determine if an analgesic that may depress the respiratory function is being administered – Consult with the physician regarding holding bronchodilators prior to testing – Instruct the client to void prior to procedure and to wear loose clothing – Remove dentures – Instruct the client to refrain from smoking or eating a heavy meal for 4 to 6 hours prior to the test
PULMONARY FUNCTION TEST (PFT) • PREPROCEDURE – Determine if an analgesic that may depress the respiratory function is being administered – Consult with the physician regarding holding bronchodilators prior to testing – Instruct the client to void prior to procedure and to wear loose clothing – Remove dentures – Instruct the client to refrain from smoking or eating a heavy meal for 4 to 6 hours prior to the test
 PULMONARY FUNCTION TEST (PFT) • POSTPROCEDURE – Resume normal diet and any bronchodilators and respiratory treatments that were held prior to the procedure
PULMONARY FUNCTION TEST (PFT) • POSTPROCEDURE – Resume normal diet and any bronchodilators and respiratory treatments that were held prior to the procedure
 LUNG BIOPSY • DESCRIPTION – A percutaneous lung biopsy is performed to obtain tissue for analysis by culture or cytologic examination – A needle biopsy is done to identify pulmonary lesions, changes in lung tissue, and the cause of pleural effusion
LUNG BIOPSY • DESCRIPTION – A percutaneous lung biopsy is performed to obtain tissue for analysis by culture or cytologic examination – A needle biopsy is done to identify pulmonary lesions, changes in lung tissue, and the cause of pleural effusion
 LUNG BIOPSY • PREPROCEDURE – Obtain informed consent – Maintain NPO status prior to the procedure – Inform the client that a local anesthetic will be used but that a sensation of pressure during needle insertion and aspiration may be felt – Administer analgesics and sedatives as prescribed
LUNG BIOPSY • PREPROCEDURE – Obtain informed consent – Maintain NPO status prior to the procedure – Inform the client that a local anesthetic will be used but that a sensation of pressure during needle insertion and aspiration may be felt – Administer analgesics and sedatives as prescribed
 LUNG BIOPSY • POSTPROCEDURE – Monitor vital signs – Apply a dressing to the biopsy site and monitor for drainage or bleeding – Monitor for signs of respiratory distress, and notify the physician if they occur – Monitor for signs of pneumothorax and air emboli, and notify the physician if they occur – Prepare the client for chest x-ray film if prescribed
LUNG BIOPSY • POSTPROCEDURE – Monitor vital signs – Apply a dressing to the biopsy site and monitor for drainage or bleeding – Monitor for signs of respiratory distress, and notify the physician if they occur – Monitor for signs of pneumothorax and air emboli, and notify the physician if they occur – Prepare the client for chest x-ray film if prescribed
 VENTILATION PERFUSION LUNG SCAN • DESCRIPTION – In the perfusion scan, blood flow to the lungs is evaluated – The ventilation scan determines the patency of the pulmonary airways and detects abnormalities in ventilation – A radionuclide may be injected for the procedure
VENTILATION PERFUSION LUNG SCAN • DESCRIPTION – In the perfusion scan, blood flow to the lungs is evaluated – The ventilation scan determines the patency of the pulmonary airways and detects abnormalities in ventilation – A radionuclide may be injected for the procedure
 VENTILATION PERFUSION LUNG SCAN • PREPROCEDURE – Obtain informed consent – Assess for allergies to dye, iodine, or seafood – Remove jewelry around the chest area – Review breathing methods, which may be required during testing – Establish an IV access – Administer sedation if prescribed – Have emergency resuscitation equipment available
VENTILATION PERFUSION LUNG SCAN • PREPROCEDURE – Obtain informed consent – Assess for allergies to dye, iodine, or seafood – Remove jewelry around the chest area – Review breathing methods, which may be required during testing – Establish an IV access – Administer sedation if prescribed – Have emergency resuscitation equipment available
 VENTILATION PERFUSION LUNG SCAN • POSTPROCEDURE – Monitor client for reaction to the radionuclide – For 24 hours following the procedure, rubber gloves worn when urine is being discarded should be washed with soap and water before removing; then, the hands should be washed after the gloves are removed – Instruct client to wash hands carefully with soap and water for 24 hours following the procedure
VENTILATION PERFUSION LUNG SCAN • POSTPROCEDURE – Monitor client for reaction to the radionuclide – For 24 hours following the procedure, rubber gloves worn when urine is being discarded should be washed with soap and water before removing; then, the hands should be washed after the gloves are removed – Instruct client to wash hands carefully with soap and water for 24 hours following the procedure
 SKIN TESTS • DESCRIPTION – An intradermal injection used to assist in diagnosing various infectious diseases • PREPROCEDURE – Determine hypersensitivity or previous reactions to skin tests
SKIN TESTS • DESCRIPTION – An intradermal injection used to assist in diagnosing various infectious diseases • PREPROCEDURE – Determine hypersensitivity or previous reactions to skin tests
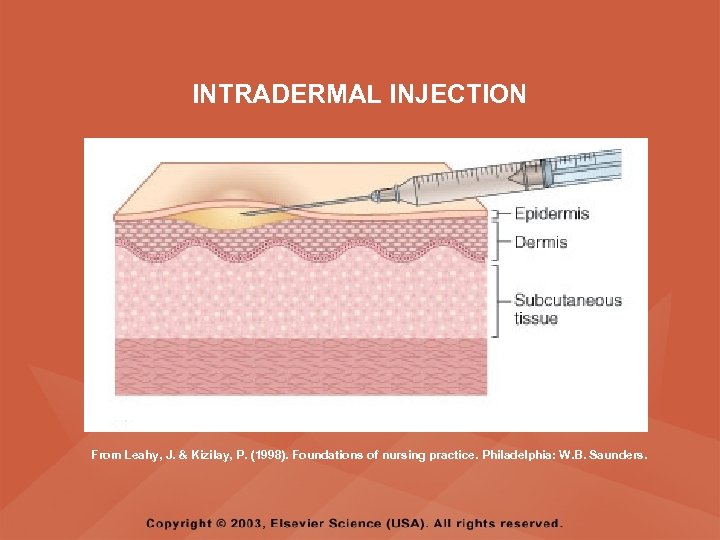 INTRADERMAL INJECTION From Leahy, J. & Kizilay, P. (1998). Foundations of nursing practice. Philadelphia: W. B. Saunders.
INTRADERMAL INJECTION From Leahy, J. & Kizilay, P. (1998). Foundations of nursing practice. Philadelphia: W. B. Saunders.
 SKIN TESTS • PROCEDURE – Use a test site that is free from excessive body hair, dermatitis, and blemishes – Apply at the upper one third of inner surface of left arm – Circle and mark the injection test site – Document the date, time, and test site
SKIN TESTS • PROCEDURE – Use a test site that is free from excessive body hair, dermatitis, and blemishes – Apply at the upper one third of inner surface of left arm – Circle and mark the injection test site – Document the date, time, and test site
 SKIN TESTS • POSTPROCEDURE – Advise the client not to scratch the test site to prevent infection and abscess formation – Instruct the client to avoid washing the test site – Interpret the reaction at the injection site 24 to 72 hours after administration of the test antigen – Assess the test site for the amount of induration (hard swelling) in millimeters and the presence of erythema and vesiculation (small blister-like elevations)
SKIN TESTS • POSTPROCEDURE – Advise the client not to scratch the test site to prevent infection and abscess formation – Instruct the client to avoid washing the test site – Interpret the reaction at the injection site 24 to 72 hours after administration of the test antigen – Assess the test site for the amount of induration (hard swelling) in millimeters and the presence of erythema and vesiculation (small blister-like elevations)
 ARTERIAL BLOOD GASES (ABGs) • DESCRIPTION – Measures the dissolved oxygen and carbon dioxide in the arterial blood and reveals the acid-base state and how well the oxygen is being carried to the body
ARTERIAL BLOOD GASES (ABGs) • DESCRIPTION – Measures the dissolved oxygen and carbon dioxide in the arterial blood and reveals the acid-base state and how well the oxygen is being carried to the body
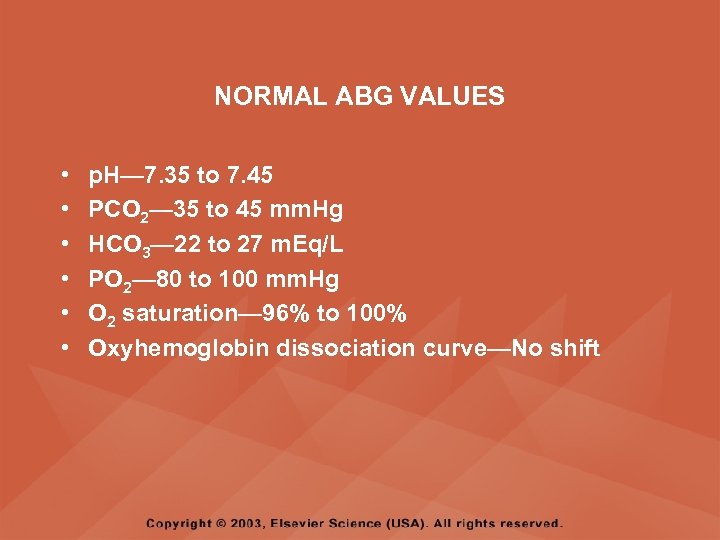 NORMAL ABG VALUES • • • p. H— 7. 35 to 7. 45 PCO 2— 35 to 45 mm. Hg HCO 3— 22 to 27 m. Eq/L PO 2— 80 to 100 mm. Hg O 2 saturation— 96% to 100% Oxyhemoglobin dissociation curve—No shift
NORMAL ABG VALUES • • • p. H— 7. 35 to 7. 45 PCO 2— 35 to 45 mm. Hg HCO 3— 22 to 27 m. Eq/L PO 2— 80 to 100 mm. Hg O 2 saturation— 96% to 100% Oxyhemoglobin dissociation curve—No shift
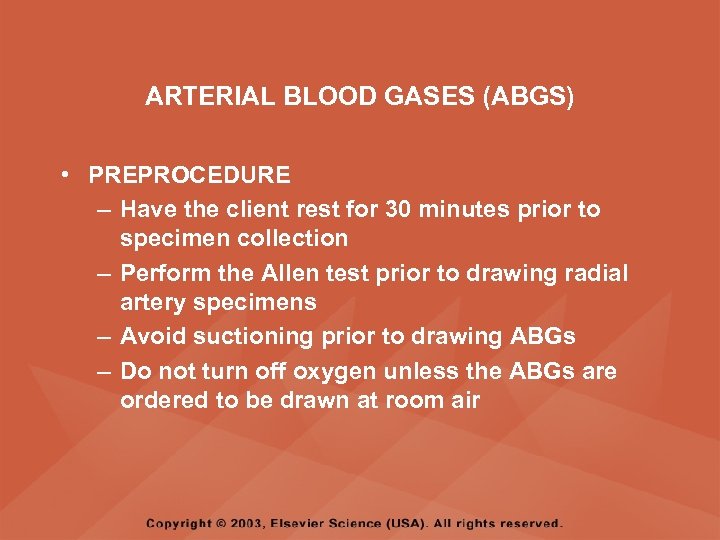 ARTERIAL BLOOD GASES (ABGS) • PREPROCEDURE – Have the client rest for 30 minutes prior to specimen collection – Perform the Allen test prior to drawing radial artery specimens – Avoid suctioning prior to drawing ABGs – Do not turn off oxygen unless the ABGs are ordered to be drawn at room air
ARTERIAL BLOOD GASES (ABGS) • PREPROCEDURE – Have the client rest for 30 minutes prior to specimen collection – Perform the Allen test prior to drawing radial artery specimens – Avoid suctioning prior to drawing ABGs – Do not turn off oxygen unless the ABGs are ordered to be drawn at room air
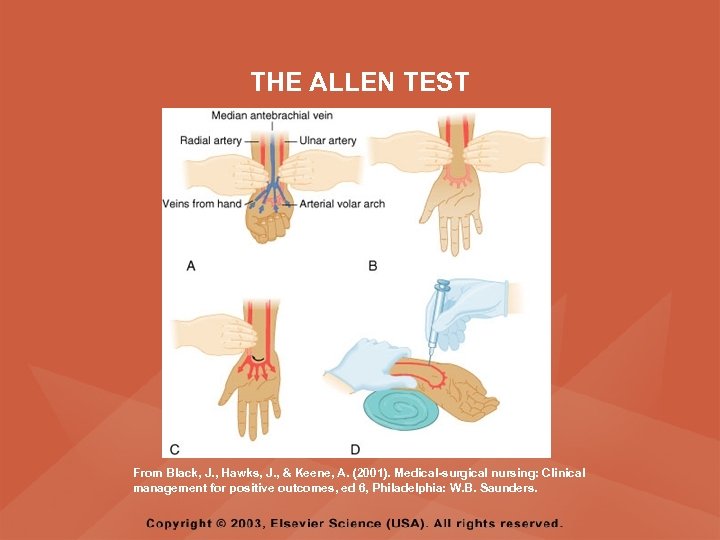 THE ALLEN TEST From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
THE ALLEN TEST From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders.
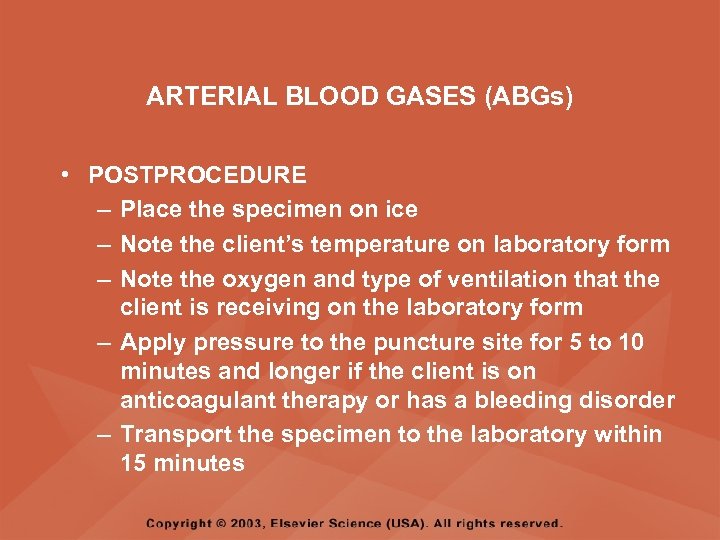 ARTERIAL BLOOD GASES (ABGs) • POSTPROCEDURE – Place the specimen on ice – Note the client’s temperature on laboratory form – Note the oxygen and type of ventilation that the client is receiving on the laboratory form – Apply pressure to the puncture site for 5 to 10 minutes and longer if the client is on anticoagulant therapy or has a bleeding disorder – Transport the specimen to the laboratory within 15 minutes
ARTERIAL BLOOD GASES (ABGs) • POSTPROCEDURE – Place the specimen on ice – Note the client’s temperature on laboratory form – Note the oxygen and type of ventilation that the client is receiving on the laboratory form – Apply pressure to the puncture site for 5 to 10 minutes and longer if the client is on anticoagulant therapy or has a bleeding disorder – Transport the specimen to the laboratory within 15 minutes
 PULSE OXIMETRY • DESCRIPTION – A noninvasive test that registers the oxygen saturation of the client’s hemoglobin – This arterial oxygen saturation (Sa. O 2) is recorded as a percentage – The normal value is 95 to 100%
PULSE OXIMETRY • DESCRIPTION – A noninvasive test that registers the oxygen saturation of the client’s hemoglobin – This arterial oxygen saturation (Sa. O 2) is recorded as a percentage – The normal value is 95 to 100%
 PULSE OXIMETRY • DESCRIPTION – After a hypoxic client uses up the readily available oxygen (measured as the arterial oxygen pressure, Pa. O 2, on arterial blood gas testing), the reserve oxygen, that oxygen attached to the hemoglobin (Sa. O 2), is drawn on to provide oxygen to the tissues – A pulse oximeter reading can alert the nurse to hypoxemia before clinical signs occur
PULSE OXIMETRY • DESCRIPTION – After a hypoxic client uses up the readily available oxygen (measured as the arterial oxygen pressure, Pa. O 2, on arterial blood gas testing), the reserve oxygen, that oxygen attached to the hemoglobin (Sa. O 2), is drawn on to provide oxygen to the tissues – A pulse oximeter reading can alert the nurse to hypoxemia before clinical signs occur
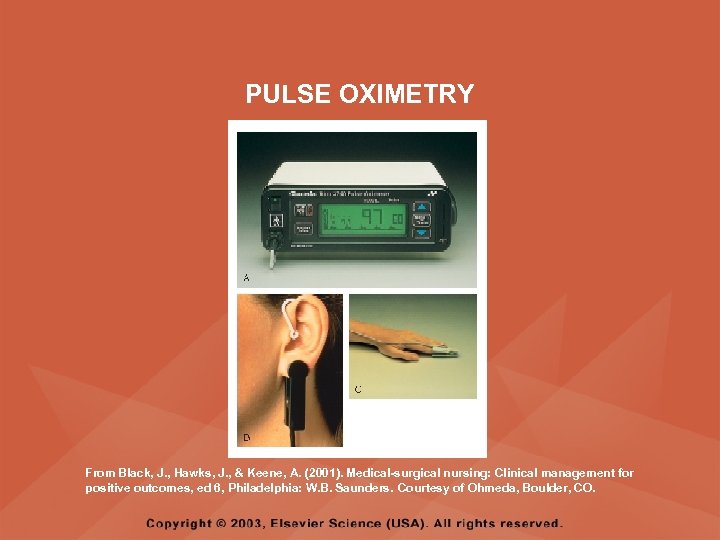 PULSE OXIMETRY From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders. Courtesy of Ohmeda, Boulder, CO.
PULSE OXIMETRY From Black, J. , Hawks, J. , & Keene, A. (2001). Medical-surgical nursing: Clinical management for positive outcomes, ed 6, Philadelphia: W. B. Saunders. Courtesy of Ohmeda, Boulder, CO.
 PULSE OXIMETRY • PROCEDURE – A sensor is placed on the client’s finger, toe, nose, earlobe, or forehead to measure oxygen saturation, which is then displayed on a monitor – Maintain the transducer at heart level – Do not select an extremity with an impediment to blood flow – Results lower than 91% necessitate immediate treatment – If the Sa. O 2 is below 85%, the body’s tissues have a difficult time becoming oxygenated; an Sa. O 2 of less than 70% is life-threatening
PULSE OXIMETRY • PROCEDURE – A sensor is placed on the client’s finger, toe, nose, earlobe, or forehead to measure oxygen saturation, which is then displayed on a monitor – Maintain the transducer at heart level – Do not select an extremity with an impediment to blood flow – Results lower than 91% necessitate immediate treatment – If the Sa. O 2 is below 85%, the body’s tissues have a difficult time becoming oxygenated; an Sa. O 2 of less than 70% is life-threatening


