68bda06e23c669521ee2bf152bf32e43.ppt
- Количество слайдов: 60
 Respiratory Failure in Children Daniel Sloniewsky, MD Associate Professor Division of Critical Care Department of Pediatrics Stony Brook University Hospital
Respiratory Failure in Children Daniel Sloniewsky, MD Associate Professor Division of Critical Care Department of Pediatrics Stony Brook University Hospital
 Definitions: Acute Respiratory Failure ARF is the inability of the respiratory system to deliver O 2 and remove CO 2 at a sufficient rate to meet the body’s metabolic demands Can be hypoxic or hypercarbic ABG abnormalities – Pa. CO 2 > 55 mm Hg (with low p. H) – Pa. O 2 < 60 mm Hg – Sa. O 2 < 90% (in absence of cyanotic CHD)
Definitions: Acute Respiratory Failure ARF is the inability of the respiratory system to deliver O 2 and remove CO 2 at a sufficient rate to meet the body’s metabolic demands Can be hypoxic or hypercarbic ABG abnormalities – Pa. CO 2 > 55 mm Hg (with low p. H) – Pa. O 2 < 60 mm Hg – Sa. O 2 < 90% (in absence of cyanotic CHD)
 Problems with Oxygenation Hypoxemia: Decrease in tissue O 2 delivery – Hypoxic Hypoxemia -- Lung Disease – Ischemic Hypoxemia -- Decreased Blood Flow -- DO 2 = O 2 content x Cardiac Output – Anemic Hypoxemia -- Decreased O 2 -Carrying Capacity -- O 2 Content = (1. 39 x Hg. B x Sa. O 2) + (0. 003)(Pa. O 2)
Problems with Oxygenation Hypoxemia: Decrease in tissue O 2 delivery – Hypoxic Hypoxemia -- Lung Disease – Ischemic Hypoxemia -- Decreased Blood Flow -- DO 2 = O 2 content x Cardiac Output – Anemic Hypoxemia -- Decreased O 2 -Carrying Capacity -- O 2 Content = (1. 39 x Hg. B x Sa. O 2) + (0. 003)(Pa. O 2)
 Hypoxic Hypoxemia: Where is the problem? FIO 2 (Ex. Altitude) Decreased Air Entry -- Sedation (Ex. Opioid Overdose) -- Respiratory Muscle Weakness (Ex. SMA) -- Airway Obstruction (Ex. Croup, Asthma, etc) V/Q Mismatches (Ex. Atelectasis, ARDS) Shunting (Ex. CHD, pulmonary hypertension) Diffusion Abnormalities (Ex. Pulmonary Fibrosis, ARDS)
Hypoxic Hypoxemia: Where is the problem? FIO 2 (Ex. Altitude) Decreased Air Entry -- Sedation (Ex. Opioid Overdose) -- Respiratory Muscle Weakness (Ex. SMA) -- Airway Obstruction (Ex. Croup, Asthma, etc) V/Q Mismatches (Ex. Atelectasis, ARDS) Shunting (Ex. CHD, pulmonary hypertension) Diffusion Abnormalities (Ex. Pulmonary Fibrosis, ARDS)
 Acute Respiratory Failure: Problems with Ventilation Hypercapnea (increased CO 2) can be seen with: 1. Increased Dead Space (areas not involved in gas exchange) (Ex. Asthma, Pulmonary HTN) 2. Decreased Alveolar Ventilation - Decreased Tidal Volume or Respiratory Rate (Ex. Coma, Overdose, MG, ARDS, etc) 3. Obstructed Airways (Ex. Asthma) 4. Increased CO 2 production (Ex. Burns, Overfeeding) CO 2 diffuses easily across alveolar-capillary membrane so diffusion problems usually do not cause hypercapnea
Acute Respiratory Failure: Problems with Ventilation Hypercapnea (increased CO 2) can be seen with: 1. Increased Dead Space (areas not involved in gas exchange) (Ex. Asthma, Pulmonary HTN) 2. Decreased Alveolar Ventilation - Decreased Tidal Volume or Respiratory Rate (Ex. Coma, Overdose, MG, ARDS, etc) 3. Obstructed Airways (Ex. Asthma) 4. Increased CO 2 production (Ex. Burns, Overfeeding) CO 2 diffuses easily across alveolar-capillary membrane so diffusion problems usually do not cause hypercapnea
 Acute Respiratory Failure: How to Diagnose Clinical Exam -- MOST IMPORTANT 1. Changes in RR and Breathing Effort: Question - Why do infants “tire out? ” 2. Changes in lung exam (stridor, wheeze, etc. ) 3. Cyanosis – definition? Flushing, tachycardia, HA, confusion – seen with hypercarbia Mental Status acute
Acute Respiratory Failure: How to Diagnose Clinical Exam -- MOST IMPORTANT 1. Changes in RR and Breathing Effort: Question - Why do infants “tire out? ” 2. Changes in lung exam (stridor, wheeze, etc. ) 3. Cyanosis – definition? Flushing, tachycardia, HA, confusion – seen with hypercarbia Mental Status acute
 Chronic Hypoxemia/Hypercarbia Clinical signs/lab evidence of chronic hypoxia: -- Clubbing – seen with chronic hypoxemia -- What might you see on abdominal exam? -- Labs: Polycythemia Lab evidence of hypercarbia
Chronic Hypoxemia/Hypercarbia Clinical signs/lab evidence of chronic hypoxia: -- Clubbing – seen with chronic hypoxemia -- What might you see on abdominal exam? -- Labs: Polycythemia Lab evidence of hypercarbia
 Hypoxic Hypoxemia: How to Diagnose Pulse oximetry – How does it work? What are its limitations? Arterial Blood Gas – What information does this provide that pulse-ox does not?
Hypoxic Hypoxemia: How to Diagnose Pulse oximetry – How does it work? What are its limitations? Arterial Blood Gas – What information does this provide that pulse-ox does not?
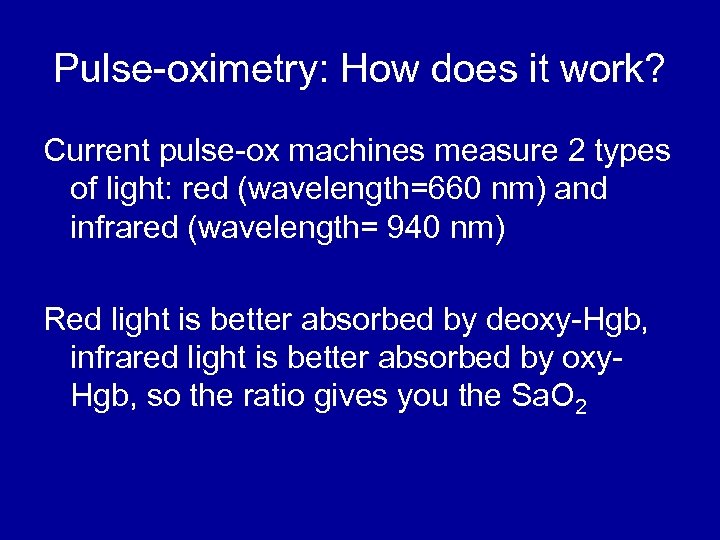 Pulse-oximetry: How does it work? Current pulse-ox machines measure 2 types of light: red (wavelength=660 nm) and infrared (wavelength= 940 nm) Red light is better absorbed by deoxy-Hgb, infrared light is better absorbed by oxy. Hgb, so the ratio gives you the Sa. O 2
Pulse-oximetry: How does it work? Current pulse-ox machines measure 2 types of light: red (wavelength=660 nm) and infrared (wavelength= 940 nm) Red light is better absorbed by deoxy-Hgb, infrared light is better absorbed by oxy. Hgb, so the ratio gives you the Sa. O 2
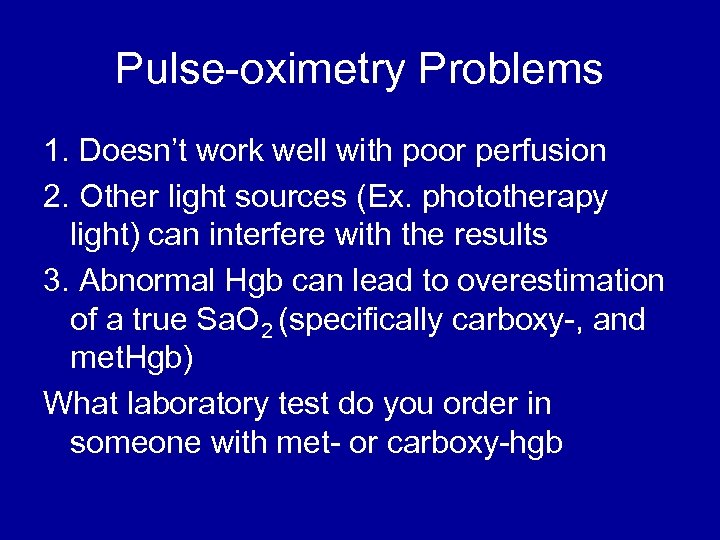 Pulse-oximetry Problems 1. Doesn’t work well with poor perfusion 2. Other light sources (Ex. phototherapy light) can interfere with the results 3. Abnormal Hgb can lead to overestimation of a true Sa. O 2 (specifically carboxy-, and met. Hgb) What laboratory test do you order in someone with met- or carboxy-hgb
Pulse-oximetry Problems 1. Doesn’t work well with poor perfusion 2. Other light sources (Ex. phototherapy light) can interfere with the results 3. Abnormal Hgb can lead to overestimation of a true Sa. O 2 (specifically carboxy-, and met. Hgb) What laboratory test do you order in someone with met- or carboxy-hgb
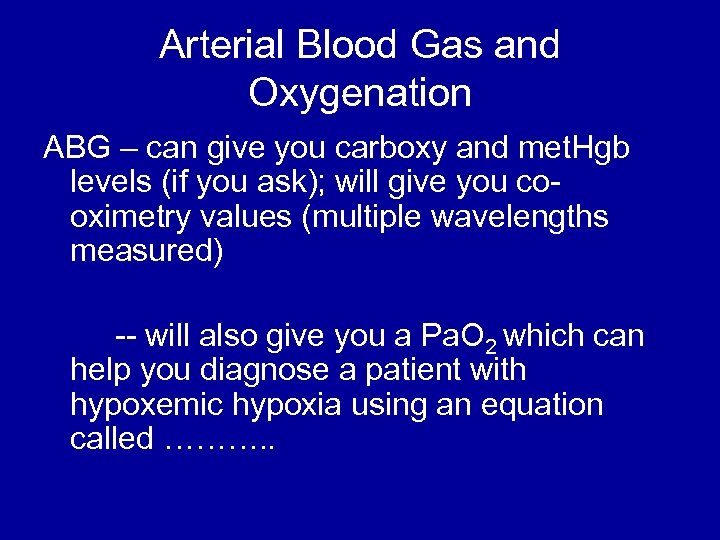 Arterial Blood Gas and Oxygenation ABG – can give you carboxy and met. Hgb levels (if you ask); will give you cooximetry values (multiple wavelengths measured) -- will also give you a Pa. O 2 which can help you diagnose a patient with hypoxemic hypoxia using an equation called ………. .
Arterial Blood Gas and Oxygenation ABG – can give you carboxy and met. Hgb levels (if you ask); will give you cooximetry values (multiple wavelengths measured) -- will also give you a Pa. O 2 which can help you diagnose a patient with hypoxemic hypoxia using an equation called ………. .
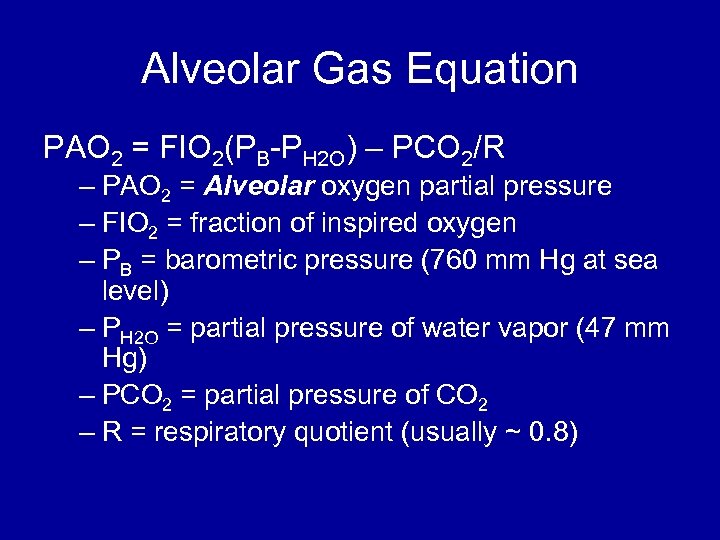 Alveolar Gas Equation PAO 2 = FIO 2(PB-PH 2 O) – PCO 2/R – PAO 2 = Alveolar oxygen partial pressure – FIO 2 = fraction of inspired oxygen – PB = barometric pressure (760 mm Hg at sea level) – PH 2 O = partial pressure of water vapor (47 mm Hg) – PCO 2 = partial pressure of CO 2 – R = respiratory quotient (usually ~ 0. 8)
Alveolar Gas Equation PAO 2 = FIO 2(PB-PH 2 O) – PCO 2/R – PAO 2 = Alveolar oxygen partial pressure – FIO 2 = fraction of inspired oxygen – PB = barometric pressure (760 mm Hg at sea level) – PH 2 O = partial pressure of water vapor (47 mm Hg) – PCO 2 = partial pressure of CO 2 – R = respiratory quotient (usually ~ 0. 8)
 Alveolar Gas Equation So at room air at sea level, your PAO 2 should be 100 On 100% FIO 2 at sea level, your PAO 2 should be 663 The difference between Alveolar (PAO 2) and arterial (Pa. O 2) oxygen is called the A-a gradient and should be less than 20; this will help you figure out if this is hypoxic hypoxemia and the degree of hypoxia
Alveolar Gas Equation So at room air at sea level, your PAO 2 should be 100 On 100% FIO 2 at sea level, your PAO 2 should be 663 The difference between Alveolar (PAO 2) and arterial (Pa. O 2) oxygen is called the A-a gradient and should be less than 20; this will help you figure out if this is hypoxic hypoxemia and the degree of hypoxia
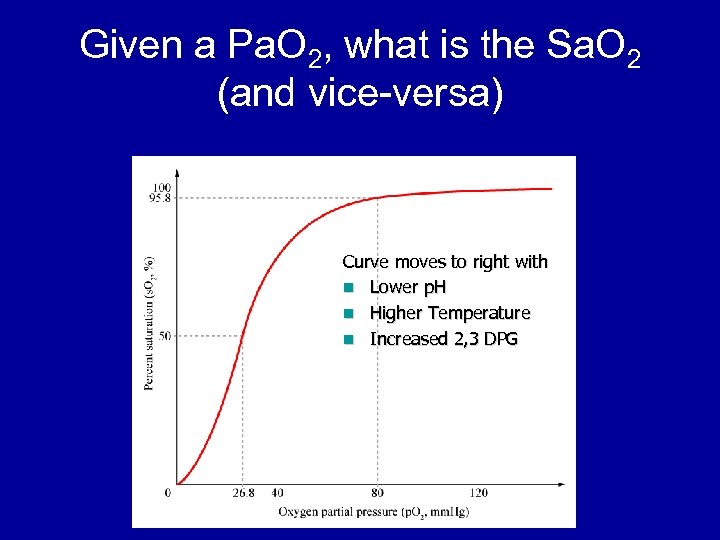 Given a Pa. O 2, what is the Sa. O 2 (and vice-versa) Curve moves to right with n Lower p. H n Higher Temperature n Increased 2, 3 DPG
Given a Pa. O 2, what is the Sa. O 2 (and vice-versa) Curve moves to right with n Lower p. H n Higher Temperature n Increased 2, 3 DPG
 Hypercarbic Respiratory Failure: Who cares about CO 2 and p. H? What makes you breathe? Primarily p. H (can be Pa. O 2 in some patients) What happens to you if you are too alkalotic or acidotic? Acidosis: AMS, impaired cardiac contractility, pulmonary vasoconstriction, metabolic abnormalities, etc. Alkalosis: tetany (sec. to decreased i. Ca), arrhythmias, etc. Does it matter what the source of the altered p. H is? Yes. For example: metabolic acidosis is worse for you than respiratory acidosis.
Hypercarbic Respiratory Failure: Who cares about CO 2 and p. H? What makes you breathe? Primarily p. H (can be Pa. O 2 in some patients) What happens to you if you are too alkalotic or acidotic? Acidosis: AMS, impaired cardiac contractility, pulmonary vasoconstriction, metabolic abnormalities, etc. Alkalosis: tetany (sec. to decreased i. Ca), arrhythmias, etc. Does it matter what the source of the altered p. H is? Yes. For example: metabolic acidosis is worse for you than respiratory acidosis.
 Arterial Blood Gas, p. H, and Ventilation p. H < 7. 35 with high CO 2: respiratory acidosis p. H > 7. 35 with high CO 2: compensated respiratory acidosis p. H < 7. 35 with low bicarb: metabolic acidosis p. H > 7. 35 with low bicarb: compensated metabolic acidosis What is a base deficit?
Arterial Blood Gas, p. H, and Ventilation p. H < 7. 35 with high CO 2: respiratory acidosis p. H > 7. 35 with high CO 2: compensated respiratory acidosis p. H < 7. 35 with low bicarb: metabolic acidosis p. H > 7. 35 with low bicarb: compensated metabolic acidosis What is a base deficit?
 Base Deficit Given a normal p. CO 2, how much base would be needed to correct the p. H. Ex. 7. 35/28/80/-15
Base Deficit Given a normal p. CO 2, how much base would be needed to correct the p. H. Ex. 7. 35/28/80/-15
 Arterial Blood Gas, p. H, and Ventilation p. H > 7. 45 with low CO 2: respiratory alkalosis p. H < 7. 45 with low CO 2: compensated respiratory alkalosis p. H > 7. 45 with high bicarb: metabolic alkalosis p. H < 7. 45 with high bicarb: compensated metabolic alkalosis
Arterial Blood Gas, p. H, and Ventilation p. H > 7. 45 with low CO 2: respiratory alkalosis p. H < 7. 45 with low CO 2: compensated respiratory alkalosis p. H > 7. 45 with high bicarb: metabolic alkalosis p. H < 7. 45 with high bicarb: compensated metabolic alkalosis
 How to Approach an ABG First – Is this an arterial or venous blood gas? Second - does the patient have an acidosis or an alkalosis – Look at the p. H Third, what is the primary problem – metabolic or respiratory – Look at the p. CO 2 – If the p. CO 2 change is in the opposite direction of the p. H change, the primary problem is respiratory – You never overcompensate
How to Approach an ABG First – Is this an arterial or venous blood gas? Second - does the patient have an acidosis or an alkalosis – Look at the p. H Third, what is the primary problem – metabolic or respiratory – Look at the p. CO 2 – If the p. CO 2 change is in the opposite direction of the p. H change, the primary problem is respiratory – You never overcompensate
 How to Approach an ABG Next, don’t forget to look at the effectiveness of oxygenation, (and look at the patient) – your patient may have a significantly increased work of breathing in order to maintain a “normal” blood gas – metabolic acidosis with a concomitant respiratory acidosis is concerning
How to Approach an ABG Next, don’t forget to look at the effectiveness of oxygenation, (and look at the patient) – your patient may have a significantly increased work of breathing in order to maintain a “normal” blood gas – metabolic acidosis with a concomitant respiratory acidosis is concerning
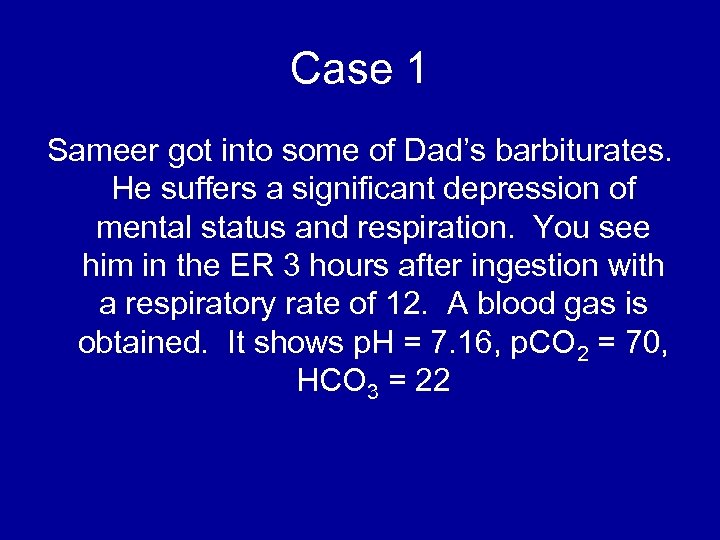 Case 1 Sameer got into some of Dad’s barbiturates. He suffers a significant depression of mental status and respiration. You see him in the ER 3 hours after ingestion with a respiratory rate of 12. A blood gas is obtained. It shows p. H = 7. 16, p. CO 2 = 70, HCO 3 = 22
Case 1 Sameer got into some of Dad’s barbiturates. He suffers a significant depression of mental status and respiration. You see him in the ER 3 hours after ingestion with a respiratory rate of 12. A blood gas is obtained. It shows p. H = 7. 16, p. CO 2 = 70, HCO 3 = 22
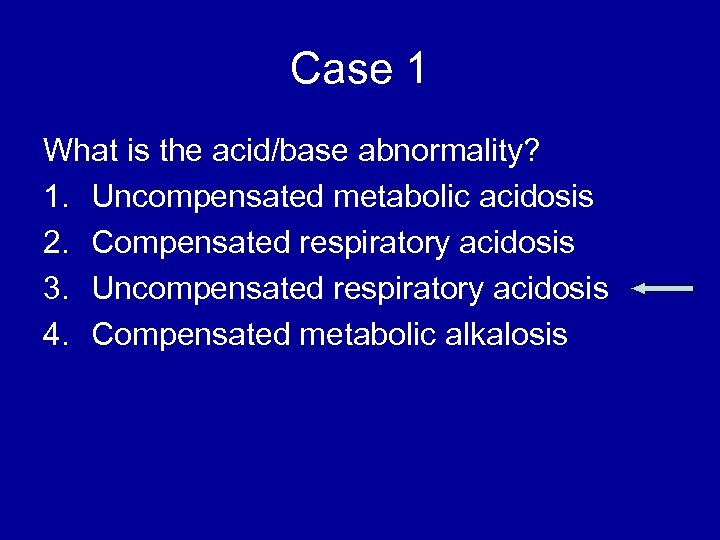 Case 1 What is the acid/base abnormality? 1. Uncompensated metabolic acidosis 2. Compensated respiratory acidosis 3. Uncompensated respiratory acidosis 4. Compensated metabolic alkalosis
Case 1 What is the acid/base abnormality? 1. Uncompensated metabolic acidosis 2. Compensated respiratory acidosis 3. Uncompensated respiratory acidosis 4. Compensated metabolic alkalosis
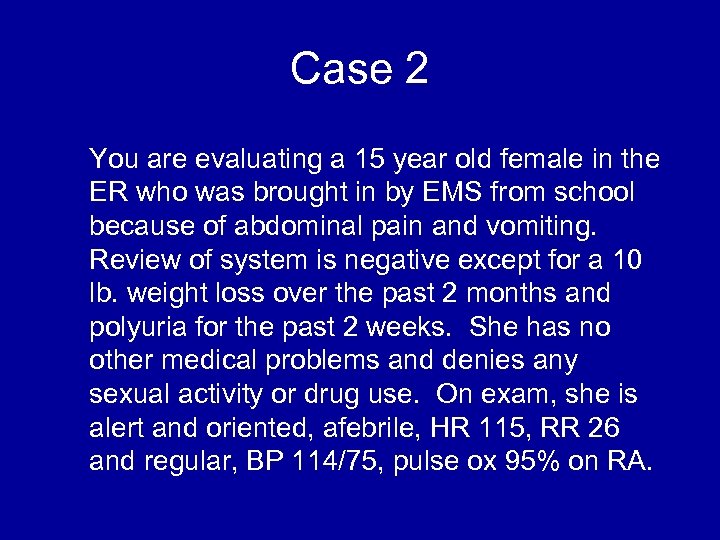 Case 2 You are evaluating a 15 year old female in the ER who was brought in by EMS from school because of abdominal pain and vomiting. Review of system is negative except for a 10 lb. weight loss over the past 2 months and polyuria for the past 2 weeks. She has no other medical problems and denies any sexual activity or drug use. On exam, she is alert and oriented, afebrile, HR 115, RR 26 and regular, BP 114/75, pulse ox 95% on RA.
Case 2 You are evaluating a 15 year old female in the ER who was brought in by EMS from school because of abdominal pain and vomiting. Review of system is negative except for a 10 lb. weight loss over the past 2 months and polyuria for the past 2 weeks. She has no other medical problems and denies any sexual activity or drug use. On exam, she is alert and oriented, afebrile, HR 115, RR 26 and regular, BP 114/75, pulse ox 95% on RA.
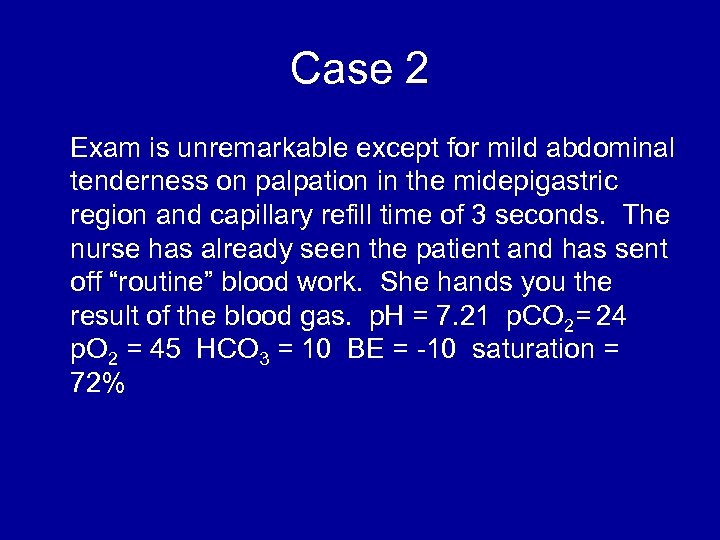 Case 2 Exam is unremarkable except for mild abdominal tenderness on palpation in the midepigastric region and capillary refill time of 3 seconds. The nurse has already seen the patient and has sent off “routine” blood work. She hands you the result of the blood gas. p. H = 7. 21 p. CO 2= 24 p. O 2 = 45 HCO 3 = 10 BE = -10 saturation = 72%
Case 2 Exam is unremarkable except for mild abdominal tenderness on palpation in the midepigastric region and capillary refill time of 3 seconds. The nurse has already seen the patient and has sent off “routine” blood work. She hands you the result of the blood gas. p. H = 7. 21 p. CO 2= 24 p. O 2 = 45 HCO 3 = 10 BE = -10 saturation = 72%
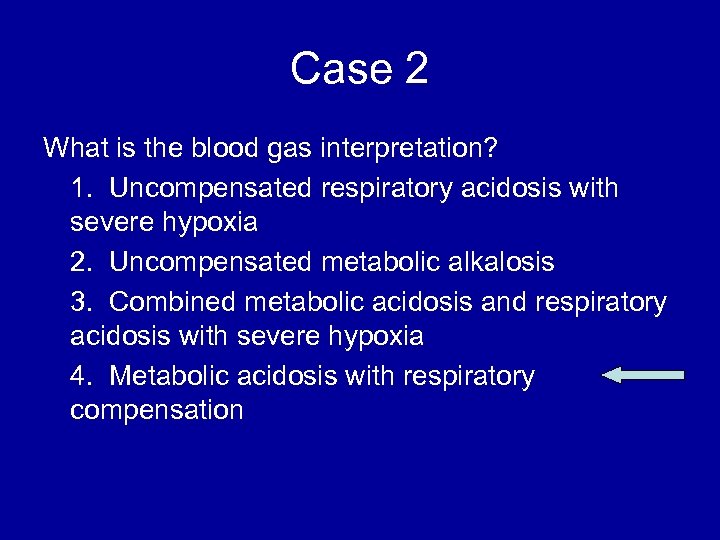 Case 2 What is the blood gas interpretation? 1. Uncompensated respiratory acidosis with severe hypoxia 2. Uncompensated metabolic alkalosis 3. Combined metabolic acidosis and respiratory acidosis with severe hypoxia 4. Metabolic acidosis with respiratory compensation
Case 2 What is the blood gas interpretation? 1. Uncompensated respiratory acidosis with severe hypoxia 2. Uncompensated metabolic alkalosis 3. Combined metabolic acidosis and respiratory acidosis with severe hypoxia 4. Metabolic acidosis with respiratory compensation
 Case 3 10 year old with history of ALL and neutropenia presents with tachypnea. He has no O 2 requirement but is breathing 30 – 40 times/minute. Lung exam (other than the tachypnea) is normal. CXR shows no infiltrate. An ABG is done: 7. 45/30/90/22 on room air. Does this patient need a bronchoscopy to diagnose his respiratory compromise? Why or why not?
Case 3 10 year old with history of ALL and neutropenia presents with tachypnea. He has no O 2 requirement but is breathing 30 – 40 times/minute. Lung exam (other than the tachypnea) is normal. CXR shows no infiltrate. An ABG is done: 7. 45/30/90/22 on room air. Does this patient need a bronchoscopy to diagnose his respiratory compromise? Why or why not?
 Case 3 Answer: No; This is a trick question because he doesn’t have respiratory compromise The patient is tachypneic for some other reason than acidosis, hypercarbia, or hypoxia (i. e. increased intracranial pressure, burgeoning sepsis, etc)
Case 3 Answer: No; This is a trick question because he doesn’t have respiratory compromise The patient is tachypneic for some other reason than acidosis, hypercarbia, or hypoxia (i. e. increased intracranial pressure, burgeoning sepsis, etc)
 Other Laboratory Findings in ARF CXR Abnormalities Complete Blood Count (look at WBC and Hgb, which may suggest chronic hypoxia) Electrolyte Abnormalities (look at bicarbonate)
Other Laboratory Findings in ARF CXR Abnormalities Complete Blood Count (look at WBC and Hgb, which may suggest chronic hypoxia) Electrolyte Abnormalities (look at bicarbonate)
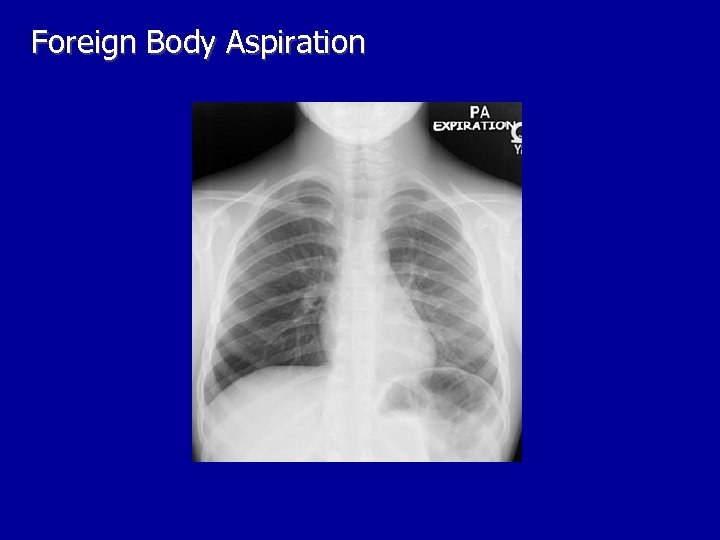 Foreign Body Aspiration
Foreign Body Aspiration
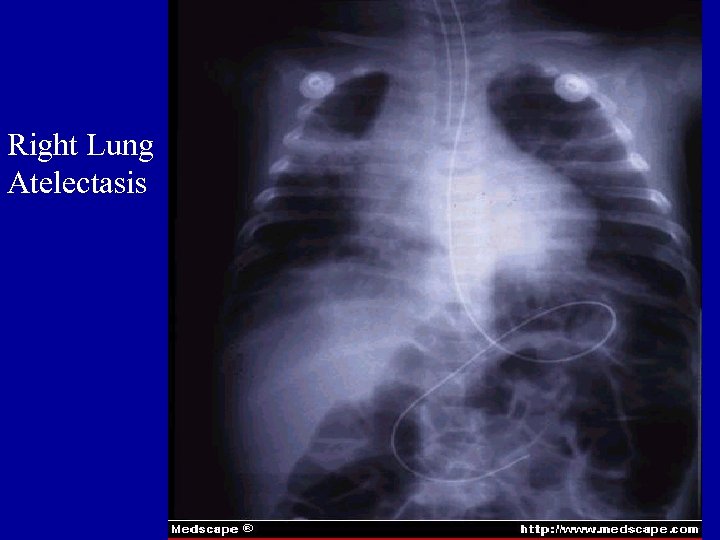 Right Lung Atelectasis
Right Lung Atelectasis
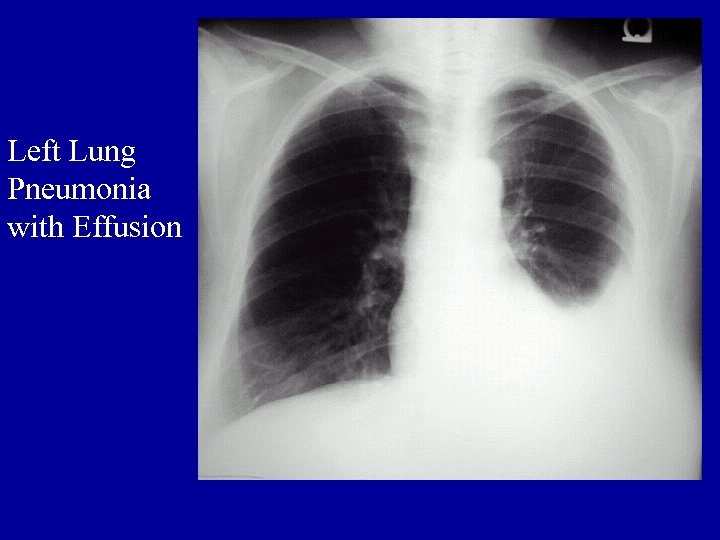 Left Lung Pneumonia with Effusion
Left Lung Pneumonia with Effusion
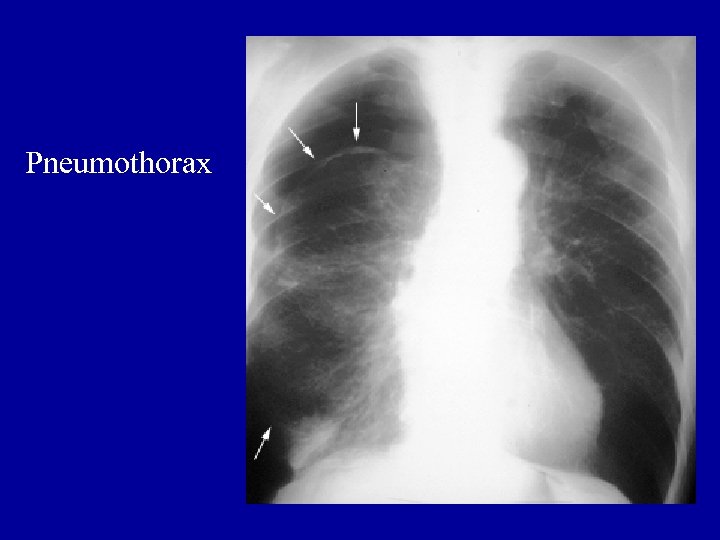 Pneumothorax
Pneumothorax
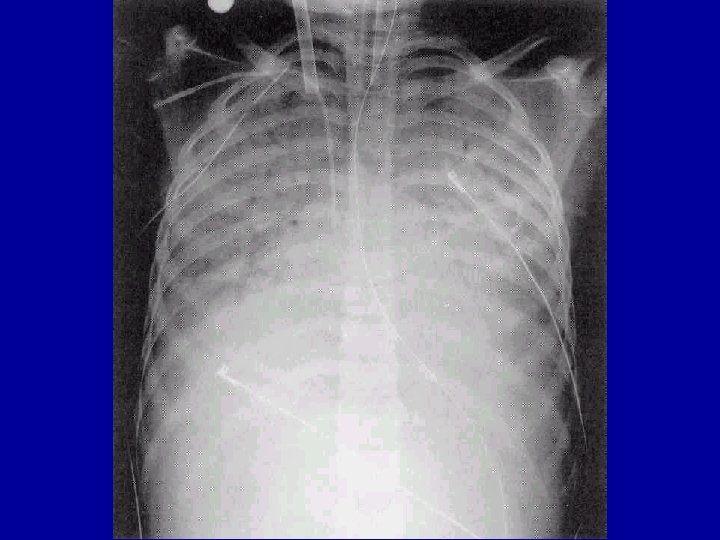
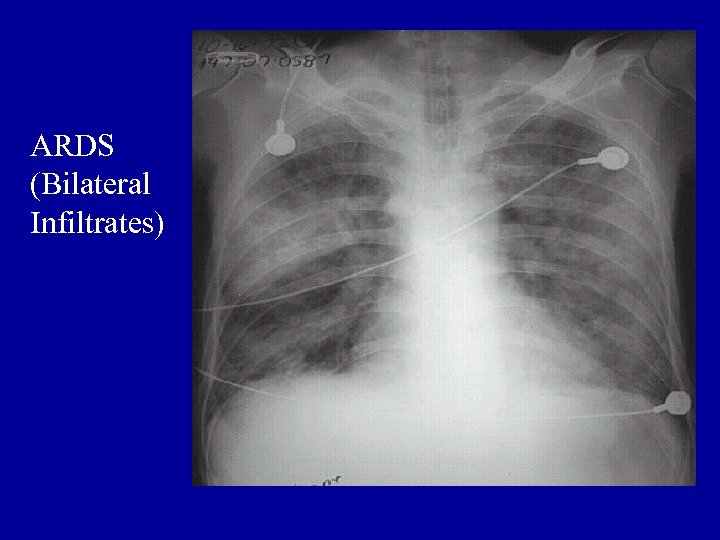 ARDS (Bilateral Infiltrates)
ARDS (Bilateral Infiltrates)
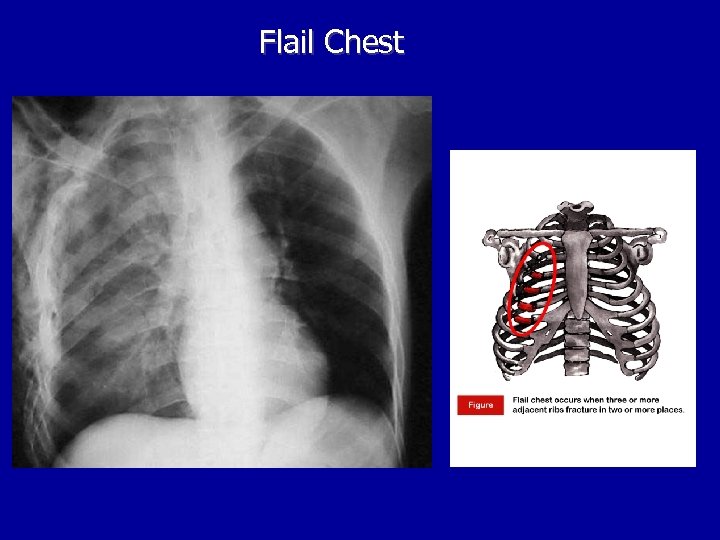 Flail Chest
Flail Chest
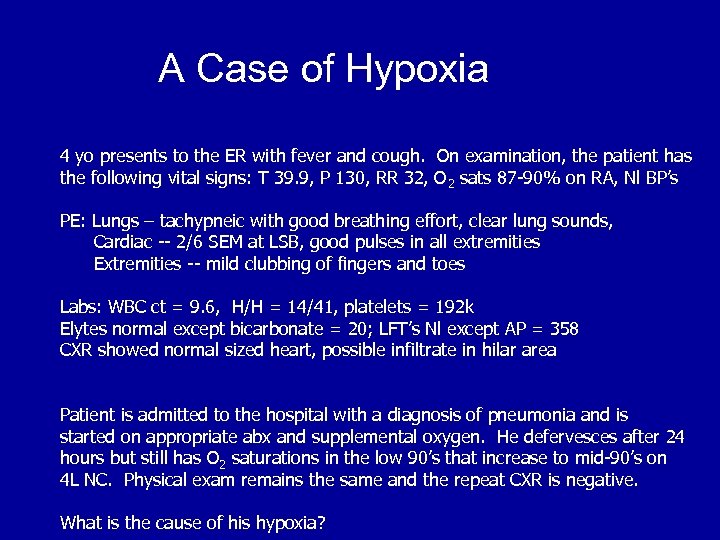 A Case of Hypoxia 4 yo presents to the ER with fever and cough. On examination, the patient has the following vital signs: T 39. 9, P 130, RR 32, O 2 sats 87 -90% on RA, Nl BP’s PE: Lungs – tachypneic with good breathing effort, clear lung sounds, Cardiac -- 2/6 SEM at LSB, good pulses in all extremities Extremities -- mild clubbing of fingers and toes Labs: WBC ct = 9. 6, H/H = 14/41, platelets = 192 k Elytes normal except bicarbonate = 20; LFT’s Nl except AP = 358 CXR showed normal sized heart, possible infiltrate in hilar area Patient is admitted to the hospital with a diagnosis of pneumonia and is started on appropriate abx and supplemental oxygen. He defervesces after 24 hours but still has O 2 saturations in the low 90’s that increase to mid-90’s on 4 L NC. Physical exam remains the same and the repeat CXR is negative. What is the cause of his hypoxia?
A Case of Hypoxia 4 yo presents to the ER with fever and cough. On examination, the patient has the following vital signs: T 39. 9, P 130, RR 32, O 2 sats 87 -90% on RA, Nl BP’s PE: Lungs – tachypneic with good breathing effort, clear lung sounds, Cardiac -- 2/6 SEM at LSB, good pulses in all extremities Extremities -- mild clubbing of fingers and toes Labs: WBC ct = 9. 6, H/H = 14/41, platelets = 192 k Elytes normal except bicarbonate = 20; LFT’s Nl except AP = 358 CXR showed normal sized heart, possible infiltrate in hilar area Patient is admitted to the hospital with a diagnosis of pneumonia and is started on appropriate abx and supplemental oxygen. He defervesces after 24 hours but still has O 2 saturations in the low 90’s that increase to mid-90’s on 4 L NC. Physical exam remains the same and the repeat CXR is negative. What is the cause of his hypoxia?
 Clinical Scenario Decreased O 2 Availability? No Decreased Air Entry? No V/Q Mismatches? Possible Shunt? Possible Diffusion Problems? Possible What lab test do you want to prove this?
Clinical Scenario Decreased O 2 Availability? No Decreased Air Entry? No V/Q Mismatches? Possible Shunt? Possible Diffusion Problems? Possible What lab test do you want to prove this?
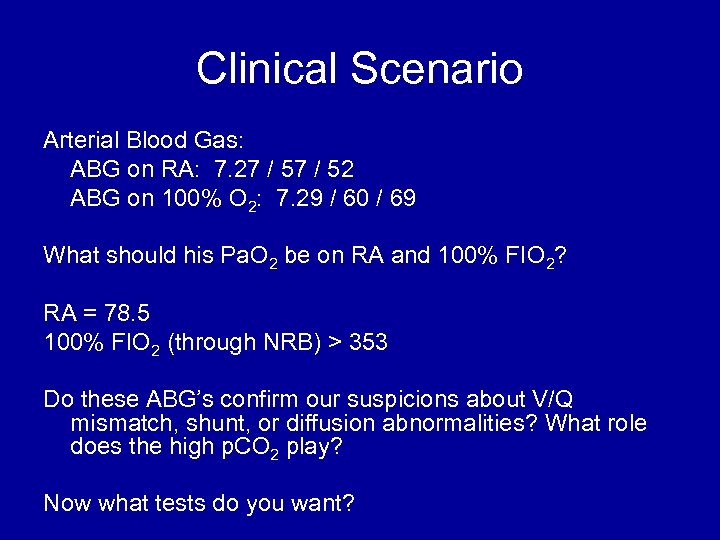 Clinical Scenario Arterial Blood Gas: ABG on RA: 7. 27 / 52 ABG on 100% O 2: 7. 29 / 60 / 69 What should his Pa. O 2 be on RA and 100% FIO 2? RA = 78. 5 100% FIO 2 (through NRB) > 353 Do these ABG’s confirm our suspicions about V/Q mismatch, shunt, or diffusion abnormalities? What role does the high p. CO 2 play? Now what tests do you want?
Clinical Scenario Arterial Blood Gas: ABG on RA: 7. 27 / 52 ABG on 100% O 2: 7. 29 / 60 / 69 What should his Pa. O 2 be on RA and 100% FIO 2? RA = 78. 5 100% FIO 2 (through NRB) > 353 Do these ABG’s confirm our suspicions about V/Q mismatch, shunt, or diffusion abnormalities? What role does the high p. CO 2 play? Now what tests do you want?
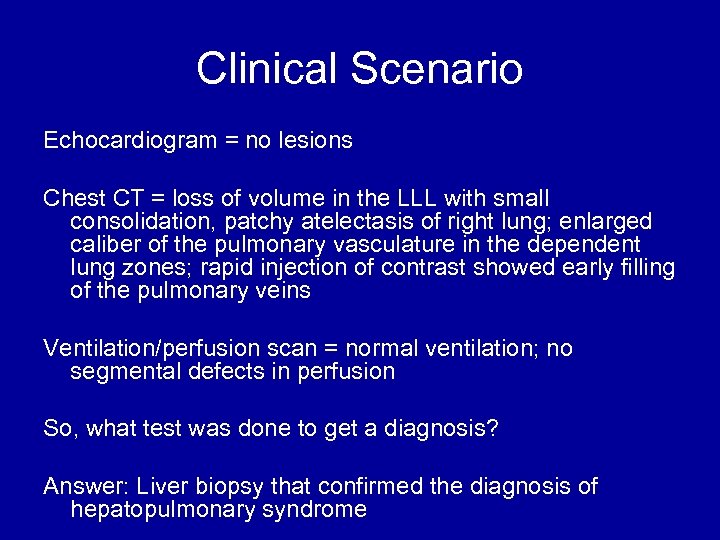 Clinical Scenario Echocardiogram = no lesions Chest CT = loss of volume in the LLL with small consolidation, patchy atelectasis of right lung; enlarged caliber of the pulmonary vasculature in the dependent lung zones; rapid injection of contrast showed early filling of the pulmonary veins Ventilation/perfusion scan = normal ventilation; no segmental defects in perfusion So, what test was done to get a diagnosis? Answer: Liver biopsy that confirmed the diagnosis of hepatopulmonary syndrome
Clinical Scenario Echocardiogram = no lesions Chest CT = loss of volume in the LLL with small consolidation, patchy atelectasis of right lung; enlarged caliber of the pulmonary vasculature in the dependent lung zones; rapid injection of contrast showed early filling of the pulmonary veins Ventilation/perfusion scan = normal ventilation; no segmental defects in perfusion So, what test was done to get a diagnosis? Answer: Liver biopsy that confirmed the diagnosis of hepatopulmonary syndrome
 ARF -- Treatment Monitoring – invasive (ABG, PAC) or noninvasive (pulseoximeter) Prevention – Encourage coughing, frequent position changes, reflux precautions, decompress abdomen, etc.
ARF -- Treatment Monitoring – invasive (ABG, PAC) or noninvasive (pulseoximeter) Prevention – Encourage coughing, frequent position changes, reflux precautions, decompress abdomen, etc.
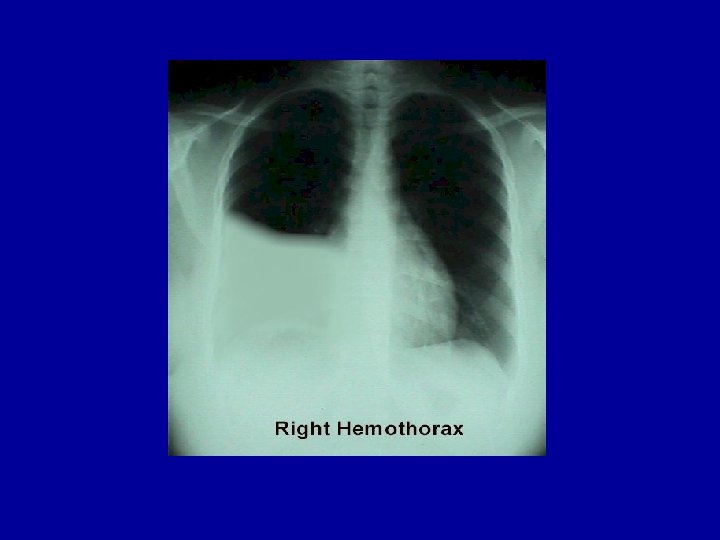
 ARF -- Treatment Surgical: Thoracostomy tubes Medications: – b-agonists – Anticholinergics – Anti-inflammatory agents (steroids, NSAIDS) – Surfactant – Nitric Oxide
ARF -- Treatment Surgical: Thoracostomy tubes Medications: – b-agonists – Anticholinergics – Anti-inflammatory agents (steroids, NSAIDS) – Surfactant – Nitric Oxide
 ARF -- Treatment O 2 Delivery Systems: Low vs. High Flow Low Flow: – Nasal Cannula: FIO 2 < 40% (1 L/min ~ 3%) – Blow-by O 2 High Flow: – Head Hood: Flow >10 l/min – Venturi Face Masks: FIO 2 ~ 50% – Nonrebreather Mask: FIO 2 ~ 80 -100% – Bag-Mask-Valve Units: FIO 2 ~ 100%
ARF -- Treatment O 2 Delivery Systems: Low vs. High Flow Low Flow: – Nasal Cannula: FIO 2 < 40% (1 L/min ~ 3%) – Blow-by O 2 High Flow: – Head Hood: Flow >10 l/min – Venturi Face Masks: FIO 2 ~ 50% – Nonrebreather Mask: FIO 2 ~ 80 -100% – Bag-Mask-Valve Units: FIO 2 ~ 100%
 ARF -- Treatment Continuous or Bilevel Positive Pressure (CPAP or BIPAP) -- applied through a tight -fitting mask Best applied in an awake, cooperative patient who is expected to improve in 4872 hours.
ARF -- Treatment Continuous or Bilevel Positive Pressure (CPAP or BIPAP) -- applied through a tight -fitting mask Best applied in an awake, cooperative patient who is expected to improve in 4872 hours.
 ARF – Treatment with Mechanical Ventilation Always Remember: Bag-mask ventilation is an effective method to oxygenate patients: use BMV if conditions are not ideal for intubation Mechanical Ventilation: Indications – – – Airway Protection Respiratory Failure Shock Treatment of Intracranial Hypertension Other (for procedures, pulmonary toilet, etc. )
ARF – Treatment with Mechanical Ventilation Always Remember: Bag-mask ventilation is an effective method to oxygenate patients: use BMV if conditions are not ideal for intubation Mechanical Ventilation: Indications – – – Airway Protection Respiratory Failure Shock Treatment of Intracranial Hypertension Other (for procedures, pulmonary toilet, etc. )
 Mechanical Ventilation: Modes AC – assist control – no spontaneous breaths – delivers full breath with any ventilator and patient initiated effort SIMV -- synchronized intermittent mandatory ventilation – ventilator breaths synchronized with patient’s own breaths – weaning mode
Mechanical Ventilation: Modes AC – assist control – no spontaneous breaths – delivers full breath with any ventilator and patient initiated effort SIMV -- synchronized intermittent mandatory ventilation – ventilator breaths synchronized with patient’s own breaths – weaning mode
 Mechanical Ventilation: Modes Pressure Ventilation (Control) – the size of the breath is determined by the pressure that is set – the tidal volume then depends on the lung compliance (it is the dependent variable) Volume Ventilation (Control) – the size of the breath is determined by the volume that is set – the pressure is the dependent variable
Mechanical Ventilation: Modes Pressure Ventilation (Control) – the size of the breath is determined by the pressure that is set – the tidal volume then depends on the lung compliance (it is the dependent variable) Volume Ventilation (Control) – the size of the breath is determined by the volume that is set – the pressure is the dependent variable
 Mechanical Ventilation: Goals Your goals for gas exchange when a patient is on a ventilator must not be so rigid as to cause further injury to the lung when trying to obtain them. Oxygenation is more important than ventilation You should try to keep the FIO 2 < 60%, the PIP < 35 -40 cm H 20, and the TV ~6 -8 cc/kg
Mechanical Ventilation: Goals Your goals for gas exchange when a patient is on a ventilator must not be so rigid as to cause further injury to the lung when trying to obtain them. Oxygenation is more important than ventilation You should try to keep the FIO 2 < 60%, the PIP < 35 -40 cm H 20, and the TV ~6 -8 cc/kg
 Mechanical Ventilation: Terminology Mean Airway Pressure (MAP): the average pressure over a respiratory cycle, measured at the proximal airway Peak Inspiratory Pressure (PIP): the maximum amount of pressure needed to deliver a breath Positive End Expiratory Pressure (PEEP): pressure applied at the end of exhalation I time: total time spent during inspiration
Mechanical Ventilation: Terminology Mean Airway Pressure (MAP): the average pressure over a respiratory cycle, measured at the proximal airway Peak Inspiratory Pressure (PIP): the maximum amount of pressure needed to deliver a breath Positive End Expiratory Pressure (PEEP): pressure applied at the end of exhalation I time: total time spent during inspiration
 Mechanical Ventilation: Terminology Tidal Volume: the size (volume) of the breath – goal ~ 6 -10 cc/kg Minute Ventilation: total volume of air inspired in one minute Compliance: relationship of volume to pressure – C = DV / DP
Mechanical Ventilation: Terminology Tidal Volume: the size (volume) of the breath – goal ~ 6 -10 cc/kg Minute Ventilation: total volume of air inspired in one minute Compliance: relationship of volume to pressure – C = DV / DP
 Mechanical Ventilation Oxygenation – determined by FIO 2 and Mean Airway Pressure – MAP is determined by PEEP, PIP, and inspiratory time (I time) Ventilation – determined by rate and TV – rate x TV = MV
Mechanical Ventilation Oxygenation – determined by FIO 2 and Mean Airway Pressure – MAP is determined by PEEP, PIP, and inspiratory time (I time) Ventilation – determined by rate and TV – rate x TV = MV
 Mechanical Ventilation -Supportive Care Fluids and electrolytes: permissive hypercapnia Nutrition HOB up at 30 o Suctioning/Chest PT
Mechanical Ventilation -Supportive Care Fluids and electrolytes: permissive hypercapnia Nutrition HOB up at 30 o Suctioning/Chest PT
 Mechanical Ventilation -Monitoring ABG/VBG Pulse-oximetry Et. CO 2 -- depends on reason for respiratory failure (not good with obstructive diseases like asthma or if there is a big air leak around the ETT)
Mechanical Ventilation -Monitoring ABG/VBG Pulse-oximetry Et. CO 2 -- depends on reason for respiratory failure (not good with obstructive diseases like asthma or if there is a big air leak around the ETT)
 Mechanical Ventilation -Weaning Is the problem solved? Is the patient awake? Is the patient NPO Is there an airleak around the ETT What are the mode of ventilation and settings?
Mechanical Ventilation -Weaning Is the problem solved? Is the patient awake? Is the patient NPO Is there an airleak around the ETT What are the mode of ventilation and settings?
 Mechanical Ventilation -Complications Oxygen Toxicity: keep O 2 < 60% Barotrauma/Volutrauma: Keep PIP < 35 -40 and TV < or = to 6 -8 cc/kg Atelectasis Ventilator Associated Pneumonia: keep HOB up at 30 o Fluid Retention Airway Trauma: uncuffed tubes when <6 yo
Mechanical Ventilation -Complications Oxygen Toxicity: keep O 2 < 60% Barotrauma/Volutrauma: Keep PIP < 35 -40 and TV < or = to 6 -8 cc/kg Atelectasis Ventilator Associated Pneumonia: keep HOB up at 30 o Fluid Retention Airway Trauma: uncuffed tubes when <6 yo
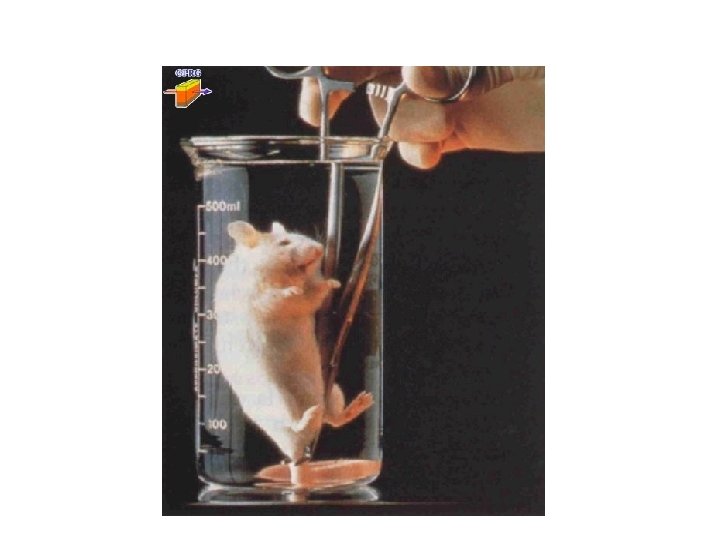
 ARF -- Alternate Therapies HFOV -- High Frequency Oscillatory Ventilation: used for problems with oxygenation, not very good for ventilation ECMO -- Extra-corporeal membrane oxygenation Liquid Ventilation – oxygen dissolves well in perfluorocarbons which can be used for gas exchange: only used in the lab
ARF -- Alternate Therapies HFOV -- High Frequency Oscillatory Ventilation: used for problems with oxygenation, not very good for ventilation ECMO -- Extra-corporeal membrane oxygenation Liquid Ventilation – oxygen dissolves well in perfluorocarbons which can be used for gas exchange: only used in the lab

 Summary When a patient is in respiratory failure, you must decide the primary gas exchange problem. While the clinical exam is the most important method of diagnosing someone with ARF, an ABG can help you with the diagnosis and can tell you the degree of hypoxia or hypercarbia
Summary When a patient is in respiratory failure, you must decide the primary gas exchange problem. While the clinical exam is the most important method of diagnosing someone with ARF, an ABG can help you with the diagnosis and can tell you the degree of hypoxia or hypercarbia
 Summary If hypoxia is the problem, going through the algorithm may help you decide which tests and therapies you need If hypercarbia is the problem, going through that algorithm may help you manage the patient A thoughtful, goal-directed approach to therapies must also be used in treating respiratory failure.
Summary If hypoxia is the problem, going through the algorithm may help you decide which tests and therapies you need If hypercarbia is the problem, going through that algorithm may help you manage the patient A thoughtful, goal-directed approach to therapies must also be used in treating respiratory failure.


