дыхательная недостаточность 15.02.2010_1.ppt
- Количество слайдов: 77
 Respiratory failure Docent of the department of internal medicine #2 Panevskaya G. N.
Respiratory failure Docent of the department of internal medicine #2 Panevskaya G. N.
 Respiration n Respiration is a gas exchange between the organism and its environment. Function of respiratory system is to transfer O 2 from atmosphere to blood and remove CO 2 from blood to maintain metabolism in organism. n It includes external and internal respiration.
Respiration n Respiration is a gas exchange between the organism and its environment. Function of respiratory system is to transfer O 2 from atmosphere to blood and remove CO 2 from blood to maintain metabolism in organism. n It includes external and internal respiration.
 Respiratory system includes CNS (medulla) n Peripheral nervous system (phrenic nerve) n Respiratory muscles ( diaphragm ) n Chest wall n Upper airway n Lungs n Bronchial tree n Alveoli n Pulmonary vasculature n
Respiratory system includes CNS (medulla) n Peripheral nervous system (phrenic nerve) n Respiratory muscles ( diaphragm ) n Chest wall n Upper airway n Lungs n Bronchial tree n Alveoli n Pulmonary vasculature n
 Internal respiration n Internal respiration is intracellular process of biological oxidation provided by enzymes, energy substances, etc
Internal respiration n Internal respiration is intracellular process of biological oxidation provided by enzymes, energy substances, etc
 Respiratory muscles n Diaphragm is the only inspiratory muscle that participates in a quiet respiration. n In hyperventilation mm. intercostales externi muscles, muscles of the shoulders and the neck (mm. scaleni, mm. sternocleidomastoidei)
Respiratory muscles n Diaphragm is the only inspiratory muscle that participates in a quiet respiration. n In hyperventilation mm. intercostales externi muscles, muscles of the shoulders and the neck (mm. scaleni, mm. sternocleidomastoidei)
 Respiratory muscles. Expiration Normally expiration is passive, it‘s provided by elasticity of the lungs and the chest wall. n In bronchial obstruction expiration is active, it requires support of the expiratory muscles. n The expiratory muscles: mm. intercostales interni, muscles of anterior abdominal wall, diaphragm n
Respiratory muscles. Expiration Normally expiration is passive, it‘s provided by elasticity of the lungs and the chest wall. n In bronchial obstruction expiration is active, it requires support of the expiratory muscles. n The expiratory muscles: mm. intercostales interni, muscles of anterior abdominal wall, diaphragm n
 Diffusive capacity of lungs n Transport of oxygen and CO 2 between the lungs and the cells performs through the alveolar- capillary membrane that consists of the endothelium of capillaries, the alveolar wall, the lung surfactant. It is characterized by diffusive capacity of the lungs (DLco).
Diffusive capacity of lungs n Transport of oxygen and CO 2 between the lungs and the cells performs through the alveolar- capillary membrane that consists of the endothelium of capillaries, the alveolar wall, the lung surfactant. It is characterized by diffusive capacity of the lungs (DLco).
 Nonrespiratory functions of lungs n Synthesis of the lung surfactant n Filtration cells aggregates, derivatives of fibrin degradation n Synthesis of prostacyclin that suppresses platelets aggregation and thromboxane А 2 n Participation in histamine and serotonin metabolism. 50% of serotonin is inactivated by system of monooxydase during the first passage through the lungs.
Nonrespiratory functions of lungs n Synthesis of the lung surfactant n Filtration cells aggregates, derivatives of fibrin degradation n Synthesis of prostacyclin that suppresses platelets aggregation and thromboxane А 2 n Participation in histamine and serotonin metabolism. 50% of serotonin is inactivated by system of monooxydase during the first passage through the lungs.
 Nonrespiratory functions of lungs Participation in kinin metabolism. 80% of bradykinin is inactivated in the lungs. n Synthesis of angiotensin II (endothelium of capillaries) from angiotensin I n Participation in catecholamine' metabolism predominantly of norepinephrine n Synthesis and destruction of prostaglandins, thromboxane and leukotrienes n
Nonrespiratory functions of lungs Participation in kinin metabolism. 80% of bradykinin is inactivated in the lungs. n Synthesis of angiotensin II (endothelium of capillaries) from angiotensin I n Participation in catecholamine' metabolism predominantly of norepinephrine n Synthesis and destruction of prostaglandins, thromboxane and leukotrienes n
 Structure of the respiratory system n n n The lungs have to provide a large surface area for gas exchange and the alveoli walls have to present minimal resistance to gas diffusion. About 10000 L of air are inhaled daily For maximum efficiency ventilation must be matched accurately to blood flow through the pulmonary capillary bed. There approximately 300 million alveoli in each lung. Their total surface area is 40 -80 m². The epithelium lining consists of type 1 and type 2 pneumocytes.
Structure of the respiratory system n n n The lungs have to provide a large surface area for gas exchange and the alveoli walls have to present minimal resistance to gas diffusion. About 10000 L of air are inhaled daily For maximum efficiency ventilation must be matched accurately to blood flow through the pulmonary capillary bed. There approximately 300 million alveoli in each lung. Their total surface area is 40 -80 m². The epithelium lining consists of type 1 and type 2 pneumocytes.
 Respiratory failure is inability of the lung to meet the metabolic demands of the body ( normally Ра 02 -90 -95 mm. Hg, Ра. С 02 - 35 -45 mm. Hg. This can be from failure of tissue oxygenation and/or failure of CO 2 homeostasis n Clinically a respiratory failure is defined as Pa. O 2 <60 mm Hg while breathing air, or a Pa. CO 2 >50 mm Hg. n
Respiratory failure is inability of the lung to meet the metabolic demands of the body ( normally Ра 02 -90 -95 mm. Hg, Ра. С 02 - 35 -45 mm. Hg. This can be from failure of tissue oxygenation and/or failure of CO 2 homeostasis n Clinically a respiratory failure is defined as Pa. O 2 <60 mm Hg while breathing air, or a Pa. CO 2 >50 mm Hg. n
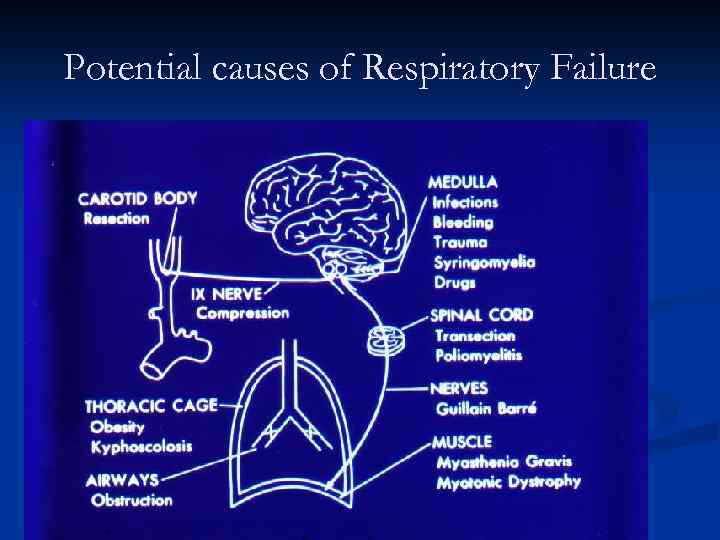 Potential causes of Respiratory Failure
Potential causes of Respiratory Failure
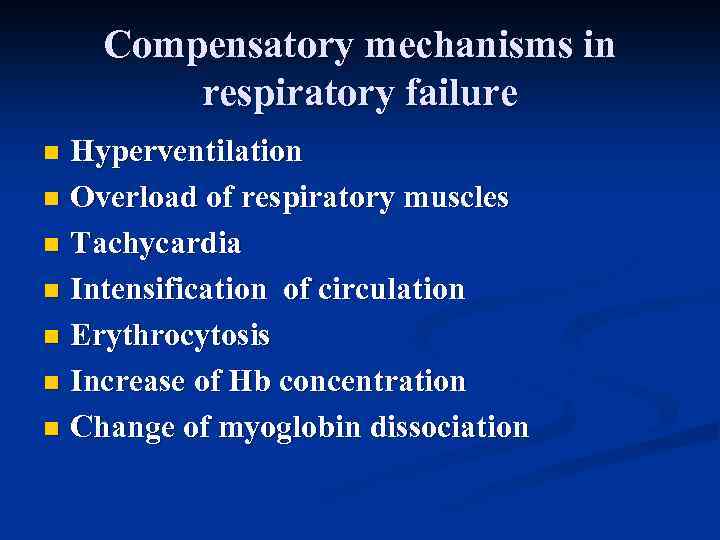 Compensatory mechanisms in respiratory failure Hyperventilation n Overload of respiratory muscles n Tachycardia n Intensification of circulation n Erythrocytosis n Increase of Hb concentration n Change of myoglobin dissociation n
Compensatory mechanisms in respiratory failure Hyperventilation n Overload of respiratory muscles n Tachycardia n Intensification of circulation n Erythrocytosis n Increase of Hb concentration n Change of myoglobin dissociation n
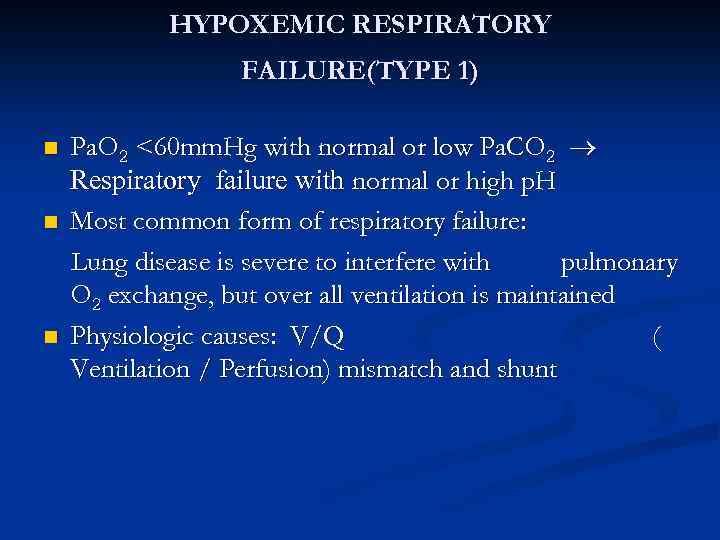 HYPOXEMIC RESPIRATORY FAILURE(TYPE 1) n n n Pa. O 2 <60 mm. Hg with normal or low Pa. CO 2 Respiratory failure with normal or high p. H Most common form of respiratory failure: Lung disease is severe to interfere with pulmonary O 2 exchange, but over all ventilation is maintained Physiologic causes: V/Q ( Ventilation / Perfusion) mismatch and shunt
HYPOXEMIC RESPIRATORY FAILURE(TYPE 1) n n n Pa. O 2 <60 mm. Hg with normal or low Pa. CO 2 Respiratory failure with normal or high p. H Most common form of respiratory failure: Lung disease is severe to interfere with pulmonary O 2 exchange, but over all ventilation is maintained Physiologic causes: V/Q ( Ventilation / Perfusion) mismatch and shunt
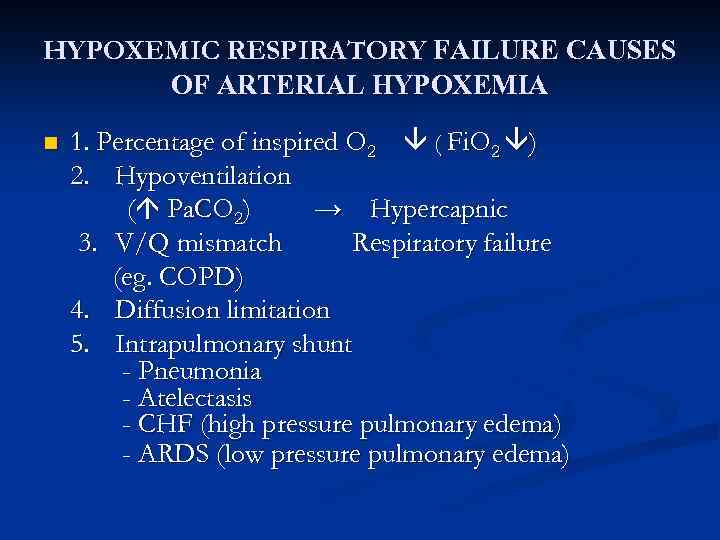 HYPOXEMIC RESPIRATORY FAILURE CAUSES OF ARTERIAL HYPOXEMIA n 1. Percentage of inspired O 2 ( Fi. O 2 ) 2. Hypoventilation ( Pa. CO 2) → Hypercapnic 3. V/Q mismatch Respiratory failure (eg. COPD) 4. Diffusion limitation 5. Intrapulmonary shunt - Pneumonia - Atelectasis - CHF (high pressure pulmonary edema) - ARDS (low pressure pulmonary edema)
HYPOXEMIC RESPIRATORY FAILURE CAUSES OF ARTERIAL HYPOXEMIA n 1. Percentage of inspired O 2 ( Fi. O 2 ) 2. Hypoventilation ( Pa. CO 2) → Hypercapnic 3. V/Q mismatch Respiratory failure (eg. COPD) 4. Diffusion limitation 5. Intrapulmonary shunt - Pneumonia - Atelectasis - CHF (high pressure pulmonary edema) - ARDS (low pressure pulmonary edema)
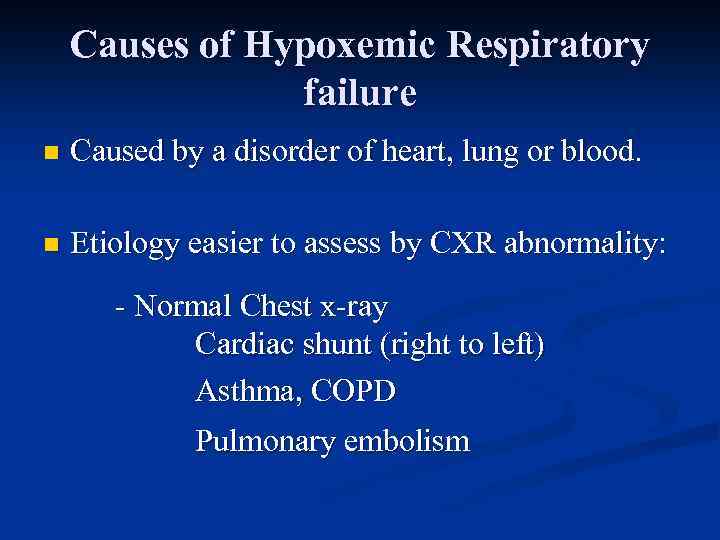 Causes of Hypoxemic Respiratory failure n Caused by a disorder of heart, lung or blood. n Etiology easier to assess by CXR abnormality: - Normal Chest x-ray Cardiac shunt (right to left) Asthma, COPD Pulmonary embolism
Causes of Hypoxemic Respiratory failure n Caused by a disorder of heart, lung or blood. n Etiology easier to assess by CXR abnormality: - Normal Chest x-ray Cardiac shunt (right to left) Asthma, COPD Pulmonary embolism
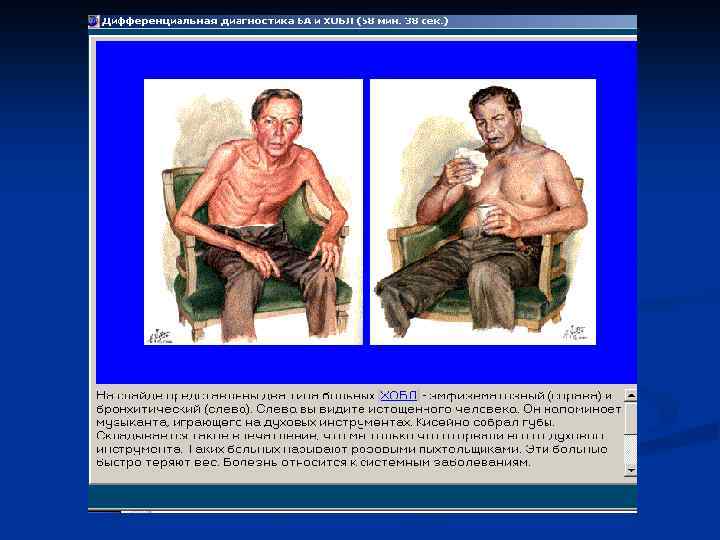
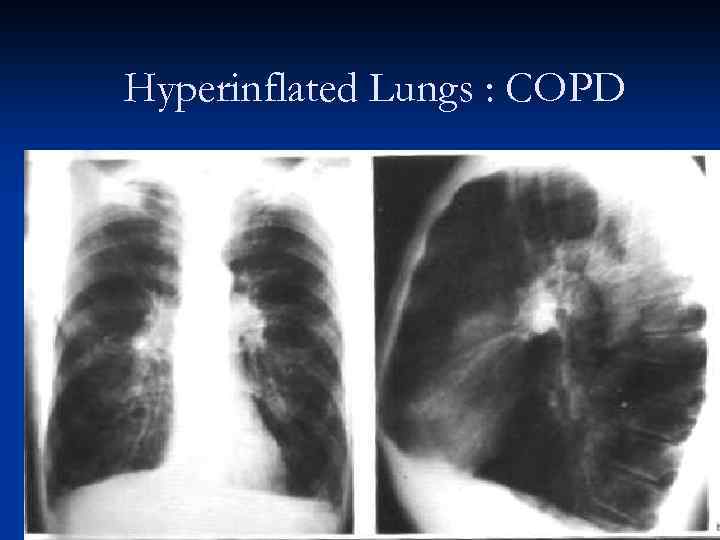 Hyperinflated Lungs : COPD
Hyperinflated Lungs : COPD
 Causes of Hypoxemic Respiratory failure (cont’d. ) • Focal infiltrates on CXR Atelectasis Pneumonia
Causes of Hypoxemic Respiratory failure (cont’d. ) • Focal infiltrates on CXR Atelectasis Pneumonia
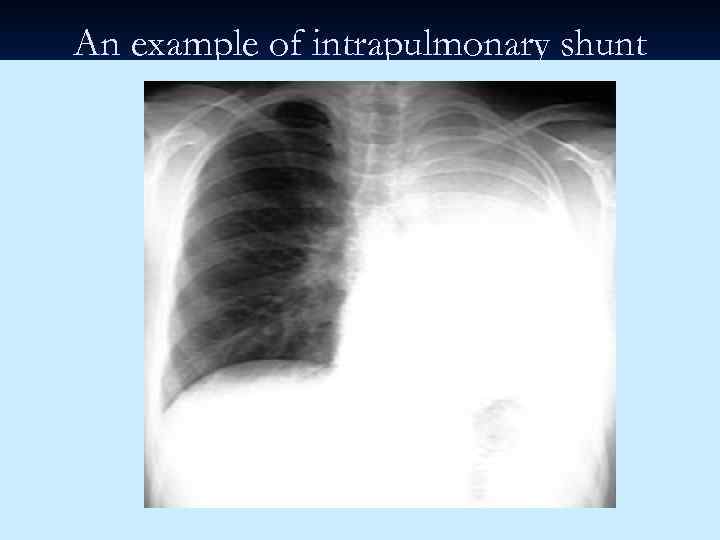 An example of intrapulmonary shunt
An example of intrapulmonary shunt
 Causes of Hypoxemic Respiratory Failure (cont’d. ) Diffuse infiltrates on CXR n Cardiogenic Pulmonary Edema n Non cardiogenic pulmonary edema (ARDS) n Interstitial pneumonitis or fibrosis n Infections
Causes of Hypoxemic Respiratory Failure (cont’d. ) Diffuse infiltrates on CXR n Cardiogenic Pulmonary Edema n Non cardiogenic pulmonary edema (ARDS) n Interstitial pneumonitis or fibrosis n Infections
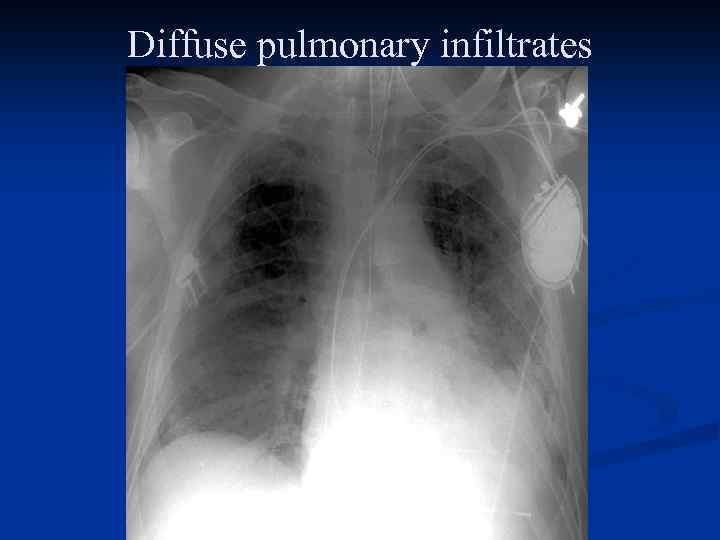 Diffuse pulmonary infiltrates
Diffuse pulmonary infiltrates
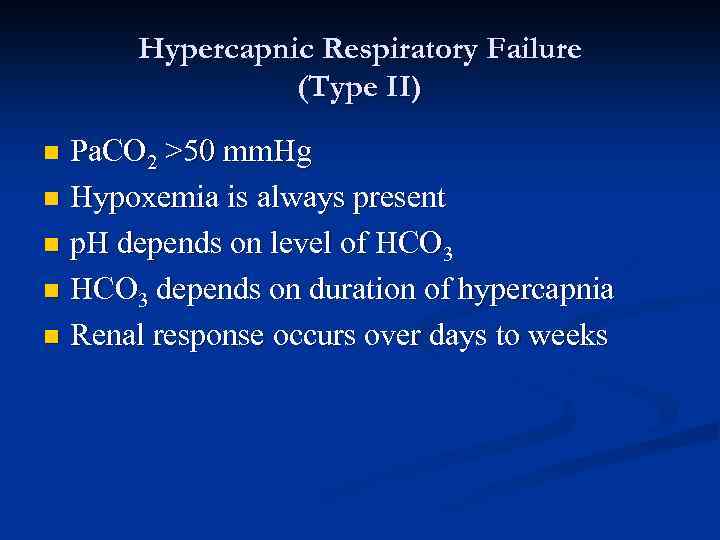 Hypercapnic Respiratory Failure (Type II) Pa. CO 2 >50 mm. Hg n Hypoxemia is always present n p. H depends on level of HCO 3 n HCO 3 depends on duration of hypercapnia n Renal response occurs over days to weeks n
Hypercapnic Respiratory Failure (Type II) Pa. CO 2 >50 mm. Hg n Hypoxemia is always present n p. H depends on level of HCO 3 n HCO 3 depends on duration of hypercapnia n Renal response occurs over days to weeks n
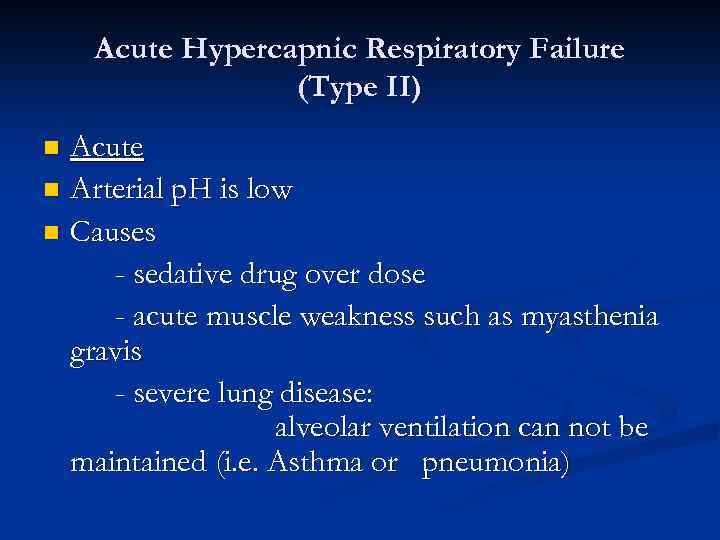 Acute Hypercapnic Respiratory Failure (Type II) Acute n Arterial p. H is low n Causes - sedative drug over dose - acute muscle weakness such as myasthenia gravis - severe lung disease: alveolar ventilation can not be maintained (i. e. Asthma or pneumonia) n
Acute Hypercapnic Respiratory Failure (Type II) Acute n Arterial p. H is low n Causes - sedative drug over dose - acute muscle weakness such as myasthenia gravis - severe lung disease: alveolar ventilation can not be maintained (i. e. Asthma or pneumonia) n
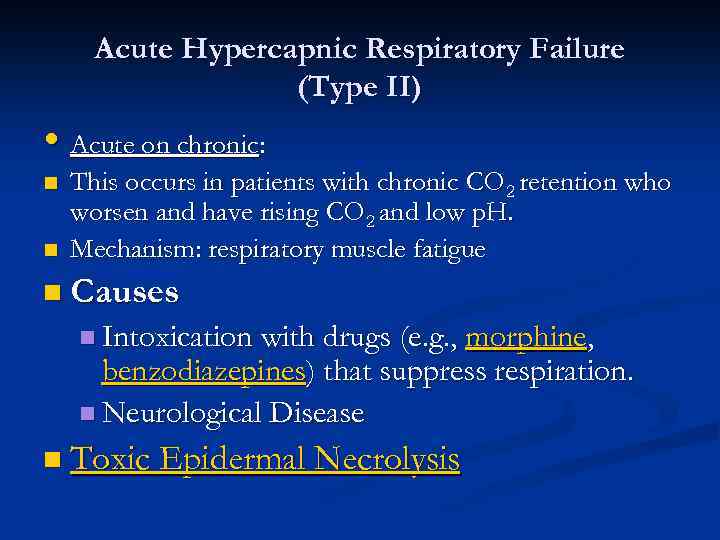 Acute Hypercapnic Respiratory Failure (Type II) • Acute on chronic: n n This occurs in patients with chronic CO 2 retention who worsen and have rising CO 2 and low p. H. Mechanism: respiratory muscle fatigue n Causes n Intoxication with drugs (e. g. , morphine, benzodiazepines) that suppress respiration. n Neurological Disease n Toxic Epidermal Necrolysis
Acute Hypercapnic Respiratory Failure (Type II) • Acute on chronic: n n This occurs in patients with chronic CO 2 retention who worsen and have rising CO 2 and low p. H. Mechanism: respiratory muscle fatigue n Causes n Intoxication with drugs (e. g. , morphine, benzodiazepines) that suppress respiration. n Neurological Disease n Toxic Epidermal Necrolysis
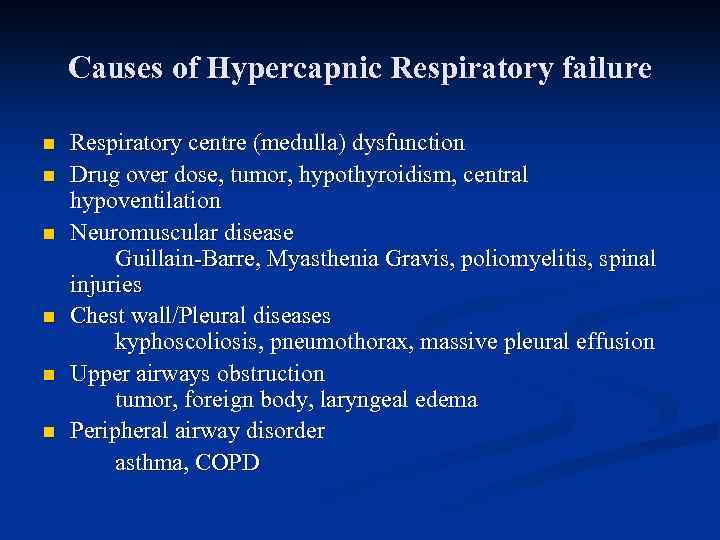 Causes of Hypercapnic Respiratory failure n n n Respiratory centre (medulla) dysfunction Drug over dose, tumor, hypothyroidism, central hypoventilation Neuromuscular disease Guillain-Barre, Myasthenia Gravis, poliomyelitis, spinal injuries Chest wall/Pleural diseases kyphoscoliosis, pneumothorax, massive pleural effusion Upper airways obstruction tumor, foreign body, laryngeal edema Peripheral airway disorder asthma, COPD
Causes of Hypercapnic Respiratory failure n n n Respiratory centre (medulla) dysfunction Drug over dose, tumor, hypothyroidism, central hypoventilation Neuromuscular disease Guillain-Barre, Myasthenia Gravis, poliomyelitis, spinal injuries Chest wall/Pleural diseases kyphoscoliosis, pneumothorax, massive pleural effusion Upper airways obstruction tumor, foreign body, laryngeal edema Peripheral airway disorder asthma, COPD
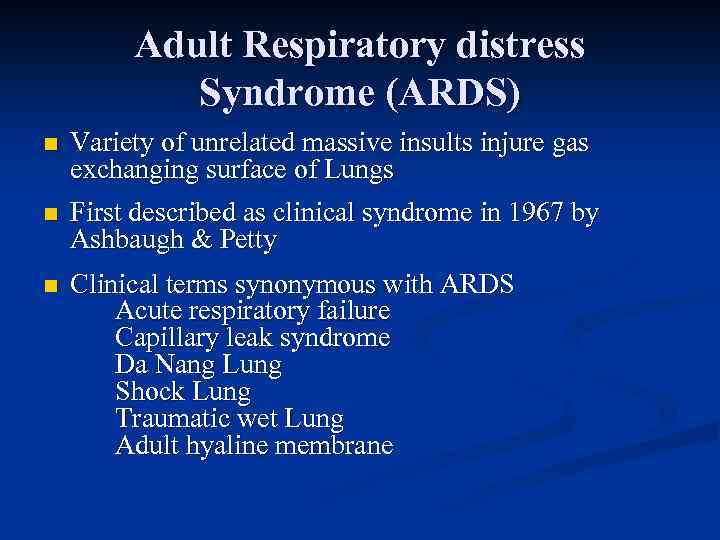 Adult Respiratory distress Syndrome (ARDS) n Variety of unrelated massive insults injure gas exchanging surface of Lungs n First described as clinical syndrome in 1967 by Ashbaugh & Petty n Clinical terms synonymous with ARDS Acute respiratory failure Capillary leak syndrome Da Nang Lung Shock Lung Traumatic wet Lung Adult hyaline membrane
Adult Respiratory distress Syndrome (ARDS) n Variety of unrelated massive insults injure gas exchanging surface of Lungs n First described as clinical syndrome in 1967 by Ashbaugh & Petty n Clinical terms synonymous with ARDS Acute respiratory failure Capillary leak syndrome Da Nang Lung Shock Lung Traumatic wet Lung Adult hyaline membrane
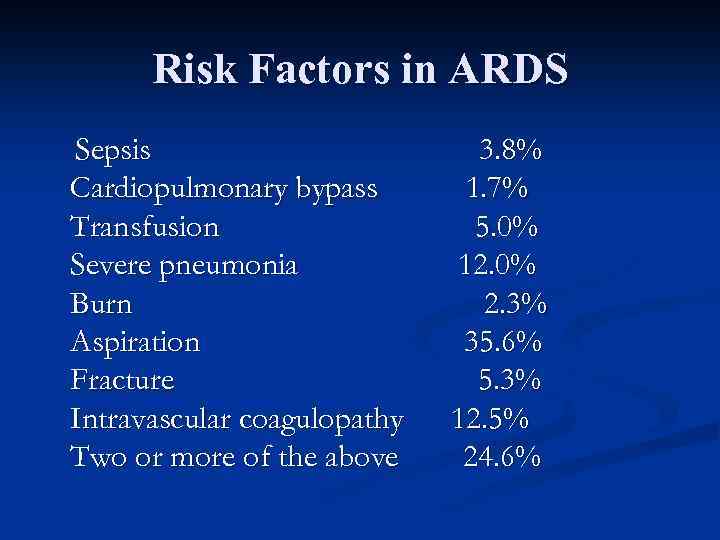 Risk Factors in ARDS Sepsis Cardiopulmonary bypass Transfusion Severe pneumonia Burn Aspiration Fracture Intravascular coagulopathy Two or more of the above 3. 8% 1. 7% 5. 0% 12. 0% 2. 3% 35. 6% 5. 3% 12. 5% 24. 6%
Risk Factors in ARDS Sepsis Cardiopulmonary bypass Transfusion Severe pneumonia Burn Aspiration Fracture Intravascular coagulopathy Two or more of the above 3. 8% 1. 7% 5. 0% 12. 0% 2. 3% 35. 6% 5. 3% 12. 5% 24. 6%
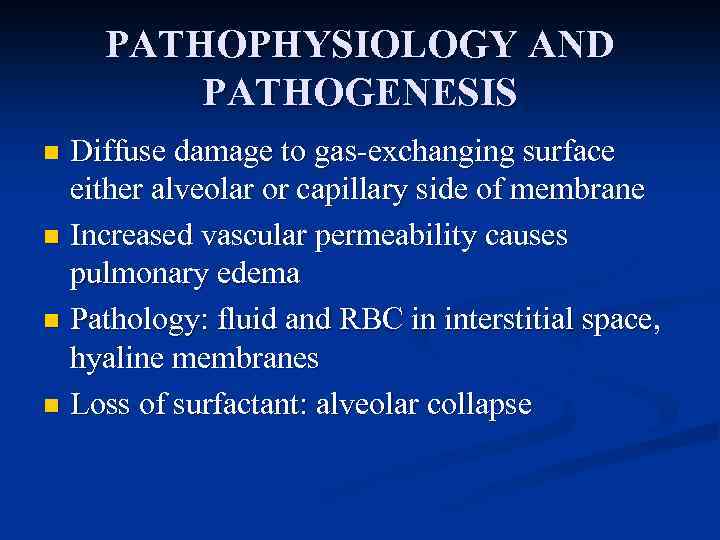 PATHOPHYSIOLOGY AND PATHOGENESIS Diffuse damage to gas-exchanging surface either alveolar or capillary side of membrane n Increased vascular permeability causes pulmonary edema n Pathology: fluid and RBC in interstitial space, hyaline membranes n Loss of surfactant: alveolar collapse n
PATHOPHYSIOLOGY AND PATHOGENESIS Diffuse damage to gas-exchanging surface either alveolar or capillary side of membrane n Increased vascular permeability causes pulmonary edema n Pathology: fluid and RBC in interstitial space, hyaline membranes n Loss of surfactant: alveolar collapse n
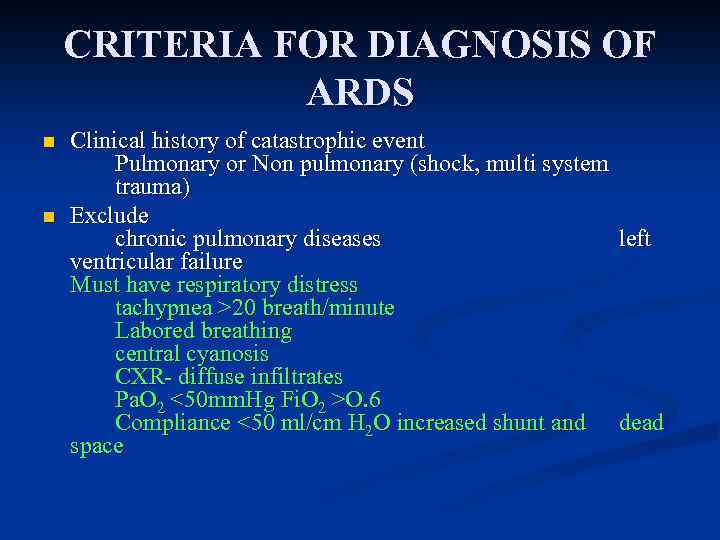 CRITERIA FOR DIAGNOSIS OF ARDS n n Clinical history of catastrophic event Pulmonary or Non pulmonary (shock, multi system trauma) Exclude chronic pulmonary diseases left ventricular failure Must have respiratory distress tachypnea >20 breath/minute Labored breathing central cyanosis CXR- diffuse infiltrates Pa. O 2 <50 mm. Hg Fi. O 2 >O. 6 Compliance <50 ml/cm H 2 O increased shunt and dead space
CRITERIA FOR DIAGNOSIS OF ARDS n n Clinical history of catastrophic event Pulmonary or Non pulmonary (shock, multi system trauma) Exclude chronic pulmonary diseases left ventricular failure Must have respiratory distress tachypnea >20 breath/minute Labored breathing central cyanosis CXR- diffuse infiltrates Pa. O 2 <50 mm. Hg Fi. O 2 >O. 6 Compliance <50 ml/cm H 2 O increased shunt and dead space
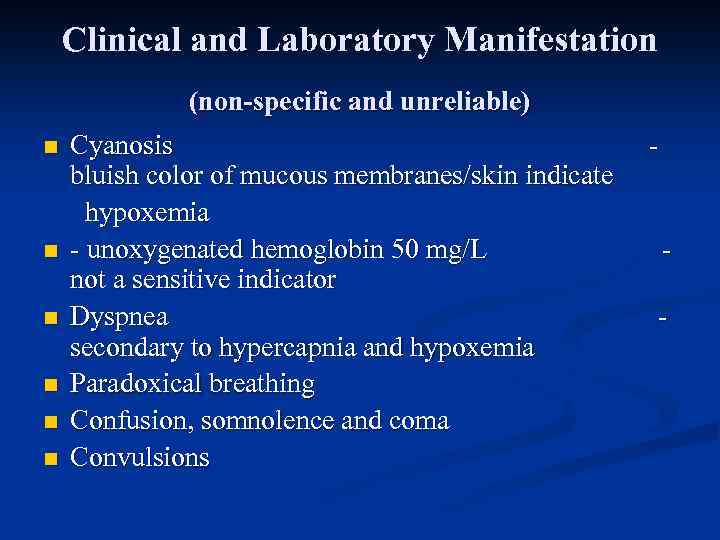 Clinical and Laboratory Manifestation (non-specific and unreliable) n n n Cyanosis bluish color of mucous membranes/skin indicate hypoxemia - unoxygenated hemoglobin 50 mg/L not a sensitive indicator Dyspnea secondary to hypercapnia and hypoxemia Paradoxical breathing Confusion, somnolence and coma Convulsions - -
Clinical and Laboratory Manifestation (non-specific and unreliable) n n n Cyanosis bluish color of mucous membranes/skin indicate hypoxemia - unoxygenated hemoglobin 50 mg/L not a sensitive indicator Dyspnea secondary to hypercapnia and hypoxemia Paradoxical breathing Confusion, somnolence and coma Convulsions - -
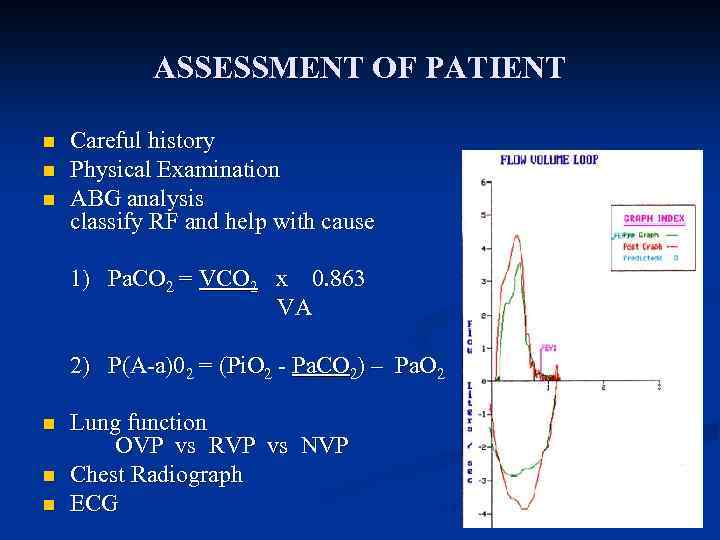 ASSESSMENT OF PATIENT n n n Careful history Physical Examination ABG analysis classify RF and help with cause - 1) Pa. CO 2 = VCO 2 x 0. 863 VA 2) P(A-a)02 = (Pi. O 2 - Pa. CO 2) – Pa. O 2 n n n Lung function OVP vs RVP vs NVP Chest Radiograph ECG R
ASSESSMENT OF PATIENT n n n Careful history Physical Examination ABG analysis classify RF and help with cause - 1) Pa. CO 2 = VCO 2 x 0. 863 VA 2) P(A-a)02 = (Pi. O 2 - Pa. CO 2) – Pa. O 2 n n n Lung function OVP vs RVP vs NVP Chest Radiograph ECG R
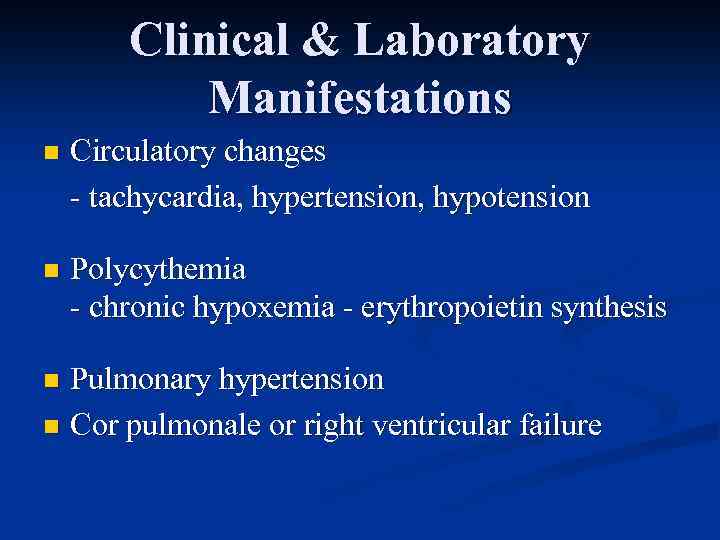 Clinical & Laboratory Manifestations n Circulatory changes - tachycardia, hypertension, hypotension n Polycythemia - chronic hypoxemia - erythropoietin synthesis Pulmonary hypertension n Cor pulmonale or right ventricular failure n
Clinical & Laboratory Manifestations n Circulatory changes - tachycardia, hypertension, hypotension n Polycythemia - chronic hypoxemia - erythropoietin synthesis Pulmonary hypertension n Cor pulmonale or right ventricular failure n
 Management of Respiratory Failure Principles Hypoxemia may cause death in RF n Primary objective is to reverse and prevent hypoxemia n Secondary objective is to control Pa. CO 2 and respiratory acidosis n Treatment of underlying disease n Patient’s CNS and CVS must be monitored and treated n
Management of Respiratory Failure Principles Hypoxemia may cause death in RF n Primary objective is to reverse and prevent hypoxemia n Secondary objective is to control Pa. CO 2 and respiratory acidosis n Treatment of underlying disease n Patient’s CNS and CVS must be monitored and treated n
 Oxygen Therapy n n n Supplemental O 2 therapy essential titration based on Sa. O 2, Pa. O 2 levels and Pa. CO 2 Goal is to prevent tissue hypoxia Tissue hypoxia occurs (normal Hb & C. O. ) - venous Pa. O 2 < 20 mm. Hg or Sa. O 2 < 40% - arterial Pa. O 2 < 38 mm. Hg or Sa. O 2 < 70% Increase arterial Pa. O 2 > 60 mm. Hg(Sa. O 2 > 90%) or venous Sa. O 2 > 60% O 2 dose either flow rate (L/min) or Fi. O 2 (%)
Oxygen Therapy n n n Supplemental O 2 therapy essential titration based on Sa. O 2, Pa. O 2 levels and Pa. CO 2 Goal is to prevent tissue hypoxia Tissue hypoxia occurs (normal Hb & C. O. ) - venous Pa. O 2 < 20 mm. Hg or Sa. O 2 < 40% - arterial Pa. O 2 < 38 mm. Hg or Sa. O 2 < 70% Increase arterial Pa. O 2 > 60 mm. Hg(Sa. O 2 > 90%) or venous Sa. O 2 > 60% O 2 dose either flow rate (L/min) or Fi. O 2 (%)
 Risks of Oxygen Therapy n n O 2 toxicity: very high levels(>1000 mm. Hg) CNS toxicity and seizures - lower levels (Fi. O 2 > 60%) and longer exposure: capillary damage, leak and pulmonary fibrosis - Pa. O 2 >150 can cause retrolental fibroplasia Fi. O 2 35 to 40% can be safely tolerated indefinitely CO 2 narcosis: Pa. CO 2 may increase severely to cause respiratory acidosis, somnolence and coma - Pa. CO 2 increase secondary to combination of a) abolition of hypoxic drive to breathe b) increase in dead space - -
Risks of Oxygen Therapy n n O 2 toxicity: very high levels(>1000 mm. Hg) CNS toxicity and seizures - lower levels (Fi. O 2 > 60%) and longer exposure: capillary damage, leak and pulmonary fibrosis - Pa. O 2 >150 can cause retrolental fibroplasia Fi. O 2 35 to 40% can be safely tolerated indefinitely CO 2 narcosis: Pa. CO 2 may increase severely to cause respiratory acidosis, somnolence and coma - Pa. CO 2 increase secondary to combination of a) abolition of hypoxic drive to breathe b) increase in dead space - -
 Oxygen Therapy
Oxygen Therapy
 Oxygen Therapy
Oxygen Therapy
 MECHANICAL VENTILATION n n Non invasive with a mask Invasive with an endobronchial tube MV can be volume or pressure cycled hypercapnia: MV increases alveolar ventilation and lowers Pa. CO 2, corrects p. H rests fatigues respiratory muscles For - For hypoxemia: O 2 therapy alone does not correct hypoxemia caused by shunt - Most common cause of shunt is fluid filled or collapsed alveoli (Pulmonary edema)
MECHANICAL VENTILATION n n Non invasive with a mask Invasive with an endobronchial tube MV can be volume or pressure cycled hypercapnia: MV increases alveolar ventilation and lowers Pa. CO 2, corrects p. H rests fatigues respiratory muscles For - For hypoxemia: O 2 therapy alone does not correct hypoxemia caused by shunt - Most common cause of shunt is fluid filled or collapsed alveoli (Pulmonary edema)

 POSITIVE END EXPIRATORY PRESSURE (PEEP) n n n PEEP increases the end expiratory lung volume (FRC) PEEP recruits collapsed alveoli and prevents recollapse FRC increases, therefore lung becomes more compliant Reversal of atelectasis diminishes intrapulmonary shunt Excessive PEEP has adverse effects decreased cardiac output barotrauma (pneumothorax, pneumomediastinum) increased physiologic dead space increased work of breathing
POSITIVE END EXPIRATORY PRESSURE (PEEP) n n n PEEP increases the end expiratory lung volume (FRC) PEEP recruits collapsed alveoli and prevents recollapse FRC increases, therefore lung becomes more compliant Reversal of atelectasis diminishes intrapulmonary shunt Excessive PEEP has adverse effects decreased cardiac output barotrauma (pneumothorax, pneumomediastinum) increased physiologic dead space increased work of breathing
 Chronic respiratory failure n Appears during some months or years n Onset is gradual. n It may be after acute respiratory failure
Chronic respiratory failure n Appears during some months or years n Onset is gradual. n It may be after acute respiratory failure
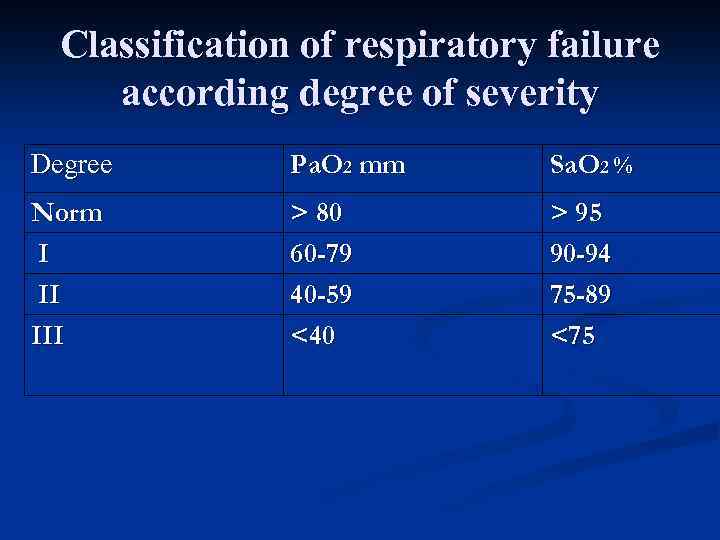 Classification of respiratory failure according degree of severity Degree Ра. О 2 mm Sa. O 2 % Norm I II III > 80 60 -79 40 -59 <40 > 95 90 -94 75 -89 <75
Classification of respiratory failure according degree of severity Degree Ра. О 2 mm Sa. O 2 % Norm I II III > 80 60 -79 40 -59 <40 > 95 90 -94 75 -89 <75
 Respiratory failure n Compensation n Decompensation
Respiratory failure n Compensation n Decompensation
 Affection of airways Bronchial asthma COPD Spasm of the larynx Foreign body Edema of the larynx Lung bleeding Mucoviscidosis Bronchiolitis Aspiration syndrome
Affection of airways Bronchial asthma COPD Spasm of the larynx Foreign body Edema of the larynx Lung bleeding Mucoviscidosis Bronchiolitis Aspiration syndrome
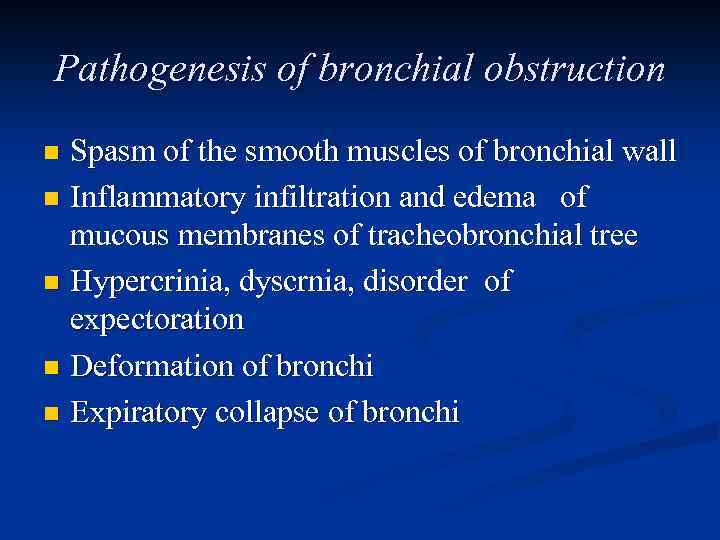 Pathogenesis of bronchial obstruction Spasm of the smooth muscles of bronchial wall n Inflammatory infiltration and edema of mucous membranes of tracheobronchial tree n Hypercrinia, dyscrnia, disorder of expectoration n Deformation of bronchi n Expiratory collapse of bronchi n
Pathogenesis of bronchial obstruction Spasm of the smooth muscles of bronchial wall n Inflammatory infiltration and edema of mucous membranes of tracheobronchial tree n Hypercrinia, dyscrnia, disorder of expectoration n Deformation of bronchi n Expiratory collapse of bronchi n
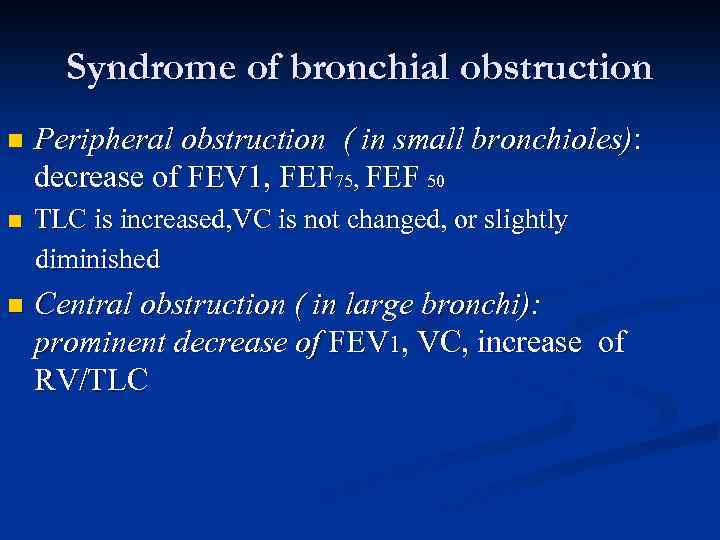 Syndrome of bronchial obstruction n Peripheral obstruction ( in small bronchioles): decrease of FEV 1, FEF 75, FEF 50 n TLC is increased, VC is not changed, or slightly diminished n Central obstruction ( in large bronchi): prominent decrease of FEV 1, VC, increase of RV/TLC
Syndrome of bronchial obstruction n Peripheral obstruction ( in small bronchioles): decrease of FEV 1, FEF 75, FEF 50 n TLC is increased, VC is not changed, or slightly diminished n Central obstruction ( in large bronchi): prominent decrease of FEV 1, VC, increase of RV/TLC
 Affection of lung parenchyma Pnemonia n Atelectasis n Pulmonary edema n Alveolitis n Pulmonary fibrosis n Sarcoidosis n
Affection of lung parenchyma Pnemonia n Atelectasis n Pulmonary edema n Alveolitis n Pulmonary fibrosis n Sarcoidosis n
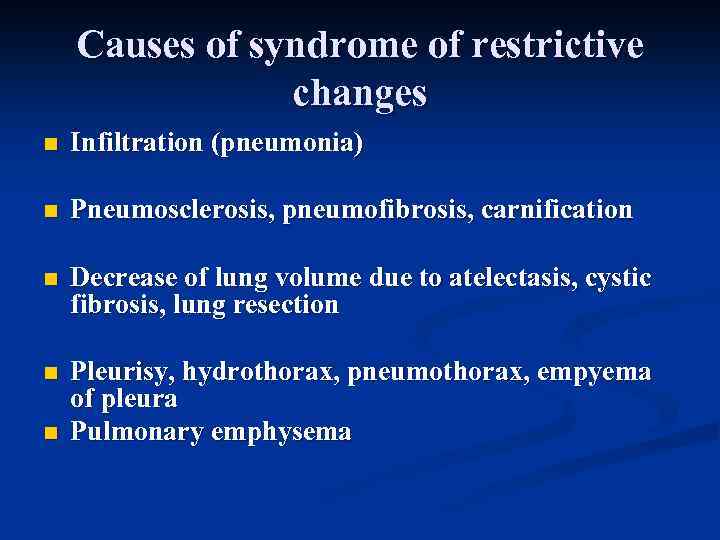 Causes of syndrome of restrictive changes n Infiltration (pneumonia) n Pneumosclerosis, pneumofibrosis, carnification n Decrease of lung volume due to atelectasis, cystic fibrosis, lung resection n Pleurisy, hydrothorax, pneumothorax, empyema of pleura Pulmonary emphysema n
Causes of syndrome of restrictive changes n Infiltration (pneumonia) n Pneumosclerosis, pneumofibrosis, carnification n Decrease of lung volume due to atelectasis, cystic fibrosis, lung resection n Pleurisy, hydrothorax, pneumothorax, empyema of pleura Pulmonary emphysema n
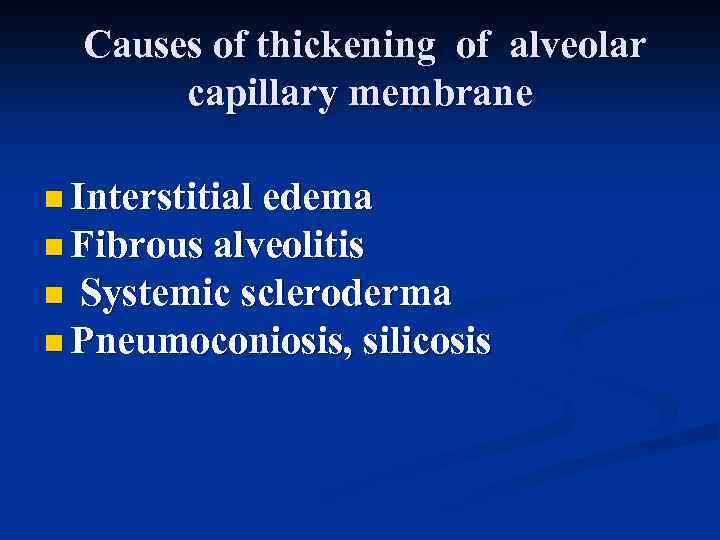 Causes of thickening of alveolar capillary membrane n Interstitial edema n Fibrous alveolitis Systemic scleroderma n Pneumoconiosis, silicosis n
Causes of thickening of alveolar capillary membrane n Interstitial edema n Fibrous alveolitis Systemic scleroderma n Pneumoconiosis, silicosis n
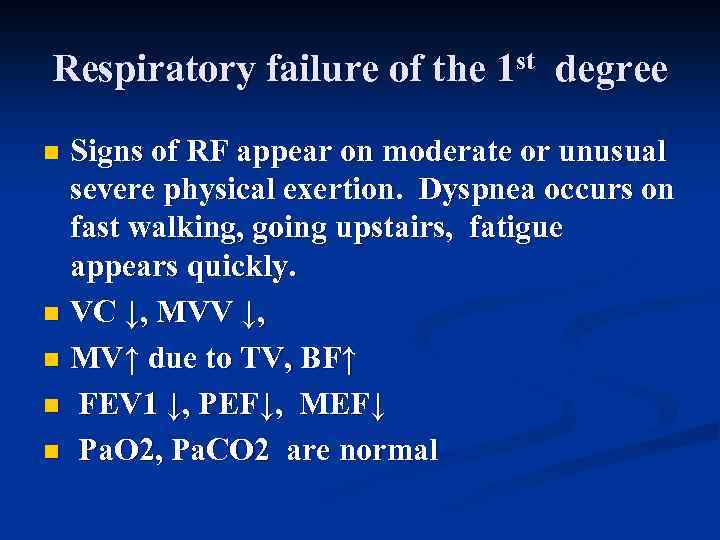 Respiratory failure of the 1 st degree Signs of RF appear on moderate or unusual severe physical exertion. Dyspnea occurs on fast walking, going upstairs, fatigue appears quickly. n VC ↓, МVV ↓, n MV↑ due to TV, BF↑ n FEV 1 ↓, PEF↓, МEF↓ n Ра. О 2, Ра. СО 2 are normal n
Respiratory failure of the 1 st degree Signs of RF appear on moderate or unusual severe physical exertion. Dyspnea occurs on fast walking, going upstairs, fatigue appears quickly. n VC ↓, МVV ↓, n MV↑ due to TV, BF↑ n FEV 1 ↓, PEF↓, МEF↓ n Ра. О 2, Ра. СО 2 are normal n
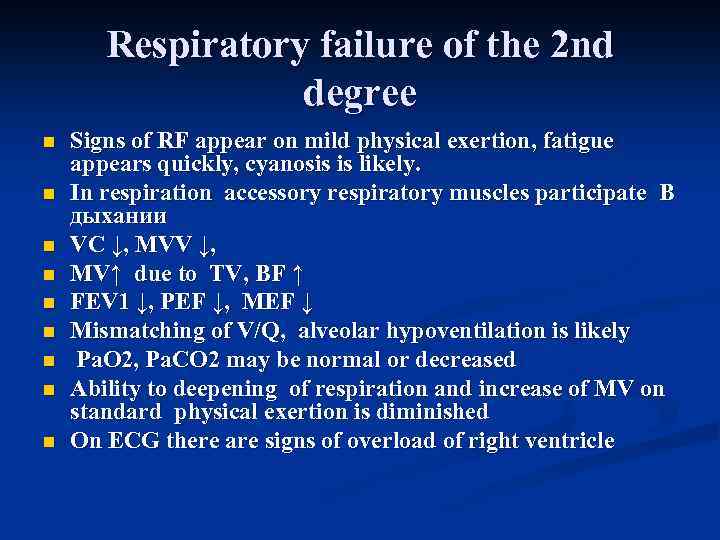 Respiratory failure of the 2 nd degree n n n n n Signs of RF appear on mild physical exertion, fatigue appears quickly, cyanosis is likely. In respiration accessory respiratory muscles participate В дыхании VC ↓, МVV ↓, MV↑ due to TV, BF ↑ FEV 1 ↓, PEF ↓, MEF ↓ Mismatching of V/Q, alveolar hypoventilation is likely Ра. О 2, Ра. СО 2 may be normal or decreased Ability to deepening of respiration and increase of MV on standard physical exertion is diminished On ECG there are signs of overload of right ventricle
Respiratory failure of the 2 nd degree n n n n n Signs of RF appear on mild physical exertion, fatigue appears quickly, cyanosis is likely. In respiration accessory respiratory muscles participate В дыхании VC ↓, МVV ↓, MV↑ due to TV, BF ↑ FEV 1 ↓, PEF ↓, MEF ↓ Mismatching of V/Q, alveolar hypoventilation is likely Ра. О 2, Ра. СО 2 may be normal or decreased Ability to deepening of respiration and increase of MV on standard physical exertion is diminished On ECG there are signs of overload of right ventricle
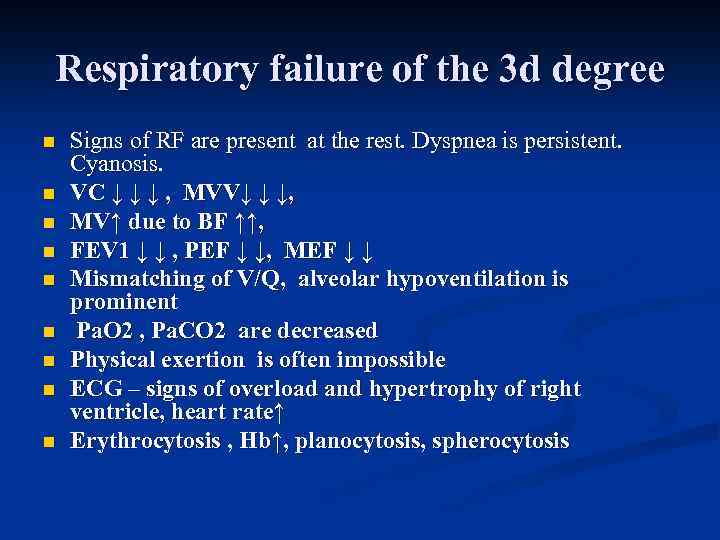 Respiratory failure of the 3 d degree n n n n n Signs of RF are present at the rest. Dyspnea is persistent. Cyanosis. VC ↓ ↓ ↓ , MVV↓ ↓ ↓, MV↑ due to BF ↑↑, FEV 1 ↓ ↓ , PEF ↓ ↓, MEF ↓ ↓ Mismatching of V/Q, alveolar hypoventilation is prominent Ра. О 2 , Ра. СО 2 are decreased Physical exertion is often impossible ECG – signs of overload and hypertrophy of right ventricle, heart rate↑ Erythrocytosis , Нb↑, planocytosis, spherocytosis
Respiratory failure of the 3 d degree n n n n n Signs of RF are present at the rest. Dyspnea is persistent. Cyanosis. VC ↓ ↓ ↓ , MVV↓ ↓ ↓, MV↑ due to BF ↑↑, FEV 1 ↓ ↓ , PEF ↓ ↓, MEF ↓ ↓ Mismatching of V/Q, alveolar hypoventilation is prominent Ра. О 2 , Ра. СО 2 are decreased Physical exertion is often impossible ECG – signs of overload and hypertrophy of right ventricle, heart rate↑ Erythrocytosis , Нb↑, planocytosis, spherocytosis
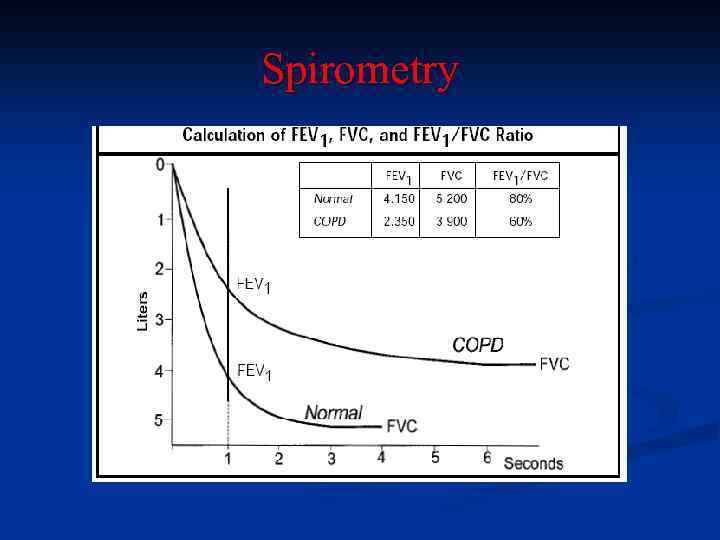 Spirometry
Spirometry
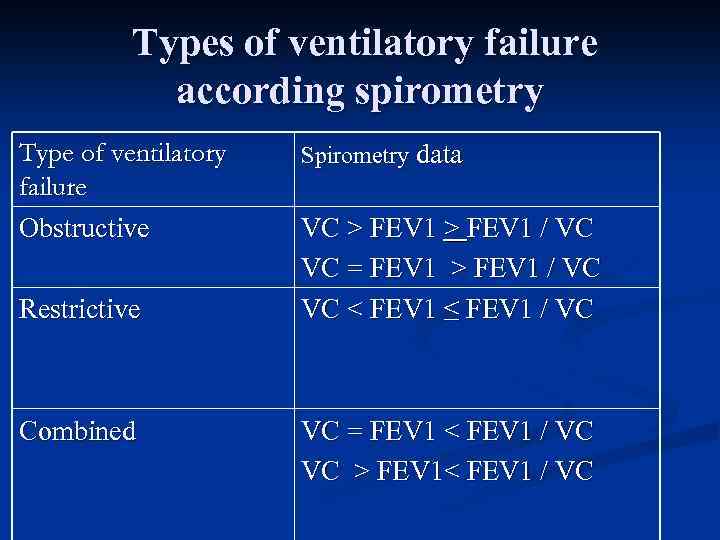 Types of ventilatory failure according spirometry Type of ventilatory failure Obstructive Restrictive Combined Spirometry data VC > FEV 1 / VC VC = FEV 1 > FEV 1 / VC VC < FEV 1 ≤ FEV 1 / VC VC = FEV 1 < FEV 1 / VC VC > FEV 1< FEV 1 / VC
Types of ventilatory failure according spirometry Type of ventilatory failure Obstructive Restrictive Combined Spirometry data VC > FEV 1 / VC VC = FEV 1 > FEV 1 / VC VC < FEV 1 ≤ FEV 1 / VC VC = FEV 1 < FEV 1 / VC VC > FEV 1< FEV 1 / VC
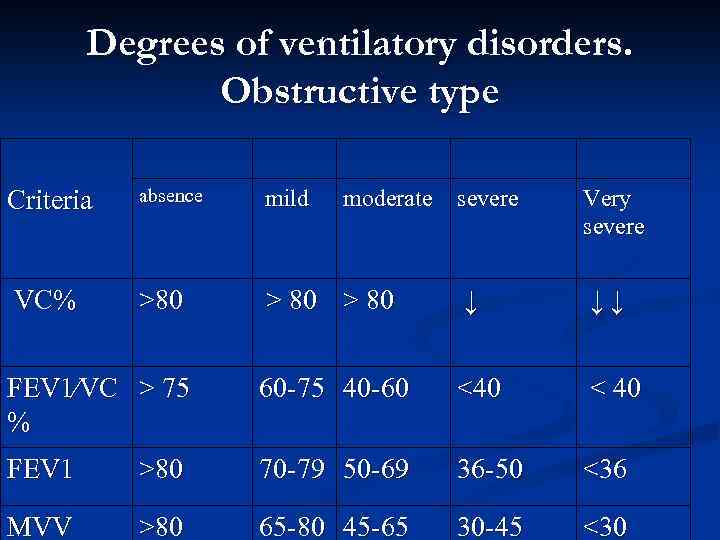 Degrees of ventilatory disorders. Obstructive type absence mild >80 > 80 ↓ ↓↓ FEV 1⁄VC > 75 % 60 -75 40 -60 <40 < 40 FEV 1 >80 70 -79 50 -69 36 -50 <36 МVV >80 65 -80 45 -65 30 -45 <30 Criteria VC% moderate severe Very severe
Degrees of ventilatory disorders. Obstructive type absence mild >80 > 80 ↓ ↓↓ FEV 1⁄VC > 75 % 60 -75 40 -60 <40 < 40 FEV 1 >80 70 -79 50 -69 36 -50 <36 МVV >80 65 -80 45 -65 30 -45 <30 Criteria VC% moderate severe Very severe
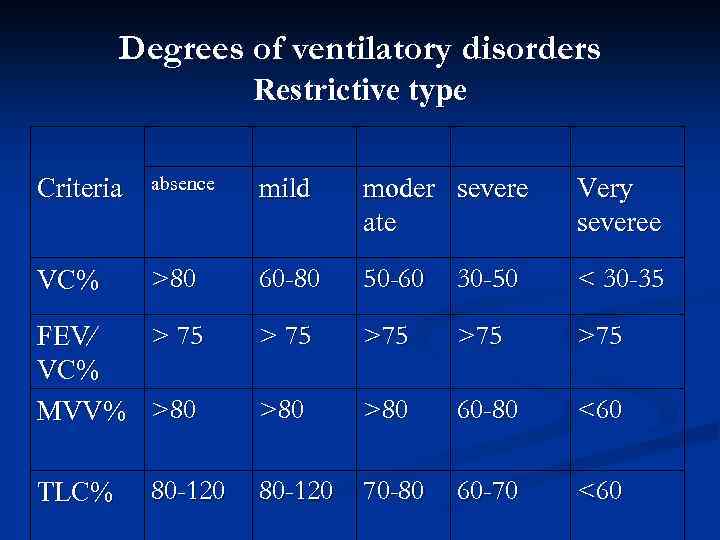 Degrees of ventilatory disorders Restrictive type Criteria absence mild moder severe ate Very severeе VC% >80 60 -80 50 -60 30 -50 < 30 -35 > 75 >75 >80 >80 60 -80 <60 80 -120 70 -80 60 -70 <60 > 75 FEV⁄ VC% МVV% >80 TLC% 80 -120
Degrees of ventilatory disorders Restrictive type Criteria absence mild moder severe ate Very severeе VC% >80 60 -80 50 -60 30 -50 < 30 -35 > 75 >75 >80 >80 60 -80 <60 80 -120 70 -80 60 -70 <60 > 75 FEV⁄ VC% МVV% >80 TLC% 80 -120
 Diagnostics of respiratory failure n n n Clinical examination CBC (erythrocytosis) Sputum analysis CXR Spirometry Pulse oxymetry Oxygen test Determination of Ра 02, Ра. С 02 Physical exercise test Time of saturation and desaturation of O 2 Investigation of respiratory muscles Diffusion lung capacity ( DLco)
Diagnostics of respiratory failure n n n Clinical examination CBC (erythrocytosis) Sputum analysis CXR Spirometry Pulse oxymetry Oxygen test Determination of Ра 02, Ра. С 02 Physical exercise test Time of saturation and desaturation of O 2 Investigation of respiratory muscles Diffusion lung capacity ( DLco)
 Treatment Prolonged oxygentherapy n Not less then 15 - 18 hours/24 hrs n Concentrators of O 2 n 25 -30% O 2 - gas mixture n Objective: decrease of alveolar hypoxia n Objective : Decrease of pulmonary hypertension n
Treatment Prolonged oxygentherapy n Not less then 15 - 18 hours/24 hrs n Concentrators of O 2 n 25 -30% O 2 - gas mixture n Objective: decrease of alveolar hypoxia n Objective : Decrease of pulmonary hypertension n
 Treatmnt of bronchial obstruction Broncodilators ▪ ß-2 agonists ▪ Anticholinergic broncholytics ▪ Theophyllins Mucolytics ▪ ▪ Glucocorticoids
Treatmnt of bronchial obstruction Broncodilators ▪ ß-2 agonists ▪ Anticholinergic broncholytics ▪ Theophyllins Mucolytics ▪ ▪ Glucocorticoids
 Lung vasodilators ■Theophyllins n ß 2 -agonists n α-adrenoblockers n Ca- channels blockers n ACE-Inhibitors
Lung vasodilators ■Theophyllins n ß 2 -agonists n α-adrenoblockers n Ca- channels blockers n ACE-Inhibitors
 Other methods O 2 -therapy n Heliox n Mechanical lung ventilation n Electric stimulation of diaphragm n Lung transplantation n
Other methods O 2 -therapy n Heliox n Mechanical lung ventilation n Electric stimulation of diaphragm n Lung transplantation n
 Cor pulmonale n Cor pulmonale is hypertrophy and /or dilation of right ventricle that occurs due to pulmonary disorders
Cor pulmonale n Cor pulmonale is hypertrophy and /or dilation of right ventricle that occurs due to pulmonary disorders
 Classification Professor Вотчал Б. Е. , 1962 n Acute cor pulmonale develops during some hours or days n Subacute cor pulmonale develops during some weeks or months. n Хроническое легочное сердце развивается в течение ряда лет. n
Classification Professor Вотчал Б. Е. , 1962 n Acute cor pulmonale develops during some hours or days n Subacute cor pulmonale develops during some weeks or months. n Хроническое легочное сердце развивается в течение ряда лет. n
 Легочное сердце n Острая перегрузка правого желудочка, возникающая вследствие заболеваний, первично нарушающих функцию и (или) структуру легких, в т. ч. и сосудов легких, например, при ТЭЛА, называется острым легочным сердцем.
Легочное сердце n Острая перегрузка правого желудочка, возникающая вследствие заболеваний, первично нарушающих функцию и (или) структуру легких, в т. ч. и сосудов легких, например, при ТЭЛА, называется острым легочным сердцем.
 Хроническое легочное сердце n Хроническое легочное сердце - гипертрофия, дилатация и недостаточность правого желудочка, развивающиеся при заболеваниях, первично нарушающих функцию и (или) структуру легких, в т. ч. и сосудов легких. n Врожденные и приобретенные пороки сердца и левожелудочковая недостаточность не являются причиной легочного сердца
Хроническое легочное сердце n Хроническое легочное сердце - гипертрофия, дилатация и недостаточность правого желудочка, развивающиеся при заболеваниях, первично нарушающих функцию и (или) структуру легких, в т. ч. и сосудов легких. n Врожденные и приобретенные пороки сердца и левожелудочковая недостаточность не являются причиной легочного сердца
 Этиология хронического легочного сердца n Заболевания, первично поражающие систему органов дыхания (ХОЗЛ, бронхиальная астма, диффузный интерстициальный пневмофиброз, бронхоэктазы, пневмокониозы, эмфизема легких, паразитарные заболевания легких, саркоидоз и др)
Этиология хронического легочного сердца n Заболевания, первично поражающие систему органов дыхания (ХОЗЛ, бронхиальная астма, диффузный интерстициальный пневмофиброз, бронхоэктазы, пневмокониозы, эмфизема легких, паразитарные заболевания легких, саркоидоз и др)
 Этиология хронического легочного сердца n Изменение подвижности грудной клетки (кифосколиоз, торакопластика, плевриты, истощение, синдром Пиквика и др)
Этиология хронического легочного сердца n Изменение подвижности грудной клетки (кифосколиоз, торакопластика, плевриты, истощение, синдром Пиквика и др)
 Этиология хронического легочного сердца n Патологические процессы, первично поражающие легочные сосуды (первичная легочная гипертензия, узелковый периартериит и другие васкулиты, эмболии , тромбоэмболии, олпухоли средостения и аневризмы, сдавливающие артерии и вены
Этиология хронического легочного сердца n Патологические процессы, первично поражающие легочные сосуды (первичная легочная гипертензия, узелковый периартериит и другие васкулиты, эмболии , тромбоэмболии, олпухоли средостения и аневризмы, сдавливающие артерии и вены
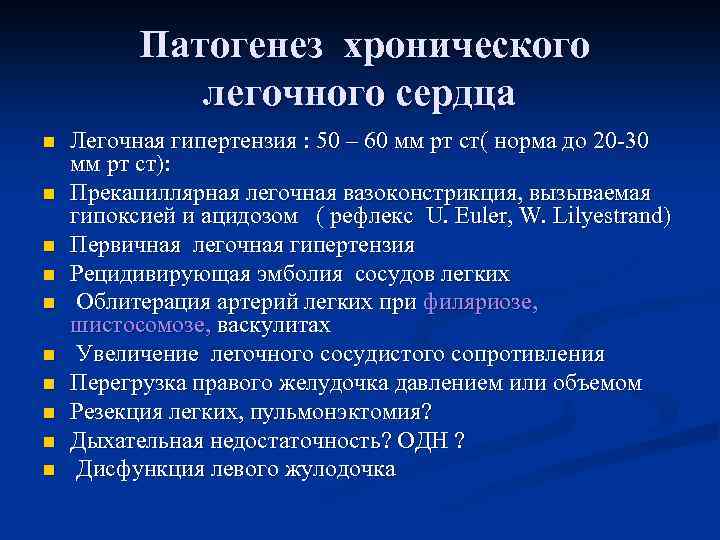 Патогенез хронического легочного сердца n n n n n Легочная гипертензия : 50 – 60 мм рт ст( норма до 20 -30 мм рт ст): Прекапиллярная легочная вазоконстрикция, вызываемая гипоксией и ацидозом ( рефлекс U. Euler, W. Lilyestrand) Первичная легочная гипертензия Рецидивирующая эмболия сосудов легких Облитерация артерий легких при филяриозе, шистосомозе, васкулитах Увеличение легочного сосудистого сопротивления Перегрузка правого желудочка давлением или объемом Резекция легких, пульмонэктомия? Дыхательная недостаточность? ОДН ? Дисфункция левого жулодочка
Патогенез хронического легочного сердца n n n n n Легочная гипертензия : 50 – 60 мм рт ст( норма до 20 -30 мм рт ст): Прекапиллярная легочная вазоконстрикция, вызываемая гипоксией и ацидозом ( рефлекс U. Euler, W. Lilyestrand) Первичная легочная гипертензия Рецидивирующая эмболия сосудов легких Облитерация артерий легких при филяриозе, шистосомозе, васкулитах Увеличение легочного сосудистого сопротивления Перегрузка правого желудочка давлением или объемом Резекция легких, пульмонэктомия? Дыхательная недостаточность? ОДН ? Дисфункция левого жулодочка
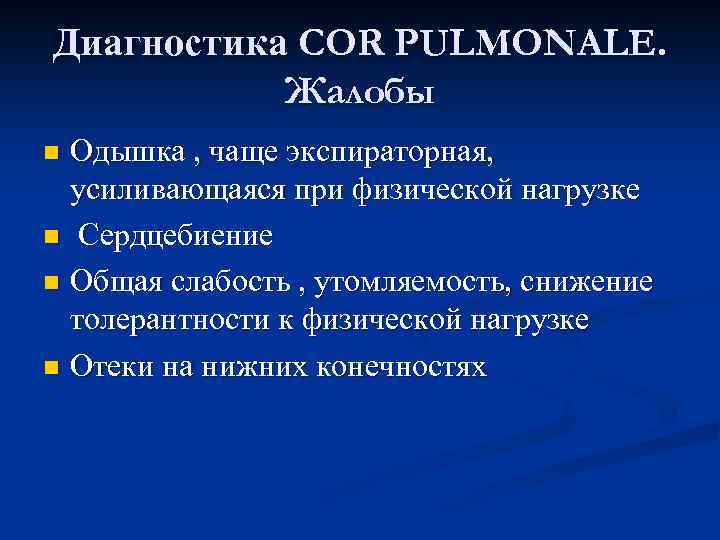 Диагностика COR PULMONALE. Жалобы Одышка , чаще экспираторная, усиливающаяся при физической нагрузке n Сердцебиение n Общая слабость , утомляемость, снижение толерантности к физической нагрузке n Отеки на нижних конечностях n
Диагностика COR PULMONALE. Жалобы Одышка , чаще экспираторная, усиливающаяся при физической нагрузке n Сердцебиение n Общая слабость , утомляемость, снижение толерантности к физической нагрузке n Отеки на нижних конечностях n
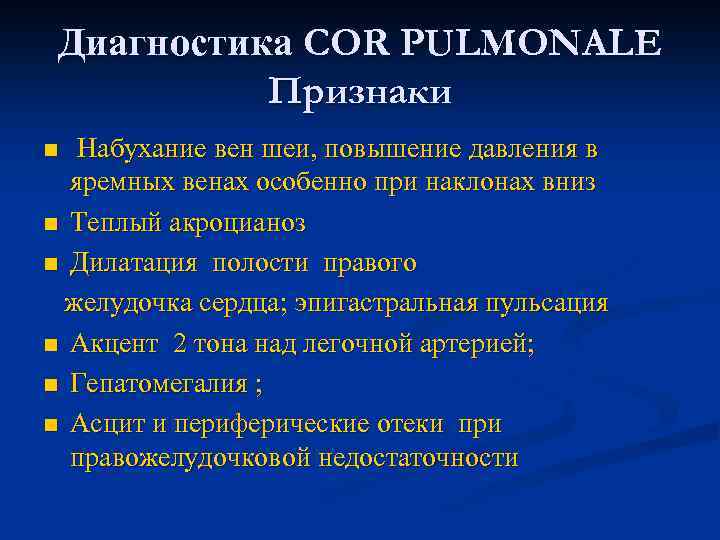 Диагностика COR PULMONALE Признаки Набухание вен шеи, повышение давления в яремных венах особенно при наклонах вниз n Теплый акроцианоз n Дилатация полости правого желудочка сердца; эпигастральная пульсация n Акцент 2 тона над легочной артерией; n Гепатомегалия ; n Асцит и периферические отеки правожелудочковой недостаточности n
Диагностика COR PULMONALE Признаки Набухание вен шеи, повышение давления в яремных венах особенно при наклонах вниз n Теплый акроцианоз n Дилатация полости правого желудочка сердца; эпигастральная пульсация n Акцент 2 тона над легочной артерией; n Гепатомегалия ; n Асцит и периферические отеки правожелудочковой недостаточности n
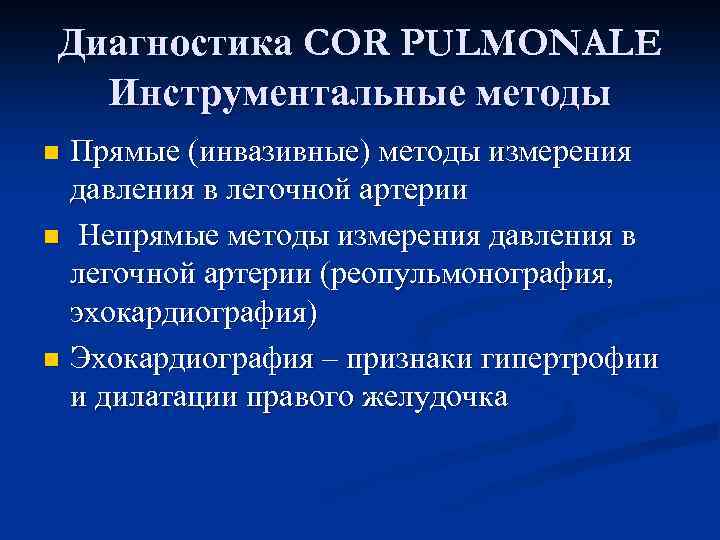 Диагностика COR PULMONALE Инструментальные методы Прямые (инвазивные) методы измерения давления в легочной артерии n Непрямые методы измерения давления в легочной артерии (реопульмонография, эхокардиография) n Эхокардиография – признаки гипертрофии и дилатации правого желудочка n
Диагностика COR PULMONALE Инструментальные методы Прямые (инвазивные) методы измерения давления в легочной артерии n Непрямые методы измерения давления в легочной артерии (реопульмонография, эхокардиография) n Эхокардиография – признаки гипертрофии и дилатации правого желудочка n
 Рентгенологические признаки Выбухание ствола легочной артерии n Усиление сосудистого рисунка корней легкого при относительно светлой периферии n Расширение правой нисходящей легочной артерии ( в норме 15 мм) n
Рентгенологические признаки Выбухание ствола легочной артерии n Усиление сосудистого рисунка корней легкого при относительно светлой периферии n Расширение правой нисходящей легочной артерии ( в норме 15 мм) n
 ЭКГ признаки cor pulmonale n n n Высокий, остроконечный зубец Р ΙΙ, ΙΙΙ, a. VF (Рpulmonale) >2 -2, 5 мм Отклонение электрической оси сердца вправо Увеличение амплитуды зубца R> 5 мм в V 1, V 2, a. VR r. SR-, или S- тип гипертрофии правого желудочка Полная или неполная блокада правой ножки пучка Гиса
ЭКГ признаки cor pulmonale n n n Высокий, остроконечный зубец Р ΙΙ, ΙΙΙ, a. VF (Рpulmonale) >2 -2, 5 мм Отклонение электрической оси сердца вправо Увеличение амплитуды зубца R> 5 мм в V 1, V 2, a. VR r. SR-, или S- тип гипертрофии правого желудочка Полная или неполная блокада правой ножки пучка Гиса
 Эхокардиографические признаки легочного сердца n n n n Утолщение миокарда передней стенки ПЖ ( > 3 -5 мм) и МЖП Расширение полости ПЖ Снижение скорости сокращения ПЖ Систолическое трепетание створок клапанов легочной артерии Вдавливание МЖП в полость ЛЖ Расширение ствола легочной артерии Диастолическое выбухание ствола легочной артерии в полость ПЖ Снижение фракции выброса ПЖ ( норма – 55% и выше)
Эхокардиографические признаки легочного сердца n n n n Утолщение миокарда передней стенки ПЖ ( > 3 -5 мм) и МЖП Расширение полости ПЖ Снижение скорости сокращения ПЖ Систолическое трепетание створок клапанов легочной артерии Вдавливание МЖП в полость ЛЖ Расширение ствола легочной артерии Диастолическое выбухание ствола легочной артерии в полость ПЖ Снижение фракции выброса ПЖ ( норма – 55% и выше)
 COR PULMONALE Лечение Диуретики ( фуросемид, торасемид, спиронолактоны) n и АПФ n Блокаторы рецепторов ангиотензина II n Сердечные гликозиды (дигоксин) n
COR PULMONALE Лечение Диуретики ( фуросемид, торасемид, спиронолактоны) n и АПФ n Блокаторы рецепторов ангиотензина II n Сердечные гликозиды (дигоксин) n


