ffb94dad5024a0e330517c553e354ef7.ppt
- Количество слайдов: 62
 Respiratory Dysfunction in Children Chapter 46
Respiratory Dysfunction in Children Chapter 46
 Acute Pharyngitis • Most often viral, if bacterial is Group A Streptococcus • If child has “cold” symptoms it is probably not Strep Throat • Strep Throat is high fever, raging sore throat and the absence of cough, runny nose. Throat is very red and may have exudate • Page 1431 for picture
Acute Pharyngitis • Most often viral, if bacterial is Group A Streptococcus • If child has “cold” symptoms it is probably not Strep Throat • Strep Throat is high fever, raging sore throat and the absence of cough, runny nose. Throat is very red and may have exudate • Page 1431 for picture
 Tonsillitis • Rx for simple tonsil infection – Cool mist – Salt water gargles – Throat lozenges – Cool, liquid diet – acetaminophen
Tonsillitis • Rx for simple tonsil infection – Cool mist – Salt water gargles – Throat lozenges – Cool, liquid diet – acetaminophen
 Tonsillectomy • A 5 year old female is returned to the day surgery unit following a tonsillectomy. The post anesthesia care unit nurse reports that there were no complications during surgery. The child was medicated for pain on arrival in the recovery room. • What are the immediate nursing actions upon the child’s return to the day surgery unit?
Tonsillectomy • A 5 year old female is returned to the day surgery unit following a tonsillectomy. The post anesthesia care unit nurse reports that there were no complications during surgery. The child was medicated for pain on arrival in the recovery room. • What are the immediate nursing actions upon the child’s return to the day surgery unit?
 Tonsillectomy, post surgical actions • Assess lover of consciousness, vital signs and airway • Assess operative site for bleeding • Note frequent swallowing. • Upright or side lying position • Clear liquids • Ice collar, medicate for pain • Instruct parents
Tonsillectomy, post surgical actions • Assess lover of consciousness, vital signs and airway • Assess operative site for bleeding • Note frequent swallowing. • Upright or side lying position • Clear liquids • Ice collar, medicate for pain • Instruct parents
 Appropriate or not appropriate? • • • Place child in a side lying position Routine suctioning of the oropharynx Providing red jello to eat Providing warm milk and cookies Administer pain medication
Appropriate or not appropriate? • • • Place child in a side lying position Routine suctioning of the oropharynx Providing red jello to eat Providing warm milk and cookies Administer pain medication
 Earliest sign of hemmorhage? • Labored breathing and increase respiratory rate? • Decreased heart rate? • Frequent throat clearing with restlessness? • Dark brown emesis? • Bright red emesis? • Pallor?
Earliest sign of hemmorhage? • Labored breathing and increase respiratory rate? • Decreased heart rate? • Frequent throat clearing with restlessness? • Dark brown emesis? • Bright red emesis? • Pallor?
 Indication for tonsillectomy • What are three indications for a tonsillectomy?
Indication for tonsillectomy • What are three indications for a tonsillectomy?
 Indication for tonsillectomy • Repeated tonsillitis • Airway obstruction and /or sleep apnea due to enlarged tonsils • Chronic feeding difficulty due to inability to swallow from enlarged tonsils.
Indication for tonsillectomy • Repeated tonsillitis • Airway obstruction and /or sleep apnea due to enlarged tonsils • Chronic feeding difficulty due to inability to swallow from enlarged tonsils.
 Tonsillectomy, Post surgical • What are the nursing priorities in the recovery period prior to discharge?
Tonsillectomy, Post surgical • What are the nursing priorities in the recovery period prior to discharge?
 Nursing priorities • • • No evidence of bleeding Tolerates soft diet Routinely swallows clear liquids Manageable level of discomfort Voids at least one time VS stable.
Nursing priorities • • • No evidence of bleeding Tolerates soft diet Routinely swallows clear liquids Manageable level of discomfort Voids at least one time VS stable.
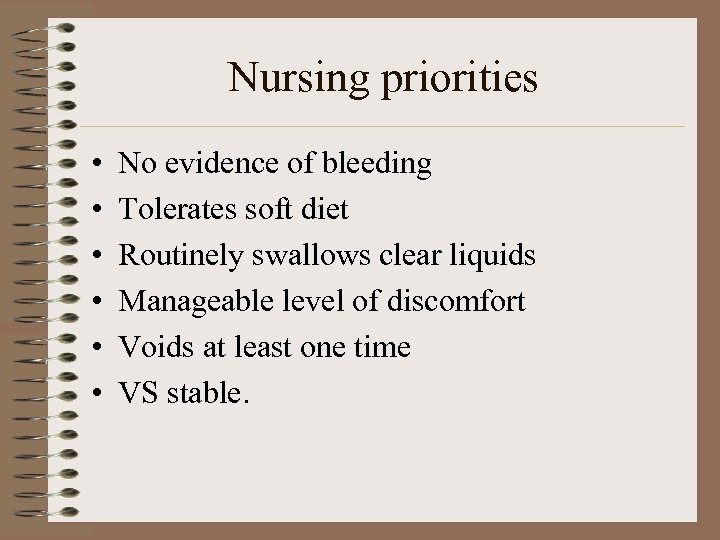
 Otitis Media
Otitis Media
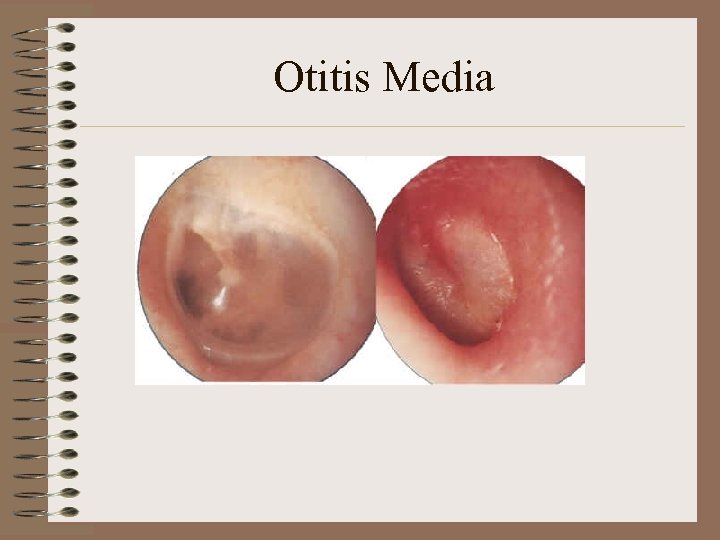 Otitis Media
Otitis Media
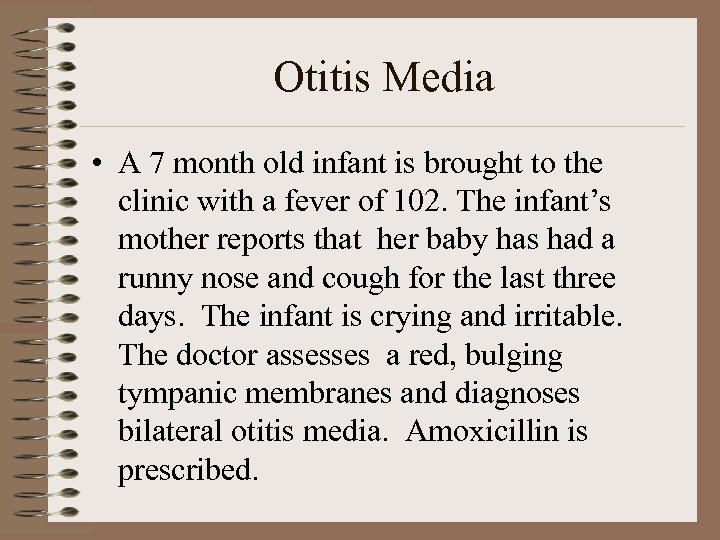 Otitis Media • A 7 month old infant is brought to the clinic with a fever of 102. The infant’s mother reports that her baby has had a runny nose and cough for the last three days. The infant is crying and irritable. The doctor assesses a red, bulging tympanic membranes and diagnoses bilateral otitis media. Amoxicillin is prescribed.
Otitis Media • A 7 month old infant is brought to the clinic with a fever of 102. The infant’s mother reports that her baby has had a runny nose and cough for the last three days. The infant is crying and irritable. The doctor assesses a red, bulging tympanic membranes and diagnoses bilateral otitis media. Amoxicillin is prescribed.
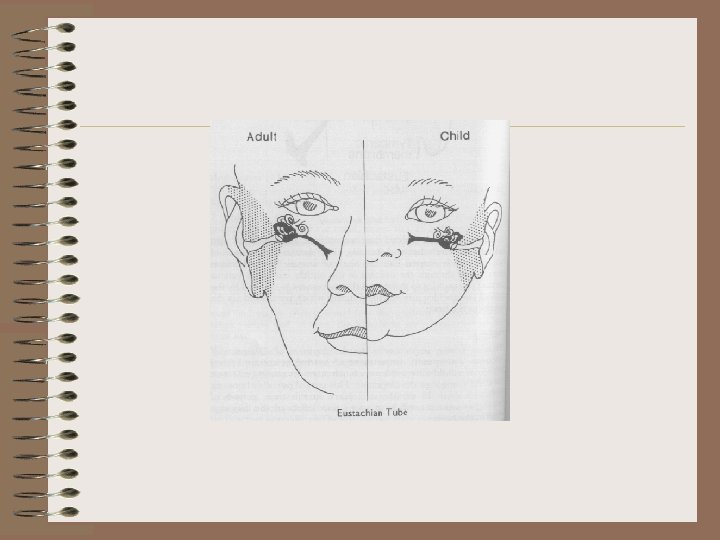
 Pathology of OM • Read section on 1434. • Infants have a shorter, narrower and more horizontal tube than adults.
Pathology of OM • Read section on 1434. • Infants have a shorter, narrower and more horizontal tube than adults.
 OM • The child’s mother asks the nurse what she can do to prevent additional ear infections. What will the nurse tell her about risk factors associated with OM?
OM • The child’s mother asks the nurse what she can do to prevent additional ear infections. What will the nurse tell her about risk factors associated with OM?
 Risk Factors associated with OM • Bottle feeding in supine position • Parental smoking • Exposure to sick children and/or having a respiratory illness • Winter months • 3 months to 3 years
Risk Factors associated with OM • Bottle feeding in supine position • Parental smoking • Exposure to sick children and/or having a respiratory illness • Winter months • 3 months to 3 years
 Symptoms of Otitis Media • What are the symptoms of otitis media you can teach to your patients?
Symptoms of Otitis Media • What are the symptoms of otitis media you can teach to your patients?
 Symptoms of OM • • Rubbing or pulling at the ear Rolling head from side to side Hearing loss, loud speech Fever, irritability Sleep problems URI symptoms Purulent material coming from ear
Symptoms of OM • • Rubbing or pulling at the ear Rolling head from side to side Hearing loss, loud speech Fever, irritability Sleep problems URI symptoms Purulent material coming from ear
 Instructions for OM • Take all the doses of medication • Comfort measures: – antipyretics/analgesics – Warm compresses • Teach risk factors • RTC for progressive symptoms
Instructions for OM • Take all the doses of medication • Comfort measures: – antipyretics/analgesics – Warm compresses • Teach risk factors • RTC for progressive symptoms
 Complications of OM • • • Hearing loss Ruptured membrane Mastoiditis Chronic OM Meningitis, brain abscess Speech difficulties
Complications of OM • • • Hearing loss Ruptured membrane Mastoiditis Chronic OM Meningitis, brain abscess Speech difficulties
 Croup Syndromes • • Epiglottis Laryngotracheobronchitis Spasmodic Laryngitis Bacterial Tracheitis
Croup Syndromes • • Epiglottis Laryngotracheobronchitis Spasmodic Laryngitis Bacterial Tracheitis
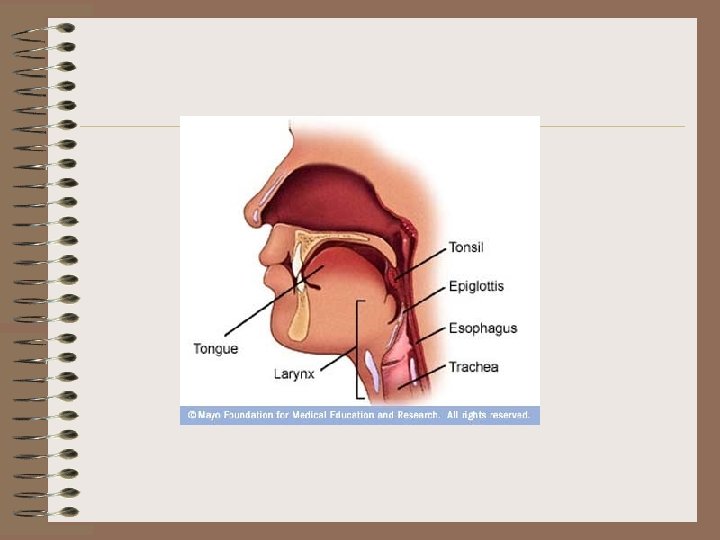
 Epiglottis • Very serious inflammation of the epiglottis and surrounding region • Peak age 2 -5 • EMERGENCY SITUATION
Epiglottis • Very serious inflammation of the epiglottis and surrounding region • Peak age 2 -5 • EMERGENCY SITUATION
 Epiglottis; clinical manifestations • • Fever Sick in appearance Insists on sitting up right and foward Chin thrust out, mouth open DROOLING Anxious and agitated Absence of spontaneous cough
Epiglottis; clinical manifestations • • Fever Sick in appearance Insists on sitting up right and foward Chin thrust out, mouth open DROOLING Anxious and agitated Absence of spontaneous cough
 Epiglottitis; Nursing measures • • • Extremely quiet and calm environment DO NOT separate parent from child LEAVE CHILD sitting upright on parents lap NO TONGUE BLADE Prepare for emergency trach, have emergency equipment at bedside • Blow by oxygen • Probable intubation and antibiotics
Epiglottitis; Nursing measures • • • Extremely quiet and calm environment DO NOT separate parent from child LEAVE CHILD sitting upright on parents lap NO TONGUE BLADE Prepare for emergency trach, have emergency equipment at bedside • Blow by oxygen • Probable intubation and antibiotics
 Laryngotracheobronchitis • See symptoms on box 46 -7 page 1438
Laryngotracheobronchitis • See symptoms on box 46 -7 page 1438
 Croup; Clinical Presentation • • • Begins with URI sx Harsh bark cough Inspiratory stridor Temp remains lower 100. 4 to 102. 2 Peak 3 -5 days; last 7 -10 days See progression of Symptoms page 1438 box 46 -7
Croup; Clinical Presentation • • • Begins with URI sx Harsh bark cough Inspiratory stridor Temp remains lower 100. 4 to 102. 2 Peak 3 -5 days; last 7 -10 days See progression of Symptoms page 1438 box 46 -7
 Croup, Management • Mist therapy • Oxygen support if necessary • Inhaled epinephrine; mucosal vasoconstriction with subsequent decrease in subglottic edema • Corticosteroids p. o. or inhaled • Hydration management – Follow urinary output (1 -2 ml/kg/hr) – Weigh daily – IV if po fluids not tolerated
Croup, Management • Mist therapy • Oxygen support if necessary • Inhaled epinephrine; mucosal vasoconstriction with subsequent decrease in subglottic edema • Corticosteroids p. o. or inhaled • Hydration management – Follow urinary output (1 -2 ml/kg/hr) – Weigh daily – IV if po fluids not tolerated
 Acute Spasmodic Laryngitis • Occurs chiefly at night accompanied by URI Sx during the day. • Paroxysmal attacks of laryngeal obstruction • Managed by humidity usually at home.
Acute Spasmodic Laryngitis • Occurs chiefly at night accompanied by URI Sx during the day. • Paroxysmal attacks of laryngeal obstruction • Managed by humidity usually at home.
 Bacterial Tracheitis • • • Upper trachea involvement May cause serious airway obstruction Unresponsive to croup therapy Higher fever Thick purulent tracheal secretions RX: intubation, antibiotics, O 2, Sx, antipyretics
Bacterial Tracheitis • • • Upper trachea involvement May cause serious airway obstruction Unresponsive to croup therapy Higher fever Thick purulent tracheal secretions RX: intubation, antibiotics, O 2, Sx, antipyretics
 Bronchiolitis • Viral infection of the bronchioles • Usually caused by Respiratory Syncytial Virus • URI sxs followed by development of wheezing and s/s respiratory distress • Wall of bronchi inflamed; emphysema like obstruction • Mucus and exudate are present • Page 1440 for description
Bronchiolitis • Viral infection of the bronchioles • Usually caused by Respiratory Syncytial Virus • URI sxs followed by development of wheezing and s/s respiratory distress • Wall of bronchi inflamed; emphysema like obstruction • Mucus and exudate are present • Page 1440 for description
 Bronchiolitis, Patient Care • Much like croup • Bronchodilators may be effective and a trial of them is usually initiated • The literature however as well as your book says that bronchodilators, corticosteroids and antibiotics are not effective against bronchiolitis • Ribavirin has a possible use in rx of bronchiolitis
Bronchiolitis, Patient Care • Much like croup • Bronchodilators may be effective and a trial of them is usually initiated • The literature however as well as your book says that bronchodilators, corticosteroids and antibiotics are not effective against bronchiolitis • Ribavirin has a possible use in rx of bronchiolitis
 Respiratory Syncythial Virus • • RSV Epidemic in winter months Infants 2 -7 months most seriously effected Premies are very vulnerable to this virus, hence the immunization with Synergis (immune globulin) • Direct contact of respiratory secretions and lives on fomites for a long time • Incubation period 4 days; communicability 3 -8 days but in infants up to a month
Respiratory Syncythial Virus • • RSV Epidemic in winter months Infants 2 -7 months most seriously effected Premies are very vulnerable to this virus, hence the immunization with Synergis (immune globulin) • Direct contact of respiratory secretions and lives on fomites for a long time • Incubation period 4 days; communicability 3 -8 days but in infants up to a month
 Paluizumab • < 32 wk gestation up to 6 mos age • <28 wk gestation up to 12 mos age • 32 -35 wk gestation with additional risk factors • Infants under 24 months with CHD • Page 1441
Paluizumab • < 32 wk gestation up to 6 mos age • <28 wk gestation up to 12 mos age • 32 -35 wk gestation with additional risk factors • Infants under 24 months with CHD • Page 1441
 RSV-IGIV • • 750 mg/kg Use in immunocompromised infants Contraindicated in pts with cyanotic CHD Do not give MMR and varicella within 9 months of RSV-IGIV • Recommended in children under 24 months with chronic lung disease requiring treatment in the last 6 months. • Given once a month
RSV-IGIV • • 750 mg/kg Use in immunocompromised infants Contraindicated in pts with cyanotic CHD Do not give MMR and varicella within 9 months of RSV-IGIV • Recommended in children under 24 months with chronic lung disease requiring treatment in the last 6 months. • Given once a month
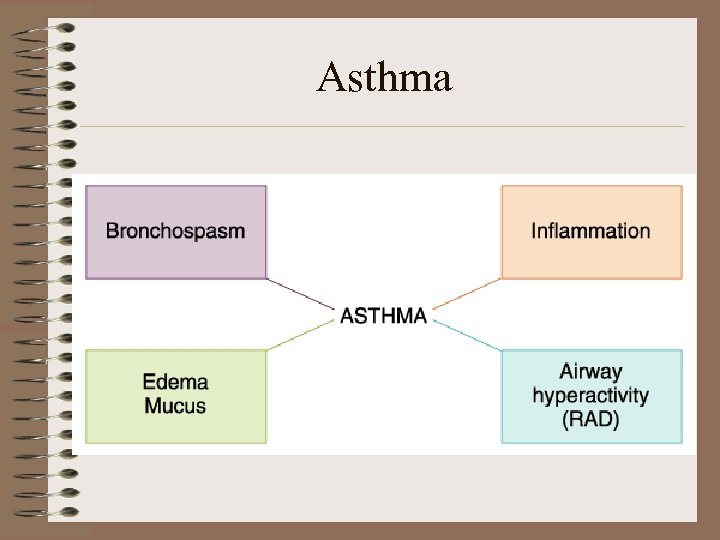 Asthma
Asthma
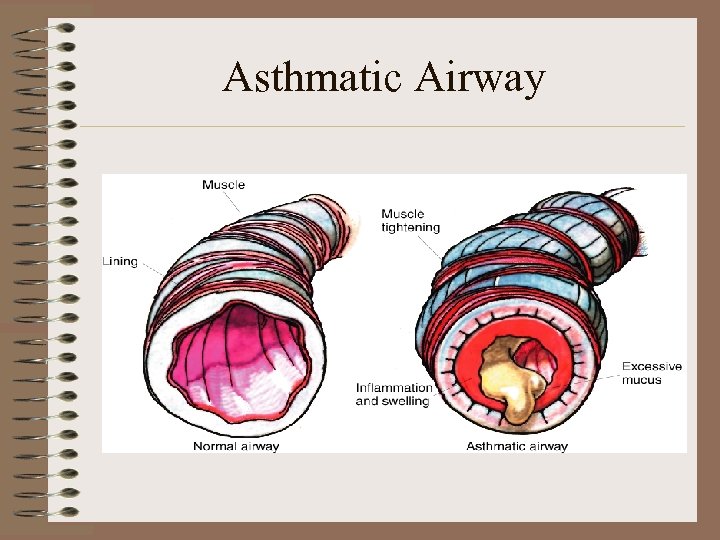 Asthmatic Airway
Asthmatic Airway
 Asthma; manifestations • • Slow or abrupt onset Obstruction worst on expiration Trapped air causes hypo inflation Increased breathing effort Increased strain on heart Cough, wheeze Air hunger
Asthma; manifestations • • Slow or abrupt onset Obstruction worst on expiration Trapped air causes hypo inflation Increased breathing effort Increased strain on heart Cough, wheeze Air hunger
 Asthma; treatment • Bronchodilators • Cromolyn (inhibits the release of histamine) – Is a preventative med; onset 1 week • Corticosteroids • Environmental Control
Asthma; treatment • Bronchodilators • Cromolyn (inhibits the release of histamine) – Is a preventative med; onset 1 week • Corticosteroids • Environmental Control
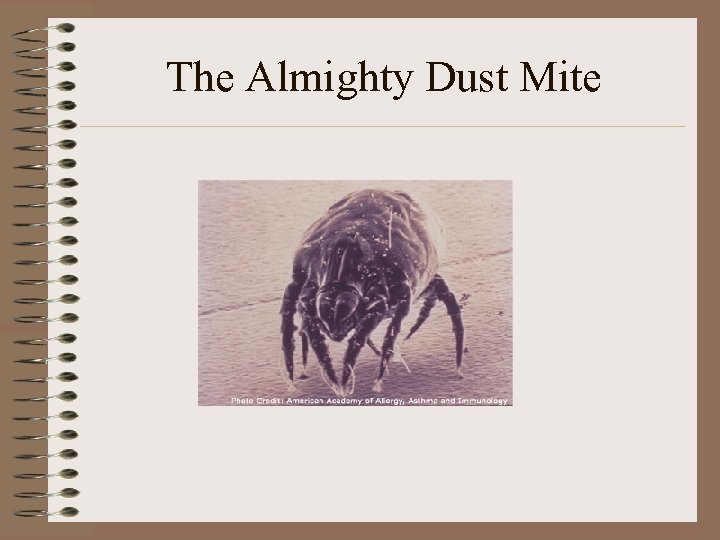 The Almighty Dust Mite
The Almighty Dust Mite
 Allergy Proofing the Home • • Pet dander Mold Dust Mites Smoking Stuffed toys House Plants Mattress and pillow encasing • • Carpet free Duct cleaning HEPA vacuums/filters Bedding changes frequently • Low humidity • Avoid wool and down bedding • Acrosan
Allergy Proofing the Home • • Pet dander Mold Dust Mites Smoking Stuffed toys House Plants Mattress and pillow encasing • • Carpet free Duct cleaning HEPA vacuums/filters Bedding changes frequently • Low humidity • Avoid wool and down bedding • Acrosan
 Asthma; self care • Peak flow meter the golden standard of care – Utilized with a asthma care plan/diary p 1451 – See page 1456 for use of peak flow meter • Use of a combination of steroid inhaler with albuterol inhaler • Proper use of MDI page 1456 • Rinsing of mouth after usage of steroid inhaler
Asthma; self care • Peak flow meter the golden standard of care – Utilized with a asthma care plan/diary p 1451 – See page 1456 for use of peak flow meter • Use of a combination of steroid inhaler with albuterol inhaler • Proper use of MDI page 1456 • Rinsing of mouth after usage of steroid inhaler
 Cystic Fibrosis • Northern European descent, recessive trait • Is an exocrine gland dysfunction – Increased viscosity of mucous gland secretions – Loss of electrolyte in sweat due to abnormal chloride movement • Multi System Disease – – Respiratory Digestive Skin Reproductive
Cystic Fibrosis • Northern European descent, recessive trait • Is an exocrine gland dysfunction – Increased viscosity of mucous gland secretions – Loss of electrolyte in sweat due to abnormal chloride movement • Multi System Disease – – Respiratory Digestive Skin Reproductive
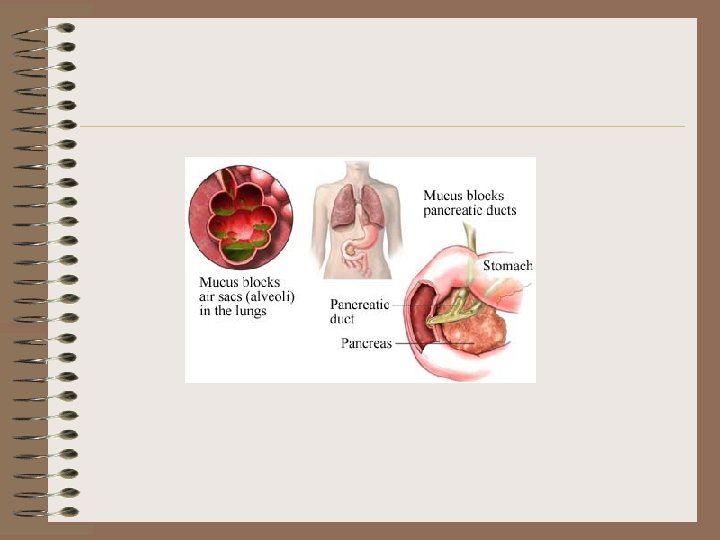
 Cystic Fibrosis; Respiratory pathology • Thick mucous secretions obstruct airways – Obstructive emphysema – Atelectasis – Barrel shaped chest and clubbing of the fingers – High risk for respiratory infections
Cystic Fibrosis; Respiratory pathology • Thick mucous secretions obstruct airways – Obstructive emphysema – Atelectasis – Barrel shaped chest and clubbing of the fingers – High risk for respiratory infections
 Cystic Fibrosis Digestive and Pancreatic Involvement • Thick secretions prevent digestive enzymes from flowing, hence poor absorption of food • Bile duct blockage leading to biliary cirrhosis and portal hypertension • Bulky foul smelling stools due to undigested fat • Impaction; rectal prolapse, meconium ileus • Signs of malnutrition: distended abdomen and muscle wasting
Cystic Fibrosis Digestive and Pancreatic Involvement • Thick secretions prevent digestive enzymes from flowing, hence poor absorption of food • Bile duct blockage leading to biliary cirrhosis and portal hypertension • Bulky foul smelling stools due to undigested fat • Impaction; rectal prolapse, meconium ileus • Signs of malnutrition: distended abdomen and muscle wasting
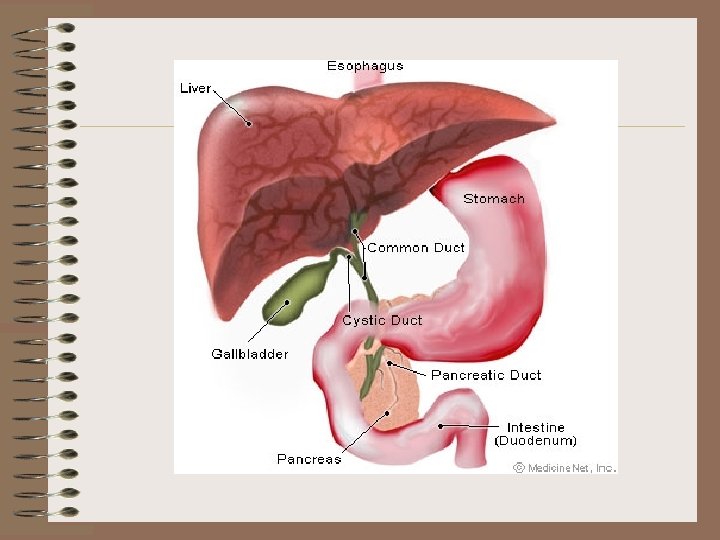
 Other Pancreatic Complications • • Pancreatitis Insulin-dependent diabetes Gallstones Liver cirrhosis
Other Pancreatic Complications • • Pancreatitis Insulin-dependent diabetes Gallstones Liver cirrhosis
 Cystic Fibrosis skin pathology • Loose large amounts of salt through their skin • Cystic fibrosis is diagnosed with a “sweat test” • At high risk for heat prostration, dehydration, hyponatremia
Cystic Fibrosis skin pathology • Loose large amounts of salt through their skin • Cystic fibrosis is diagnosed with a “sweat test” • At high risk for heat prostration, dehydration, hyponatremia
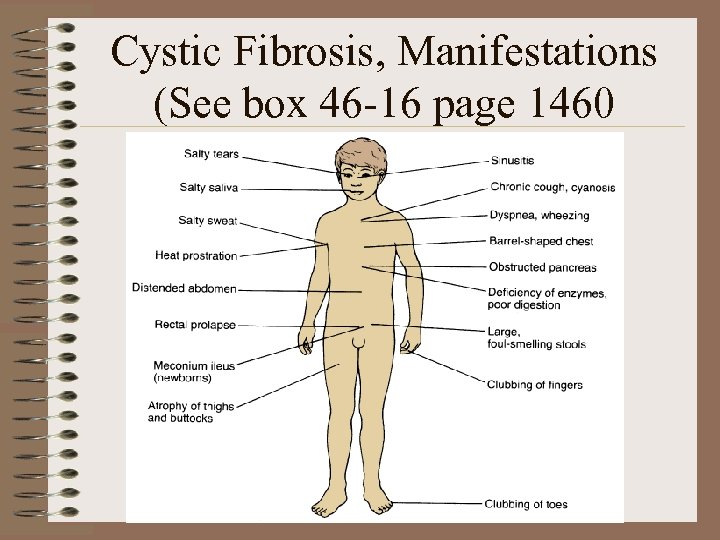 Cystic Fibrosis, Manifestations (See box 46 -16 page 1460
Cystic Fibrosis, Manifestations (See box 46 -16 page 1460
 Cystic Fibrosis; management • Bronchodilators (Albuterol) • Vitamins ADEK • Pulmozyme; Dornase – mucolytic; breaks down DNA in mucous – Nebulized medication • Pancrelipase (pancreatic enzyme) – Enteric coated or microcapsules, do not crush • Antibiotics – Lean body mass increases clearance rate and doses may be higher than average population – Inhaled antibiotics are utilized in resistant infections • Chest Physiotherapy • Exercise Program • High protein, high caloric diet, increase salt
Cystic Fibrosis; management • Bronchodilators (Albuterol) • Vitamins ADEK • Pulmozyme; Dornase – mucolytic; breaks down DNA in mucous – Nebulized medication • Pancrelipase (pancreatic enzyme) – Enteric coated or microcapsules, do not crush • Antibiotics – Lean body mass increases clearance rate and doses may be higher than average population – Inhaled antibiotics are utilized in resistant infections • Chest Physiotherapy • Exercise Program • High protein, high caloric diet, increase salt
 Pulmozyme • • • 2. 5 mg bid per nebulizer Do not dilute Do not combine other meds in nebulizer Refrigerate Avoid light Check solution; should be clear
Pulmozyme • • • 2. 5 mg bid per nebulizer Do not dilute Do not combine other meds in nebulizer Refrigerate Avoid light Check solution; should be clear
 Chronic Lung Disease of Infancy • Thickening of alveolar walls and the bronchiolar epithelium • Chronic Respiratory Distress • Chronic disease often requiring tracheostomy and ongoing dependence on O 2 • Formerly called Broncho Pulmonary Dysplasia • Page 819
Chronic Lung Disease of Infancy • Thickening of alveolar walls and the bronchiolar epithelium • Chronic Respiratory Distress • Chronic disease often requiring tracheostomy and ongoing dependence on O 2 • Formerly called Broncho Pulmonary Dysplasia • Page 819
 Chronic Lung Disease etiology • • • Pulmonary immaturity Surfactant deficiency Lung injury Barotrauma Inflammation caused by oxygen exposure This disease has decreased due to antenatal steroids, use of surfactant, minimizing lung trauma due to ventilation and oxygenation.
Chronic Lung Disease etiology • • • Pulmonary immaturity Surfactant deficiency Lung injury Barotrauma Inflammation caused by oxygen exposure This disease has decreased due to antenatal steroids, use of surfactant, minimizing lung trauma due to ventilation and oxygenation.
 Pertussis • Incubation of 3 -12 days • 6 weeks: catarrhal, paroxysmal, convalescent • Fever absent • Intense coughing with characteristic whoop in paroxysmal stage
Pertussis • Incubation of 3 -12 days • 6 weeks: catarrhal, paroxysmal, convalescent • Fever absent • Intense coughing with characteristic whoop in paroxysmal stage
 Pertussis complications • • Apnea in infants <6 months Conjunctival hemorrhage and petechiae Encephalopathy “infants are more vulne to serious complications such as dehydration, hernia, pneumonia, apnea, hypoxic encephalopathy, seizures and death”. Nursing 2006
Pertussis complications • • Apnea in infants <6 months Conjunctival hemorrhage and petechiae Encephalopathy “infants are more vulne to serious complications such as dehydration, hernia, pneumonia, apnea, hypoxic encephalopathy, seizures and death”. Nursing 2006
 Pertussis Care • • Related to the severity of the symptoms Erythromycin drug of choice for rx O 2 Monitor HR RR O 2 Sat Monitor impact on feeding and vomitting Apnea monitor in infants Droplet precautions
Pertussis Care • • Related to the severity of the symptoms Erythromycin drug of choice for rx O 2 Monitor HR RR O 2 Sat Monitor impact on feeding and vomitting Apnea monitor in infants Droplet precautions
 Foreign Body Aspiration • nuts, raisins, sunflower seeds, improperly chewed pieces of meat and small smooth items such as grapes, hot dogs, and sausages • Dried foods may cause progressive obstruction as they absorb water. • Balloons!
Foreign Body Aspiration • nuts, raisins, sunflower seeds, improperly chewed pieces of meat and small smooth items such as grapes, hot dogs, and sausages • Dried foods may cause progressive obstruction as they absorb water. • Balloons!
 Foreign Body Aspiration History • sudden episode of coughing or choking while eating with subsequent wheezing, coughing, or stridor. • symptoms may include stridor, recurrent or persistent croup, and voice changes. • Persistent pneumonia • as many as one third of parents were unaware of the aspiration
Foreign Body Aspiration History • sudden episode of coughing or choking while eating with subsequent wheezing, coughing, or stridor. • symptoms may include stridor, recurrent or persistent croup, and voice changes. • Persistent pneumonia • as many as one third of parents were unaware of the aspiration
 Foreign Body Aspiration; Care • Symptom related. If acute your care may be quite similar to epiglottitis or croup in the ER • Radiographic and broncoscopy • Antibiotics not necessary unless s/s infection • Occasional use of corticosteroids for inflammation • Use of Heimlich manuever vs watchful care • In stridorous patients, racemic epinephrine via a nebulizer • In unstable patients, rapid sequence intubation may be needed • Have emergency equipment ready
Foreign Body Aspiration; Care • Symptom related. If acute your care may be quite similar to epiglottitis or croup in the ER • Radiographic and broncoscopy • Antibiotics not necessary unless s/s infection • Occasional use of corticosteroids for inflammation • Use of Heimlich manuever vs watchful care • In stridorous patients, racemic epinephrine via a nebulizer • In unstable patients, rapid sequence intubation may be needed • Have emergency equipment ready


