Respiratory disorders in newborns. The occurrence of RD

Respiratory disorders in newborns
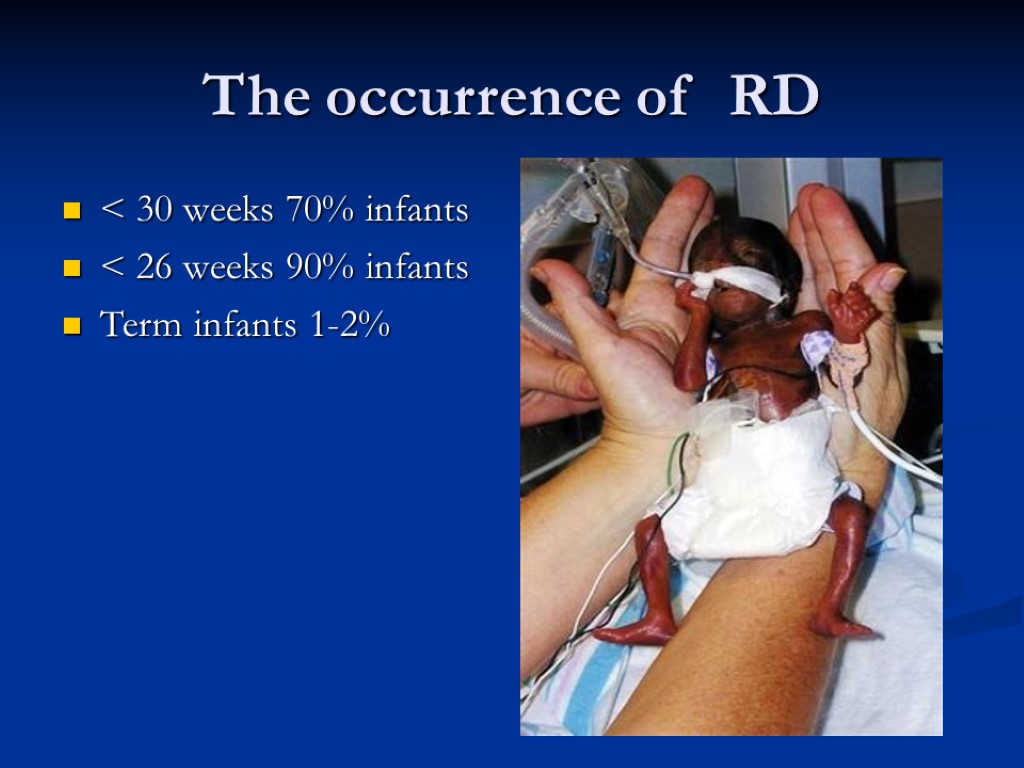
The occurrence of RD < 30 weeks 70% infants < 26 weeks 90% infants Term infants 1-2%
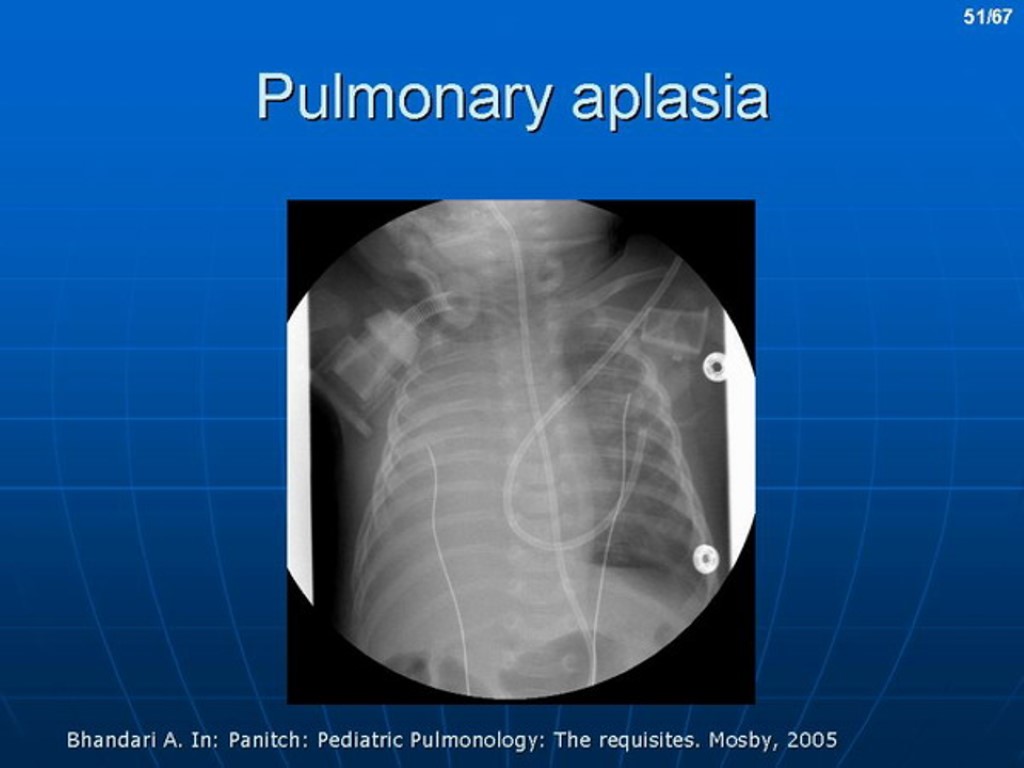
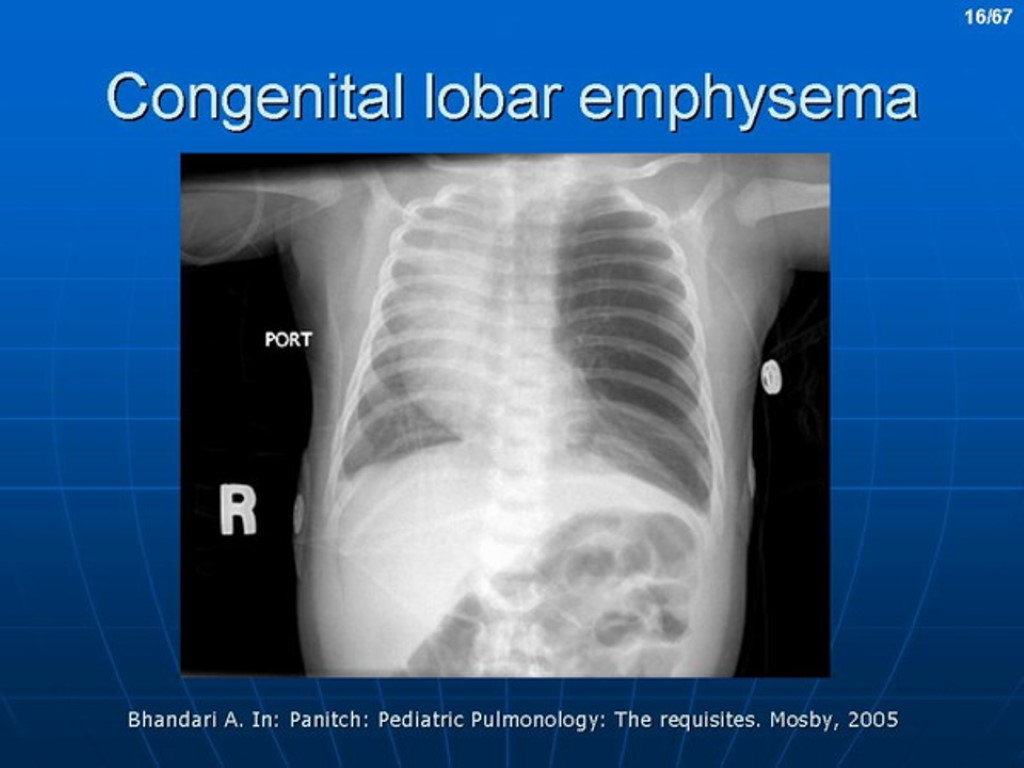
Causes of Respiratory Disorders in the newborn Pulmonary: Congenital disease of lung (aplasia, agenesia) Choanal atresia Lung hemorrhage Pneumonia, Pneumotorax Hyaline membrane disease Aspiration of meconium, amniotic fluid, blood, milk Transient tachipnea (RDS II type)
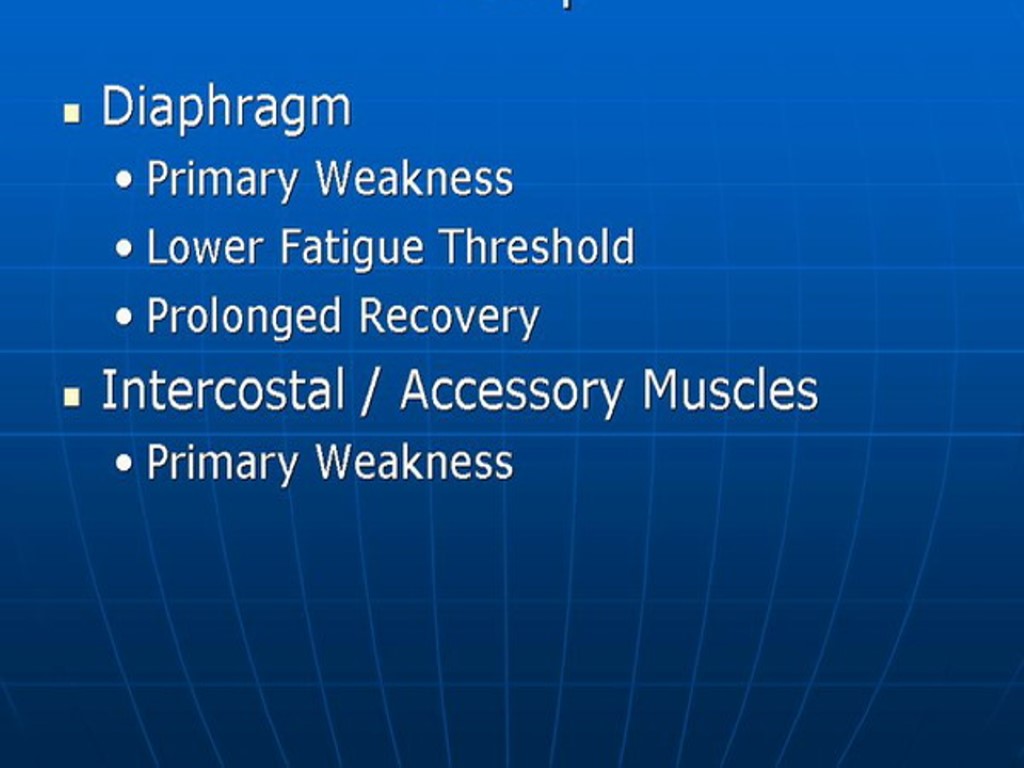
Causes of Respiratory Disorders in the newborn Extrapulmonary Cerebral defects of CNS intracranial hemorrhage nervus phrenicus palsy birth injury, brain edema neuromuscular disease
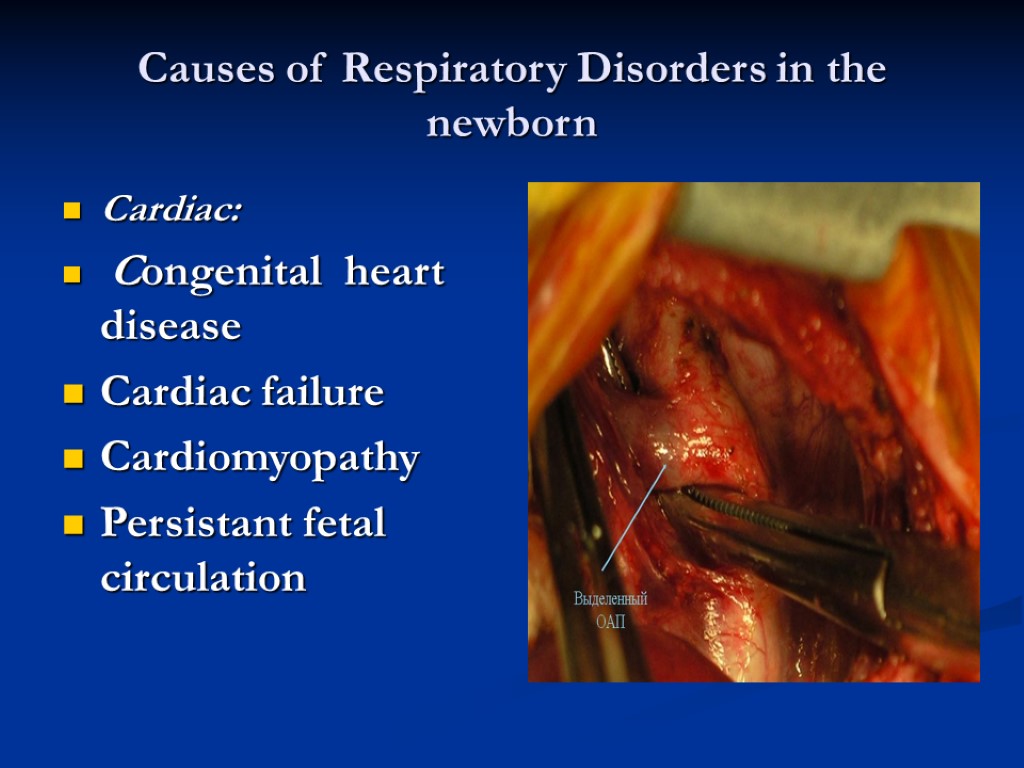
Causes of Respiratory Disorders in the newborn Cardiac: Congenital heart disease Cardiac failure Cardiomyopathy Persistant fetal circulation
Causes of Respiratory Disorders in the newborn Gastrointestinal: Tracheoesophagal fistula Diaphragmatic hernia Metabolic Hypoxia, hypothermia, hypoglycemia, acidosis, congenital hypothyroidism Hematological: Acute bleeding Hypovolemia Polycytemia Infectional: sepsis & meningitis
Respiratory distress syndrome RDS RDS – non infection pathology of lung, that is formated intrauterine, intrapartum and during early neonatal period RDS I type - is same as Hyaline membrane disease (HMD) RDS is a cause of death of 30-80% of infants
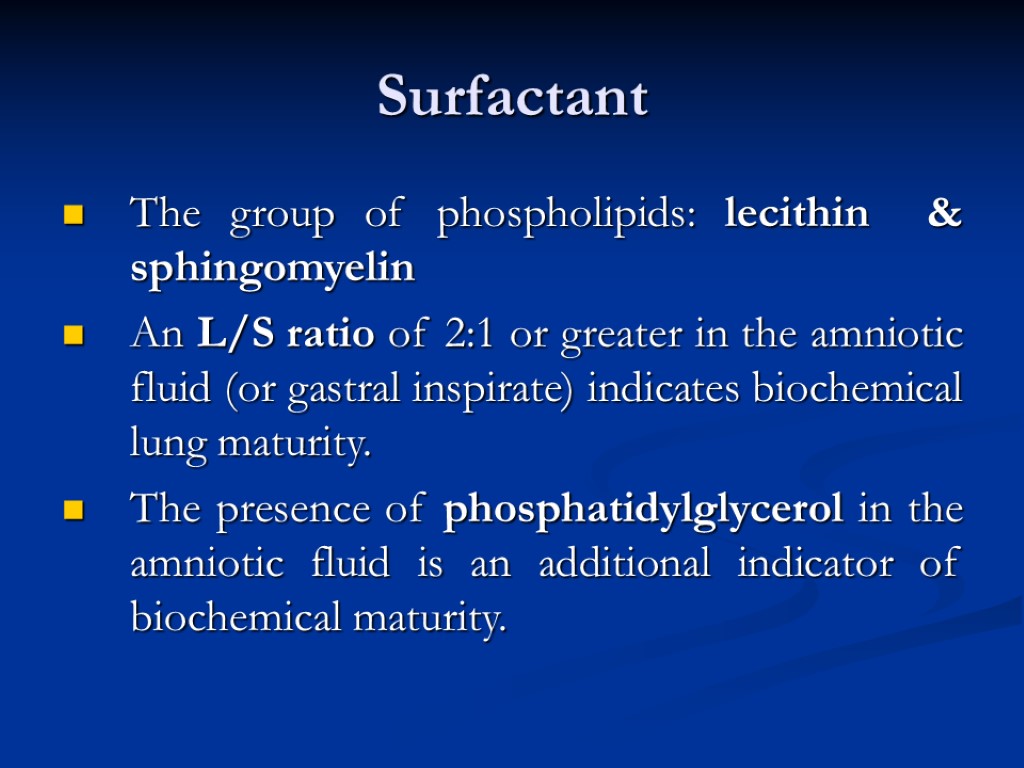
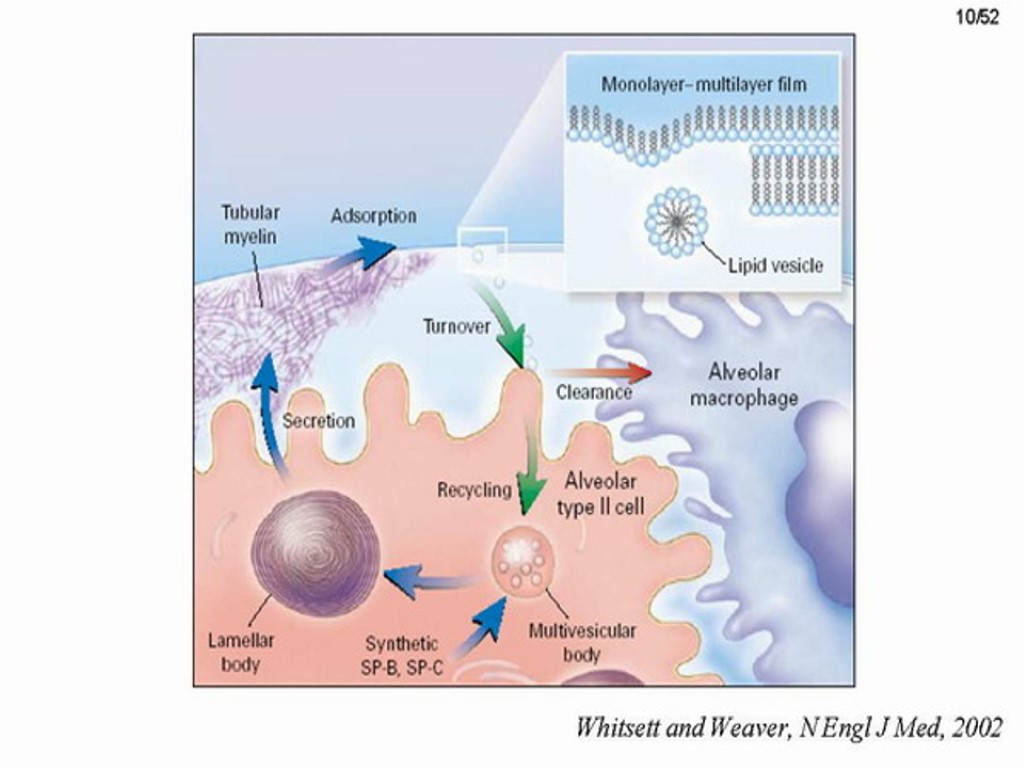
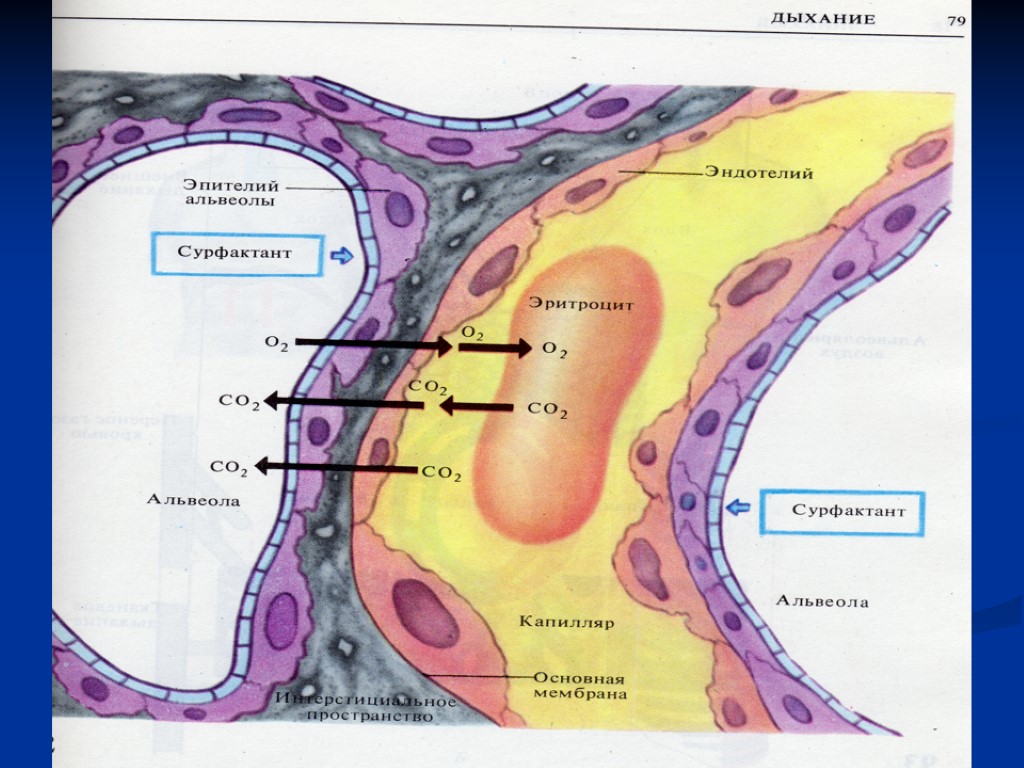
Surfactant The group of phospholipids: lecithin & sphingomyelin An L/S ratio of 2:1 or greater in the amniotic fluid (or gastral inspirate) indicates biochemical lung maturity. The presence of phosphatidylglycerol in the amniotic fluid is an additional indicator of biochemical maturity.
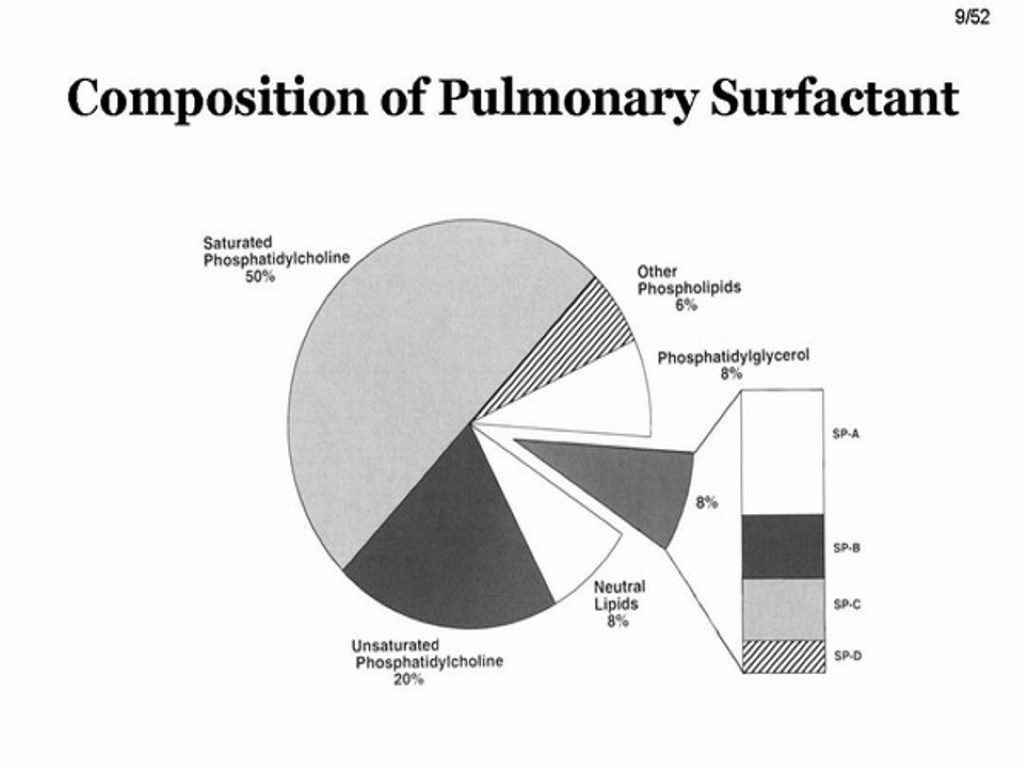
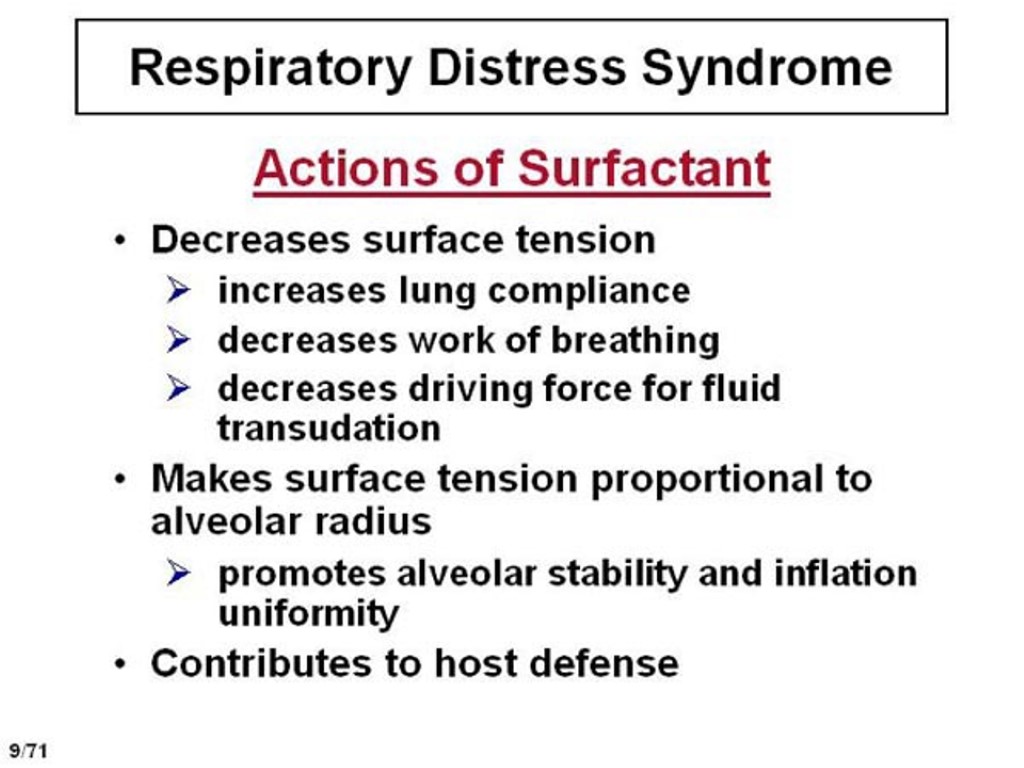
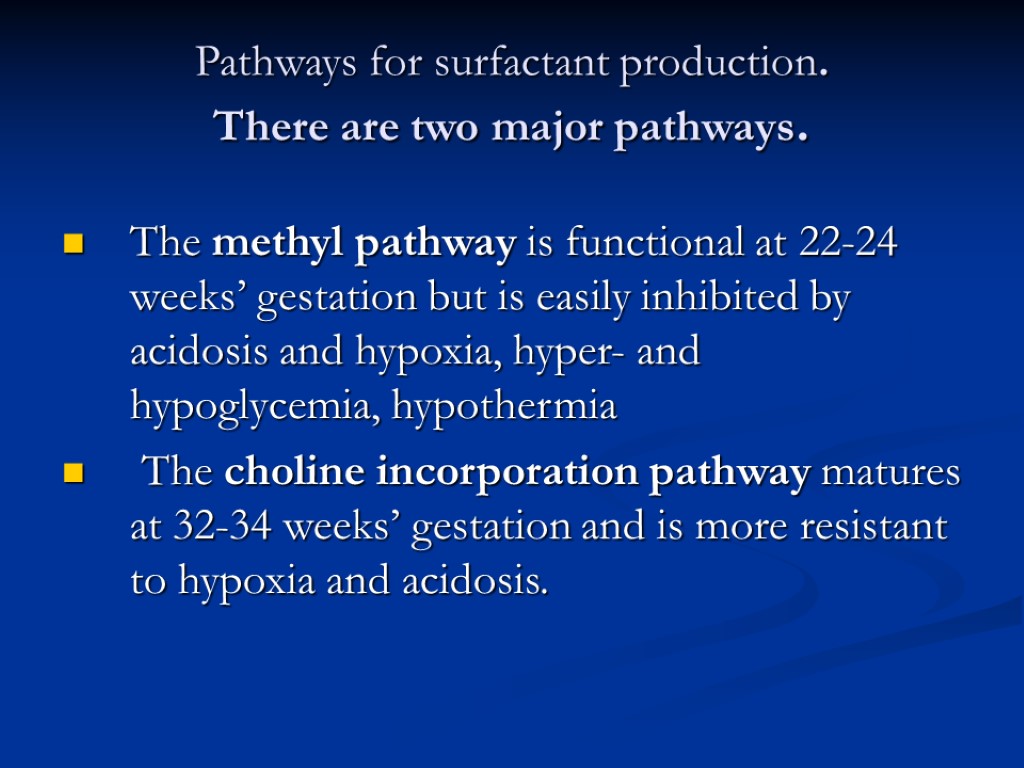
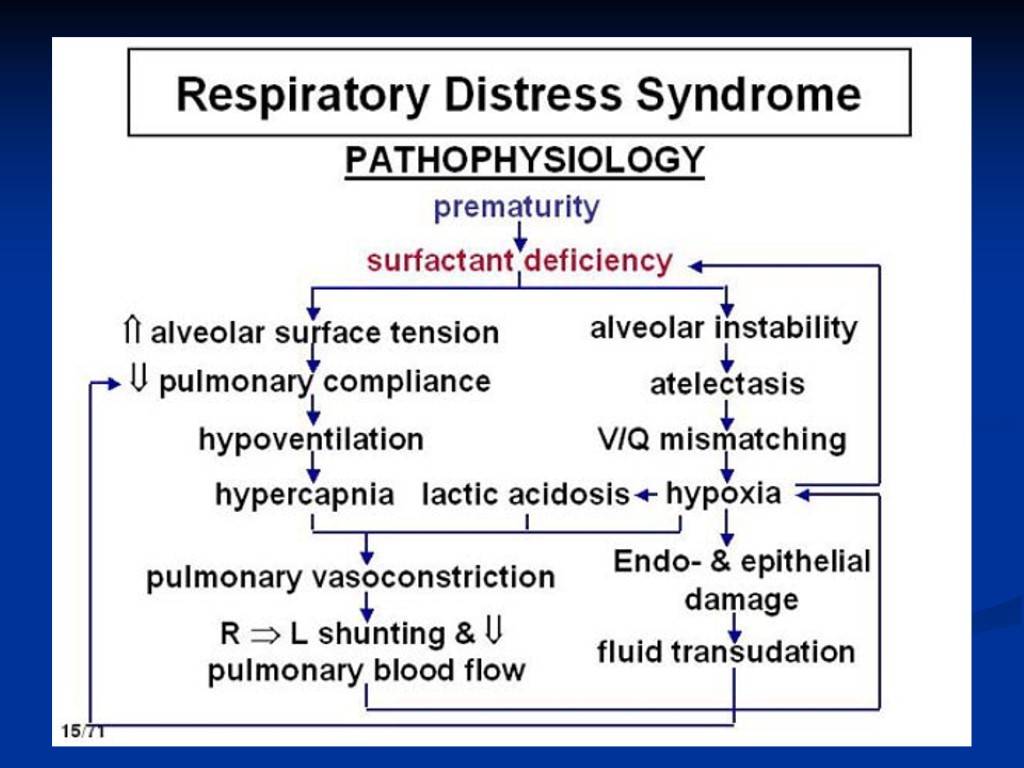
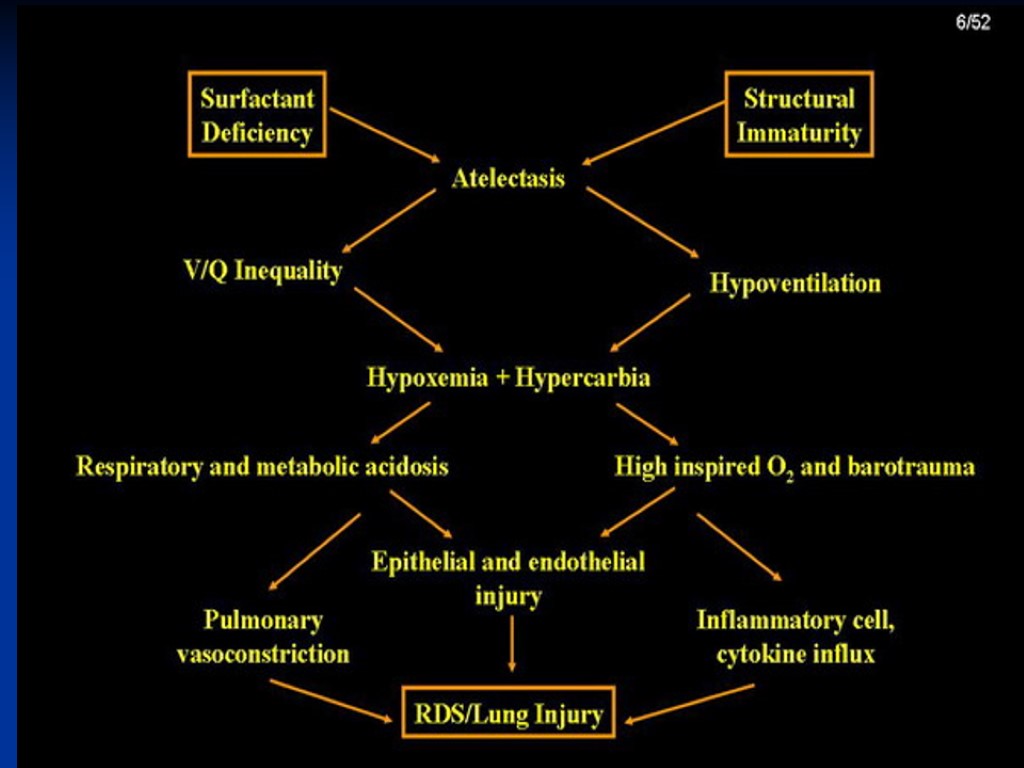
Pathways for surfactant production. There are two major pathways. The methyl pathway is functional at 22-24 weeks’ gestation but is easily inhibited by acidosis and hypoxia, hyper- and hypoglycemia, hypothermia The choline incorporation pathway matures at 32-34 weeks’ gestation and is more resistant to hypoxia and acidosis.
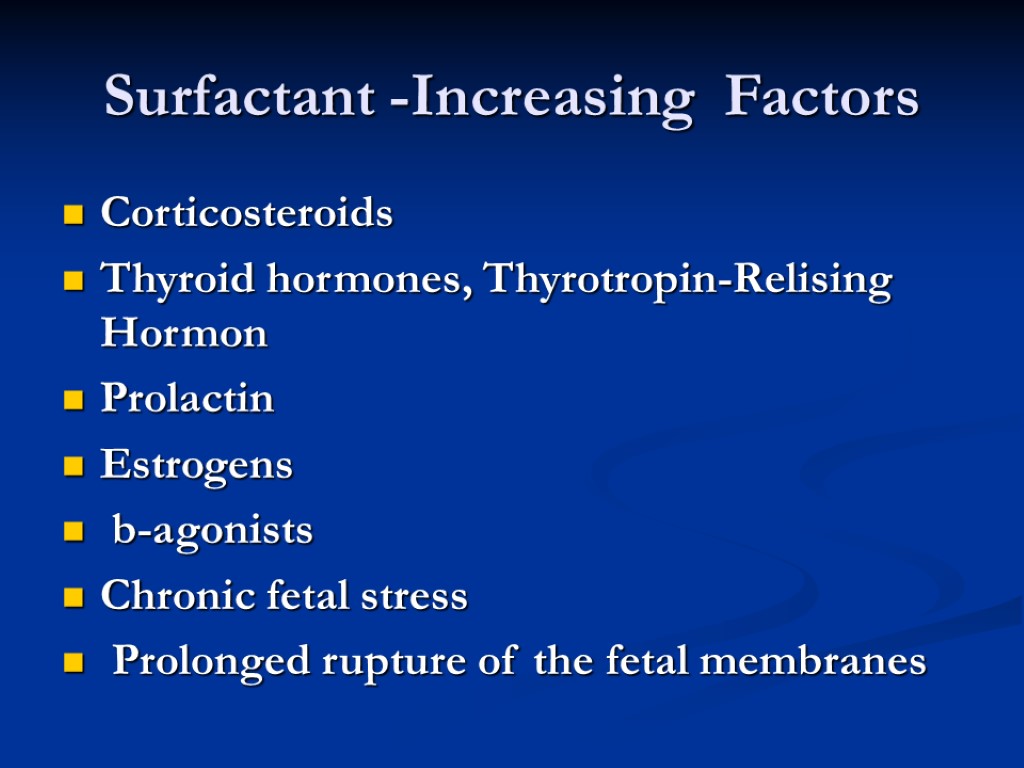
Surfactant -Increasing Factors Corticosteroids Thyroid hormones, Thyrotropin-Relising Hormon Prolactin Estrogens b-agonists Chronic fetal stress Prolonged rupture of the fetal membranes
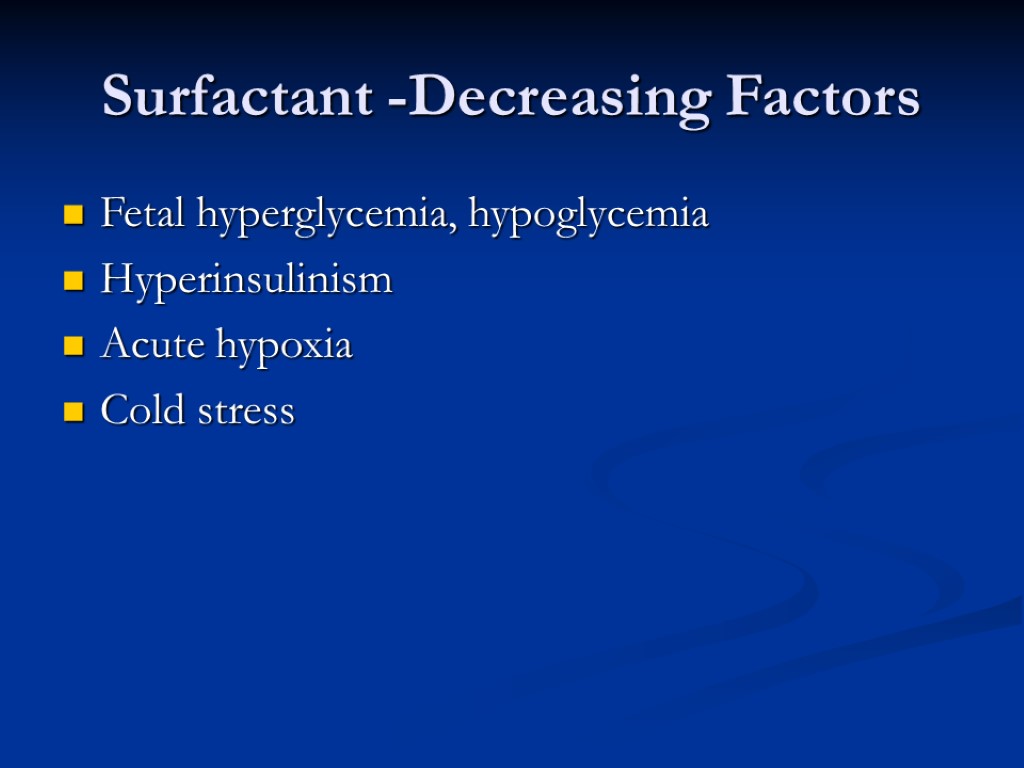
Surfactant -Decreasing Factors Fetal hyperglycemia, hypoglycemia Hyperinsulinism Acute hypoxia Cold stress
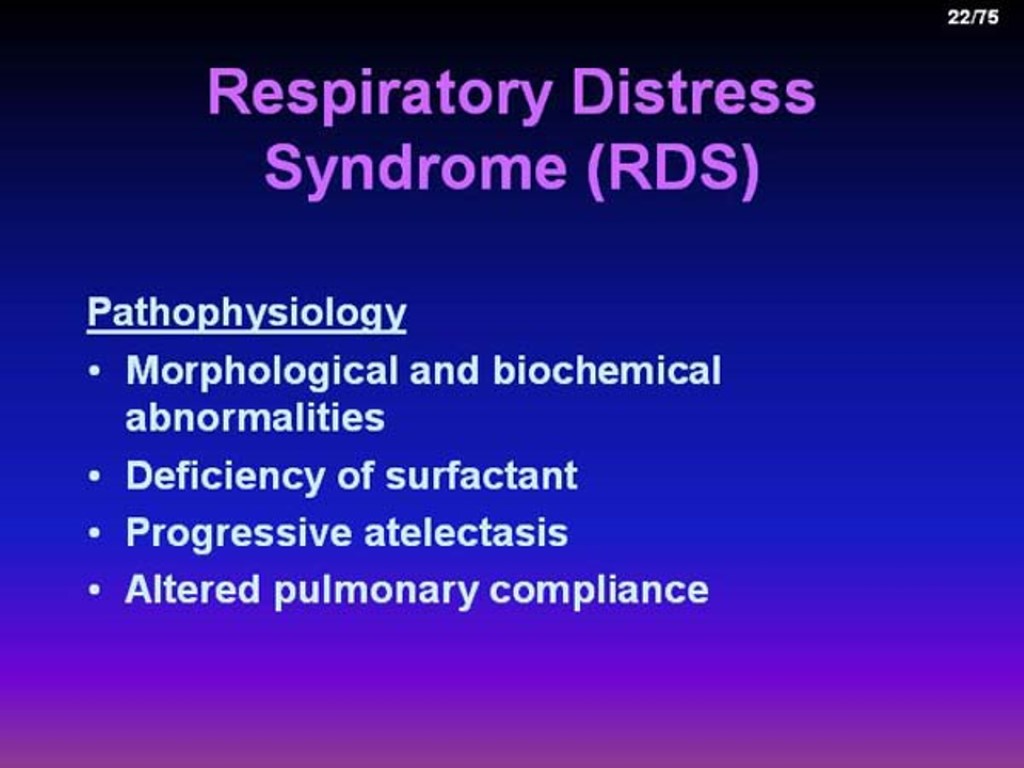
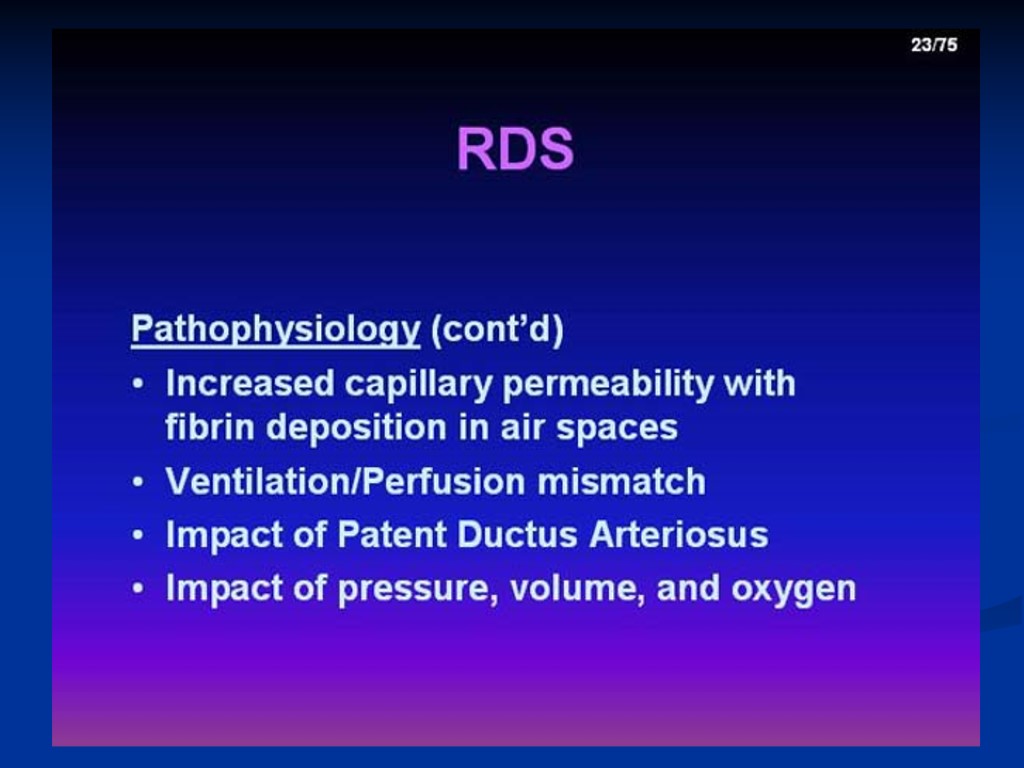
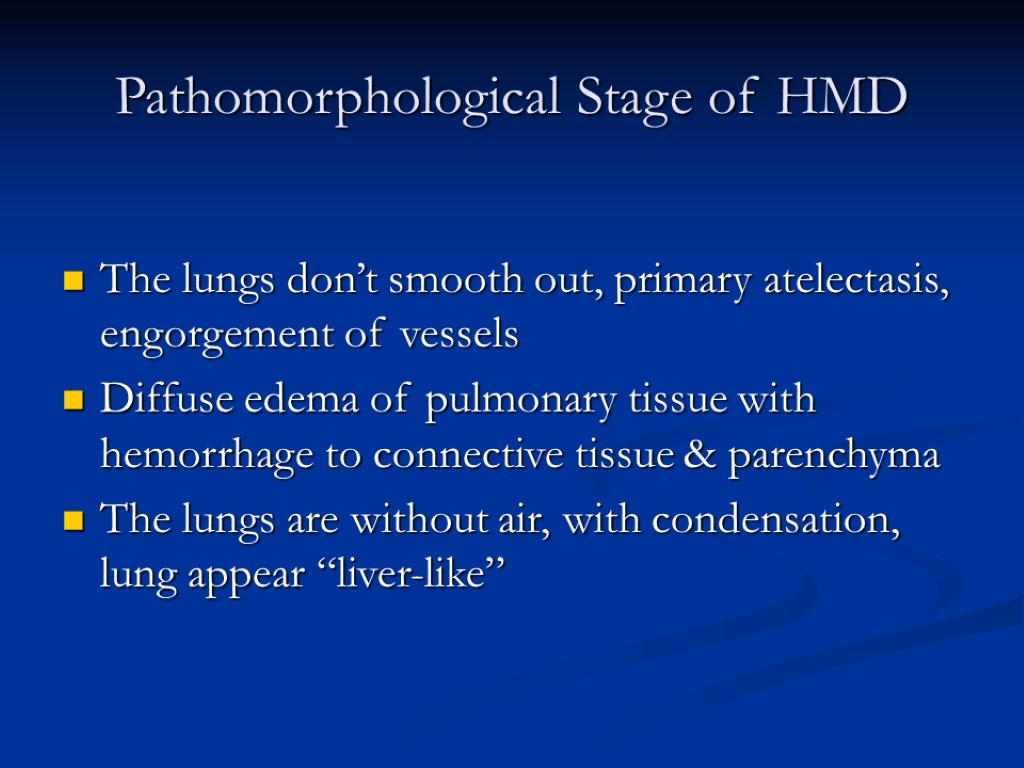
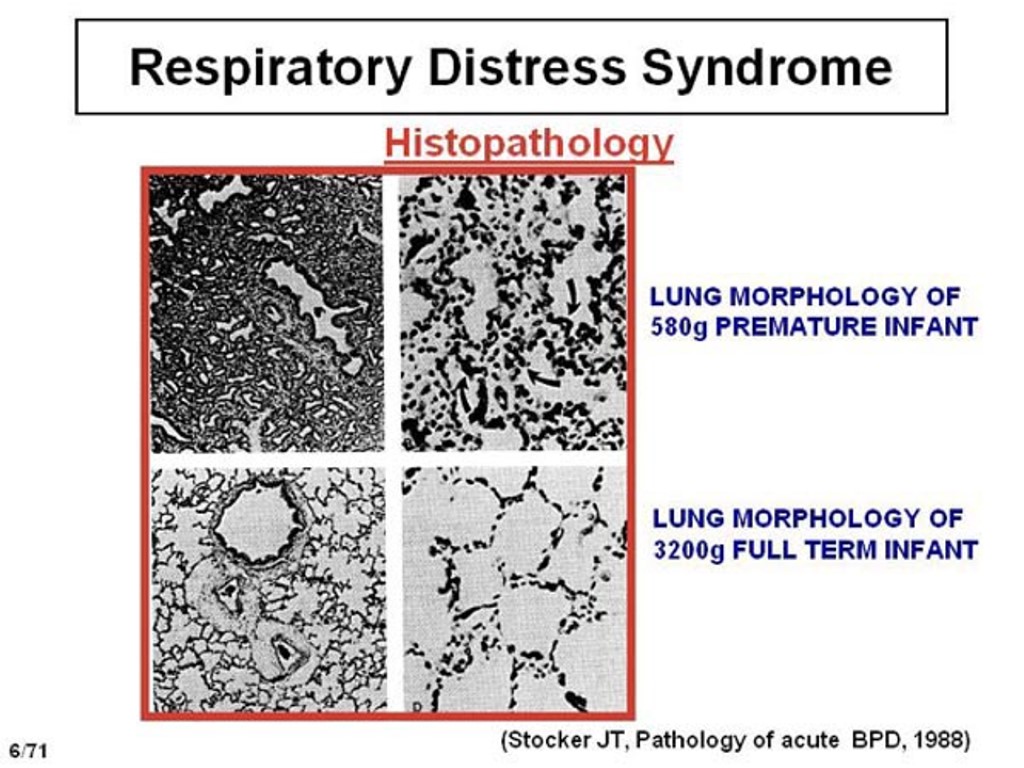
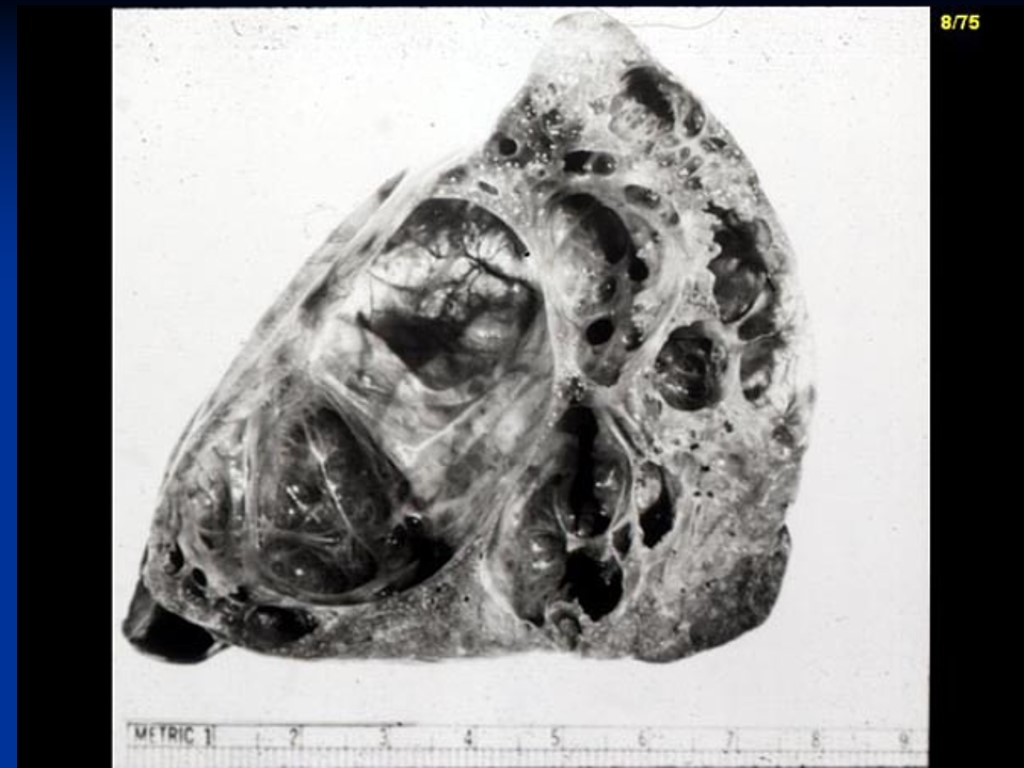
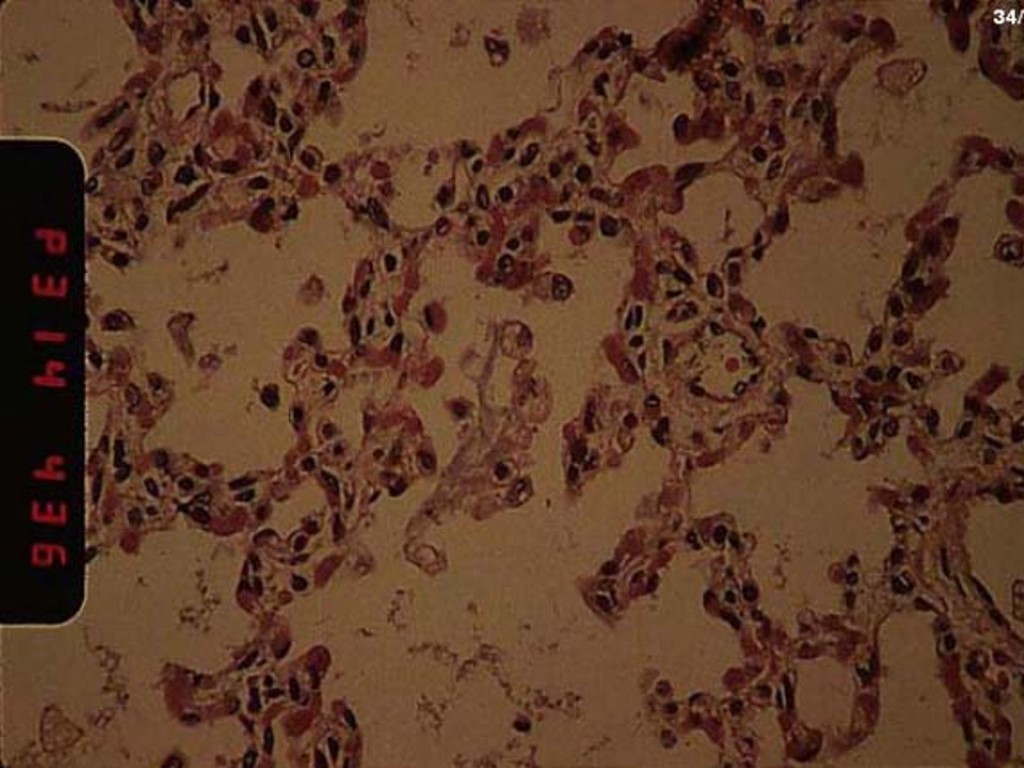
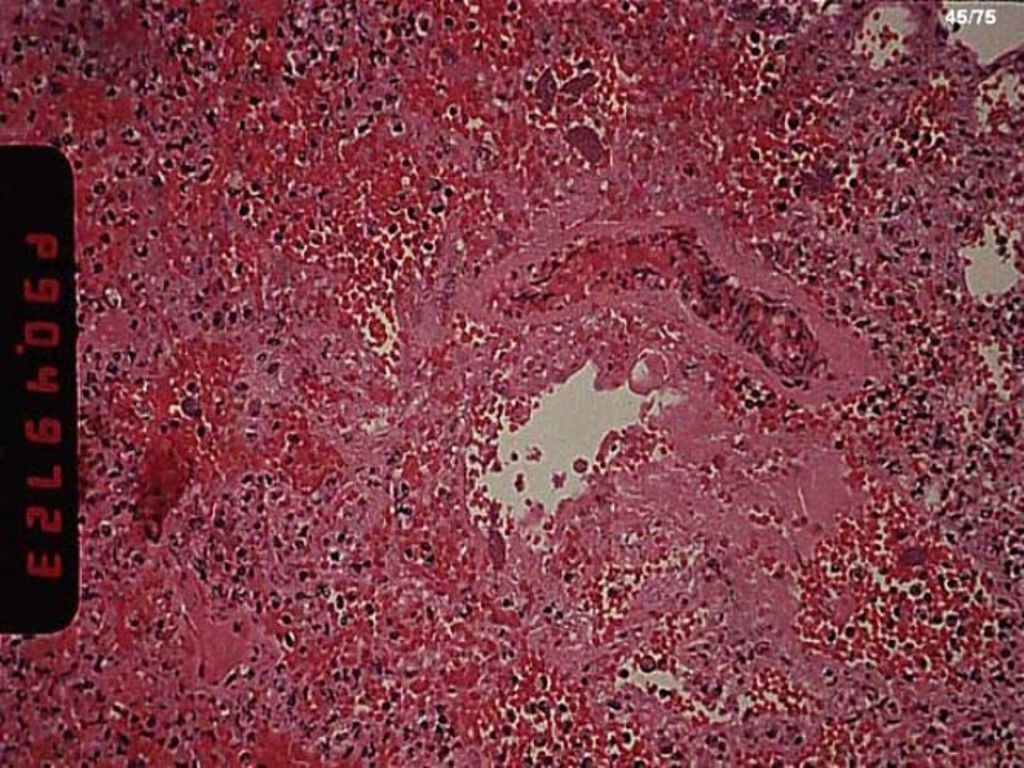
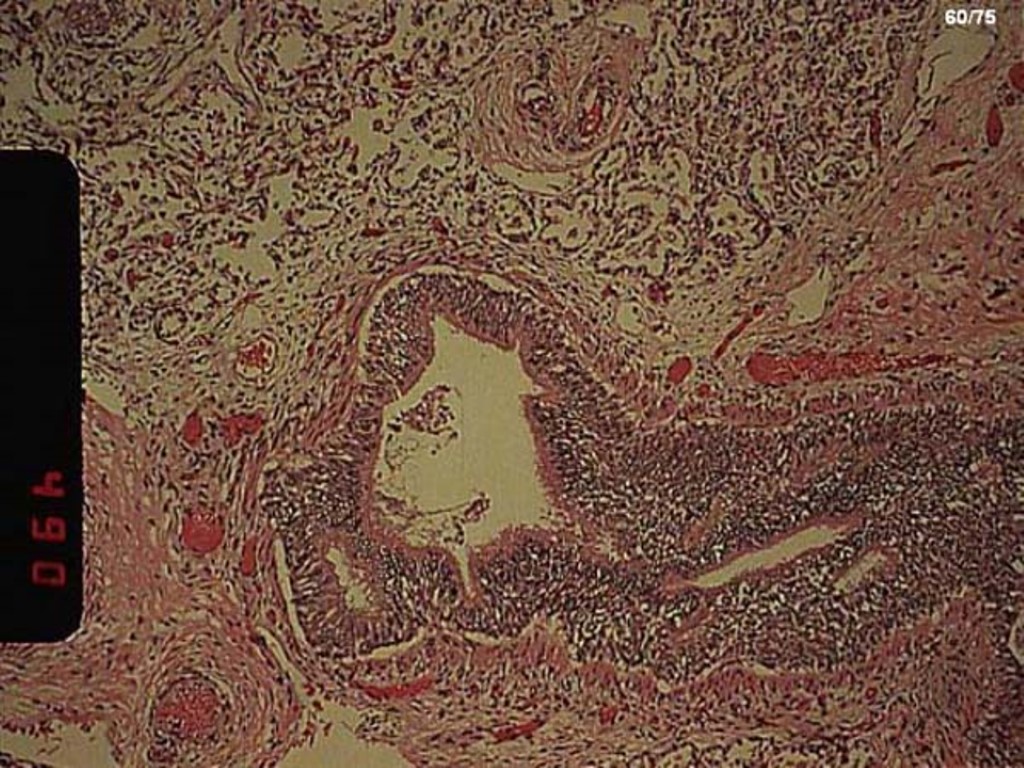
Pathomorphological Stage of HMD The lungs don’t smooth out, primary atelectasis, engorgement of vessels Diffuse edema of pulmonary tissue with hemorrhage to connective tissue & parenchyma The lungs are without air, with condensation, lung appear “liver-like”
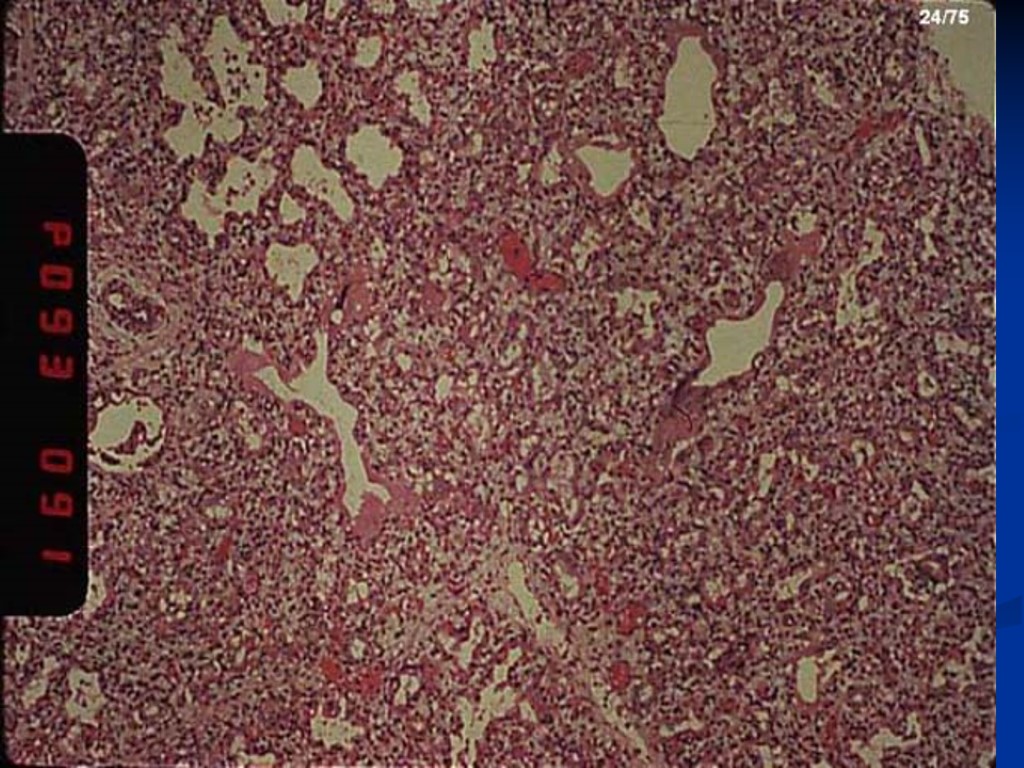
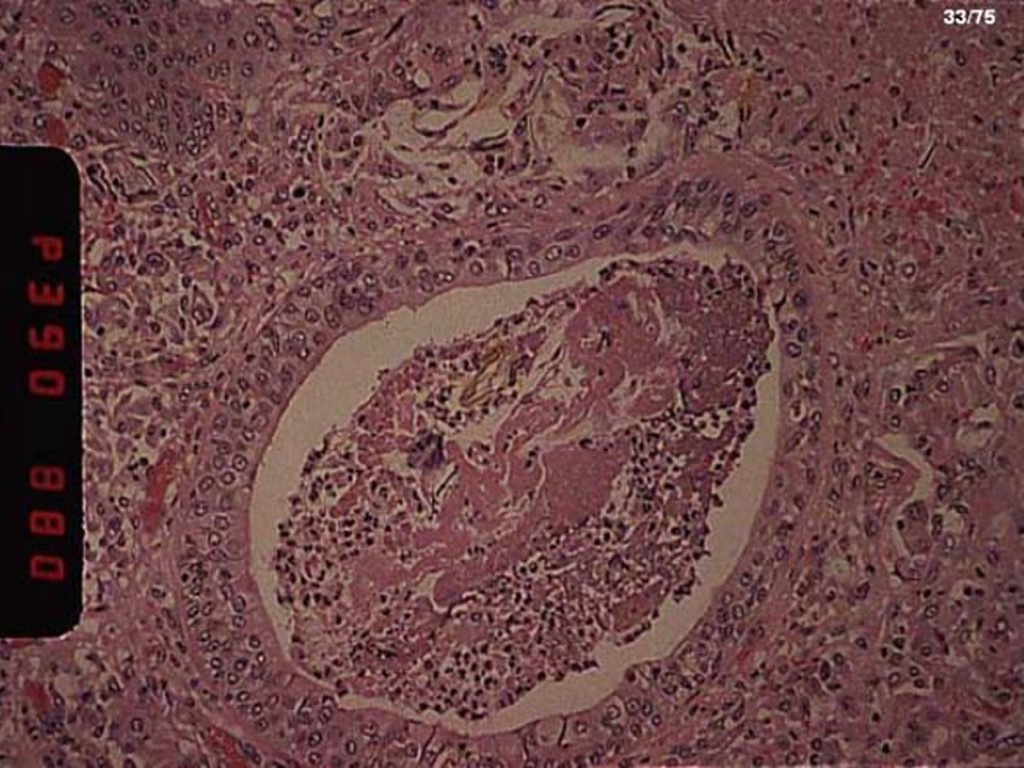
Histology of lung
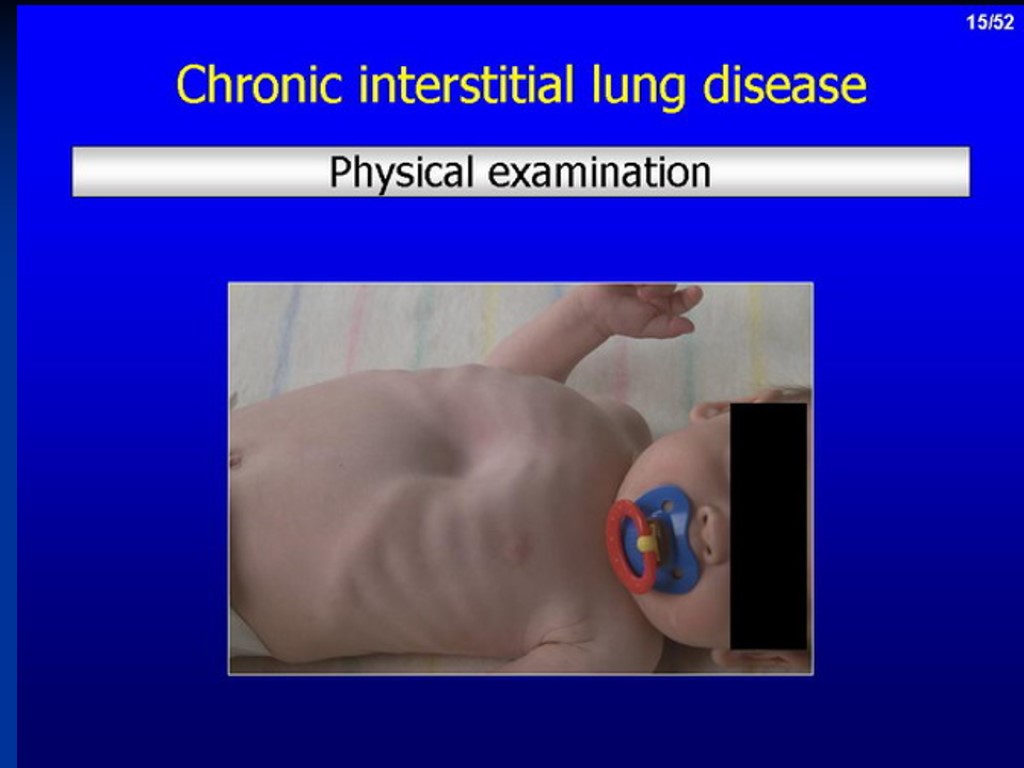
Clinical features: appear soon after birth usually < 6 hours cyanosis rapid shallow respiration >60/min expiratory audible grunting apnea Intercostal, and subcostal, and xiphoid retraction flaring of alea nasi breath sounds diminished with crepitating on deep inspiration at lung bases the general sign of hypoxia: hypotonic, hyporeflexic cardiac insufficiency, pattern ductus arteriosus


The clinical peculiarities of RDS in newborn with body weigh 1000g & < 30 weeks gestation Classic manifestations are rare Prolonged development of symptoms of RD Early sign is general cyanosis on the purple skin Upper chest intercostals & subcostal retraction Absent: nares dilatation, expiratory grant, tachipnoe
For assessment of degree of RDS Silverman scale Downes scale
Diagnosis of RDS Antenatal and intranatal period: 1. Examination of amniotic fluid Lecithin sphingomyelin ratio: >2 - full maturation 1,5-1,99-borderline maturation 1,0-1,49-mild form of HMD <1-associated with severe RDS 2. Bubble stability test: Amniotic fluid is shaken with alcohol. Production of static bubbles indicates good maturation of surfactant.
Diagnosis of RDS Postnatal period Gastric aspirate shake test should be done within one hour 0,5 ml of gastric aspirate + 1 ml absolute alcohol. Shake vigorously for 15 sec. If the bubbles cover less then 13 of liquid surface there are increased chances of RDS Low pO2<50 mm Hg pCO2>50 mm Hg Acidosis pH<7,2
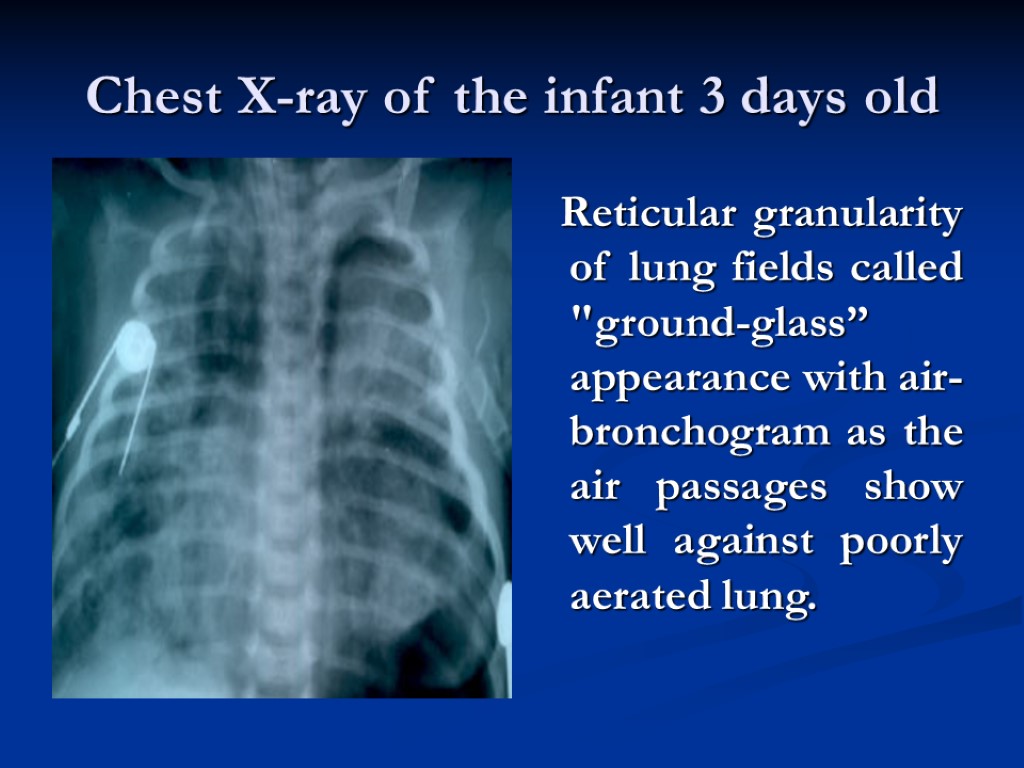
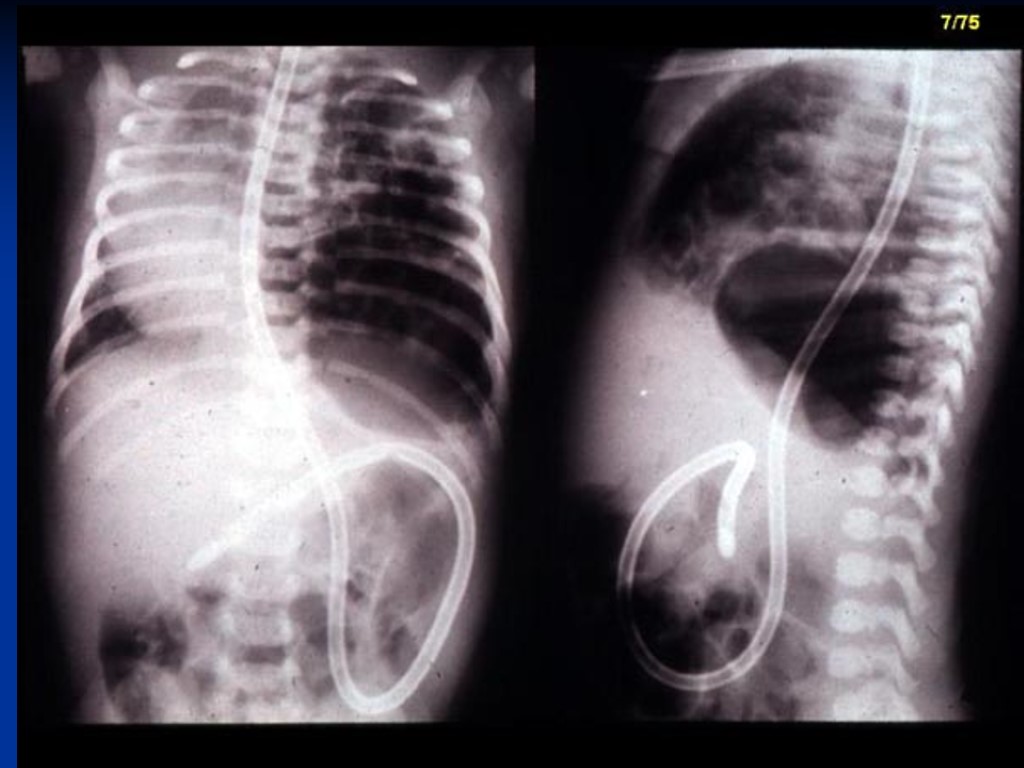
Chest X-ray of the infant 3 days old Reticular granularity of lung fields called "ground-glass” appearance with air-bronchogram as the air passages show well against poorly aerated lung.
Sings indicating bad prognosis increased apnea air hunger or hypoxia progressive cyanosis decrease or absence of grunting absent breath sounds despite chest movement hypothermia irregular breathing acidosis (death usually occurs within first 3 days)
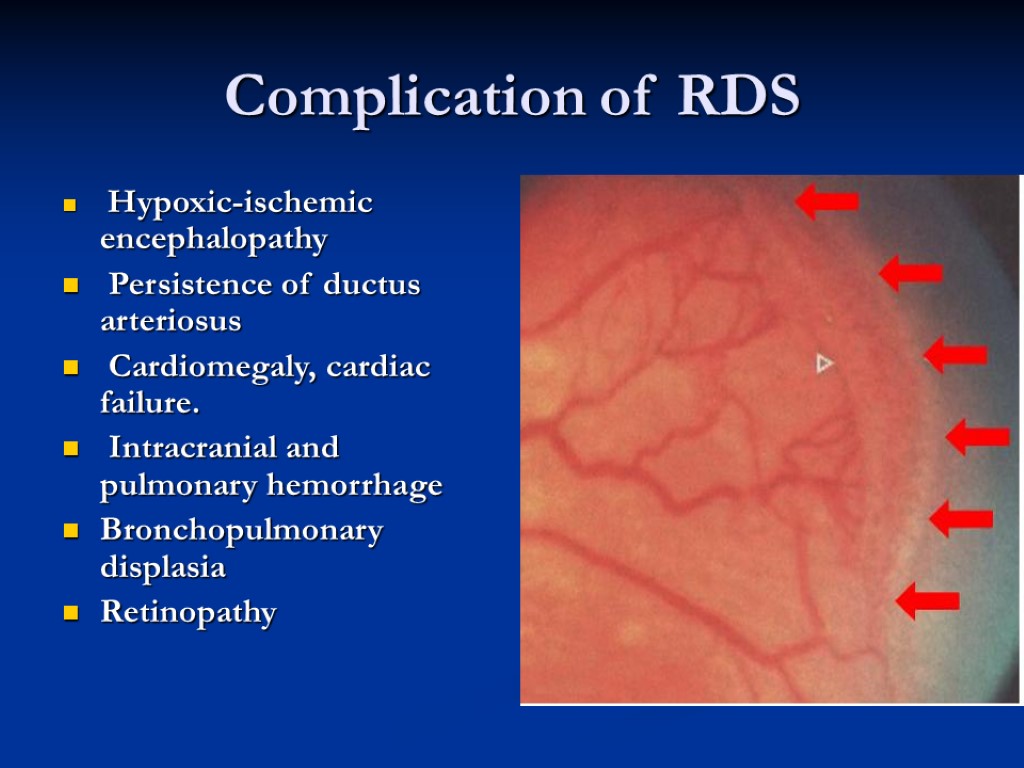
Complication of RDS Hypoxic-ischemic encephalopathy Persistence of ductus arteriosus Cardiomegaly, cardiac failure. Intracranial and pulmonary hemorrhage Bronchopulmonary displasia Retinopathy
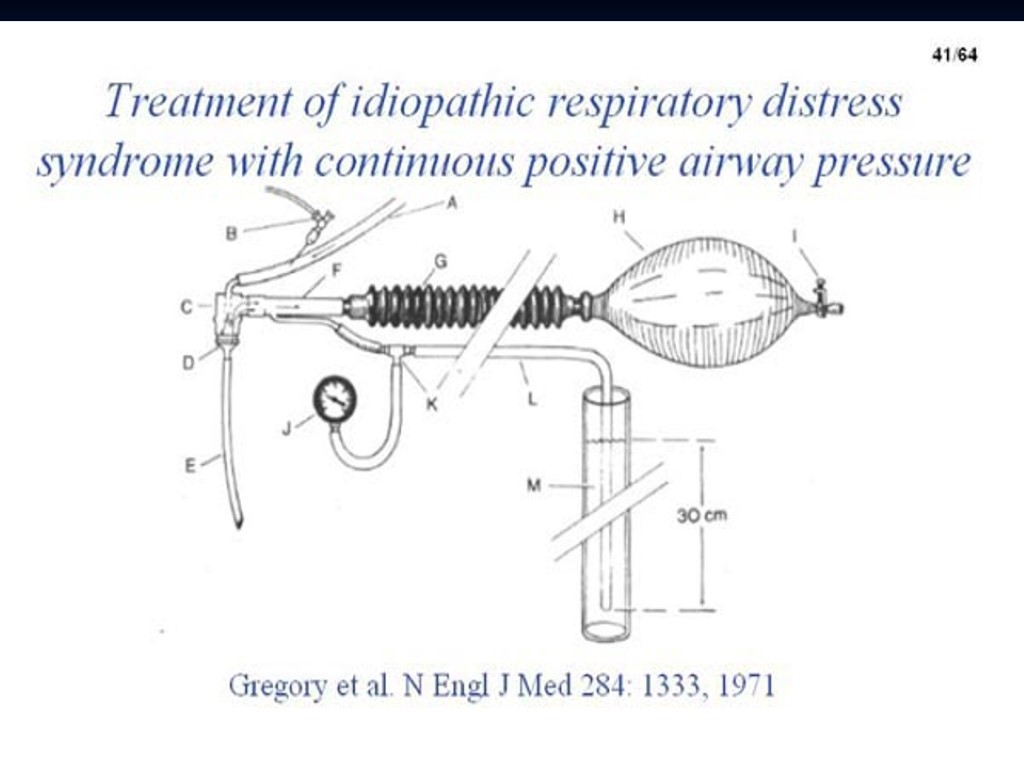
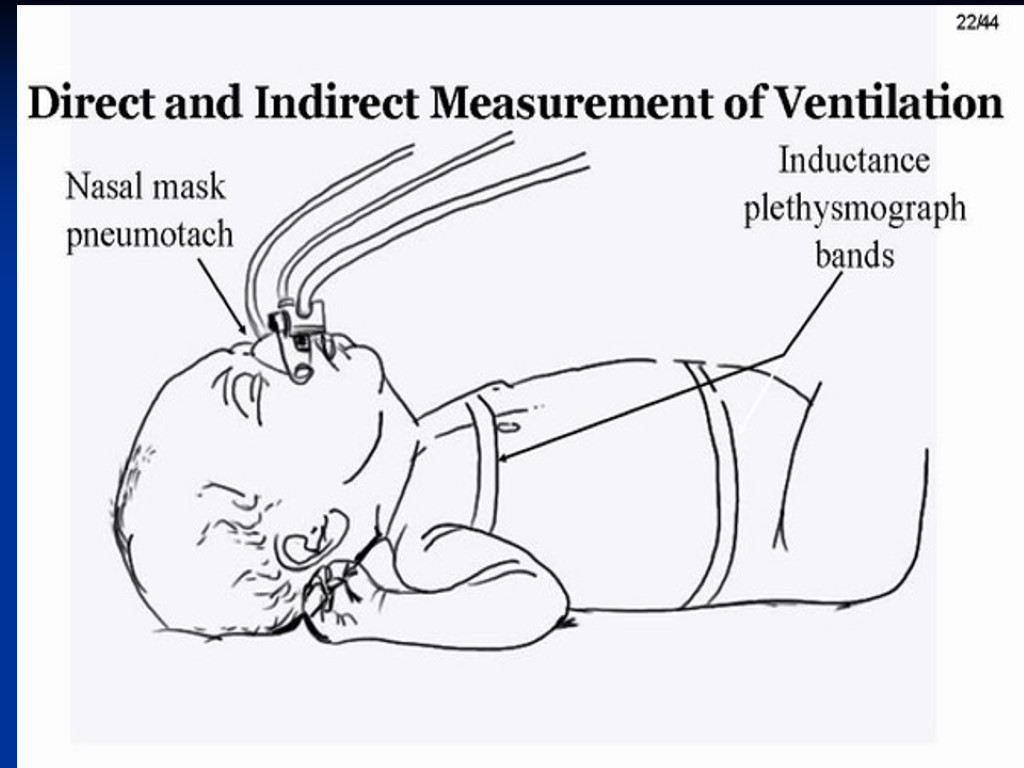
Managment “minimal child stimulation” with supplying of the normal body temperature Adequate gas exchange - oxygenation. Assisted ventilation mainly CPAP or mask and bag resuscitator or variable pressure respirator with endotracheal tube
Management (c’d) Adequate Ventilation is if pCO 2 40-60 mm Hg pO 2 50-70 mm Hg pH > 7.25 Sp O2 88-93%
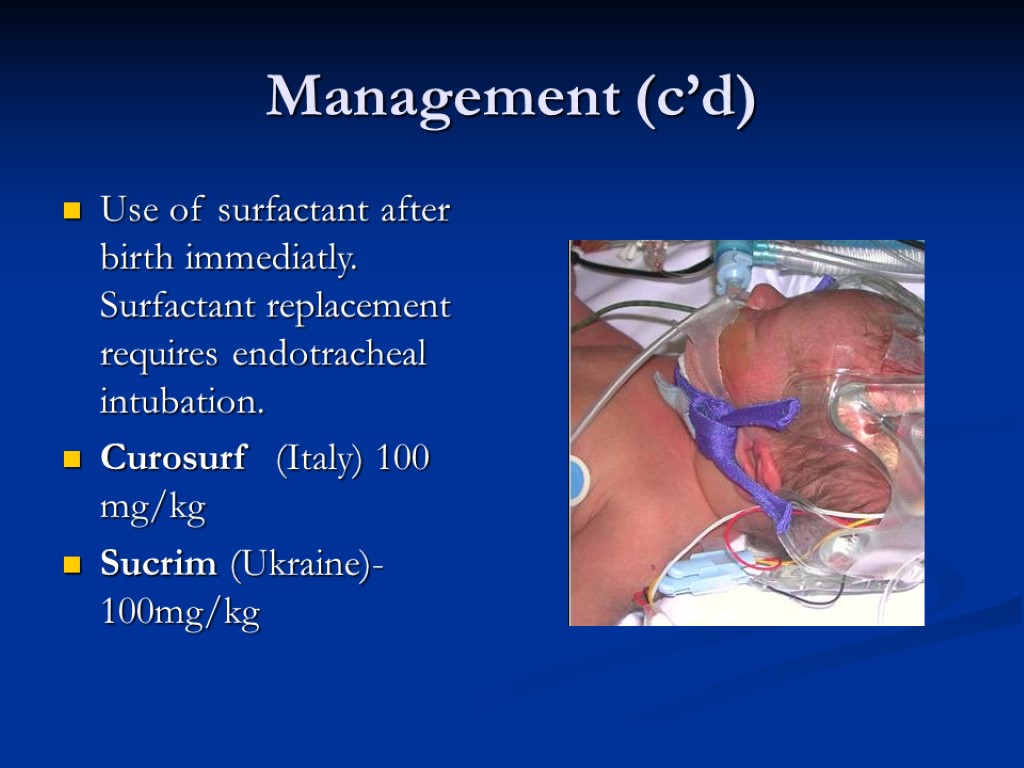
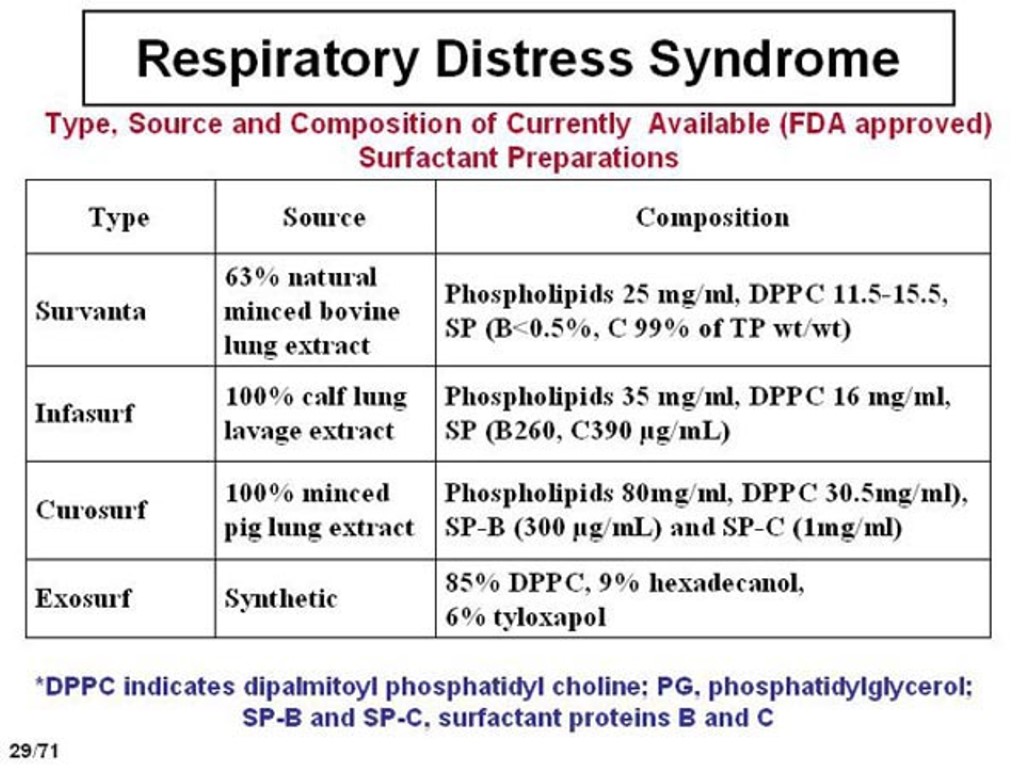
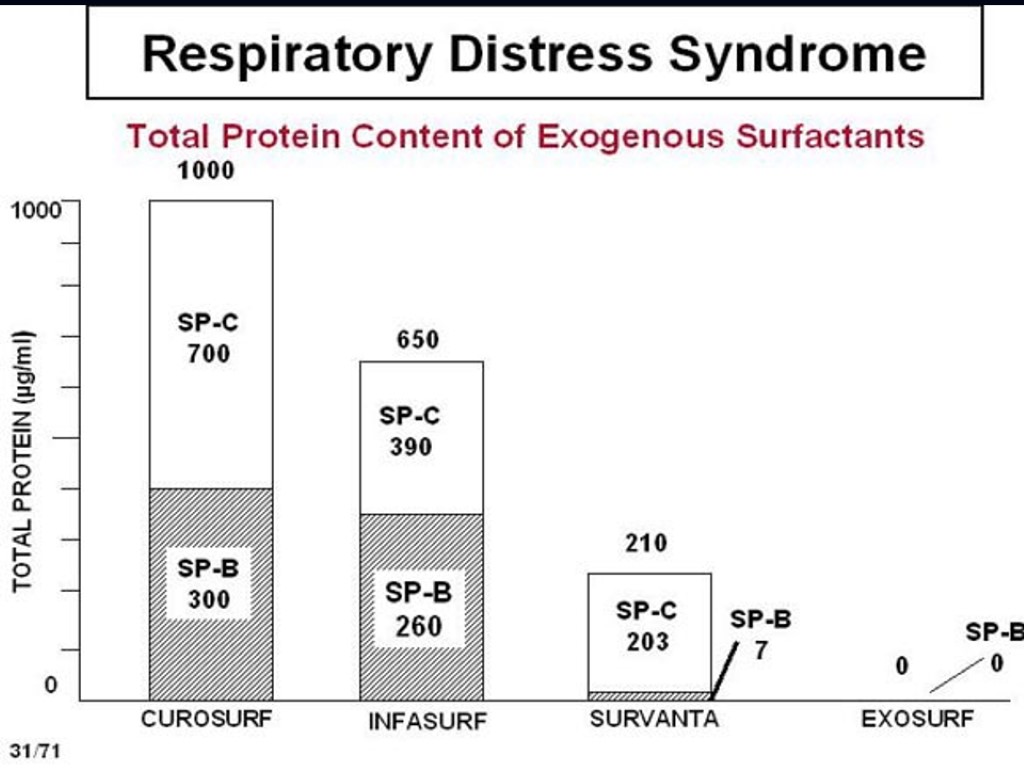
Management (c’d) Use of surfactant after birth immediatly. Surfactant replacement requires endotracheal intubation. Curosurf (Italy) 100 mg/kg Sucrim (Ukraine)- 100mg/kg
Management (c’d) Antibiotics prevent superinfection (RDS and congenital pneumonia have the same clinical picture and they can develop both)) Prevention and treatment hypoglycemia, hypocalcaemia and hemorrhage
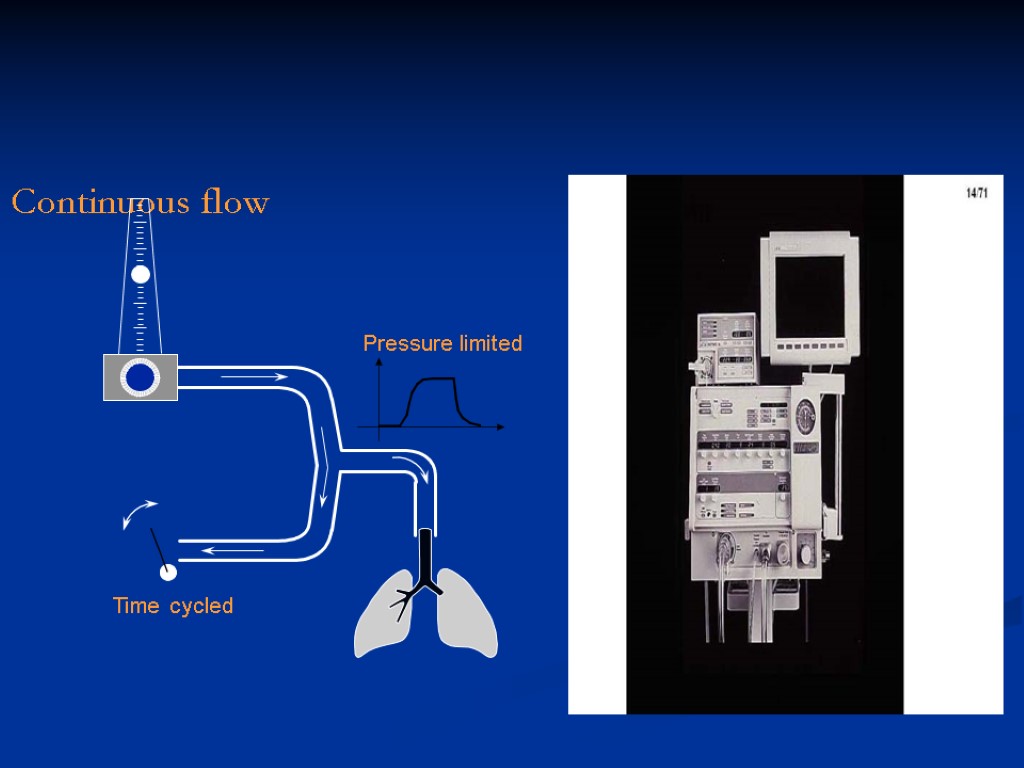
Continuous flow

RDS
RDS


RDS
Prevention of RDS. prevention of prematurity managment of high risk pregnancy and labour antenatal administration of synthetic steroid to mother 24 to 72 hours prior to delivery. Betamethasone acetate 6 mg or 6 mg Betamethasone phosphate (antenatal using of GCS decrease the RDS, death, IVH, NEC, PDA, BPD (Evidence Medicine))
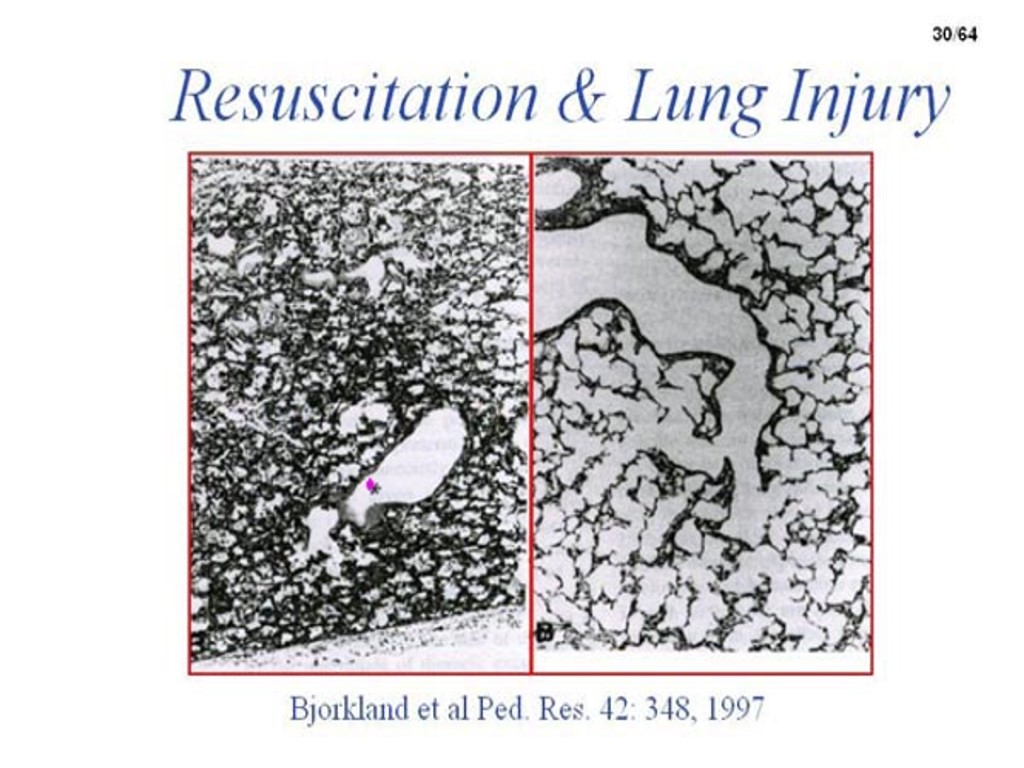
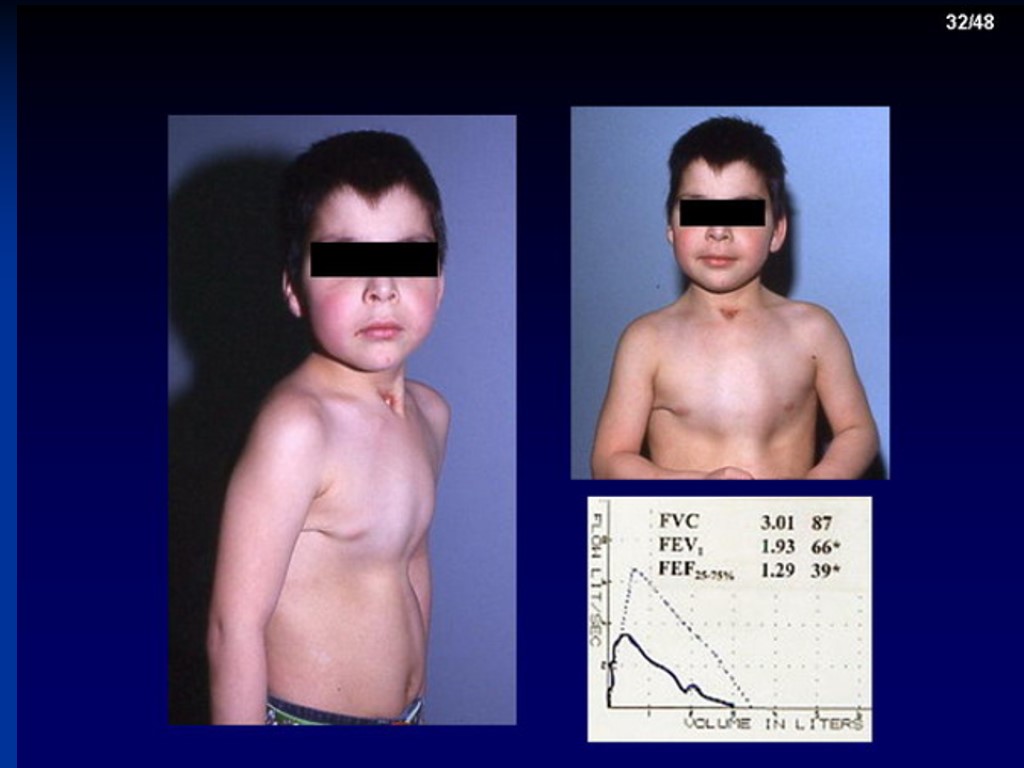
Ventilation’s Complications Persistent pulmonary hypertension Pneumotorax Emphysema Cardiac failure, PDA, hypovolemia Intaventricular hemorrhage Sepsis,pneumonia BPD (death due to RS – viral infection) Retinopathy (blind infant) Neurological pathology

CDH

MAS
MAS
MAS
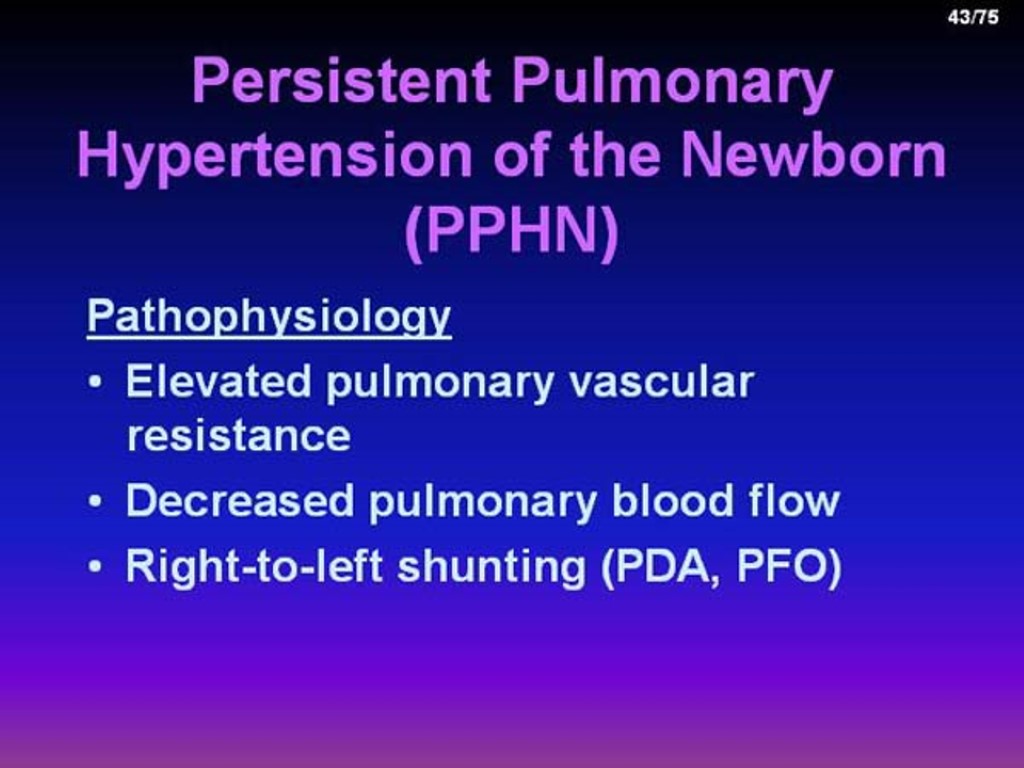
PPHN
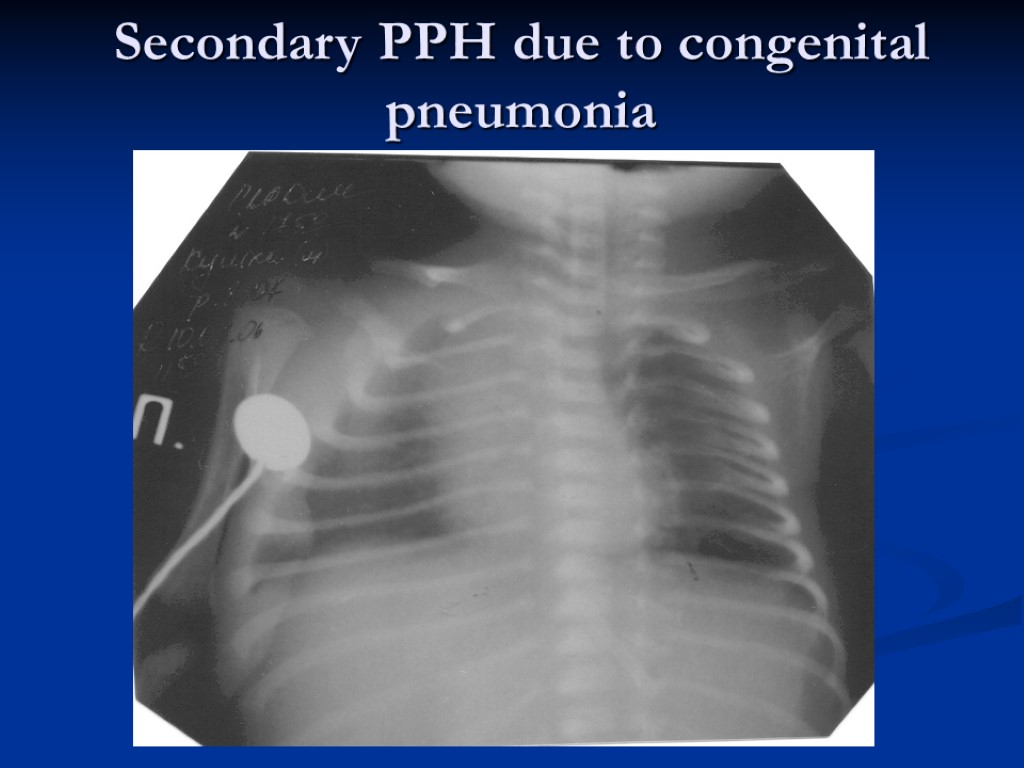
Secondary PPH due to congenital pneumonia
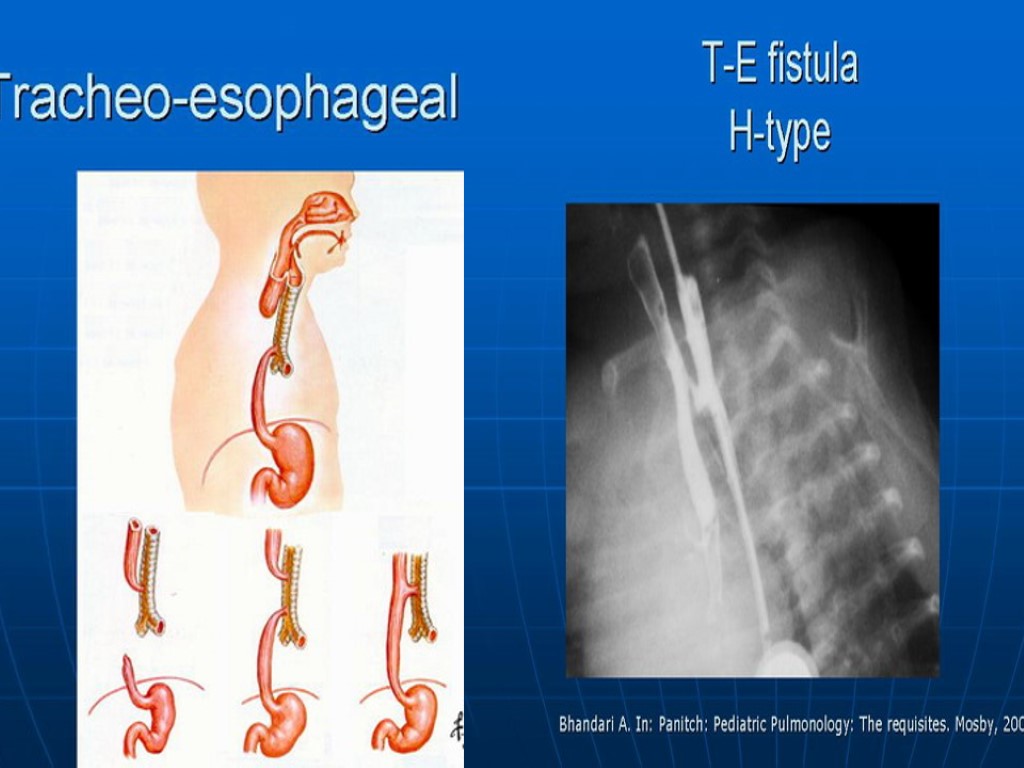
???
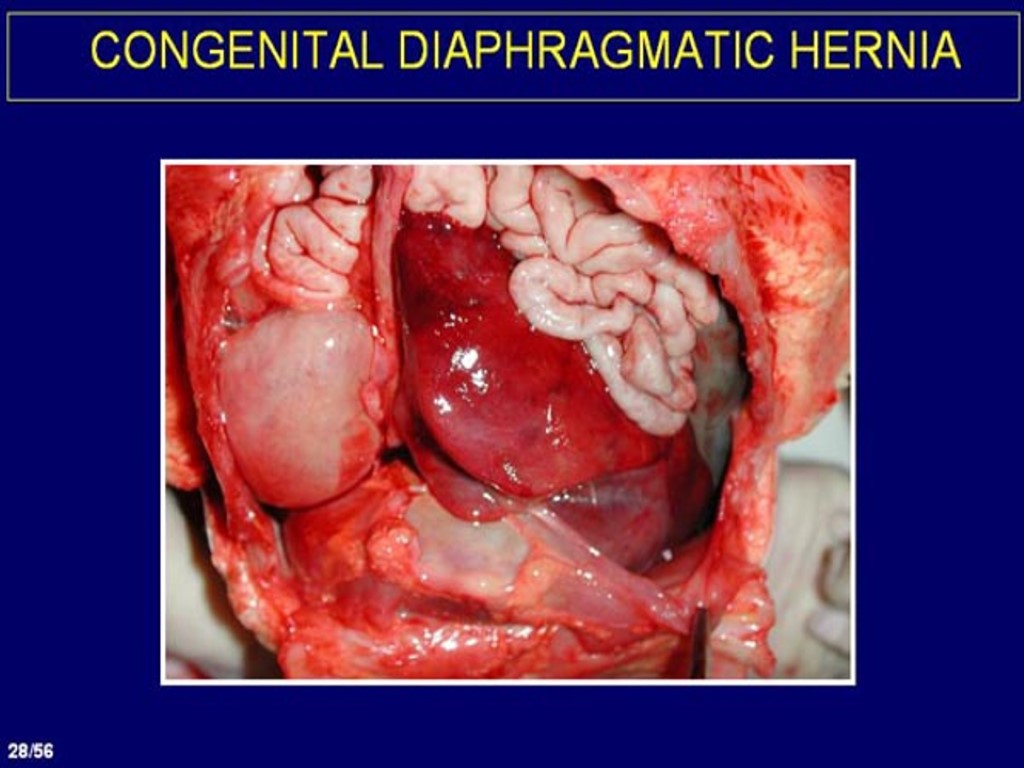
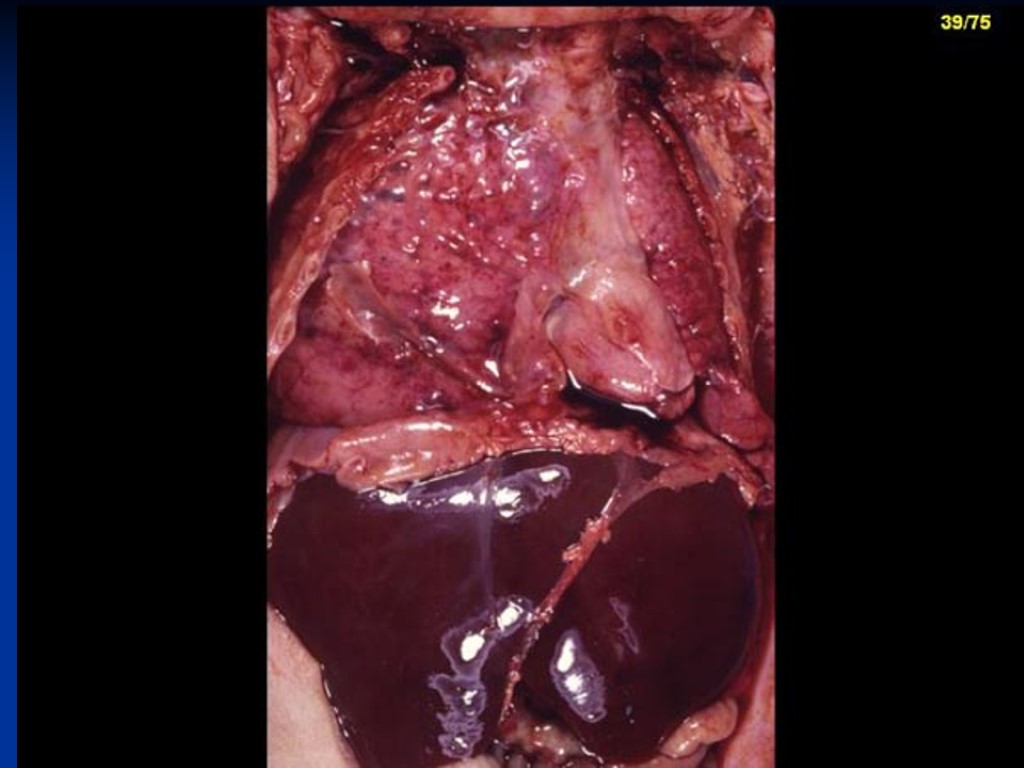
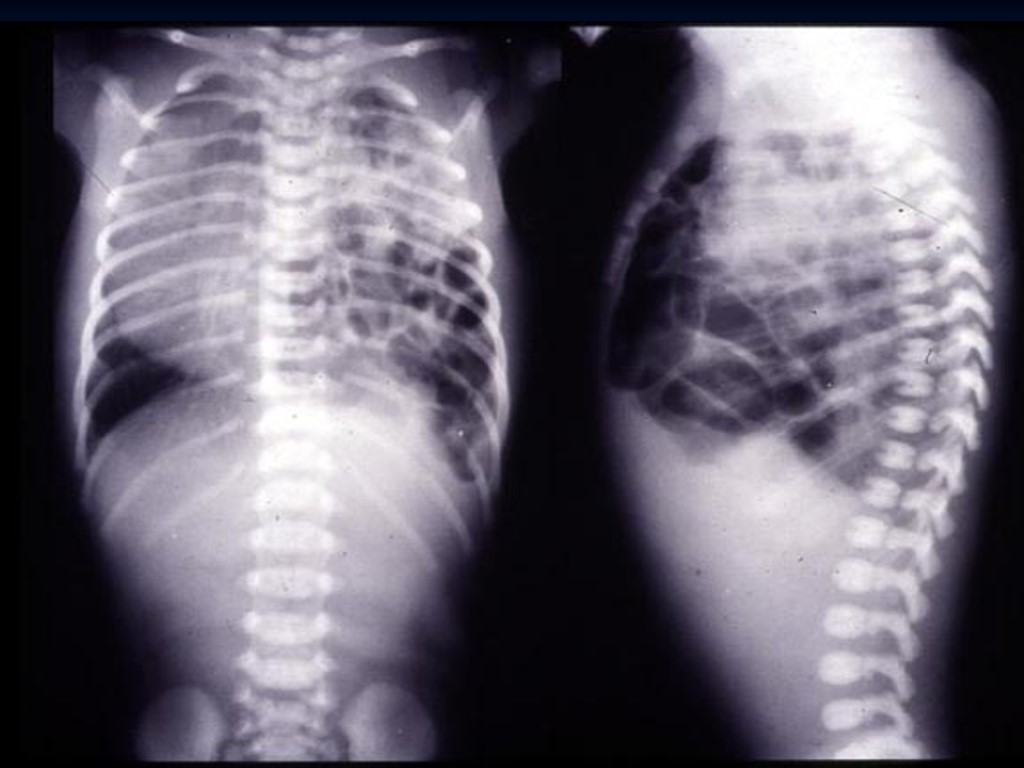
CDH
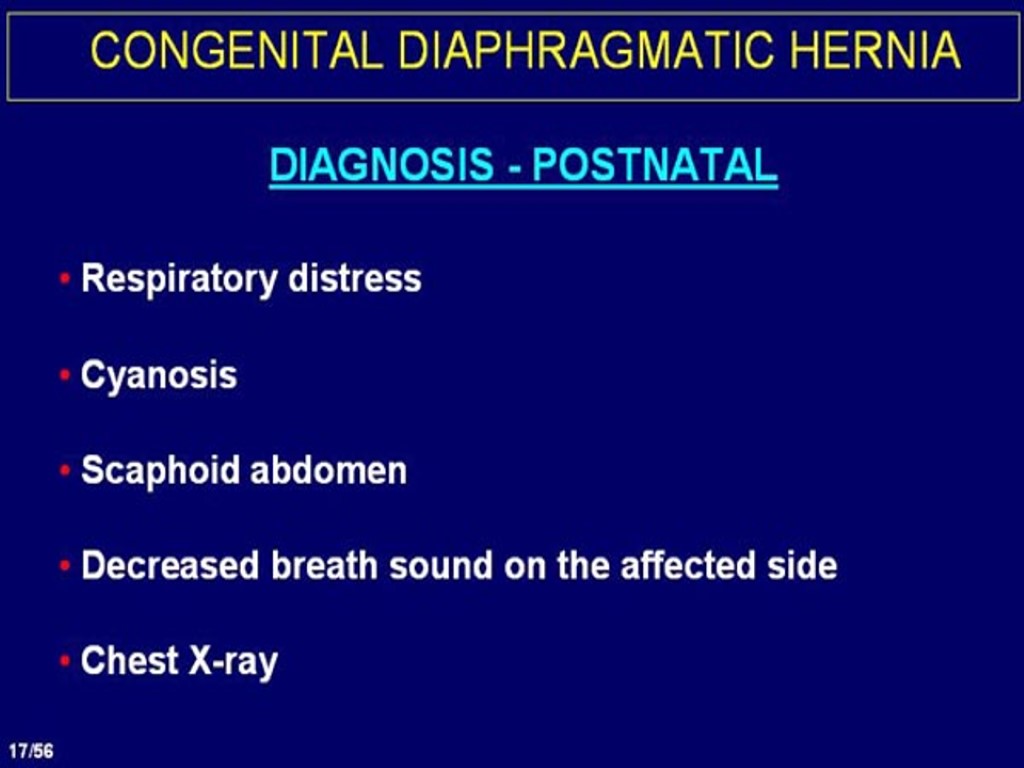
CDH

CDH
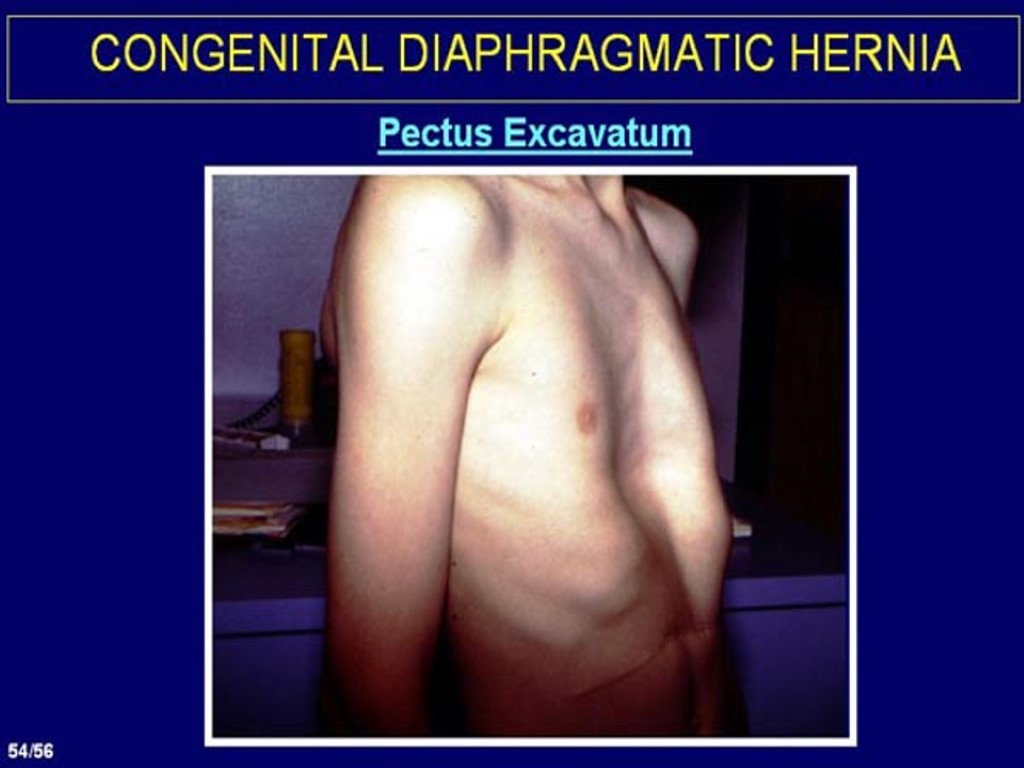
CDH
RDS
PPHN
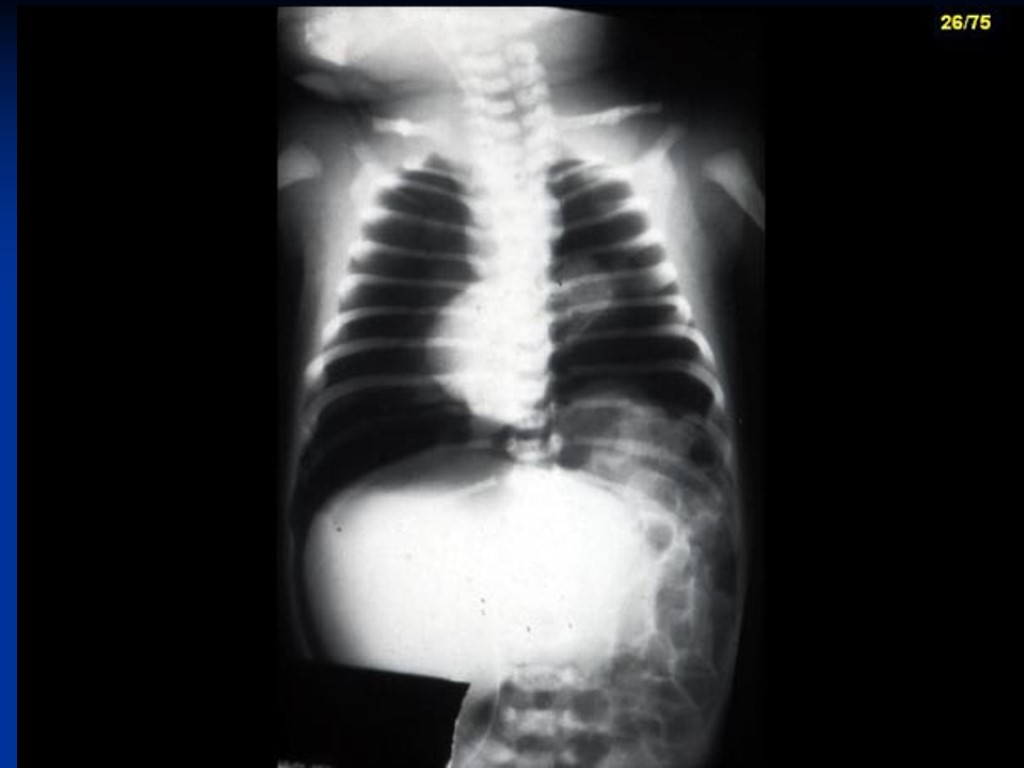
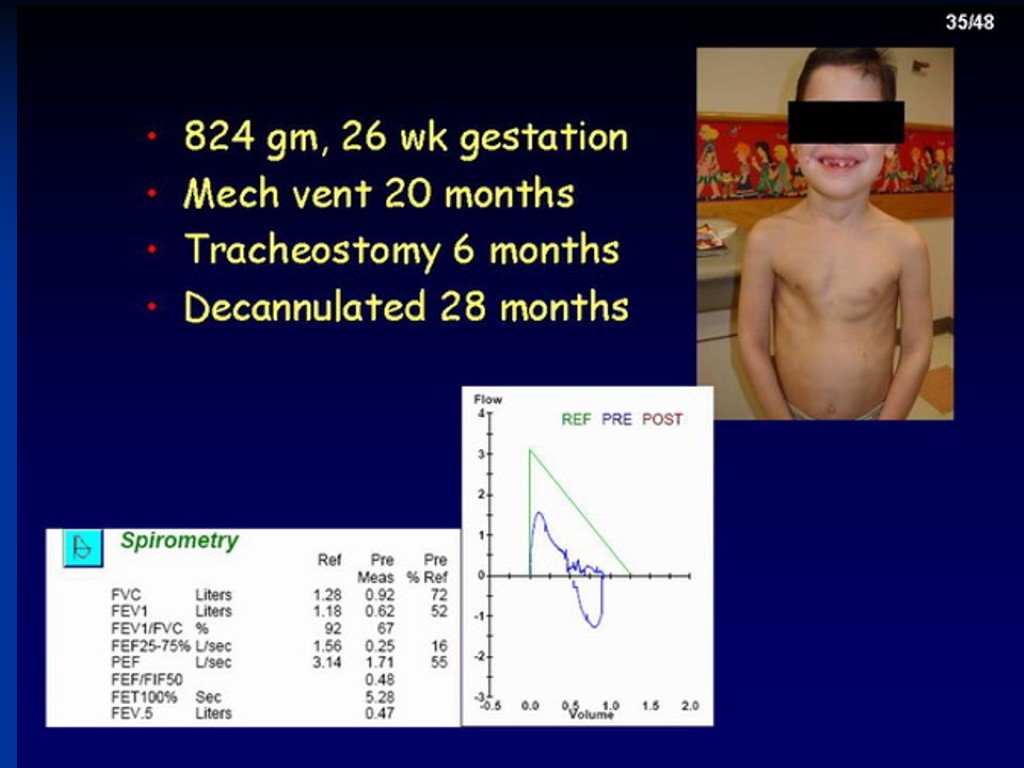
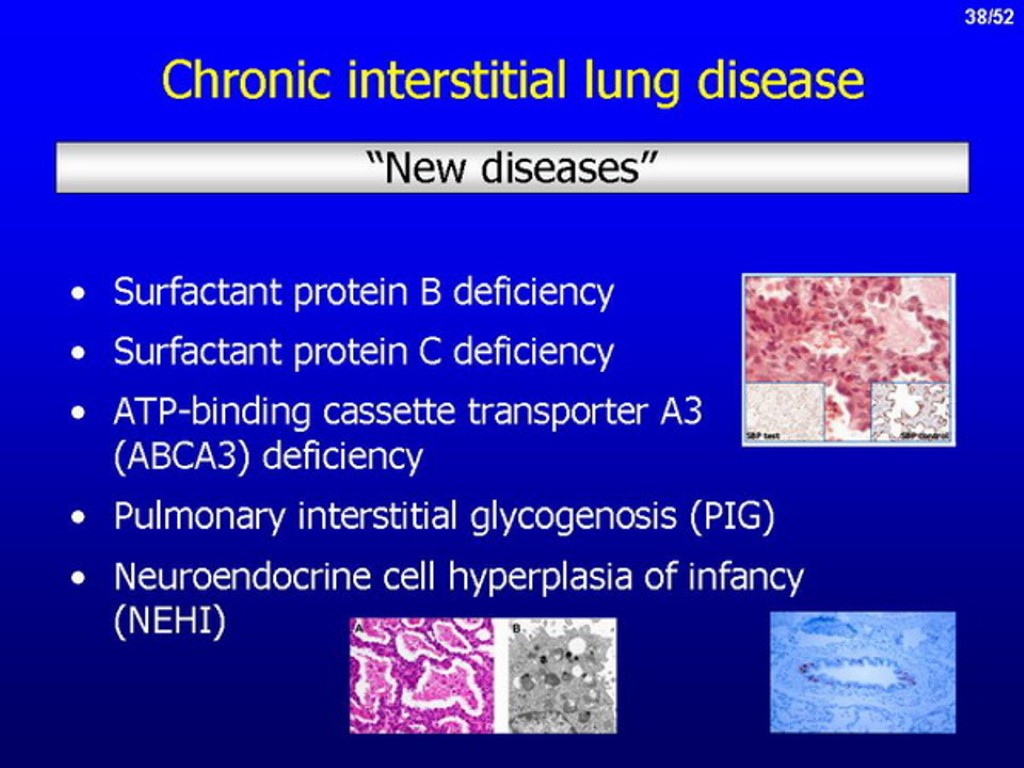
BPD
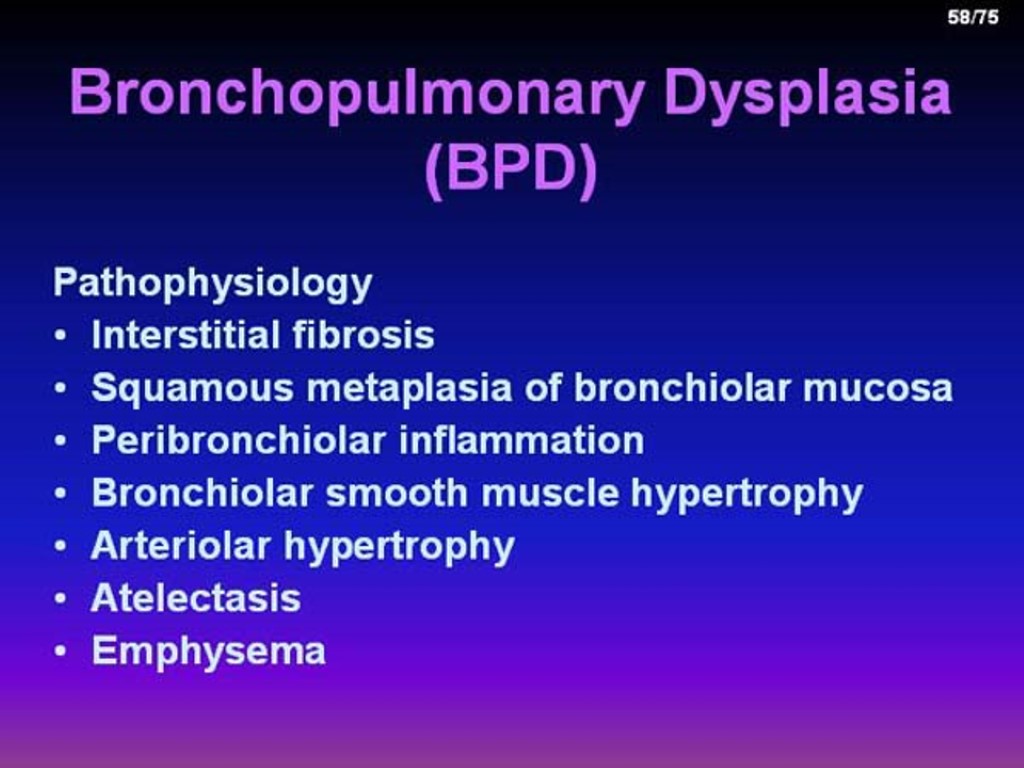
BPD
BPD

Thank you !!!
respiratory_distress_syndrom.ppt
- Количество слайдов: 80

