Дыхание.ppt
- Количество слайдов: 94
 RESPIRATION
RESPIRATION
 RESPIRATION Introduction Containing: inspiration & expiration Functions: Obtain O 2 from external environment Remove CO 2 form the body Respiratory processes: Pulmonary ventilation Gas exchange in the lung Gas transport in the blood Gas exchange in the tissue
RESPIRATION Introduction Containing: inspiration & expiration Functions: Obtain O 2 from external environment Remove CO 2 form the body Respiratory processes: Pulmonary ventilation Gas exchange in the lung Gas transport in the blood Gas exchange in the tissue
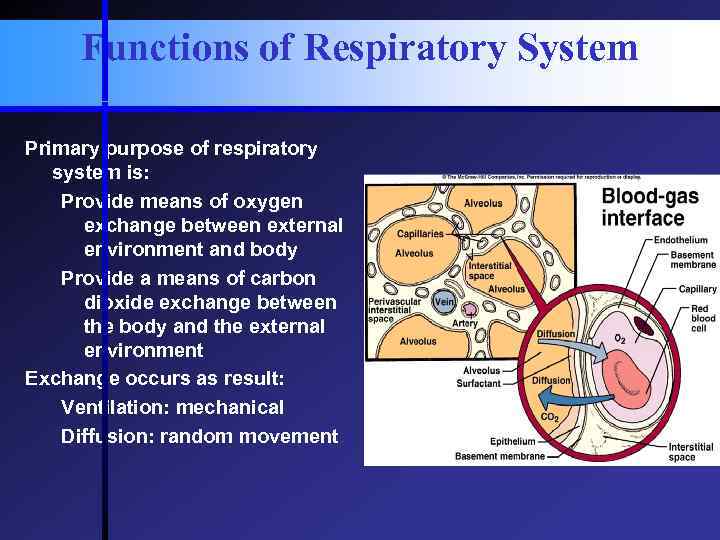 Functions of Respiratory System Primary purpose of respiratory system is: Provide means of oxygen exchange between external environment and body Provide a means of carbon dioxide exchange between the body and the external environment Exchange occurs as result: Ventilation: mechanical Diffusion: random movement
Functions of Respiratory System Primary purpose of respiratory system is: Provide means of oxygen exchange between external environment and body Provide a means of carbon dioxide exchange between the body and the external environment Exchange occurs as result: Ventilation: mechanical Diffusion: random movement
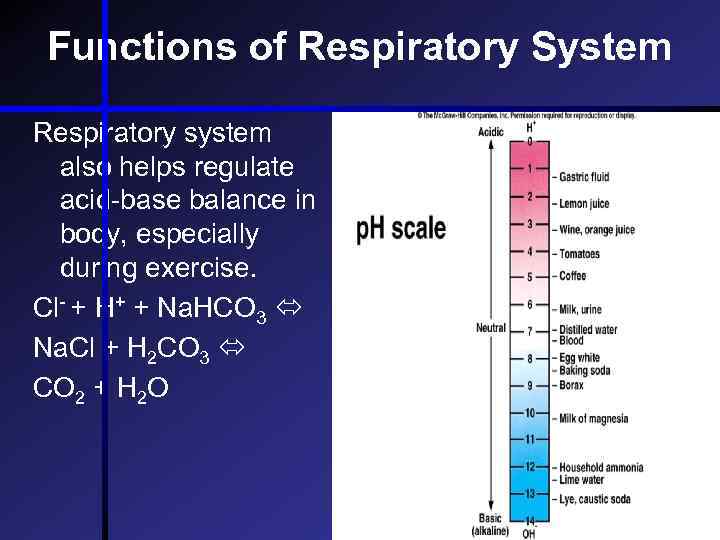 Functions of Respiratory System Respiratory system also helps regulate acid-base balance in body, especially during exercise. Cl- + H+ + Na. HCO 3 Na. Cl + H 2 CO 3 CO 2 + H 2 O
Functions of Respiratory System Respiratory system also helps regulate acid-base balance in body, especially during exercise. Cl- + H+ + Na. HCO 3 Na. Cl + H 2 CO 3 CO 2 + H 2 O
 Functional Zones of Air Passages • Conducting zone – passageways leading to respiratory zone – area where no gas exchange occurs – nasal cavity, pharynx, larynx, trachea, bronchioles • Respiratory zone – where gas exchange actually occurs – alveoli
Functional Zones of Air Passages • Conducting zone – passageways leading to respiratory zone – area where no gas exchange occurs – nasal cavity, pharynx, larynx, trachea, bronchioles • Respiratory zone – where gas exchange actually occurs – alveoli
 Roles of Conducting Zone • • Warms air Mucus traps small particles Cilia sweep particles upwards Macrophages engulf foreign particles
Roles of Conducting Zone • • Warms air Mucus traps small particles Cilia sweep particles upwards Macrophages engulf foreign particles
 Roles of Respiratory Zone • Provides large surface area for gas exchange – 300 million alveoli – Total surface area is 60 – 80 square meters or about size of half a tennis court • Provides a very thin barrier for gas exchange – 2 cell layers thick
Roles of Respiratory Zone • Provides large surface area for gas exchange – 300 million alveoli – Total surface area is 60 – 80 square meters or about size of half a tennis court • Provides a very thin barrier for gas exchange – 2 cell layers thick
 Alveoli • Type II alveolar cells secrete pulmonary surfactant – form a monomolecular layer over alveolar surfaces – surfactant stabilizes alveolar volume by reducing surface tension created by moisture
Alveoli • Type II alveolar cells secrete pulmonary surfactant – form a monomolecular layer over alveolar surfaces – surfactant stabilizes alveolar volume by reducing surface tension created by moisture
 § 1. Pulmonary ventilation Definition Principles of pulmonary ventilation * Driving force Direct ~: pressure changes in alveoli Source ~: contraction of respiratory muscles Inspiratory muscles: Diaphragm, External intercostal muscle Expiratory muscles: Diaphragm, Ext- & Internal intercostals Accessory respiratory muscles
§ 1. Pulmonary ventilation Definition Principles of pulmonary ventilation * Driving force Direct ~: pressure changes in alveoli Source ~: contraction of respiratory muscles Inspiratory muscles: Diaphragm, External intercostal muscle Expiratory muscles: Diaphragm, Ext- & Internal intercostals Accessory respiratory muscles
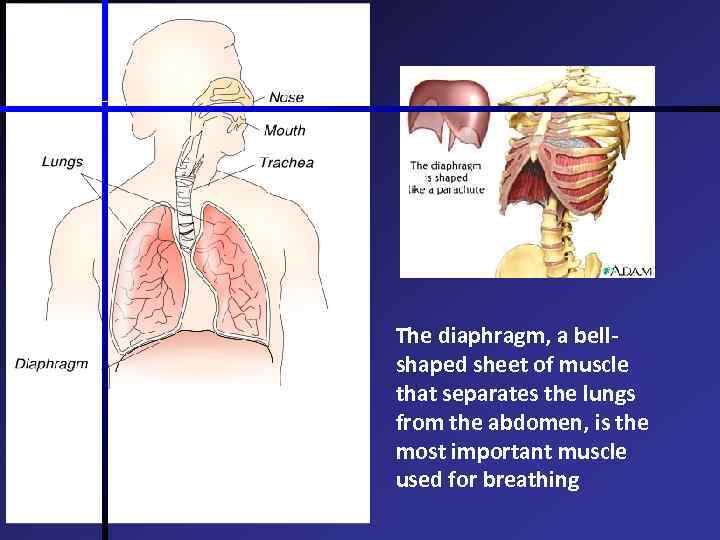 The diaphragm, a bellshaped sheet of muscle that separates the lungs from the abdomen, is the most important muscle used for breathing
The diaphragm, a bellshaped sheet of muscle that separates the lungs from the abdomen, is the most important muscle used for breathing
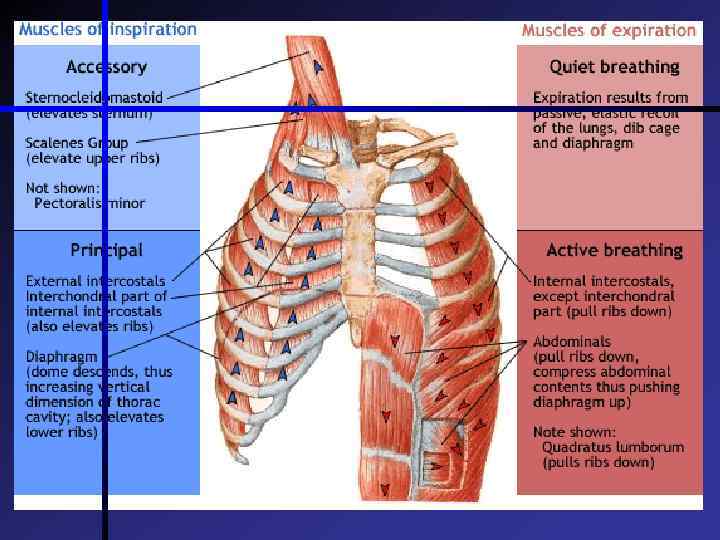
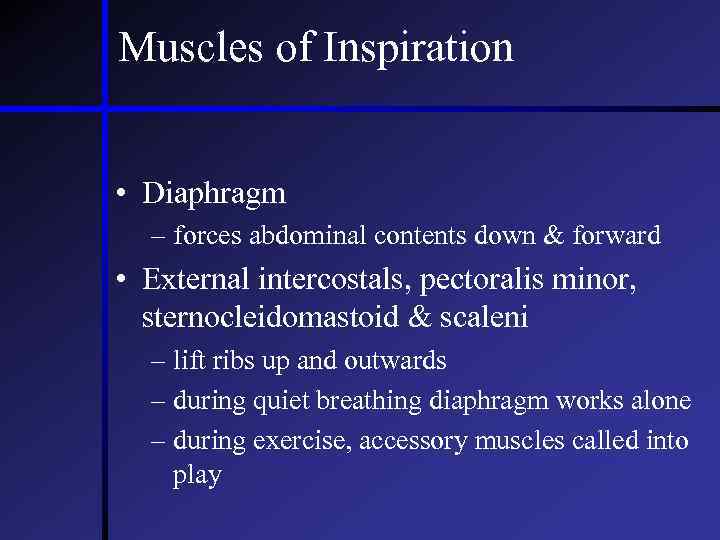 Muscles of Inspiration • Diaphragm – forces abdominal contents down & forward • External intercostals, pectoralis minor, sternocleidomastoid & scaleni – lift ribs up and outwards – during quiet breathing diaphragm works alone – during exercise, accessory muscles called into play
Muscles of Inspiration • Diaphragm – forces abdominal contents down & forward • External intercostals, pectoralis minor, sternocleidomastoid & scaleni – lift ribs up and outwards – during quiet breathing diaphragm works alone – during exercise, accessory muscles called into play
 INHALATION - also called INSPIRATION, - air is pulled into the LUNGS
INHALATION - also called INSPIRATION, - air is pulled into the LUNGS
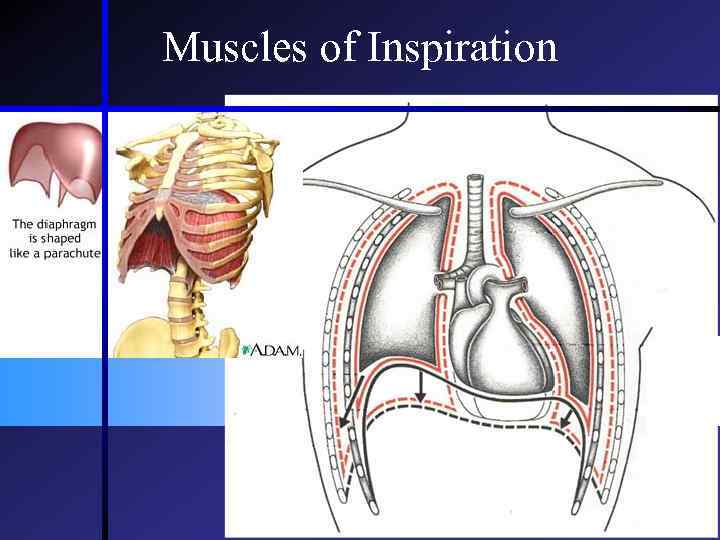 Muscles of Inspiration
Muscles of Inspiration
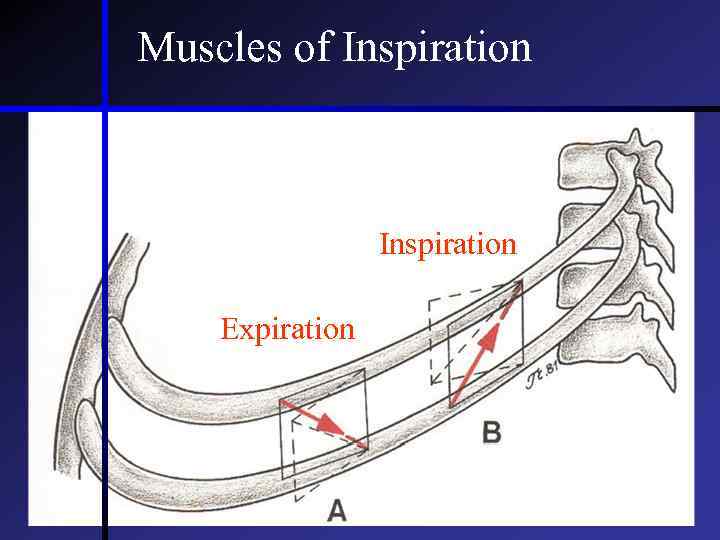 Muscles of Inspiration Expiration
Muscles of Inspiration Expiration
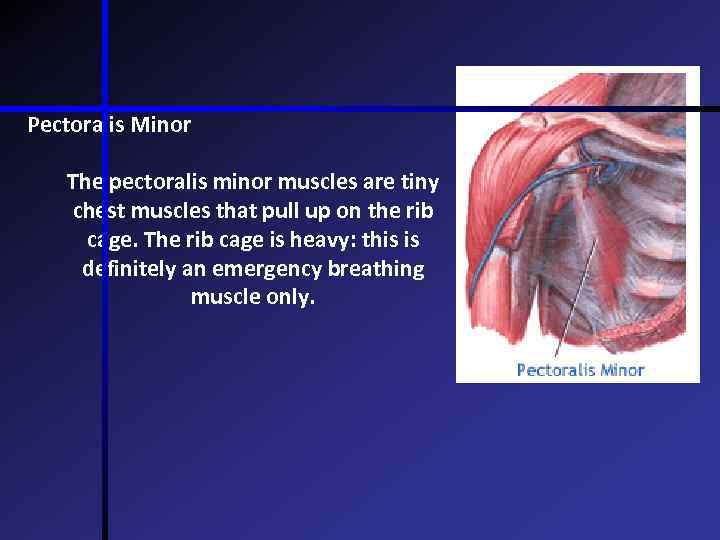 Pectoralis Minor The pectoralis minor muscles are tiny chest muscles that pull up on the rib cage. The rib cage is heavy: this is definitely an emergency breathing muscle only.
Pectoralis Minor The pectoralis minor muscles are tiny chest muscles that pull up on the rib cage. The rib cage is heavy: this is definitely an emergency breathing muscle only.
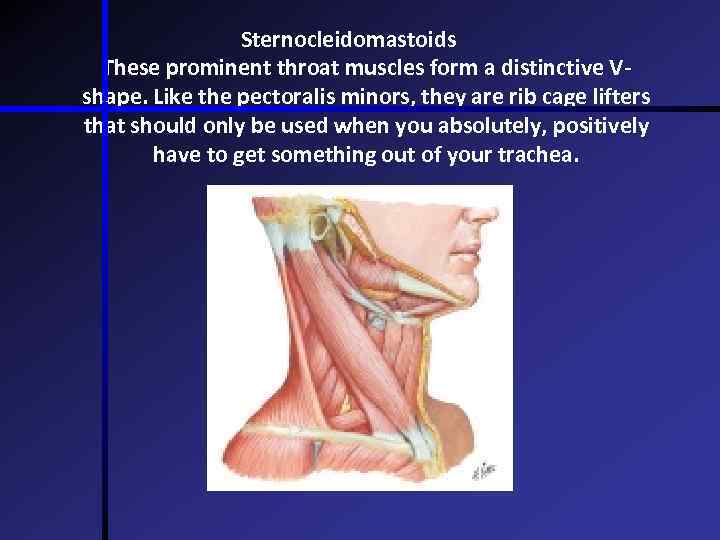 Sternocleidomastoids These prominent throat muscles form a distinctive Vshape. Like the pectoralis minors, they are rib cage lifters that should only be used when you absolutely, positively have to get something out of your trachea.
Sternocleidomastoids These prominent throat muscles form a distinctive Vshape. Like the pectoralis minors, they are rib cage lifters that should only be used when you absolutely, positively have to get something out of your trachea.
 EXHALATION - also called EXPIRATION - air is pushed out of the Lungs These Two actions deliver oxygen to the Alveoli, and remove Carbon dioxide
EXHALATION - also called EXPIRATION - air is pushed out of the Lungs These Two actions deliver oxygen to the Alveoli, and remove Carbon dioxide
 Expiration during quiet breathing is passive due to elastic recoil of chest cavity Decrease in lung size force air out of lungs During exercise and voluntary hyperventilation, – rectus abdominus, transverse abdominus: push diaphragm up – internal intercostals: pull ribs downwards Muscles of Expiration
Expiration during quiet breathing is passive due to elastic recoil of chest cavity Decrease in lung size force air out of lungs During exercise and voluntary hyperventilation, – rectus abdominus, transverse abdominus: push diaphragm up – internal intercostals: pull ribs downwards Muscles of Expiration
 At rest – the passive process!
At rest – the passive process!
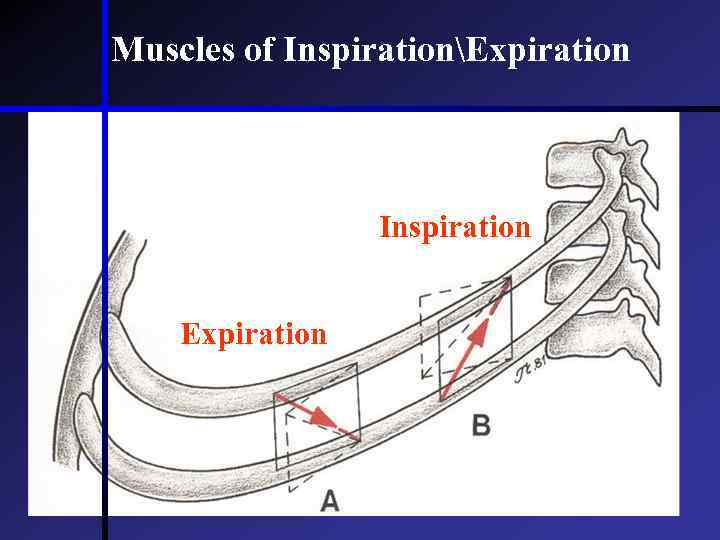 Muscles of InspirationExpiration Inspiration Expiration
Muscles of InspirationExpiration Inspiration Expiration
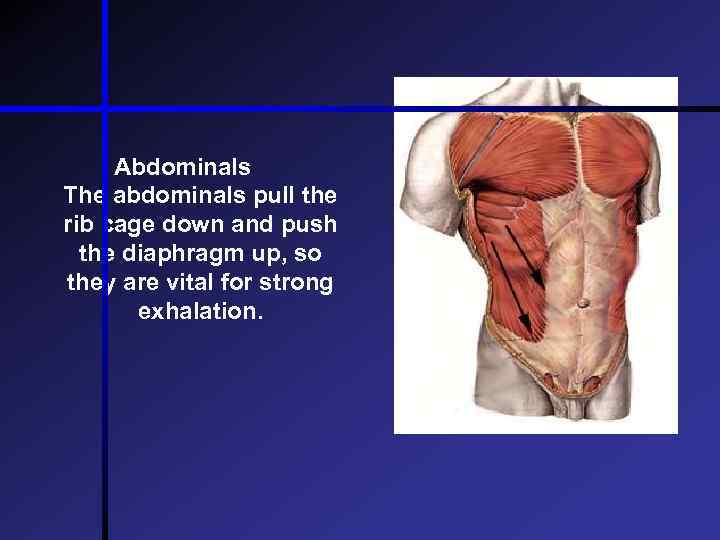 Abdominals The abdominals pull the rib cage down and push the diaphragm up, so they are vital for strong exhalation.
Abdominals The abdominals pull the rib cage down and push the diaphragm up, so they are vital for strong exhalation.
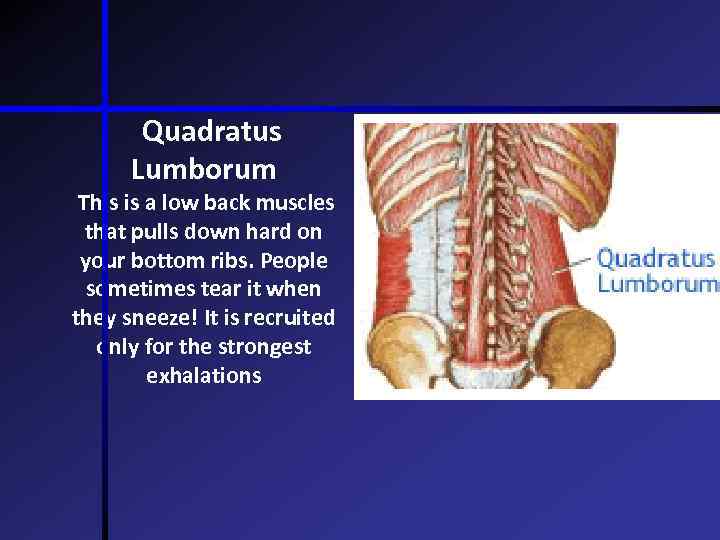 Quadratus Lumborum This is a low back muscles that pulls down hard on your bottom ribs. People sometimes tear it when they sneeze! It is recruited only for the strongest exhalations
Quadratus Lumborum This is a low back muscles that pulls down hard on your bottom ribs. People sometimes tear it when they sneeze! It is recruited only for the strongest exhalations
 Types of respiration Eupnea & Forced breathing (Deep breathing) Abdominal & Thoracic breathing Principles of pulmonary ventilation Contraction (Relaxation) of inspiratory muscles Expansion (Reduction) of thoracic cavity (? )Distension (Recoil) of alveoli Intrapulmonary pressure ( )<(>) atmospheric pressure Air flows into (out of) the alveoli
Types of respiration Eupnea & Forced breathing (Deep breathing) Abdominal & Thoracic breathing Principles of pulmonary ventilation Contraction (Relaxation) of inspiratory muscles Expansion (Reduction) of thoracic cavity (? )Distension (Recoil) of alveoli Intrapulmonary pressure ( )<(>) atmospheric pressure Air flows into (out of) the alveoli
 Intrapulmonary pressure Inspiratory phase: <1 sm H 2 O Expiratory phase: >1 sm H 2 O At the end of inspiration or expiration: =1 atm Intrapleural pressure Concept & Changes during respiratory cycle More negative as inspiratory processing Less negative as expiratory processing Measurement & Expression Direct & Indirect measurement 775 mm. Hg or 5 mm. Hg Always < 1 atm under static condition
Intrapulmonary pressure Inspiratory phase: <1 sm H 2 O Expiratory phase: >1 sm H 2 O At the end of inspiration or expiration: =1 atm Intrapleural pressure Concept & Changes during respiratory cycle More negative as inspiratory processing Less negative as expiratory processing Measurement & Expression Direct & Indirect measurement 775 mm. Hg or 5 mm. Hg Always < 1 atm under static condition
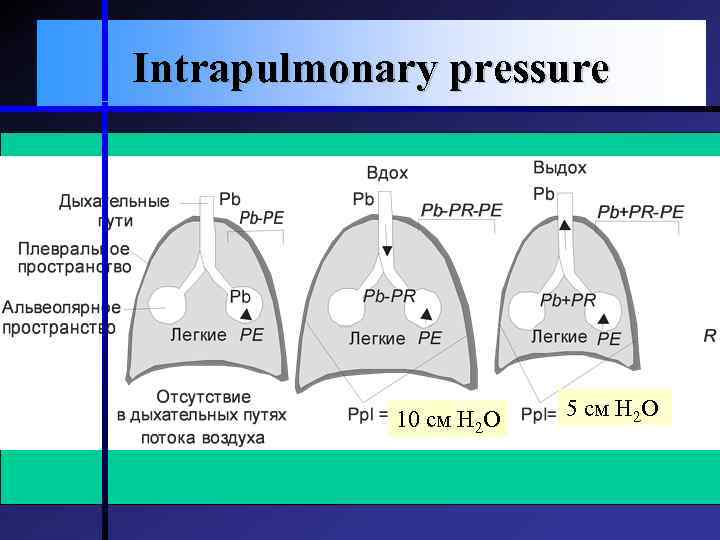 Intrapulmonary pressure 10 см Н 2 О 5 см Н 2 О
Intrapulmonary pressure 10 см Н 2 О 5 см Н 2 О
 Air Flow into Lungs • Differences in pressure pulls air into the lungs – pressure within the lungs becomes less than the atmospheric pressure – bulk flow (from high pressure to low pressure)
Air Flow into Lungs • Differences in pressure pulls air into the lungs – pressure within the lungs becomes less than the atmospheric pressure – bulk flow (from high pressure to low pressure)
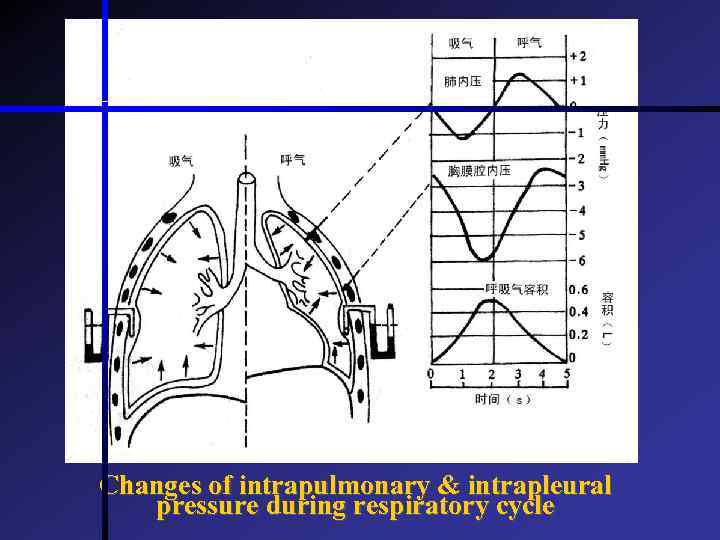 Changes of intrapulmonary & intrapleural pressure during respiratory cycle
Changes of intrapulmonary & intrapleural pressure during respiratory cycle
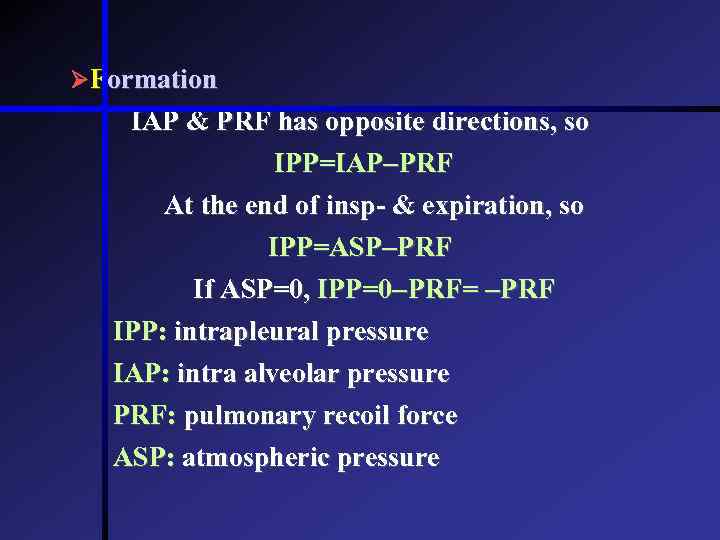 Formation IAP & PRF has opposite directions, so IPP=IAP PRF At the end of insp- & expiration, so IPP=ASP PRF If ASP=0, IPP=0 PRF= PRF IPP: intrapleural pressure IAP: intra alveolar pressure PRF: pulmonary recoil force ASP: atmospheric pressure
Formation IAP & PRF has opposite directions, so IPP=IAP PRF At the end of insp- & expiration, so IPP=ASP PRF If ASP=0, IPP=0 PRF= PRF IPP: intrapleural pressure IAP: intra alveolar pressure PRF: pulmonary recoil force ASP: atmospheric pressure
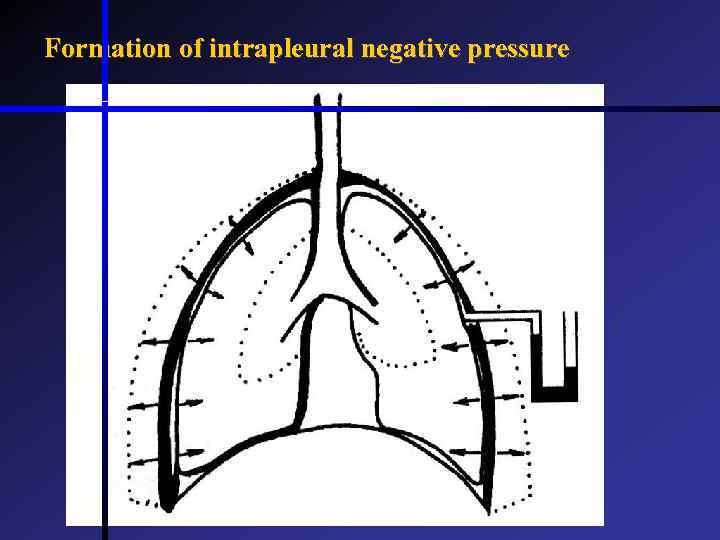 Formation of intrapleural negative pressure
Formation of intrapleural negative pressure
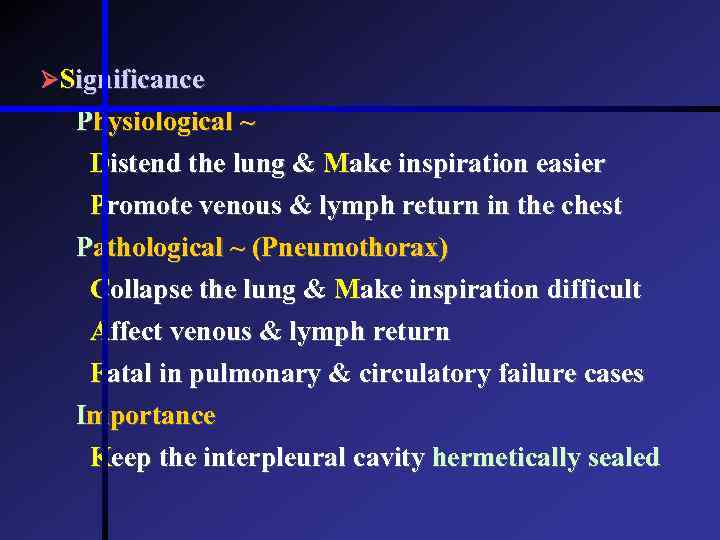 Significance Physiological ~ Distend the lung & Make inspiration easier Promote venous & lymph return in the chest Pathological ~ (Pneumothorax) Collapse the lung & Make inspiration difficult Affect venous & lymph return Fatal in pulmonary & circulatory failure cases Importance Keep the interpleural cavity hermetically sealed
Significance Physiological ~ Distend the lung & Make inspiration easier Promote venous & lymph return in the chest Pathological ~ (Pneumothorax) Collapse the lung & Make inspiration difficult Affect venous & lymph return Fatal in pulmonary & circulatory failure cases Importance Keep the interpleural cavity hermetically sealed
 * Resistance to breathing Elastic ~ of the lung Elastic ~ & Compliance CL=1/RL= VL/ PL(L/cm. H 2 O) Static compliance (Cst) of the lung S shaped curve, divided into 3 portions Flattened upper portion Steep middle portion Flattened lower portion Special compliance (Csp) Csp = CL/TLC
* Resistance to breathing Elastic ~ of the lung Elastic ~ & Compliance CL=1/RL= VL/ PL(L/cm. H 2 O) Static compliance (Cst) of the lung S shaped curve, divided into 3 portions Flattened upper portion Steep middle portion Flattened lower portion Special compliance (Csp) Csp = CL/TLC
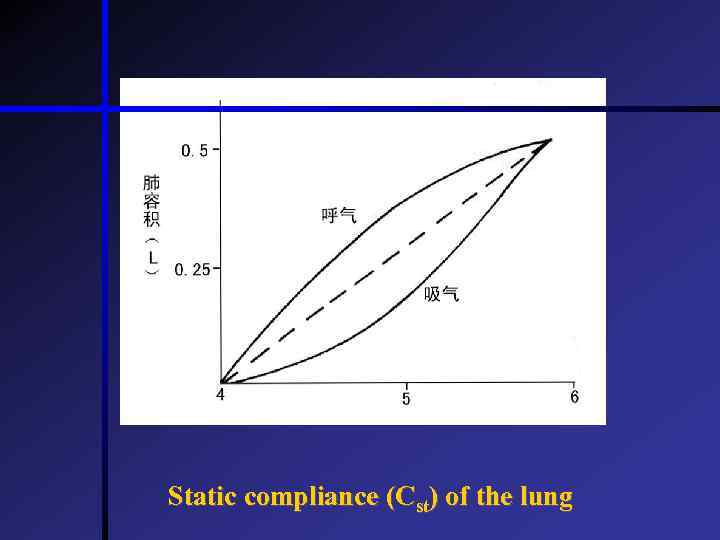 Static compliance (Cst) of the lung
Static compliance (Cst) of the lung
 S shaped compliance curve of the lung
S shaped compliance curve of the lung
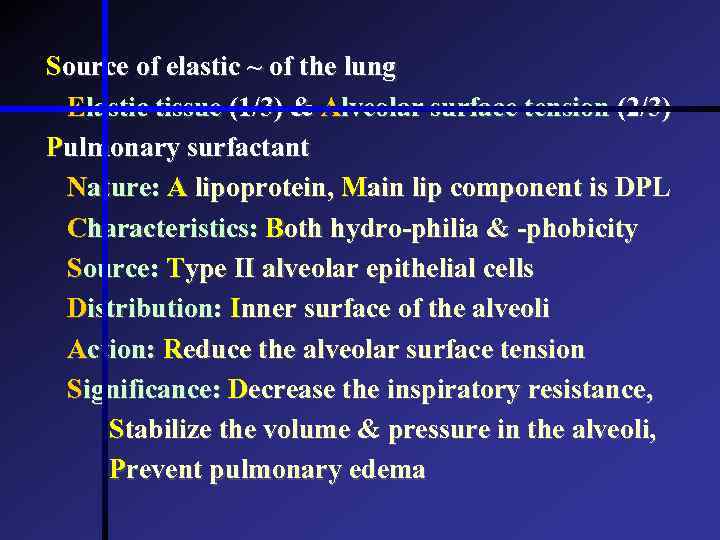 Source of elastic ~ of the lung Elastic tissue (1/3) & Alveolar surface tension (2/3) Pulmonary surfactant Nature: A lipoprotein, Main lip component is DPL Characteristics: Both hydro-philia & -phobicity Source: Type II alveolar epithelial cells Distribution: Inner surface of the alveoli Action: Reduce the alveolar surface tension Significance: Decrease the inspiratory resistance, Stabilize the volume & pressure in the alveoli, Prevent pulmonary edema
Source of elastic ~ of the lung Elastic tissue (1/3) & Alveolar surface tension (2/3) Pulmonary surfactant Nature: A lipoprotein, Main lip component is DPL Characteristics: Both hydro-philia & -phobicity Source: Type II alveolar epithelial cells Distribution: Inner surface of the alveoli Action: Reduce the alveolar surface tension Significance: Decrease the inspiratory resistance, Stabilize the volume & pressure in the alveoli, Prevent pulmonary edema
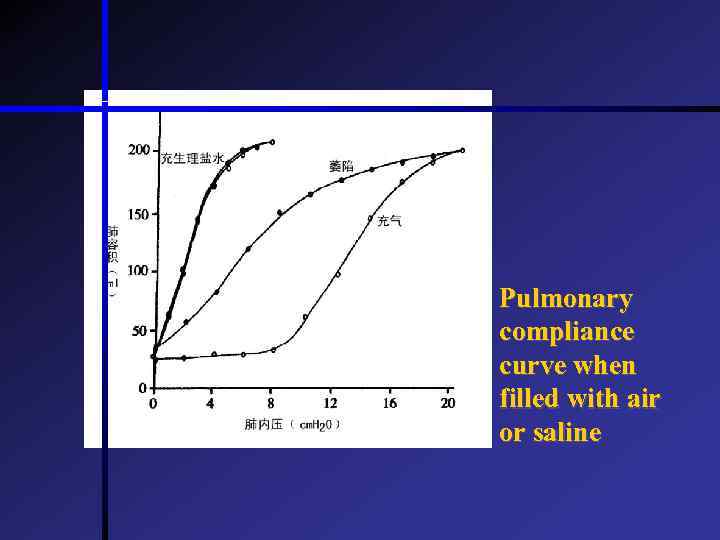 Pulmonary compliance curve when filled with air or saline
Pulmonary compliance curve when filled with air or saline
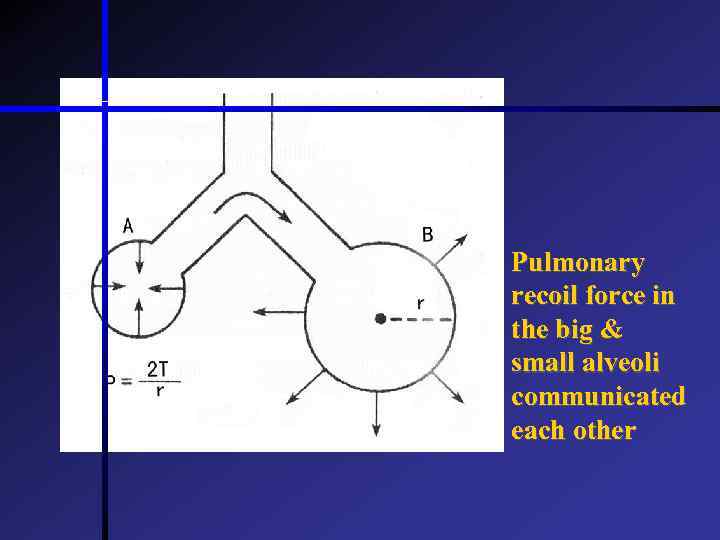 Pulmonary recoil force in the big & small alveoli communicated each other
Pulmonary recoil force in the big & small alveoli communicated each other
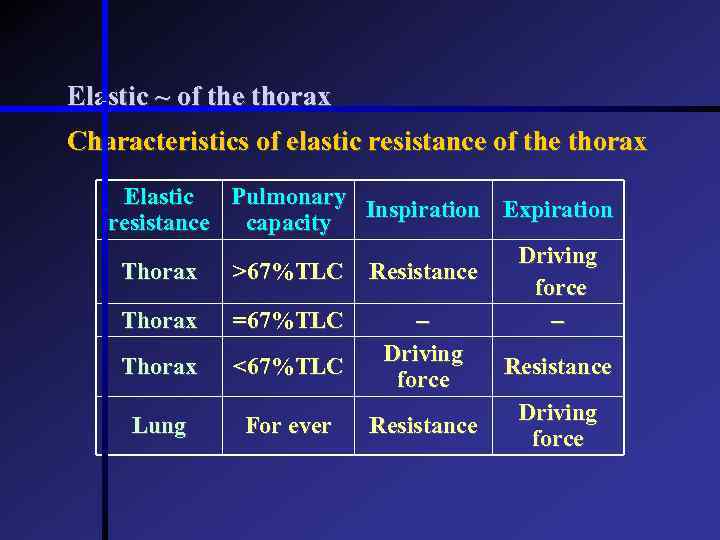 Elastic ~ of the thorax Characteristics of elastic resistance of the thorax Elastic Pulmonary Inspiration Expiration resistance capacity Driving Thorax >67%TLC Resistance force Thorax =67%TLC Driving Thorax <67%TLC Resistance force Driving Lung For ever Resistance force
Elastic ~ of the thorax Characteristics of elastic resistance of the thorax Elastic Pulmonary Inspiration Expiration resistance capacity Driving Thorax >67%TLC Resistance force Thorax =67%TLC Driving Thorax <67%TLC Resistance force Driving Lung For ever Resistance force
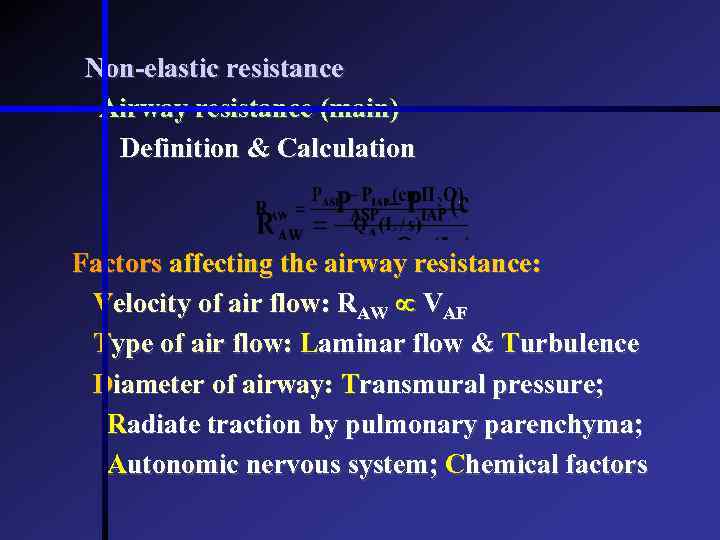 Non-elastic resistance Airway resistance (main) Definition & Calculation Factors affecting the airway resistance: Velocity of air flow: RAW VAF Type of air flow: Laminar flow & Turbulence Diameter of airway: Transmural pressure; Radiate traction by pulmonary parenchyma; Autonomic nervous system; Chemical factors
Non-elastic resistance Airway resistance (main) Definition & Calculation Factors affecting the airway resistance: Velocity of air flow: RAW VAF Type of air flow: Laminar flow & Turbulence Diameter of airway: Transmural pressure; Radiate traction by pulmonary parenchyma; Autonomic nervous system; Chemical factors
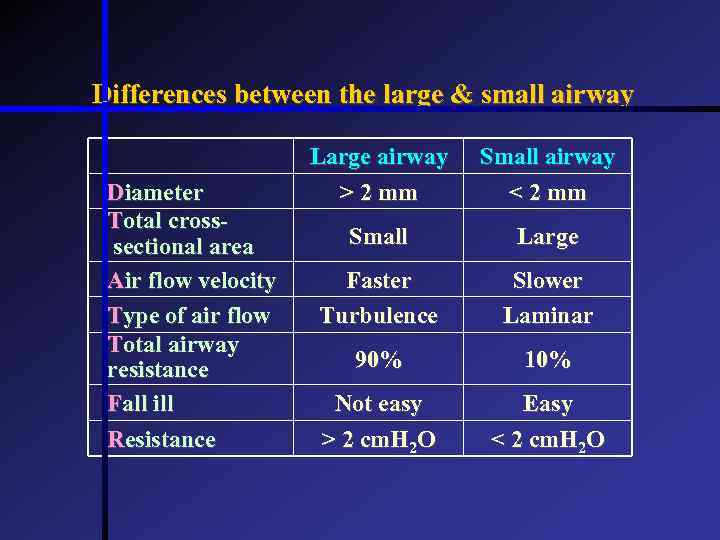 Differences between the large & small airway Diameter Total crosssectional area Air flow velocity Type of air flow Total airway resistance Fall ill Resistance Large airway > 2 mm Small airway < 2 mm Small Large Faster Turbulence Slower Laminar 90% 10% Not easy > 2 cm. H 2 O Easy < 2 cm. H 2 O
Differences between the large & small airway Diameter Total crosssectional area Air flow velocity Type of air flow Total airway resistance Fall ill Resistance Large airway > 2 mm Small airway < 2 mm Small Large Faster Turbulence Slower Laminar 90% 10% Not easy > 2 cm. H 2 O Easy < 2 cm. H 2 O
 Pulmonary volume & capacity
Pulmonary volume & capacity
 Pulmonary volume & capacity * Tidal volume (TV) * Inspiratory reserve volume (IRV) * TExpiratory reserve volume (ERV) * Residual volume (RV) * Inspiratory capacity (IC) * Functional residual capacity (FRC) * Vital capacity (VC) * Forced vital capacity (FVC) & Forced expiratory capacity (FEC) * Total lung capacity (TLC)
Pulmonary volume & capacity * Tidal volume (TV) * Inspiratory reserve volume (IRV) * TExpiratory reserve volume (ERV) * Residual volume (RV) * Inspiratory capacity (IC) * Functional residual capacity (FRC) * Vital capacity (VC) * Forced vital capacity (FVC) & Forced expiratory capacity (FEC) * Total lung capacity (TLC)
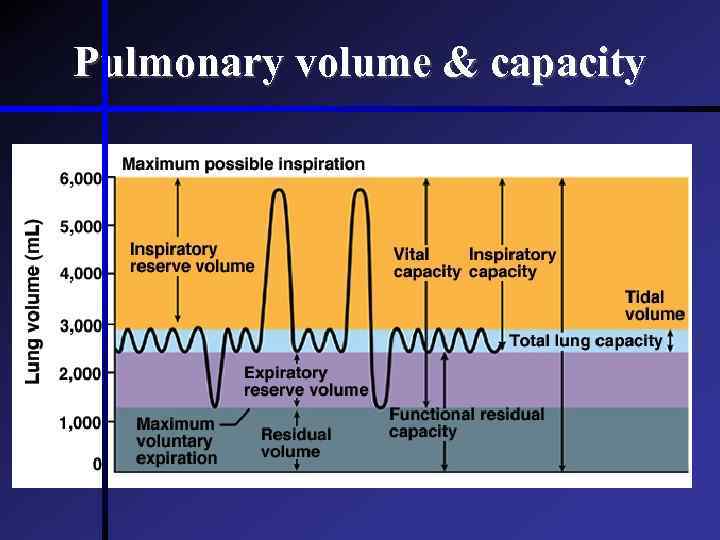 Pulmonary volume & capacity
Pulmonary volume & capacity
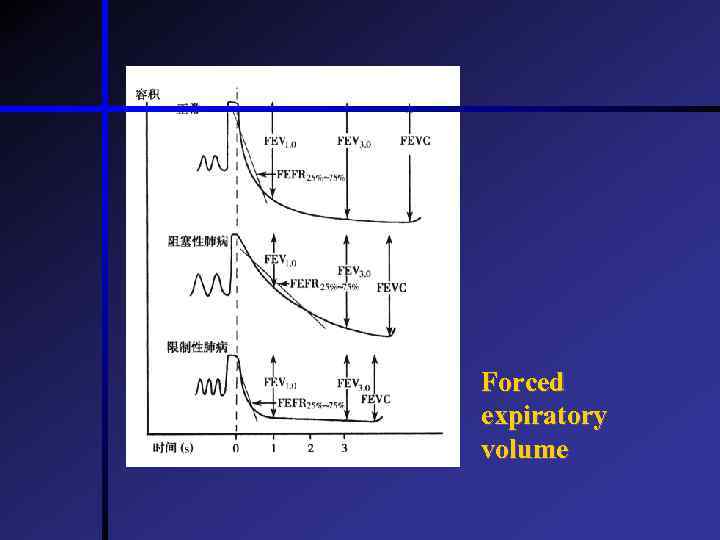 Forced expiratory volume
Forced expiratory volume
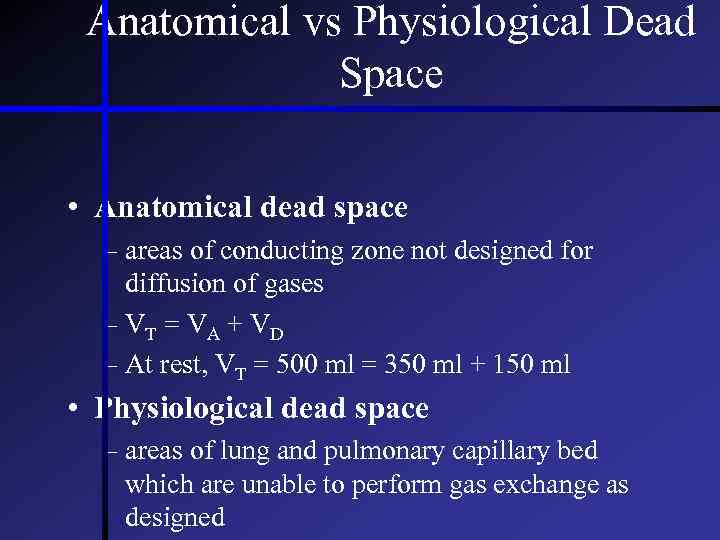 Anatomical vs Physiological Dead Space • Anatomical dead space – areas of conducting zone not designed for diffusion of gases – VT = V A + V D – At rest, VT = 500 ml = 350 ml + 150 ml • Physiological dead space – areas of lung and pulmonary capillary bed which are unable to perform gas exchange as designed
Anatomical vs Physiological Dead Space • Anatomical dead space – areas of conducting zone not designed for diffusion of gases – VT = V A + V D – At rest, VT = 500 ml = 350 ml + 150 ml • Physiological dead space – areas of lung and pulmonary capillary bed which are unable to perform gas exchange as designed
 Physiologic Dead Space • Optimal diffusion requires matching of ventilation to perfusion: 1 ventilated alveoli/ 1 blood perfused alveoli • Ventilation / perfusion is not equal across the lung • Top of lung is poorly perfused – V / Q = 3. 3 at top of lung • Bottom of lung has more perfusion than ventilation – V / Q =. 63 at bottom of lung • V / Q values above. 5 are generally adequate
Physiologic Dead Space • Optimal diffusion requires matching of ventilation to perfusion: 1 ventilated alveoli/ 1 blood perfused alveoli • Ventilation / perfusion is not equal across the lung • Top of lung is poorly perfused – V / Q = 3. 3 at top of lung • Bottom of lung has more perfusion than ventilation – V / Q =. 63 at bottom of lung • V / Q values above. 5 are generally adequate
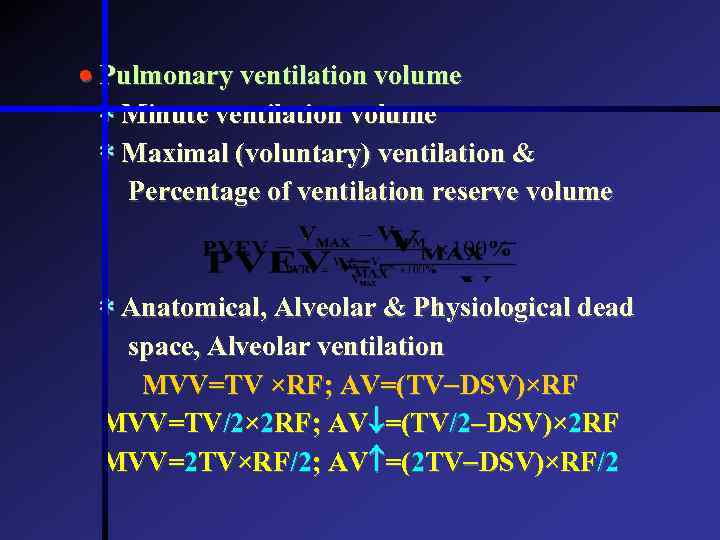 Pulmonary ventilation volume * Minute ventilation volume * Maximal (voluntary) ventilation & Percentage of ventilation reserve volume * Anatomical, Alveolar & Physiological dead space, Alveolar ventilation MVV=TV ×RF; AV=(TV DSV)×RF MVV=TV/2× 2 RF; AV =(TV/2 DSV)× 2 RF MVV=2 TV×RF/2; AV =(2 TV DSV)×RF/2
Pulmonary ventilation volume * Minute ventilation volume * Maximal (voluntary) ventilation & Percentage of ventilation reserve volume * Anatomical, Alveolar & Physiological dead space, Alveolar ventilation MVV=TV ×RF; AV=(TV DSV)×RF MVV=TV/2× 2 RF; AV =(TV/2 DSV)× 2 RF MVV=2 TV×RF/2; AV =(2 TV DSV)×RF/2
 Processes of gas exchange
Processes of gas exchange
 Factors affecting gas exchange * Diffusion rate of gas * Ventilation/perfusion ratio (V/Q) Definition & its normal value (0. 84) If V /Q > 0. 84: Alveolar dead space V /Q < 0. 84: Functional A-V shunt Anoxia occurs more easily than CO 2 retention Affecting by gravity when a person stands
Factors affecting gas exchange * Diffusion rate of gas * Ventilation/perfusion ratio (V/Q) Definition & its normal value (0. 84) If V /Q > 0. 84: Alveolar dead space V /Q < 0. 84: Functional A-V shunt Anoxia occurs more easily than CO 2 retention Affecting by gravity when a person stands
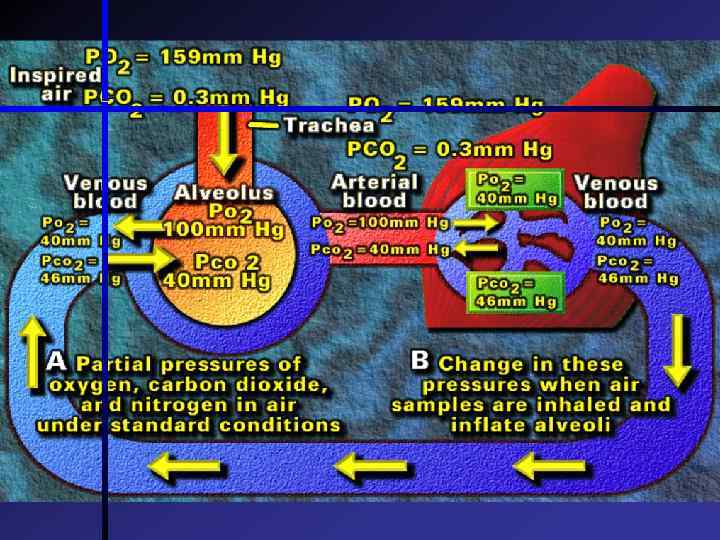
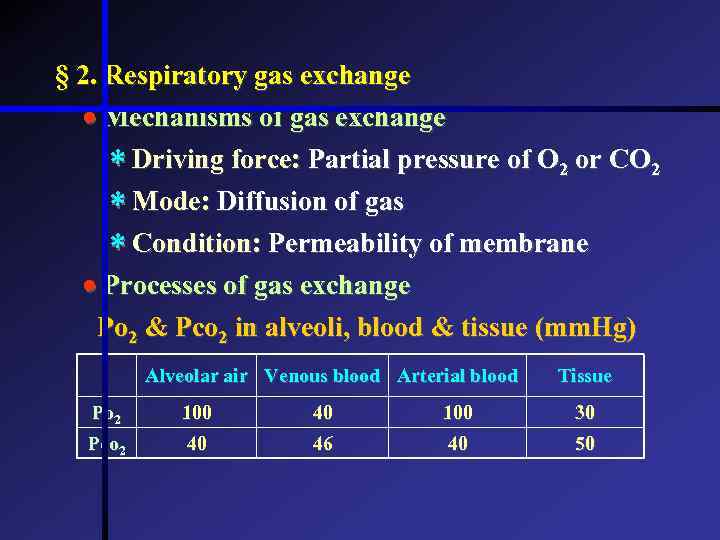 § 2. Respiratory gas exchange Mechanisms of gas exchange * Driving force: Partial pressure of O 2 or CO 2 * Mode: Diffusion of gas * Condition: Permeability of membrane Processes of gas exchange Po 2 & Pco 2 in alveoli, blood & tissue (mm. Hg) Alveolar air Venous blood Arterial blood Tissue Po 2 100 40 100 30 Pco 2 40 46 40 50
§ 2. Respiratory gas exchange Mechanisms of gas exchange * Driving force: Partial pressure of O 2 or CO 2 * Mode: Diffusion of gas * Condition: Permeability of membrane Processes of gas exchange Po 2 & Pco 2 in alveoli, blood & tissue (mm. Hg) Alveolar air Venous blood Arterial blood Tissue Po 2 100 40 100 30 Pco 2 40 46 40 50
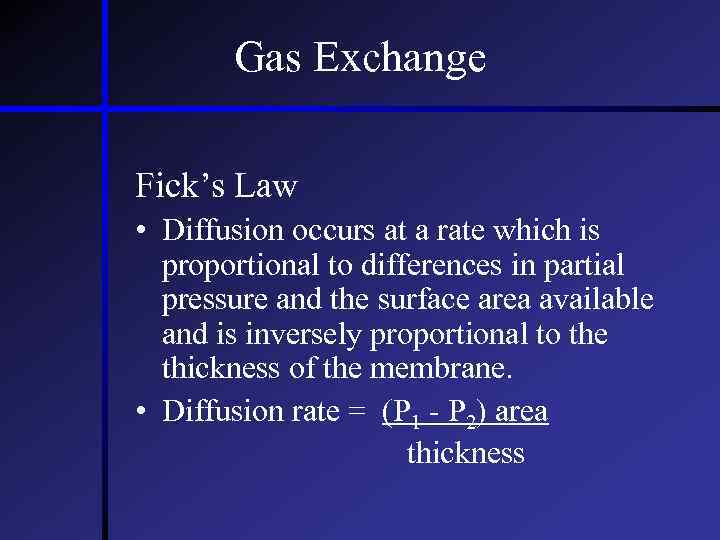 Gas Exchange Fick’s Law • Diffusion occurs at a rate which is proportional to differences in partial pressure and the surface area available and is inversely proportional to the thickness of the membrane. • Diffusion rate = (P 1 - P 2) area thickness
Gas Exchange Fick’s Law • Diffusion occurs at a rate which is proportional to differences in partial pressure and the surface area available and is inversely proportional to the thickness of the membrane. • Diffusion rate = (P 1 - P 2) area thickness
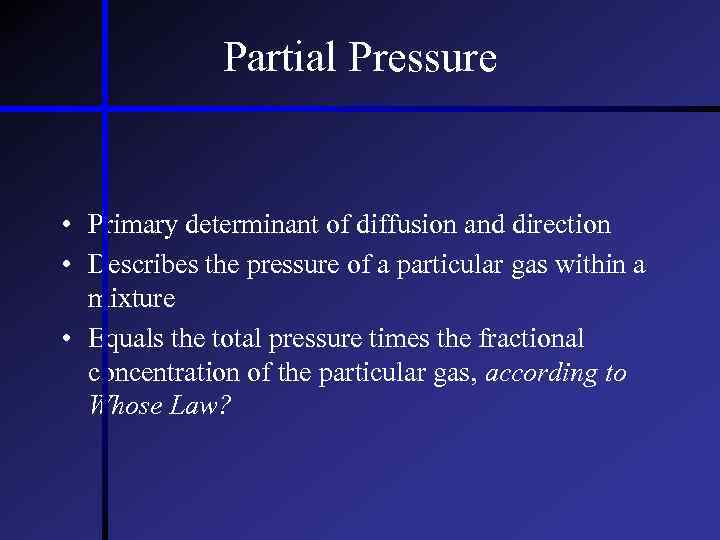 Partial Pressure • Primary determinant of diffusion and direction • Describes the pressure of a particular gas within a mixture • Equals the total pressure times the fractional concentration of the particular gas, according to Whose Law?
Partial Pressure • Primary determinant of diffusion and direction • Describes the pressure of a particular gas within a mixture • Equals the total pressure times the fractional concentration of the particular gas, according to Whose Law?
 Other Diffusion Factors • Length of diffusion pathway – alveolar membrane, interstitial fluid, capillary membrane, plasma, RBC • Surface area available for diffusion – capillary density, number of functioning alveoli
Other Diffusion Factors • Length of diffusion pathway – alveolar membrane, interstitial fluid, capillary membrane, plasma, RBC • Surface area available for diffusion – capillary density, number of functioning alveoli
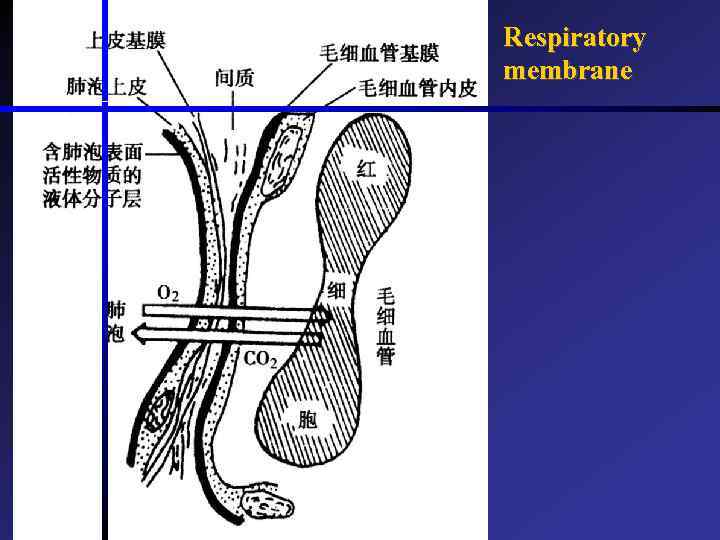 Respiratory membrane
Respiratory membrane
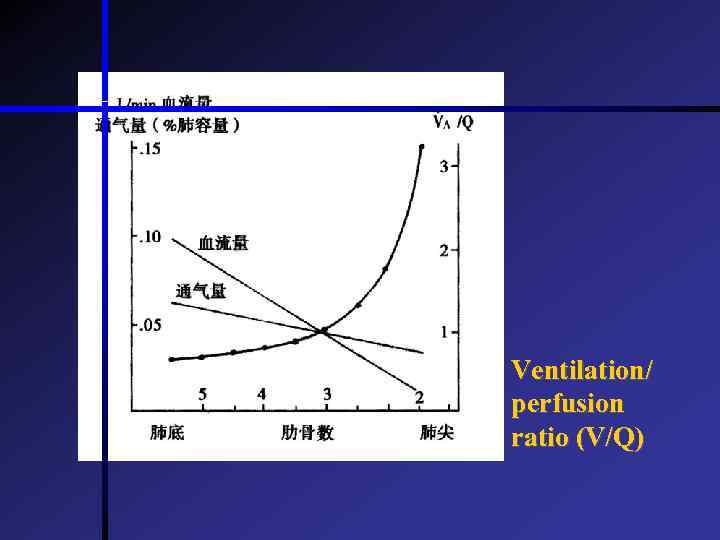 Ventilation/ perfusion ratio (V/Q)
Ventilation/ perfusion ratio (V/Q)
 Oxygen Transport in the Blood • Dissolved in plasma – amount is proportional to partial pressure – O 2 is poorly soluble in plasma • average. 3 ml O 2 / 100 ml blood • Combined with hemoglobin – each hemoglobin molecule combines with 4 O 2 – average 20 ml O 2 / 100 ml blood
Oxygen Transport in the Blood • Dissolved in plasma – amount is proportional to partial pressure – O 2 is poorly soluble in plasma • average. 3 ml O 2 / 100 ml blood • Combined with hemoglobin – each hemoglobin molecule combines with 4 O 2 – average 20 ml O 2 / 100 ml blood
 Oxygen Capacity of Hemoglobin • • • Percent saturation (%SO 2) is Men average grams of proportion of hemoglobin bound hemoglobin = 15/100 ml with oxygen. Women average grams of • Even with sufficient atmospheric hemoglobin = 14/100 ml oxygen, adequate pulmonary Amount of O 2 per gram of ventilation, & optimum hemoglobin = 1. 34 ml diffusing capacity, Hb not Maximal amount of O 2 that become 100% saturated. combine 100 ml blood = • SO 2 arterial blood at rest = 98% – 20. 1 ml O 2 for men • Hemoglobin carries 19. 7 ml O 2 – 18. 8 ml O 2 for women (. 98 x 20. 1) and. 3 ml dissolved if 100% saturated. in 100 ml blood at 100 mm Hg as in the lungs.
Oxygen Capacity of Hemoglobin • • • Percent saturation (%SO 2) is Men average grams of proportion of hemoglobin bound hemoglobin = 15/100 ml with oxygen. Women average grams of • Even with sufficient atmospheric hemoglobin = 14/100 ml oxygen, adequate pulmonary Amount of O 2 per gram of ventilation, & optimum hemoglobin = 1. 34 ml diffusing capacity, Hb not Maximal amount of O 2 that become 100% saturated. combine 100 ml blood = • SO 2 arterial blood at rest = 98% – 20. 1 ml O 2 for men • Hemoglobin carries 19. 7 ml O 2 – 18. 8 ml O 2 for women (. 98 x 20. 1) and. 3 ml dissolved if 100% saturated. in 100 ml blood at 100 mm Hg as in the lungs.
 Oxygen Capacity of Hemoglobin • Tissue PO 2 in cell fluids at rest averages 40 mm Hg. • Dissolved oxygen in arterial blood readily diffuses into cells. • This causes Hb to release its oxygen. • At 40 mm Hg, Hb holds about 75% of total capacity for oxygen (15 m. L O 2). • Arteriovenous-oxygen difference at rest = 5 m. L O 2
Oxygen Capacity of Hemoglobin • Tissue PO 2 in cell fluids at rest averages 40 mm Hg. • Dissolved oxygen in arterial blood readily diffuses into cells. • This causes Hb to release its oxygen. • At 40 mm Hg, Hb holds about 75% of total capacity for oxygen (15 m. L O 2). • Arteriovenous-oxygen difference at rest = 5 m. L O 2
 Hb Saturation Differences in Arteries and Veins Arteriovenous O 2 difference • Reveals the amount of oxygen extracted by the tissues • Rest: 20 – 15 = 5 ml O 2 per 100 ml blood • Exercise: 20 – 5 or 4 = 15 - 16 ml O 2 per 100 ml blood
Hb Saturation Differences in Arteries and Veins Arteriovenous O 2 difference • Reveals the amount of oxygen extracted by the tissues • Rest: 20 – 15 = 5 ml O 2 per 100 ml blood • Exercise: 20 – 5 or 4 = 15 - 16 ml O 2 per 100 ml blood
 Oxygen Capacity of Hemoglobin • During exercise, tissue PO 2 decreases to about 20 mm Hg. • Hemoglobin retains about 25% or 5 m. L O 2 (. 25 x 20. 1). • A-v O 2 difference = 20. 1 – 5 = 15 m. L/100. • During exhaustive exercise, tissue PO 2 about 3 mm Hg, Hb releases all.
Oxygen Capacity of Hemoglobin • During exercise, tissue PO 2 decreases to about 20 mm Hg. • Hemoglobin retains about 25% or 5 m. L O 2 (. 25 x 20. 1). • A-v O 2 difference = 20. 1 – 5 = 15 m. L/100. • During exhaustive exercise, tissue PO 2 about 3 mm Hg, Hb releases all.
 Blood Conditions Influencing O 2 Saturation of Hemoglobin • • • PO 2 Temperature p. H PCO 2 2, 3 -DPG (also called 2, 3 -BPG)
Blood Conditions Influencing O 2 Saturation of Hemoglobin • • • PO 2 Temperature p. H PCO 2 2, 3 -DPG (also called 2, 3 -BPG)
 Resting Conditions • • p. H = 7. 4 Temperature = 37 degrees Celsius Arterial PO 2 = 100 mm Hg Mixed venous PO 2 = 40 mm Hg
Resting Conditions • • p. H = 7. 4 Temperature = 37 degrees Celsius Arterial PO 2 = 100 mm Hg Mixed venous PO 2 = 40 mm Hg
 Changes with Exercise • • • p. H drops Temperature rises PO 2 at the tissues decreases PCO 2 rises No change in 2, 3 -DPG
Changes with Exercise • • • p. H drops Temperature rises PO 2 at the tissues decreases PCO 2 rises No change in 2, 3 -DPG
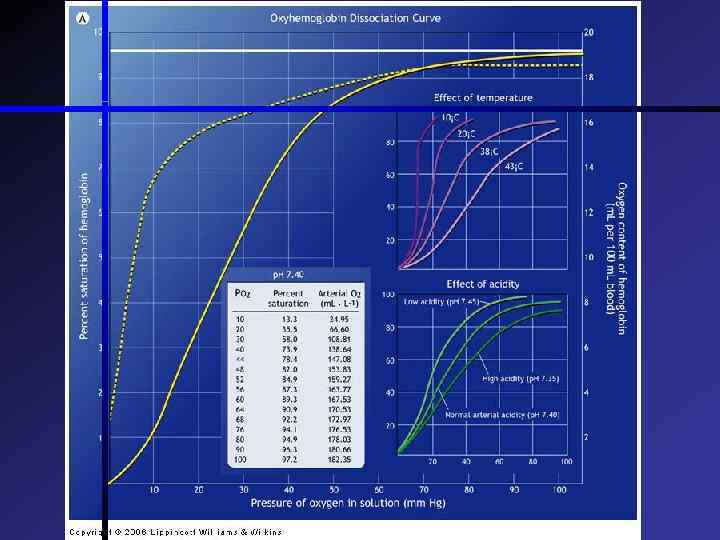
 Bohr Shift • Shift to the right in the oxyhemoglobin dissociation curve • Loading of O 2 is not affected – the flat upper portion is not altered • Unloading of O 2 is enhanced – along steep lower portion, more O 2 is unloaded at a given PO 2 with the shift
Bohr Shift • Shift to the right in the oxyhemoglobin dissociation curve • Loading of O 2 is not affected – the flat upper portion is not altered • Unloading of O 2 is enhanced – along steep lower portion, more O 2 is unloaded at a given PO 2 with the shift
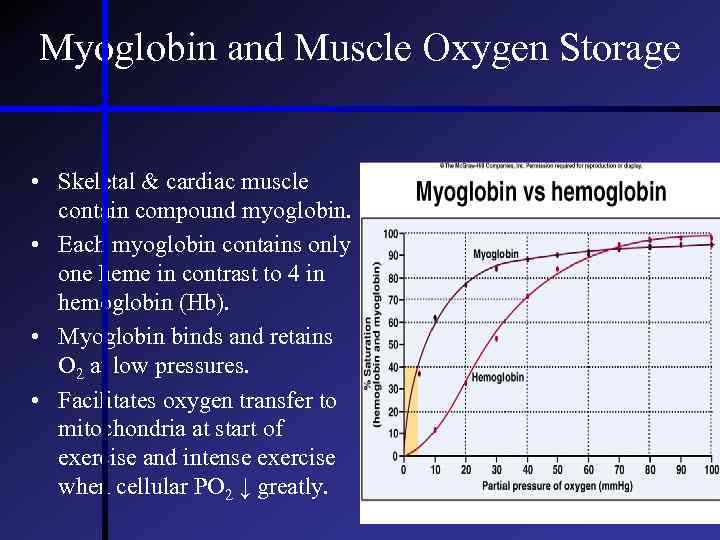 Myoglobin and Muscle Oxygen Storage • Skeletal & cardiac muscle contain compound myoglobin. • Each myoglobin contains only one heme in contrast to 4 in hemoglobin (Hb). • Myoglobin binds and retains O 2 at low pressures. • Facilitates oxygen transfer to mitochondria at start of exercise and intense exercise when cellular PO 2 ↓ greatly.
Myoglobin and Muscle Oxygen Storage • Skeletal & cardiac muscle contain compound myoglobin. • Each myoglobin contains only one heme in contrast to 4 in hemoglobin (Hb). • Myoglobin binds and retains O 2 at low pressures. • Facilitates oxygen transfer to mitochondria at start of exercise and intense exercise when cellular PO 2 ↓ greatly.
 § 3. Gas transport in the blood Oxygen transport * Forms of transport Physically diffusion & Combination with Hb * Characteristics of Hb combined with O 2 Fast, reversible, need not enzyme, oxygenate with Fe 2+, O 2 combined with Hb is 4: 1, S shaped oxygen dissociation curve * Oxygen capacity, content & saturation * Cyanosis & carbon monoxide poisoning
§ 3. Gas transport in the blood Oxygen transport * Forms of transport Physically diffusion & Combination with Hb * Characteristics of Hb combined with O 2 Fast, reversible, need not enzyme, oxygenate with Fe 2+, O 2 combined with Hb is 4: 1, S shaped oxygen dissociation curve * Oxygen capacity, content & saturation * Cyanosis & carbon monoxide poisoning
 * Oxygen dissociation curve Definition & why it is in S shaped Physiological advantages of S shaped curve The flattened upper portion (60~100 mm. Hg) The steep middle portion (40~60 mm. Hg) The steep lower portion (15~40 mm. Hg) Factors affecting oxygen dissociation curve Concept of P 50, affinity to O 2, right or left shift Factors: p. H & Pco 2 (Bohr effect), temperature, 2, 3 -DPG, others (Fe 2+ Fe 3+, CO)
* Oxygen dissociation curve Definition & why it is in S shaped Physiological advantages of S shaped curve The flattened upper portion (60~100 mm. Hg) The steep middle portion (40~60 mm. Hg) The steep lower portion (15~40 mm. Hg) Factors affecting oxygen dissociation curve Concept of P 50, affinity to O 2, right or left shift Factors: p. H & Pco 2 (Bohr effect), temperature, 2, 3 -DPG, others (Fe 2+ Fe 3+, CO)
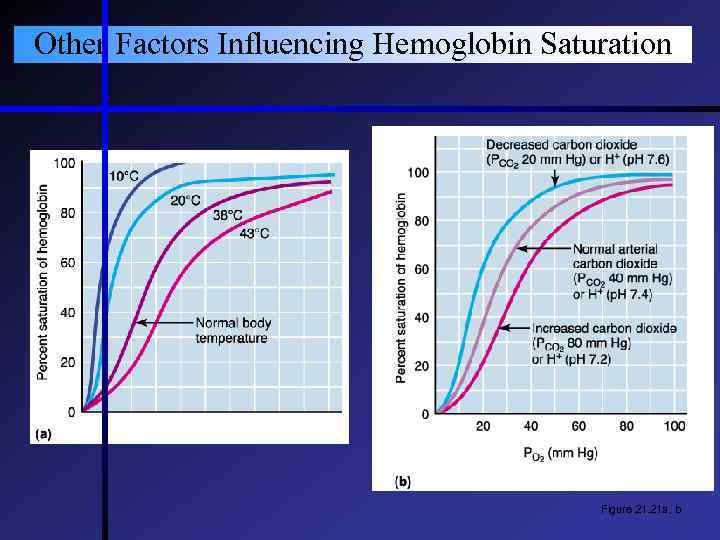 Other Factors Influencing Hemoglobin Saturation Figure 21. 21 a, b
Other Factors Influencing Hemoglobin Saturation Figure 21. 21 a, b
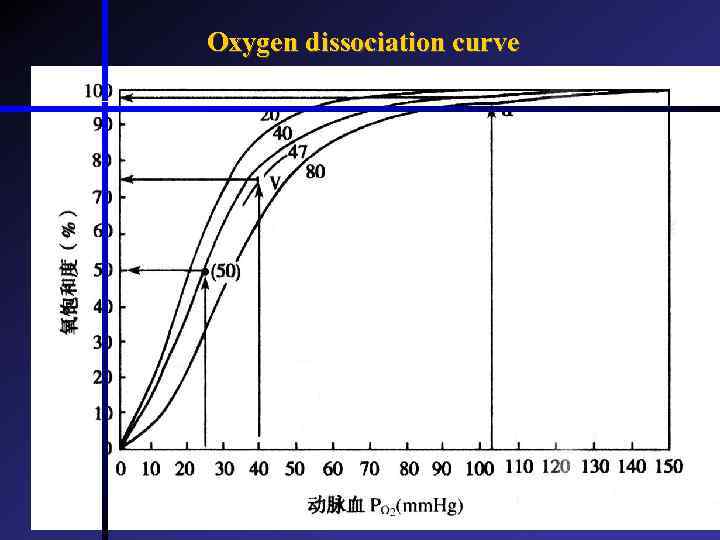 Oxygen dissociation curve
Oxygen dissociation curve
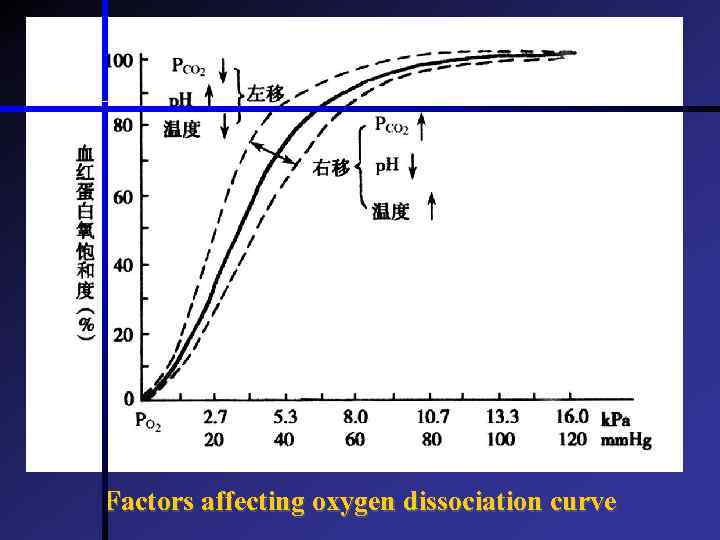 Factors affecting oxygen dissociation curve
Factors affecting oxygen dissociation curve
 Carbon Dioxide Transport • Carbon dioxide is transported in the blood in three forms – Dissolved in plasma – 7 to 10% – Chemically bound to hemoglobin – 20% is carried in red blood cells as carbaminohemoglobin – Bicarbonate ion in plasma – 70% is transported as Carbon Dioxide Transport bicarbonate (HCO 3–)
Carbon Dioxide Transport • Carbon dioxide is transported in the blood in three forms – Dissolved in plasma – 7 to 10% – Chemically bound to hemoglobin – 20% is carried in red blood cells as carbaminohemoglobin – Bicarbonate ion in plasma – 70% is transported as Carbon Dioxide Transport bicarbonate (HCO 3–)
 Carbon Dioxide Transport in the Blood
Carbon Dioxide Transport in the Blood
 Transport and Exchange of Carbon Dioxide Figure 21. 22 a
Transport and Exchange of Carbon Dioxide Figure 21. 22 a
 Transport and Exchange of Carbon Dioxide • At the tissues – Bicarbonate quickly diffuses from red blood cells into the plasma – Chloride shift – to counterbalance the outrush of negative bicarbonate ions from the red blood cells, chloride ions (Cl–) move from the plasma into the erythrocytes
Transport and Exchange of Carbon Dioxide • At the tissues – Bicarbonate quickly diffuses from red blood cells into the plasma – Chloride shift – to counterbalance the outrush of negative bicarbonate ions from the red blood cells, chloride ions (Cl–) move from the plasma into the erythrocytes
 Transport and Exchange of Carbon Dioxide • At the lungs, these processes are reversed – Bicarbonate ions move into the red blood cells and bind with hydrogen ions to form carbonic acid – Carbonic acid is then split by carbonic anhydrase to release carbon dioxide and water – Carbon dioxide then diffuses from the blood into the alveoli
Transport and Exchange of Carbon Dioxide • At the lungs, these processes are reversed – Bicarbonate ions move into the red blood cells and bind with hydrogen ions to form carbonic acid – Carbonic acid is then split by carbonic anhydrase to release carbon dioxide and water – Carbon dioxide then diffuses from the blood into the alveoli
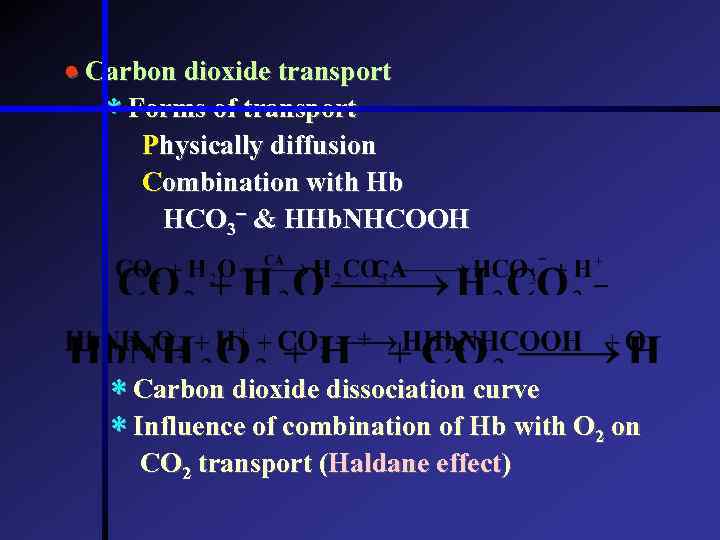 Carbon dioxide transport * Forms of transport Physically diffusion Combination with Hb HCO 3 & HHb. NHCOOH * Carbon dioxide dissociation curve * Influence of combination of Hb with O 2 on CO 2 transport (Haldane effect)
Carbon dioxide transport * Forms of transport Physically diffusion Combination with Hb HCO 3 & HHb. NHCOOH * Carbon dioxide dissociation curve * Influence of combination of Hb with O 2 on CO 2 transport (Haldane effect)
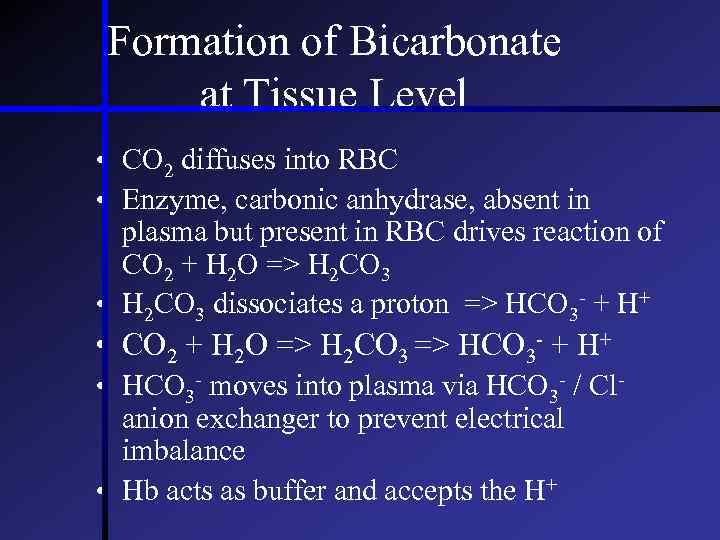 Formation of Bicarbonate at Tissue Level • CO 2 diffuses into RBC • Enzyme, carbonic anhydrase, absent in plasma but present in RBC drives reaction of CO 2 + H 2 O => H 2 CO 3 • H 2 CO 3 dissociates a proton => HCO 3 - + H+ • CO 2 + H 2 O => H 2 CO 3 => HCO 3 - + H+ • HCO 3 - moves into plasma via HCO 3 - / Clanion exchanger to prevent electrical imbalance • Hb acts as buffer and accepts the H+
Formation of Bicarbonate at Tissue Level • CO 2 diffuses into RBC • Enzyme, carbonic anhydrase, absent in plasma but present in RBC drives reaction of CO 2 + H 2 O => H 2 CO 3 • H 2 CO 3 dissociates a proton => HCO 3 - + H+ • CO 2 + H 2 O => H 2 CO 3 => HCO 3 - + H+ • HCO 3 - moves into plasma via HCO 3 - / Clanion exchanger to prevent electrical imbalance • Hb acts as buffer and accepts the H+
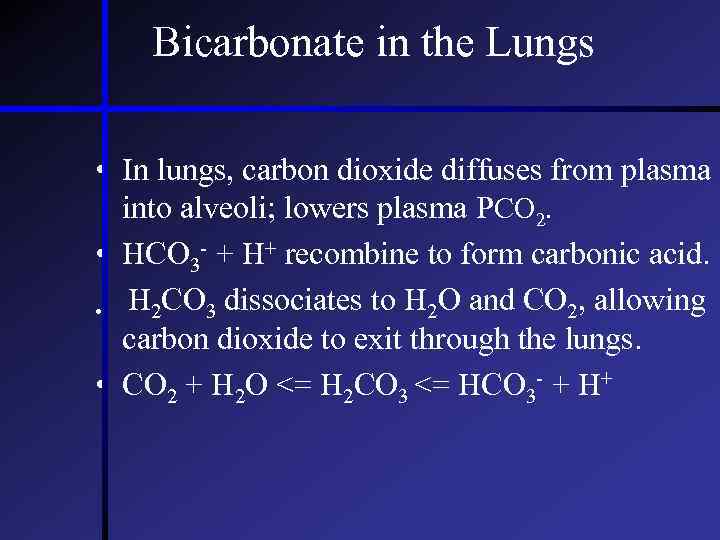 Bicarbonate in the Lungs • In lungs, carbon dioxide diffuses from plasma into alveoli; lowers plasma PCO 2. • HCO 3 - + H+ recombine to form carbonic acid. • H 2 CO 3 dissociates to H 2 O and CO 2, allowing carbon dioxide to exit through the lungs. • CO 2 + H 2 O <= H 2 CO 3 <= HCO 3 - + H+
Bicarbonate in the Lungs • In lungs, carbon dioxide diffuses from plasma into alveoli; lowers plasma PCO 2. • HCO 3 - + H+ recombine to form carbonic acid. • H 2 CO 3 dissociates to H 2 O and CO 2, allowing carbon dioxide to exit through the lungs. • CO 2 + H 2 O <= H 2 CO 3 <= HCO 3 - + H+
 Carbon dioxide dissociation curve
Carbon dioxide dissociation curve
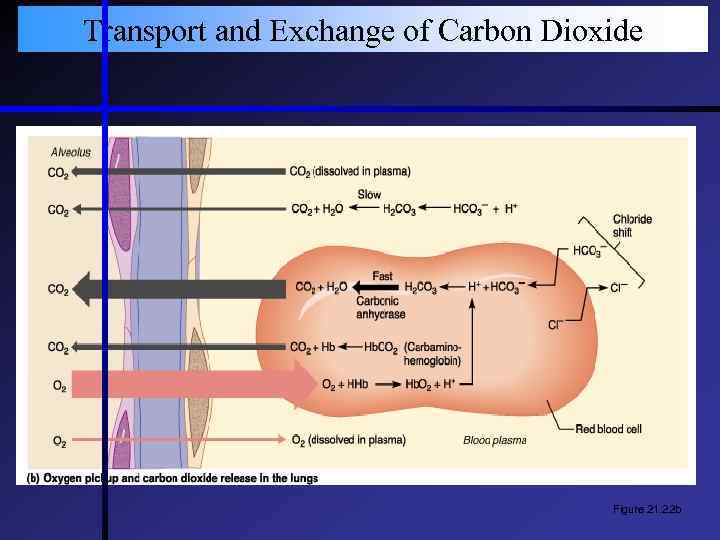 Transport and Exchange of Carbon Dioxide Figure 21. 22 b
Transport and Exchange of Carbon Dioxide Figure 21. 22 b
 Haldane Effect • The amount of carbon dioxide transported is markedly affected by the PO 2 • Haldane effect – the lower the PO 2 and hemoglobin saturation with oxygen, the more carbon dioxide can be carried in the blood • At the tissues, as more carbon dioxide enters the blood: – More oxygen dissociates from hemoglobin (Bohr Haldane Effect effect) – More carbon dioxide combines with hemoglobin, and more bicarbonate ions are formed • This situation is reversed in pulmonary circulation
Haldane Effect • The amount of carbon dioxide transported is markedly affected by the PO 2 • Haldane effect – the lower the PO 2 and hemoglobin saturation with oxygen, the more carbon dioxide can be carried in the blood • At the tissues, as more carbon dioxide enters the blood: – More oxygen dissociates from hemoglobin (Bohr Haldane Effect effect) – More carbon dioxide combines with hemoglobin, and more bicarbonate ions are formed • This situation is reversed in pulmonary circulation
 Regulation of respiratory activity
Regulation of respiratory activity
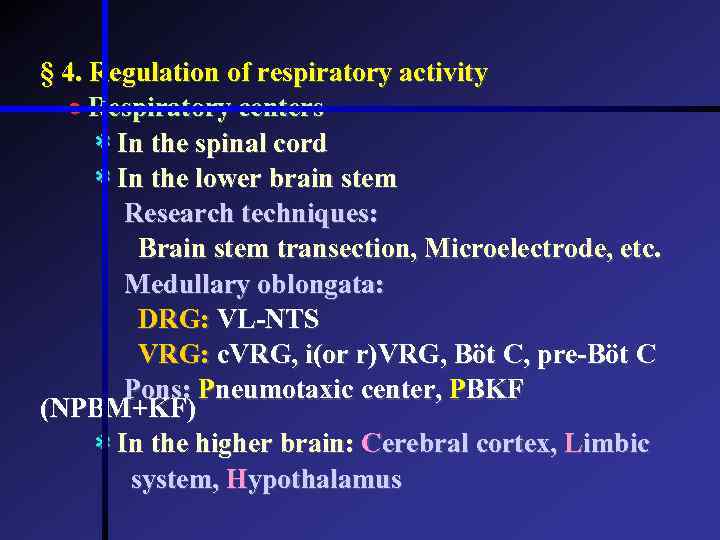 § 4. Regulation of respiratory activity Respiratory centers * In the spinal cord * In the lower brain stem Research techniques: Brain stem transection, Microelectrode, etc. Medullary oblongata: DRG: VL-NTS VRG: c. VRG, i(or r)VRG, Böt C, pre-Böt C Pons: Pneumotaxic center, PBKF (NPBM+KF) * In the higher brain: Cerebral cortex, Limbic system, Hypothalamus
§ 4. Regulation of respiratory activity Respiratory centers * In the spinal cord * In the lower brain stem Research techniques: Brain stem transection, Microelectrode, etc. Medullary oblongata: DRG: VL-NTS VRG: c. VRG, i(or r)VRG, Böt C, pre-Böt C Pons: Pneumotaxic center, PBKF (NPBM+KF) * In the higher brain: Cerebral cortex, Limbic system, Hypothalamus
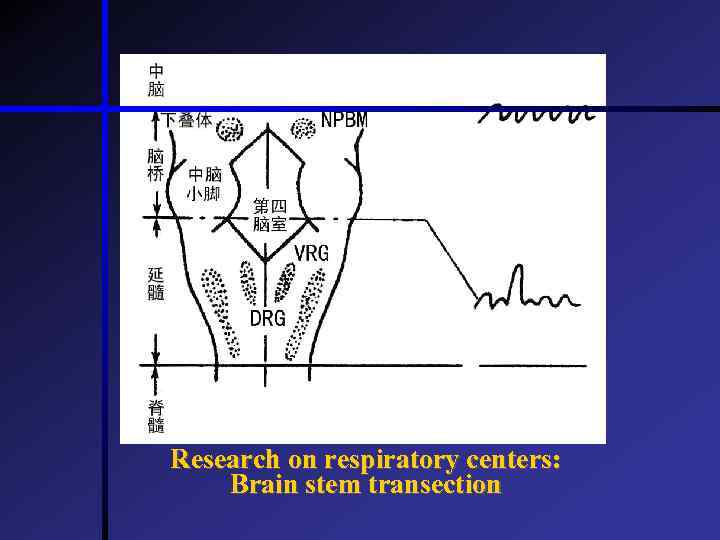 Research on respiratory centers: Brain stem transection
Research on respiratory centers: Brain stem transection
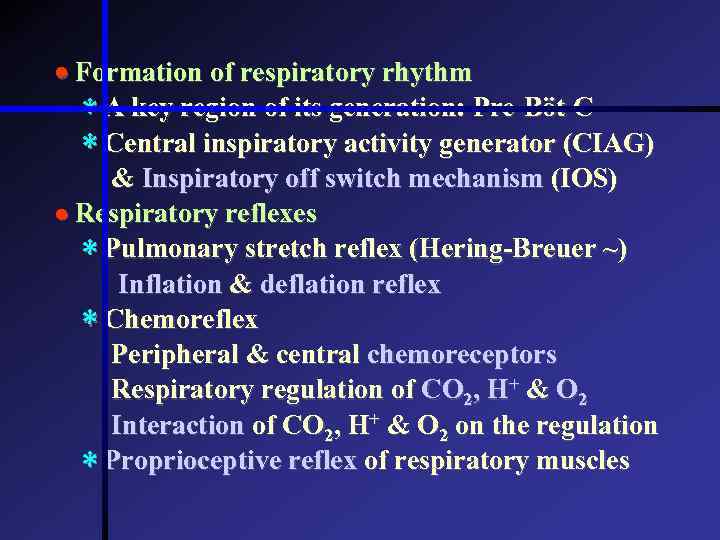 Formation of respiratory rhythm * A key region of its generation: Pre-Böt C * Central inspiratory activity generator (CIAG) & Inspiratory off switch mechanism (IOS) Respiratory reflexes * Pulmonary stretch reflex (Hering-Breuer ~) Inflation & deflation reflex * Chemoreflex Peripheral & central chemoreceptors Respiratory regulation of CO 2, H+ & O 2 Interaction of CO 2, H+ & O 2 on the regulation * Proprioceptive reflex of respiratory muscles
Formation of respiratory rhythm * A key region of its generation: Pre-Böt C * Central inspiratory activity generator (CIAG) & Inspiratory off switch mechanism (IOS) Respiratory reflexes * Pulmonary stretch reflex (Hering-Breuer ~) Inflation & deflation reflex * Chemoreflex Peripheral & central chemoreceptors Respiratory regulation of CO 2, H+ & O 2 Interaction of CO 2, H+ & O 2 on the regulation * Proprioceptive reflex of respiratory muscles
 + PBKF CIAG, Insp. Neurons + − + IOS + + Insp. Muscular Neurons + Insp. movement + PSR
+ PBKF CIAG, Insp. Neurons + − + IOS + + Insp. Muscular Neurons + Insp. movement + PSR
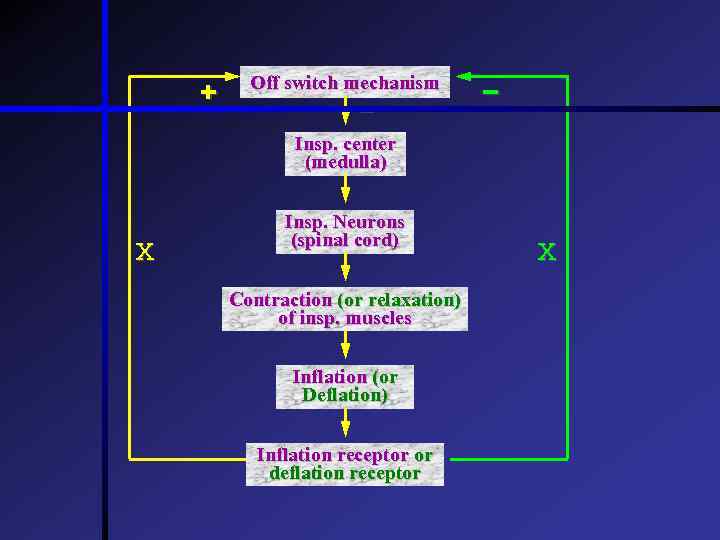 + Off switch mechanism − − Insp. center (medulla) Ⅹ Insp. Neurons (spinal cord) Contraction (or relaxation) of insp. muscles Inflation (or Deflation) Inflation receptor or deflation receptor Ⅹ
+ Off switch mechanism − − Insp. center (medulla) Ⅹ Insp. Neurons (spinal cord) Contraction (or relaxation) of insp. muscles Inflation (or Deflation) Inflation receptor or deflation receptor Ⅹ
![Paco 2 [H+]a Pao 2 O 2 CO 2 H+ Carotid & aortic bodies Paco 2 [H+]a Pao 2 O 2 CO 2 H+ Carotid & aortic bodies](https://present5.com/presentation/3/50203289_397304914.pdf-img/50203289_397304914.pdf-91.jpg) Paco 2 [H+]a Pao 2 O 2 CO 2 H+ Carotid & aortic bodies (− ) O 2 HCO 3 CO 2+H 2 O H+ H+ Blood CSF BBB Resp. Center (Medulla) Resp. A & F Central chemoreceptor A: amplitude; F: frequency BBB: blood-brain barrier CSF: cerebrospinal fluid
Paco 2 [H+]a Pao 2 O 2 CO 2 H+ Carotid & aortic bodies (− ) O 2 HCO 3 CO 2+H 2 O H+ H+ Blood CSF BBB Resp. Center (Medulla) Resp. A & F Central chemoreceptor A: amplitude; F: frequency BBB: blood-brain barrier CSF: cerebrospinal fluid
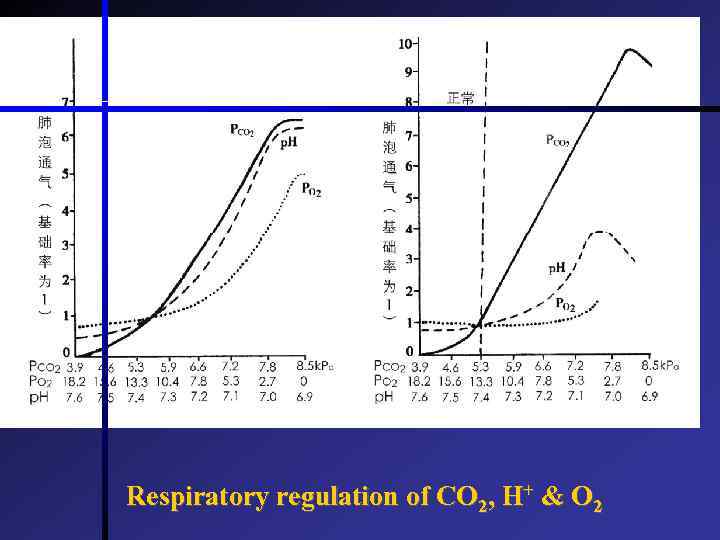 Respiratory regulation of CO 2, H+ & O 2
Respiratory regulation of CO 2, H+ & O 2