c75aac22958ef0644d5052b48d7c36a2.ppt
- Количество слайдов: 24
 Reproductive Health and Preconception Care of HIVInfected Women Development & Implementation of National Recommendations
Reproductive Health and Preconception Care of HIVInfected Women Development & Implementation of National Recommendations
 Disclosure With support from the Centers for Disease Control and Prevention The findings and conclusions in this presentation are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Disclosure With support from the Centers for Disease Control and Prevention The findings and conclusions in this presentation are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
 Objectives • To briefly describe the importance of caring for the reproductive health of HIV-infected women in the US. • To describe the process of developing nationallevel recommendations to improve the reproductive health of HIV-infected women. • List selected recommendations made by the Expert Panel on Reproductive Health and Preconception Care of HIV-infected Women. • To discuss progress toward implementing these recommendations to date.
Objectives • To briefly describe the importance of caring for the reproductive health of HIV-infected women in the US. • To describe the process of developing nationallevel recommendations to improve the reproductive health of HIV-infected women. • List selected recommendations made by the Expert Panel on Reproductive Health and Preconception Care of HIV-infected Women. • To discuss progress toward implementing these recommendations to date.
 Preconception Care of HIV-infected Women (1) • Reproductive health needs not being met • Separation of GYN and HIV care • Preconception counseling and care not being addressed pro-actively • Reproductive health care often not a priority for patients or providers
Preconception Care of HIV-infected Women (1) • Reproductive health needs not being met • Separation of GYN and HIV care • Preconception counseling and care not being addressed pro-actively • Reproductive health care often not a priority for patients or providers
 Preconception Care of HIV-infected Women (2) • With improved survival and health and decreased risk of MTCT, many HIV+ women are choosing to conceive • Effective contraceptive is underused; unplanned pregnancies are common • Women face barriers related to stigma, safe conception with serodiscordant partners, and other issues
Preconception Care of HIV-infected Women (2) • With improved survival and health and decreased risk of MTCT, many HIV+ women are choosing to conceive • Effective contraceptive is underused; unplanned pregnancies are common • Women face barriers related to stigma, safe conception with serodiscordant partners, and other issues
 Preconception Care of HIV-infected Women
Preconception Care of HIV-infected Women
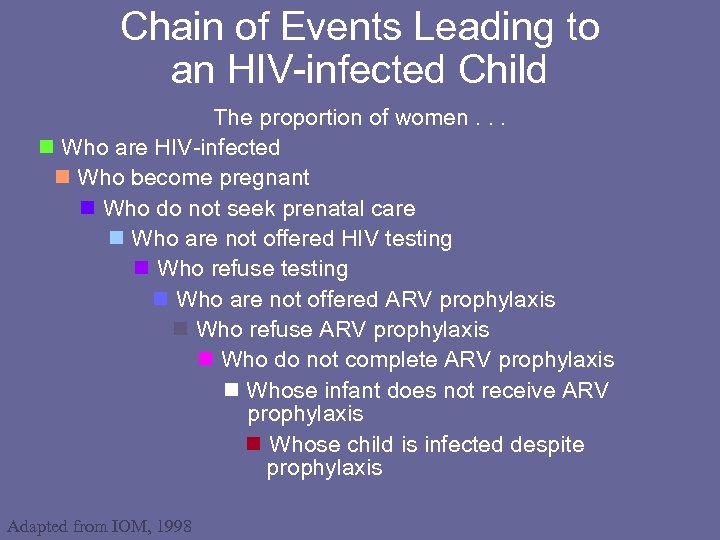 Chain of Events Leading to an HIV-infected Child The proportion of women. . . Who are HIV-infected Who become pregnant Who do not seek prenatal care Who are not offered HIV testing Who refuse testing Who are not offered ARV prophylaxis Who refuse ARV prophylaxis Who do not complete ARV prophylaxis Whose infant does not receive ARV prophylaxis Whose child is infected despite prophylaxis Adapted from IOM, 1998
Chain of Events Leading to an HIV-infected Child The proportion of women. . . Who are HIV-infected Who become pregnant Who do not seek prenatal care Who are not offered HIV testing Who refuse testing Who are not offered ARV prophylaxis Who refuse ARV prophylaxis Who do not complete ARV prophylaxis Whose infant does not receive ARV prophylaxis Whose child is infected despite prophylaxis Adapted from IOM, 1998
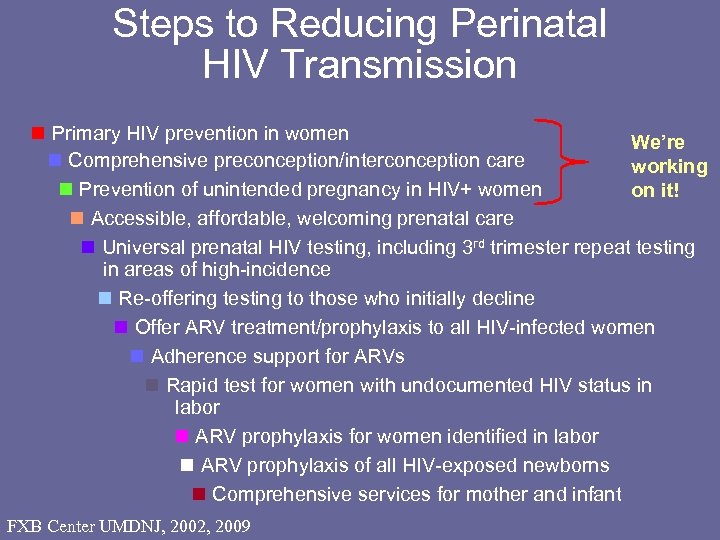 Steps to Reducing Perinatal HIV Transmission Primary HIV prevention in women We’re Comprehensive preconception/interconception care working Prevention of unintended pregnancy in HIV+ women on it! Accessible, affordable, welcoming prenatal care Universal prenatal HIV testing, including 3 rd trimester repeat testing in areas of high-incidence Re-offering testing to those who initially decline Offer ARV treatment/prophylaxis to all HIV-infected women Adherence support for ARVs Rapid test for women with undocumented HIV status in labor ARV prophylaxis for women identified in labor ARV prophylaxis of all HIV-exposed newborns Comprehensive services for mother and infant FXB Center UMDNJ, 2002, 2009
Steps to Reducing Perinatal HIV Transmission Primary HIV prevention in women We’re Comprehensive preconception/interconception care working Prevention of unintended pregnancy in HIV+ women on it! Accessible, affordable, welcoming prenatal care Universal prenatal HIV testing, including 3 rd trimester repeat testing in areas of high-incidence Re-offering testing to those who initially decline Offer ARV treatment/prophylaxis to all HIV-infected women Adherence support for ARVs Rapid test for women with undocumented HIV status in labor ARV prophylaxis for women identified in labor ARV prophylaxis of all HIV-exposed newborns Comprehensive services for mother and infant FXB Center UMDNJ, 2002, 2009
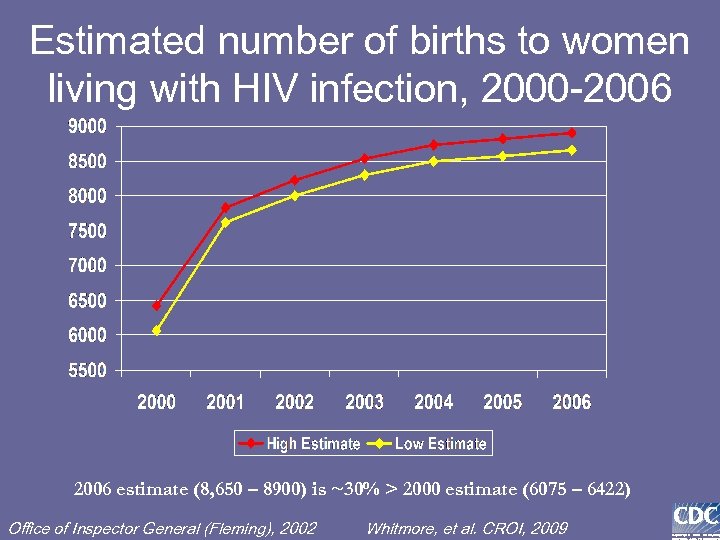 Estimated number of births to women living with HIV infection, 2000 -2006 estimate (8, 650 – 8900) is ~30% > 2000 estimate (6075 – 6422) Office of Inspector General (Fleming), 2002 Whitmore, et al. CROI, 2009
Estimated number of births to women living with HIV infection, 2000 -2006 estimate (8, 650 – 8900) is ~30% > 2000 estimate (6075 – 6422) Office of Inspector General (Fleming), 2002 Whitmore, et al. CROI, 2009
 Live Births Among HIV+ Women Before and After HAART Availability Sharma, et al. AJOG 2007 • Comparison of live birth rates 1994 -1995 (pre -HAART era) and 2001 -2002 (HAART era) in HIV+ and HIV- women 15 -44 yrs • In HAART era 150% increase in live birth rate among HIV+ women vs. 5% increase among HIV- women
Live Births Among HIV+ Women Before and After HAART Availability Sharma, et al. AJOG 2007 • Comparison of live birth rates 1994 -1995 (pre -HAART era) and 2001 -2002 (HAART era) in HIV+ and HIV- women 15 -44 yrs • In HAART era 150% increase in live birth rate among HIV+ women vs. 5% increase among HIV- women
 Clinicians Fail to Routinely Provide Reproductive Counseling to HIV-Infected Women in the US (Averitt Bridge et al. 2008) Women Living Positive Survey • Interviewed 700 HIV+ women – 31% were contemplating pregnancy or had been pregnant – 48% were not asked by their HIV provider if they wanted to have a child • Of women who had thought about pregnancy or who were pregnant – 41% had not discussed HIV treatment change in event of pregnancy – 29% said their HIV provider did not explain the effects of HIV medication on them or their baby
Clinicians Fail to Routinely Provide Reproductive Counseling to HIV-Infected Women in the US (Averitt Bridge et al. 2008) Women Living Positive Survey • Interviewed 700 HIV+ women – 31% were contemplating pregnancy or had been pregnant – 48% were not asked by their HIV provider if they wanted to have a child • Of women who had thought about pregnancy or who were pregnant – 41% had not discussed HIV treatment change in event of pregnancy – 29% said their HIV provider did not explain the effects of HIV medication on them or their baby
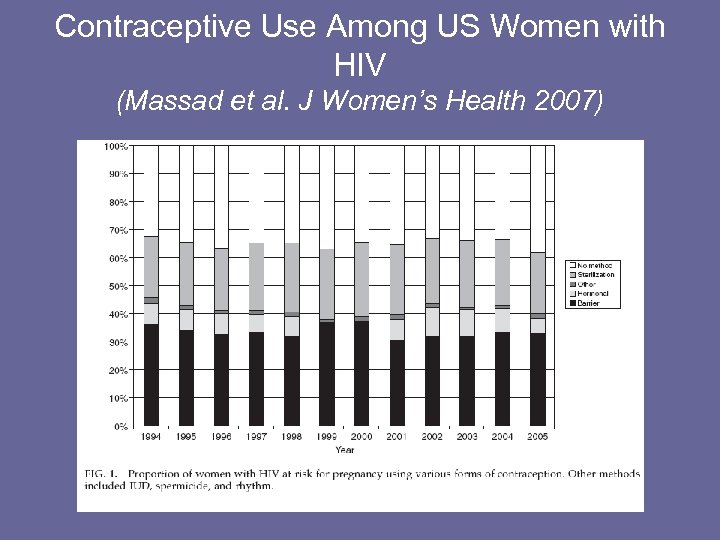 Contraceptive Use Among US Women with HIV (Massad et al. J Women’s Health 2007)
Contraceptive Use Among US Women with HIV (Massad et al. J Women’s Health 2007)
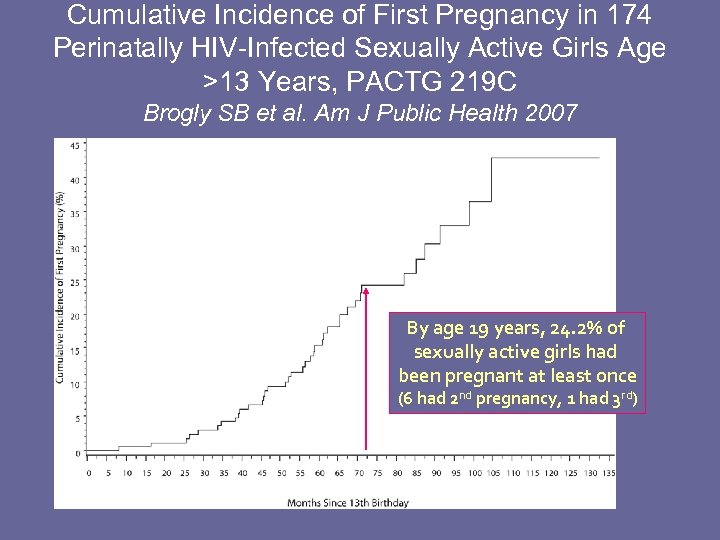 Cumulative Incidence of First Pregnancy in 174 Perinatally HIV-Infected Sexually Active Girls Age >13 Years, PACTG 219 C Brogly SB et al. Am J Public Health 2007 Screen for pregnancy in HIVinfected Adolescents! By age 19 years, 24. 2% of sexually active girls had been pregnant at least once (6 had 2 nd pregnancy, 1 had 3 rd)
Cumulative Incidence of First Pregnancy in 174 Perinatally HIV-Infected Sexually Active Girls Age >13 Years, PACTG 219 C Brogly SB et al. Am J Public Health 2007 Screen for pregnancy in HIVinfected Adolescents! By age 19 years, 24. 2% of sexually active girls had been pregnant at least once (6 had 2 nd pregnancy, 1 had 3 rd)
 Background of Recommendations Spring 2008 • Key informant interviews • Literature review • Key topics, process, & invitees identifed July 2008 • “Expert Panel” sponsored by CDC/FXB – 32 participants – governmental, academic and community representatives
Background of Recommendations Spring 2008 • Key informant interviews • Literature review • Key topics, process, & invitees identifed July 2008 • “Expert Panel” sponsored by CDC/FXB – 32 participants – governmental, academic and community representatives
 The Meeting • Presentations laid groundwork • Facilitated small group work • Development of national recommendations with action steps – Integrate RH and HIV care – Primary HIV prevention • Large group report back with discussion • “One Wish” • Buy-in for ongoing process
The Meeting • Presentations laid groundwork • Facilitated small group work • Development of national recommendations with action steps – Integrate RH and HIV care – Primary HIV prevention • Large group report back with discussion • “One Wish” • Buy-in for ongoing process
 After the Meeting • Recommendations prioritized – High/low impact and resources • Expert Panel ongoing planning calls • Publication and dissemination of recommendations – AIDS - Journal of the International AIDS Society – APHA 2009 – AIDS Alliance “Voices” 2010 – ANAC 2008 & 2010
After the Meeting • Recommendations prioritized – High/low impact and resources • Expert Panel ongoing planning calls • Publication and dissemination of recommendations – AIDS - Journal of the International AIDS Society – APHA 2009 – AIDS Alliance “Voices” 2010 – ANAC 2008 & 2010
 Policy Recommendations • Integrate adult and perinatal US treatment guidelines on preconception care • Organize talking-points about data needs and present to stakeholders in funding research • Advocate to CMS for reimbursement of services • Advocate for Ryan White to include additional funding for women – Include Title X grantees to improve linkages – Co-locate clinics • Conduct Special Project of National Significance (SPNS) projects to demonstrate integration of Title X and Ryan White care providers and services • Collaborate with ACOG on defining preconception care in context of HIV infection
Policy Recommendations • Integrate adult and perinatal US treatment guidelines on preconception care • Organize talking-points about data needs and present to stakeholders in funding research • Advocate to CMS for reimbursement of services • Advocate for Ryan White to include additional funding for women – Include Title X grantees to improve linkages – Co-locate clinics • Conduct Special Project of National Significance (SPNS) projects to demonstrate integration of Title X and Ryan White care providers and services • Collaborate with ACOG on defining preconception care in context of HIV infection
 Program/Services Recommendations • Assemble and disseminate best practices that link Title X agencies and Ryan White agencies • Add a HRSA quality indicator on preconception care • Develop trainings for HIV providers that increase comfort and knowledge about HIV and pregnancy • Hold joint trainings for HIV and Title X providers • Advocate to the AETCs to increase their focus on women’s health • Develop tools for busy HIV providers to streamline preconception care and counseling • Create mentoring program for new HIV providers
Program/Services Recommendations • Assemble and disseminate best practices that link Title X agencies and Ryan White agencies • Add a HRSA quality indicator on preconception care • Develop trainings for HIV providers that increase comfort and knowledge about HIV and pregnancy • Hold joint trainings for HIV and Title X providers • Advocate to the AETCs to increase their focus on women’s health • Develop tools for busy HIV providers to streamline preconception care and counseling • Create mentoring program for new HIV providers
 Research/Data Recommendations • Perform a “fishing expedition” of existing data • Perform research that will address the following gaps in data – # of HIV-infected women who deliver per year? – # of HIV-infected women who get pregnant each year? – How many of these pregnancies are repeat pregnancies? • Conduct studies on – the efficacy of hormonal contraception for HIV-infected women – the effectiveness of reproductive health technologies for HIVinfected women on HAART – Pre- exposure prophylaxis (Pr. EP) for discordant couples
Research/Data Recommendations • Perform a “fishing expedition” of existing data • Perform research that will address the following gaps in data – # of HIV-infected women who deliver per year? – # of HIV-infected women who get pregnant each year? – How many of these pregnancies are repeat pregnancies? • Conduct studies on – the efficacy of hormonal contraception for HIV-infected women – the effectiveness of reproductive health technologies for HIVinfected women on HAART – Pre- exposure prophylaxis (Pr. EP) for discordant couples
 Progress on Recommendations (1) • Integration of adult and perinatal guidelines • Joined forces with like-minded advocates to write AIDS correspondence piece • Joint training for family planning and HIV providers • ACOG survey – Perinatal HIV screening practices – Routine HIV screening practices – Useful preconception care tools
Progress on Recommendations (1) • Integration of adult and perinatal guidelines • Joined forces with like-minded advocates to write AIDS correspondence piece • Joint training for family planning and HIV providers • ACOG survey – Perinatal HIV screening practices – Routine HIV screening practices – Useful preconception care tools
 Progress on Recommendations (2) • Publication and promotion of recommendations – include Title X and HIV experts • Preconception care and counseling tool • CDC Institute on perinatal prevention, including preconception care, at Ryan White All-Grantees meeting in 2010
Progress on Recommendations (2) • Publication and promotion of recommendations – include Title X and HIV experts • Preconception care and counseling tool • CDC Institute on perinatal prevention, including preconception care, at Ryan White All-Grantees meeting in 2010
 Progress on Recommendations (3) • Preconception care incorporated into CDC’s national framework for perinatal elimination – Letter to Office of National AIDS Policy – Ongoing work of the perinatal elimination stakeholders group
Progress on Recommendations (3) • Preconception care incorporated into CDC’s national framework for perinatal elimination – Letter to Office of National AIDS Policy – Ongoing work of the perinatal elimination stakeholders group
 Conclusions • Assuring the reproductive health for HIVinfected women in the US is a means to an end – the end being comprehensive care for women and progress toward the elimination of HIV-infection in children. • The assembly of experts and ongoing working groups are a mechanism to forward changes to both clinical care and HIV policy in the US.
Conclusions • Assuring the reproductive health for HIVinfected women in the US is a means to an end – the end being comprehensive care for women and progress toward the elimination of HIV-infection in children. • The assembly of experts and ongoing working groups are a mechanism to forward changes to both clinical care and HIV policy in the US.
 Thank You To Dr. Jean Anderson for many of her slides for this presentation & To the members of the CDC/FXB Expert Panel
Thank You To Dr. Jean Anderson for many of her slides for this presentation & To the members of the CDC/FXB Expert Panel


