7870d7ad59f2e7aab80e2c04b2be6af5.ppt
- Количество слайдов: 39
Remittance Advice and Financial Updates Presented by EDS Provider Field Consultants October 2009
Agenda • Session Objectives • Remittance Advice (RA) – General Information • The 835 Electronic RA • Sections of the RA • Codes (EOB, ARC, and REMARK) • Edits and Audits • Review of RA Handout • Accounts Receivable • Other Provider Level Adjustments • Primary Medical Provider (PMP) Administrative Payments • Voiding Checks • Electronic Funds Transfers (EFT) Remittance Advice and Financial Updates 2 / October 2009
Session Objectives At the end of this session, providers will be able to: • Learn how to read and understand the weekly Remittance Advice (RA) • Determine why claims deny or suspend • Use your RA and Web inter. Change to follow up on claims • Understand the 835 Transaction • Realize the benefits of electronic funds transfers (EFT) • Understand financial transactions; refunds, accounts receivable (A/R), claim specific and nonclaim-specific transactions • Understand how the EDS system applies edits and audits to properly adjudicate claims Remittance Advice and Financial Updates 3 / October 2009
Remittance Advice – General Information • The most significant tool the IHCP provider has to monitor participation in the program is the weekly Remittance Advice (RA) • The RA provides information about claims processing and financial activity • The Web inter. Change Claim Inquiry/Show More Claim Information functions provide similar information on an individual claim basis • The HIPAA 835 -Health Care Claim Payment Advice is the electronic version of the RA Remittance Advice and Financial Updates 4 / October 2009
Remittance Advice – General Information Beginning September 1, 2009: • Providers must access their RAs online through Web inter. Change • RAs will be available at the beginning of the week in Adobe portable document format (PDF) • A rolling four weeks of paperless RAs will be available online – Once the rolling four weeks has passed, the RA can be requested by contacting EDS Customer Assistance at 800577 -1278 • A charge of 15 cents per page will apply • Can request whole RAs only • Copies of the RAs in Adobe PDF may be saved to providers’ personal storage devices for future reference Remittance Advice and Financial Updates 5 / October 2009
Remittance Advice – General Information • RAs are issued weekly in an Adobe PDF format – Providers enrolled in electronic funds transfer (EFT) receive a copy of their check via Web inter. Change – Providers not enrolled with EFT will obtain a paper check that will be mailed weekly • Providers who wish to receive RA information electronically (HIPAA 835 transaction) must contract with an approved vendor who has completed the trading partner profile and agreement • The IHCP 835 Transaction Companion Guide is available at www. indianamedicaid. com, and the Web inter. Change HELP function Remittance Advice and Financial Updates 6 / October 2009
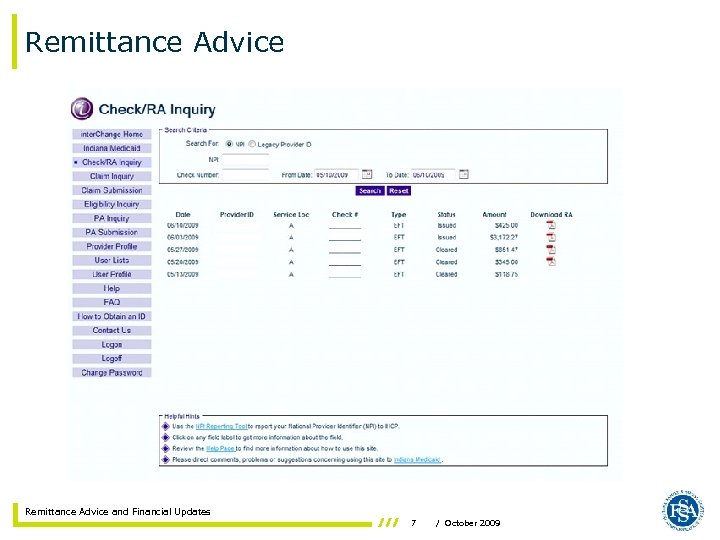
Remittance Advice and Financial Updates 7 / October 2009
Remittance Advice – General Information • RAs provide information about adjudicated claims that are paid, denied, adjusted, and claims in process • The RA outlines claim information at the HEADER (claim level) and the DETAIL (service line level) • Each section of the RA, such as Claims Paid or Claims Denied, totals the information at the end of that section Remittance Advice and Financial Updates 8 / October 2009
Remittance Advice – Section Descriptions • Claims Paid – This section shows claims with a paid status, including claims paid at zero • Claims Denied – This section shows detailed information for denied claims Remittance Advice and Financial Updates 9 / October 2009
Remittance Advice – Section Descriptions • Claims in Process – This section lists claims in the processing cycle that have not yet been finalized, such as the following: – Claims that have attachments – Claims that require manual pricing – Voids and Replacements that have not finalized – Suspended Claims – Claims in process will ultimately be shown as paid, denied or adjusted on a subsequent RA – Claims in suspense only appear in the RA for the week in which they first suspend, until they are paid or denied Note: The RA will repeat each section for each claim type, such as inpatient, outpatient, and crossover Remittance Advice and Financial Updates 10 / October 2009
Remittance Advice – Section Descriptions • Claim Void/Replacements – This section lists claims that have been voided or replaced – Each adjusted claim shows two header internal control number (ICN) lines: • The first header line is for the original claim (mother claim) • The second header line is for the replacement claim (daughter claim) » If a claim is voided or replaced in the same financial cycle as the original claim, the original claim will appear in the denied claim section, and the void/replacement will show in the void/replacement section • Financial Transactions – This section lists the provider level adjustments, which include nonclaim-specific payouts, refunds, and accounts receivable (A/R) transactions Remittance Advice and Financial Updates 11 / October 2009
Remittance Advice – Section Descriptions • EOB Code Descriptions – This section lists Explanation of Benefit (EOB) codes applied to submitted claims, along with the respective narratives that explain why the claim suspended, denied, or did not pay in full – These codes provide the most information as to why the claim denied • ARC Code Descriptions – This section lists Adjustment Reason Codes (ARCs) along with respective code narratives that reflect the adjustments in payment between billed amounts and allowed or payment amounts Note: The narratives for EOB and ARC codes are listed at the end of the RA Remittance Advice and Financial Updates 12 / October 2009
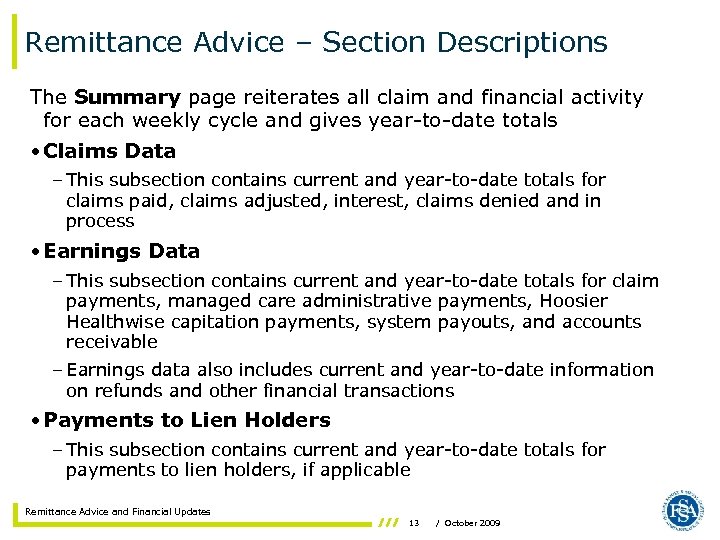
Remittance Advice – Section Descriptions The Summary page reiterates all claim and financial activity for each weekly cycle and gives year-to-date totals • Claims Data – This subsection contains current and year-to-date totals for claims paid, claims adjusted, interest, claims denied and in process • Earnings Data – This subsection contains current and year-to-date totals for claim payments, managed care administrative payments, Hoosier Healthwise capitation payments, system payouts, and accounts receivable – Earnings data also includes current and year-to-date information on refunds and other financial transactions • Payments to Lien Holders – This subsection contains current and year-to-date totals for payments to lien holders, if applicable Remittance Advice and Financial Updates 13 / October 2009
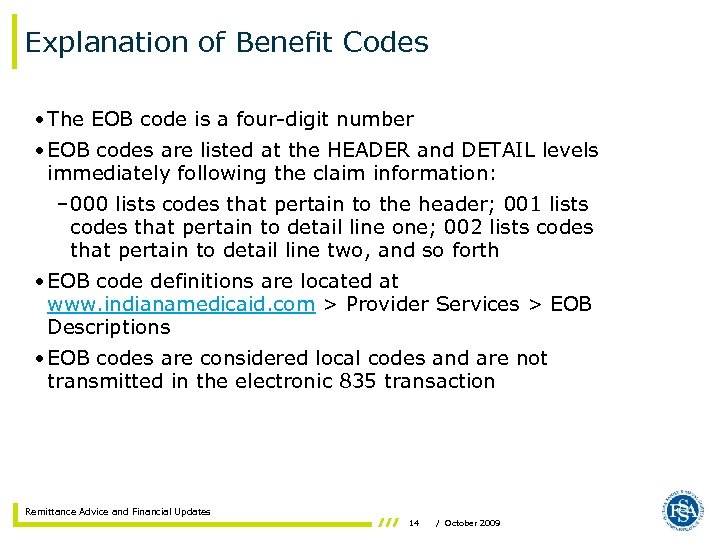
Explanation of Benefit Codes • The EOB code is a four-digit number • EOB codes are listed at the HEADER and DETAIL levels immediately following the claim information: – 000 lists codes that pertain to the header; 001 lists codes that pertain to detail line one; 002 lists codes that pertain to detail line two, and so forth • EOB code definitions are located at www. indianamedicaid. com > Provider Services > EOB Descriptions • EOB codes are considered local codes and are not transmitted in the electronic 835 transaction Remittance Advice and Financial Updates 14 / October 2009
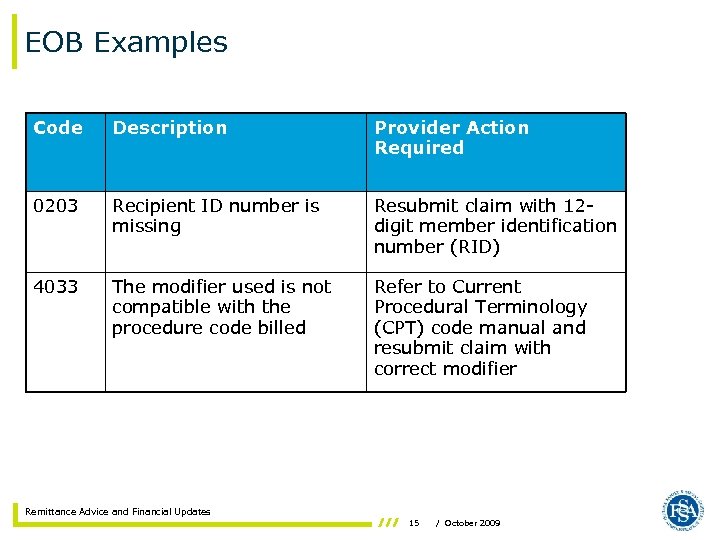
EOB Examples Code Description Provider Action Required 0203 Recipient ID number is missing Resubmit claim with 12 digit member identification number (RID) 4033 The modifier used is not compatible with the procedure code billed Refer to Current Procedural Terminology (CPT) code manual and resubmit claim with correct modifier Remittance Advice and Financial Updates 15 / October 2009
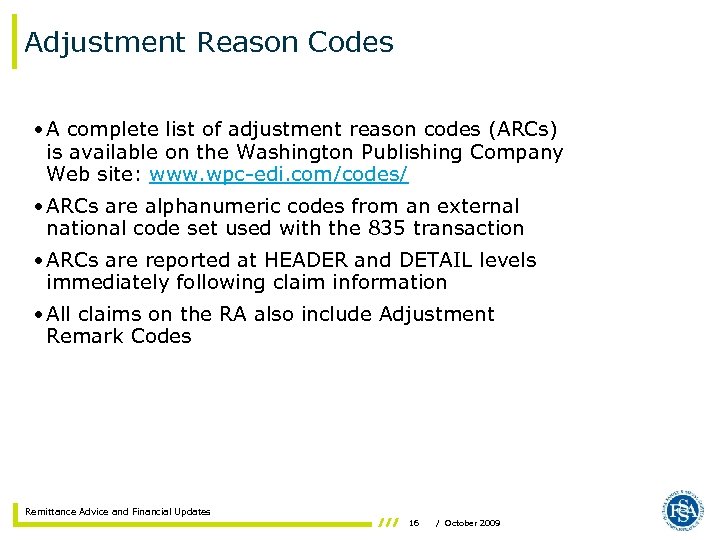
Adjustment Reason Codes • A complete list of adjustment reason codes (ARCs) is available on the Washington Publishing Company Web site: www. wpc-edi. com/codes/ • ARCs are alphanumeric codes from an external national code set used with the 835 transaction • ARCs are reported at HEADER and DETAIL levels immediately following claim information • All claims on the RA also include Adjustment Remark Codes Remittance Advice and Financial Updates 16 / October 2009
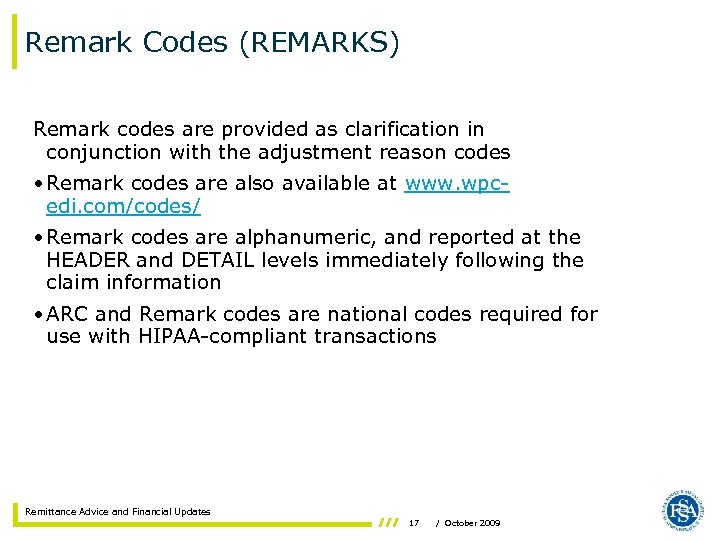
Remark Codes (REMARKS) Remark codes are provided as clarification in conjunction with the adjustment reason codes • Remark codes are also available at www. wpc- edi. com/codes/ • Remark codes are alphanumeric, and reported at the HEADER and DETAIL levels immediately following the claim information • ARC and Remark codes are national codes required for use with HIPAA-compliant transactions Remittance Advice and Financial Updates 17 / October 2009
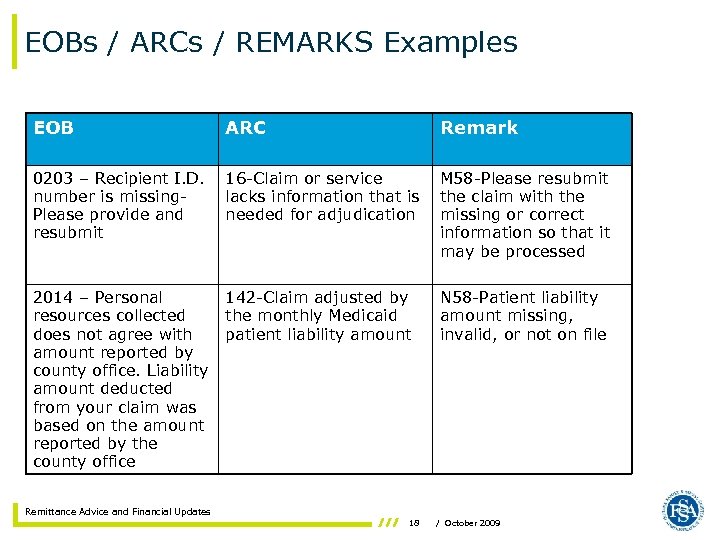
EOBs / ARCs / REMARKS Examples EOB ARC Remark 0203 – Recipient I. D. number is missing. Please provide and resubmit 16 -Claim or service lacks information that is needed for adjudication M 58 -Please resubmit the claim with the missing or correct information so that it may be processed 2014 – Personal resources collected does not agree with amount reported by county office. Liability amount deducted from your claim was based on the amount reported by the county office 142 -Claim adjusted by the monthly Medicaid patient liability amount N 58 -Patient liability amount missing, invalid, or not on file Remittance Advice and Financial Updates 18 / October 2009
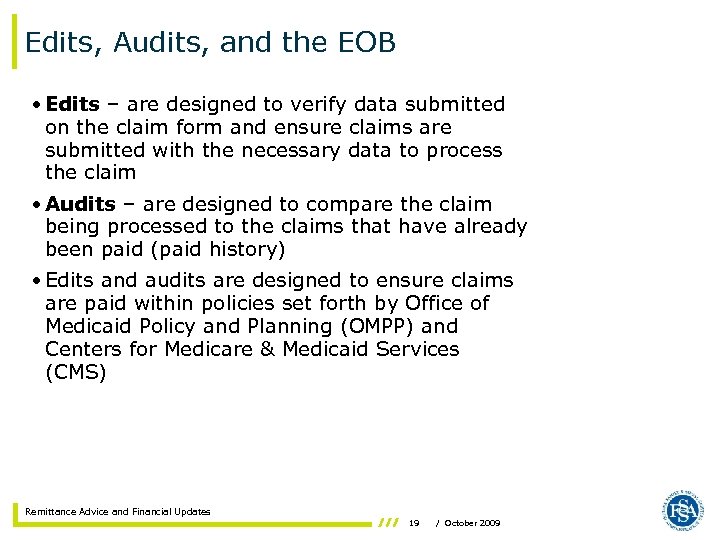
Edits, Audits, and the EOB • Edits – are designed to verify data submitted on the claim form and ensure claims are submitted with the necessary data to process the claim • Audits – are designed to compare the claim being processed to the claims that have already been paid (paid history) • Edits and audits are designed to ensure claims are paid within policies set forth by Office of Medicaid Policy and Planning (OMPP) and Centers for Medicare & Medicaid Services (CMS) Remittance Advice and Financial Updates 19 / October 2009
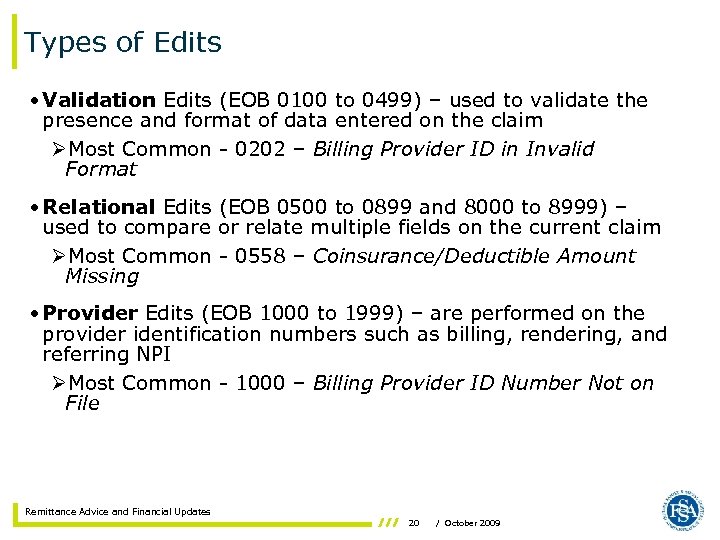
Types of Edits • Validation Edits (EOB 0100 to 0499) – used to validate the presence and format of data entered on the claim ØMost Common - 0202 – Billing Provider ID in Invalid Format • Relational Edits (EOB 0500 to 0899 and 8000 to 8999) – used to compare or relate multiple fields on the current claim ØMost Common - 0558 – Coinsurance/Deductible Amount Missing • Provider Edits (EOB 1000 to 1999) – are performed on the provider identification numbers such as billing, rendering, and referring NPI ØMost Common - 1000 – Billing Provider ID Number Not on File Remittance Advice and Financial Updates 20 / October 2009
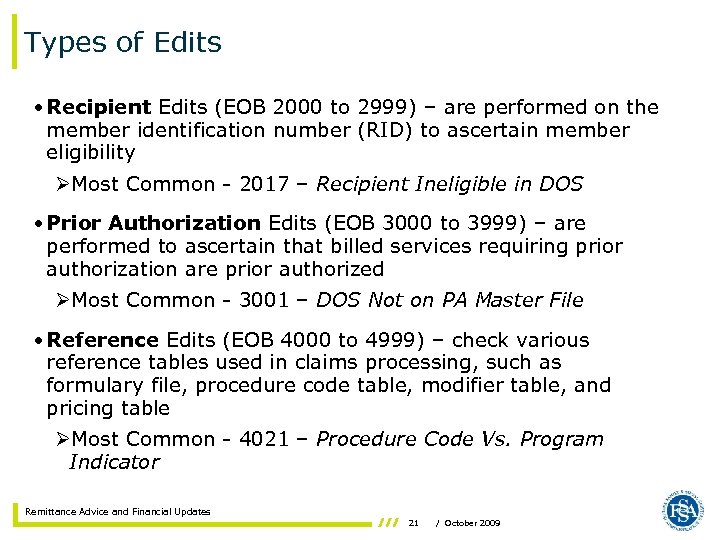
Types of Edits • Recipient Edits (EOB 2000 to 2999) – are performed on the member identification number (RID) to ascertain member eligibility ØMost Common - 2017 – Recipient Ineligible in DOS • Prior Authorization Edits (EOB 3000 to 3999) – are performed to ascertain that billed services requiring prior authorization are prior authorized ØMost Common - 3001 – DOS Not on PA Master File • Reference Edits (EOB 4000 to 4999) – check various reference tables used in claims processing, such as formulary file, procedure code table, modifier table, and pricing table ØMost Common - 4021 – Procedure Code Vs. Program Indicator Remittance Advice and Financial Updates 21 / October 2009
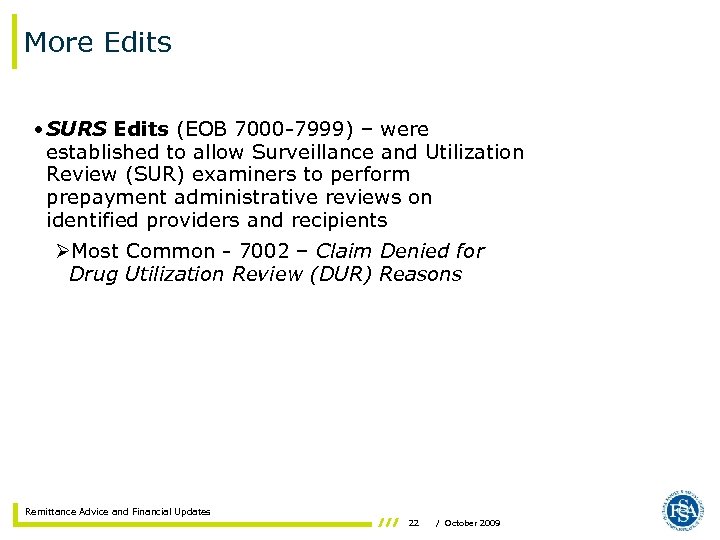
More Edits • SURS Edits (EOB 7000 -7999) – were established to allow Surveillance and Utilization Review (SUR) examiners to perform prepayment administrative reviews on identified providers and recipients ØMost Common - 7002 – Claim Denied for Drug Utilization Review (DUR) Reasons Remittance Advice and Financial Updates 22 / October 2009
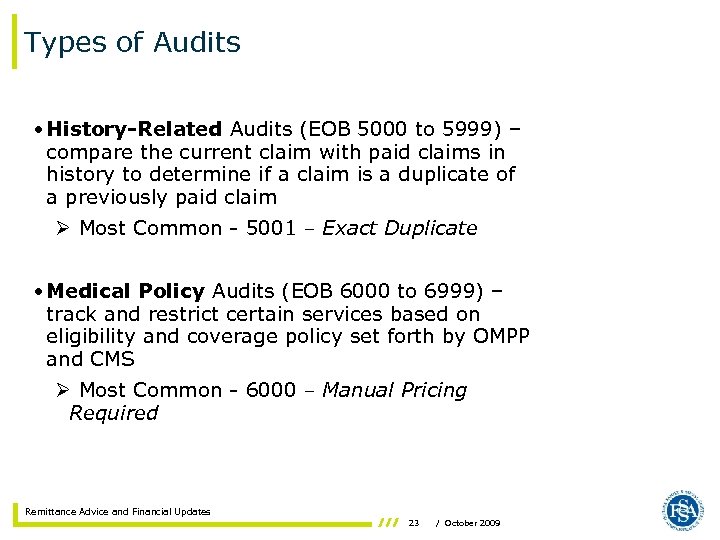
Types of Audits • History-Related Audits (EOB 5000 to 5999) – compare the current claim with paid claims in history to determine if a claim is a duplicate of a previously paid claim Ø Most Common - 5001 – Exact Duplicate • Medical Policy Audits (EOB 6000 to 6999) – track and restrict certain services based on eligibility and coverage policy set forth by OMPP and CMS Ø Most Common - 6000 – Manual Pricing Required Remittance Advice and Financial Updates 23 / October 2009
RA Handout Review Please refer to your RA handout Remittance Advice and Financial Updates 24 / October 2009
Accounts Receivable (A/R) • An accounts receivable is established when the OMPP or one of its contractors determines that a provider owes money to the IHCP • An accounts receivable may be established either automatically or manually Remittance Advice and Financial Updates 25 / October 2009
Accounts Receivable (A/R) • Automatically established ARs are set up for adjustments when the net reimbursement is less than the original payment • ICNs begin with ‘ 5’: Ø 50 – Noncheck-related adjustment Ø 51 – Check-related adjustment Ø 54 – Provider voids check with adjustment Ø 55 – Long-term care (LTC) retro-rate adjustments Ø 56 – Mass adjustments initiated by EDS Ø 59 – Point of Service (POS) reversals Ø 62 – Electronic replacement Ø 63 – Electronic void Remittance Advice and Financial Updates 26 / October 2009
Accounts Receivable (A/R) • Manually established ARs are set up for: Ø Repayment Agreements Ø Tax Assessments for Intermediate Care Facilities for the Mentally Retarded (ICF/MR) and Community Residential Facility for the Developmentally Disabled (CRF/DD) Ø SUR Audits Remittance Advice and Financial Updates 27 / October 2009
Accounts Receivable (A/R) • Four methods to recoup an A/R: – The claim offset process occurs when the A/R is systematically deducted from the weekly RA payment until the full amount is recouped – The provider recognizes that an overpayment exists and sends a refund check to satisfy the A/R – The provider makes an agreement to make installment payments – An inactive provider number’s A/R is transferred to another active provider number that shares the same tax identification number • If an A/R is not recovered within 15 business days, EDS mails a transfer letter (if the provider shares a common TIN with another provider), or a demand letter requesting repayment Remittance Advice and Financial Updates 28 / October 2009
Other Provider Level Adjustments • ICF/MR and CRF/DD Tax Assessments – An assessment in conjunction with the rate-setting process • System Payouts (Nonclaim-specific) – When a provider is due a refund that cannot be tied to a specific claim • Partial Provider Payment and Repayment Agreements – When a provider has specific claims processing issues that are causing an undue financial hardship • Nonclaim-Specific Refunds – When a provider refunds money that cannot be tied to a specific claim • Liens Against Provider Payments – When EDS must process IRS or court-ordered liens Remittance Advice and Financial Updates 29 / October 2009
Primary Medical Provider – Monthly Administrative Fee • Providers who participate in Care Select as primary medical providers (PMPs) receive a monthly administrative fee per member – $15 per member per month – A panel of 150 members = $2250 • The aggregate administrative fee payment appears on the summary page of the RA under the heading Managed Care Administrative Payment • Both the current and year-to-date administrative fee payments made to the PMP are listed Remittance Advice and Financial Updates 30 / October 2009
Voiding a Check • A provider that receives an IHCP check and wants to return the entire amount, can return the check to EDS for voiding • The claims associated with that check will be voided automatically • When necessary, claims must be resubmitted to EDS for processing • A provider can initiate a check void for the following reasons: – The wrong provider received the payment – The IHCP incorrectly paid the claim twice – The payment was made payable to the wrong service location Remittance Advice and Financial Updates 31 / October 2009
Stop Payment and Check Reissue • A stop payment request should be made when: – The provider does not receive its check within 14 calendar days after the RA has been posted to the Web • To request that a check be reissued, call the EDS Customer Assistance Unit at (317) 655 -3240 or 1 -800 -577 -1278 • The provider must confirm the Pay To address • EDS will confirm that the check has not cleared before stopping payment and reissuing a check • Avoid reissues by: – Keeping addresses current in your Provider Profile • View your provider profile online via Web inter. Change – Enrolling in Electronic Funds Transfer (EFT) Remittance Advice and Financial Updates 32 / October 2009
Electronic Funds Transfer (EFT) • Advantages: – Expedites cash flow – Prevents lost checks – Automates deposits to your account – Cost effective – Easy to implement Remittance Advice and Financial Updates 33 / October 2009
Electronic Funds Transfer (EFT) • EFT information on the RA – EFT check number begins with ‘ 9’ and can be seen via Web inter. Change • Payment is directly deposited to your account – EFTs deposited by Wednesday each week • If no deposit occurs, call Customer Assistance • When EFT rejections occur, provider will receive a paper check instead – Common reasons for lack of deposit: • Wrong bank routing number • Incorrect account number • Account has been closed – To correct, please update on the Web inter. Change Remittance Advice and Financial Updates 34 / October 2009
Electronic Funds Transfer (EFT) How to Enroll • Providers can enroll to receive EFTs via Web inter. Change under the Provider Profile menu option • Providers may also complete a paper EFT form – www. indianamedicaid. com – Click Provider Services, Provider Enrollment • Complete the EFT form • Include a voided check with the EFT form and mail to provider enrollment – Allow four weeks for processing Remittance Advice and Financial Updates 35 / October 2009
Electronic Funds Transfer (EFT) • How EDS coordinates with your bank – EDS must have the American Banking Association (ABA) transit routing number – Your bank account number for deposit and type of account (for example: checking or savings) – What action is being authorized • Start • Change • Cancellation – If all is in order, EFT will begin within three payment cycles – Continue to receive paper checks until EFT is successfully established Remittance Advice and Financial Updates 36 / October 2009
Helpful Tools Avenues of Resolution • IHCP Web site at www. indianamedicaid. com • IHCP Provider Manual (Web, CD-ROM, or paper) • Customer Assistance – 1 -800 -577 -1278, or – (317) 655 -3240 in the Indianapolis local area • Written Correspondence – P. O. Box 7263 Indianapolis, IN 46207 -7263 • Provider Relations field consultant – View a current territory map and contact information online at www. indianamedicaid. com Remittance Advice and Financial Updates 37 / October 2009
Questions Remittance Advice and Financial Updates 38 / October 2009
Office of Medicaid Policy and Planning (OMPP) 402 W. Washington St, Room W 374 Indianapolis, IN 46204 EDS, an HP Company 950 N. Meridian St. , Suite 1150 Indianapolis, IN 46204 EDS and the EDS logo are registered trademarks of Hewlett-Packard Development Company, LP. HP is an equal opportunity employer and values the diversity of its people. © 2009 Hewlett-Packard Development Company, LP. October 2009
7870d7ad59f2e7aab80e2c04b2be6af5.ppt