c899cbf3d91a2952ced6357e59d9a522.ppt
- Количество слайдов: 42
 Relationship, Communication and Efficiency: A Team Development Model 2008 STFM / AAFP Conference on Practice Improvement Savannah, Georgia Larry Mauksch, M. Ed University of Washington Department of Family Medicine
Relationship, Communication and Efficiency: A Team Development Model 2008 STFM / AAFP Conference on Practice Improvement Savannah, Georgia Larry Mauksch, M. Ed University of Washington Department of Family Medicine
 Acknowledgements Marillac Clinic n The Everett Clinic n Wentachee Valley Clinic n Dan Cherkin, Ph. D n William Phillips, MD, MPH n Karen Sherman, Ph. D n Julia Smith, MD n Rene Hawkes n
Acknowledgements Marillac Clinic n The Everett Clinic n Wentachee Valley Clinic n Dan Cherkin, Ph. D n William Phillips, MD, MPH n Karen Sherman, Ph. D n Julia Smith, MD n Rene Hawkes n
 Outline • Rationale: The current system is not working well • Process: mastery takes practice • Goal: making the patient’s visit path satisfying, effective and efficient • Content: • Communication, Relationship and Efficiency • Agenda setting and patient activation • Team Development
Outline • Rationale: The current system is not working well • Process: mastery takes practice • Goal: making the patient’s visit path satisfying, effective and efficient • Content: • Communication, Relationship and Efficiency • Agenda setting and patient activation • Team Development
 PRACTICE RECOMMENDATION #1 • • Physicians and other health care team members should be trained in communication skills that promote shared decision making and self management Strength of evidence: • • • Communication training is likely to promote patient centered care. Strength of evidence A Communication training may increase patient satisfaction and engagement in self care. Strength of evidence B. There is less evidence that training can improve performance of others beside physicians. 17 Randomized controlled trials examined. Lewin SA, et al. . Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database of Systematic Reviews 2001, Issue 4. http: //www. cochrane. org/reviews/en/ab 003267. html
PRACTICE RECOMMENDATION #1 • • Physicians and other health care team members should be trained in communication skills that promote shared decision making and self management Strength of evidence: • • • Communication training is likely to promote patient centered care. Strength of evidence A Communication training may increase patient satisfaction and engagement in self care. Strength of evidence B. There is less evidence that training can improve performance of others beside physicians. 17 Randomized controlled trials examined. Lewin SA, et al. . Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database of Systematic Reviews 2001, Issue 4. http: //www. cochrane. org/reviews/en/ab 003267. html
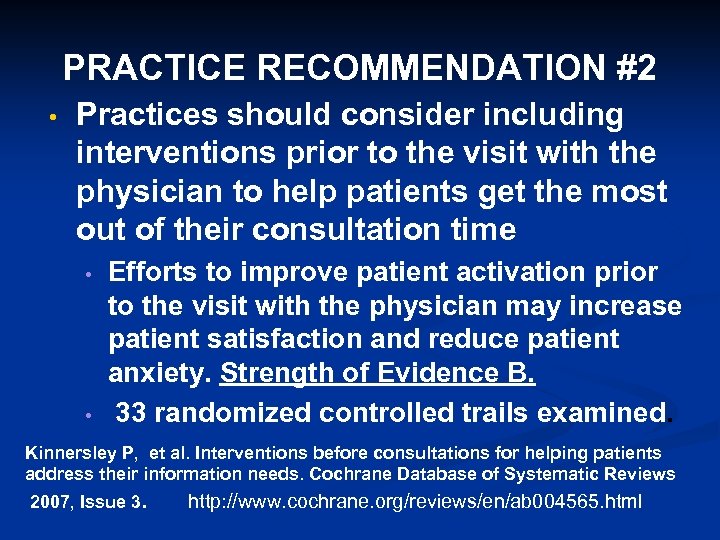 PRACTICE RECOMMENDATION #2 • Practices should consider including interventions prior to the visit with the physician to help patients get the most out of their consultation time • • Efforts to improve patient activation prior to the visit with the physician may increase patient satisfaction and reduce patient anxiety. Strength of Evidence B. 33 randomized controlled trails examined. Kinnersley P, et al. Interventions before consultations for helping patients address their information needs. Cochrane Database of Systematic Reviews 2007, Issue 3. http: //www. cochrane. org/reviews/en/ab 004565. html
PRACTICE RECOMMENDATION #2 • Practices should consider including interventions prior to the visit with the physician to help patients get the most out of their consultation time • • Efforts to improve patient activation prior to the visit with the physician may increase patient satisfaction and reduce patient anxiety. Strength of Evidence B. 33 randomized controlled trails examined. Kinnersley P, et al. Interventions before consultations for helping patients address their information needs. Cochrane Database of Systematic Reviews 2007, Issue 3. http: //www. cochrane. org/reviews/en/ab 004565. html
 Rationale Why change the clinic system?
Rationale Why change the clinic system?
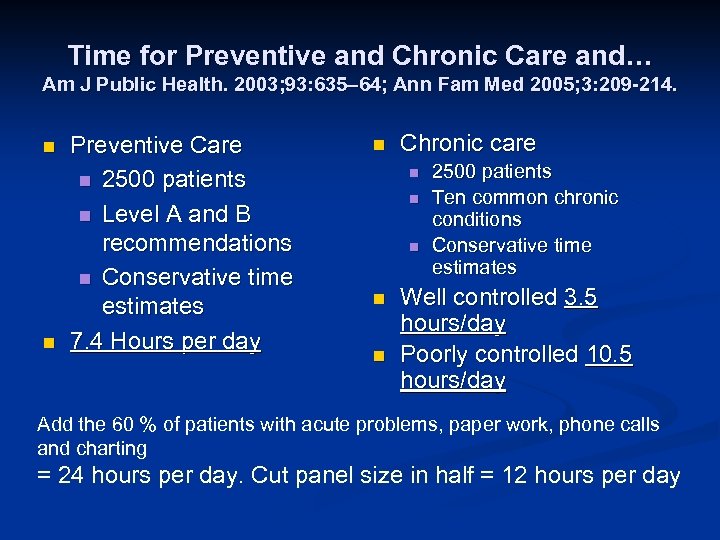 Time for Preventive and Chronic Care and… Am J Public Health. 2003; 93: 635– 64; Ann Fam Med 2005; 3: 209 -214. n n Preventive Care n 2500 patients n Level A and B recommendations n Conservative time estimates 7. 4 Hours per day n Chronic care n n n 2500 patients Ten common chronic conditions Conservative time estimates Well controlled 3. 5 hours/day Poorly controlled 10. 5 hours/day Add the 60 % of patients with acute problems, paper work, phone calls and charting = 24 hours per day. Cut panel size in half = 12 hours per day
Time for Preventive and Chronic Care and… Am J Public Health. 2003; 93: 635– 64; Ann Fam Med 2005; 3: 209 -214. n n Preventive Care n 2500 patients n Level A and B recommendations n Conservative time estimates 7. 4 Hours per day n Chronic care n n n 2500 patients Ten common chronic conditions Conservative time estimates Well controlled 3. 5 hours/day Poorly controlled 10. 5 hours/day Add the 60 % of patients with acute problems, paper work, phone calls and charting = 24 hours per day. Cut panel size in half = 12 hours per day
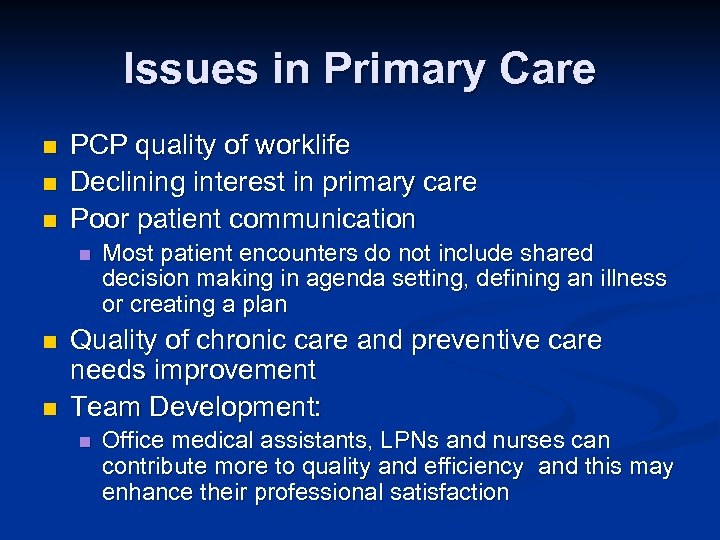 Issues in Primary Care n n n PCP quality of worklife Declining interest in primary care Poor patient communication n Most patient encounters do not include shared decision making in agenda setting, defining an illness or creating a plan Quality of chronic care and preventive care needs improvement Team Development: n Office medical assistants, LPNs and nurses can contribute more to quality and efficiency and this may enhance their professional satisfaction
Issues in Primary Care n n n PCP quality of worklife Declining interest in primary care Poor patient communication n Most patient encounters do not include shared decision making in agenda setting, defining an illness or creating a plan Quality of chronic care and preventive care needs improvement Team Development: n Office medical assistants, LPNs and nurses can contribute more to quality and efficiency and this may enhance their professional satisfaction
 Communication, Time Use and Teamwork • Increased use of quality enhancing communication skills can increase, decrease or not affect visit length • Determinants • • Communication style of team members Number of problems/issues addressed Unacknowledged psychosocial problems and their affect on the communication process Problem complexity Transparency of visit structure and process Individual and team training Pre-visit agenda setting and patient activation Self management support
Communication, Time Use and Teamwork • Increased use of quality enhancing communication skills can increase, decrease or not affect visit length • Determinants • • Communication style of team members Number of problems/issues addressed Unacknowledged psychosocial problems and their affect on the communication process Problem complexity Transparency of visit structure and process Individual and team training Pre-visit agenda setting and patient activation Self management support
 Five Questions for the Team • Have we made a connection with this patient? • Have we confirmed what is most important to this patient today? • And to us? • Do we understand the patient’s view on today’s health concern(s)? • Is the patient invested in the plan? • How confident is the patient in being able to carry out the plan?
Five Questions for the Team • Have we made a connection with this patient? • Have we confirmed what is most important to this patient today? • And to us? • Do we understand the patient’s view on today’s health concern(s)? • Is the patient invested in the plan? • How confident is the patient in being able to carry out the plan?
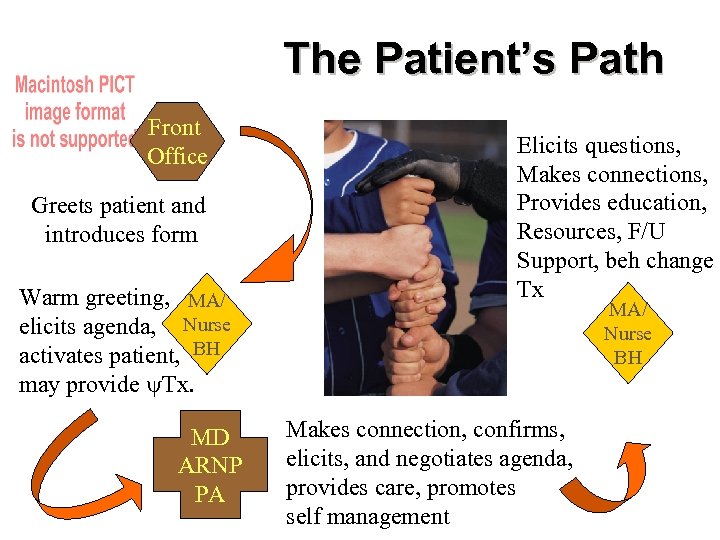 The Patient’s Path Front Office Greets patient and introduces form Warm greeting, MA/ elicits agenda, Nurse activates patient, BH may provide Tx. MD ARNP PA Elicits questions, Makes connections, Provides education, Resources, F/U Support, beh change Tx MA/ Nurse BH Makes connection, confirms, elicits, and negotiates agenda, provides care, promotes self management
The Patient’s Path Front Office Greets patient and introduces form Warm greeting, MA/ elicits agenda, Nurse activates patient, BH may provide Tx. MD ARNP PA Elicits questions, Makes connections, Provides education, Resources, F/U Support, beh change Tx MA/ Nurse BH Makes connection, confirms, elicits, and negotiates agenda, provides care, promotes self management
 Process Change is hard won n Systems resist change and revert to earlier states of function n Mastery requires practice n
Process Change is hard won n Systems resist change and revert to earlier states of function n Mastery requires practice n
 Process Components n Use of experiential elements to promote skill development n Interdependent elements n Integration of structures to sustain change and innovation
Process Components n Use of experiential elements to promote skill development n Interdependent elements n Integration of structures to sustain change and innovation
 Experiential elements to promote skill development Using peer role models to establish organizational culture n Using peer role models to demonstrate skills n Using structured observation (observation forms) n Peer observation n Team member observation n
Experiential elements to promote skill development Using peer role models to establish organizational culture n Using peer role models to demonstrate skills n Using structured observation (observation forms) n Peer observation n Team member observation n
 Interdependent elements n Communication and relationship skills n Mindfulness n Team meetings to practice skills and discuss innovation
Interdependent elements n Communication and relationship skills n Mindfulness n Team meetings to practice skills and discuss innovation
 Integration of structures to sustain change and innovation n Regular peer observation n Regular huddles n Regular team meetings focused on team investment, celebration, innovation and sustaining change
Integration of structures to sustain change and innovation n Regular peer observation n Regular huddles n Regular team meetings focused on team investment, celebration, innovation and sustaining change
 Content Communication skills n Agenda setting n Patient activation n Team development work n
Content Communication skills n Agenda setting n Patient activation n Team development work n
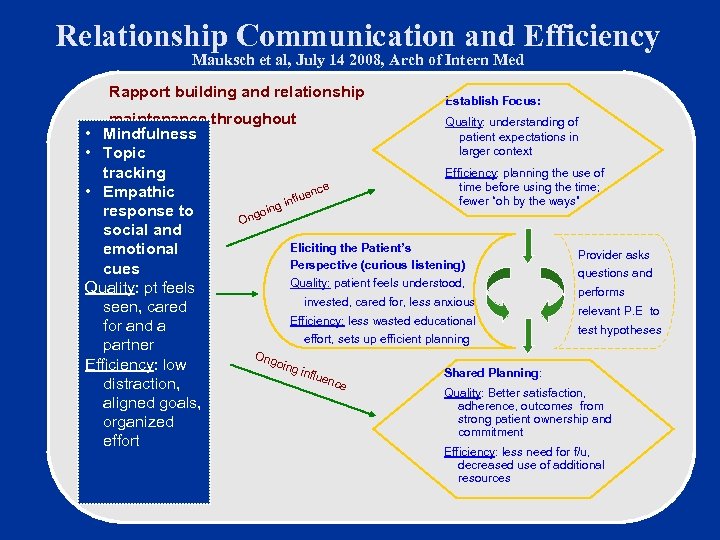 Relationship Communication and Efficiency Mauksch et al, July 14 2008, Arch of Intern Med Rapport building and relationship Establish Focus: maintenance throughout Quality: understanding of • Mindfulness patient expectations in larger context • Topic Efficiency: planning the use of tracking time before using the time; e nc • Empathic flue fewer “oh by the ways” g in response to goin On social and Eliciting the Patient’s emotional Provider asks Perspective (curious listening) cues questions and Quality: patient feels understood, Quality: pt feels performs invested, cared for, less anxious seen, cared relevant P. E to Efficiency: less wasted educational for and a test hypotheses effort, sets up efficient planning partner Ong oing Efficiency: low influ Shared Planning: enc e distraction, Quality: Better satisfaction, aligned goals, adherence, outcomes from strong patient ownership and organized commitment effort Efficiency: less need for f/u, decreased use of additional resources
Relationship Communication and Efficiency Mauksch et al, July 14 2008, Arch of Intern Med Rapport building and relationship Establish Focus: maintenance throughout Quality: understanding of • Mindfulness patient expectations in larger context • Topic Efficiency: planning the use of tracking time before using the time; e nc • Empathic flue fewer “oh by the ways” g in response to goin On social and Eliciting the Patient’s emotional Provider asks Perspective (curious listening) cues questions and Quality: patient feels understood, Quality: pt feels performs invested, cared for, less anxious seen, cared relevant P. E to Efficiency: less wasted educational for and a test hypotheses effort, sets up efficient planning partner Ong oing Efficiency: low influ Shared Planning: enc e distraction, Quality: Better satisfaction, aligned goals, adherence, outcomes from strong patient ownership and organized commitment effort Efficiency: less need for f/u, decreased use of additional resources
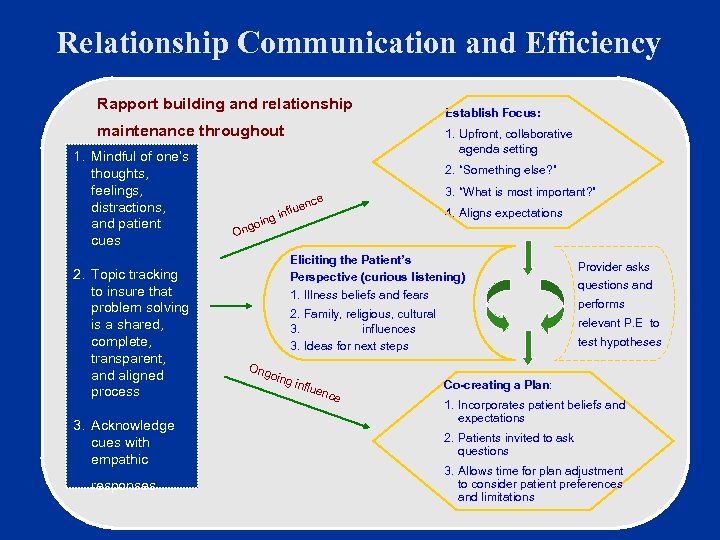 Relationship Communication and Efficiency Rapport building and relationship maintenance throughout 1. Mindful of one’s thoughts, feelings, distractions, and patient cues 2. Topic tracking to insure that problem solving is a shared, complete, transparent, and aligned process 3. Acknowledge cues with empathic responses Establish Focus: 1. Upfront, collaborative agenda setting 2. “Something else? ” g goin 3. “What is most important? ” ce luen inf 4. Aligns expectations On Eliciting the Patient’s Perspective (curious listening) 1. Illness beliefs and fears 2. Family, religious, cultural 3. influences 3. Ideas for next steps Ong oing influ enc e Provider asks questions and performs relevant P. E to test hypotheses Co-creating a Plan: 1. Incorporates patient beliefs and expectations 2. Patients invited to ask questions 3. Allows time for plan adjustment to consider patient preferences and limitations
Relationship Communication and Efficiency Rapport building and relationship maintenance throughout 1. Mindful of one’s thoughts, feelings, distractions, and patient cues 2. Topic tracking to insure that problem solving is a shared, complete, transparent, and aligned process 3. Acknowledge cues with empathic responses Establish Focus: 1. Upfront, collaborative agenda setting 2. “Something else? ” g goin 3. “What is most important? ” ce luen inf 4. Aligns expectations On Eliciting the Patient’s Perspective (curious listening) 1. Illness beliefs and fears 2. Family, religious, cultural 3. influences 3. Ideas for next steps Ong oing influ enc e Provider asks questions and performs relevant P. E to test hypotheses Co-creating a Plan: 1. Incorporates patient beliefs and expectations 2. Patients invited to ask questions 3. Allows time for plan adjustment to consider patient preferences and limitations
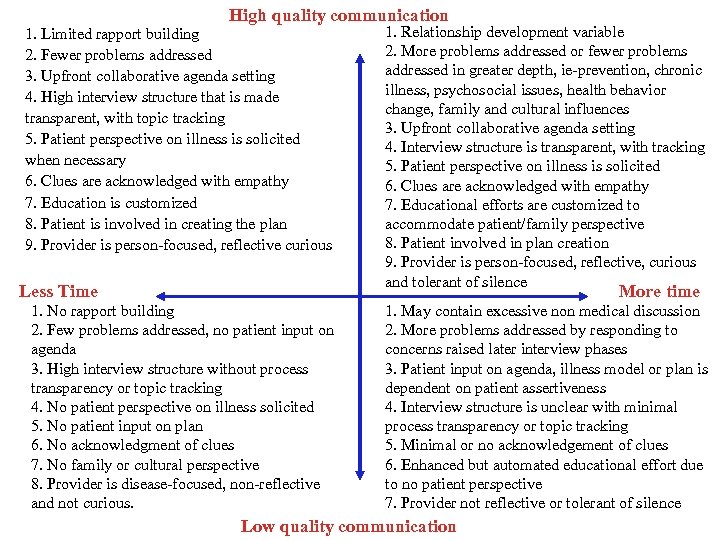 High quality communication 1. Limited rapport building 2. Fewer problems addressed 3. Upfront collaborative agenda setting 4. High interview structure that is made transparent, with topic tracking 5. Patient perspective on illness is solicited when necessary 6. Clues are acknowledged with empathy 7. Education is customized 8. Patient is involved in creating the plan 9. Provider is person-focused, reflective curious Less Time 1. Relationship development variable 2. More problems addressed or fewer problems addressed in greater depth, ie-prevention, chronic illness, psychosocial issues, health behavior change, family and cultural influences 3. Upfront collaborative agenda setting 4. Interview structure is transparent, with tracking 5. Patient perspective on illness is solicited 6. Clues are acknowledged with empathy 7. Educational efforts are customized to accommodate patient/family perspective 8. Patient involved in plan creation 9. Provider is person-focused, reflective, curious and tolerant of silence More time 1. No rapport building 2. Few problems addressed, no patient input on agenda 3. High interview structure without process transparency or topic tracking 4. No patient perspective on illness solicited 5. No patient input on plan 6. No acknowledgment of clues 7. No family or cultural perspective 8. Provider is disease-focused, non-reflective and not curious. 1. May contain excessive non medical discussion 2. More problems addressed by responding to concerns raised later interview phases 3. Patient input on agenda, illness model or plan is dependent on patient assertiveness 4. Interview structure is unclear with minimal process transparency or topic tracking 5. Minimal or no acknowledgement of clues 6. Enhanced but automated educational effort due to no patient perspective 7. Provider not reflective or tolerant of silence Low quality communication
High quality communication 1. Limited rapport building 2. Fewer problems addressed 3. Upfront collaborative agenda setting 4. High interview structure that is made transparent, with topic tracking 5. Patient perspective on illness is solicited when necessary 6. Clues are acknowledged with empathy 7. Education is customized 8. Patient is involved in creating the plan 9. Provider is person-focused, reflective curious Less Time 1. Relationship development variable 2. More problems addressed or fewer problems addressed in greater depth, ie-prevention, chronic illness, psychosocial issues, health behavior change, family and cultural influences 3. Upfront collaborative agenda setting 4. Interview structure is transparent, with tracking 5. Patient perspective on illness is solicited 6. Clues are acknowledged with empathy 7. Educational efforts are customized to accommodate patient/family perspective 8. Patient involved in plan creation 9. Provider is person-focused, reflective, curious and tolerant of silence More time 1. No rapport building 2. Few problems addressed, no patient input on agenda 3. High interview structure without process transparency or topic tracking 4. No patient perspective on illness solicited 5. No patient input on plan 6. No acknowledgment of clues 7. No family or cultural perspective 8. Provider is disease-focused, non-reflective and not curious. 1. May contain excessive non medical discussion 2. More problems addressed by responding to concerns raised later interview phases 3. Patient input on agenda, illness model or plan is dependent on patient assertiveness 4. Interview structure is unclear with minimal process transparency or topic tracking 5. Minimal or no acknowledgement of clues 6. Enhanced but automated educational effort due to no patient perspective 7. Provider not reflective or tolerant of silence Low quality communication
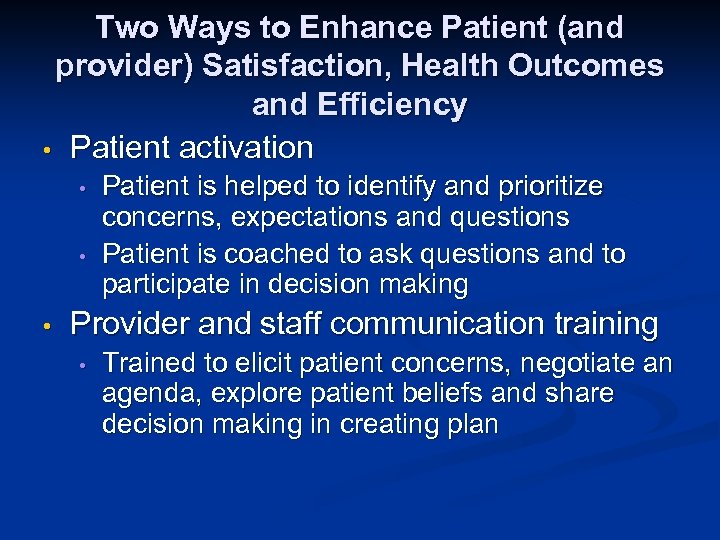 Two Ways to Enhance Patient (and provider) Satisfaction, Health Outcomes and Efficiency • Patient activation • • • Patient is helped to identify and prioritize concerns, expectations and questions Patient is coached to ask questions and to participate in decision making Provider and staff communication training • Trained to elicit patient concerns, negotiate an agenda, explore patient beliefs and share decision making in creating plan
Two Ways to Enhance Patient (and provider) Satisfaction, Health Outcomes and Efficiency • Patient activation • • • Patient is helped to identify and prioritize concerns, expectations and questions Patient is coached to ask questions and to participate in decision making Provider and staff communication training • Trained to elicit patient concerns, negotiate an agenda, explore patient beliefs and share decision making in creating plan
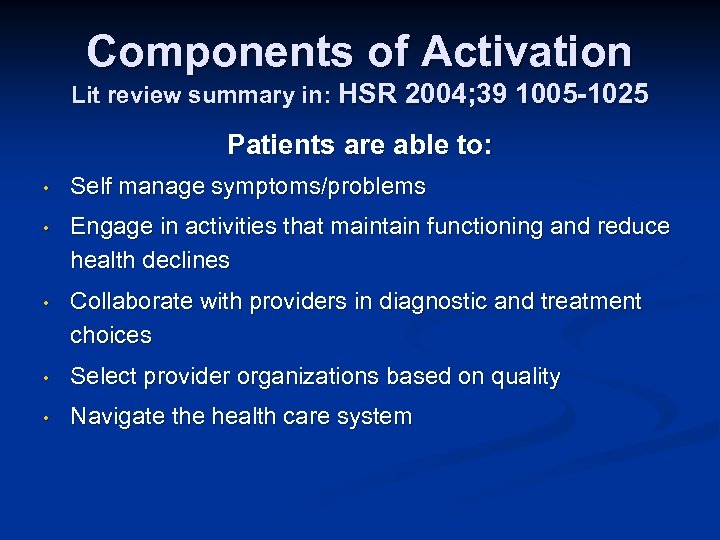 Components of Activation Lit review summary in: HSR 2004; 39 1005 -1025 Patients are able to: • Self manage symptoms/problems • Engage in activities that maintain functioning and reduce health declines • Collaborate with providers in diagnostic and treatment choices • Select provider organizations based on quality • Navigate the health care system
Components of Activation Lit review summary in: HSR 2004; 39 1005 -1025 Patients are able to: • Self manage symptoms/problems • Engage in activities that maintain functioning and reduce health declines • Collaborate with providers in diagnostic and treatment choices • Select provider organizations based on quality • Navigate the health care system
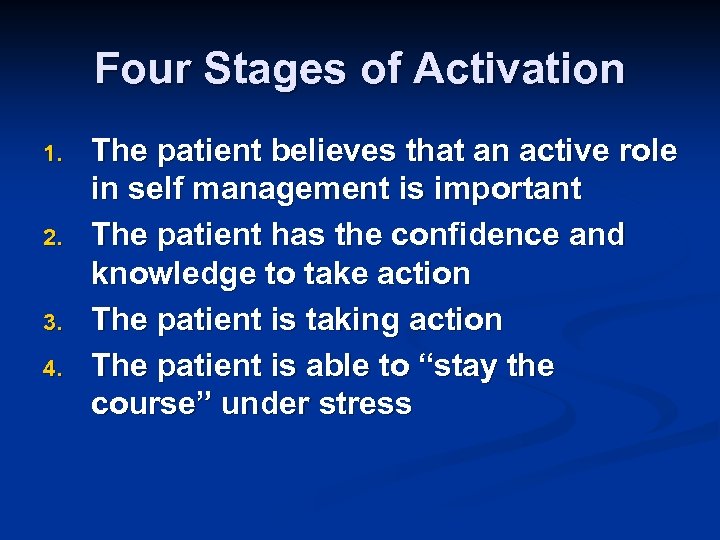 Four Stages of Activation 1. 2. 3. 4. The patient believes that an active role in self management is important The patient has the confidence and knowledge to take action The patient is taking action The patient is able to “stay the course” under stress
Four Stages of Activation 1. 2. 3. 4. The patient believes that an active role in self management is important The patient has the confidence and knowledge to take action The patient is taking action The patient is able to “stay the course” under stress
 Front Desk Statement • “ Please take a few moments and fill out this form. It helps us know what is most important to address for you today. ”
Front Desk Statement • “ Please take a few moments and fill out this form. It helps us know what is most important to address for you today. ”
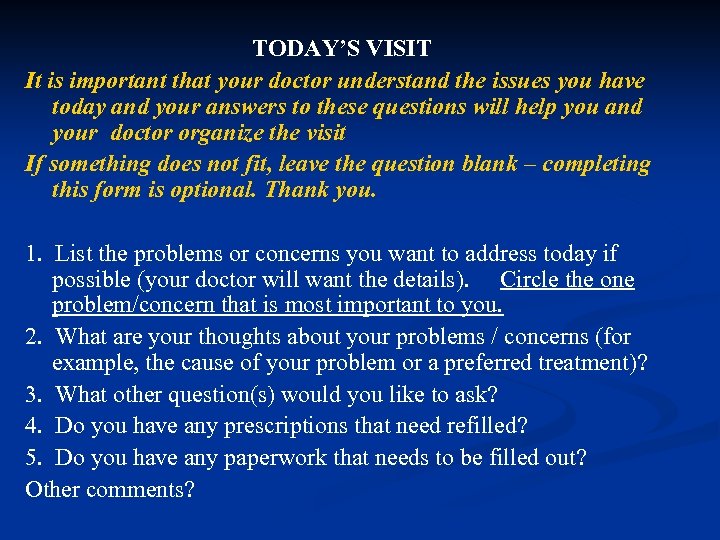 TODAY’S VISIT It is important that your doctor understand the issues you have today and your answers to these questions will help you and your doctor organize the visit If something does not fit, leave the question blank – completing this form is optional. Thank you. 1. List the problems or concerns you want to address today if possible (your doctor will want the details). Circle the one problem/concern that is most important to you. 2. What are your thoughts about your problems / concerns (for example, the cause of your problem or a preferred treatment)? 3. What other question(s) would you like to ask? 4. Do you have any prescriptions that need refilled? 5. Do you have any paperwork that needs to be filled out? Other comments?
TODAY’S VISIT It is important that your doctor understand the issues you have today and your answers to these questions will help you and your doctor organize the visit If something does not fit, leave the question blank – completing this form is optional. Thank you. 1. List the problems or concerns you want to address today if possible (your doctor will want the details). Circle the one problem/concern that is most important to you. 2. What are your thoughts about your problems / concerns (for example, the cause of your problem or a preferred treatment)? 3. What other question(s) would you like to ask? 4. Do you have any prescriptions that need refilled? 5. Do you have any paperwork that needs to be filled out? Other comments?
 The MA/LPN and the Front-Side of Outpatient Care
The MA/LPN and the Front-Side of Outpatient Care
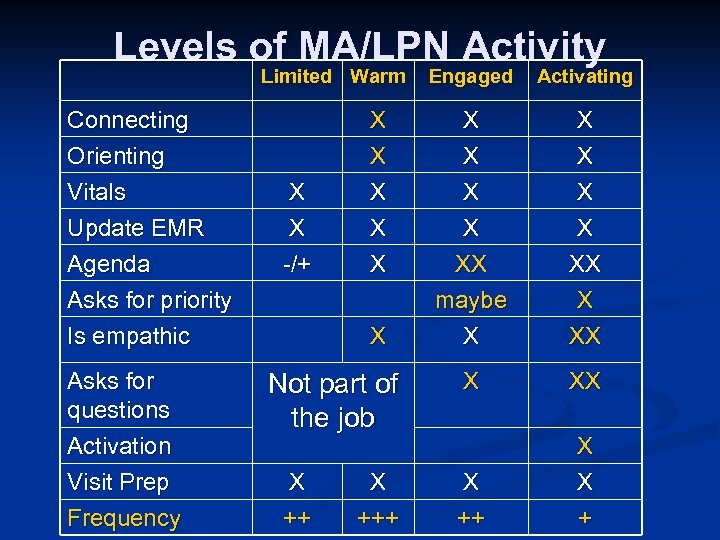 Levels of MA/LPN Activity Limited Warm Connecting Orienting Vitals Update EMR Agenda Asks for priority Is empathic Asks for questions Activation Visit Prep Frequency Activating X X X XX maybe X XX X X -/+ Engaged X XX X ++ X X + Not part of the job X +++
Levels of MA/LPN Activity Limited Warm Connecting Orienting Vitals Update EMR Agenda Asks for priority Is empathic Asks for questions Activation Visit Prep Frequency Activating X X X XX maybe X XX X X -/+ Engaged X XX X ++ X X + Not part of the job X +++
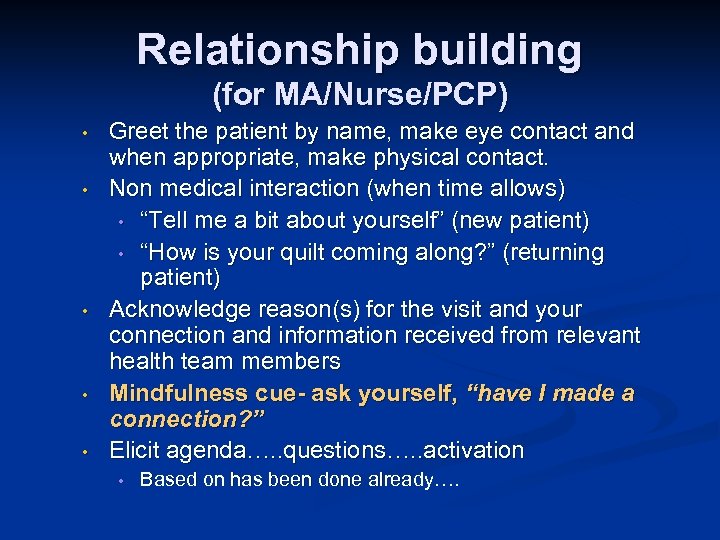 Relationship building (for MA/Nurse/PCP) • • • Greet the patient by name, make eye contact and when appropriate, make physical contact. Non medical interaction (when time allows) • “Tell me a bit about yourself” (new patient) • “How is your quilt coming along? ” (returning patient) Acknowledge reason(s) for the visit and your connection and information received from relevant health team members Mindfulness cue- ask yourself, “have I made a connection? ” Elicit agenda…. . questions…. . activation • Based on has been done already….
Relationship building (for MA/Nurse/PCP) • • • Greet the patient by name, make eye contact and when appropriate, make physical contact. Non medical interaction (when time allows) • “Tell me a bit about yourself” (new patient) • “How is your quilt coming along? ” (returning patient) Acknowledge reason(s) for the visit and your connection and information received from relevant health team members Mindfulness cue- ask yourself, “have I made a connection? ” Elicit agenda…. . questions…. . activation • Based on has been done already….
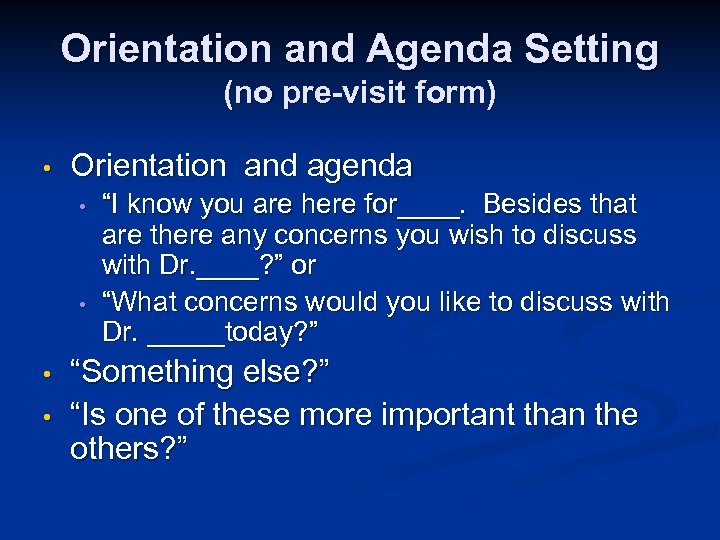 Orientation and Agenda Setting (no pre-visit form) • Orientation and agenda • • “I know you are here for____. Besides that are there any concerns you wish to discuss with Dr. ____? ” or “What concerns would you like to discuss with Dr. _____today? ” “Something else? ” “Is one of these more important than the others? ”
Orientation and Agenda Setting (no pre-visit form) • Orientation and agenda • • “I know you are here for____. Besides that are there any concerns you wish to discuss with Dr. ____? ” or “What concerns would you like to discuss with Dr. _____today? ” “Something else? ” “Is one of these more important than the others? ”
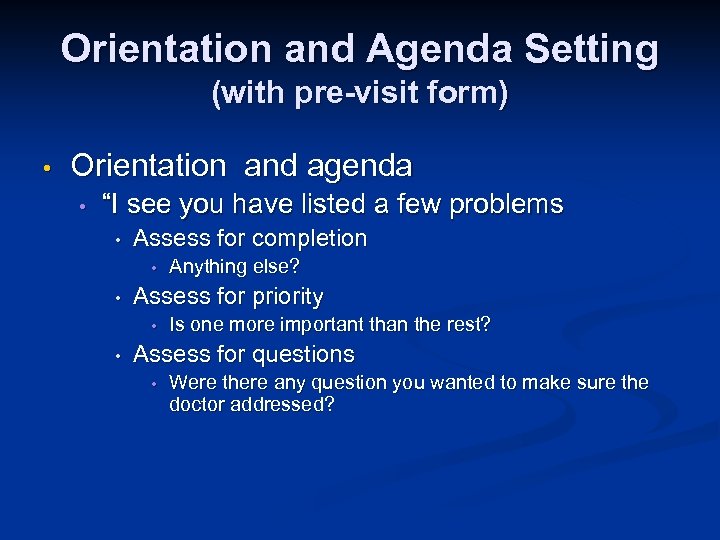 Orientation and Agenda Setting (with pre-visit form) • Orientation and agenda • “I see you have listed a few problems • Assess for completion • • Assess for priority • • Anything else? Is one more important than the rest? Assess for questions • Were there any question you wanted to make sure the doctor addressed?
Orientation and Agenda Setting (with pre-visit form) • Orientation and agenda • “I see you have listed a few problems • Assess for completion • • Assess for priority • • Anything else? Is one more important than the rest? Assess for questions • Were there any question you wanted to make sure the doctor addressed?
 Patient Activation “Your questions (or ideas) are important. Make sure you bring those up with Dr. Goodwill.
Patient Activation “Your questions (or ideas) are important. Make sure you bring those up with Dr. Goodwill.
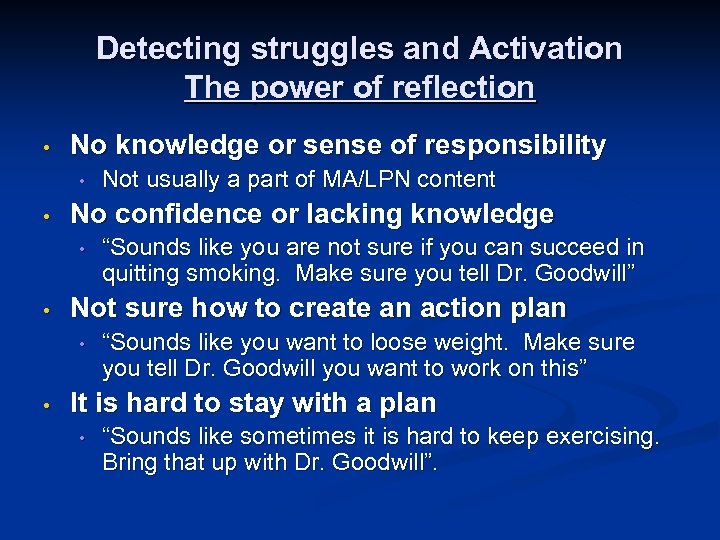 Detecting struggles and Activation The power of reflection • No knowledge or sense of responsibility • • No confidence or lacking knowledge • • “Sounds like you are not sure if you can succeed in quitting smoking. Make sure you tell Dr. Goodwill” Not sure how to create an action plan • • Not usually a part of MA/LPN content “Sounds like you want to loose weight. Make sure you tell Dr. Goodwill you want to work on this” It is hard to stay with a plan • “Sounds like sometimes it is hard to keep exercising. Bring that up with Dr. Goodwill”.
Detecting struggles and Activation The power of reflection • No knowledge or sense of responsibility • • No confidence or lacking knowledge • • “Sounds like you are not sure if you can succeed in quitting smoking. Make sure you tell Dr. Goodwill” Not sure how to create an action plan • • Not usually a part of MA/LPN content “Sounds like you want to loose weight. Make sure you tell Dr. Goodwill you want to work on this” It is hard to stay with a plan • “Sounds like sometimes it is hard to keep exercising. Bring that up with Dr. Goodwill”.
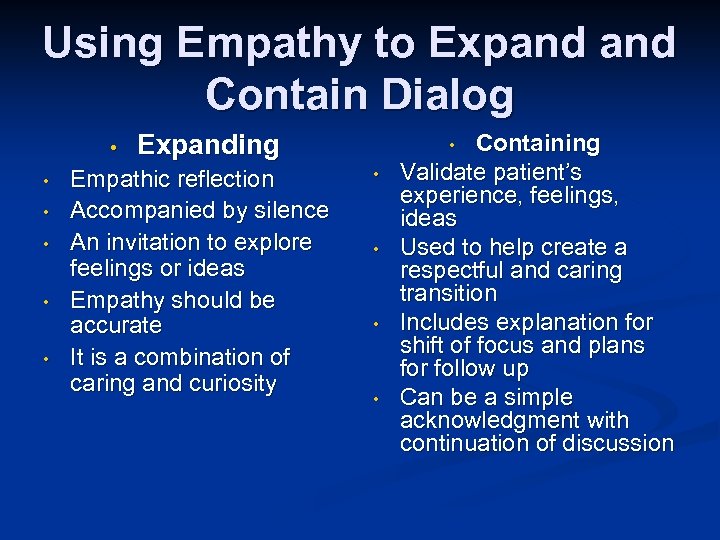 Using Empathy to Expand Contain Dialog • • • Expanding Empathic reflection Accompanied by silence An invitation to explore feelings or ideas Empathy should be accurate It is a combination of caring and curiosity Containing Validate patient’s experience, feelings, ideas Used to help create a respectful and caring transition Includes explanation for shift of focus and plans for follow up Can be a simple acknowledgment with continuation of discussion • • •
Using Empathy to Expand Contain Dialog • • • Expanding Empathic reflection Accompanied by silence An invitation to explore feelings or ideas Empathy should be accurate It is a combination of caring and curiosity Containing Validate patient’s experience, feelings, ideas Used to help create a respectful and caring transition Includes explanation for shift of focus and plans for follow up Can be a simple acknowledgment with continuation of discussion • • •
 The MD/ARNP/PA and the Front-Side of Outpatient Care
The MD/ARNP/PA and the Front-Side of Outpatient Care
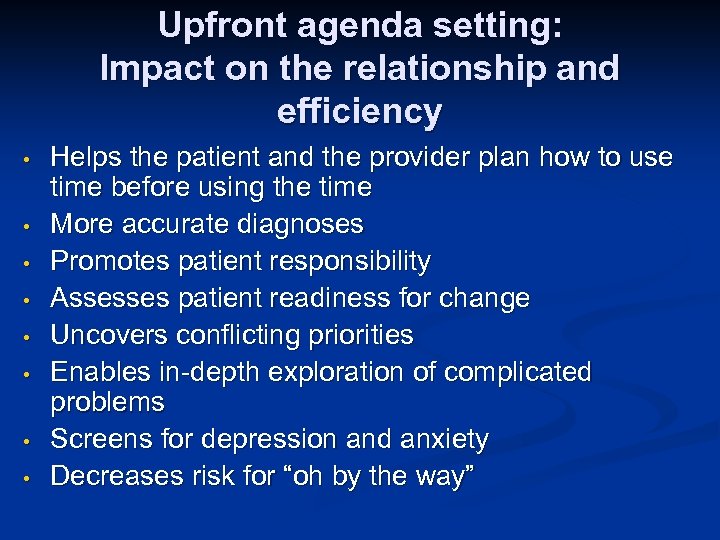 Upfront agenda setting: Impact on the relationship and efficiency • • Helps the patient and the provider plan how to use time before using the time More accurate diagnoses Promotes patient responsibility Assesses patient readiness for change Uncovers conflicting priorities Enables in-depth exploration of complicated problems Screens for depression and anxiety Decreases risk for “oh by the way”
Upfront agenda setting: Impact on the relationship and efficiency • • Helps the patient and the provider plan how to use time before using the time More accurate diagnoses Promotes patient responsibility Assesses patient readiness for change Uncovers conflicting priorities Enables in-depth exploration of complicated problems Screens for depression and anxiety Decreases risk for “oh by the way”
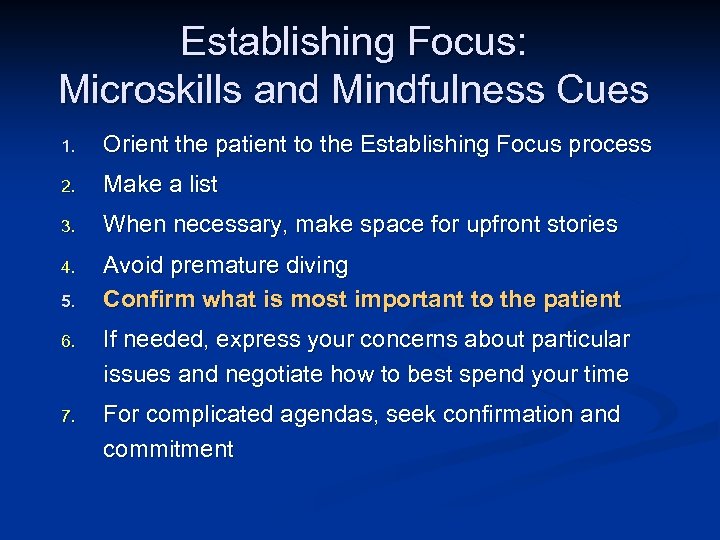 Establishing Focus: Microskills and Mindfulness Cues 1. Orient the patient to the Establishing Focus process 2. Make a list 3. When necessary, make space for upfront stories 4. Avoid premature diving Confirm what is most important to the patient 5. 6. If needed, express your concerns about particular issues and negotiate how to best spend your time 7. For complicated agendas, seek confirmation and commitment
Establishing Focus: Microskills and Mindfulness Cues 1. Orient the patient to the Establishing Focus process 2. Make a list 3. When necessary, make space for upfront stories 4. Avoid premature diving Confirm what is most important to the patient 5. 6. If needed, express your concerns about particular issues and negotiate how to best spend your time 7. For complicated agendas, seek confirmation and commitment
 If a previst form is filled out • Confirm priority out loud • • Always ask, “Is there something else? ” • • “So your headaches are your main concern” “Are there any other concerns? ” Negotiate priorities if: • • There are too many issues A topic you want to address is not on the patient’s list
If a previst form is filled out • Confirm priority out loud • • Always ask, “Is there something else? ” • • “So your headaches are your main concern” “Are there any other concerns? ” Negotiate priorities if: • • There are too many issues A topic you want to address is not on the patient’s list
 Teams need time to grow • Longer meetings to: • • • Share experiences Share vision Problem solve Celebrate Pass information (should not dominate the agenda) Huddles • • Problem solve Support Anticipate Celebrate
Teams need time to grow • Longer meetings to: • • • Share experiences Share vision Problem solve Celebrate Pass information (should not dominate the agenda) Huddles • • Problem solve Support Anticipate Celebrate
 Team Development Strategy • Find time to observe one another • • • MA/Nurses observe on another and PCPs observe one another MA/Nurses and PCP observe one another Note: • • • Ideas for clinical improvement Ways to be more efficient without compromising quality Questions
Team Development Strategy • Find time to observe one another • • • MA/Nurses observe on another and PCPs observe one another MA/Nurses and PCP observe one another Note: • • • Ideas for clinical improvement Ways to be more efficient without compromising quality Questions
 Team Discussion Questions • • • n Do we want to use an agenda setting form? Who will develop and test the form? When will it be handed out and by whom? What should be communicated between MA/Nurse and MD/PA/ARNP at every visit? How? What are the back up plans? Extra Credit: what do we want to confirm with the patient before the patient leaves the office? n Hint: think about system navigation, behavior change, follow-up.
Team Discussion Questions • • • n Do we want to use an agenda setting form? Who will develop and test the form? When will it be handed out and by whom? What should be communicated between MA/Nurse and MD/PA/ARNP at every visit? How? What are the back up plans? Extra Credit: what do we want to confirm with the patient before the patient leaves the office? n Hint: think about system navigation, behavior change, follow-up.
 PCP Online Training 30 -35 minutes n Teaches core communication, relationship and efficiency skills n Teaches form use n https: //catalysttools. washington. edu/webq/ survey/mauksch/57898 n
PCP Online Training 30 -35 minutes n Teaches core communication, relationship and efficiency skills n Teaches form use n https: //catalysttools. washington. edu/webq/ survey/mauksch/57898 n
 References: Communication, Efficiency, Teamwork, Medical Home • Mauksch, L. , Dugdale, D. , Dodson, S. , Epstein, R. Relationship, Communication and Efficiency: Creating a clinical model from a literature review. Archives of Internal Medicine, 2008, 168, 1387 -1395. • Bodenheimer, T. , Laing, B. The teamlet model. Annals of Family Medicine, 2007, 5, 457 -461. • Epstein, R. , Mauksch, L. , Carroll, J. , Jaen, C. Have you really addressed your patient’s concerns? Family Practice Mgmt, 2008, March, 35 -40. • Crabtree, BF. , Mc. Daniel, R. , Nutting, P. , et al. Closing the physician-staff divide: A step toward creating the medical home. 2008 Family Practice Management, April, 20 -24. • Fiscella K, Epstein RM. So much to do, so little time: care for the socially disadvantaged and the 15 -minute visit. Arch Intern Med. Sep 22 2008; 168(17): 1843 -1852. • Mauksch, L. , Reitz, R. , Tucker, S. , Hurd, S. , Russo, J. , Katon, W. Improving Quality of Care for Mental Illness in an Uninsured, Low Income Primary Care Population, General Hospital Psychiatry, 2007, 29, 302 -309
References: Communication, Efficiency, Teamwork, Medical Home • Mauksch, L. , Dugdale, D. , Dodson, S. , Epstein, R. Relationship, Communication and Efficiency: Creating a clinical model from a literature review. Archives of Internal Medicine, 2008, 168, 1387 -1395. • Bodenheimer, T. , Laing, B. The teamlet model. Annals of Family Medicine, 2007, 5, 457 -461. • Epstein, R. , Mauksch, L. , Carroll, J. , Jaen, C. Have you really addressed your patient’s concerns? Family Practice Mgmt, 2008, March, 35 -40. • Crabtree, BF. , Mc. Daniel, R. , Nutting, P. , et al. Closing the physician-staff divide: A step toward creating the medical home. 2008 Family Practice Management, April, 20 -24. • Fiscella K, Epstein RM. So much to do, so little time: care for the socially disadvantaged and the 15 -minute visit. Arch Intern Med. Sep 22 2008; 168(17): 1843 -1852. • Mauksch, L. , Reitz, R. , Tucker, S. , Hurd, S. , Russo, J. , Katon, W. Improving Quality of Care for Mental Illness in an Uninsured, Low Income Primary Care Population, General Hospital Psychiatry, 2007, 29, 302 -309


