bac64e241afaee639fe96c144152bf2e.ppt
- Количество слайдов: 28
“REHABBING” AMPUTEES: Caught between AROC and a hard place? Craig Evans Physiotherapist Rankin Park Limb Centre
Is anyone else finding it harder? • Are patients : – More unwell? – More comorbities? – Older? – Less motivated? – Lower socioeconomic groups? – More challenging accommodation? MORE COMPLEX?
DATA? …. AROC!
Data Collection • The AROC data collection compares our Data with similar units and national data • The CORE report should be considered in conjunction with relevant Impairment Specific reports and the Target Outcomes report for your facility • The AROC database is only as good as the quality and completeness of the data that are submitted to it.
Results summarised Admission: 1. RPC has increased complexity of patients 2. Increased comorbidities 3. Increased patients with carer and support 4. Decreased admission FIM’s Inpatient: 1. Increased LOS ( Due to external service issues ) 2. Decreased complications ( RPC good nursing care ) Discharge: 1. Lower FIM scores 2. Increased FIM change 3. Increased services at home but increased discharge to home
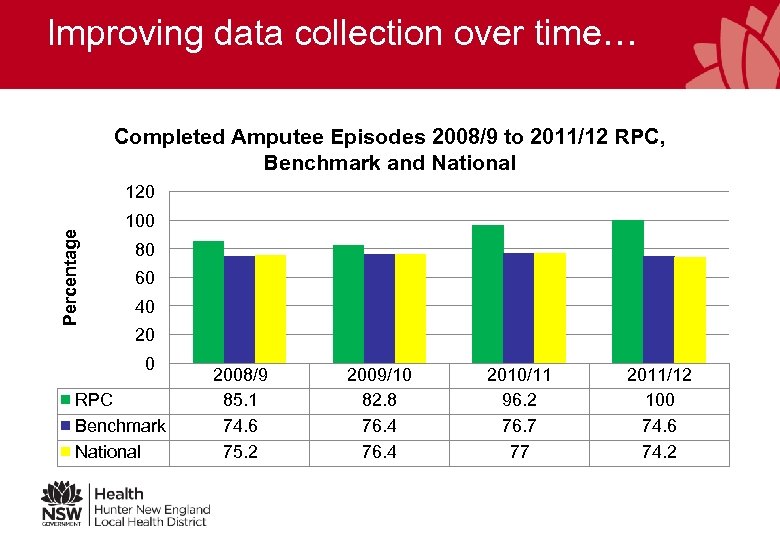
Improving data collection over time… Completed Amputee Episodes 2008/9 to 2011/12 RPC, Benchmark and National Percentage 120 100 80 60 40 20 0 RPC Benchmark National 2008/9 85. 1 74. 6 75. 2 2009/10 82. 8 76. 4 2010/11 96. 2 76. 7 77 2011/12 100 74. 6 74. 2
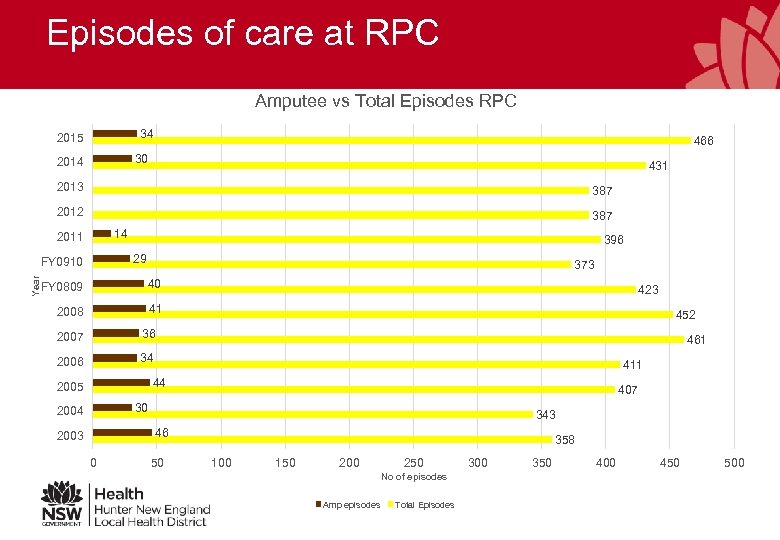
Episodes of care at RPC Amputee vs Total Episodes RPC 34 2015 466 30 2014 431 2013 387 2012 387 14 2011 29 FY 0910 Year 396 373 FY 0809 40 2008 41 2007 452 36 2006 423 34 461 411 44 2005 407 30 2004 343 46 2003 0 50 358 100 150 200 250 No of episodes Amp episodes Total Episodes 300 350 400 450 500

FIM change over 10 + years FIM Change versus time 25 FIM change 20 15 10 5 0 RPC amps FIM Change RPC all FIM Change Benchmark FIM Change National 2003 13. 7 19. 2 12. 9 2004 12. 1 18. 3 10. 7 2005 12. 8 18. 4 11. 6 2006 20. 2 12 2007 16. 5 19. 6 12. 4 2008 14. 5 18. 4 12. 7 FY 0809 16. 9 19. 5 14. 6 Years FY 0910 15. 3 20. 1 16 15. 9 2011 13. 9 18. 1 15. 2 15. 4 2012 18 18. 7 15. 9 16. 1 2013 2014 2015 12 19. 4 16. 2

Average Age change over the years Age vs Treatment Year 80 70 60 Age 50 40 30 20 10 0 2003 2004 2005 2006 2007 2008 FY 0809 FY 0910 2011 Treatment Year RPC amps RPC all Benchmark 2012 2013 2014 2015

More FIM data… ADMISSION & DISCHARGE FIM : RPC VS BENCHMARK/NATIONAL 120 100 80 60 40 20 0 RPC FIM Adm RPC FIM D/C Bench FIM Adm Bench FIM D/C Nat FIM Adm Nat FIM D/c 2003 85. 7 99 89. 4 102. 4 2004 77 89. 1 90. 2 101. 1 2005 80. 6 93. 5 91. 4 102. 9 2006 81. 5 100. 6 90. 4 102. 6 2007 87 103. 4 90. 2 102. 9 2008 86. 5 101. 7 89. 1 102. 2 FY 0809 89. 9 106. 8 91. 8 106. 4 FY 0910 95. 9 109. 3 89. 5 105. 4 2011 93. 2 107. 1 90. 8 106 2012 2013 2014 2015 97. 2 109. 3 88. 5 104. 7

Overall admissions Mean AROC RPC LOS Amputee Trends Compared to Benchmarks and National 2006/7 to 2011/12 50 45 40 35 30 25 20 15 10 5 0 2006/7 RPC 38. 9 Bench. Mark 31. 1 National 30. 9 2007/8 33. 6 32. 3 31. 4 2008/9 44 35. 6 34. 6 2009/10 2010/11 2011/12 37. 6 25 30. 8 40. 3 36. 7 36. 1 38. 7 35. 4 34. 5

Comorbidities… Comorbidity Amputee Trends 2006/7 - 2011/12 60 Percentage 50 40 30 20 10 0 AMP Comorbidities 0 (%) AMP Comorbidities 1 (%) AMP Comorbidities 2 (%) AMP Comorbidities 3 (%) AMP Comobidities 4 (%) 2006/7 2007/8 2008/9 2009/10 2010/11 2011/12 32. 3 5. 5 0 0 11. 5 0. 49 49. 2 40. 6 37. 1 22. 4 27. 3 26. 9 14. 7 33. 3 25. 5 44 34. 6 0. 98 17. 8 21. 2 21. 3 27. 2 25. 3 23 26. 4 25 42. 5 34. 4 23 1. 7 15. 6 17. 5 18 20. 2 20. 5 20. 3 23. 5 27. 7 25. 5 17. 2 26. 9 0. 73 8. 7 11. 4 13. 6 15. 1 13. 6 15. 4 2. 9 8. 3 6. 3 11. 1 3. 8 0. 25 8. 4 9 9. 8 14. 8 13. 1 14. 2

So why are our patients “less rehabbable”?

So why are our patients “less rehabbable”? • • More complex patients - definitely Better pre-amputation interventions Reduced “Life reserve” Economics: Public vs private – Private insurance – socioeconomics issue reduced – “Rural” – lower SE groups – Motivation?

Better Interventions & “Life Reserve” Life span Birth to death Living with comorbidity “Life Reserve” E. G diabetes. Requiring medical management of a condition. The time frame from hospitalization due to comorbidity including rehab til mortality

Better Interventions & “Life Reserve” Life span Birth to death Living with comorbidity “Life Reserve” Improvements in interventions increase the time frame of relative wellness prior to requirement for rehab Less life reserve due to age and “managed” comorbidities. By the time they reach here their potential for rehab is reduced.

What makes a good rehab candidate?

What makes a good rehab candidate? • Motivation • Potential – physical, cognitive • Support “House, nous and spouse”

What then should be our expectations? • • How good should our patients get? Walking ADLs Home Predictors of outcome?

Predictors of function: Taylor et al 2005 • Pre-op factors ? = post-op function / mortality • With view to performing palliative AKA vs functional BKA • >= 70 y. o – 3 x or more chance of death, nonambulatory, non-prosthetic user, functionally dependent within 1 year • Other pre op predictive factors – nonambulatory / transfers only; dementia; coronary artery disease; ESRD

Predictors of function : Schoppen et al (2003) Best predictors: – Age at amputation important for general functioning. – Standing balance on the unaffected limb at 2 weeks post amputation – significant predictor of all functional outcome parameters – Memory +/- mood/cognitive ability – Comorbidity (DM and other but not cardiopulmonary disease) – No social predictors were significant

Predictors of function: Gailey et al, 2002 • AMPPRO / AMPno. PRO (Gailey et al, 2002) – more a functional test than a predictor.

Predictors of function : Whyte And Carroll (2004) • Patients with phantom pain (questionnaire, 62% response rate, 315 subjects) Catastrophizing can account for 11% overall level of disability

Predictors of prosthetic non-use: Roffman et al (2014)

What does all this mean for us? • Patients are getting more complex, not necessarily older. • There are predictors of function to use as a guide. (Need to be more objective? ABF) • “Rehabbing” the pre-amputees – vascular rehab?

References: • • • AROC Reports --- John Hunter Hospital (Rankin Park Unit) 2003 -2015 Gailey RS, Roach KE, Applegate EB, Cho B, Cunniffe B, Licht S, Maguire M, Nash MS. (2002). “The Amputee Mobility Predictor: an instrument to assess determinants of the lower-limb amputee ability to ambulate. ” Arch Phys Med Rehabil 2002; 83: 613 -27. Schoppen T, Boonstra A, Groothoff JW, de Vries J, Go¨eken LN, Eisma WH. (2003) “Physical, mental, and social predictors of functional outcome in unilateral lower-limb amputees. ” Arch Phys Med Rehabil 2003; 84: 803 -11. Whyte and Carroll (2004). “The relationship between catastrophizing and disability in amputees experiencing phantom pain. ” Disability & Rehabilitation 26(11): 649 -54. Taylor SM et al (2005). “Pre-operative clinical factors predict post-operative functional outcomes after major lower limb amputation: An analysis of 553 consecutive patients” Journal of Vascular Surgery 2005; 42: 227 -235 Roffman CE, Buchanan J, Allison GT (2014) “Predictors of non-use of prostheses by people with lower limb amputation after discharge from rehabilitation: development and validation of clinical prediction rules. ” Journal of Physiotherapy 60: 224– 231

Acknowledgements • CNC/CNS at RPC – Merridie Rees, Helen Baines and Judith Dunne • Tara and Jackie from AROC
bac64e241afaee639fe96c144152bf2e.ppt