e5ec78b627ee0f07f9f5f5d2d5aca9a1.ppt
- Количество слайдов: 119
 Region X SOP Review Changes and Rationales ECRN CE Mod IV 2011 Condell Medical Center EMS System WATCH FOR INFORMATION ON CRITICAL MEDICATION SHORTAGES Objectives and preparation by Sharon Hopkins, RN, BSN, EMT-P Revised 2. 1. 12 1
Region X SOP Review Changes and Rationales ECRN CE Mod IV 2011 Condell Medical Center EMS System WATCH FOR INFORMATION ON CRITICAL MEDICATION SHORTAGES Objectives and preparation by Sharon Hopkins, RN, BSN, EMT-P Revised 2. 1. 12 1
 Objectives Upon successful completion of this module, the ECRN will be able to: v Discuss changes to the Region X SOP’s v Discuss changes in drug administration based on the 2010 AHA guideline changes v Acknowledge changes in oxygen administration v Review the SOP drugs v Acknowledge resources in the SOP’s for medication information 2
Objectives Upon successful completion of this module, the ECRN will be able to: v Discuss changes to the Region X SOP’s v Discuss changes in drug administration based on the 2010 AHA guideline changes v Acknowledge changes in oxygen administration v Review the SOP drugs v Acknowledge resources in the SOP’s for medication information 2
 Objectives v. Review the indications for EMS treatments v. Review contents in the skills section v. Review contents in the reference section v. Review case scenarios v. Successfully complete the quiz with a score of 80% or better 3
Objectives v. Review the indications for EMS treatments v. Review contents in the skills section v. Review contents in the reference section v. Review case scenarios v. Successfully complete the quiz with a score of 80% or better 3
 Critical Shortage Medications • Nation-wide issue • Will need to flexible in responding to alternatives • Critical shortage: LDiazepam (Valium) LEtomidate LFentanyl LOndansetron (Zofran)
Critical Shortage Medications • Nation-wide issue • Will need to flexible in responding to alternatives • Critical shortage: LDiazepam (Valium) LEtomidate LFentanyl LOndansetron (Zofran)
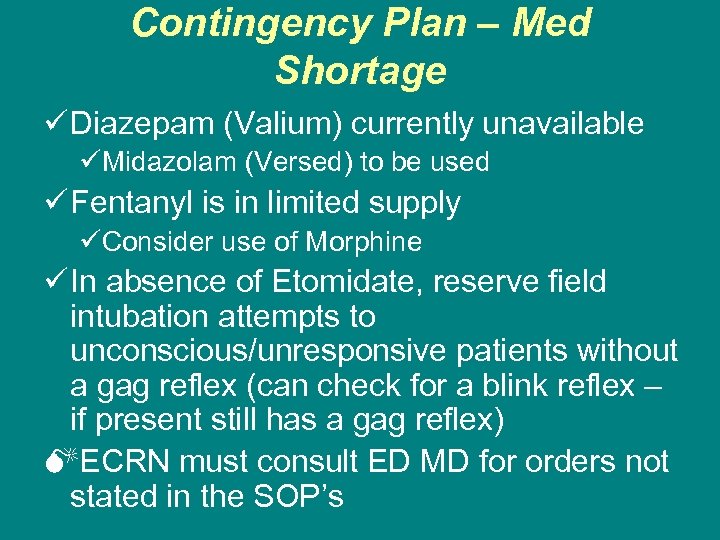 Contingency Plan – Med Shortage ü Diazepam (Valium) currently unavailable üMidazolam (Versed) to be used ü Fentanyl is in limited supply üConsider use of Morphine ü In absence of Etomidate, reserve field intubation attempts to unconscious/unresponsive patients without a gag reflex (can check for a blink reflex – if present still has a gag reflex) MECRN must consult ED MD for orders not stated in the SOP’s
Contingency Plan – Med Shortage ü Diazepam (Valium) currently unavailable üMidazolam (Versed) to be used ü Fentanyl is in limited supply üConsider use of Morphine ü In absence of Etomidate, reserve field intubation attempts to unconscious/unresponsive patients without a gag reflex (can check for a blink reflex – if present still has a gag reflex) MECRN must consult ED MD for orders not stated in the SOP’s
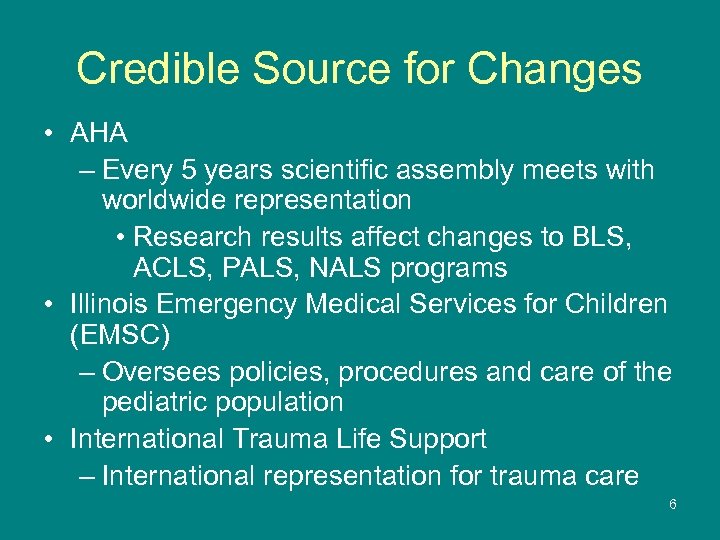 Credible Source for Changes • AHA – Every 5 years scientific assembly meets with worldwide representation • Research results affect changes to BLS, ACLS, PALS, NALS programs • Illinois Emergency Medical Services for Children (EMSC) – Oversees policies, procedures and care of the pediatric population • International Trauma Life Support – International representation for trauma care 6
Credible Source for Changes • AHA – Every 5 years scientific assembly meets with worldwide representation • Research results affect changes to BLS, ACLS, PALS, NALS programs • Illinois Emergency Medical Services for Children (EMSC) – Oversees policies, procedures and care of the pediatric population • International Trauma Life Support – International representation for trauma care 6
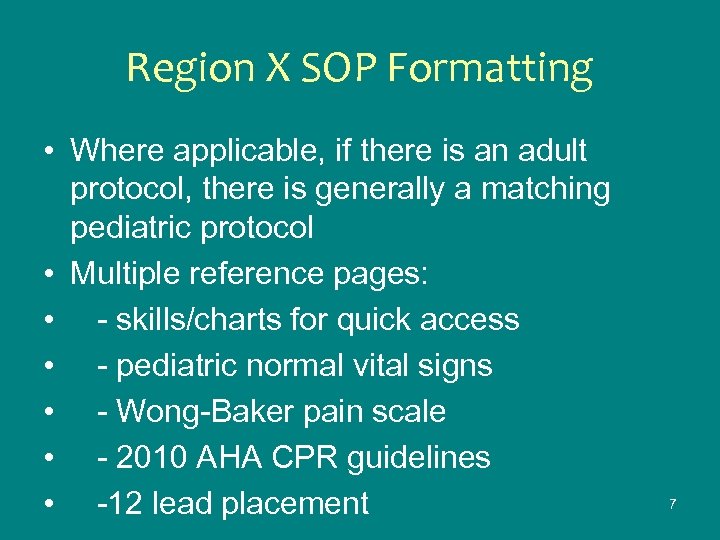 Region X SOP Formatting • Where applicable, if there is an adult protocol, there is generally a matching pediatric protocol • Multiple reference pages: • - skills/charts for quick access • - pediatric normal vital signs • - Wong-Baker pain scale • - 2010 AHA CPR guidelines • -12 lead placement 7
Region X SOP Formatting • Where applicable, if there is an adult protocol, there is generally a matching pediatric protocol • Multiple reference pages: • - skills/charts for quick access • - pediatric normal vital signs • - Wong-Baker pain scale • - 2010 AHA CPR guidelines • -12 lead placement 7
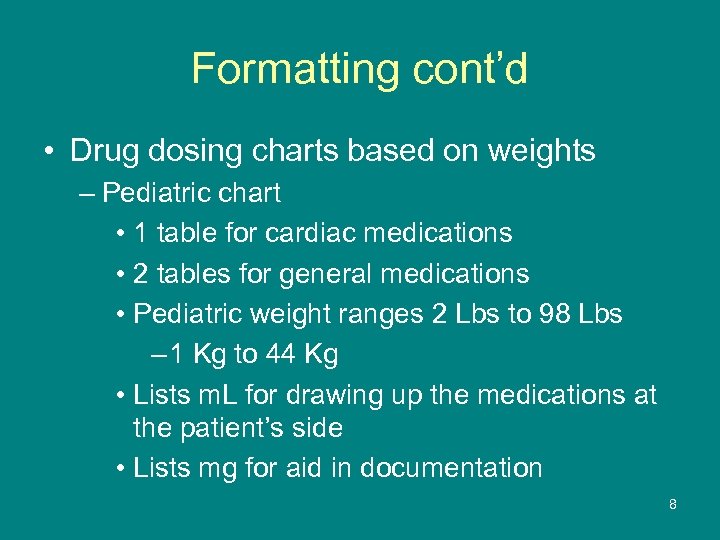 Formatting cont’d • Drug dosing charts based on weights – Pediatric chart • 1 table for cardiac medications • 2 tables for general medications • Pediatric weight ranges 2 Lbs to 98 Lbs – 1 Kg to 44 Kg • Lists m. L for drawing up the medications at the patient’s side • Lists mg for aid in documentation 8
Formatting cont’d • Drug dosing charts based on weights – Pediatric chart • 1 table for cardiac medications • 2 tables for general medications • Pediatric weight ranges 2 Lbs to 98 Lbs – 1 Kg to 44 Kg • Lists m. L for drawing up the medications at the patient’s side • Lists mg for aid in documentation 8
 Broselow Tape • Broselow tape available and used as a reference tool • Benefit – Guides in choosing equipment sizes • Limitations – Not all meds in ml which is information needed when at the beside – May not be as familiar with drug name used • Diazepam for Valium; Naloxone for Narcan; crystalloids for normal saline
Broselow Tape • Broselow tape available and used as a reference tool • Benefit – Guides in choosing equipment sizes • Limitations – Not all meds in ml which is information needed when at the beside – May not be as familiar with drug name used • Diazepam for Valium; Naloxone for Narcan; crystalloids for normal saline
 Formatting cont’d – Adult chart • Lists medications that must be given by weight – Etomidate – Fentanyl – Lidocaine for drug assisted intubation • Adult weight ranges 88 Lbs to 300 Lbs – 40 kg – to 136 Kg 10
Formatting cont’d – Adult chart • Lists medications that must be given by weight – Etomidate – Fentanyl – Lidocaine for drug assisted intubation • Adult weight ranges 88 Lbs to 300 Lbs – 40 kg – to 136 Kg 10
 Abbreviations for Documentation • Last 2 pages list out abbreviations, acronyms, symbols – Common and medically accepted list • Hospital and EMS resources • Watch use of abbreviations for misinterpretation – ie: MSO 4 is morphine (Mg. SO 4 is mag sulfate and sounds similar!!!) • Whenever possible, words should be fully spelled out to avoid confusion 11
Abbreviations for Documentation • Last 2 pages list out abbreviations, acronyms, symbols – Common and medically accepted list • Hospital and EMS resources • Watch use of abbreviations for misinterpretation – ie: MSO 4 is morphine (Mg. SO 4 is mag sulfate and sounds similar!!!) • Whenever possible, words should be fully spelled out to avoid confusion 11
 Global Change • Oxygen administration – Patient must be assessed for need before automatically administering oxygen üBreathlessness üSigns of heart failure üSigns of shock üSp. O 2 <94% – O 2 not required/not found useful • Uncomplicated acute MI (AMI) or ACS patient without signs of hypoxemia or heart failure 12
Global Change • Oxygen administration – Patient must be assessed for need before automatically administering oxygen üBreathlessness üSigns of heart failure üSigns of shock üSp. O 2 <94% – O 2 not required/not found useful • Uncomplicated acute MI (AMI) or ACS patient without signs of hypoxemia or heart failure 12
 Pulse Oximetry vs Capnography • Capnography gives an instant and current snapshot of patient’s ventilation status – Measures exhaled CO 2 – Changes immediately if perfusion returns (ROSC) or if ventilation drops • Pulse oximetry change is delayed in time from the actual incident – Can also be falsely elevated in carbon monoxide exposure giving false sense of security
Pulse Oximetry vs Capnography • Capnography gives an instant and current snapshot of patient’s ventilation status – Measures exhaled CO 2 – Changes immediately if perfusion returns (ROSC) or if ventilation drops • Pulse oximetry change is delayed in time from the actual incident – Can also be falsely elevated in carbon monoxide exposure giving false sense of security
 Capnography • Departments that have the device will use the device • Normal readings (patient perfusing and ventilating self) are 35 -45 mm. Hg – Just like a blood gas result • Readings during effective CPR are >10 mm. HG • Reading <8 mm. Hg during CPR require reevaluation of technique, equipment and patient
Capnography • Departments that have the device will use the device • Normal readings (patient perfusing and ventilating self) are 35 -45 mm. Hg – Just like a blood gas result • Readings during effective CPR are >10 mm. HG • Reading <8 mm. Hg during CPR require reevaluation of technique, equipment and patient
 Global Reinforcement • Fluid challenges – Global formula is 20 m. L/kg all ages • Adults receive fluid in increments of 200 m. L – Move toward total goal (usually 1 – 2 L) – Reassess as you move past each 200 m. L increment • Pediatric total calculated at 20 m. L/kg – As you move toward total goal, reassess every 200 m. L • Example: Pediatric patient to get 480 m. L of fluid – Reassess at 200 m. L; 400 m. L; then 80 m. L 15
Global Reinforcement • Fluid challenges – Global formula is 20 m. L/kg all ages • Adults receive fluid in increments of 200 m. L – Move toward total goal (usually 1 – 2 L) – Reassess as you move past each 200 m. L increment • Pediatric total calculated at 20 m. L/kg – As you move toward total goal, reassess every 200 m. L • Example: Pediatric patient to get 480 m. L of fluid – Reassess at 200 m. L; 400 m. L; then 80 m. L 15
 Securing the Airway • A vague term: - indicates to do what is necessary to ventilate and oxygenate the patient after your assessment of the situation Question: The patient has snoring respirations – What would be done initially for the airway? • Reposition the patient – One of the least attempted maneuvers – Often most overlooked technique 16
Securing the Airway • A vague term: - indicates to do what is necessary to ventilate and oxygenate the patient after your assessment of the situation Question: The patient has snoring respirations – What would be done initially for the airway? • Reposition the patient – One of the least attempted maneuvers – Often most overlooked technique 16
 Question - Securing the Airway • The patient is unresponsive and breathing 4 times per minute – What would be the initial response for airway? • Begin to support ventilations via BVM – 5 -6 breaths per minute • EMS is working a full arrest – They have performed CPR, defibrillated, secured IV access, and started medications – What can now be done to secure the airway? • Intubate the patient (ETT, King airway, combitube) • Apply cervical collar to keep tube in place 17
Question - Securing the Airway • The patient is unresponsive and breathing 4 times per minute – What would be the initial response for airway? • Begin to support ventilations via BVM – 5 -6 breaths per minute • EMS is working a full arrest – They have performed CPR, defibrillated, secured IV access, and started medications – What can now be done to secure the airway? • Intubate the patient (ETT, King airway, combitube) • Apply cervical collar to keep tube in place 17
 Predicting Difficult Intubation • A tool: Mallampati score • The pharynx is viewed (the oral cavity) – Scoring • • I – Entire tonsil or tonsillar bed visible II – Upper half of tonsil or tonsil bed seen III – Soft and hard palates are clearly visible IV – Only hard palate is visible – The higher the score, the higher the degree of potential intubation difficulty, the more likely an alternate airway device is used 18
Predicting Difficult Intubation • A tool: Mallampati score • The pharynx is viewed (the oral cavity) – Scoring • • I – Entire tonsil or tonsillar bed visible II – Upper half of tonsil or tonsil bed seen III – Soft and hard palates are clearly visible IV – Only hard palate is visible – The higher the score, the higher the degree of potential intubation difficulty, the more likely an alternate airway device is used 18
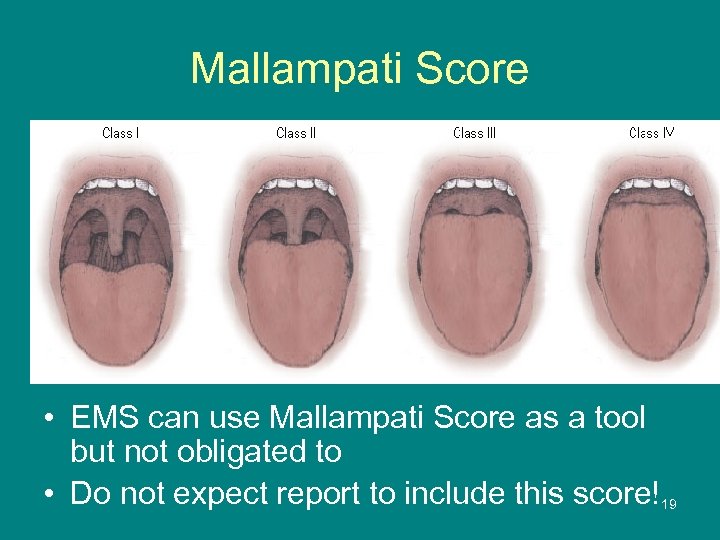 Mallampati Score • EMS can use Mallampati Score as a tool but not obligated to • Do not expect report to include this score!19
Mallampati Score • EMS can use Mallampati Score as a tool but not obligated to • Do not expect report to include this score!19
 Alternative to Endotracheal Intubation • EMS may place the King airway - more likely if failure with ETT • Some EMS may place the combitube- rare • If unable to place a device, may assist ventilations via BVM – Non-intubated patient with a pulse • Ventilate once every 5 -6 seconds – Intubated patient with any device • Ventilate once every 6 -8 seconds
Alternative to Endotracheal Intubation • EMS may place the King airway - more likely if failure with ETT • Some EMS may place the combitube- rare • If unable to place a device, may assist ventilations via BVM – Non-intubated patient with a pulse • Ventilate once every 5 -6 seconds – Intubated patient with any device • Ventilate once every 6 -8 seconds
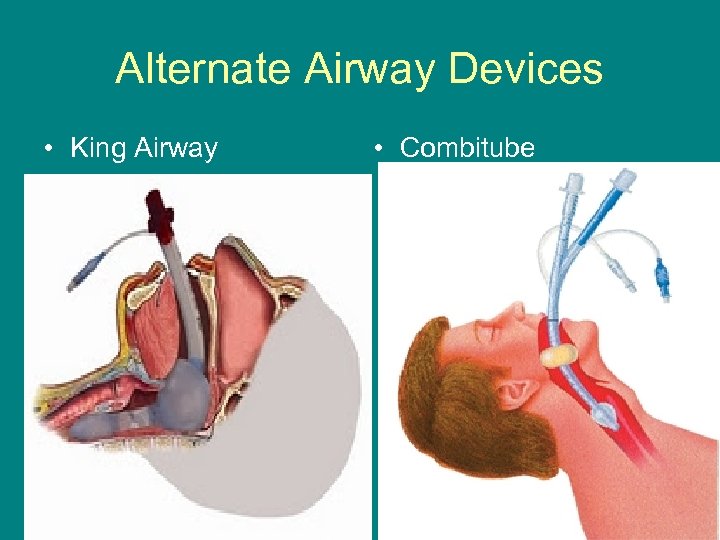 Alternate Airway Devices • King Airway • Combitube
Alternate Airway Devices • King Airway • Combitube
 Global Additions • Pain is considered the 5 th vital sign – All trauma patients and many medical patients need pain evaluated and documented • Time of onset • EMS to be as specific as possible – Most important to obtain and communicate to ED staff in presence of suspected acute stroke 22
Global Additions • Pain is considered the 5 th vital sign – All trauma patients and many medical patients need pain evaluated and documented • Time of onset • EMS to be as specific as possible – Most important to obtain and communicate to ED staff in presence of suspected acute stroke 22
 CPR Changes • Change from A-B-C to C-A B – After assessing responsiveness, begin compressions • Add 2 ventilations after the initial compressions – There was too long of a delay in starting compressions – There is always residual oxygen left in the lungs • Immediately resume compressions after each defibrillation attempt • Change compressors every 2 minutes during 10 second pause to check rhythm 23
CPR Changes • Change from A-B-C to C-A B – After assessing responsiveness, begin compressions • Add 2 ventilations after the initial compressions – There was too long of a delay in starting compressions – There is always residual oxygen left in the lungs • Immediately resume compressions after each defibrillation attempt • Change compressors every 2 minutes during 10 second pause to check rhythm 23
 CPR changes cont’d • Pulse checks performed ONLY if there is a rhythm viewed that should produce a pulse – So NO pulse check for VF or asystole • ROSC - If patient is resuscitated from cardiac arrest, remains unconscious, and pulse is maintained for a minimum of 5 minutes, start to cool the patient – Ice packs in areas with superficial blood vessels • Back of neck, axilla (armpits), groin, over IV 24 site
CPR changes cont’d • Pulse checks performed ONLY if there is a rhythm viewed that should produce a pulse – So NO pulse check for VF or asystole • ROSC - If patient is resuscitated from cardiac arrest, remains unconscious, and pulse is maintained for a minimum of 5 minutes, start to cool the patient – Ice packs in areas with superficial blood vessels • Back of neck, axilla (armpits), groin, over IV 24 site
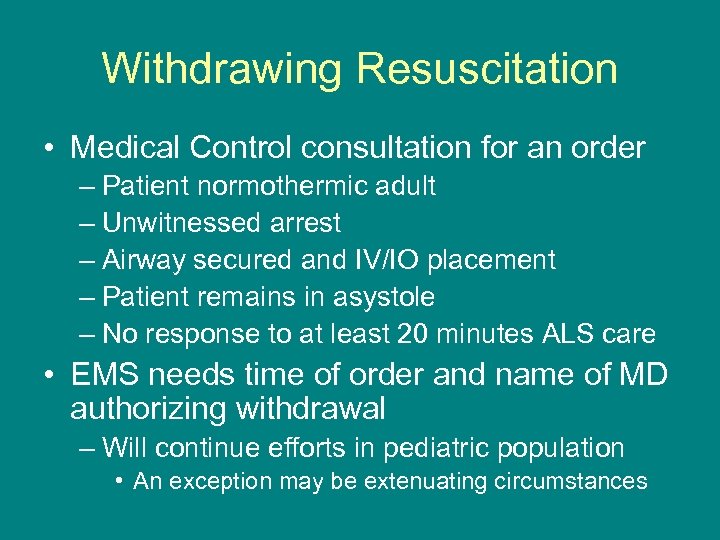 Withdrawing Resuscitation • Medical Control consultation for an order – Patient normothermic adult – Unwitnessed arrest – Airway secured and IV/IO placement – Patient remains in asystole – No response to at least 20 minutes ALS care • EMS needs time of order and name of MD authorizing withdrawal – Will continue efforts in pediatric population • An exception may be extenuating circumstances
Withdrawing Resuscitation • Medical Control consultation for an order – Patient normothermic adult – Unwitnessed arrest – Airway secured and IV/IO placement – Patient remains in asystole – No response to at least 20 minutes ALS care • EMS needs time of order and name of MD authorizing withdrawal – Will continue efforts in pediatric population • An exception may be extenuating circumstances
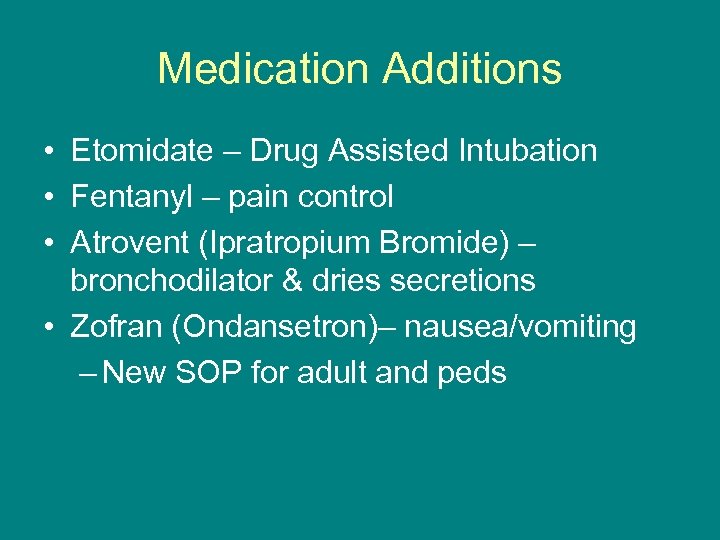 Medication Additions • Etomidate – Drug Assisted Intubation • Fentanyl – pain control • Atrovent (Ipratropium Bromide) – bronchodilator & dries secretions • Zofran (Ondansetron)– nausea/vomiting – New SOP for adult and peds
Medication Additions • Etomidate – Drug Assisted Intubation • Fentanyl – pain control • Atrovent (Ipratropium Bromide) – bronchodilator & dries secretions • Zofran (Ondansetron)– nausea/vomiting – New SOP for adult and peds
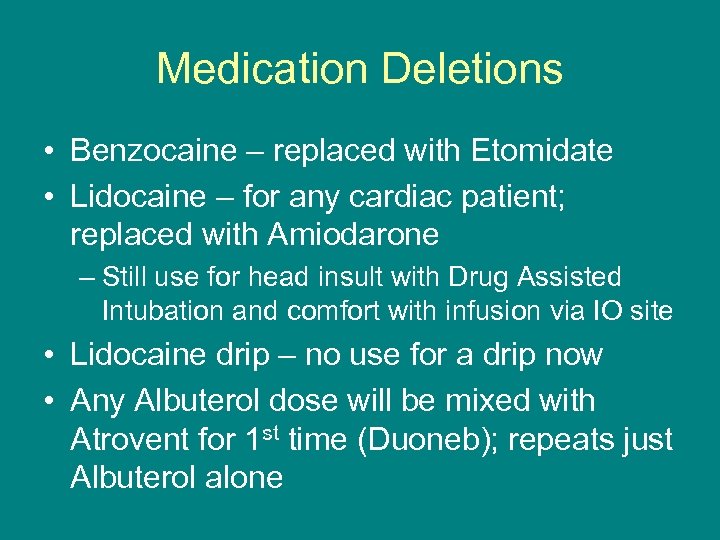 Medication Deletions • Benzocaine – replaced with Etomidate • Lidocaine – for any cardiac patient; replaced with Amiodarone – Still use for head insult with Drug Assisted Intubation and comfort with infusion via IO site • Lidocaine drip – no use for a drip now • Any Albuterol dose will be mixed with Atrovent for 1 st time (Duoneb); repeats just Albuterol alone
Medication Deletions • Benzocaine – replaced with Etomidate • Lidocaine – for any cardiac patient; replaced with Amiodarone – Still use for head insult with Drug Assisted Intubation and comfort with infusion via IO site • Lidocaine drip – no use for a drip now • Any Albuterol dose will be mixed with Atrovent for 1 st time (Duoneb); repeats just Albuterol alone
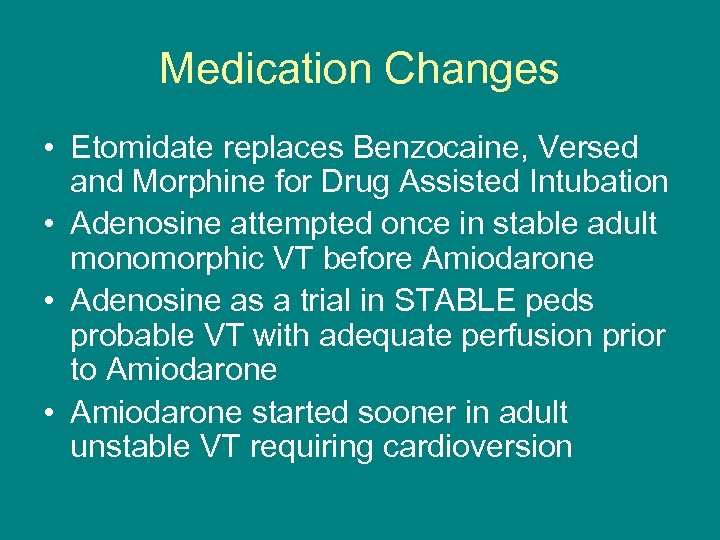 Medication Changes • Etomidate replaces Benzocaine, Versed and Morphine for Drug Assisted Intubation • Adenosine attempted once in stable adult monomorphic VT before Amiodarone • Adenosine as a trial in STABLE peds probable VT with adequate perfusion prior to Amiodarone • Amiodarone started sooner in adult unstable VT requiring cardioversion
Medication Changes • Etomidate replaces Benzocaine, Versed and Morphine for Drug Assisted Intubation • Adenosine attempted once in stable adult monomorphic VT before Amiodarone • Adenosine as a trial in STABLE peds probable VT with adequate perfusion prior to Amiodarone • Amiodarone started sooner in adult unstable VT requiring cardioversion
 Medication Changes cont’d • Versed 1 st line med for active seizures and behavioral situations – can be given IN (intranasally) avoiding needle stick potential • Fentanyl – 1 st pain med over Morphine – Morphine still 1 st for Acute Coronary Syndrome and burns if IV line is established
Medication Changes cont’d • Versed 1 st line med for active seizures and behavioral situations – can be given IN (intranasally) avoiding needle stick potential • Fentanyl – 1 st pain med over Morphine – Morphine still 1 st for Acute Coronary Syndrome and burns if IV line is established
 SOP Revisions • The following are SOP revisions effective February 1, 2012 – Affects Condell and Highland Park EMS System paramedics – Vista System paramedics will follow previous version SOP until March 1, 2012
SOP Revisions • The following are SOP revisions effective February 1, 2012 – Affects Condell and Highland Park EMS System paramedics – Vista System paramedics will follow previous version SOP until March 1, 2012
 Drug Assisted Intubation • Name change to SOP – Better reflects what is being done • Lidocaine necessary if head insult - medical or trauma (1. 5 mg/kg IVP/IO) – Eliminates cough reflex to prevent ICP • Etomidate (0. 3 mg/kg IVP/IO; max 20 mg) – As hypnotic, sedative • Replaces initial Versed, Morphine, Benzocaine • Versed (2 mg IVP/IO every 2 min to max 20 mg) – To keep patient sedated 31
Drug Assisted Intubation • Name change to SOP – Better reflects what is being done • Lidocaine necessary if head insult - medical or trauma (1. 5 mg/kg IVP/IO) – Eliminates cough reflex to prevent ICP • Etomidate (0. 3 mg/kg IVP/IO; max 20 mg) – As hypnotic, sedative • Replaces initial Versed, Morphine, Benzocaine • Versed (2 mg IVP/IO every 2 min to max 20 mg) – To keep patient sedated 31
 Peds Drug Assisted Intubation • NEW!!! • Similar to adult process • Added Atropine as a pre-medication – Avoid potential bradycardia from stimulation during intubation attempts
Peds Drug Assisted Intubation • NEW!!! • Similar to adult process • Added Atropine as a pre-medication – Avoid potential bradycardia from stimulation during intubation attempts
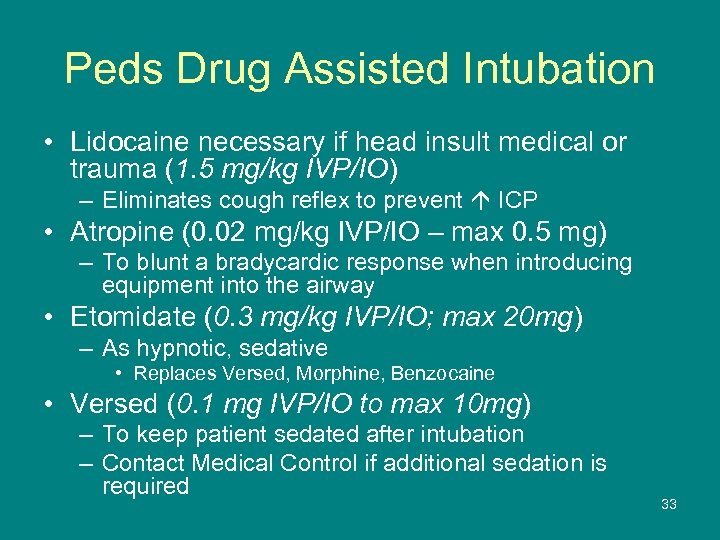 Peds Drug Assisted Intubation • Lidocaine necessary if head insult medical or trauma (1. 5 mg/kg IVP/IO) – Eliminates cough reflex to prevent ICP • Atropine (0. 02 mg/kg IVP/IO – max 0. 5 mg) – To blunt a bradycardic response when introducing equipment into the airway • Etomidate (0. 3 mg/kg IVP/IO; max 20 mg) – As hypnotic, sedative • Replaces Versed, Morphine, Benzocaine • Versed (0. 1 mg IVP/IO to max 10 mg) – To keep patient sedated after intubation – Contact Medical Control if additional sedation is required 33
Peds Drug Assisted Intubation • Lidocaine necessary if head insult medical or trauma (1. 5 mg/kg IVP/IO) – Eliminates cough reflex to prevent ICP • Atropine (0. 02 mg/kg IVP/IO – max 0. 5 mg) – To blunt a bradycardic response when introducing equipment into the airway • Etomidate (0. 3 mg/kg IVP/IO; max 20 mg) – As hypnotic, sedative • Replaces Versed, Morphine, Benzocaine • Versed (0. 1 mg IVP/IO to max 10 mg) – To keep patient sedated after intubation – Contact Medical Control if additional sedation is required 33
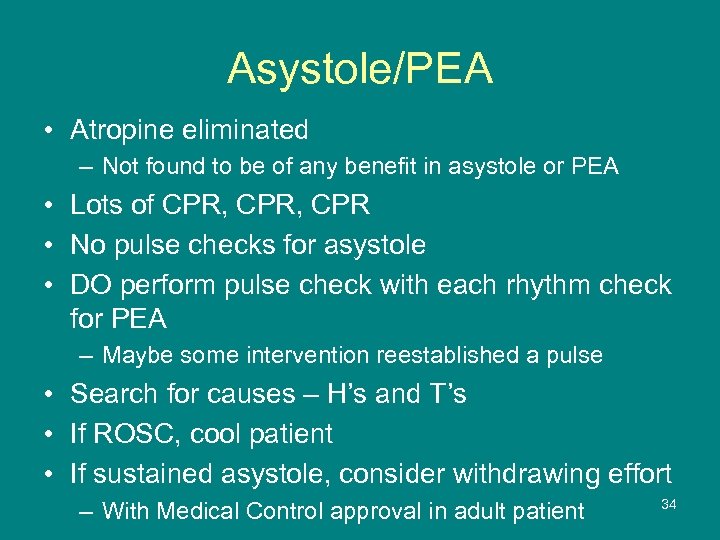 Asystole/PEA • Atropine eliminated – Not found to be of any benefit in asystole or PEA • Lots of CPR, CPR • No pulse checks for asystole • DO perform pulse check with each rhythm check for PEA – Maybe some intervention reestablished a pulse • Search for causes – H’s and T’s • If ROSC, cool patient • If sustained asystole, consider withdrawing effort – With Medical Control approval in adult patient 34
Asystole/PEA • Atropine eliminated – Not found to be of any benefit in asystole or PEA • Lots of CPR, CPR • No pulse checks for asystole • DO perform pulse check with each rhythm check for PEA – Maybe some intervention reestablished a pulse • Search for causes – H’s and T’s • If ROSC, cool patient • If sustained asystole, consider withdrawing effort – With Medical Control approval in adult patient 34
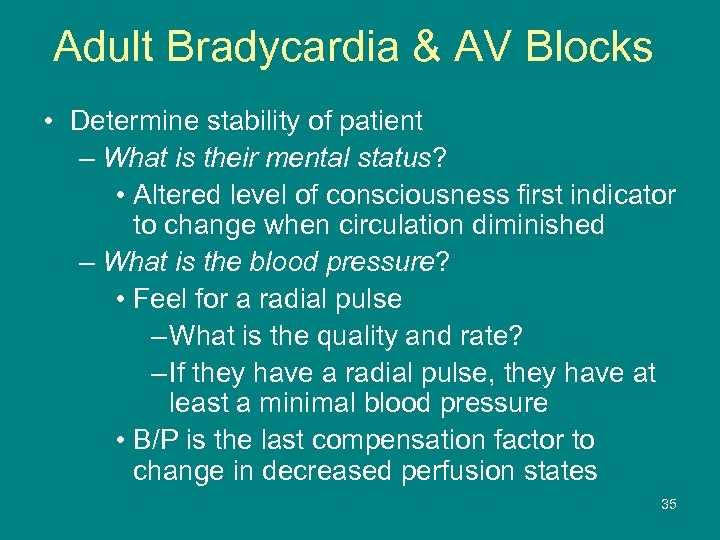 Adult Bradycardia & AV Blocks • Determine stability of patient – What is their mental status? • Altered level of consciousness first indicator to change when circulation diminished – What is the blood pressure? • Feel for a radial pulse – What is the quality and rate? – If they have a radial pulse, they have at least a minimal blood pressure • B/P is the last compensation factor to change in decreased perfusion states 35
Adult Bradycardia & AV Blocks • Determine stability of patient – What is their mental status? • Altered level of consciousness first indicator to change when circulation diminished – What is the blood pressure? • Feel for a radial pulse – What is the quality and rate? – If they have a radial pulse, they have at least a minimal blood pressure • B/P is the last compensation factor to change in decreased perfusion states 35
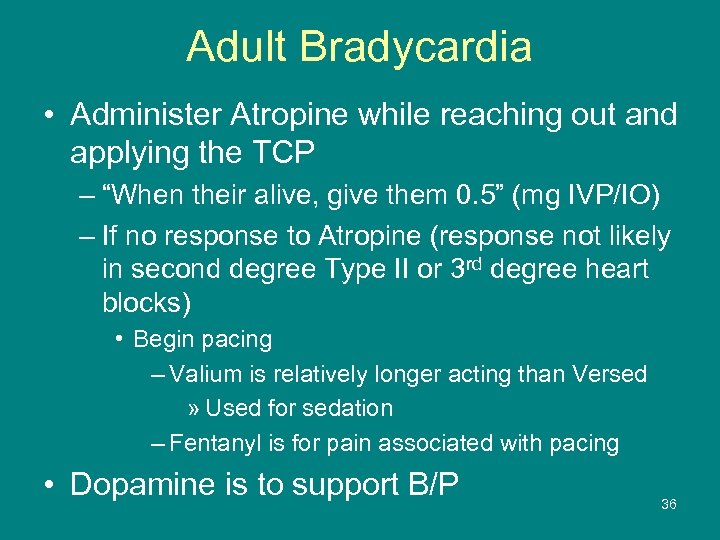 Adult Bradycardia • Administer Atropine while reaching out and applying the TCP – “When their alive, give them 0. 5” (mg IVP/IO) – If no response to Atropine (response not likely in second degree Type II or 3 rd degree heart blocks) • Begin pacing – Valium is relatively longer acting than Versed » Used for sedation – Fentanyl is for pain associated with pacing • Dopamine is to support B/P 36
Adult Bradycardia • Administer Atropine while reaching out and applying the TCP – “When their alive, give them 0. 5” (mg IVP/IO) – If no response to Atropine (response not likely in second degree Type II or 3 rd degree heart blocks) • Begin pacing – Valium is relatively longer acting than Versed » Used for sedation – Fentanyl is for pain associated with pacing • Dopamine is to support B/P 36
 Adult Acute Coronary Syndrome • Obtaining a 12 lead as soon as possible will help direct patient care – To give or hold Nitroglycerin • Held in presence of ST elevation in II, III, a. VF (inferior wall MI) • Held if Viagra type drug use past 24 -48 hours • Held if systolic B/P <90 – Results determine activation of hospital cardiac alert • Aspirin is important to inhibit platelet aggregation – Better to get an extra dose than to not have a dose – Can hold if patient reliable and DID take ASA • Per AHA, Morphine is the preferred drug in AMI 37
Adult Acute Coronary Syndrome • Obtaining a 12 lead as soon as possible will help direct patient care – To give or hold Nitroglycerin • Held in presence of ST elevation in II, III, a. VF (inferior wall MI) • Held if Viagra type drug use past 24 -48 hours • Held if systolic B/P <90 – Results determine activation of hospital cardiac alert • Aspirin is important to inhibit platelet aggregation – Better to get an extra dose than to not have a dose – Can hold if patient reliable and DID take ASA • Per AHA, Morphine is the preferred drug in AMI 37
 Adult Cardiogenic Shock • EMS starts at 5 mcg/kg/min • Expanded dose ranges added for dopamine ü 5 mcg/kg/min ü 10 mcg/kg/min ü 15 mcg/kg/min ü 20 mcg/kg/min • Easy way to calculate 5 mcg/kg/min – – – Determine patient weight in pounds Take first 2 numbers Subtract 2 That’s where to start the minidrip (Ex: 180 # 18 – 2 = 16 mini drips per minute) 38
Adult Cardiogenic Shock • EMS starts at 5 mcg/kg/min • Expanded dose ranges added for dopamine ü 5 mcg/kg/min ü 10 mcg/kg/min ü 15 mcg/kg/min ü 20 mcg/kg/min • Easy way to calculate 5 mcg/kg/min – – – Determine patient weight in pounds Take first 2 numbers Subtract 2 That’s where to start the minidrip (Ex: 180 # 18 – 2 = 16 mini drips per minute) 38
 Adult SVT/Rapid A Fib/Flutter • Determine if the patient is stable or not üCheck level of consciousness üCheck blood pressure • Patient determined to be unstable or relatively stable – Remember that patients will have symptoms if pulse rapid » Having symptoms doesn’t necessarily make someone unstable, just symptomatic 39
Adult SVT/Rapid A Fib/Flutter • Determine if the patient is stable or not üCheck level of consciousness üCheck blood pressure • Patient determined to be unstable or relatively stable – Remember that patients will have symptoms if pulse rapid » Having symptoms doesn’t necessarily make someone unstable, just symptomatic 39
 Valsalva Maneuvers if Stable • Need to stimulate the vagus nerve to slow down the impulses in rapid heart rates – Have patient bear down (carefully) for 10 seconds – Have patient blow through a straw • Can’t blow through a straw? – Have patient stick their thumb in their mouth and blow against the thumb – Effective for pediatric population 40
Valsalva Maneuvers if Stable • Need to stimulate the vagus nerve to slow down the impulses in rapid heart rates – Have patient bear down (carefully) for 10 seconds – Have patient blow through a straw • Can’t blow through a straw? – Have patient stick their thumb in their mouth and blow against the thumb – Effective for pediatric population 40
 Managing Sedation & Pain with Cardioversion • Cardioversion is a painful procedure • Versed used to sedate/relax the patient and act as a hypnotic – Not something you want to have memory of! • Fentanyl can be used to manage any complaints of pain after the procedure – There may be residual discomfort in the chest 41
Managing Sedation & Pain with Cardioversion • Cardioversion is a painful procedure • Versed used to sedate/relax the patient and act as a hypnotic – Not something you want to have memory of! • Fentanyl can be used to manage any complaints of pain after the procedure – There may be residual discomfort in the chest 41
 Adult VF/Pulseless VT • Begin CPR (C-A-B) until defibrillator ready • Biphasic joules amount is based on brand of defibrillator • Resume CPR immediately after each shock is delivered • Alternate Epinephrine 1: 10, 000 with 2 rounds of Amiodarone (300 mg 1 st dose, then 150 mg 2 nd dose in 3 -5 minutes) – Amiodarone more effective and studied/effects reviewed more than Lidocaine 42
Adult VF/Pulseless VT • Begin CPR (C-A-B) until defibrillator ready • Biphasic joules amount is based on brand of defibrillator • Resume CPR immediately after each shock is delivered • Alternate Epinephrine 1: 10, 000 with 2 rounds of Amiodarone (300 mg 1 st dose, then 150 mg 2 nd dose in 3 -5 minutes) – Amiodarone more effective and studied/effects reviewed more than Lidocaine 42
 Adult VT with Pulse • Stable monomorphic – From beat to beat the complexes have same shape and form – Trial dose of Adenosine • Trying to determine if rhythm is SVT with aberrancy or VT • Relatively safe for diagnosis and treatment • NOT okay if irregular or polymorphic VT – May deteriorate to VF • If SVT with aberrancy, may transiently slow down or convert to sinus rhythm 43
Adult VT with Pulse • Stable monomorphic – From beat to beat the complexes have same shape and form – Trial dose of Adenosine • Trying to determine if rhythm is SVT with aberrancy or VT • Relatively safe for diagnosis and treatment • NOT okay if irregular or polymorphic VT – May deteriorate to VF • If SVT with aberrancy, may transiently slow down or convert to sinus rhythm 43
 Monomorphic vs Polymorphic VT • Monomorphic – complexes appear the same • Polymorphic – complexes change beat to beat 44
Monomorphic vs Polymorphic VT • Monomorphic – complexes appear the same • Polymorphic – complexes change beat to beat 44
 Adult VT with Pulse • Polymorphic VT – Complexes vary from beat to beat – If stable, treatment with Amiodarone • Amiodarone must be administered slowly in the non-arrested patient (over 10 minutes) – Watch for hypotension • Unstable patient with any tachycardia – Losing consciousness – Poor perfusion (B/P <90 mm. Hg) • Need to cardiovert 45
Adult VT with Pulse • Polymorphic VT – Complexes vary from beat to beat – If stable, treatment with Amiodarone • Amiodarone must be administered slowly in the non-arrested patient (over 10 minutes) – Watch for hypotension • Unstable patient with any tachycardia – Losing consciousness – Poor perfusion (B/P <90 mm. Hg) • Need to cardiovert 45
 Cardioversion • Start at relatively low doses/joules • Increase joules as needed • This is a painful procedure – Versed used to sedate patient and as amnesic • Relatively short acting • Benefit – it can be given IN via MAD – Manage pain with Fentanyl • Will want/need an IV in this population at some time – more unstable patient 46
Cardioversion • Start at relatively low doses/joules • Increase joules as needed • This is a painful procedure – Versed used to sedate patient and as amnesic • Relatively short acting • Benefit – it can be given IN via MAD – Manage pain with Fentanyl • Will want/need an IV in this population at some time – more unstable patient 46
 Adult & Peds Seizures • Why is Versed used? – Shorter acting than Valium • Both are Benzodiazepines – Versed can also be given via the IN route via MAD • Reduces exposure to inadvertent needle sticks 47
Adult & Peds Seizures • Why is Versed used? – Shorter acting than Valium • Both are Benzodiazepines – Versed can also be given via the IN route via MAD • Reduces exposure to inadvertent needle sticks 47
 Adult & Peds Seizures • Need to determine cause of seizure activity – If epileptic, head injury, brain tumor type causes, patient will most likely respond to a Benzodiazepine (i. e. : Versed) – If seizure due to lowered blood sugar level, the patient needs glucose • The brain is starving for sugar, needs Glucose • Glucagon is a hormone to release sugar stores if available; it is not sugar – Given IM/IN in absence of IV access 48
Adult & Peds Seizures • Need to determine cause of seizure activity – If epileptic, head injury, brain tumor type causes, patient will most likely respond to a Benzodiazepine (i. e. : Versed) – If seizure due to lowered blood sugar level, the patient needs glucose • The brain is starving for sugar, needs Glucose • Glucagon is a hormone to release sugar stores if available; it is not sugar – Given IM/IN in absence of IV access 48
 Adult & Peds Burns • Why is Morphine used for pain for the patient with burns? – Morphine is longer acting than Fentanyl • Therefore, less doses should have to administered in the field – In burns, we know why the patient is having pain; don’t need it “worn off” for assessment at hospital • In absence of IV access, Fentanyl can be given IN via MAD 49
Adult & Peds Burns • Why is Morphine used for pain for the patient with burns? – Morphine is longer acting than Fentanyl • Therefore, less doses should have to administered in the field – In burns, we know why the patient is having pain; don’t need it “worn off” for assessment at hospital • In absence of IV access, Fentanyl can be given IN via MAD 49
 Adult & Peds Pain Management • Fentanyl 0. 5 mcg/kg (adult & peds) – Synthetic narcotic – Relatively short acting – If respiratory depression, can be reversed with Narcan • Support respirations via BVM if needed – Can be given variety of routes • IVP/IN/IO – Dose calculated by patient weight • FYI - A 875 pound patient would get 198 mcg (max is 200 mcg) 50
Adult & Peds Pain Management • Fentanyl 0. 5 mcg/kg (adult & peds) – Synthetic narcotic – Relatively short acting – If respiratory depression, can be reversed with Narcan • Support respirations via BVM if needed – Can be given variety of routes • IVP/IN/IO – Dose calculated by patient weight • FYI - A 875 pound patient would get 198 mcg (max is 200 mcg) 50
 Adult & Peds Nausea Management • Zofran (ondansetron) is a frequently used medication – Adults & peds >40 kg – 4 mg – Peds <40 kg 0. 1 mg/kg • If nausea is relieved, the patient may not need other medication for a secondary problem (i. e. : abdominal pain with nausea) • Often causes drowsiness – Watch airway for aspiration precautions 51
Adult & Peds Nausea Management • Zofran (ondansetron) is a frequently used medication – Adults & peds >40 kg – 4 mg – Peds <40 kg 0. 1 mg/kg • If nausea is relieved, the patient may not need other medication for a secondary problem (i. e. : abdominal pain with nausea) • Often causes drowsiness – Watch airway for aspiration precautions 51
 Peds Bradycardia • The pediatric etiology of bradycardia is different than the adult population • First drug is Epinephrine 1: 10, 000 – 0. 01 mg/kg IVP/IO – Repeated every 3 -5 minutes if no response • Medical Control to be contacted to consider Atropine order – Most peds patients do not have sick hearts so usually do not respond to Atropine 52
Peds Bradycardia • The pediatric etiology of bradycardia is different than the adult population • First drug is Epinephrine 1: 10, 000 – 0. 01 mg/kg IVP/IO – Repeated every 3 -5 minutes if no response • Medical Control to be contacted to consider Atropine order – Most peds patients do not have sick hearts so usually do not respond to Atropine 52
 Peds VF/Pulseless VT • Begin CPR (C-A-B) until defibrillator ready • Defibrillation is 2 joules/kg; then 4 j/kg • Resume CPR immediately after each shock is delivered • Alternate Epinephrine 1: 10, 000 with 2 rounds of Amiodarone (5 mg/kg 1 st dose, then 5 mg/kg 2 nd dose in 3 -5 minutes) – Amiodarone more effective and studied/effects reviewed more than Lidocaine 53
Peds VF/Pulseless VT • Begin CPR (C-A-B) until defibrillator ready • Defibrillation is 2 joules/kg; then 4 j/kg • Resume CPR immediately after each shock is delivered • Alternate Epinephrine 1: 10, 000 with 2 rounds of Amiodarone (5 mg/kg 1 st dose, then 5 mg/kg 2 nd dose in 3 -5 minutes) – Amiodarone more effective and studied/effects reviewed more than Lidocaine 53
 SOP Skill References • Placed in the SOP’s as a quick “how-to” reference • Step by step detail to complete a skill • Located at the back of the SOP’s 54
SOP Skill References • Placed in the SOP’s as a quick “how-to” reference • Step by step detail to complete a skill • Located at the back of the SOP’s 54
 King Airway • New to the Region • Alternative airway adjunct • Used as a backup when intubation with the endotracheal tube cannot be accomplished • Cannot be used in presence of a gag reflex – Check for the blink reflex, if present then gag is still present – Etomidate used to sedate the patient • Will control the gag reflex 55
King Airway • New to the Region • Alternative airway adjunct • Used as a backup when intubation with the endotracheal tube cannot be accomplished • Cannot be used in presence of a gag reflex – Check for the blink reflex, if present then gag is still present – Etomidate used to sedate the patient • Will control the gag reflex 55
 King Airway • Contraindications – Height less than 4 feet • Our tubes sizes are #3, #4, #5 – Sizes match up with heights » #3 for 4 -5' heights (yellow tip) (think 3 -4 -5) » #4 for 5 -6' heights (red tip) (think 4 -5 -6) » #5 for >6' heights (purple tip) (think 5 -6) – Do not want to insert with diseased/damaged esophagus • Could tear through esophageal wall 56
King Airway • Contraindications – Height less than 4 feet • Our tubes sizes are #3, #4, #5 – Sizes match up with heights » #3 for 4 -5' heights (yellow tip) (think 3 -4 -5) » #4 for 5 -6' heights (red tip) (think 4 -5 -6) » #5 for >6' heights (purple tip) (think 5 -6) – Do not want to insert with diseased/damaged esophagus • Could tear through esophageal wall 56
 King Airway • • Distal cuff sits in and seals esophagus Proximal cuff seals oropharynx Air enters trachea between the cuffs King does NOT fully protect the airway from potential aspiration following vomiting – ETT is superior in aspiration protection – Decision by ED MD to extubate King airway and replace with ETT prior to admission • No meds administered thru King airway • Ventilate once every 6 -8 seconds via King 57
King Airway • • Distal cuff sits in and seals esophagus Proximal cuff seals oropharynx Air enters trachea between the cuffs King does NOT fully protect the airway from potential aspiration following vomiting – ETT is superior in aspiration protection – Decision by ED MD to extubate King airway and replace with ETT prior to admission • No meds administered thru King airway • Ventilate once every 6 -8 seconds via King 57
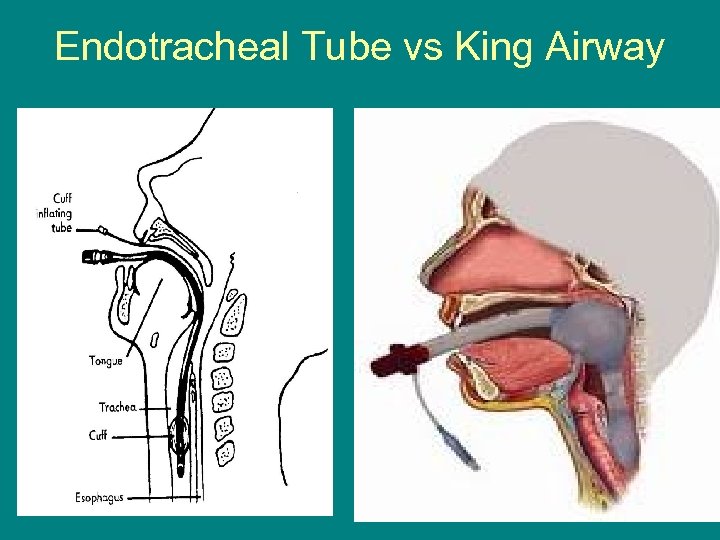 Endotracheal Tube vs King Airway 58
Endotracheal Tube vs King Airway 58
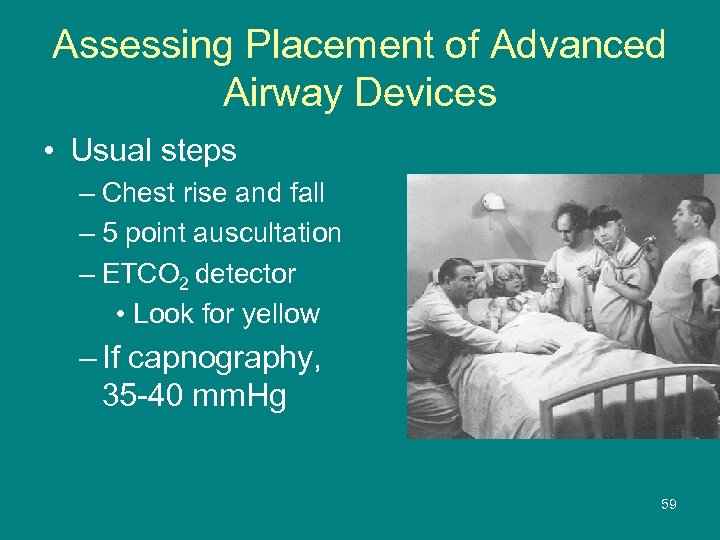 Assessing Placement of Advanced Airway Devices • Usual steps – Chest rise and fall – 5 point auscultation – ETCO 2 detector • Look for yellow – If capnography, 35 -40 mm. Hg reading 59
Assessing Placement of Advanced Airway Devices • Usual steps – Chest rise and fall – 5 point auscultation – ETCO 2 detector • Look for yellow – If capnography, 35 -40 mm. Hg reading 59
 Removing King Airway • Prepare alternate airway equipment • Deflate cuffs – One pilot used for both cuffs – Can hold 45 -90 ml air depending on size tube • Extubate similar to removing an ETT • Prepare to oxygenate and ventilate patient as needed • Secure airway with appropriate alternate method
Removing King Airway • Prepare alternate airway equipment • Deflate cuffs – One pilot used for both cuffs – Can hold 45 -90 ml air depending on size tube • Extubate similar to removing an ETT • Prepare to oxygenate and ventilate patient as needed • Secure airway with appropriate alternate method
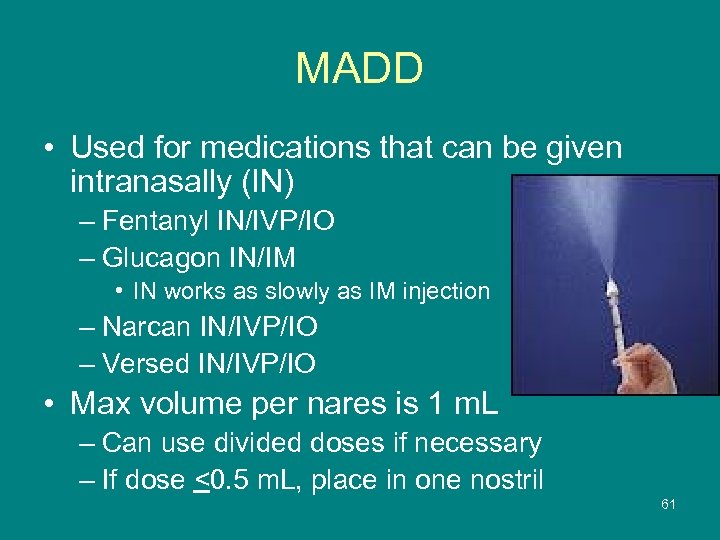 MADD • Used for medications that can be given intranasally (IN) – Fentanyl IN/IVP/IO – Glucagon IN/IM • IN works as slowly as IM injection – Narcan IN/IVP/IO – Versed IN/IVP/IO • Max volume per nares is 1 m. L – Can use divided doses if necessary – If dose <0. 5 m. L, place in one nostril 61
MADD • Used for medications that can be given intranasally (IN) – Fentanyl IN/IVP/IO – Glucagon IN/IM • IN works as slowly as IM injection – Narcan IN/IVP/IO – Versed IN/IVP/IO • Max volume per nares is 1 m. L – Can use divided doses if necessary – If dose <0. 5 m. L, place in one nostril 61
 Intraosseous Infusions • Regardless of site used, equipment is the same üSite preparation material / cleanser üDrill üNeedle üPrimed EZ connect tubing üPrimed IV tubing spiked to IV fluid bag üPressure bag üMethod to secure the site • Lidocaine useful for pain control during infusion 62
Intraosseous Infusions • Regardless of site used, equipment is the same üSite preparation material / cleanser üDrill üNeedle üPrimed EZ connect tubing üPrimed IV tubing spiked to IV fluid bag üPressure bag üMethod to secure the site • Lidocaine useful for pain control during infusion 62
 Humeral IO Site • Used as a backup to a peripheral IV site • Situation in which you NEED IV access • Proximal humeral site a backup in the adult patient population – Primary site should be the proximal tibial area 63
Humeral IO Site • Used as a backup to a peripheral IV site • Situation in which you NEED IV access • Proximal humeral site a backup in the adult patient population – Primary site should be the proximal tibial area 63
 Sizing an IO Needle • Assess patient to determine the size needle to use for the site used – Palpate over your wrist in line with the thumb • Do you feel the bone? • If you feel the child’s tibia like this, use the shorter pink needle – Palpate the inside crook of your elbow • Do you feel the meatiness? • If you feel the child’s tibia like this, use the middle sized blue needle – Humeral site for the adult • Always use the long yellow needle 64
Sizing an IO Needle • Assess patient to determine the size needle to use for the site used – Palpate over your wrist in line with the thumb • Do you feel the bone? • If you feel the child’s tibia like this, use the shorter pink needle – Palpate the inside crook of your elbow • Do you feel the meatiness? • If you feel the child’s tibia like this, use the middle sized blue needle – Humeral site for the adult • Always use the long yellow needle 64
 Adult Humeral Head Site Need to keep arm immobilized after needle placement 65
Adult Humeral Head Site Need to keep arm immobilized after needle placement 65
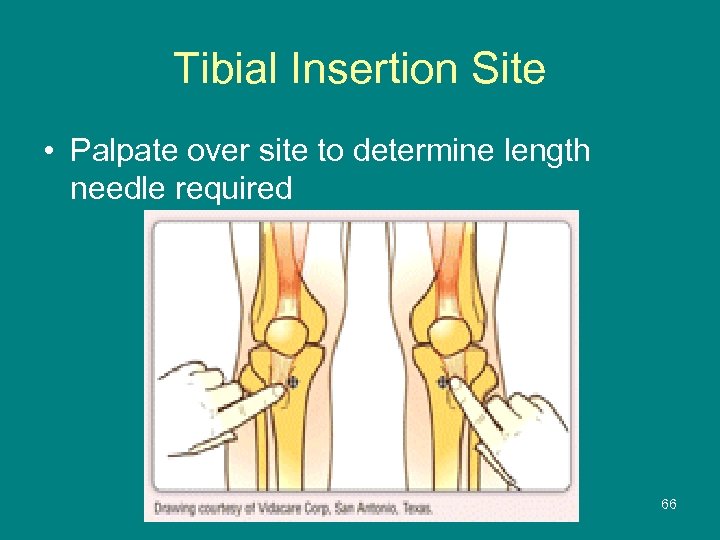 Tibial Insertion Site • Palpate over site to determine length needle required 66
Tibial Insertion Site • Palpate over site to determine length needle required 66
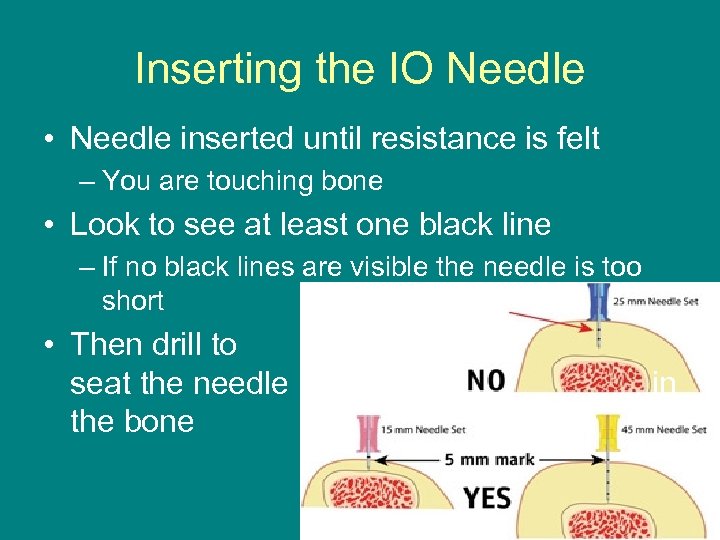 Inserting the IO Needle • Needle inserted until resistance is felt – You are touching bone • Look to see at least one black line – If no black lines are visible the needle is too short • Then drill to seat the needle the bone in 67
Inserting the IO Needle • Needle inserted until resistance is felt – You are touching bone • Look to see at least one black line – If no black lines are visible the needle is too short • Then drill to seat the needle the bone in 67
 Removing an IO Needle • Establish an alternate IV site • Stop IO infusion system • Remove IV tubing and EZ connect extension tubing • Connect a syringe to needle hub – Gives you something to hold onto • As you turn syringe clockwise, exert steady, gentle pull – Turning counter clockwise just disconnects the syringe – It takes quite a few turns to remove the needle • As the needle is removed, place bandaid over site
Removing an IO Needle • Establish an alternate IV site • Stop IO infusion system • Remove IV tubing and EZ connect extension tubing • Connect a syringe to needle hub – Gives you something to hold onto • As you turn syringe clockwise, exert steady, gentle pull – Turning counter clockwise just disconnects the syringe – It takes quite a few turns to remove the needle • As the needle is removed, place bandaid over site
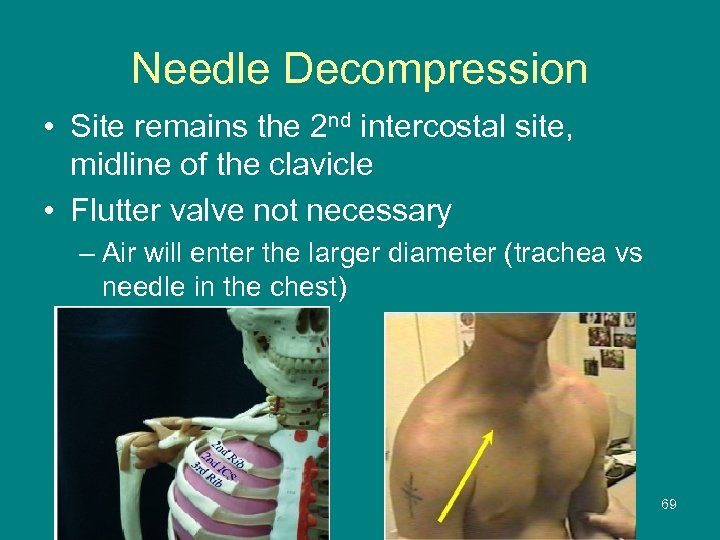 Needle Decompression • Site remains the 2 nd intercostal site, midline of the clavicle • Flutter valve not necessary – Air will enter the larger diameter (trachea vs needle in the chest) 69
Needle Decompression • Site remains the 2 nd intercostal site, midline of the clavicle • Flutter valve not necessary – Air will enter the larger diameter (trachea vs needle in the chest) 69
 2010 AHA CPR Guidelines • You should have been updated in the 2010 AHA guidelines by now or heard of the changes • Key points – Push hard, push fast (rate at least 100/minute) – Ventilate slower • 1 breath every 6 seconds • Immediately resume CPR after each defibrillation attempt • Switch compressors every 2 minutes 70
2010 AHA CPR Guidelines • You should have been updated in the 2010 AHA guidelines by now or heard of the changes • Key points – Push hard, push fast (rate at least 100/minute) – Ventilate slower • 1 breath every 6 seconds • Immediately resume CPR after each defibrillation attempt • Switch compressors every 2 minutes 70
 ROSC & Cooling • Return of spontaneous circulation – – Following cardiac arrest Patient remains unconscious & unresponsive Pulse is present at least 5 minutes B/P able to be maintained >90 • Not recommended for respiratory arrest • Remember – if patient is able to complain about the coldness of the ice packs, they don’t need to be cooled • Ice packs used by EMS 71
ROSC & Cooling • Return of spontaneous circulation – – Following cardiac arrest Patient remains unconscious & unresponsive Pulse is present at least 5 minutes B/P able to be maintained >90 • Not recommended for respiratory arrest • Remember – if patient is able to complain about the coldness of the ice packs, they don’t need to be cooled • Ice packs used by EMS 71
 SOP References • Placed in the SOP’s to be immediately available for review as needed • Are adjuncts to the SOP’s • Useful information available that can be referenced – Nice to have available when you are not sure of a process – Contains reference tables of norms • Vital signs • Equipment 72
SOP References • Placed in the SOP’s to be immediately available for review as needed • Are adjuncts to the SOP’s • Useful information available that can be referenced – Nice to have available when you are not sure of a process – Contains reference tables of norms • Vital signs • Equipment 72
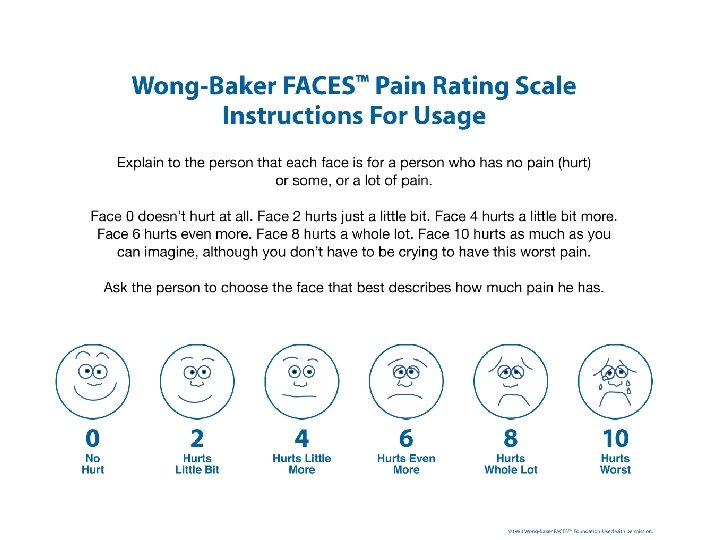
 Pain Scales • Wong-Baker FACESTM Pain Rating Scale – – Useful for 3 year-old and older Useful for non-English speaking patients Point to the face and read the description Ask the patient to point to the face that describes their pain • FLACC Pain Scale – An observer related method to assess for pain – Evaluates the face, legs, activity, crying, and consolability • Copyright 1983, Wong-Baker FACESTM Foundation, www. Wong. Baker. FACES. org. Used with permission. 73
Pain Scales • Wong-Baker FACESTM Pain Rating Scale – – Useful for 3 year-old and older Useful for non-English speaking patients Point to the face and read the description Ask the patient to point to the face that describes their pain • FLACC Pain Scale – An observer related method to assess for pain – Evaluates the face, legs, activity, crying, and consolability • Copyright 1983, Wong-Baker FACESTM Foundation, www. Wong. Baker. FACES. org. Used with permission. 73
 74
74
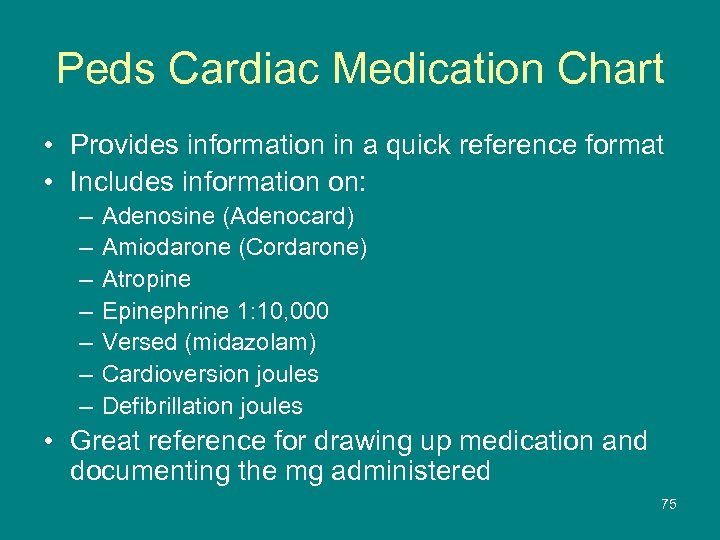 Peds Cardiac Medication Chart • Provides information in a quick reference format • Includes information on: – – – – Adenosine (Adenocard) Amiodarone (Cordarone) Atropine Epinephrine 1: 10, 000 Versed (midazolam) Cardioversion joules Defibrillation joules • Great reference for drawing up medication and documenting the mg administered 75
Peds Cardiac Medication Chart • Provides information in a quick reference format • Includes information on: – – – – Adenosine (Adenocard) Amiodarone (Cordarone) Atropine Epinephrine 1: 10, 000 Versed (midazolam) Cardioversion joules Defibrillation joules • Great reference for drawing up medication and documenting the mg administered 75
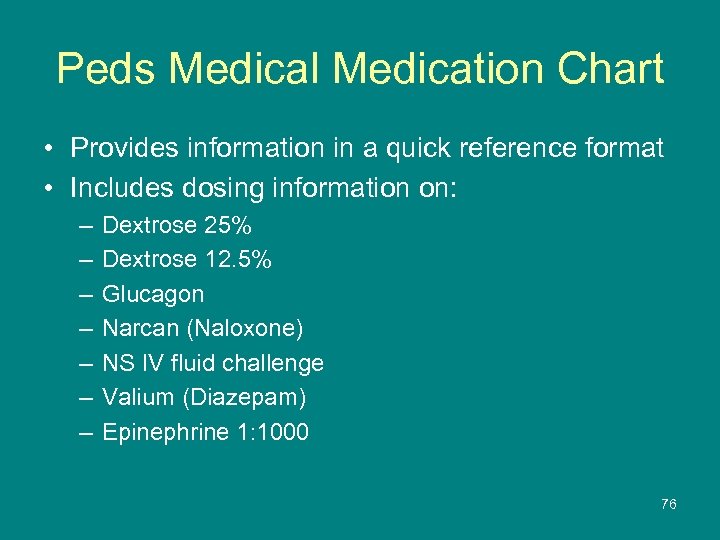 Peds Medical Medication Chart • Provides information in a quick reference format • Includes dosing information on: – – – – Dextrose 25% Dextrose 12. 5% Glucagon Narcan (Naloxone) NS IV fluid challenge Valium (Diazepam) Epinephrine 1: 1000 76
Peds Medical Medication Chart • Provides information in a quick reference format • Includes dosing information on: – – – – Dextrose 25% Dextrose 12. 5% Glucagon Narcan (Naloxone) NS IV fluid challenge Valium (Diazepam) Epinephrine 1: 1000 76
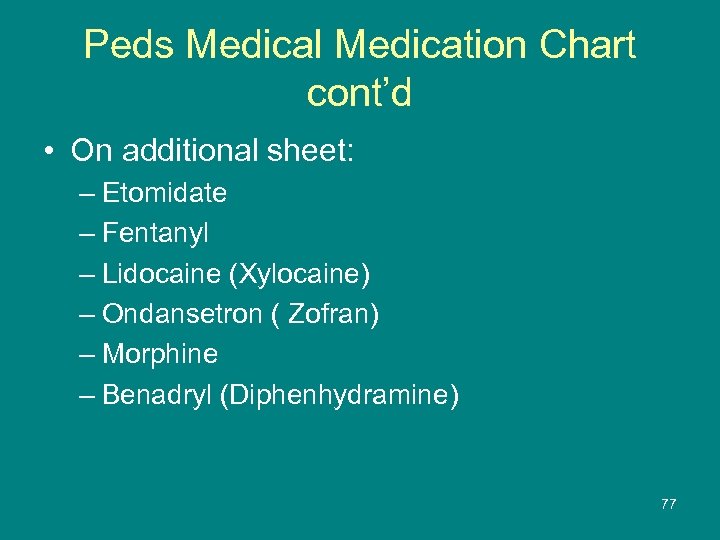 Peds Medical Medication Chart cont’d • On additional sheet: – Etomidate – Fentanyl – Lidocaine (Xylocaine) – Ondansetron ( Zofran) – Morphine – Benadryl (Diphenhydramine) 77
Peds Medical Medication Chart cont’d • On additional sheet: – Etomidate – Fentanyl – Lidocaine (Xylocaine) – Ondansetron ( Zofran) – Morphine – Benadryl (Diphenhydramine) 77
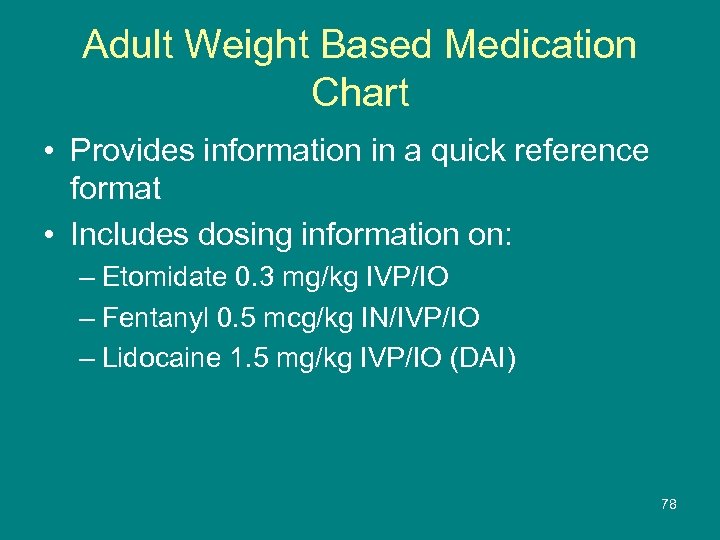 Adult Weight Based Medication Chart • Provides information in a quick reference format • Includes dosing information on: – Etomidate 0. 3 mg/kg IVP/IO – Fentanyl 0. 5 mcg/kg IN/IVP/IO – Lidocaine 1. 5 mg/kg IVP/IO (DAI) 78
Adult Weight Based Medication Chart • Provides information in a quick reference format • Includes dosing information on: – Etomidate 0. 3 mg/kg IVP/IO – Fentanyl 0. 5 mcg/kg IN/IVP/IO – Lidocaine 1. 5 mg/kg IVP/IO (DAI) 78
 Drug Information List • Reference guide listing information on medications used in the Region X SOP’s – Information not all inclusive • Supplement to other drug reference material 79
Drug Information List • Reference guide listing information on medications used in the Region X SOP’s – Information not all inclusive • Supplement to other drug reference material 79
 Region X Drug Route Options • Lists routes appropriate for the list of medications used in the Region x SOP’s • Choice of drug route is based upon patient assessment at the time of need • If any question of the appropriateness of the route, Medical Control will be contacted and consulted • For ANY orders from Medical Control, the ECRN MUST consult with the ED MD 80
Region X Drug Route Options • Lists routes appropriate for the list of medications used in the Region x SOP’s • Choice of drug route is based upon patient assessment at the time of need • If any question of the appropriateness of the route, Medical Control will be contacted and consulted • For ANY orders from Medical Control, the ECRN MUST consult with the ED MD 80
 Region X SOP Medications • The following are medication guidelines • Each medication lists the SOP it is associated with – Currently, there are shortages for manufacturing of some medications – Note, substitutions may need to be considered 81
Region X SOP Medications • The following are medication guidelines • Each medication lists the SOP it is associated with – Currently, there are shortages for manufacturing of some medications – Note, substitutions may need to be considered 81
 Adenosine in Region X SOP’s (Adenocard) • To slow the ventricular response • Can be a diagnostic tool ~Adult stable SVT ~Adult stable monomorphic Ventricular Tachycardia ~Pediatric Tachycardia with Adequate Perfusion (probable stable SVT or stable VT) ~Pediatric Tachycardia with Poor Perfusion – probable SVT 82
Adenosine in Region X SOP’s (Adenocard) • To slow the ventricular response • Can be a diagnostic tool ~Adult stable SVT ~Adult stable monomorphic Ventricular Tachycardia ~Pediatric Tachycardia with Adequate Perfusion (probable stable SVT or stable VT) ~Pediatric Tachycardia with Poor Perfusion – probable SVT 82
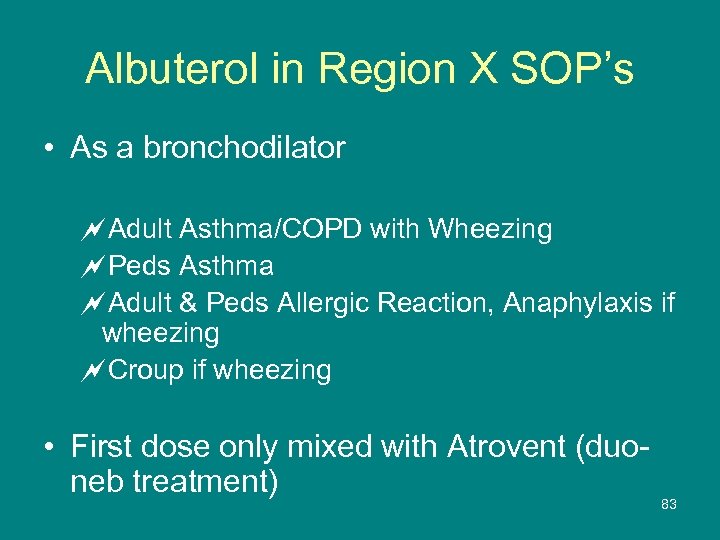 Albuterol in Region X SOP’s • As a bronchodilator ~Adult Asthma/COPD with Wheezing ~Peds Asthma ~Adult & Peds Allergic Reaction, Anaphylaxis if wheezing ~Croup if wheezing • First dose only mixed with Atrovent (duoneb treatment) 83
Albuterol in Region X SOP’s • As a bronchodilator ~Adult Asthma/COPD with Wheezing ~Peds Asthma ~Adult & Peds Allergic Reaction, Anaphylaxis if wheezing ~Croup if wheezing • First dose only mixed with Atrovent (duoneb treatment) 83
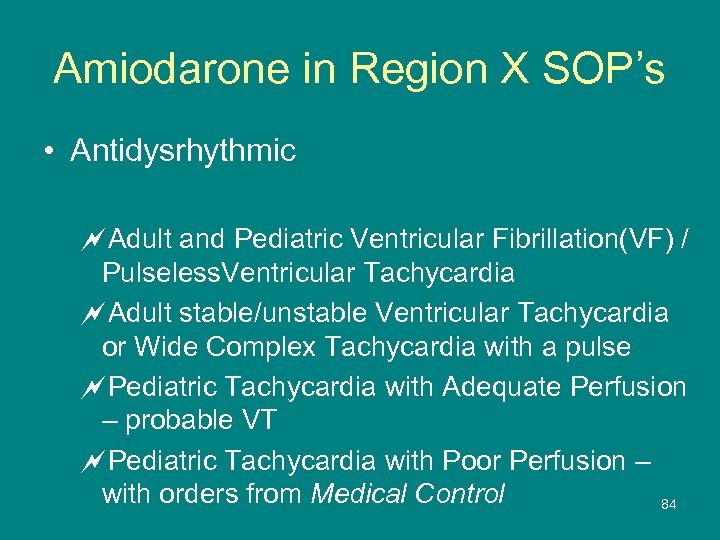 Amiodarone in Region X SOP’s • Antidysrhythmic ~Adult and Pediatric Ventricular Fibrillation(VF) / Pulseless. Ventricular Tachycardia ~Adult stable/unstable Ventricular Tachycardia or Wide Complex Tachycardia with a pulse ~Pediatric Tachycardia with Adequate Perfusion – probable VT ~Pediatric Tachycardia with Poor Perfusion – with orders from Medical Control 84
Amiodarone in Region X SOP’s • Antidysrhythmic ~Adult and Pediatric Ventricular Fibrillation(VF) / Pulseless. Ventricular Tachycardia ~Adult stable/unstable Ventricular Tachycardia or Wide Complex Tachycardia with a pulse ~Pediatric Tachycardia with Adequate Perfusion – probable VT ~Pediatric Tachycardia with Poor Perfusion – with orders from Medical Control 84
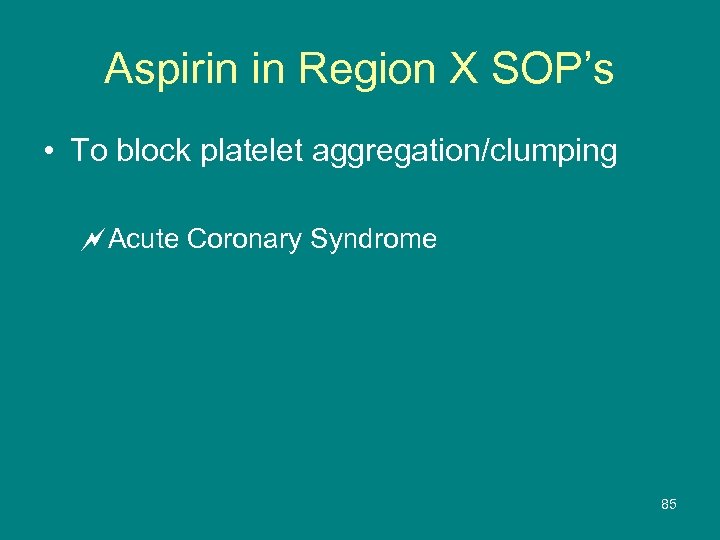 Aspirin in Region X SOP’s • To block platelet aggregation/clumping ~Acute Coronary Syndrome 85
Aspirin in Region X SOP’s • To block platelet aggregation/clumping ~Acute Coronary Syndrome 85
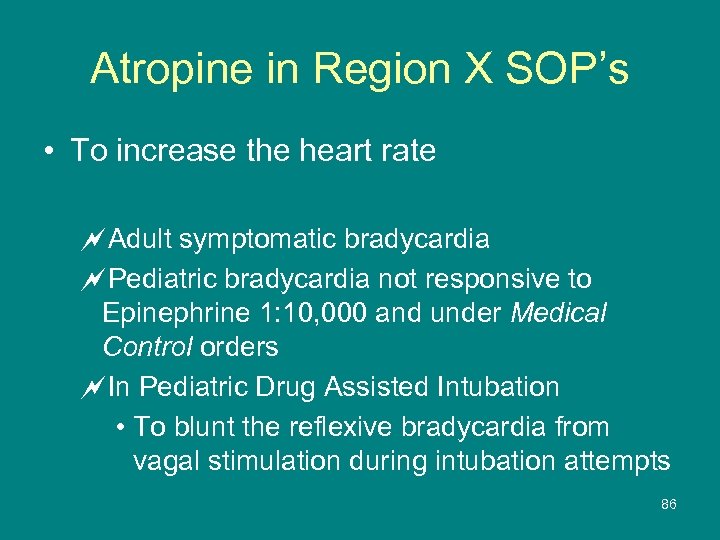 Atropine in Region X SOP’s • To increase the heart rate ~Adult symptomatic bradycardia ~Pediatric bradycardia not responsive to Epinephrine 1: 10, 000 and under Medical Control orders ~In Pediatric Drug Assisted Intubation • To blunt the reflexive bradycardia from vagal stimulation during intubation attempts 86
Atropine in Region X SOP’s • To increase the heart rate ~Adult symptomatic bradycardia ~Pediatric bradycardia not responsive to Epinephrine 1: 10, 000 and under Medical Control orders ~In Pediatric Drug Assisted Intubation • To blunt the reflexive bradycardia from vagal stimulation during intubation attempts 86
 Atrovent® in Region X SOP’s (Ipratropium Bromide) • Ih-prah-trow-pea-um • Bronchodilator, to reduce bronchospasm – Dries secretions • Mixed with first dose Albuterol only ~Adult Asthma/COPD with Wheezing ~Pediatric Asthma ~Adult and Pediatric Allergic Reaction / Anaphylaxis if wheezing ~Croup if wheezing 87
Atrovent® in Region X SOP’s (Ipratropium Bromide) • Ih-prah-trow-pea-um • Bronchodilator, to reduce bronchospasm – Dries secretions • Mixed with first dose Albuterol only ~Adult Asthma/COPD with Wheezing ~Pediatric Asthma ~Adult and Pediatric Allergic Reaction / Anaphylaxis if wheezing ~Croup if wheezing 87
 Benadryl in Region X SOP’s (Diphenhydramine) • Antihistamine to stop the release of histamines and stop the resultant signs and symptoms that occur ~Adult and Pediatric Allergic Reaction and Anaphylaxis 88
Benadryl in Region X SOP’s (Diphenhydramine) • Antihistamine to stop the release of histamines and stop the resultant signs and symptoms that occur ~Adult and Pediatric Allergic Reaction and Anaphylaxis 88
 Dextrose in Region X SOP’s • To replace low sugar levels ~Adult and Pediatric Altered Mental Status if blood sugar <60 ~Stroke if blood sugar <60 ~Diabetic Emergencies if blood sugar <60 ~Adult and Pediatric Seizures if blood sugar <60 ~Head Injuries if blood sugar <60 89
Dextrose in Region X SOP’s • To replace low sugar levels ~Adult and Pediatric Altered Mental Status if blood sugar <60 ~Stroke if blood sugar <60 ~Diabetic Emergencies if blood sugar <60 ~Adult and Pediatric Seizures if blood sugar <60 ~Head Injuries if blood sugar <60 89
 Dopamine in Region X SOP’s • To support failing blood pressures by improving contractility ~Adult Bradycardia when Atropine ineffective ~Cardiogenic Shock 90
Dopamine in Region X SOP’s • To support failing blood pressures by improving contractility ~Adult Bradycardia when Atropine ineffective ~Cardiogenic Shock 90
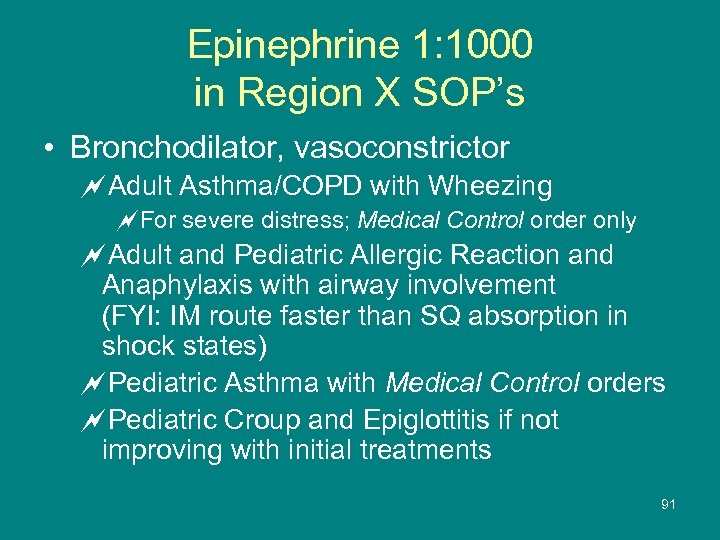 Epinephrine 1: 1000 in Region X SOP’s • Bronchodilator, vasoconstrictor ~Adult Asthma/COPD with Wheezing ~For severe distress; Medical Control order only ~Adult and Pediatric Allergic Reaction and Anaphylaxis with airway involvement (FYI: IM route faster than SQ absorption in shock states) ~Pediatric Asthma with Medical Control orders ~Pediatric Croup and Epiglottitis if not improving with initial treatments 91
Epinephrine 1: 1000 in Region X SOP’s • Bronchodilator, vasoconstrictor ~Adult Asthma/COPD with Wheezing ~For severe distress; Medical Control order only ~Adult and Pediatric Allergic Reaction and Anaphylaxis with airway involvement (FYI: IM route faster than SQ absorption in shock states) ~Pediatric Asthma with Medical Control orders ~Pediatric Croup and Epiglottitis if not improving with initial treatments 91
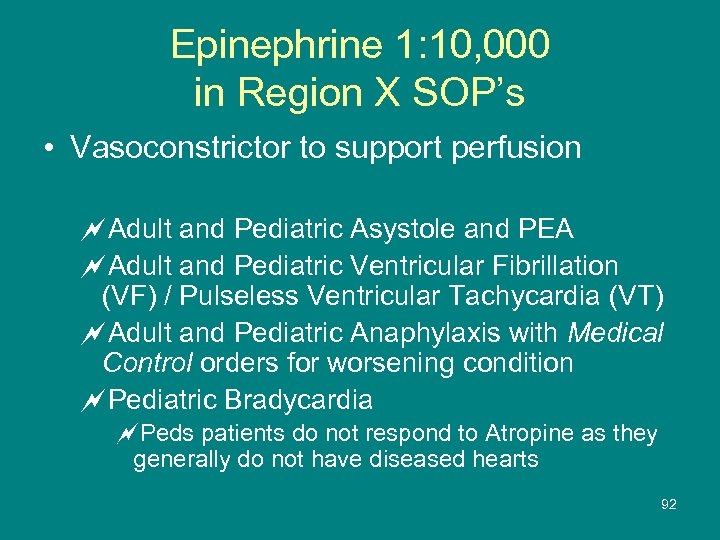 Epinephrine 1: 10, 000 in Region X SOP’s • Vasoconstrictor to support perfusion ~Adult and Pediatric Asystole and PEA ~Adult and Pediatric Ventricular Fibrillation (VF) / Pulseless Ventricular Tachycardia (VT) ~Adult and Pediatric Anaphylaxis with Medical Control orders for worsening condition ~Pediatric Bradycardia ~Peds patients do not respond to Atropine as they generally do not have diseased hearts 92
Epinephrine 1: 10, 000 in Region X SOP’s • Vasoconstrictor to support perfusion ~Adult and Pediatric Asystole and PEA ~Adult and Pediatric Ventricular Fibrillation (VF) / Pulseless Ventricular Tachycardia (VT) ~Adult and Pediatric Anaphylaxis with Medical Control orders for worsening condition ~Pediatric Bradycardia ~Peds patients do not respond to Atropine as they generally do not have diseased hearts 92
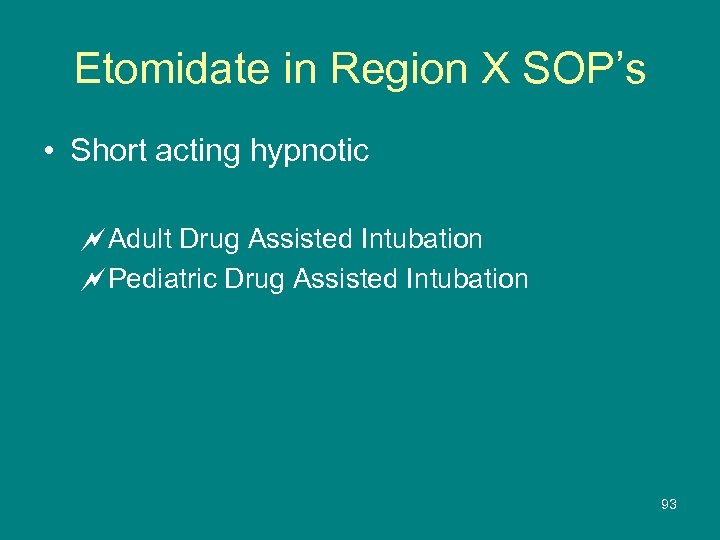 Etomidate in Region X SOP’s • Short acting hypnotic ~Adult Drug Assisted Intubation ~Pediatric Drug Assisted Intubation 93
Etomidate in Region X SOP’s • Short acting hypnotic ~Adult Drug Assisted Intubation ~Pediatric Drug Assisted Intubation 93
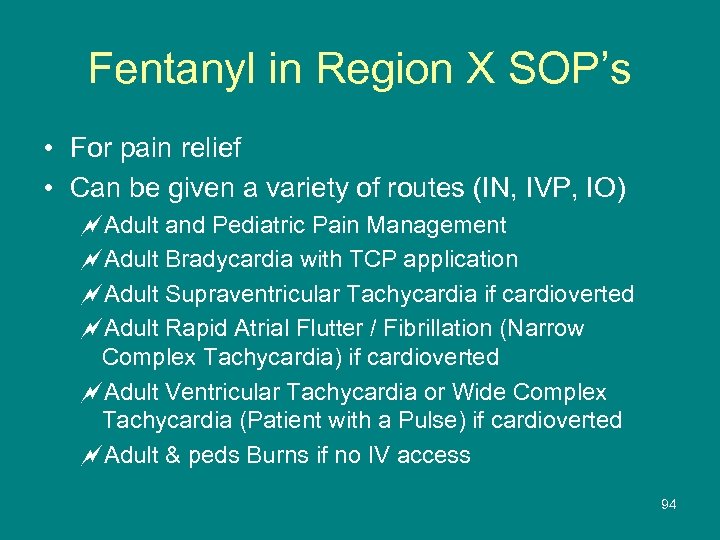 Fentanyl in Region X SOP’s • For pain relief • Can be given a variety of routes (IN, IVP, IO) ~Adult and Pediatric Pain Management ~Adult Bradycardia with TCP application ~Adult Supraventricular Tachycardia if cardioverted ~Adult Rapid Atrial Flutter / Fibrillation (Narrow Complex Tachycardia) if cardioverted ~Adult Ventricular Tachycardia or Wide Complex Tachycardia (Patient with a Pulse) if cardioverted ~Adult & peds Burns if no IV access 94
Fentanyl in Region X SOP’s • For pain relief • Can be given a variety of routes (IN, IVP, IO) ~Adult and Pediatric Pain Management ~Adult Bradycardia with TCP application ~Adult Supraventricular Tachycardia if cardioverted ~Adult Rapid Atrial Flutter / Fibrillation (Narrow Complex Tachycardia) if cardioverted ~Adult Ventricular Tachycardia or Wide Complex Tachycardia (Patient with a Pulse) if cardioverted ~Adult & peds Burns if no IV access 94
 Glucagon in Region X SOP’s • Hormone to stimulate the release of sugar stores (is not a sugar) ~Adult and Pediatric Altered Mental Status if no IV access and blood sugar <60 ~Stroke if no IV access and blood sugar <60 ~Diabetic if no IV access and blood sugar <60 ~Adult and Pediatric Seizures if no IV access and blood sugar <60 ~Head Injury if no IV access and blood sugar <60 95
Glucagon in Region X SOP’s • Hormone to stimulate the release of sugar stores (is not a sugar) ~Adult and Pediatric Altered Mental Status if no IV access and blood sugar <60 ~Stroke if no IV access and blood sugar <60 ~Diabetic if no IV access and blood sugar <60 ~Adult and Pediatric Seizures if no IV access and blood sugar <60 ~Head Injury if no IV access and blood sugar <60 95
 Lasix in Region X SOP’s • Diuretic ~Pulmonary Edema ~Hypertensive Emergency 96
Lasix in Region X SOP’s • Diuretic ~Pulmonary Edema ~Hypertensive Emergency 96
 Lidocaine in Region X SOP’s • To blunt the cough reflex to prevent an increase in intracranial pressure during intubation ~Adult Drug Assisted Intubation ~Pediatric Drug Assisted Intubation • For pain relief during infusion of fluids via IO sites ~Adult EZ IO insertion ~Pediatric EZ IO insertion 97
Lidocaine in Region X SOP’s • To blunt the cough reflex to prevent an increase in intracranial pressure during intubation ~Adult Drug Assisted Intubation ~Pediatric Drug Assisted Intubation • For pain relief during infusion of fluids via IO sites ~Adult EZ IO insertion ~Pediatric EZ IO insertion 97
 Morphine in Region X SOP’s • Opioid, narcotic, pain relief, reduces preload via vasodilation ~Acute Coronary Syndrome ~Pulmonary Edema ~Adult and Pediatric Burns if IV access available 98
Morphine in Region X SOP’s • Opioid, narcotic, pain relief, reduces preload via vasodilation ~Acute Coronary Syndrome ~Pulmonary Edema ~Adult and Pediatric Burns if IV access available 98
 Narcan in Region X SOP’s (Naloxone) • Narcotic antagonist to reverse respiratory depression ~Adult and Pediatric Altered Mental Status ~Adult and Pediatric Pain Management if respiratory depression occurs following Fentanyl 99
Narcan in Region X SOP’s (Naloxone) • Narcotic antagonist to reverse respiratory depression ~Adult and Pediatric Altered Mental Status ~Adult and Pediatric Pain Management if respiratory depression occurs following Fentanyl 99
 Nitroglycerin in Region X SOP’s • Venodilator to reduce the preload and reduce the work load of the heart ~Acute Coronary syndrome ~Pulmonary Edema ~Hypertension Emergency with orders from Medical Control 100
Nitroglycerin in Region X SOP’s • Venodilator to reduce the preload and reduce the work load of the heart ~Acute Coronary syndrome ~Pulmonary Edema ~Hypertension Emergency with orders from Medical Control 100
 Valium in Region X SOP’s (Diazepam) • Benzodiazepine • Relax the patient, reduce anxiety, amnesic ~Adult Bradycardia when the TCP is used ~Adult and Pediatric Heat Emergencies if the patient begins to shiver during the cooling process ~Behavioral Emergencies – if additional sedation required after Versed 101
Valium in Region X SOP’s (Diazepam) • Benzodiazepine • Relax the patient, reduce anxiety, amnesic ~Adult Bradycardia when the TCP is used ~Adult and Pediatric Heat Emergencies if the patient begins to shiver during the cooling process ~Behavioral Emergencies – if additional sedation required after Versed 101
 Verapamil in Region X SOP’s • To slow down rapid atrial fibrillation and flutter ~Adult Supraventricular Tachycardia (Narrow Complex Tachycardia (SVT) - stable ~Adult Rapid Atrial Flutter / Fibrillation (Narrow Complex Tachycardia) - stable 102
Verapamil in Region X SOP’s • To slow down rapid atrial fibrillation and flutter ~Adult Supraventricular Tachycardia (Narrow Complex Tachycardia (SVT) - stable ~Adult Rapid Atrial Flutter / Fibrillation (Narrow Complex Tachycardia) - stable 102
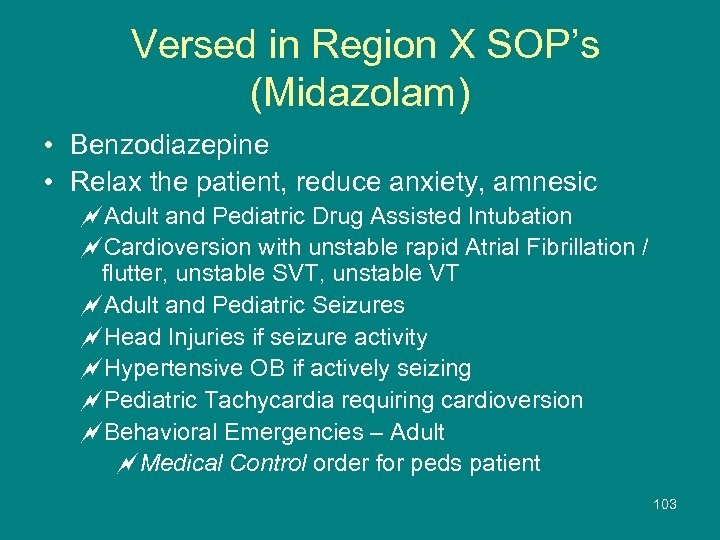 Versed in Region X SOP’s (Midazolam) • Benzodiazepine • Relax the patient, reduce anxiety, amnesic ~Adult and Pediatric Drug Assisted Intubation ~Cardioversion with unstable rapid Atrial Fibrillation / flutter, unstable SVT, unstable VT ~Adult and Pediatric Seizures ~Head Injuries if seizure activity ~Hypertensive OB if actively seizing ~Pediatric Tachycardia requiring cardioversion ~Behavioral Emergencies – Adult ~Medical Control order for peds patient 103
Versed in Region X SOP’s (Midazolam) • Benzodiazepine • Relax the patient, reduce anxiety, amnesic ~Adult and Pediatric Drug Assisted Intubation ~Cardioversion with unstable rapid Atrial Fibrillation / flutter, unstable SVT, unstable VT ~Adult and Pediatric Seizures ~Head Injuries if seizure activity ~Hypertensive OB if actively seizing ~Pediatric Tachycardia requiring cardioversion ~Behavioral Emergencies – Adult ~Medical Control order for peds patient 103
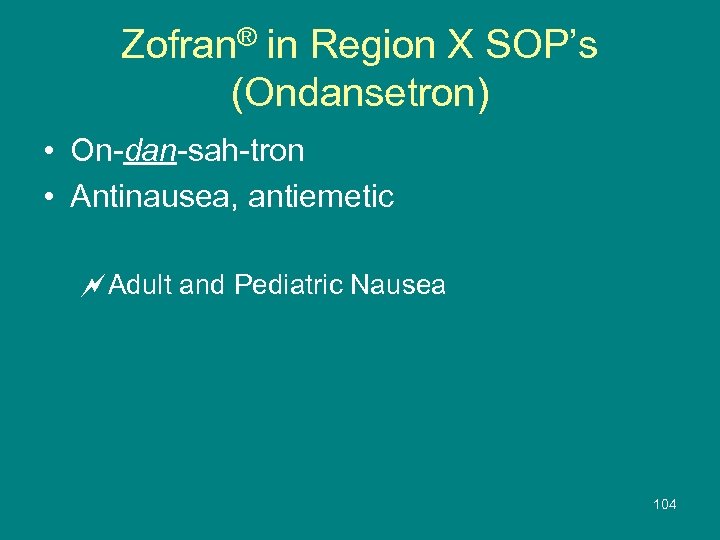 Zofran® in Region X SOP’s (Ondansetron) • On-dan-sah-tron • Antinausea, antiemetic ~Adult and Pediatric Nausea 104
Zofran® in Region X SOP’s (Ondansetron) • On-dan-sah-tron • Antinausea, antiemetic ~Adult and Pediatric Nausea 104
 Case Scenario Practice • Read the cases • Determine the appropriate ECRN response • Click on the slide / press “page down” and the answer will appear
Case Scenario Practice • Read the cases • Determine the appropriate ECRN response • Click on the slide / press “page down” and the answer will appear
 Case Scenario #1 • EMS arrives to the ED with a patient that has been intubated • Report did not indicate any trauma • Why would the patient have a cervical collar in place? – Applying a cervical collar after intubation minimizes neck movement – The distal tip of the ETT is less likely to slip out of place if a cervical collar is applied along with the usual methods of securing the airway in place
Case Scenario #1 • EMS arrives to the ED with a patient that has been intubated • Report did not indicate any trauma • Why would the patient have a cervical collar in place? – Applying a cervical collar after intubation minimizes neck movement – The distal tip of the ETT is less likely to slip out of place if a cervical collar is applied along with the usual methods of securing the airway in place
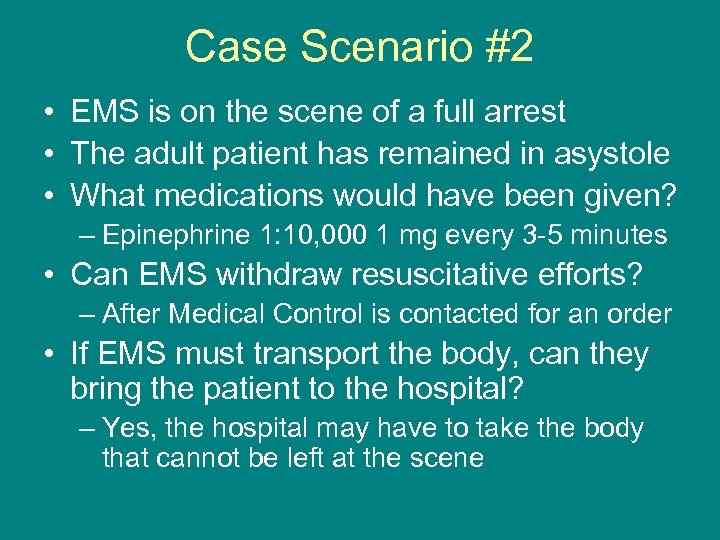 Case Scenario #2 • EMS is on the scene of a full arrest • The adult patient has remained in asystole • What medications would have been given? – Epinephrine 1: 10, 000 1 mg every 3 -5 minutes • Can EMS withdraw resuscitative efforts? – After Medical Control is contacted for an order • If EMS must transport the body, can they bring the patient to the hospital? – Yes, the hospital may have to take the body that cannot be left at the scene
Case Scenario #2 • EMS is on the scene of a full arrest • The adult patient has remained in asystole • What medications would have been given? – Epinephrine 1: 10, 000 1 mg every 3 -5 minutes • Can EMS withdraw resuscitative efforts? – After Medical Control is contacted for an order • If EMS must transport the body, can they bring the patient to the hospital? – Yes, the hospital may have to take the body that cannot be left at the scene
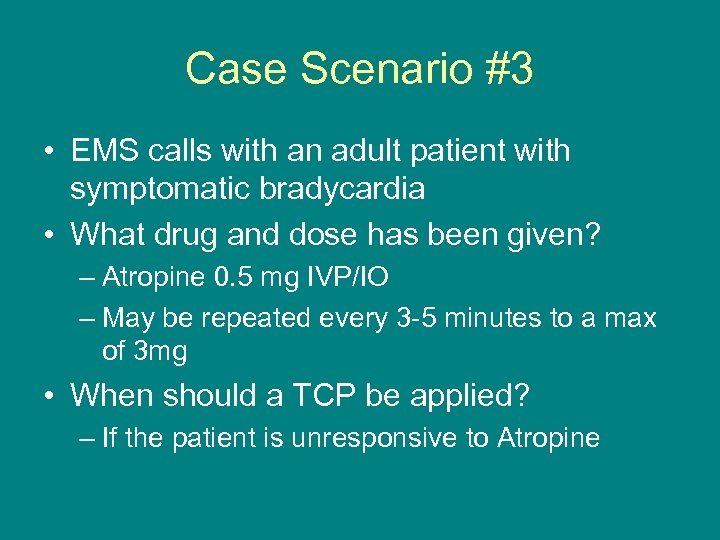 Case Scenario #3 • EMS calls with an adult patient with symptomatic bradycardia • What drug and dose has been given? – Atropine 0. 5 mg IVP/IO – May be repeated every 3 -5 minutes to a max of 3 mg • When should a TCP be applied? – If the patient is unresponsive to Atropine
Case Scenario #3 • EMS calls with an adult patient with symptomatic bradycardia • What drug and dose has been given? – Atropine 0. 5 mg IVP/IO – May be repeated every 3 -5 minutes to a max of 3 mg • When should a TCP be applied? – If the patient is unresponsive to Atropine
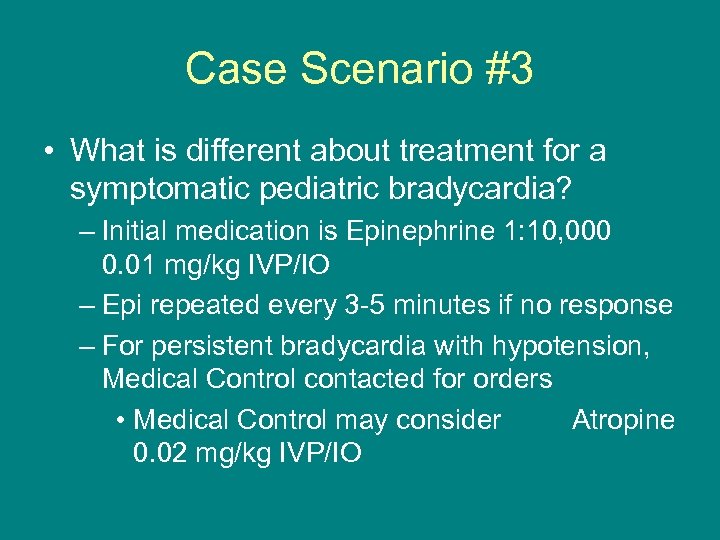 Case Scenario #3 • What is different about treatment for a symptomatic pediatric bradycardia? – Initial medication is Epinephrine 1: 10, 000 0. 01 mg/kg IVP/IO – Epi repeated every 3 -5 minutes if no response – For persistent bradycardia with hypotension, Medical Control contacted for orders • Medical Control may consider Atropine 0. 02 mg/kg IVP/IO
Case Scenario #3 • What is different about treatment for a symptomatic pediatric bradycardia? – Initial medication is Epinephrine 1: 10, 000 0. 01 mg/kg IVP/IO – Epi repeated every 3 -5 minutes if no response – For persistent bradycardia with hypotension, Medical Control contacted for orders • Medical Control may consider Atropine 0. 02 mg/kg IVP/IO
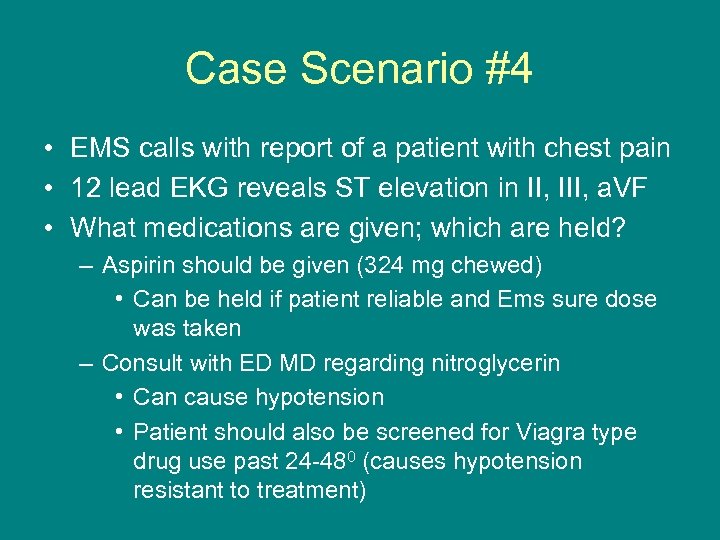 Case Scenario #4 • EMS calls with report of a patient with chest pain • 12 lead EKG reveals ST elevation in II, III, a. VF • What medications are given; which are held? – Aspirin should be given (324 mg chewed) • Can be held if patient reliable and Ems sure dose was taken – Consult with ED MD regarding nitroglycerin • Can cause hypotension • Patient should also be screened for Viagra type drug use past 24 -480 (causes hypotension resistant to treatment)
Case Scenario #4 • EMS calls with report of a patient with chest pain • 12 lead EKG reveals ST elevation in II, III, a. VF • What medications are given; which are held? – Aspirin should be given (324 mg chewed) • Can be held if patient reliable and Ems sure dose was taken – Consult with ED MD regarding nitroglycerin • Can cause hypotension • Patient should also be screened for Viagra type drug use past 24 -480 (causes hypotension resistant to treatment)
 Case Scenario #5 • When would EMS begin to cool a patient who had been worked as an arrest? – Patient suffered a cardiac arrest (not respiratory arrest) – After the patient has pulses for at least 5 minutes – Blood pressure maintained >90 systolic – Patient remains unresponsive
Case Scenario #5 • When would EMS begin to cool a patient who had been worked as an arrest? – Patient suffered a cardiac arrest (not respiratory arrest) – After the patient has pulses for at least 5 minutes – Blood pressure maintained >90 systolic – Patient remains unresponsive
 Case Scenario #6 • How can Fentanyl be administered for Region X EMS? ü IN via MAD ü IVP ü IO • What are additional/alternative methods to address pain control? ü Positioning ü Immobilization ü Elevation ü Ice ü Distraction
Case Scenario #6 • How can Fentanyl be administered for Region X EMS? ü IN via MAD ü IVP ü IO • What are additional/alternative methods to address pain control? ü Positioning ü Immobilization ü Elevation ü Ice ü Distraction
 Case Scenario #7 • EMS is on the scene of a patient in pulmonary edema • What treatment/medications are you anticipating have been given if the patient is relatively stable? – Nitroglycerin repeated every 5 minutes x 3 – CPAP started after first NTG given – Lasix 40 mg IVP (80 mg if on med at home) – Morphine 2 mg IVP; repeated every 2 minutes to max of 10 mg if B/P remains >90
Case Scenario #7 • EMS is on the scene of a patient in pulmonary edema • What treatment/medications are you anticipating have been given if the patient is relatively stable? – Nitroglycerin repeated every 5 minutes x 3 – CPAP started after first NTG given – Lasix 40 mg IVP (80 mg if on med at home) – Morphine 2 mg IVP; repeated every 2 minutes to max of 10 mg if B/P remains >90
 Case Scenario #8 • EMS calls with a patient from a minor MVC • The 15 year-old female wants to sign a release; she has no complaints/injuries – This patient is pregnant – Can she sign a release/refusal? • Yes, she is emancipated due to the pregnancy • If she remains the parent after delivery, she remains emancipated regardless of where she is living
Case Scenario #8 • EMS calls with a patient from a minor MVC • The 15 year-old female wants to sign a release; she has no complaints/injuries – This patient is pregnant – Can she sign a release/refusal? • Yes, she is emancipated due to the pregnancy • If she remains the parent after delivery, she remains emancipated regardless of where she is living
 Case Scenario #9 • EMS calls for a conscious, alert, cooperative patient who refuses transport • The patient’s Durable Power of Attorney for Healthcare is also present – The DPOA wants the patient transported • Who gets to speak for the patient? – The DPOA gets to speak when the patient is no longer able to speak for themselves • Follow the wishes of the patient at this point
Case Scenario #9 • EMS calls for a conscious, alert, cooperative patient who refuses transport • The patient’s Durable Power of Attorney for Healthcare is also present – The DPOA wants the patient transported • Who gets to speak for the patient? – The DPOA gets to speak when the patient is no longer able to speak for themselves • Follow the wishes of the patient at this point
 Case Scenario #10 • EMS calls from the scene for an imminent delivery • If report includes a non-delivered breech birth or a prolapsed cord, what specific information do you want to hear in report? – Confirm that someone has fingers inserted into the vagina during transport • For a stuck breech, create an airway for the infant • For a prolapsed cord, push against the presenting part to allow blood flow through the cord
Case Scenario #10 • EMS calls from the scene for an imminent delivery • If report includes a non-delivered breech birth or a prolapsed cord, what specific information do you want to hear in report? – Confirm that someone has fingers inserted into the vagina during transport • For a stuck breech, create an airway for the infant • For a prolapsed cord, push against the presenting part to allow blood flow through the cord
 Case Scenario #11 • In what circumstances would the King airway be used? – Difficult/challenging intubation • 2 failed attempts via endotracheal tube (ETT) • Poor visibility of anatomy • Short, thick necks • SOP skill reference: – “Cardiac or respiratory arrest, unresponsive medical or trauma patient without a gag reflex in which endotracheal intubation is unable to be established. ”
Case Scenario #11 • In what circumstances would the King airway be used? – Difficult/challenging intubation • 2 failed attempts via endotracheal tube (ETT) • Poor visibility of anatomy • Short, thick necks • SOP skill reference: – “Cardiac or respiratory arrest, unresponsive medical or trauma patient without a gag reflex in which endotracheal intubation is unable to be established. ”
 Case Scenario #12 • In which cases is EMS mandated reporters? – Suspected child abuse – If release signed, then domestic violence reported to local police • Local community informational brochure to be offered to patient that signs a release – Suspected elder abuse/neglect
Case Scenario #12 • In which cases is EMS mandated reporters? – Suspected child abuse – If release signed, then domestic violence reported to local police • Local community informational brochure to be offered to patient that signs a release – Suspected elder abuse/neglect
 Bibliography • 2010 American Heart Association Guidelines for CPR and ECC • ITLS 6 th Edition • Illinois Emergency Medical Services for Children. Pediatric Prehospital Protocols. January 2008. • Region X EMS Standard Operating Procedures 2011 Teaching Document • CMC EMS System November 2011 CE • CMC EMS System October 2011 CE • CMC EMS System September 2011 CE • www. Kiingsystems. com/wpcontact/uploads/2010/09/INFM-63 -KLTSS. pdf • www. Wong. Baker. FACES. org 119
Bibliography • 2010 American Heart Association Guidelines for CPR and ECC • ITLS 6 th Edition • Illinois Emergency Medical Services for Children. Pediatric Prehospital Protocols. January 2008. • Region X EMS Standard Operating Procedures 2011 Teaching Document • CMC EMS System November 2011 CE • CMC EMS System October 2011 CE • CMC EMS System September 2011 CE • www. Kiingsystems. com/wpcontact/uploads/2010/09/INFM-63 -KLTSS. pdf • www. Wong. Baker. FACES. org 119


