df3c1201e9ce5b9fb0b626aeca98e3da.ppt
- Количество слайдов: 30
Reducing the Medicalization of Maternal and Newborn Care August 2013
Session Objectives The objectives of this session are to: § Introduce the concept of “medicalized” care § Provide examples of maternal and newborn health (MNH) care practices that may be harmful or life-saving § Provide examples of MNH care practices that are harmful § Provide evidence to support the harmfulness of these examples 2
What is Medicalized MNH Care? The routine use of practices during labor and childbirth that: § Are not evidence-based § Are unnecessary or unwarranted § Do not improve the health outcomes for mother or baby and may do harm § Prioritize needs of providers over needs of women § Encourage technology or interventions without proven benefit 3
Symbols of a Medicalized Model: Technology § The body as a machine § Separation between the body and the mind § Pregnancy is a medical condition that needs to be controlled 4
Symbols of a Medicalized Model: Centered on the Professional Care Giver § Centered on the provider’s needs and preferences: § Ease § Speed § Comfort § Habit/Tradition § Results in woman’s discomfort and disempowerment 5

Symbols of a Medicalized Model: Woman without Companion 6
Symbols of a Medicalized Model: Family Unit Separated During Labor & Delivery 7
Practices that May Be Harmful or Life-Saving § § § Induction or augmentation of labor Cesarean section Episiotomy Restricting food and fluids Electronic fetal monitoring Oro-pharnygeal suctioning of newborn 8
Practices That Are Harmful § Restricting ambulation/different positions during labor and choice of birth position § Lack of companion/family during labor § Over-use of anesthesia/analgesia § Separation of mother and baby § Early cord clamping § Routine enema and/or perineal shaving 9
Unnecessary/Uncontrolled Labor Induction & Augmentation Labor induction has been associated with: § More maternal interventions (epidural analgesia and cesarean section) § Increased PPH § Longer length of stay § Higher likelihood of non-reassuring fetal heart rate tracings; need for neonatal resuscitation (Glantz 2010, 2012) 10
Unnecessary /Unsafe Cesarean Sections § WHO standard is 5 -15% of all deliveries § Data from 137 countries: 54 countries had CS rates of ˂10%; 69 countries showed rates of ≥ 15% § Global saving by reduction of CS rates to 15% was ±$2. 32 billion; the cost to attain 10% CS rate was $432 million. Overuse of global resources 11 (Gibbons 2012)
Unnecessary /Unsafe Cesarean Sections (cont. ) § Increasingly indications are subjective and non-clinical § May be performed without adequate anesthesia/access to blood § Data for 106, 546 births found rate of CS delivery was positively associated with: § Postpartum antibiotic treatment § Severe maternal morbidity and mortality § Increase in perinatal mortality rates § Increase in babies admitted to neonatal intensive care § Rates of preterm delivery and neonatal mortality both rose at rates of C-S between 10% and 20% (Haberman 2013; Shah 2009; Boyle 2012; Villar 2006) 12
Unnecessary /Unsafe Cesarean Sections (cont. ) § Detrimental to births following C-section § Study: 10, 684 women – 2, 680 had prior C-S; 7, 974 had prior vaginal birth § Patients having a prior C-S: • Had more than a 2. 5 -fold risk of requiring blood transfusion • Had nearly a 4 -fold higher risk of admission to the ICU • Were 1. 5 times more likely to be readmitted to the hospital than those with a prior vaginal birth (Galyean 2009) § Future pregnancies and births need special care 13
Unnecessary/Routine Episiotomies § Episiotomies can reduce maternal and neonatal morbidity if they are restricted to evidence-based indications § RCT of 2, 606 births in 8 maternities found: § Anterior perineal trauma more common in the selective group § Severe perineal trauma, perineal pain, healing complications, and wound dehiscence were all less frequent in the selective group § In another study 14. 3% of routine group had third- or fourth -degree perineal lacerations, compared to 6. 8% in selective group (RR, 2. 12; 95% confidence interval, 1. 18 -3. 81) (Rodriquez 2008) 14
Restricting Food or Fluids in Labor § Unproven fear of aspiration if oral intake allowed § Allowing self-regulated intake of oral hydration and nutrition has been shown to help prevent ketosis and dehydration, and to reduce stress levels § Cochrane review (3, 130 women) found no justification for restricting oral fluid or food during labor (Bulletin of ACNM 2008; Singata 2012) 15
Restricting Ambulation & Choice of Birth Position § Little data to show significant effect of positions on birth outcomes § Choice of labor and birth positions encourages a woman’s sense of control and reduces need for analgesia 16
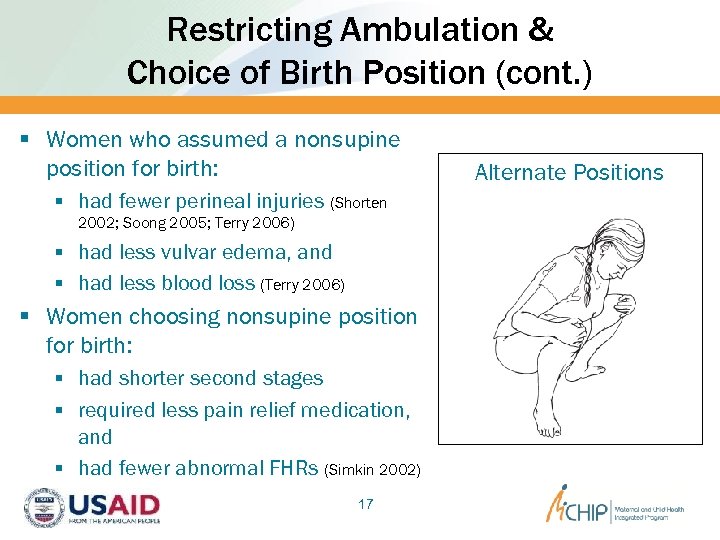
Restricting Ambulation & Choice of Birth Position (cont. ) § Women who assumed a nonsupine position for birth: § had fewer perineal injuries (Shorten 2002; Soong 2005; Terry 2006) § had less vulvar edema, and § had less blood loss (Terry 2006) § Women choosing nonsupine position for birth: § had shorter second stages § required less pain relief medication, and § had fewer abnormal FHRs (Simkin 2002) 17 Alternate Positions
Unnecessary Electronic Fetal Monitoring (EFM) Issues associated with using EFM: § Technology, maintenance and costs § Training – how to use, how to interpret Ø High inter- and intra-observer variability in interpretation of FHR tracing (ACOG 2009) § Lack of proven benefit of continuous EFM over intermittent auscultation in low-risk pregnancy (Cochrane 2013; ACOG 2009) § May restrict ambulation and positions during labor 18
Unnecessary EFM (cont. ) Continuous EFM vs. intermittent auscultation associated with: § Increased rates of operative delivery (C-S, vacuum) Ø With resulting increased risks to mother § Reduction in neonatal seizures by 50%, but…. § No reduction in neonatal death, cerebral palsy, other significant neonatal morbidity (Cochrane 2013; ACOG 2009) 19
Over-Use of Anesthesia/Analgesia § Epidural/Intrathecal anesthesia is associated with increased rates of transient fetal heart rate abnormalities (even higher when intrathecal opioids/narcotics used) § Newborns of women who receive intrathecal opioids/narcotics experience more difficulties initiating breastfeeding (Beilin 2005; Jordan 2005; Lieberman 2002; Mardirosoff 2002; Radzyminski 2003, 2005) 20
Over-Use of Anesthesia/Analgesia (cont. ) Compared with women using no pain medication or exclusively opioid pain medication during labor, women having epidurals have increased risk for: § Longer first-stage labor (Alexander 2002; Lieberman 2002; Sharma 2004) § Longer second-stage labor (Alexander 2002; Anim-Somuah 2006; Feinstein 2002; Lieberman 2002; Liu 2004; Sharma 2004) § Third- and fourth-degree tears associated with the increased incidence of instrumental vaginal deliveries (Lieberman 2002) § Fetal distress (Anim-Somuah 2006; Liu 2004) 21
Separation of Mother & Baby § Eliminating or minimizing separation for procedures whenever possible reduces distress in healthy infants and mothers (Anderson 2003; Gray 2000; Klaus 1998) § Minimizing separation during the hospital stay increases breastfeeding initiation and duration in mothers with healthy infants (Anderson 2003; Klaus 1998) 22
Separation of Mother & Baby (cont. ) § Touching, holding, and caring for healthy, sick or premature infants or infants with congenital problems enhances attachment between mothers and babies (Charpak 2001; Di. Matteo 1996; Feldman 1999; Klaus 1998; Rowe-Murray 2001; Schroeder 2006; Tessier 1998) § Eliminating or minimizing separation for procedures whenever possible reduces distress in sick or premature infants, infants with congenital problems, and mothers (Feldman 1999; Klaus 1998) 23
Unnecessary Suctioning of Newborn Literature search of 41 articles found no benefit from routine suctioning § Search found suctioning was associated with: § Perturbations in heart rate § Apnea § Delays in achieving normal oxygen saturations § Based on currently available literature, routine suctioning is more likely to cause harm than good (Velaphi 2008) 24
Early Cord Clamping: Term Infant § Evidence has problems with definitions, i. e. “early” vs. “late” § In 11 trials of 2, 989 mothers and their babies, Cochrane review found: § No significant differences for PPH (CI 0. 96 to 1. 55) § Increased need in infants for phototherapy for jaundice (CI 0. 38 to 0. 92 in the late compared with early clamping group) § Increase in newborn hemoglobin levels in the late cord clamping group compared with early cord clamping (CI 0. 28 to 4. 06), although this effect did not persist past 6 months § Infant ferritin levels remained higher in the late clamping group than the early clamping group at 6 months (Mc. Donald 2008) 25
Early Cord Clamping: Premature Infants In premature infants, Cochrane review found that early (within seconds) vs. delayed (30 -180 seconds) was associated with: § Fewer infants requiring transfusions for anemia (RR 0. 61, 95% confidence interval (CI) 0. 46 to 0. 81) § Less intraventricular hemorrhage (RR 0. 59, 95% CI 0. 41 to 0. 85) § Lower risk for necrotising enterocolitis (RR 0. 62, 95% CI 0. 43 to 0. 90) compared with immediate clamping § Peak bilirubin concentration was higher for infants allocated to delayed cord clamping compared with immediate clamping (95% CI 5. 62 to 24. 40) (Rabe 2012) 26
Respectful Maternal & Newborn Care Respectful care demonstrates: § Respect for a woman’s rights, choices, and dignity § Care that “does no harm” § Care that promotes positive parenting and improves birth outcomes § Care that is culturally sensitive and valued by the woman and her community 27
Reversing the Trend: Partnership in Care § Aim to provide respectful maternity care – that is woman centered, empowering and supportive § Care which permits free communication and full expression of trust and commitment § Be careful with language – use ‘birth’ and not ‘delivery’ § Ensure all women are treated equitably 28
Campaign for ‘Normal Birth’: Top 10 Tips for Providers 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Wait and see Build her a nest Get her off the bed Justify intervention Listen to her Keep a diary Trust your intuition Be a role model Be Positive Promote skin-to-skin contact (http: //www. rcmnormalbirth. org. uk/practice/ten-top-tips) 29

WE ALL HAVE A ROLE IN ASSURING THAT WOMEN HAVE RESPECTFUL MATERNITY CARE! THANKS!
df3c1201e9ce5b9fb0b626aeca98e3da.ppt