RECURRENT MISCARRIAGE 2013. medical council.ppt
- Количество слайдов: 52

Recurrent Abortion, Causes and Management Dr. Mazen El-Zibdeh MD DRCPI, MRCOG, FRCOG Senior Consultant Ob. Gyn. Islamic Hospital Amman-Jordan Revised , February 2013

Recurrent Abortion consecutive pregnancies before the 20 th week of gestation. It affects 1% of all women. The theoretical risk of recurrent abortion is 0 -34% Causes of (RA) are numerous and in about 40 -50% of cases etiology may not be identified.
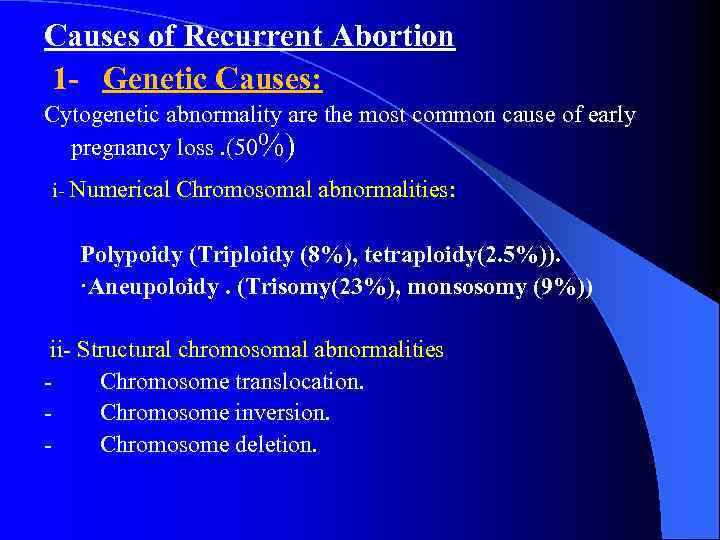
Causes of Recurrent Abortion 1 - Genetic Causes: Cytogenetic abnormality are the most common cause of early pregnancy loss. (50%) i- Numerical Chromosomal abnormalities: Polypoidy (Triploidy (8%), tetraploidy(2. 5%)). ·Aneupoloidy. (Trisomy(23%), monsosomy (9%)) ii- Structural chromosomal abnormalities - Chromosome translocation. - Chromosome inversion. - Chromosome deletion.

Genetic Factors and Recurrent Abortion Mechanism: * Transmission from a parent if the parent is a carrier - of structural abnormality. * From an error in cell division during meiosis or mitosis. 3 -5 % of couples with RPL have balanced translocation abnormalities.

Aneuploidy and Abortion l l l l Trisomy (one extra chromosome). Monosomy (one missing chromosome). Both may occur during meiotic and mitotic division. Results in zygote with either 45 chromosome or 47 chromosomes. Trisomy seen in > 50% of all chromosomally abnormal abortions. Monosomy seen in 9 -10% of all spontaneous abortion. Recurrent risk in abortions is 1. 5%.
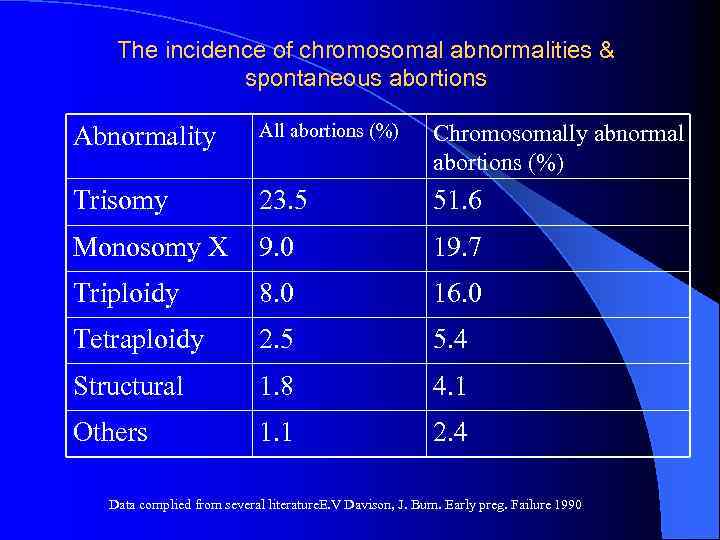
The incidence of chromosomal abnormalities & spontaneous abortions Abnormality All abortions (%) Chromosomally abnormal abortions (%) Trisomy 23. 5 51. 6 Monosomy X 9. 0 19. 7 Triploidy 8. 0 16. 0 Tetraploidy 2. 5 5. 4 Structural 1. 8 4. 1 Others 1. 1 2. 4 Data complied from several literature. E. V Davison, J. Burn. Early preg. Failure 1990
Cytogenetic assesment of couples with RM. Is useful : l to give prognosis of future pregnancy l To detect familial chromosomal problems l To apply appropriate pre-natal genetic diagnoses.
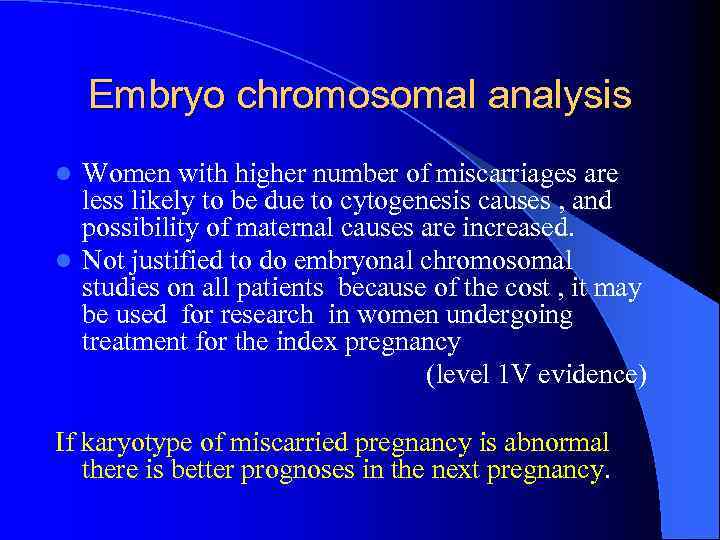
Embryo chromosomal analysis Women with higher number of miscarriages are less likely to be due to cytogenesis causes , and possibility of maternal causes are increased. l Not justified to do embryonal chromosomal studies on all patients because of the cost , it may be used for research in women undergoing treatment for the index pregnancy (level 1 V evidence) l If karyotype of miscarried pregnancy is abnormal there is better prognoses in the next pregnancy.
2 -Maternal Diseases and Abortion Severe acute maternal illness and sepsis discussed in sporadic and not in recurrent abortion. 1 - Lupus anticoagulant: Women with positive lupus AB. (1 g. G, 1 gm) Positive cardiolipin AB; (in 50%) Effect: Thrombo embolic process. Thrombo cytopenia. Placenta thrombosis.

2 Systemic lupus erthematosus (SLE) l 21% of patients with SLE will abort depending on activity and severity of the disease. l Low complement levels (C 3, C 4) and consumption of complement in the placenta.
Maternal disease & RPL (cont. ) 3. Diabetes mellitus No definite evidence that insulin dependent diabetes is associated with increased risk of abortion. 4. Thyroid dysfunction No clear evidence of hyperthyroidism as a cause of abortion. 5. Chronic gastrointestinal Disease: Crohn's dis ulcerative colitis only when disease is active. 6. Cong. Hypofibrinogenemia & factor eight deficiency 7. Endometriosis Increased level of PGF 2. 8. Sickle cell disease: ? due to micro infarction
3 - Maternal infections: Urea plasma, Mycoplasma, Listeria Chlamydia, Toxoplasma, Herpes, C. M. V.
Maternal Infection (Cont. ) l Most patients with R. A will not benefit from extensive infection work-up. l TORCH infection has limited evidences in relation to RPL. l Bacterial vaginoses : -Not certain as a cause of early miscarriage -First trimister +ve patient may have higher risk of mid trimister abortion and preterm labor. - Screening for BV is useful in women at risk to prevent mid trimister abortion and preterm labor l (evidence level 1 a)

4 -Anatomical uterine Defects and Recurrent Abortion Congenital uterine defects. l Acquired uterine defects. Effects on pregnancy: – Recurrent pregnancy loss – Preterm labour – Abnormal fetal presentation l Uterine defects seen in 1 -3% of normal women with normal pregnancy out-come. l 20 -27% of women with history of R. P. L has anatomic uterine defect. l Routine H. S. G. for diagnoses is questionable l 3 D ultrasound is good tool for diagnoses. l Corrective open surgery carries risk of adhesions and possible rapture uterus in pregnancy ; which is less likely to occur in hysteroscopic surgery. l
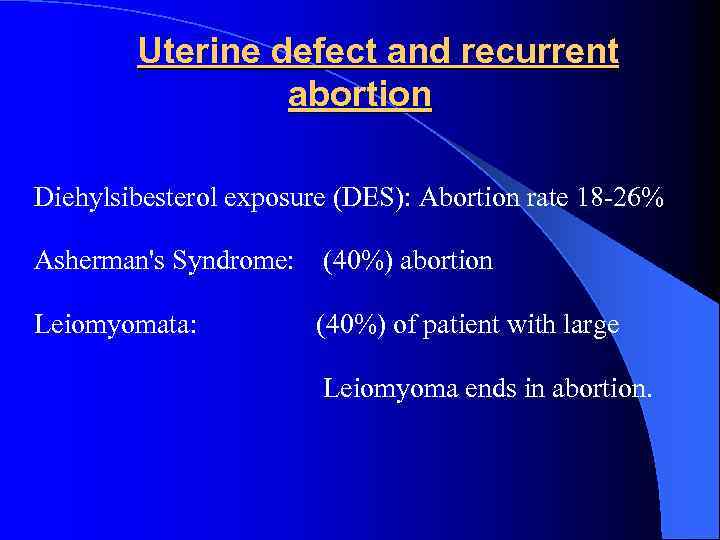
Uterine defect and recurrent abortion Diehylsibesterol exposure (DES): Abortion rate 18 -26% Asherman's Syndrome: (40%) abortion Leiomyomata: (40%) of patient with large Leiomyoma ends in abortion.
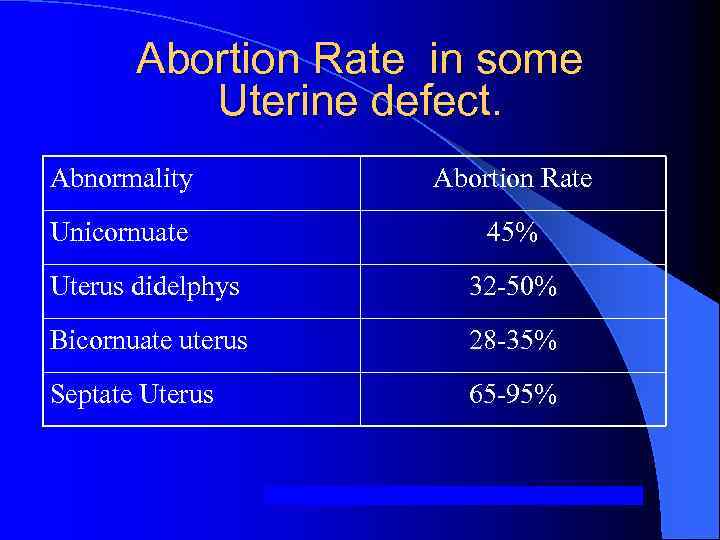
Abortion Rate in some Uterine defect. Abnormality Abortion Rate Unicornuate 45% Uterus didelphys 32 -50% Bicornuate uterus 28 -35% Septate Uterus 65 -95%

5 -Cervical incompetence Definition: Congenital or traumatic (Surgical, Obstetrical) weakness of the cervix. l Diagnosis: (usually over diagnosed) l – From previous obstetrical history. – Clinical examination in pregnancy and in non-pregnant women. – Observation of progressive effacement & dilatation of the cervix in pregnancy. l Ultrasonography, ( refere to the papers of Stewart Campell and Hassan, 2011, 2012) l l H. SG. , Hysteroscopy.
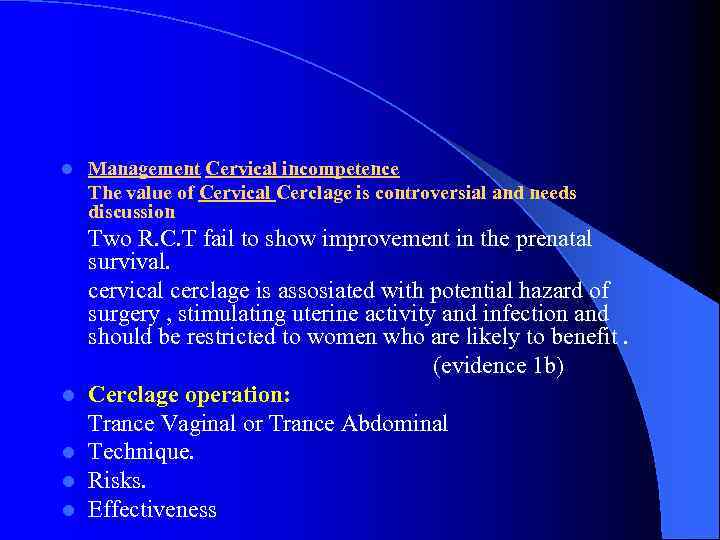
l Management Cervical incompetence The value of Cervical Cerclage is controversial and needs discussion Two R. C. T fail to show improvement in the prenatal survival. cervical cerclage is assosiated with potential hazard of surgery , stimulating uterine activity and infection and should be restricted to women who are likely to benefit. (evidence 1 b) l Cerclage operation: Trance Vaginal or Trance Abdominal l Technique. l Risks. l Effectiveness
l 6 -Endocrine factors & recurrent abortion These are controversial, it include: l Diabetes mellitus l Thyroid disease l Luteal phase defect

l A-Diabetes mellitus & abortion l No effect in women with subsclinial or adequately controlled diabetes. l In Insulin-dependent with inadequate glucose control 2 to 3 folds higher rate of abortion.
B- Thyroid disease & abortion Hypo or hyperthyroidism rarely cause recurrent abortion. Thyroid antibodies are seen more in recurrent abortions (diagnose autoimmune cause of R. A). Thyroid antibodies measurement is useful to predict pregnancy loss.
l C - Luteal phase defect l Inadequate endometrial maturation caused by insufficient. Progesterone productions or shorter duration of the luteal phase. l Low progesterone level reported in early pregnancy failure.

l Diagnosis of LPD l Clinically, from menstrual history. B. B. T. records. l Progesterone concentration. l Endometrial biopsy and histological dating. l Ultrasonography of the endometrium. l – Endometrial thickness. – Mean pulsatility index of the uterine artery. – Follicle size determination. l Endometrial protiens studies

l l l l l Treatment of luteal phase defect This is controversial when considering treatment of recurrent abortion. Several regimens are used. Progesterone supplementation (I. M, oral, vaginal). Clomiphene citrate Gonadotropins (FSH) Bromocreptin -HCG Tamoxifen Gn Rh. Lack of accurate diagnosis of LPD & lack of controlled randomized studies for the treatment make such treatments is controversial.
High L. H. level l High L. H was seen in PCO patients , its suppression did not improve pregnancy outcome. High prolactin level usually associated with delayed fertility and uncertain effect on pregnancy failure.
7 -Autoimmune factors : l Anitphospholipid antibodies. l Lupus anticoagulant. l Anticardiolipin antibodies. l Anitnuclear antibodies. l Antithyroid antibodies.

A-Antiphospholipid Antibodies (APL) Phospholipids are normal component of the cell membrane. Antibodies to phospholipids cause: l Damage the inside of the blood vessels. l Decrease the blood flow. l Formation of blood clots. l In early pregnancy interfere with formation of syncytiotrophoblast and the placental development
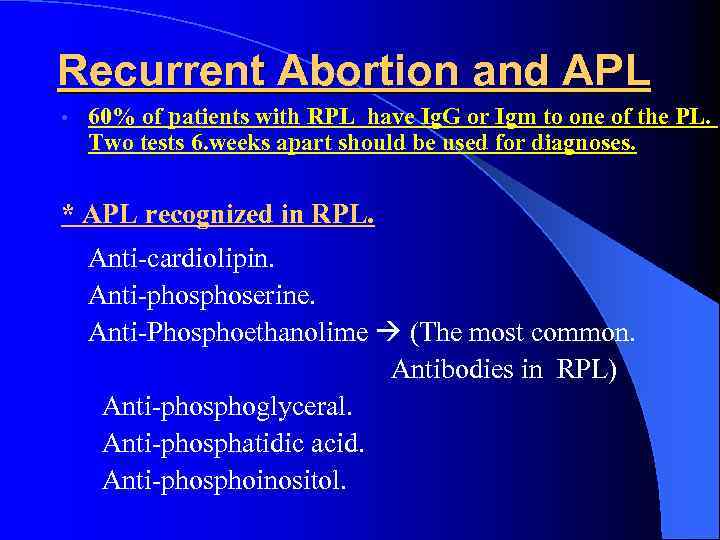
Recurrent Abortion and APL • 60% of patients with RPL have Ig. G or Igm to one of the PL. Two tests 6. weeks apart should be used for diagnoses. * APL recognized in RPL. Anti-cardiolipin. Anti-phoserine. Anti-Phosphoethanolime (The most common. Antibodies in RPL) Anti-phosphoglyceral. Anti-phosphatidic acid. Anti-phosphoinositol.
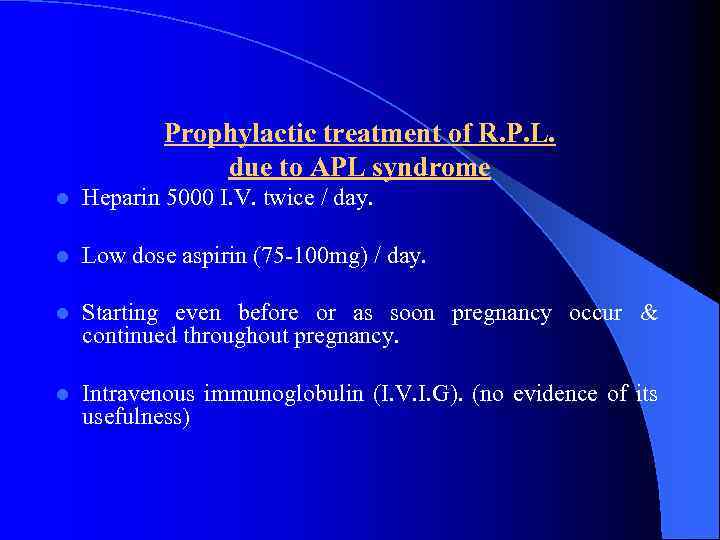
Prophylactic treatment of R. P. L. due to APL syndrome l Heparin 5000 I. V. twice / day. l Low dose aspirin (75 -100 mg) / day. l Starting even before or as soon pregnancy occur & continued throughout pregnancy. l Intravenous immunoglobulin (I. V. I. G). (no evidence of its usefulness)
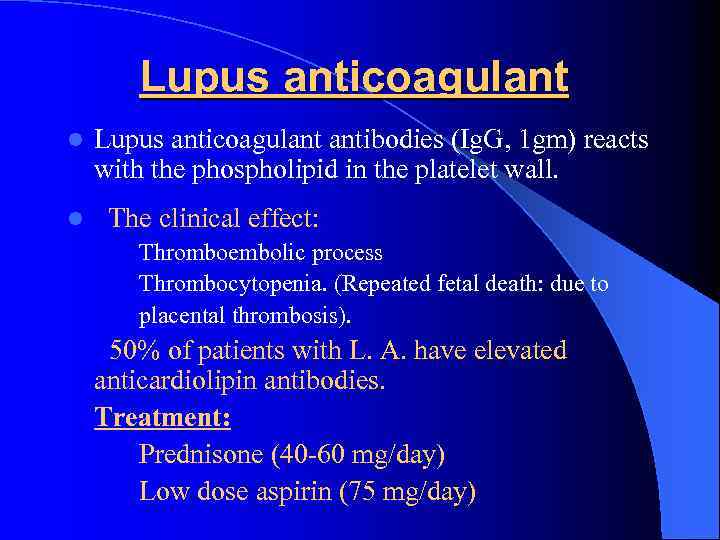
Lupus anticoagulant l Lupus anticoagulant antibodies (Ig. G, 1 gm) reacts with the phospholipid in the platelet wall. l The clinical effect: Thromboembolic process Thrombocytopenia. (Repeated fetal death: due to placental thrombosis). 50% of patients with L. A. have elevated anticardiolipin antibodies. Treatment: Prednisone (40 -60 mg/day) Low dose aspirin (75 mg/day)

l Antinuclear antibodies and RPL l l l Elevated ANA were seen in 7 -53% of women with RPL compared to 0 -8% in control. Titre of 1: 40 is used as a threshold. As a cause or RPL many reviews are contradictory. Treatment: Prednisone 40 -60 mg/day starting even before pregnancy.
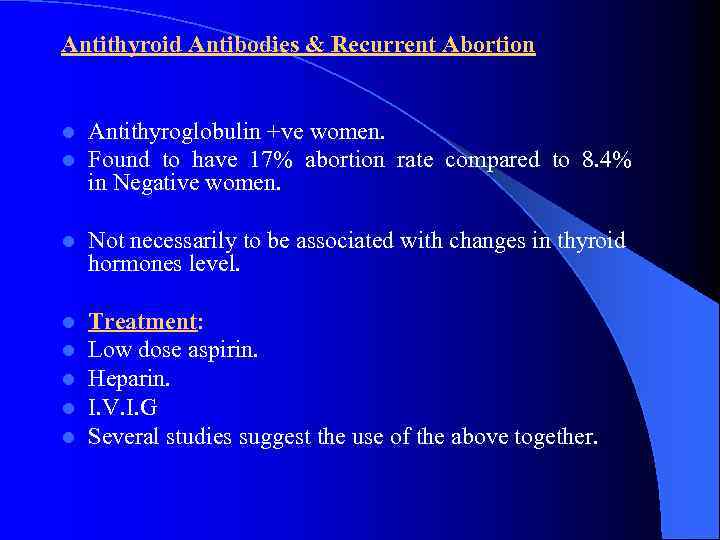
Antithyroid Antibodies & Recurrent Abortion l l Antithyroglobulin +ve women. Found to have 17% abortion rate compared to 8. 4% in Negative women. l Not necessarily to be associated with changes in thyroid hormones level. l l l Treatment: Low dose aspirin. Heparin. I. V. I. G Several studies suggest the use of the above together.
8 -Inherited thrombophelia l Inherited and acquired thrombophelia is seen in 50 -60% of cases of RPL. l Associated with increased arterial & venous thrombosis. l Associated with abnormal placental vascularisation and placental thrombosis.
Types of inherited thrombophelia l Hyper homocysteinaemia. l Factor V leiden mutation. l Protein C. and protein S. deficiency. l Anti thrombin III mutation. l Prothrombin gene mutation.
9 -Uterine Receptively l This is a complex interaction between peptide and steroid Hormone which synchronizes the preparation of endometrium for implantation and the development of the embryo. l The endometrium secretes several proteins during the luteal phase of the cycle. Several of these proteins are essential for a receptive uterus or for implantation. l l Some of these proteins enhances the embryo development and blastocyst attachment and invasion. l ( C. B. coulom. clinical ob. gyn. 1994
Endometrial proteins l l Leukemia inhibitory factor (LIF) Cytokines: – – – – Plasminogen activator inhibitor. Interleukin -1. Tumour necrosis factor-Alpha. Interferon- ∂α EGF (epidermal growth factor). EGF binding protein - 4. Granulocytes macrophages colony stimulation factory.
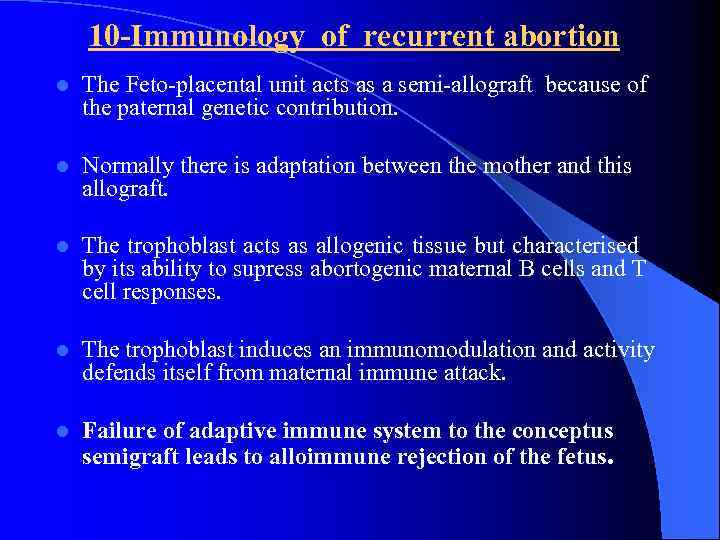
10 -Immunology of recurrent abortion l The Feto-placental unit acts as a semi-allograft because of the paternal genetic contribution. l Normally there is adaptation between the mother and this allograft. l The trophoblast acts as allogenic tissue but characterised by its ability to supress abortogenic maternal B cells and T cell responses. l The trophoblast induces an immunomodulation and activity defends itself from maternal immune attack. l Failure of adaptive immune system to the conceptus semigraft leads to alloimmune rejection of the fetus.
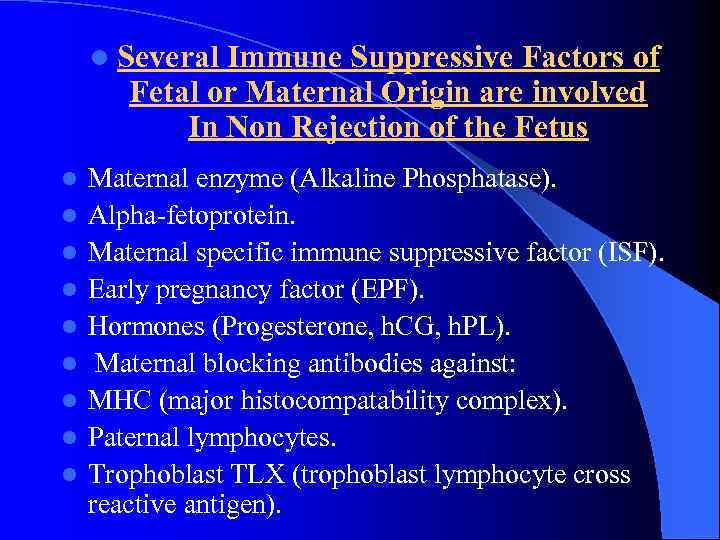
l Several Immune Suppressive Factors of Fetal or Maternal Origin are involved In Non Rejection of the Fetus l l l l l Maternal enzyme (Alkaline Phosphatase). Alpha-fetoprotein. Maternal specific immune suppressive factor (ISF). Early pregnancy factor (EPF). Hormones (Progesterone, h. CG, h. PL). Maternal blocking antibodies against: MHC (major histocompatability complex). Paternal lymphocytes. Trophoblast TLX (trophoblast lymphocyte cross reactive antigen).

Uterine and Decidual Suppressor Cells (N. K Cells) Cells that found in the decidua and the placenta they comprise 15% of the peripheral blood lymphocytes. l These N. K cells are activated to destroy the trophoblast. l There is a balance between factors that stimulate and factors that inhibit the N. K. cells activity.
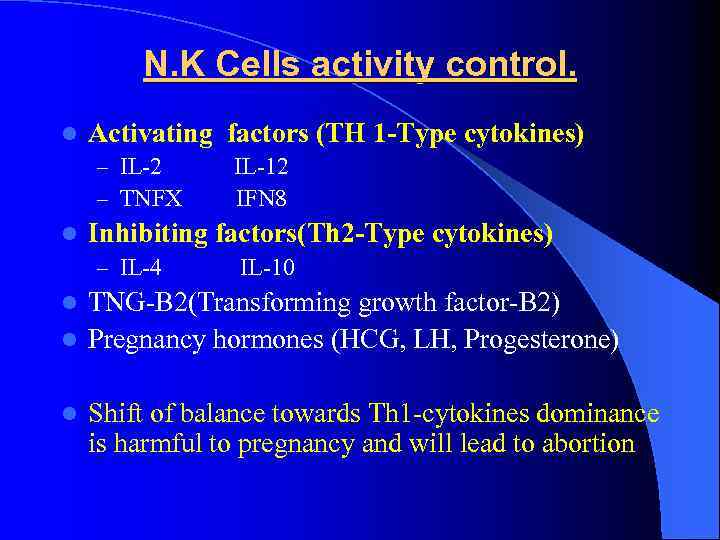
N. K Cells activity control. l Activating factors (TH 1 -Type cytokines) – IL-2 IL-12 – TNFX IFN 8 l Inhibiting factors(Th 2 -Type cytokines) – IL-4 IL-10 TNG-B 2(Transforming growth factor-B 2) l Pregnancy hormones (HCG, LH, Progesterone) l l Shift of balance towards Th 1 -cytokines dominance is harmful to pregnancy and will lead to abortion

Adaptation for maintenance of early pregnancy l These are not well understood but progesterone is believed to exert its effect by: – Restoring luteal phase insufficiency – Through general relaxing effect on the uterine muscles by suppressing endometrial prostaglandin synthesis – Recent data suggested that progesterone modulate the maternal immune response.
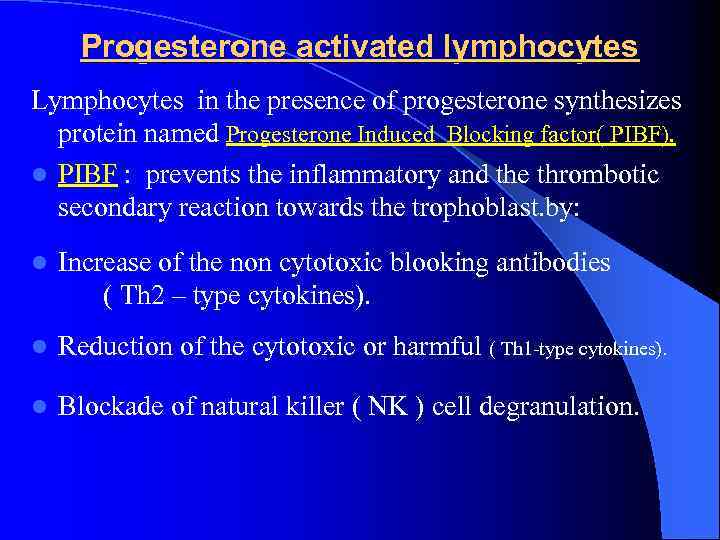
Progesterone activated lymphocytes Lymphocytes in the presence of progesterone synthesizes protein named Progesterone Induced Blocking factor( PIBF). l PIBF : prevents the inflammatory and the thrombotic secondary reaction towards the trophoblast. by: l Increase of the non cytotoxic blooking antibodies ( Th 2 – type cytokines). l Reduction of the cytotoxic or harmful ( Th 1 -type cytokines). l Blockade of natural killer ( NK ) cell degranulation.

Treatment options of Immunolgoical causes of RPL Low dose Aspirin • Heparin • Corticosteroids • Intravenous Immunoglobulin (Iv. Ig) • • • Leukocyte Infusion
l l l 11 -Semen quality, antisperm antibodies and abortion Low sperm count and low motility: No definite relationship. Sperm morphology: ? ? Diploid spermatozoa: Sperm with large head (diploid sperm) when fertilizes an egg polypoid embryo. Abnormal DNA content of the sperm. Polyspermia: higher rate of abortion (~ 20%) due to egg fertilized by many sperms. Antisperm antibodies in the female serum. Sperm agglutination and immobilization (? ? increased risk). In conclusion: Seminal characteristics and antisperm AB in female serum were not definitely found to increase risk of abortion. Polyspermia: may be a cause.
Mothers at Risk to Abortion: Presence of previous abortion. Presence of previous S. B. l Presence of previous cong. Abnormal infant. l Mother or father with known genetic defects. l Mother age > 35 years. l Father age > 53 years. l
Unexplained cases of RM: l This worsens with advanced maternal age and increased number of abortion. l Empirical treatment is to be resisted. l Psychological support and TLC has been shown to be effective approach in the management.
l l l l l Suggested Routine evaluation of RPL History: Pattern and trimester of abortion Embryonal or unembryonal Exposure to environmental toxins or drugs Known infections. Features associated with APL syndrome. Genetic relationship between parents. Family history of RPL or syndromes associated with embryonic or fetal loss. Gynecological and menstrual disorders. Previous diagnostic tests and treatment.

All patients should have the following investigations: l l l Pelvic sonography H. S. G Laparoscopy, Hysteroscopy (when anatomic abnormalities were l l l Blood group and Rh. Thyroid function test (T 3, T 4, TSH) Mid luteal phase progesterone level. Prolactin C. B. C, ESR H. V. S (bacteriology) Virology study (TORCH) Immunology test (Ig. G, Igm: ACL, ANA, APL, LA) Chromosomal analysis of both partners and P. O. C when possible Semen analysis of the husband. Blood Coagulation studies. Recently natural N. K cells level in peripheral blood? . expected).
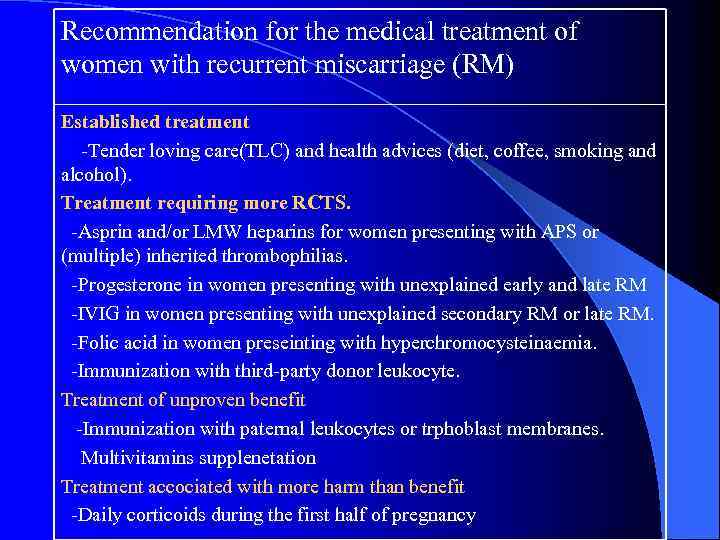
Recommendation for the medical treatment of women with recurrent miscarriage (RM) Established treatment -Tender loving care(TLC) and health advices (diet, coffee, smoking and alcohol). Treatment requiring more RCTS. -Asprin and/or LMW heparins for women presenting with APS or (multiple) inherited thrombophilias. -Progesterone in women presenting with unexplained early and late RM -IVIG in women presenting with unexplained secondary RM or late RM. -Folic acid in women preseinting with hyperchromocysteinaemia. -Immunization with third-party donor leukocyte. Treatment of unproven benefit -Immunization with paternal leukocytes or trphoblast membranes. Multivitamins supplenetation Treatment accociated with more harm than benefit -Daily corticoids during the first half of pregnancy
Conclusions (1): l Recurrent pregnancy loss is now recognized as a specific clinical condition. l Controversies surrounding the etiology and management are two reasons for concern and frustration to the couple and the physician. l It is necessary to follow a comprehensive efficient and cost effective diagnostic work up when evaluating this condition.

Conclusion (II) l When no cause is revealed with standard comprehensive evaluation (unexplained recurrent losses), alloimmune factor are proposed as an etiology. l When evaluation is negative, emotional support is important, opticism regarding successful pregnancy as approximately 60% of these patients will achieve successful pregnancy even without treatment.

Thank you for attention
RECURRENT MISCARRIAGE 2013. medical council.ppt