7baa5275bfb3b583a2e3385114d248a8.ppt
- Количество слайдов: 42
 Recognition and Emergency Management of Posterior Circulation Stroke Todd J. Crocco, MD, FACEP Professor WVU Department of Emergency Medicine November 20, 2015
Recognition and Emergency Management of Posterior Circulation Stroke Todd J. Crocco, MD, FACEP Professor WVU Department of Emergency Medicine November 20, 2015
 JB MRN#: 070982372 • 45@ time of stroke in December 2007 • Presented with H/A, dizziness, diplopia, decreased sensation and weakness right arm and leg.
JB MRN#: 070982372 • 45@ time of stroke in December 2007 • Presented with H/A, dizziness, diplopia, decreased sensation and weakness right arm and leg.
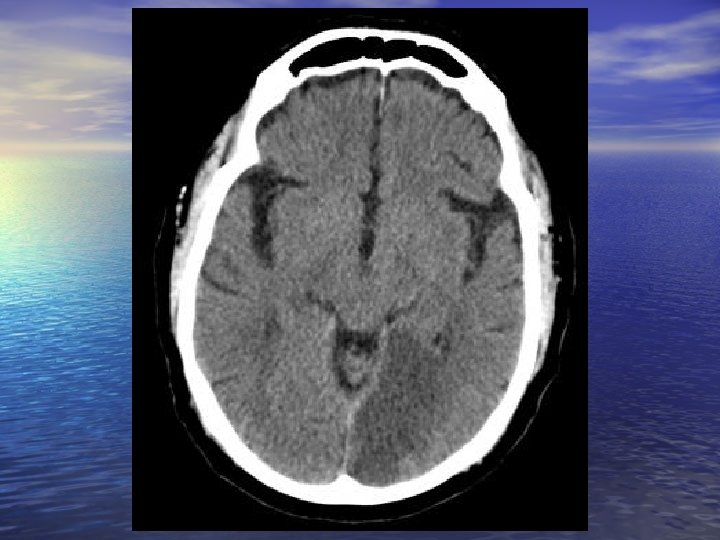
 Initial CT 12/12/2007, 0156 • Clot at the distal right vertebral artery. • Narrowing at the origin of the right pica may be secondary to small clot or stenosis. • Area of mild stenosis left vertebral artery near origin of the basilar artery adjacent to the right vertebrobasilar junction.
Initial CT 12/12/2007, 0156 • Clot at the distal right vertebral artery. • Narrowing at the origin of the right pica may be secondary to small clot or stenosis. • Area of mild stenosis left vertebral artery near origin of the basilar artery adjacent to the right vertebrobasilar junction.
 MRI 12/12/2007, 1706 • Acute small right lateral medullary infarction with what appears to be occluded distal right vertebral artery. The finding is compatible with abnormalities noted with non-opacification of the distal right vertebral artery on CT stroke protocol of 12 December 2007.
MRI 12/12/2007, 1706 • Acute small right lateral medullary infarction with what appears to be occluded distal right vertebral artery. The finding is compatible with abnormalities noted with non-opacification of the distal right vertebral artery on CT stroke protocol of 12 December 2007.
 Recurrent stroke several days later… • Readmitted several days after discharge with • dysphagia and now LEFT arm hemiplegia and left leg weakness CTA 12/21/07 was unchanged as compared to prior examination showing distal right vertebral artery thrombus, significant narrowing of the origin of right PICA, and significant stenosis of the proximal basilar artery with a 60 -70%, which is hemodynamically significant and no evidence of new thrombus.
Recurrent stroke several days later… • Readmitted several days after discharge with • dysphagia and now LEFT arm hemiplegia and left leg weakness CTA 12/21/07 was unchanged as compared to prior examination showing distal right vertebral artery thrombus, significant narrowing of the origin of right PICA, and significant stenosis of the proximal basilar artery with a 60 -70%, which is hemodynamically significant and no evidence of new thrombus.
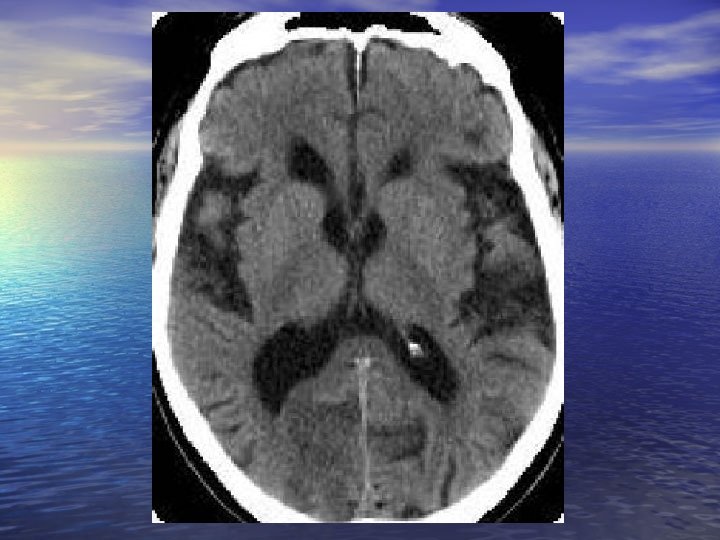
 MRI 12/23/2007, 0858 • Infarct involving the lower medulla, which has slightly increased signal than the previous exam, also, now involving the ventral medullary aspect. There is no hemorrhage identified.
MRI 12/23/2007, 0858 • Infarct involving the lower medulla, which has slightly increased signal than the previous exam, also, now involving the ventral medullary aspect. There is no hemorrhage identified.
 Reevaluation in 2010 • CTA 11/12/2010 for recurrent dizziness • Severe intracranial atherosclerotic disease involving the vertebrobasilar system with a worsening of stenosis at junction of left vertebral artery and basilar artery with chronic right distal intracranial vertebral artery occlusion. Stenosis now measures 70% or greater.
Reevaluation in 2010 • CTA 11/12/2010 for recurrent dizziness • Severe intracranial atherosclerotic disease involving the vertebrobasilar system with a worsening of stenosis at junction of left vertebral artery and basilar artery with chronic right distal intracranial vertebral artery occlusion. Stenosis now measures 70% or greater.
 MRI 12/7/2010, 1619 • 1. Encephalomalacia within the medulla consistent with tissue loss from remote infarct. There is no evidence to suggest acute or evolving infarct on today's examination. • 2. Loss of flow signal in the right skull base vertebral artery consistent with chronic occlusion depicted on study dated December 21, 2007.
MRI 12/7/2010, 1619 • 1. Encephalomalacia within the medulla consistent with tissue loss from remote infarct. There is no evidence to suggest acute or evolving infarct on today's examination. • 2. Loss of flow signal in the right skull base vertebral artery consistent with chronic occlusion depicted on study dated December 21, 2007.
 The turning point… • Recurrent episodes of intermittent vertigo and lightheadedness several times a week felt to be due to vertebral-basilar insufficiency. • 12/13/10 Enrolled in SAMMPRIS trial. Randomized to medical therapy arm. • 5’ 11’’, 306 lb, Haic 8. 3, Htn, HLD, OSA on cpap at night.
The turning point… • Recurrent episodes of intermittent vertigo and lightheadedness several times a week felt to be due to vertebral-basilar insufficiency. • 12/13/10 Enrolled in SAMMPRIS trial. Randomized to medical therapy arm. • 5’ 11’’, 306 lb, Haic 8. 3, Htn, HLD, OSA on cpap at night.
 September 2015 follow up • 53 yo WM here for follow up. He is s/p Gastric bypass • • (Roux-en-Y). Morbid obesity- lost 75 lbs prior to surgery. He has lost 48 lbs more since 12/9/14. HTN- his BP has been doing well. He is off Lisinopril. T 2 DM- his A 1 C is 4. 1, In July. he is off all meds for this. HLD- TC 127 HDL 47 LDL 72 TG 39 off CRESTOR 40 mg a day due to cost since May. He is off fenofibrate 54 mg a day. I started Atorvastatin 40 mg a day last visit.
September 2015 follow up • 53 yo WM here for follow up. He is s/p Gastric bypass • • (Roux-en-Y). Morbid obesity- lost 75 lbs prior to surgery. He has lost 48 lbs more since 12/9/14. HTN- his BP has been doing well. He is off Lisinopril. T 2 DM- his A 1 C is 4. 1, In July. he is off all meds for this. HLD- TC 127 HDL 47 LDL 72 TG 39 off CRESTOR 40 mg a day due to cost since May. He is off fenofibrate 54 mg a day. I started Atorvastatin 40 mg a day last visit.
 Posterior Circulation Ischemia Posterior circulation ischemia can range from fluctuating brainstem symptoms, caused by intermittent insufficiency of the posterior circulation (so-called VBI), to the “locked-in syndrome, " which is caused by basilar artery or bilateral vertebral artery occlusion.
Posterior Circulation Ischemia Posterior circulation ischemia can range from fluctuating brainstem symptoms, caused by intermittent insufficiency of the posterior circulation (so-called VBI), to the “locked-in syndrome, " which is caused by basilar artery or bilateral vertebral artery occlusion.
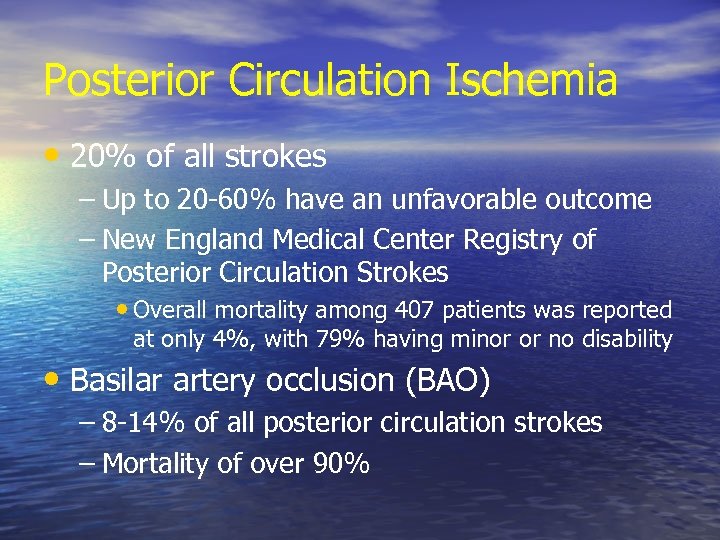 Posterior Circulation Ischemia • 20% of all strokes – Up to 20 -60% have an unfavorable outcome – New England Medical Center Registry of Posterior Circulation Strokes • Overall mortality among 407 patients was reported at only 4%, with 79% having minor or no disability • Basilar artery occlusion (BAO) – 8 -14% of all posterior circulation strokes – Mortality of over 90%
Posterior Circulation Ischemia • 20% of all strokes – Up to 20 -60% have an unfavorable outcome – New England Medical Center Registry of Posterior Circulation Strokes • Overall mortality among 407 patients was reported at only 4%, with 79% having minor or no disability • Basilar artery occlusion (BAO) – 8 -14% of all posterior circulation strokes – Mortality of over 90%
 Anatomy & Pathophysiology • Etiology thought to be local arterial atherosclerosis (large artery disease) and penetrating artery disease (lacunes) • New evidence that cardiogenic embolization is more common – 20 -50% of posterior circulation strokes
Anatomy & Pathophysiology • Etiology thought to be local arterial atherosclerosis (large artery disease) and penetrating artery disease (lacunes) • New evidence that cardiogenic embolization is more common – 20 -50% of posterior circulation strokes
 Risk Factors • Uncontrollable risk factors include – Age – Gender – Race – Family history of stroke or TIA – Personal history of diabetes
Risk Factors • Uncontrollable risk factors include – Age – Gender – Race – Family history of stroke or TIA – Personal history of diabetes
 Risk Factors • Medical stroke risk factors include – Hypertension – Heart disease (atrial fibrillation or LVH) – Previous stroke or TIA – Previous heart surgery – Carotid artery disease – Peripheral vascular disease – Smoking
Risk Factors • Medical stroke risk factors include – Hypertension – Heart disease (atrial fibrillation or LVH) – Previous stroke or TIA – Previous heart surgery – Carotid artery disease – Peripheral vascular disease – Smoking
 Risk Factors • Each decade past age 55: 2 x • Past history of stroke or a TIA: 10 x • Atrial fibrillation: 6 x • Smoking: 2 x
Risk Factors • Each decade past age 55: 2 x • Past history of stroke or a TIA: 10 x • Atrial fibrillation: 6 x • Smoking: 2 x
 Risk Factors • The most common causes for vertebrobasilar occlusion are atherosclerosis in the elderly, and trauma in the younger population
Risk Factors • The most common causes for vertebrobasilar occlusion are atherosclerosis in the elderly, and trauma in the younger population
 Signs & Symptoms • Wide variety of syndromes – Hemi or quadriparesis – Cranial nerve deficits (III-XII) – Respiratory difficulty – Altered sensorium – Vertigo – Ataxia – Multiple cranial nerve signs indicate involvement of more than one brainstem level
Signs & Symptoms • Wide variety of syndromes – Hemi or quadriparesis – Cranial nerve deficits (III-XII) – Respiratory difficulty – Altered sensorium – Vertigo – Ataxia – Multiple cranial nerve signs indicate involvement of more than one brainstem level
 Signs & Symptoms • "5 Ds” – Dizziness – peripheral or central – Diplopia – ophthmalmologic versus neurologic – Dysarthria – Dysphagia – Dystaxia
Signs & Symptoms • "5 Ds” – Dizziness – peripheral or central – Diplopia – ophthmalmologic versus neurologic – Dysarthria – Dysphagia – Dystaxia
 Signs & Symptoms • “Crossed findings” – Cranial findings on the side of the lesion and motor or sensory findings on the opposite side.
Signs & Symptoms • “Crossed findings” – Cranial findings on the side of the lesion and motor or sensory findings on the opposite side.
 Signs & Symptoms • The most frequent posterior circulation symptoms were dizziness (47%), unilateral limb weakness (41%), dysarthria (31%), headache (28%), and nausea or vomiting (27%) New England Medical Center Posterior Circulation Registry. Arch Neurol. 2012; 69(3): 346 -351.
Signs & Symptoms • The most frequent posterior circulation symptoms were dizziness (47%), unilateral limb weakness (41%), dysarthria (31%), headache (28%), and nausea or vomiting (27%) New England Medical Center Posterior Circulation Registry. Arch Neurol. 2012; 69(3): 346 -351.
 Shifting Gears…. .
Shifting Gears…. .
 What Does the ED Provide? § Availability 24/7/365 § Speed (when it matters) § Critical care skills § Very broad clinical knowledge
What Does the ED Provide? § Availability 24/7/365 § Speed (when it matters) § Critical care skills § Very broad clinical knowledge
 What Does This Imply? § 24/7 availability requires a lot of people and coordination § For speed, need to clarify the stakes § Every specialty has a “special need” § Critical care to patients with perceived critical needs § Broad knowledge base - need specialty backup
What Does This Imply? § 24/7 availability requires a lot of people and coordination § For speed, need to clarify the stakes § Every specialty has a “special need” § Critical care to patients with perceived critical needs § Broad knowledge base - need specialty backup
 Three Important Messages • The ED has limitations – ‘You want a piece of me TOO? !’ • Delays are real – ‘systems’ can fix them – Buy-in and perception is needed • Planning and communication is needed – Develop protocols
Three Important Messages • The ED has limitations – ‘You want a piece of me TOO? !’ • Delays are real – ‘systems’ can fix them – Buy-in and perception is needed • Planning and communication is needed – Develop protocols
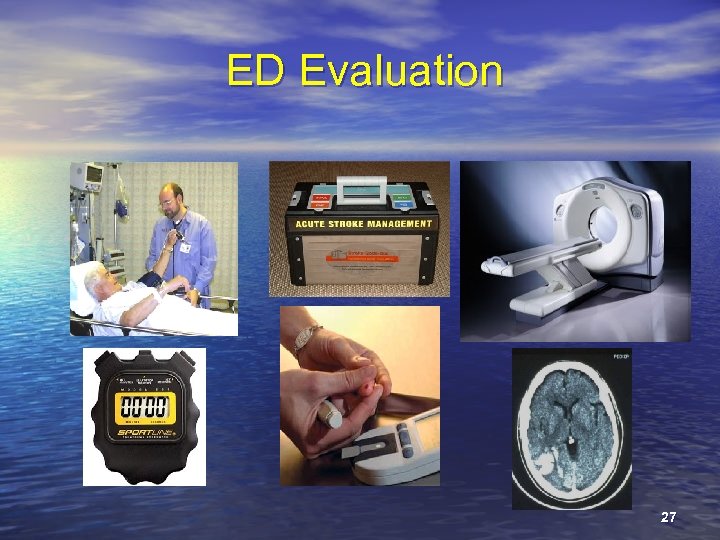 ED Evaluation 27
ED Evaluation 27
 The ED “Stroke Protocol” • Focused history and physical (ABC’s) – General and neurologic assessment • Fingerstick glucose measurement • IV access and STAT labs • Contact stroke team? • Patient monitoring – Frequent monitoring of VS and neuro exam – Oxygen and cardiac monitoring
The ED “Stroke Protocol” • Focused history and physical (ABC’s) – General and neurologic assessment • Fingerstick glucose measurement • IV access and STAT labs • Contact stroke team? • Patient monitoring – Frequent monitoring of VS and neuro exam – Oxygen and cardiac monitoring
 General Stroke Management • Activate ‘Stroke Team’ • Check glucose & labs • Two large IV lines • Oxygen as needed • Cardiac monitor • Continuous pulse-ox • CT scan…. STAT • Confirm LSNN time • Perform neurologic • exam Get “real” with rt-PA – Prepare to mix – Have pharmacy alerted • Discuss with patient and • family potential treatments Begin general management
General Stroke Management • Activate ‘Stroke Team’ • Check glucose & labs • Two large IV lines • Oxygen as needed • Cardiac monitor • Continuous pulse-ox • CT scan…. STAT • Confirm LSNN time • Perform neurologic • exam Get “real” with rt-PA – Prepare to mix – Have pharmacy alerted • Discuss with patient and • family potential treatments Begin general management
 General Stroke Management • Cardiac monitor – Observe for ischemic changes or atrial fibrillation • Intravenous fluids – Avoid D 5 W and excessive fluid administration – IV normal saline at 50 cc / hr unless otherwise required • NPO – Aspiration risk, avoid PO until swallowing assessed • Blood pressure – Function of fibrinolytic eligibility
General Stroke Management • Cardiac monitor – Observe for ischemic changes or atrial fibrillation • Intravenous fluids – Avoid D 5 W and excessive fluid administration – IV normal saline at 50 cc / hr unless otherwise required • NPO – Aspiration risk, avoid PO until swallowing assessed • Blood pressure – Function of fibrinolytic eligibility
 Team Communication • Nursing ED doc Consultants • For the ED team – just like any resuscitation • ED / Consultant communication – Absolutely critical – Complementary roles / complementary skills – Don’t say yo-yo!
Team Communication • Nursing ED doc Consultants • For the ED team – just like any resuscitation • ED / Consultant communication – Absolutely critical – Complementary roles / complementary skills – Don’t say yo-yo!
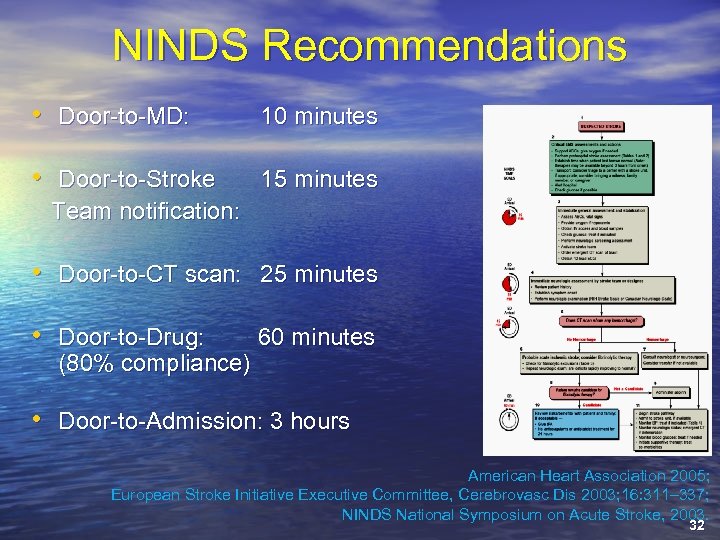 NINDS Recommendations • Door-to-MD: 10 minutes • Door-to-Stroke 15 minutes Team notification: • Door-to-CT scan: 25 minutes • Door-to-Drug: 60 minutes (80% compliance) • Door-to-Admission: 3 hours American Heart Association 2005; European Stroke Initiative Executive Committee, Cerebrovasc Dis 2003; 16: 311– 337; NINDS National Symposium on Acute Stroke, 2003. 32
NINDS Recommendations • Door-to-MD: 10 minutes • Door-to-Stroke 15 minutes Team notification: • Door-to-CT scan: 25 minutes • Door-to-Drug: 60 minutes (80% compliance) • Door-to-Admission: 3 hours American Heart Association 2005; European Stroke Initiative Executive Committee, Cerebrovasc Dis 2003; 16: 311– 337; NINDS National Symposium on Acute Stroke, 2003. 32
 Diagnosis & Evaluation • History and physical • Physical exam – Cranial nerve findings – Eye movements – Cerebellar findings combined with opposite long tract (sensory and motor) signs
Diagnosis & Evaluation • History and physical • Physical exam – Cranial nerve findings – Eye movements – Cerebellar findings combined with opposite long tract (sensory and motor) signs
 Emergency Diagnostic Studies • Brain imaging – CT or MRI? • Electrocardiogram • Complete blood count and platelet count • INR and a. PTT • Blood chemistries • Pulse oximetry, chest x-ray • CSF examination?
Emergency Diagnostic Studies • Brain imaging – CT or MRI? • Electrocardiogram • Complete blood count and platelet count • INR and a. PTT • Blood chemistries • Pulse oximetry, chest x-ray • CSF examination?
 Current Treatment Options • Physiologic optimization • No thrombolytics – Aspirin • Death / nonfatal strokes reduced 11% – Heparin • Intravenous rt-PA – Risk stratify although all subgroups benefited from thrombolytics in NINDS • Other treatments – Intra-arterial thrombolysis with rt-PA – Mechanical embolectomy 37
Current Treatment Options • Physiologic optimization • No thrombolytics – Aspirin • Death / nonfatal strokes reduced 11% – Heparin • Intravenous rt-PA – Risk stratify although all subgroups benefited from thrombolytics in NINDS • Other treatments – Intra-arterial thrombolysis with rt-PA – Mechanical embolectomy 37
 Management • IV thrombolytic therapy • Antiplatelet and antithrombotic therapy is often used, with wide variation in treatment regimens • Intra-arterial thrombolytic therapy has been used successfully for patients with suspected BAO
Management • IV thrombolytic therapy • Antiplatelet and antithrombotic therapy is often used, with wide variation in treatment regimens • Intra-arterial thrombolytic therapy has been used successfully for patients with suspected BAO
 Management • Traditionally, heparin has been used in the treatment of posterior circulation strokes, based upon uncontrolled trials showing benefit compared to historical controls
Management • Traditionally, heparin has been used in the treatment of posterior circulation strokes, based upon uncontrolled trials showing benefit compared to historical controls
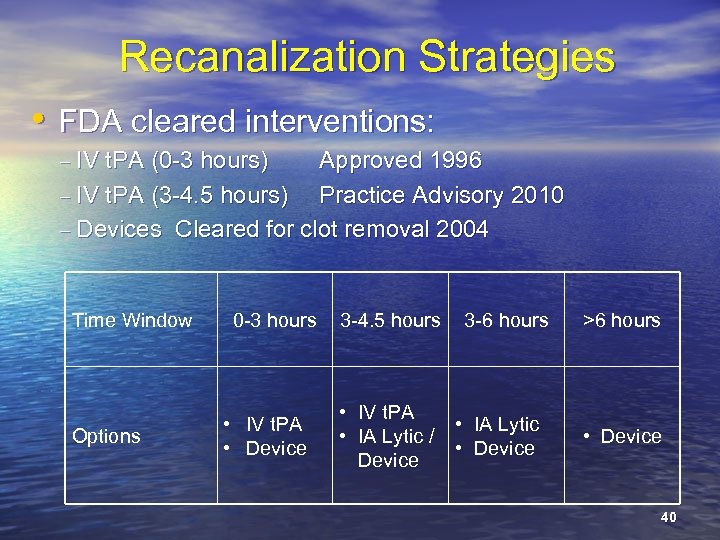 Recanalization Strategies • FDA cleared interventions: – IV t. PA (0 -3 hours) Approved 1996 – IV t. PA (3 -4. 5 hours) Practice Advisory 2010 – Devices Cleared for clot removal 2004 Time Window Options 0 -3 hours • IV t. PA • Device 3 -4. 5 hours 3 -6 hours • IV t. PA • IA Lytic / • Device >6 hours • Device 40
Recanalization Strategies • FDA cleared interventions: – IV t. PA (0 -3 hours) Approved 1996 – IV t. PA (3 -4. 5 hours) Practice Advisory 2010 – Devices Cleared for clot removal 2004 Time Window Options 0 -3 hours • IV t. PA • Device 3 -4. 5 hours 3 -6 hours • IV t. PA • IA Lytic / • Device >6 hours • Device 40
 Conclusion • Wide variety of symptoms • Crossed findings (cranial nerve findings ipsilateral, with motor and sensory findings contralateral) • 5 Ds (dizziness, diplopia, dysarthria, dysphagia, and dystaxia) • Stroke care is a team sport
Conclusion • Wide variety of symptoms • Crossed findings (cranial nerve findings ipsilateral, with motor and sensory findings contralateral) • 5 Ds (dizziness, diplopia, dysarthria, dysphagia, and dystaxia) • Stroke care is a team sport
 Questions?
Questions?


