0cc4c78ea075ce1b59120bf2b0c246b5.ppt
- Количество слайдов: 27
 Reaching the MDGs Evidence on High Impact Interventions. Agnes Soucat, World Bank and Netsanet Walelign, UNICEF Kigali June 23 -27
Reaching the MDGs Evidence on High Impact Interventions. Agnes Soucat, World Bank and Netsanet Walelign, UNICEF Kigali June 23 -27
 Why are we here today ?
Why are we here today ?
 Progress towards MDGs: inadequate Trend in Under-Five Deaths, 1960 -2015 (Millions deaths per year)
Progress towards MDGs: inadequate Trend in Under-Five Deaths, 1960 -2015 (Millions deaths per year)
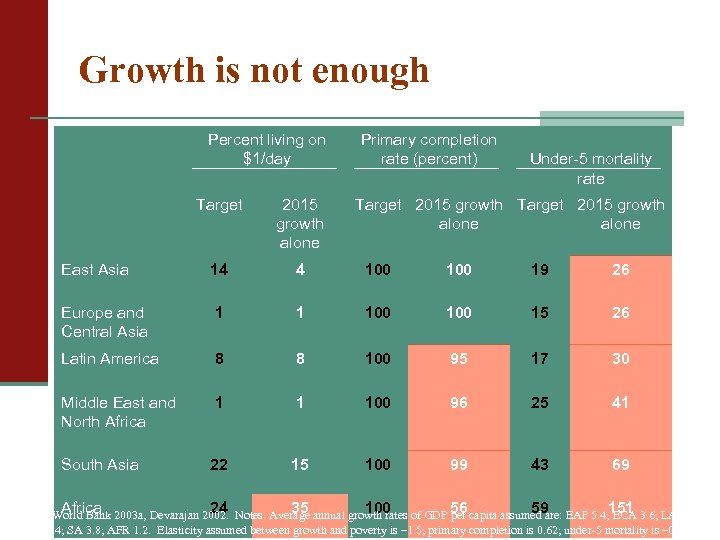 Growth is not enough Percent living on $1/day Primary completion rate (percent) Under-5 mortality rate Target 2015 growth alone East Asia 14 4 100 19 26 Europe and Central Asia 1 1 100 15 26 Latin America 8 8 100 95 17 30 Middle East and North Africa 1 1 100 96 25 41 South Asia 22 15 100 99 43 69 Africa 24 35 100 56 59 151 Sources: World Bank 2003 a, Devarajan 2002. Notes: Average annual growth rates of GDP per capita assumed are: EAP 5. 4; ECA 3. 6; LAC 1. 8; MENA 1. 4; SA 3. 8; AFR 1. 2. Elasticity assumed between growth and poverty is – 1. 5; primary completion is 0. 62; under-5 mortality is – 0. 48.
Growth is not enough Percent living on $1/day Primary completion rate (percent) Under-5 mortality rate Target 2015 growth alone East Asia 14 4 100 19 26 Europe and Central Asia 1 1 100 15 26 Latin America 8 8 100 95 17 30 Middle East and North Africa 1 1 100 96 25 41 South Asia 22 15 100 99 43 69 Africa 24 35 100 56 59 151 Sources: World Bank 2003 a, Devarajan 2002. Notes: Average annual growth rates of GDP per capita assumed are: EAP 5. 4; ECA 3. 6; LAC 1. 8; MENA 1. 4; SA 3. 8; AFR 1. 2. Elasticity assumed between growth and poverty is – 1. 5; primary completion is 0. 62; under-5 mortality is – 0. 48.
 Yet we know that some interventions are highly effective
Yet we know that some interventions are highly effective
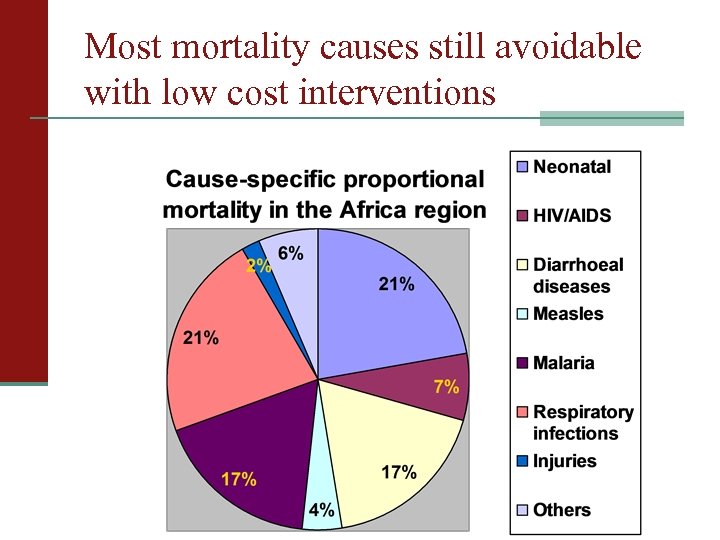 Most mortality causes still avoidable with low cost interventions
Most mortality causes still avoidable with low cost interventions
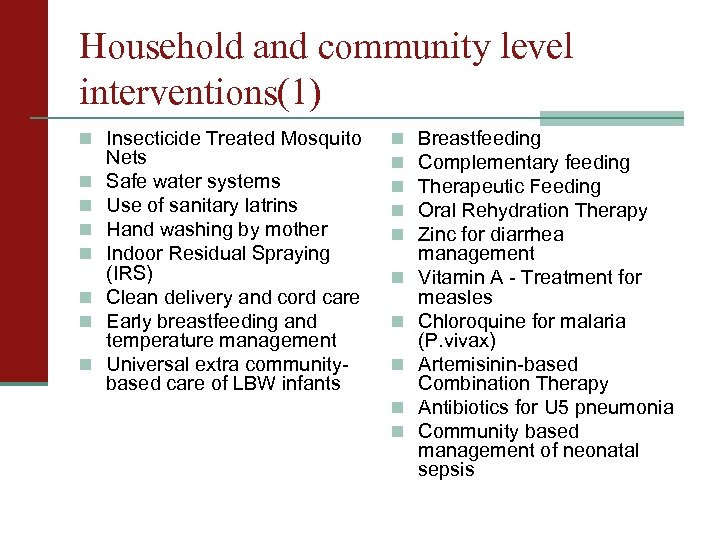 Household and community level interventions(1) n Insecticide Treated Mosquito n n n n Nets Safe water systems Use of sanitary latrins Hand washing by mother Indoor Residual Spraying (IRS) Clean delivery and cord care Early breastfeeding and temperature management Universal extra communitybased care of LBW infants n n n n n Breastfeeding Complementary feeding Therapeutic Feeding Oral Rehydration Therapy Zinc for diarrhea management Vitamin A - Treatment for measles Chloroquine for malaria (P. vivax) Artemisinin-based Combination Therapy Antibiotics for U 5 pneumonia Community based management of neonatal sepsis
Household and community level interventions(1) n Insecticide Treated Mosquito n n n n Nets Safe water systems Use of sanitary latrins Hand washing by mother Indoor Residual Spraying (IRS) Clean delivery and cord care Early breastfeeding and temperature management Universal extra communitybased care of LBW infants n n n n n Breastfeeding Complementary feeding Therapeutic Feeding Oral Rehydration Therapy Zinc for diarrhea management Vitamin A - Treatment for measles Chloroquine for malaria (P. vivax) Artemisinin-based Combination Therapy Antibiotics for U 5 pneumonia Community based management of neonatal sepsis
 Population oriented interventions (2) n Family planning n HPV vaccination n Preconceptual folate n PMTCT n VCT n Cotrimoxazole prophylaxis for n n n n n supplementation Tetanus toxoid Deworming in pregnancy Detection and treatment of asymptomatic bacteriuria Treatment of syphilis in pregnancy Prevention and treatment of iron deficiency anemia in pregnancy Intermittent preventive treatment (IPTp) for malaria in pregnancy Balanced protein energy supplements for pregnant women Supplementation in pregnancy with multi-micronutrients n n HIV+ Measles immunization BCG immunization OPV immunization DPT immunization Hib immunization Hepatitis B immunization Yellow fever immunization Meningitis immunization Pneumococcal immunization Rotavirus immunization Neonatal Vitamin A supplementation Vitamin A - supplementation Zinc preventive
Population oriented interventions (2) n Family planning n HPV vaccination n Preconceptual folate n PMTCT n VCT n Cotrimoxazole prophylaxis for n n n n n supplementation Tetanus toxoid Deworming in pregnancy Detection and treatment of asymptomatic bacteriuria Treatment of syphilis in pregnancy Prevention and treatment of iron deficiency anemia in pregnancy Intermittent preventive treatment (IPTp) for malaria in pregnancy Balanced protein energy supplements for pregnant women Supplementation in pregnancy with multi-micronutrients n n HIV+ Measles immunization BCG immunization OPV immunization DPT immunization Hib immunization Hepatitis B immunization Yellow fever immunization Meningitis immunization Pneumococcal immunization Rotavirus immunization Neonatal Vitamin A supplementation Vitamin A - supplementation Zinc preventive
 Individual clinical interventions (3) n Skilled attended delivery n Basic emergency obstetric care (Bn n n n n EOC) Resuscitation of asphyctic newborns at birth Antenatal steroids for preterm labor Antibiotics for Preterm/Prelabour Rupture of Membrane (P/PROM) Detection and management of (pre)ecclampsia (Mg Sulphate) Management of neonatal infections Antibiotics for U 5 pneumonia Antibiotics for diarrhea and enteric fevers Vitamin A - Treatment for measles Zinc for diarrhea management Clinical management of neonatal jaundice n Management of severely sick children (referral IMCI) n Chloroquine for malaria (P. vivax) n Artemisinin-based Combination Therapy n Management of complicated malaria (2 nd line drug)
Individual clinical interventions (3) n Skilled attended delivery n Basic emergency obstetric care (Bn n n n n EOC) Resuscitation of asphyctic newborns at birth Antenatal steroids for preterm labor Antibiotics for Preterm/Prelabour Rupture of Membrane (P/PROM) Detection and management of (pre)ecclampsia (Mg Sulphate) Management of neonatal infections Antibiotics for U 5 pneumonia Antibiotics for diarrhea and enteric fevers Vitamin A - Treatment for measles Zinc for diarrhea management Clinical management of neonatal jaundice n Management of severely sick children (referral IMCI) n Chloroquine for malaria (P. vivax) n Artemisinin-based Combination Therapy n Management of complicated malaria (2 nd line drug)
 Individual clinical interventions (3) n Management of opportunistic n n n infections Male circumcision Second-line ART Adult second-line ART Comprehensive emergency obstetric care (C-EOC) Other emergency acute care n Detection and management n n n of STI Management of opportunistic infections First line ART Detection and treatment of TB with first line drugs (category 1 and 3) Re-treatment of TB patients with first line drugs (category 2) MDR treatement with second line drugs
Individual clinical interventions (3) n Management of opportunistic n n n infections Male circumcision Second-line ART Adult second-line ART Comprehensive emergency obstetric care (C-EOC) Other emergency acute care n Detection and management n n n of STI Management of opportunistic infections First line ART Detection and treatment of TB with first line drugs (category 1 and 3) Re-treatment of TB patients with first line drugs (category 2) MDR treatement with second line drugs
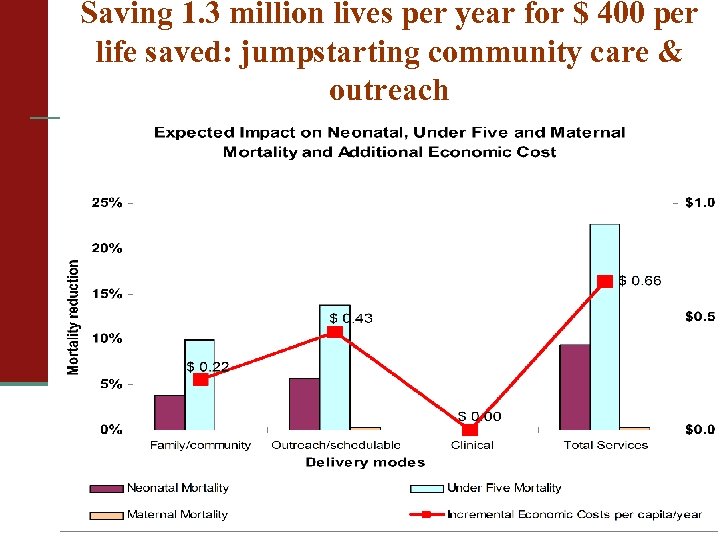 Saving 1. 3 million lives per year for $ 400 per life saved: jumpstarting community care & outreach
Saving 1. 3 million lives per year for $ 400 per life saved: jumpstarting community care & outreach
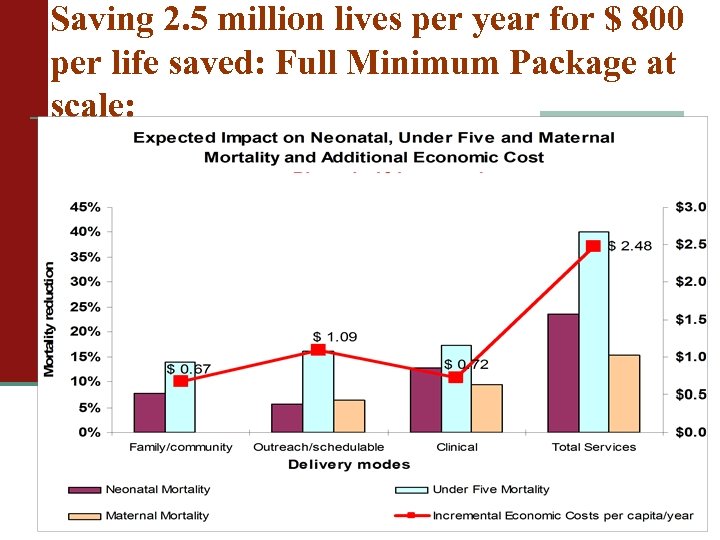 Saving 2. 5 million lives per year for $ 800 per life saved: Full Minimum Package at scale:
Saving 2. 5 million lives per year for $ 800 per life saved: Full Minimum Package at scale:
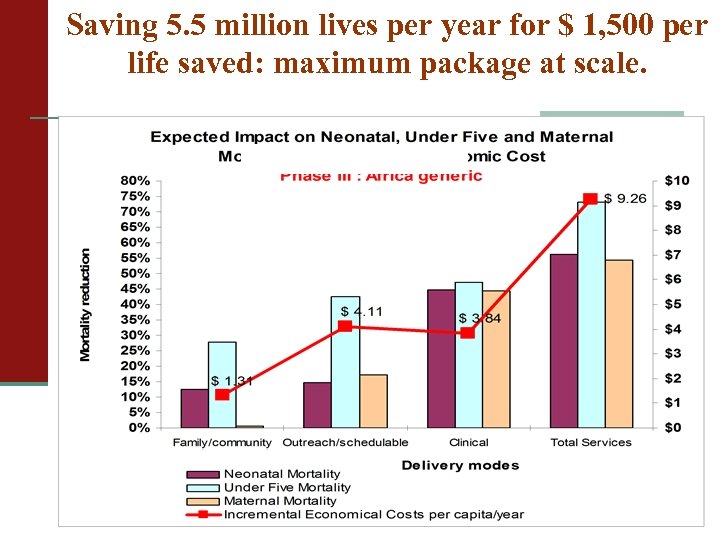 Saving 5. 5 million lives per year for $ 1, 500 per life saved: maximum package at scale.
Saving 5. 5 million lives per year for $ 1, 500 per life saved: maximum package at scale.
 So why is it not happening ?
So why is it not happening ?
 Countries use well-designed policies to achieve growth rs no and human development do s/ nt e outcomes m rn ve o G Health, Education, Poverty * er S ce vi s But…
Countries use well-designed policies to achieve growth rs no and human development do s/ nt e outcomes m rn ve o G Health, Education, Poverty * er S ce vi s But…
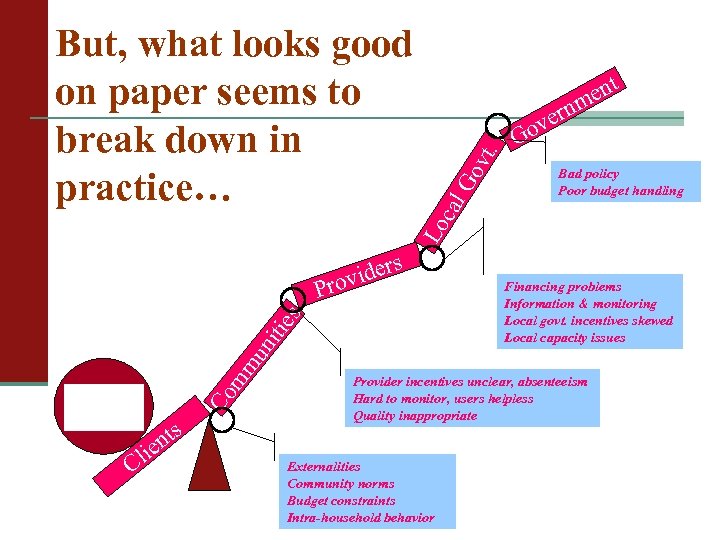 r vide ro vt. Leakage of Funds Bad policy Poor budget handling Go ies Co mm u nit nts lie C G cal s P Primary education ent m n ver o Lo But, what looks good on paper seems to break down in practice… Sub-optimal spending (Big salary bills but insufficient textbooks & materials) Financing problems Information & monitoring Local govt. incentives skewed Local capacity issues Low quality instruction Provider incentives unclear, absenteeism Hard to monitor, users helpless Quality inappropriate Lack of demand Externalities Community norms Budget constraints Intra-household behavior
r vide ro vt. Leakage of Funds Bad policy Poor budget handling Go ies Co mm u nit nts lie C G cal s P Primary education ent m n ver o Lo But, what looks good on paper seems to break down in practice… Sub-optimal spending (Big salary bills but insufficient textbooks & materials) Financing problems Information & monitoring Local govt. incentives skewed Local capacity issues Low quality instruction Provider incentives unclear, absenteeism Hard to monitor, users helpless Quality inappropriate Lack of demand Externalities Community norms Budget constraints Intra-household behavior
 Budgeting for results
Budgeting for results
 Results-based Financing Donors Sub-National Government District National Governme nt Results Based Aid Results Based Planning and Budgeting Results Based Contracting for CCT, RB bonuses Hospitals, Health Centers, Ass Households or Individuals
Results-based Financing Donors Sub-National Government District National Governme nt Results Based Aid Results Based Planning and Budgeting Results Based Contracting for CCT, RB bonuses Hospitals, Health Centers, Ass Households or Individuals
 Steps in Results-Based Budgeting Step 1: Health Systems and High Impact Interventions • Analyze health systems. • Identify major U 5 MR, NNMR, MMR Step 2: System Bottlenecks to Coverage • Analyze household surveys and service statistics, using six coverage determinants, to identify system bottlenecks to coverage & causes. • Supply side: availability of essential commodities, availability of human resources, and physical access. • Demand side: initial and timely continuous Utilization; Effective quality coverage. • Analyze strategies to address bottlenecks and set new coverage frontiers. causes. • Identify high impact health, nutrition, AIDS, & malaria interventions (level 1 -2 evidence). • Organize interventions into 3 service • delivery modes: Family oriented community-based; Population oriented schedulable; and individual oriented clinical services. • Select representative tracer interventions for each sub-package of interventions. Step 5: Budgeting and Fiscal Space • Translate marginal cost into yearly additional budget figures. • Link budget figures to national sector plans, MTEF, PRSP, and other programs. • Facilitate analysis on financing sources. • Evaluate additional funding requirement against the fiscal space for health. Step 4: Estimating Marginal Cost • Estimate marginal costs to overcome the bottlenecks and achieve new performance frontiers. • Region/country specific inputs and cost structures. Step 3: Estimating Impact • Epidemiometric model. • Estimate the impact (reduction in mortality) of overcoming the bottlenecks based on local causes of NNMR, U 5 MR and MMR. • Sources include: MDG 1 (Emory), MDG 4 (Bellagio), MDG 5 (WHO/ WB Cochran; BMJ), and MDG 6 (RBM, UNAIDS).
Steps in Results-Based Budgeting Step 1: Health Systems and High Impact Interventions • Analyze health systems. • Identify major U 5 MR, NNMR, MMR Step 2: System Bottlenecks to Coverage • Analyze household surveys and service statistics, using six coverage determinants, to identify system bottlenecks to coverage & causes. • Supply side: availability of essential commodities, availability of human resources, and physical access. • Demand side: initial and timely continuous Utilization; Effective quality coverage. • Analyze strategies to address bottlenecks and set new coverage frontiers. causes. • Identify high impact health, nutrition, AIDS, & malaria interventions (level 1 -2 evidence). • Organize interventions into 3 service • delivery modes: Family oriented community-based; Population oriented schedulable; and individual oriented clinical services. • Select representative tracer interventions for each sub-package of interventions. Step 5: Budgeting and Fiscal Space • Translate marginal cost into yearly additional budget figures. • Link budget figures to national sector plans, MTEF, PRSP, and other programs. • Facilitate analysis on financing sources. • Evaluate additional funding requirement against the fiscal space for health. Step 4: Estimating Marginal Cost • Estimate marginal costs to overcome the bottlenecks and achieve new performance frontiers. • Region/country specific inputs and cost structures. Step 3: Estimating Impact • Epidemiometric model. • Estimate the impact (reduction in mortality) of overcoming the bottlenecks based on local causes of NNMR, U 5 MR and MMR. • Sources include: MDG 1 (Emory), MDG 4 (Bellagio), MDG 5 (WHO/ WB Cochran; BMJ), and MDG 6 (RBM, UNAIDS).
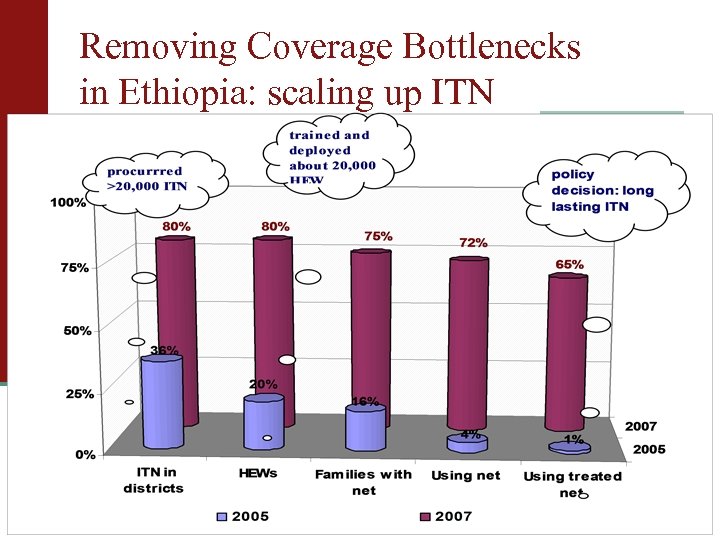 Removing Coverage Bottlenecks in Ethiopia: scaling up ITN
Removing Coverage Bottlenecks in Ethiopia: scaling up ITN
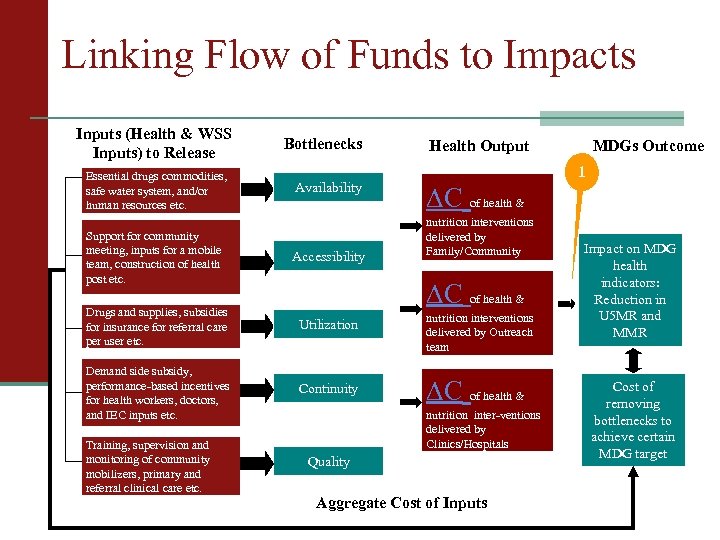 Linking Flow of Funds to Impacts Inputs (Health & WSS Inputs) to Release Essential drugs commodities, safe water system, and/or human resources etc. Bottlenecks Availability 1 ∆C of health & nutrition interventions delivered by Family/Community Support for community meeting, inputs for a mobile team, construction of health post etc. Accessibility Drugs and supplies, subsidies for insurance for referral care per user etc. Utilization nutrition interventions delivered by Outreach team Demand side subsidy, performance-based incentives for health workers, doctors, and IEC inputs etc. Continuity ∆C of health & Training, supervision and monitoring of community mobilizers, primary and referral clinical care etc. MDGs Outcome Health Output ∆C of health & nutrition inter-ventions delivered by Clinics/Hospitals Quality Aggregate Cost of Inputs Impact on MDG health indicators: Reduction in U 5 MR and MMR Cost of removing bottlenecks to achieve certain MDG target
Linking Flow of Funds to Impacts Inputs (Health & WSS Inputs) to Release Essential drugs commodities, safe water system, and/or human resources etc. Bottlenecks Availability 1 ∆C of health & nutrition interventions delivered by Family/Community Support for community meeting, inputs for a mobile team, construction of health post etc. Accessibility Drugs and supplies, subsidies for insurance for referral care per user etc. Utilization nutrition interventions delivered by Outreach team Demand side subsidy, performance-based incentives for health workers, doctors, and IEC inputs etc. Continuity ∆C of health & Training, supervision and monitoring of community mobilizers, primary and referral clinical care etc. MDGs Outcome Health Output ∆C of health & nutrition inter-ventions delivered by Clinics/Hospitals Quality Aggregate Cost of Inputs Impact on MDG health indicators: Reduction in U 5 MR and MMR Cost of removing bottlenecks to achieve certain MDG target
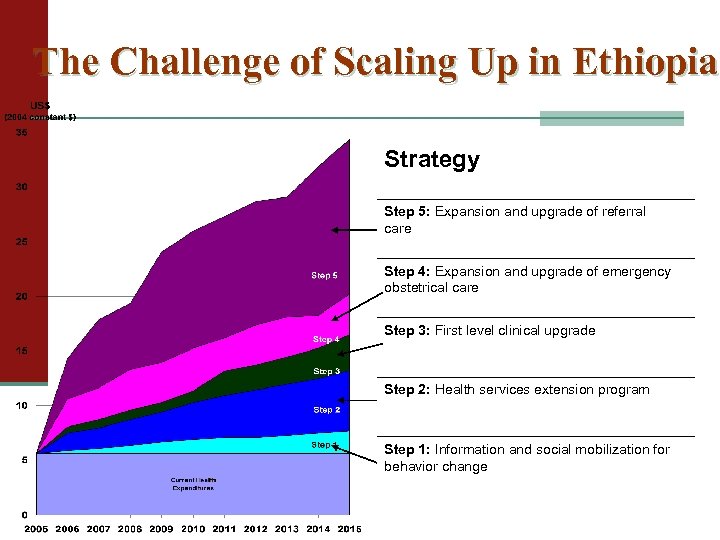 The Challenge of Scaling Up in Ethiopia Strategy Step 5: Expansion and upgrade of referral care Step 4: Expansion and upgrade of emergency obstetrical care Step 3: First level clinical upgrade Step 2: Health services extension program Step 1: Information and social mobilization for behavior change
The Challenge of Scaling Up in Ethiopia Strategy Step 5: Expansion and upgrade of referral care Step 4: Expansion and upgrade of emergency obstetrical care Step 3: First level clinical upgrade Step 2: Health services extension program Step 1: Information and social mobilization for behavior change
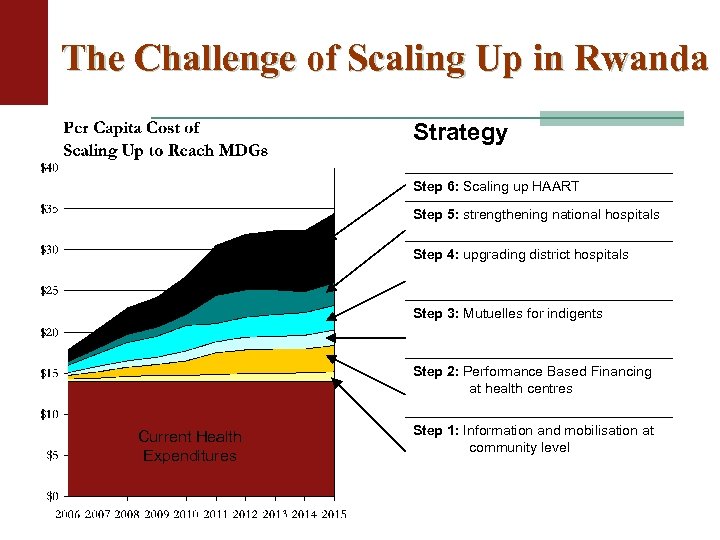 The Challenge of Scaling Up in Rwanda Strategy Step 6: Scaling up HAART Step 5: strengthening national hospitals Step 4: upgrading district hospitals Step 3: Mutuelles for indigents Step 2: Performance Based Financing at health centres Current Health Expenditures Step 1: Information and mobilisation at community level
The Challenge of Scaling Up in Rwanda Strategy Step 6: Scaling up HAART Step 5: strengthening national hospitals Step 4: upgrading district hospitals Step 3: Mutuelles for indigents Step 2: Performance Based Financing at health centres Current Health Expenditures Step 1: Information and mobilisation at community level
 Results ?
Results ?
 Dramatic decrease of malaria in Rwanda n Malaria out patient n Non Malaria out patient
Dramatic decrease of malaria in Rwanda n Malaria out patient n Non Malaria out patient
 Rwanda 2005 -2008 Indicators Contraceptive prevalence: Modern methods Delivery in Health Centers Infant Mortality rate Under-Five Mortality rate Anemia Prevalence : Children Anemia Prevalence : Women Vaccination : All Vaccination : Measles Use of Insecticide treated nets among children less than 5 Fertility DHS-2005 10% DHS-2008 27% 39% 52% 86 per 1000 152 per 1000 56% 33% 75% 86% 4% 62 per 1000 103 per 1000 48% 27% 80. 4% 90% 67% 6. 1 children 5. 5 children
Rwanda 2005 -2008 Indicators Contraceptive prevalence: Modern methods Delivery in Health Centers Infant Mortality rate Under-Five Mortality rate Anemia Prevalence : Children Anemia Prevalence : Women Vaccination : All Vaccination : Measles Use of Insecticide treated nets among children less than 5 Fertility DHS-2005 10% DHS-2008 27% 39% 52% 86 per 1000 152 per 1000 56% 33% 75% 86% 4% 62 per 1000 103 per 1000 48% 27% 80. 4% 90% 67% 6. 1 children 5. 5 children
 Rwanda: back on track for the MDGs
Rwanda: back on track for the MDGs


