ce62aa37bdd7765aafc3d178af84e224.ppt
- Количество слайдов: 67
 Radiation Therapy of Lung Cancer National Cheng Kung University Medical Center Department of Radiation Oncology 楊明維 醫師
Radiation Therapy of Lung Cancer National Cheng Kung University Medical Center Department of Radiation Oncology 楊明維 醫師
 Basis for Prescription of Irradiation Patient’s general condition Pathologic characteristics of the disease Tumor extent (staging) Goal of therapy (cure or palliation) Treatment modalities Dose of irradiation and volume
Basis for Prescription of Irradiation Patient’s general condition Pathologic characteristics of the disease Tumor extent (staging) Goal of therapy (cure or palliation) Treatment modalities Dose of irradiation and volume
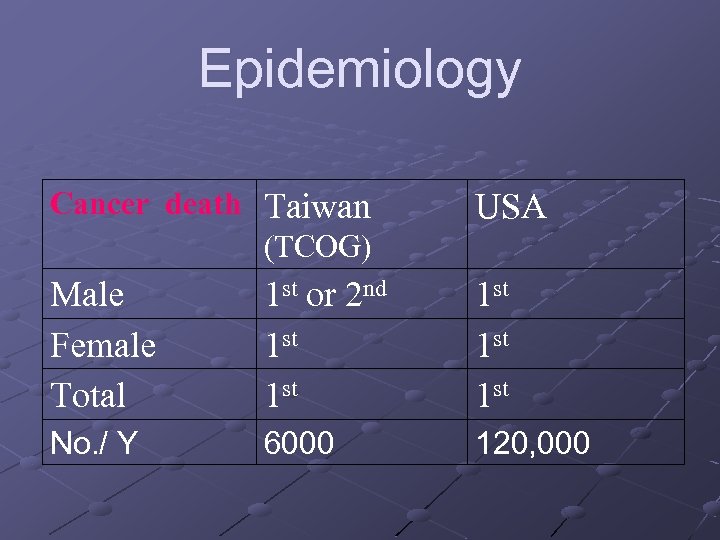 Epidemiology Cancer death Taiwan (TCOG) USA Male Female Total 1 st or 2 nd 1 st 1 st 1 st No. / Y 6000 120, 000
Epidemiology Cancer death Taiwan (TCOG) USA Male Female Total 1 st or 2 nd 1 st 1 st 1 st No. / Y 6000 120, 000
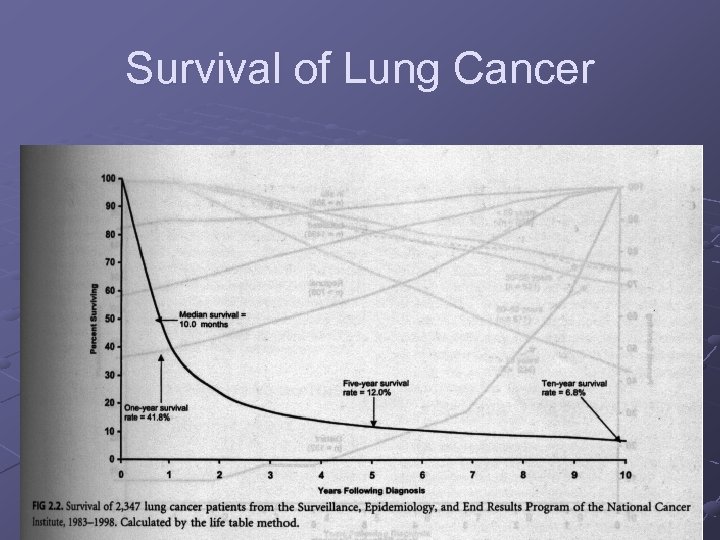 Survival of Lung Cancer
Survival of Lung Cancer
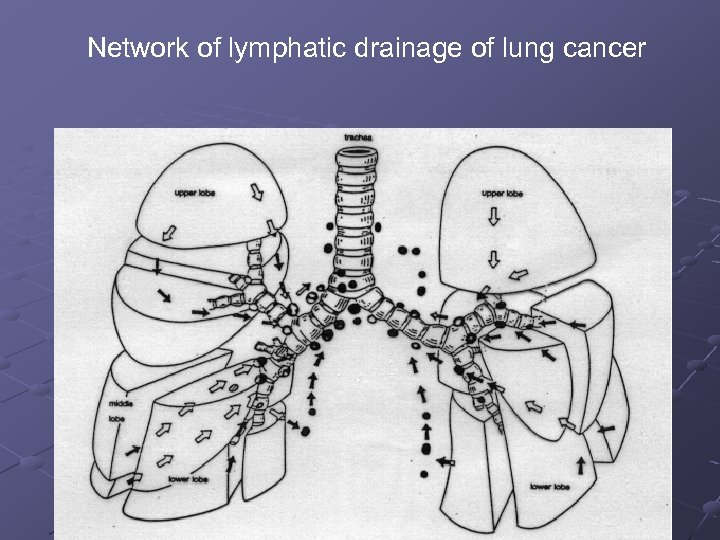 Network of lymphatic drainage of lung cancer
Network of lymphatic drainage of lung cancer
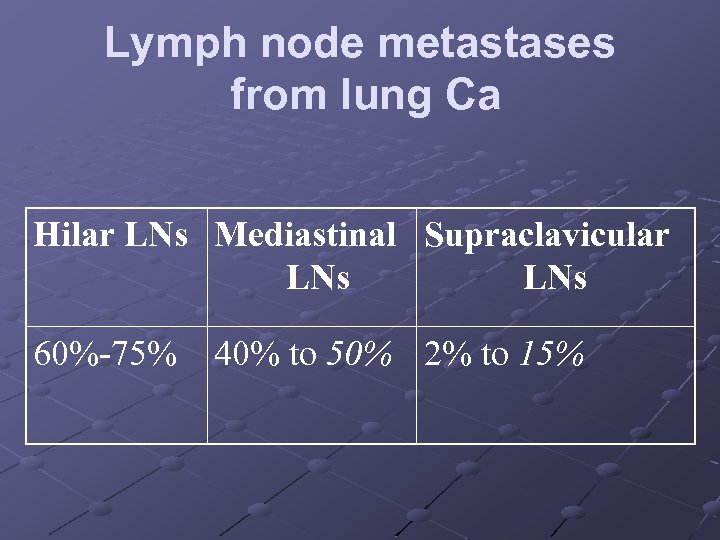 Lymph node metastases from lung Ca Hilar LNs Mediastinal Supraclavicular LNs 60%-75% 40% to 50% 2% to 15%
Lymph node metastases from lung Ca Hilar LNs Mediastinal Supraclavicular LNs 60%-75% 40% to 50% 2% to 15%
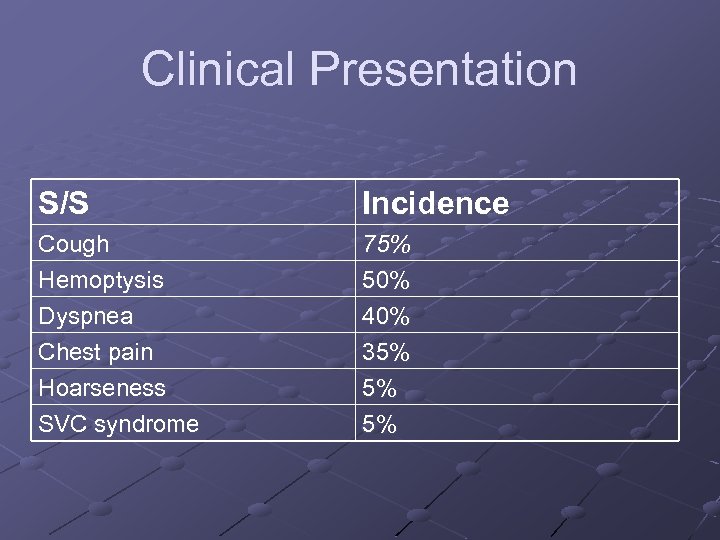 Clinical Presentation S/S Incidence Cough Hemoptysis Dyspnea Chest pain Hoarseness SVC syndrome 75% 50% 40% 35% 5% 5%
Clinical Presentation S/S Incidence Cough Hemoptysis Dyspnea Chest pain Hoarseness SVC syndrome 75% 50% 40% 35% 5% 5%
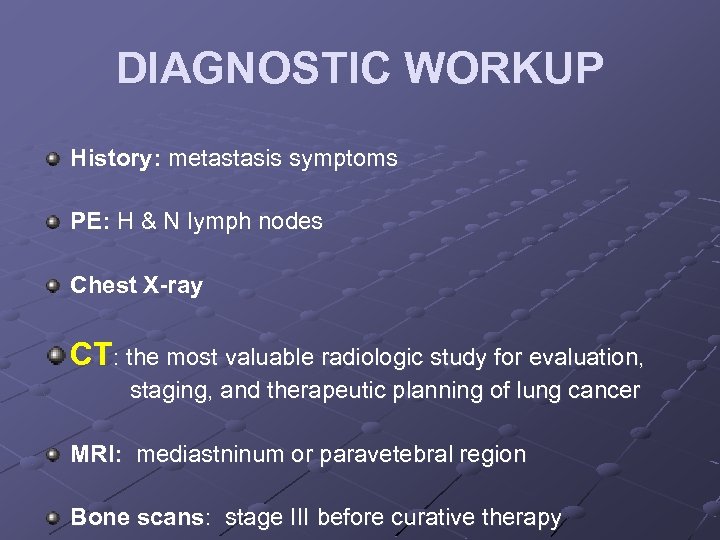 DIAGNOSTIC WORKUP History: metastasis symptoms PE: H & N lymph nodes Chest X-ray CT: the most valuable radiologic study for evaluation, staging, and therapeutic planning of lung cancer MRI: mediastninum or paravetebral region Bone scans: stage III before curative therapy
DIAGNOSTIC WORKUP History: metastasis symptoms PE: H & N lymph nodes Chest X-ray CT: the most valuable radiologic study for evaluation, staging, and therapeutic planning of lung cancer MRI: mediastninum or paravetebral region Bone scans: stage III before curative therapy
 PET influenced radiation delivery in 65% for definitive radiotherapy (Kalff et al. ). Brain CT scan: small cell carcinoma. Pulmonary function tests: ability to undergo surgical resection or withstand irradiation
PET influenced radiation delivery in 65% for definitive radiotherapy (Kalff et al. ). Brain CT scan: small cell carcinoma. Pulmonary function tests: ability to undergo surgical resection or withstand irradiation
 Sputum cytology: 20% to 30% sensitivity Bronchoscopic examination: 90% positive CT-guided Bx: 95% positive Bx: Primary tumor lesion, scalene node
Sputum cytology: 20% to 30% sensitivity Bronchoscopic examination: 90% positive CT-guided Bx: 95% positive Bx: Primary tumor lesion, scalene node
 Pathology Sputum cytology: 20% to 30% sensitivity Bronchoscopic examination: 90% positive CT-guided Bx: 95% positive Bx: Primary tumor lesion, scalene node
Pathology Sputum cytology: 20% to 30% sensitivity Bronchoscopic examination: 90% positive CT-guided Bx: 95% positive Bx: Primary tumor lesion, scalene node
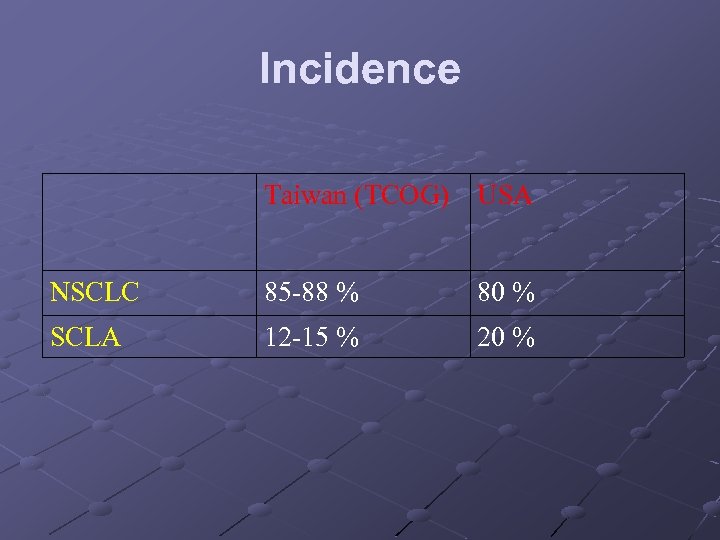 Incidence Taiwan (TCOG) USA NSCLC 85 -88 % 80 % SCLA 12 -15 % 20 %
Incidence Taiwan (TCOG) USA NSCLC 85 -88 % 80 % SCLA 12 -15 % 20 %
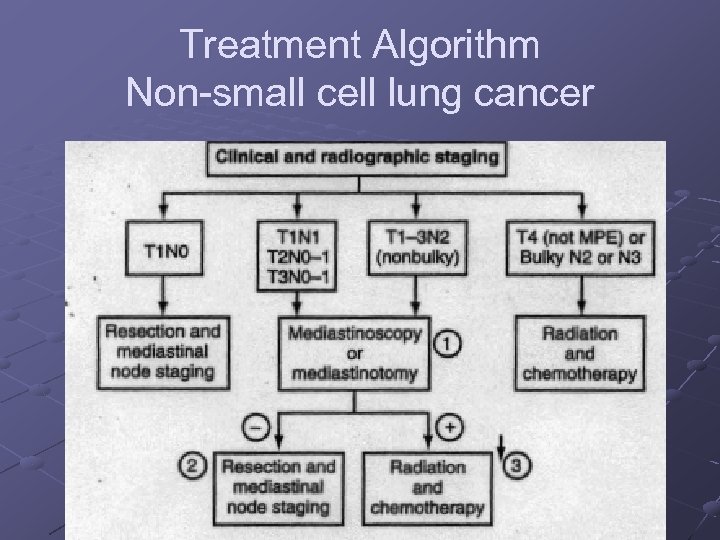 Treatment Algorithm Non small cell lung cancer
Treatment Algorithm Non small cell lung cancer
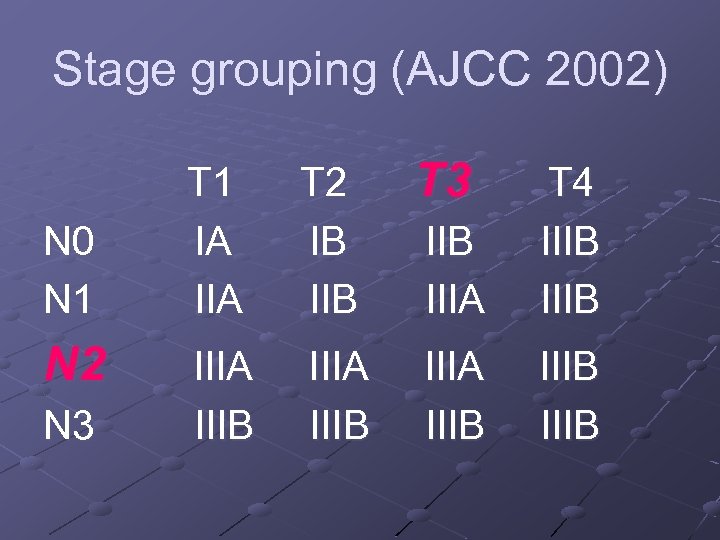 Stage grouping (AJCC 2002) N 0 N 1 N 2 N 3 T 1 IA IIA T 2 IB IIB T 3 IIB IIIA T 4 IIIB IIIA IIIB
Stage grouping (AJCC 2002) N 0 N 1 N 2 N 3 T 1 IA IIA T 2 IB IIB T 3 IIB IIIA T 4 IIIB IIIA IIIB
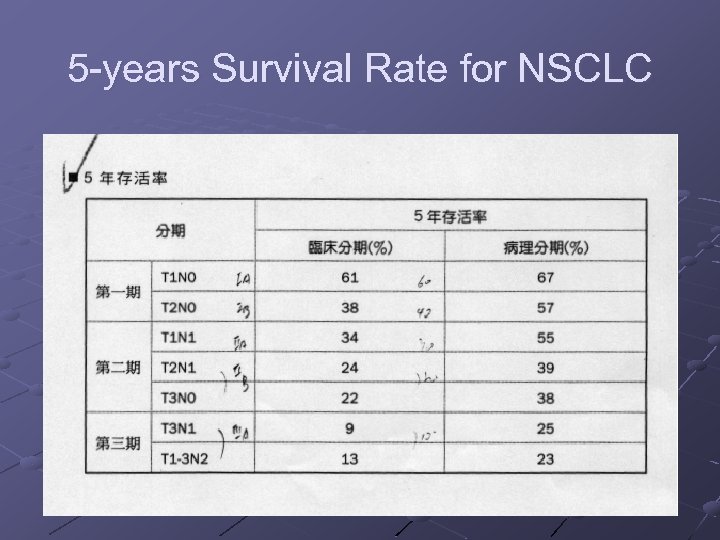 5 years Survival Rate for NSCLC
5 years Survival Rate for NSCLC
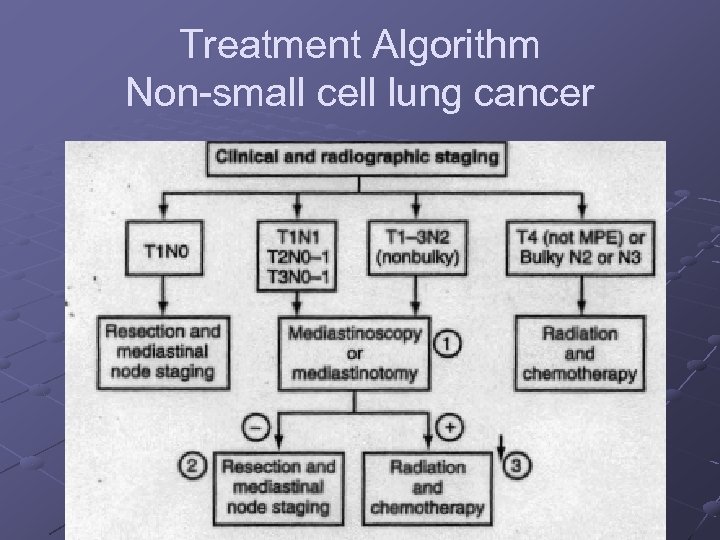 Treatment Algorithm Non small cell lung cancer
Treatment Algorithm Non small cell lung cancer
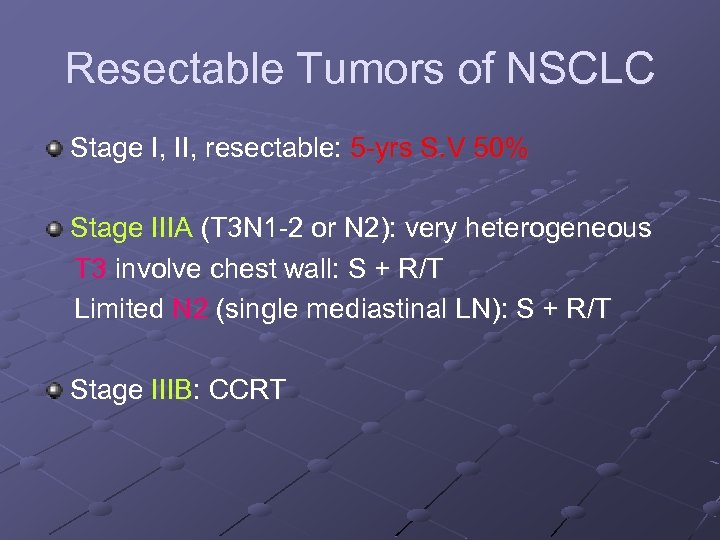 Resectable Tumors of NSCLC Stage I, II, resectable: 5 yrs S. V 50% Stage IIIA (T 3 N 1 2 or N 2): very heterogeneous T 3 involve chest wall: S + R/T Limited N 2 (single mediastinal LN): S + R/T Stage IIIB: CCRT
Resectable Tumors of NSCLC Stage I, II, resectable: 5 yrs S. V 50% Stage IIIA (T 3 N 1 2 or N 2): very heterogeneous T 3 involve chest wall: S + R/T Limited N 2 (single mediastinal LN): S + R/T Stage IIIB: CCRT
 Preoperative Irradiation Failed to show significant improvement in resectability or survival with use of preoperative irradiation.
Preoperative Irradiation Failed to show significant improvement in resectability or survival with use of preoperative irradiation.
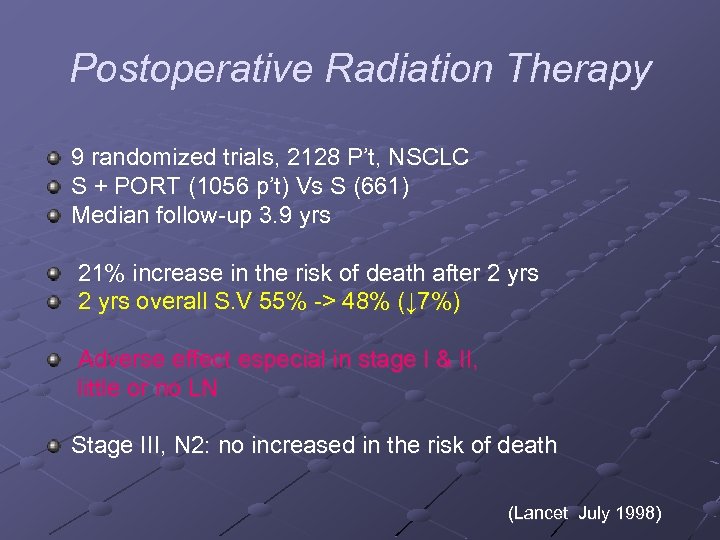 Postoperative Radiation Therapy 9 randomized trials, 2128 P’t, NSCLC S + PORT (1056 p’t) Vs S (661) Median follow up 3. 9 yrs 21% increase in the risk of death after 2 yrs overall S. V 55% > 48% (↓ 7%) Adverse effect especial in stage I & II, little or no LN Stage III, N 2: no increased in the risk of death (Lancet July 1998)
Postoperative Radiation Therapy 9 randomized trials, 2128 P’t, NSCLC S + PORT (1056 p’t) Vs S (661) Median follow up 3. 9 yrs 21% increase in the risk of death after 2 yrs overall S. V 55% > 48% (↓ 7%) Adverse effect especial in stage I & II, little or no LN Stage III, N 2: no increased in the risk of death (Lancet July 1998)
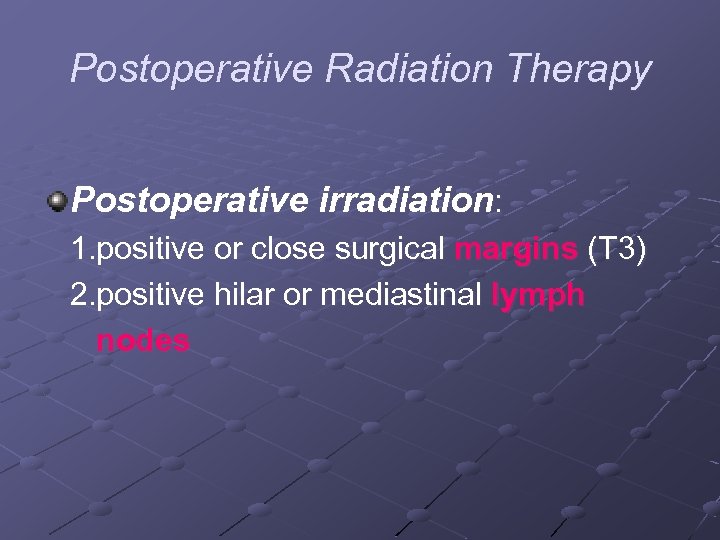 Postoperative Radiation Therapy Postoperative irradiation: 1. positive or close surgical margins (T 3) 2. positive hilar or mediastinal lymph nodes
Postoperative Radiation Therapy Postoperative irradiation: 1. positive or close surgical margins (T 3) 2. positive hilar or mediastinal lymph nodes
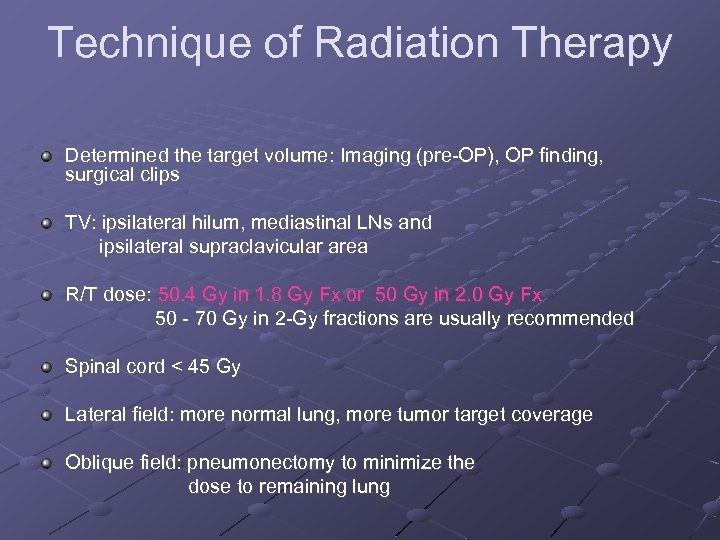 Technique of Radiation Therapy Determined the target volume: Imaging (pre OP), OP finding, surgical clips TV: ipsilateral hilum, mediastinal LNs and ipsilateral supraclavicular area R/T dose: 50. 4 Gy in 1. 8 Gy Fx or 50 Gy in 2. 0 Gy Fx 50 70 Gy in 2 Gy fractions are usually recommended Spinal cord < 45 Gy Lateral field: more normal lung, more tumor target coverage Oblique field: pneumonectomy to minimize the dose to remaining lung
Technique of Radiation Therapy Determined the target volume: Imaging (pre OP), OP finding, surgical clips TV: ipsilateral hilum, mediastinal LNs and ipsilateral supraclavicular area R/T dose: 50. 4 Gy in 1. 8 Gy Fx or 50 Gy in 2. 0 Gy Fx 50 70 Gy in 2 Gy fractions are usually recommended Spinal cord < 45 Gy Lateral field: more normal lung, more tumor target coverage Oblique field: pneumonectomy to minimize the dose to remaining lung
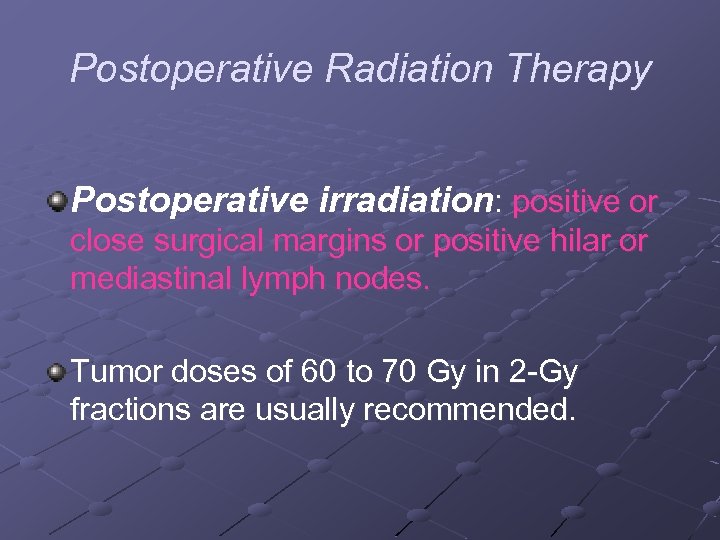 Postoperative Radiation Therapy Postoperative irradiation: positive or close surgical margins or positive hilar or mediastinal lymph nodes. Tumor doses of 60 to 70 Gy in 2 Gy fractions are usually recommended.
Postoperative Radiation Therapy Postoperative irradiation: positive or close surgical margins or positive hilar or mediastinal lymph nodes. Tumor doses of 60 to 70 Gy in 2 Gy fractions are usually recommended.
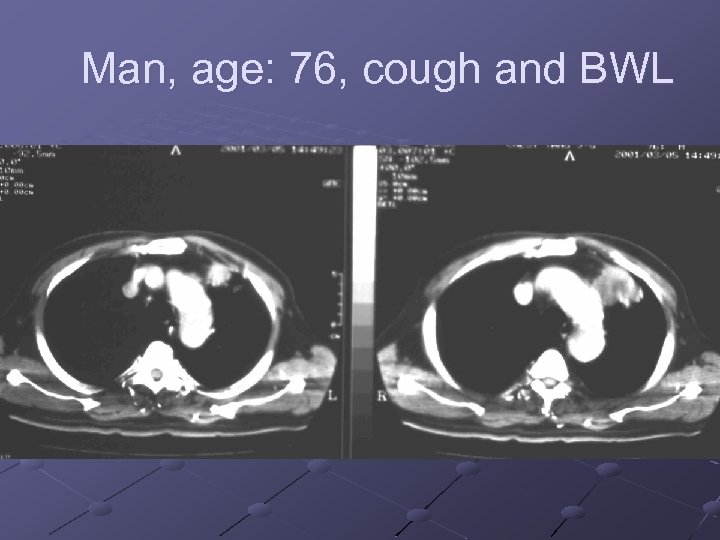 Man, age: 76, cough and BWL
Man, age: 76, cough and BWL
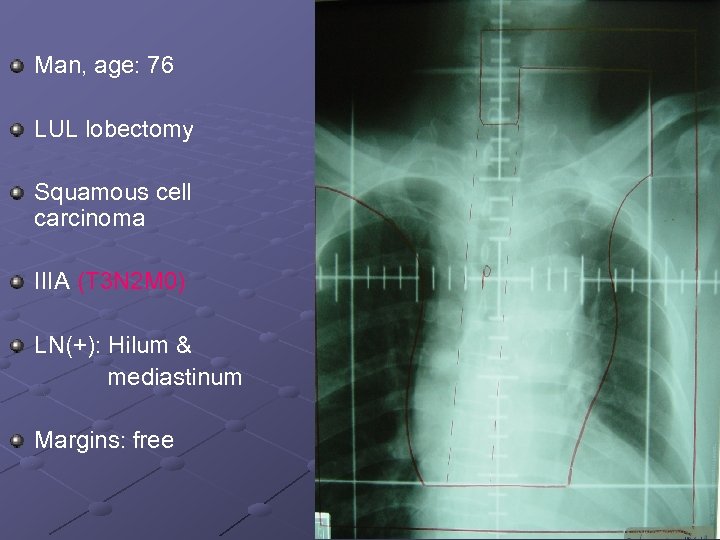 Man, age: 76 LUL lobectomy Squamous cell carcinoma IIIA (T 3 N 2 M 0) LN(+): Hilum & mediastinum Margins: free
Man, age: 76 LUL lobectomy Squamous cell carcinoma IIIA (T 3 N 2 M 0) LN(+): Hilum & mediastinum Margins: free
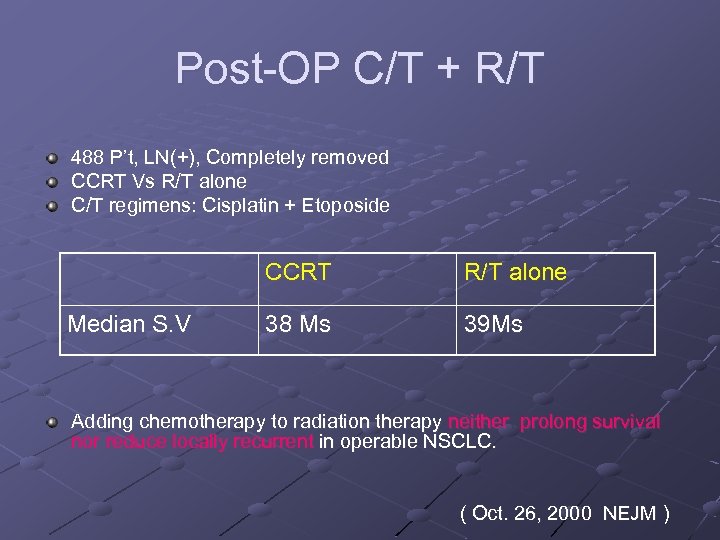 Post OP C/T + R/T 488 P’t, LN(+), Completely removed CCRT Vs R/T alone C/T regimens: Cisplatin + Etoposide CCRT Median S. V R/T alone 38 Ms 39 Ms Adding chemotherapy to radiation therapy neither prolong survival nor reduce locally recurrent in operable NSCLC. ( Oct. 26, 2000 NEJM )
Post OP C/T + R/T 488 P’t, LN(+), Completely removed CCRT Vs R/T alone C/T regimens: Cisplatin + Etoposide CCRT Median S. V R/T alone 38 Ms 39 Ms Adding chemotherapy to radiation therapy neither prolong survival nor reduce locally recurrent in operable NSCLC. ( Oct. 26, 2000 NEJM )
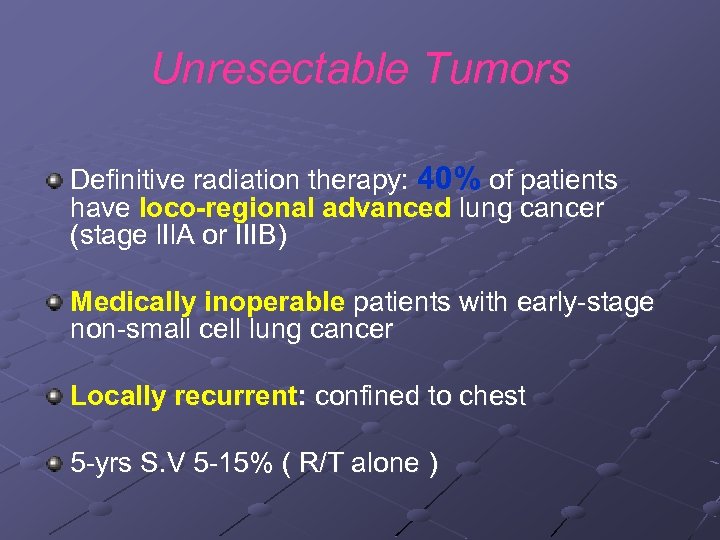 Unresectable Tumors Definitive radiation therapy: 40% of patients have loco-regional advanced lung cancer (stage l. Il. A or IIIB) Medically inoperable patients with early stage non small cell lung cancer Locally recurrent: confined to chest 5 yrs S. V 5 15% ( R/T alone )
Unresectable Tumors Definitive radiation therapy: 40% of patients have loco-regional advanced lung cancer (stage l. Il. A or IIIB) Medically inoperable patients with early stage non small cell lung cancer Locally recurrent: confined to chest 5 yrs S. V 5 15% ( R/T alone )
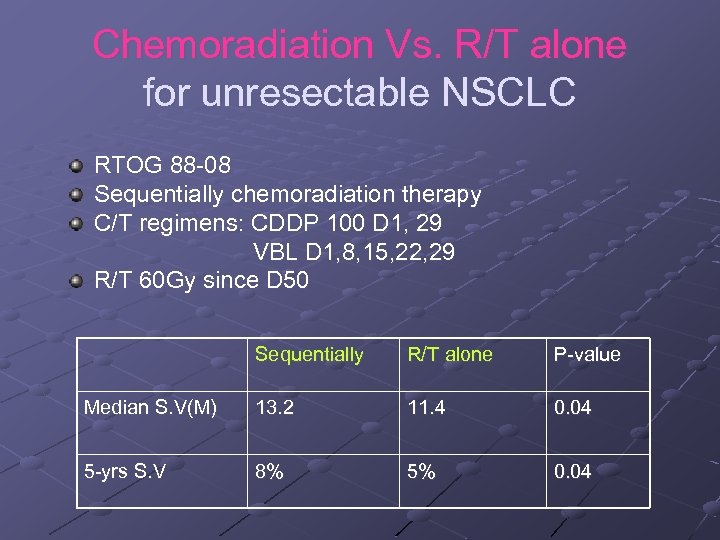 Chemoradiation Vs. R/T alone for unresectable NSCLC RTOG 88 08 Sequentially chemoradiation therapy C/T regimens: CDDP 100 D 1, 29 VBL D 1, 8, 15, 22, 29 R/T 60 Gy since D 50 Sequentially R/T alone P value Median S. V(M) 13. 2 11. 4 0. 04 5 yrs S. V 8% 5% 0. 04
Chemoradiation Vs. R/T alone for unresectable NSCLC RTOG 88 08 Sequentially chemoradiation therapy C/T regimens: CDDP 100 D 1, 29 VBL D 1, 8, 15, 22, 29 R/T 60 Gy since D 50 Sequentially R/T alone P value Median S. V(M) 13. 2 11. 4 0. 04 5 yrs S. V 8% 5% 0. 04
 Chemoradiation Therapy for unresectable NSCLC Good performance status No body weight loss or less No contraindication to C/T or R/T
Chemoradiation Therapy for unresectable NSCLC Good performance status No body weight loss or less No contraindication to C/T or R/T
 Chemotherapy alone Poorly pulmonary function for radiotherapy Malignant pleural effusion (T 4) or Metastasis (M 1) R/T for the aim of palliation
Chemotherapy alone Poorly pulmonary function for radiotherapy Malignant pleural effusion (T 4) or Metastasis (M 1) R/T for the aim of palliation
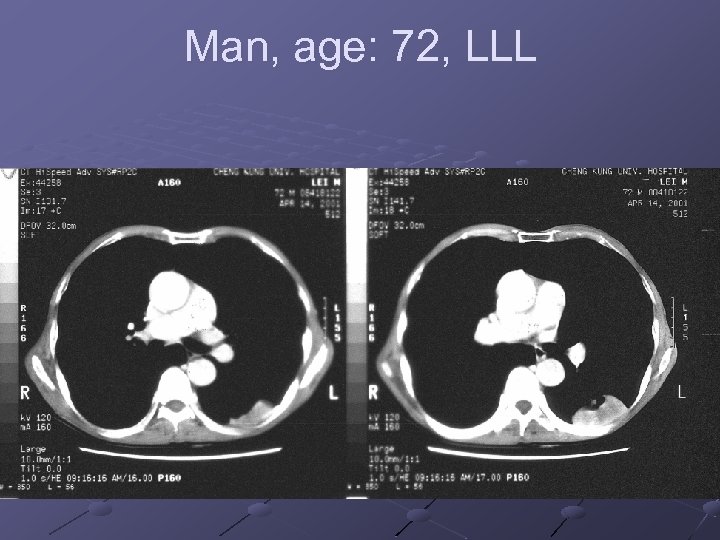 Man, age: 72, LLL
Man, age: 72, LLL
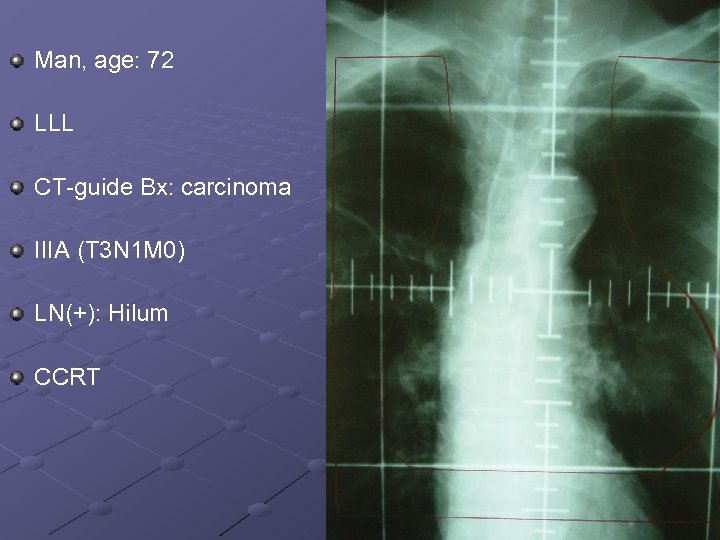 Man, age: 72 LLL CT guide Bx: carcinoma IIIA (T 3 N 1 M 0) LN(+): Hilum CCRT
Man, age: 72 LLL CT guide Bx: carcinoma IIIA (T 3 N 1 M 0) LN(+): Hilum CCRT
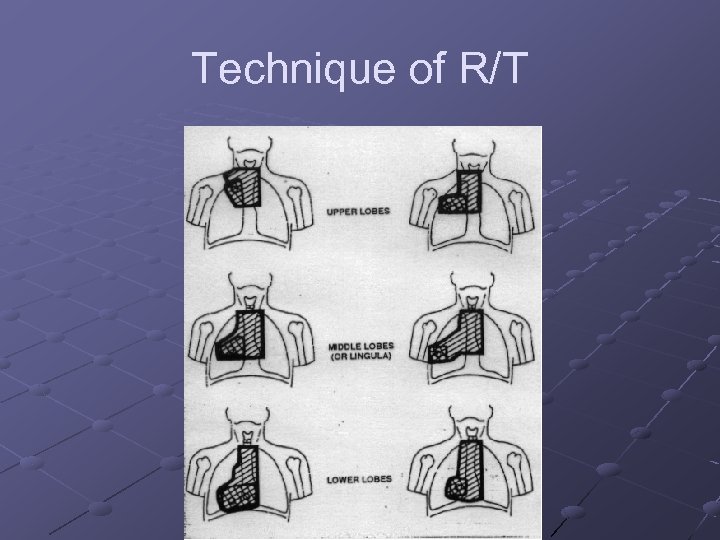 Technique of R/T
Technique of R/T
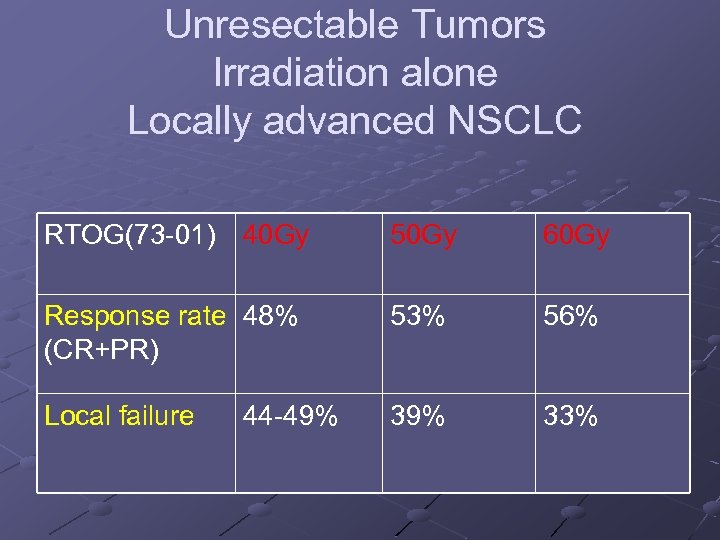 Unresectable Tumors Irradiation alone Locally advanced NSCLC RTOG(73 01) 40 Gy 50 Gy 60 Gy Response rate 48% (CR+PR) 53% 56% Local failure 39% 33% 44 49%
Unresectable Tumors Irradiation alone Locally advanced NSCLC RTOG(73 01) 40 Gy 50 Gy 60 Gy Response rate 48% (CR+PR) 53% 56% Local failure 39% 33% 44 49%
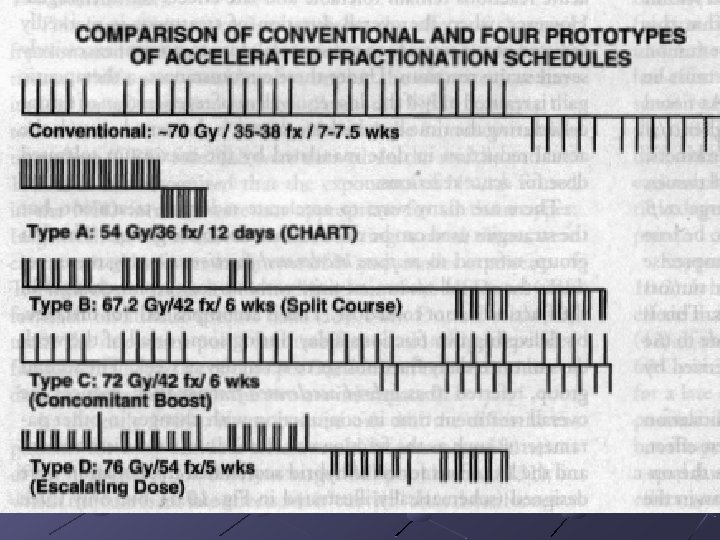
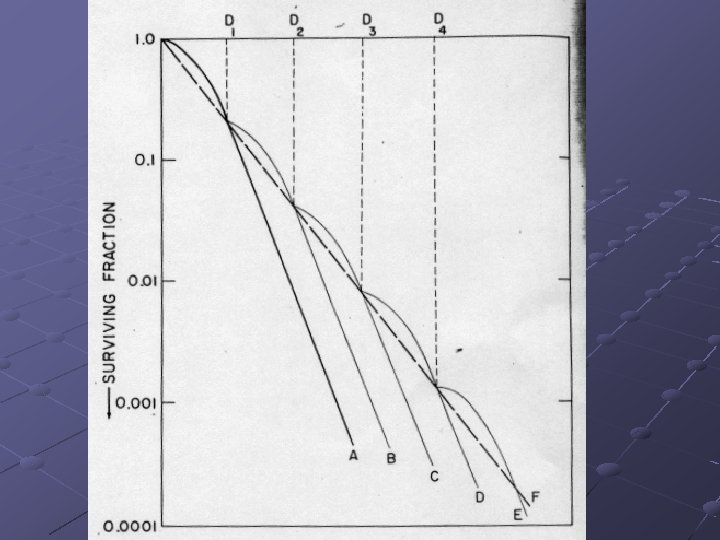
 Technique of Radiation Therapy Altered fractionation schemes Split-course radiation therapy Interval between the courses (2 4 wks) for acute toxicity recovery Cancer cell accelerated repopulation during the interval
Technique of Radiation Therapy Altered fractionation schemes Split-course radiation therapy Interval between the courses (2 4 wks) for acute toxicity recovery Cancer cell accelerated repopulation during the interval
 Technique of Radiation Therapy Altered fractionation schemes Hyperfractionated radiation scheme RTOG trial hyperfractionated radiation scheme 69. 6 Gy(Bid) Vs standard R/T 60 Gy Failed to show survival benefit for hyperfractionation Altered fractionation radiation therapy is not considered the “standard of care” (ASCO 1994; 13: 325)
Technique of Radiation Therapy Altered fractionation schemes Hyperfractionated radiation scheme RTOG trial hyperfractionated radiation scheme 69. 6 Gy(Bid) Vs standard R/T 60 Gy Failed to show survival benefit for hyperfractionation Altered fractionation radiation therapy is not considered the “standard of care” (ASCO 1994; 13: 325)
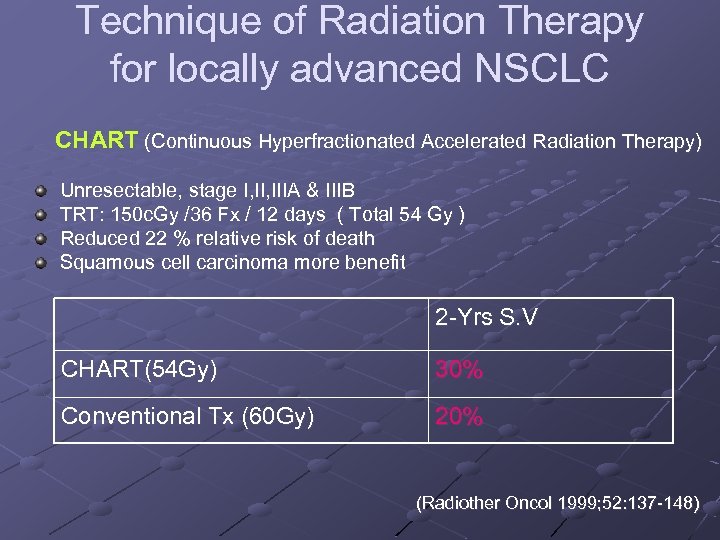 Technique of Radiation Therapy for locally advanced NSCLC CHART (Continuous Hyperfractionated Accelerated Radiation Therapy) Unresectable, stage I, IIIA & IIIB TRT: 150 c. Gy /36 Fx / 12 days ( Total 54 Gy ) Reduced 22 % relative risk of death Squamous cell carcinoma more benefit 2 Yrs S. V CHART(54 Gy) 30% Conventional Tx (60 Gy) 20% (Radiother Oncol 1999; 52: 137 148)
Technique of Radiation Therapy for locally advanced NSCLC CHART (Continuous Hyperfractionated Accelerated Radiation Therapy) Unresectable, stage I, IIIA & IIIB TRT: 150 c. Gy /36 Fx / 12 days ( Total 54 Gy ) Reduced 22 % relative risk of death Squamous cell carcinoma more benefit 2 Yrs S. V CHART(54 Gy) 30% Conventional Tx (60 Gy) 20% (Radiother Oncol 1999; 52: 137 148)
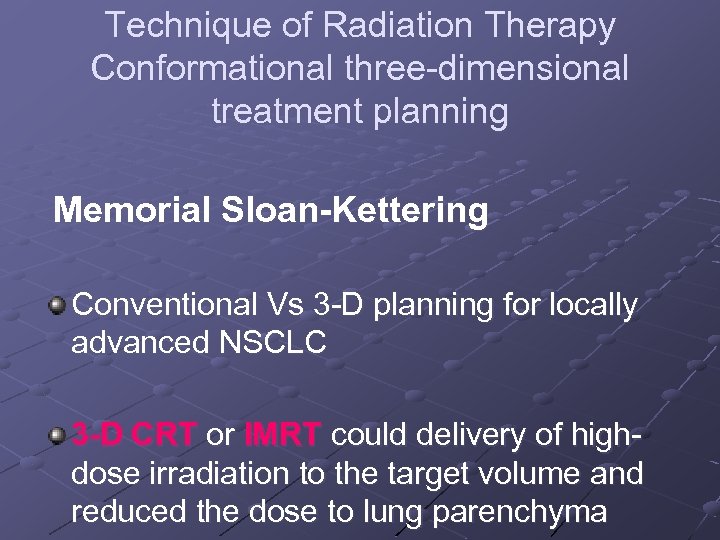 Technique of Radiation Therapy Conformational three dimensional treatment planning Memorial Sloan-Kettering Conventional Vs 3 D planning for locally advanced NSCLC 3 -D CRT or IMRT could delivery of high dose irradiation to the target volume and reduced the dose to lung parenchyma
Technique of Radiation Therapy Conformational three dimensional treatment planning Memorial Sloan-Kettering Conventional Vs 3 D planning for locally advanced NSCLC 3 -D CRT or IMRT could delivery of high dose irradiation to the target volume and reduced the dose to lung parenchyma
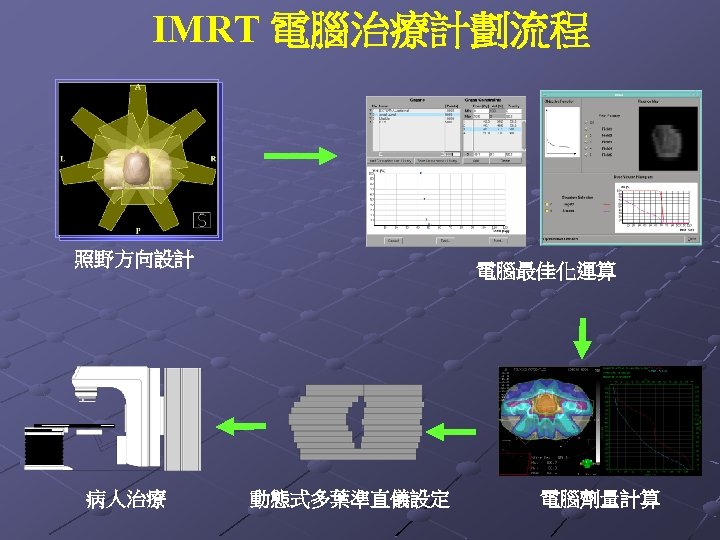 IMRT 電腦治療計劃流程 照野方向設計 病人治療 電腦最佳化運算 動態式多葉準直儀設定 電腦劑量計算
IMRT 電腦治療計劃流程 照野方向設計 病人治療 電腦最佳化運算 動態式多葉準直儀設定 電腦劑量計算
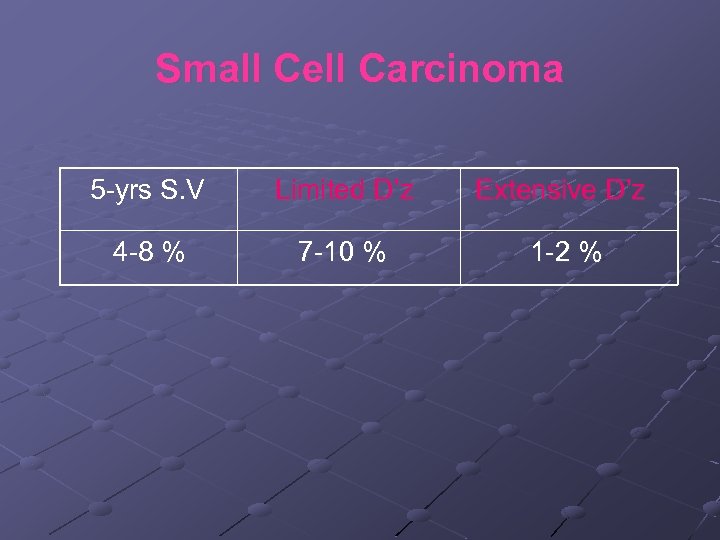 Small Cell Carcinoma 5 yrs S. V Limited D’z Extensive D’z 4 8 % 7 10 % 1 2 %
Small Cell Carcinoma 5 yrs S. V Limited D’z Extensive D’z 4 8 % 7 10 % 1 2 %
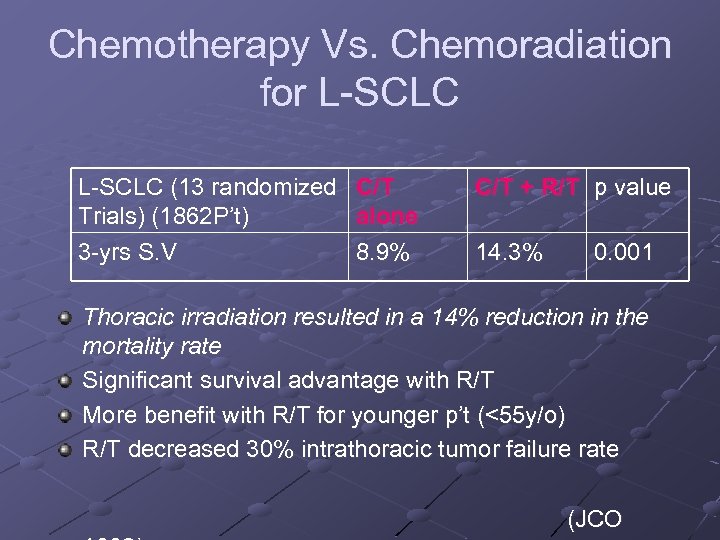 Chemotherapy Vs. Chemoradiation for L SCLC (13 randomized Trials) (1862 P’t) 3 yrs S. V C/T alone 8. 9% C/T + R/T p value 14. 3% 0. 001 Thoracic irradiation resulted in a 14% reduction in the mortality rate Significant survival advantage with R/T More benefit with R/T for younger p’t (<55 y/o) R/T decreased 30% intrathoracic tumor failure rate (JCO
Chemotherapy Vs. Chemoradiation for L SCLC (13 randomized Trials) (1862 P’t) 3 yrs S. V C/T alone 8. 9% C/T + R/T p value 14. 3% 0. 001 Thoracic irradiation resulted in a 14% reduction in the mortality rate Significant survival advantage with R/T More benefit with R/T for younger p’t (<55 y/o) R/T decreased 30% intrathoracic tumor failure rate (JCO
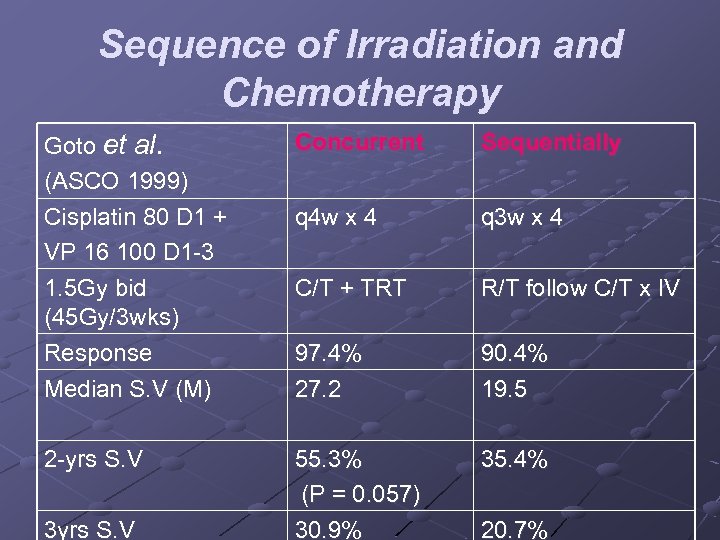 Sequence of Irradiation and Chemotherapy Goto et al. (ASCO 1999) Cisplatin 80 D 1 + VP 16 100 D 1 3 1. 5 Gy bid (45 Gy/3 wks) Response Median S. V (M) Concurrent Sequentially q 4 w x 4 q 3 w x 4 C/T + TRT R/T follow C/T x IV 97. 4% 27. 2 90. 4% 19. 5 2 yrs S. V 55. 3% (P = 0. 057) 30. 9% 35. 4% 3 yrs S. V 20. 7%
Sequence of Irradiation and Chemotherapy Goto et al. (ASCO 1999) Cisplatin 80 D 1 + VP 16 100 D 1 3 1. 5 Gy bid (45 Gy/3 wks) Response Median S. V (M) Concurrent Sequentially q 4 w x 4 q 3 w x 4 C/T + TRT R/T follow C/T x IV 97. 4% 27. 2 90. 4% 19. 5 2 yrs S. V 55. 3% (P = 0. 057) 30. 9% 35. 4% 3 yrs S. V 20. 7%
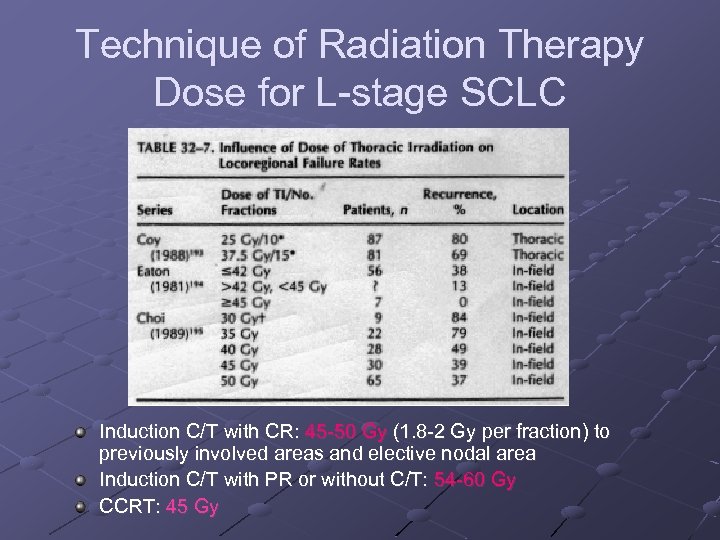 Technique of Radiation Therapy Dose for L stage SCLC Induction C/T with CR: 45 50 Gy (1. 8 2 Gy per fraction) to previously involved areas and elective nodal area Induction C/T with PR or without C/T: 54 60 Gy CCRT: 45 Gy
Technique of Radiation Therapy Dose for L stage SCLC Induction C/T with CR: 45 50 Gy (1. 8 2 Gy per fraction) to previously involved areas and elective nodal area Induction C/T with PR or without C/T: 54 60 Gy CCRT: 45 Gy
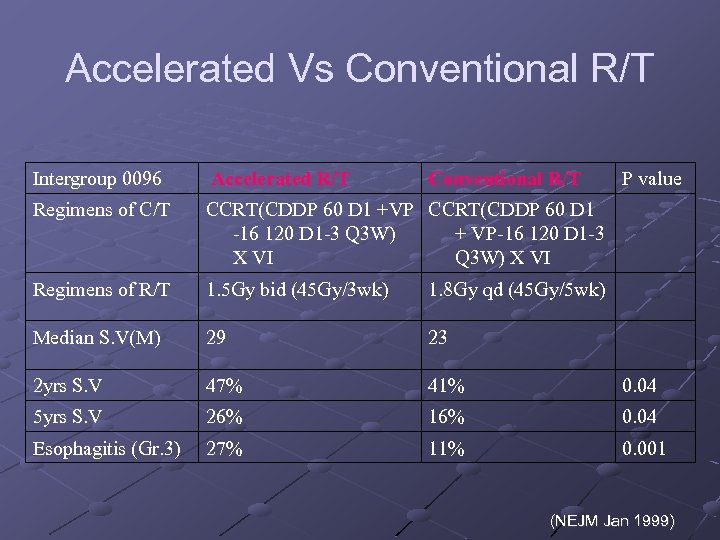 Accelerated Vs Conventional R/T Intergroup 0096 Accelerated R/T Conventional R/T P value Regimens of C/T CCRT(CDDP 60 D 1 +VP CCRT(CDDP 60 D 1 -16 120 D 1 -3 Q 3 W) + VP-16 120 D 1 -3 X VI Q 3 W) X VI Regimens of R/T 1. 5 Gy bid (45 Gy/3 wk) 1. 8 Gy qd (45 Gy/5 wk) Median S. V(M) 29 23 2 yrs S. V 47% 41% 0. 04 5 yrs S. V 26% 16% 0. 04 Esophagitis (Gr. 3) 27% 11% 0. 001 (NEJM Jan 1999)
Accelerated Vs Conventional R/T Intergroup 0096 Accelerated R/T Conventional R/T P value Regimens of C/T CCRT(CDDP 60 D 1 +VP CCRT(CDDP 60 D 1 -16 120 D 1 -3 Q 3 W) + VP-16 120 D 1 -3 X VI Q 3 W) X VI Regimens of R/T 1. 5 Gy bid (45 Gy/3 wk) 1. 8 Gy qd (45 Gy/5 wk) Median S. V(M) 29 23 2 yrs S. V 47% 41% 0. 04 5 yrs S. V 26% 16% 0. 04 Esophagitis (Gr. 3) 27% 11% 0. 001 (NEJM Jan 1999)
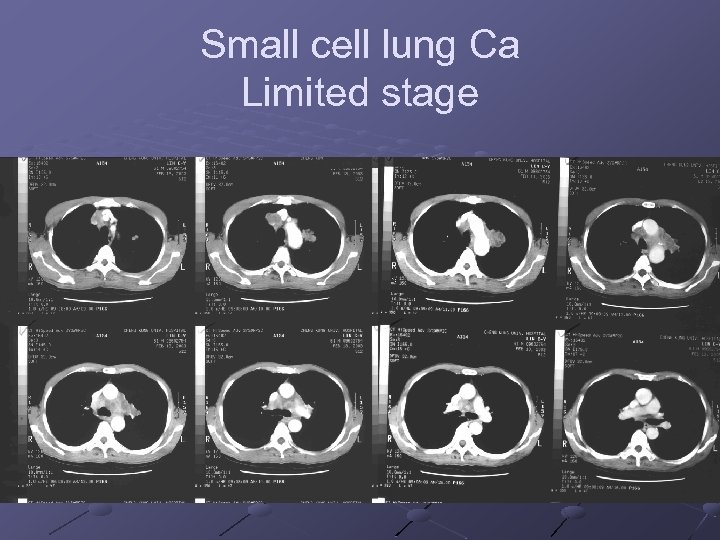 Small cell lung Ca Limited stage
Small cell lung Ca Limited stage
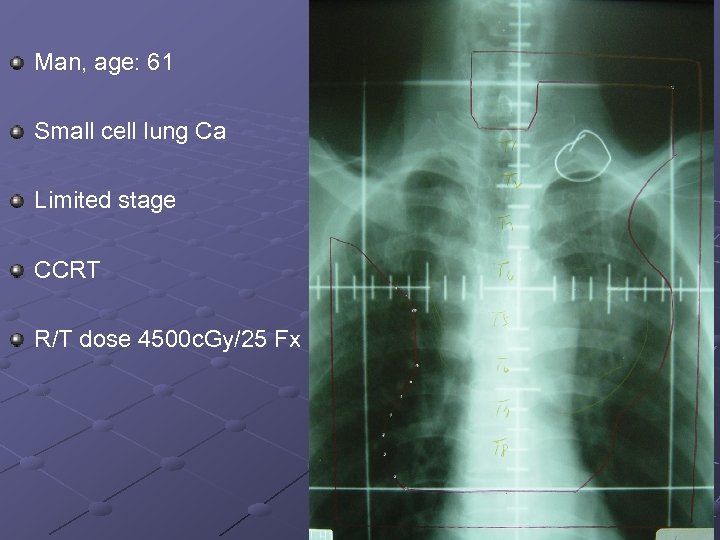 Man, age: 61 Small cell lung Ca Limited stage CCRT R/T dose 4500 c. Gy/25 Fx
Man, age: 61 Small cell lung Ca Limited stage CCRT R/T dose 4500 c. Gy/25 Fx
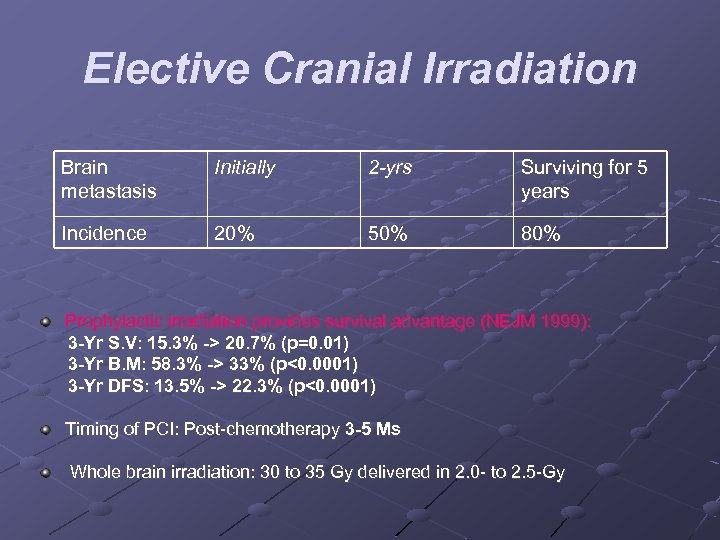 Elective Cranial Irradiation Brain metastasis Initially 2 -yrs Surviving for 5 years Incidence 20% 50% 80% Prophylactic irradiation provides survival advantage (NEJM 1999): 3 -Yr S. V: 15. 3% -> 20. 7% (p=0. 01) 3 -Yr B. M: 58. 3% -> 33% (p<0. 0001) 3 -Yr DFS: 13. 5% -> 22. 3% (p<0. 0001) Timing of PCI: Post chemotherapy 3 -5 Ms Whole brain irradiation: 30 to 35 Gy delivered in 2. 0 to 2. 5 Gy
Elective Cranial Irradiation Brain metastasis Initially 2 -yrs Surviving for 5 years Incidence 20% 50% 80% Prophylactic irradiation provides survival advantage (NEJM 1999): 3 -Yr S. V: 15. 3% -> 20. 7% (p=0. 01) 3 -Yr B. M: 58. 3% -> 33% (p<0. 0001) 3 -Yr DFS: 13. 5% -> 22. 3% (p<0. 0001) Timing of PCI: Post chemotherapy 3 -5 Ms Whole brain irradiation: 30 to 35 Gy delivered in 2. 0 to 2. 5 Gy
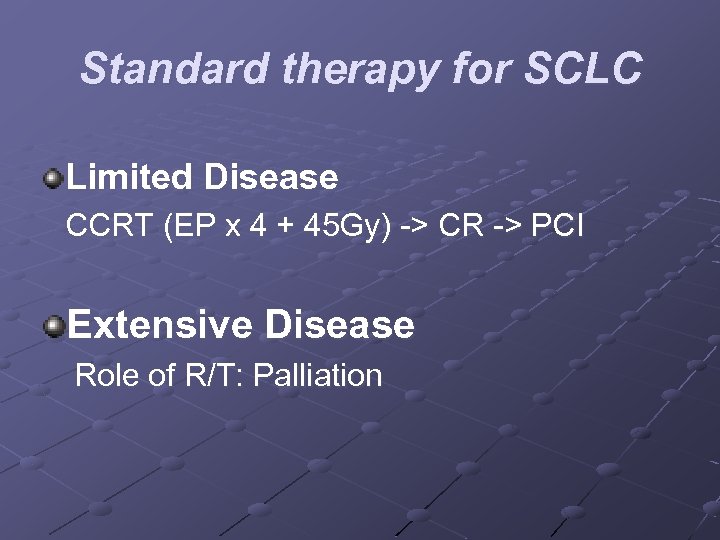 Standard therapy for SCLC Limited Disease CCRT (EP x 4 + 45 Gy) > CR > PCI Extensive Disease Role of R/T: Palliation
Standard therapy for SCLC Limited Disease CCRT (EP x 4 + 45 Gy) > CR > PCI Extensive Disease Role of R/T: Palliation
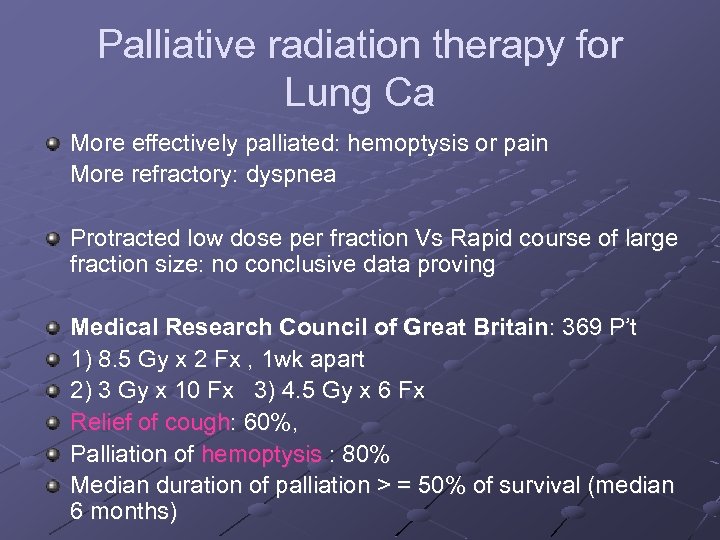 Palliative radiation therapy for Lung Ca More effectively palliated: hemoptysis or pain More refractory: dyspnea Protracted low dose per fraction Vs Rapid course of large fraction size: no conclusive data proving Medical Research Council of Great Britain: 369 P’t 1) 8. 5 Gy x 2 Fx , 1 wk apart 2) 3 Gy x 10 Fx 3) 4. 5 Gy x 6 Fx Relief of cough: 60%, Palliation of hemoptysis : 80% Median duration of palliation > = 50% of survival (median 6 months)
Palliative radiation therapy for Lung Ca More effectively palliated: hemoptysis or pain More refractory: dyspnea Protracted low dose per fraction Vs Rapid course of large fraction size: no conclusive data proving Medical Research Council of Great Britain: 369 P’t 1) 8. 5 Gy x 2 Fx , 1 wk apart 2) 3 Gy x 10 Fx 3) 4. 5 Gy x 6 Fx Relief of cough: 60%, Palliation of hemoptysis : 80% Median duration of palliation > = 50% of survival (median 6 months)
 SUPERIOR VENA CAVA SYNDROME Medical emergency Bronchogenic carcinoma: 80% Malignant lymphoma: 10% to 18% Benign causes (such as goiter): 2% to 3% Radiation therapy should be initiated as soon as possible before / after histological diagnosis Small cell carcinoma: the mode of initial therapy is controversial; both irradiation and chemotherapy are effective
SUPERIOR VENA CAVA SYNDROME Medical emergency Bronchogenic carcinoma: 80% Malignant lymphoma: 10% to 18% Benign causes (such as goiter): 2% to 3% Radiation therapy should be initiated as soon as possible before / after histological diagnosis Small cell carcinoma: the mode of initial therapy is controversial; both irradiation and chemotherapy are effective
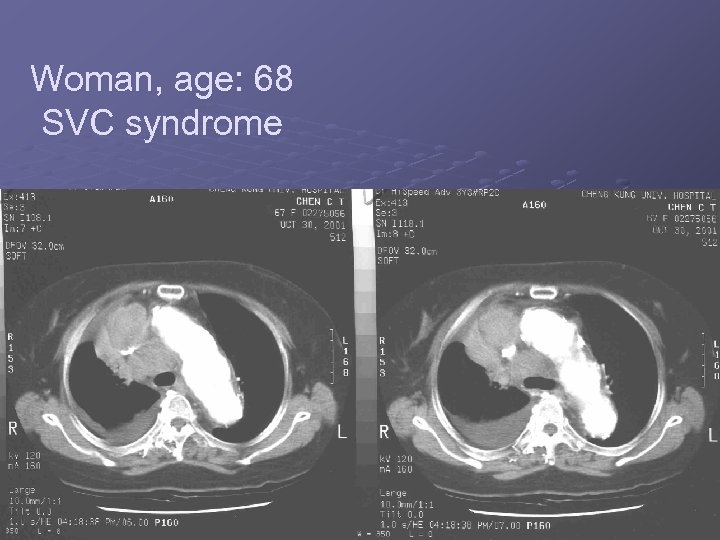 Woman, age: 68 SVC syndrome
Woman, age: 68 SVC syndrome
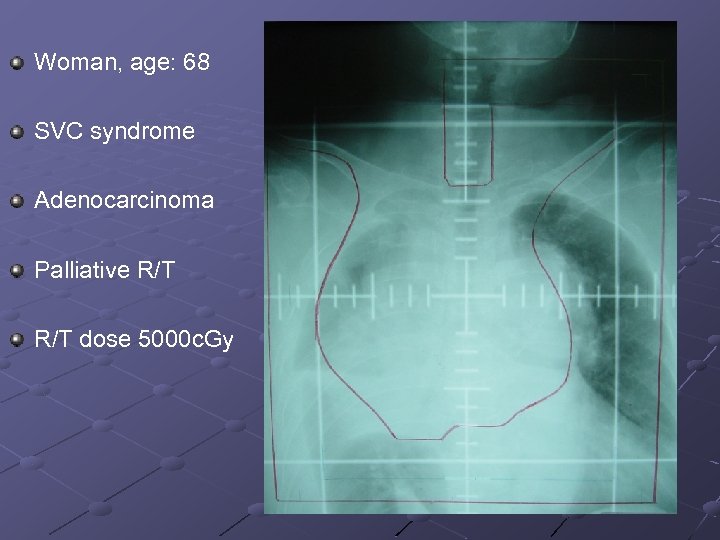 Woman, age: 68 SVC syndrome Adenocarcinoma Palliative R/T dose 5000 c. Gy
Woman, age: 68 SVC syndrome Adenocarcinoma Palliative R/T dose 5000 c. Gy
 SEQUELAE OF THERAPY Acute Sequelae Acute toxicities: esophagitis, cough, skin reaction, and fatigue Acute radiation esophagitis: begins in the 3 rd week of R/T, approximately 30 Gy Nutritional status is compromised: N G tube, temporary gastrostomy, or IV hyperalimentation
SEQUELAE OF THERAPY Acute Sequelae Acute toxicities: esophagitis, cough, skin reaction, and fatigue Acute radiation esophagitis: begins in the 3 rd week of R/T, approximately 30 Gy Nutritional status is compromised: N G tube, temporary gastrostomy, or IV hyperalimentation
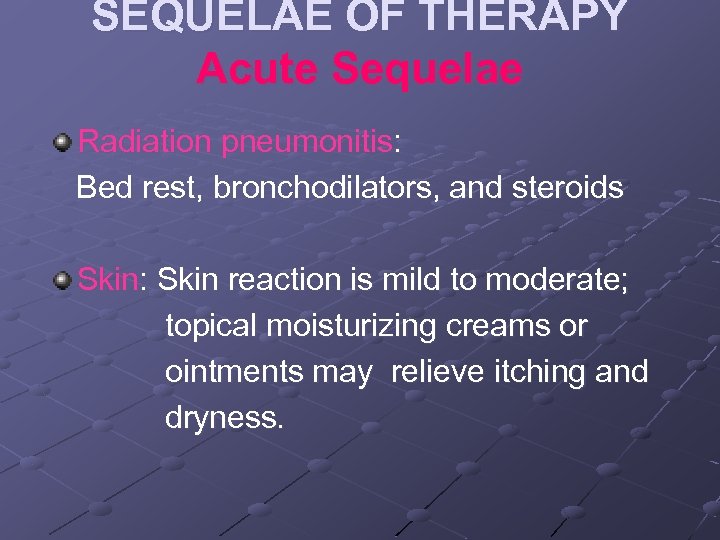 SEQUELAE OF THERAPY Acute Sequelae Radiation pneumonitis: Bed rest, bronchodilators, and steroids Skin: Skin reaction is mild to moderate; topical moisturizing creams or ointments may relieve itching and dryness.
SEQUELAE OF THERAPY Acute Sequelae Radiation pneumonitis: Bed rest, bronchodilators, and steroids Skin: Skin reaction is mild to moderate; topical moisturizing creams or ointments may relieve itching and dryness.
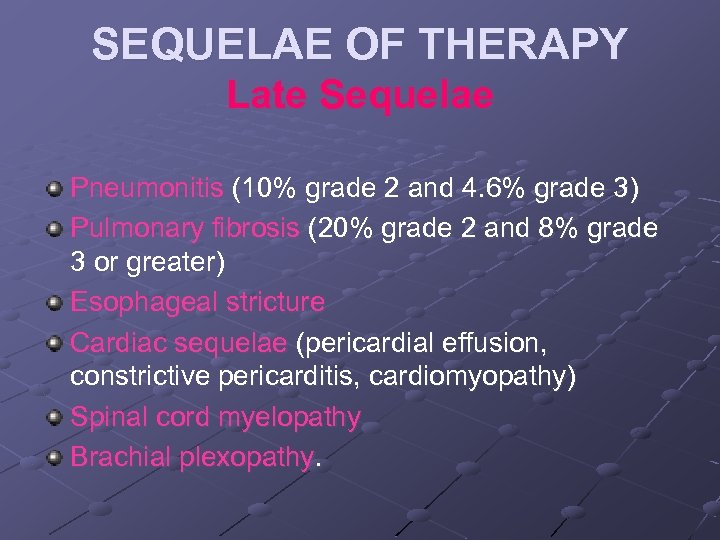 SEQUELAE OF THERAPY Late Sequelae Pneumonitis (10% grade 2 and 4. 6% grade 3) Pulmonary fibrosis (20% grade 2 and 8% grade 3 or greater) Esophageal stricture Cardiac sequelae (pericardial effusion, constrictive pericarditis, cardiomyopathy) Spinal cord myelopathy Brachial plexopathy.
SEQUELAE OF THERAPY Late Sequelae Pneumonitis (10% grade 2 and 4. 6% grade 3) Pulmonary fibrosis (20% grade 2 and 8% grade 3 or greater) Esophageal stricture Cardiac sequelae (pericardial effusion, constrictive pericarditis, cardiomyopathy) Spinal cord myelopathy Brachial plexopathy.
 Thanks for your attention !
Thanks for your attention !
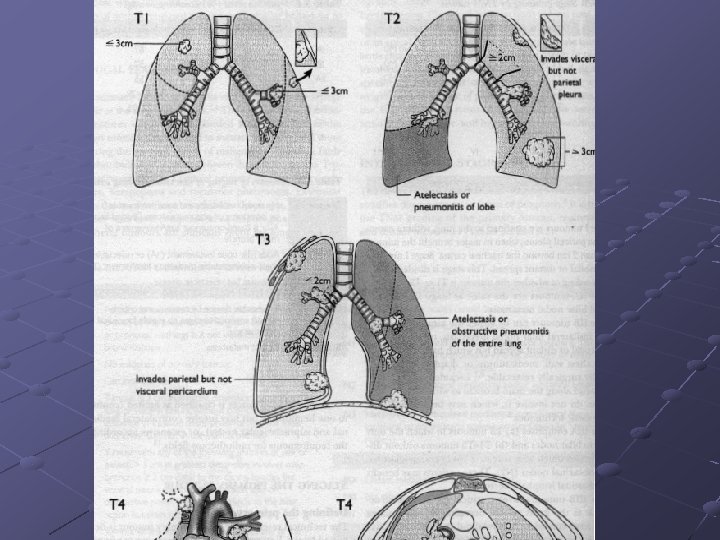
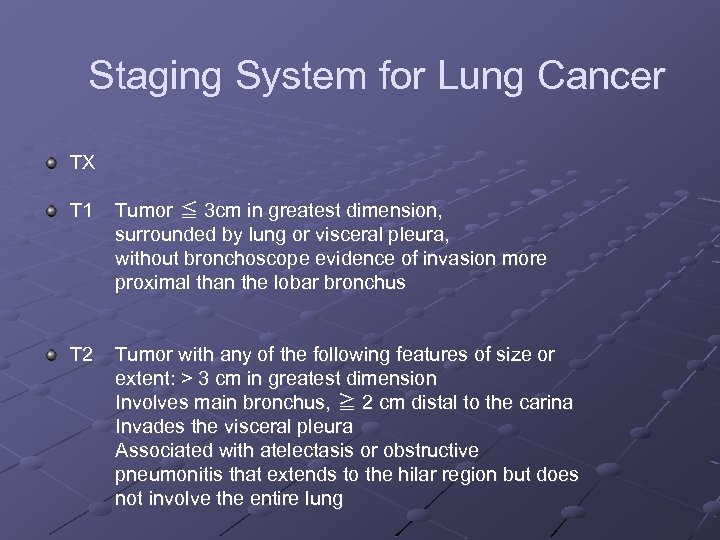 Staging System for Lung Cancer TX T 1 Tumor ≦ 3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscope evidence of invasion more proximal than the lobar bronchus T 2 Tumor with any of the following features of size or extent: > 3 cm in greatest dimension Involves main bronchus, ≧ 2 cm distal to the carina Invades the visceral pleura Associated with atelectasis or obstructive pneumonitis that extends to the hilar region but does not involve the entire lung
Staging System for Lung Cancer TX T 1 Tumor ≦ 3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscope evidence of invasion more proximal than the lobar bronchus T 2 Tumor with any of the following features of size or extent: > 3 cm in greatest dimension Involves main bronchus, ≧ 2 cm distal to the carina Invades the visceral pleura Associated with atelectasis or obstructive pneumonitis that extends to the hilar region but does not involve the entire lung
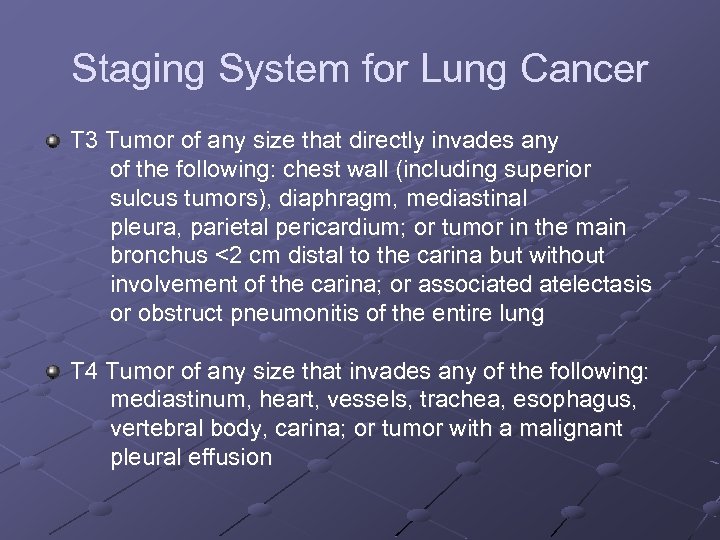 Staging System for Lung Cancer T 3 Tumor of any size that directly invades any of the following: chest wall (including superior sulcus tumors), diaphragm, mediastinal pleura, parietal pericardium; or tumor in the main bronchus <2 cm distal to the carina but without involvement of the carina; or associated atelectasis or obstruct pneumonitis of the entire lung T 4 Tumor of any size that invades any of the following: mediastinum, heart, vessels, trachea, esophagus, vertebral body, carina; or tumor with a malignant pleural effusion
Staging System for Lung Cancer T 3 Tumor of any size that directly invades any of the following: chest wall (including superior sulcus tumors), diaphragm, mediastinal pleura, parietal pericardium; or tumor in the main bronchus <2 cm distal to the carina but without involvement of the carina; or associated atelectasis or obstruct pneumonitis of the entire lung T 4 Tumor of any size that invades any of the following: mediastinum, heart, vessels, trachea, esophagus, vertebral body, carina; or tumor with a malignant pleural effusion
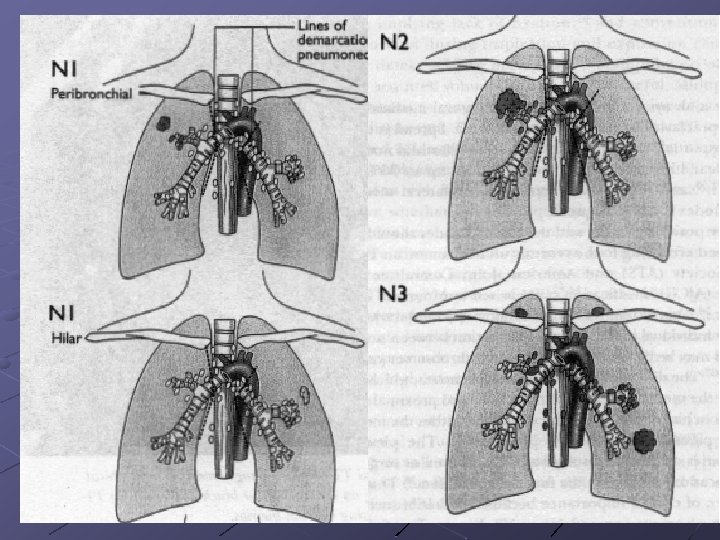
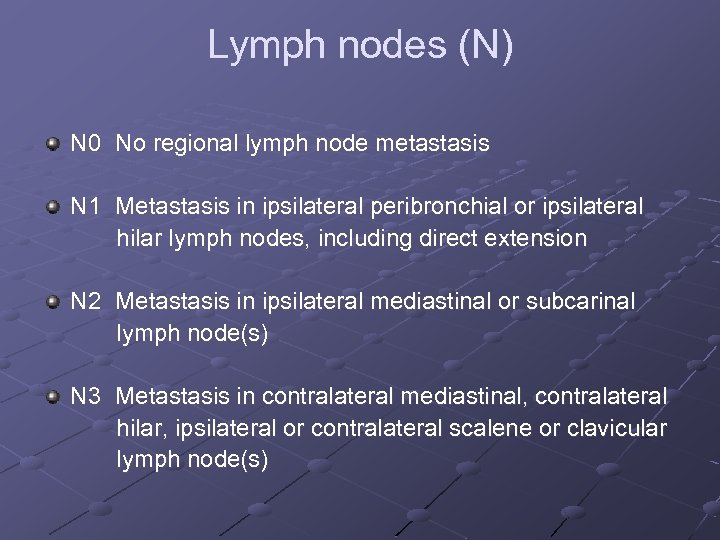 Lymph nodes (N) N 0 No regional lymph node metastasis N 1 Metastasis in ipsilateral peribronchial or ipsilateral hilar lymph nodes, including direct extension N 2 Metastasis in ipsilateral mediastinal or subcarinal lymph node(s) N 3 Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene or clavicular lymph node(s)
Lymph nodes (N) N 0 No regional lymph node metastasis N 1 Metastasis in ipsilateral peribronchial or ipsilateral hilar lymph nodes, including direct extension N 2 Metastasis in ipsilateral mediastinal or subcarinal lymph node(s) N 3 Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene or clavicular lymph node(s)
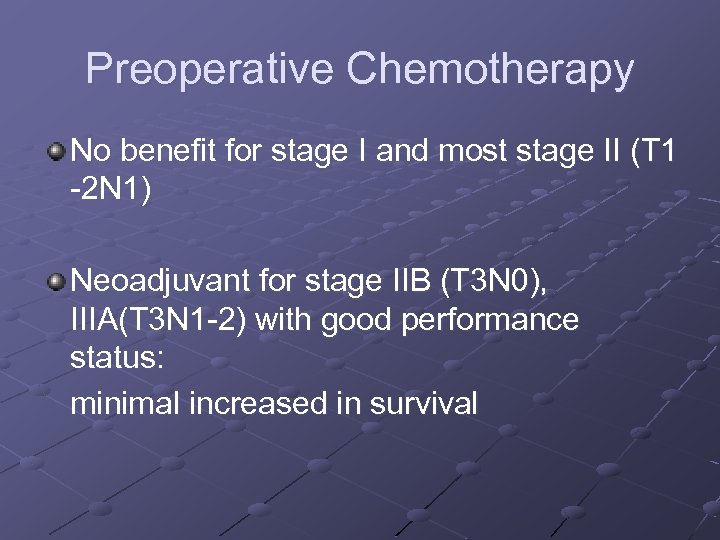 Preoperative Chemotherapy No benefit for stage I and most stage II (T 1 2 N 1) Neoadjuvant for stage IIB (T 3 N 0), IIIA(T 3 N 1 2) with good performance status: minimal increased in survival
Preoperative Chemotherapy No benefit for stage I and most stage II (T 1 2 N 1) Neoadjuvant for stage IIB (T 3 N 0), IIIA(T 3 N 1 2) with good performance status: minimal increased in survival
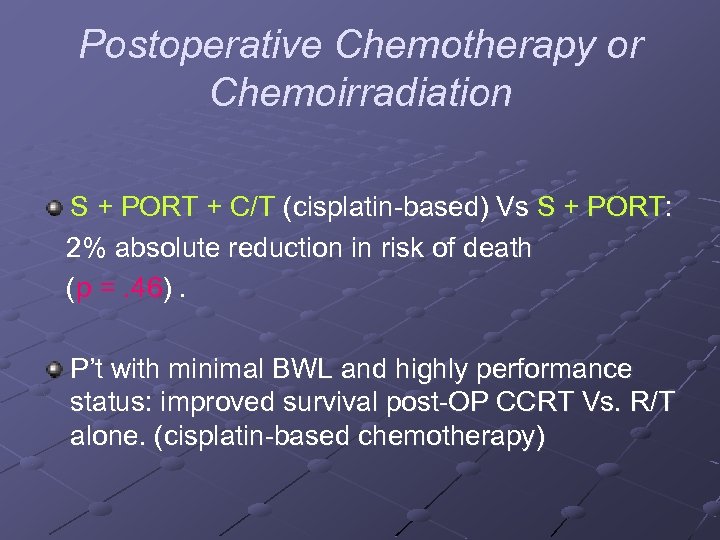 Postoperative Chemotherapy or Chemoirradiation S + PORT + C/T (cisplatin based) Vs S + PORT: 2% absolute reduction in risk of death (p =. 46). P’t with minimal BWL and highly performance status: improved survival post OP CCRT Vs. R/T alone. (cisplatin based chemotherapy)
Postoperative Chemotherapy or Chemoirradiation S + PORT + C/T (cisplatin based) Vs S + PORT: 2% absolute reduction in risk of death (p =. 46). P’t with minimal BWL and highly performance status: improved survival post OP CCRT Vs. R/T alone. (cisplatin based chemotherapy)
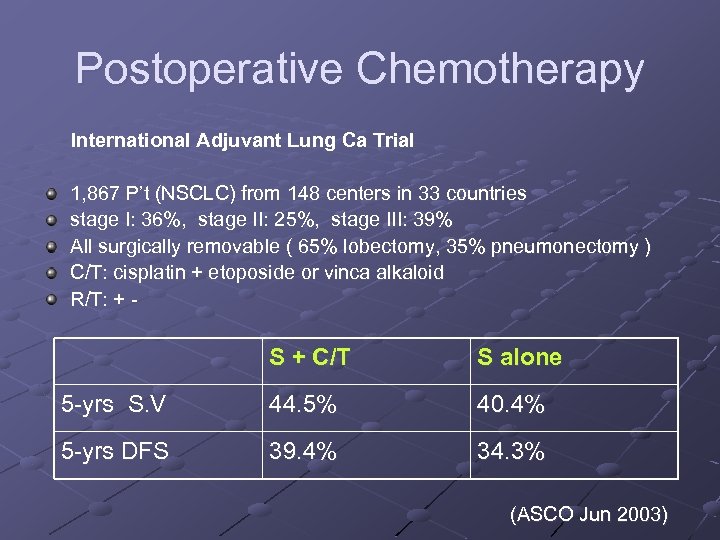 Postoperative Chemotherapy International Adjuvant Lung Ca Trial 1, 867 P’t (NSCLC) from 148 centers in 33 countries stage I: 36%, stage II: 25%, stage III: 39% All surgically removable ( 65% lobectomy, 35% pneumonectomy ) C/T: cisplatin + etoposide or vinca alkaloid R/T: + S + C/T S alone 5 yrs S. V 44. 5% 40. 4% 5 yrs DFS 39. 4% 34. 3% (ASCO Jun 2003)
Postoperative Chemotherapy International Adjuvant Lung Ca Trial 1, 867 P’t (NSCLC) from 148 centers in 33 countries stage I: 36%, stage II: 25%, stage III: 39% All surgically removable ( 65% lobectomy, 35% pneumonectomy ) C/T: cisplatin + etoposide or vinca alkaloid R/T: + S + C/T S alone 5 yrs S. V 44. 5% 40. 4% 5 yrs DFS 39. 4% 34. 3% (ASCO Jun 2003)
 Sequence of Irradiation and Chemotherapy Most randomized trials show no benefit of thoracic irradiation when administered after chemotherapy CCRT > Sequential chemoradiation therapy R/T initiation: within 6 wks or follow 2 cycles C/T R/T is given early in the course of or concurrently with chemotherapy.
Sequence of Irradiation and Chemotherapy Most randomized trials show no benefit of thoracic irradiation when administered after chemotherapy CCRT > Sequential chemoradiation therapy R/T initiation: within 6 wks or follow 2 cycles C/T R/T is given early in the course of or concurrently with chemotherapy.
 SEQUELAE OF THERAPY Late Sequelae Long term esophageal problems: stenosis, ulceration, perforation, and fistula in 5% to 15% of patients. Radiation induced cardiac disease after irradiation for lung cancer is relatively rare; pericarditis is most common. Spinal cord myelopathy may occur with doses higher than 45 Gy in 1. 8 to 2. 0 Gy frac tions; factors important in its causation are total irradiation dose, length of the irradiated cord, and fractionation schedule.
SEQUELAE OF THERAPY Late Sequelae Long term esophageal problems: stenosis, ulceration, perforation, and fistula in 5% to 15% of patients. Radiation induced cardiac disease after irradiation for lung cancer is relatively rare; pericarditis is most common. Spinal cord myelopathy may occur with doses higher than 45 Gy in 1. 8 to 2. 0 Gy frac tions; factors important in its causation are total irradiation dose, length of the irradiated cord, and fractionation schedule.


