bf7368937e8626c384539787cb252fa8.ppt
- Количество слайдов: 62
Radiation Protection Robert L. Metzger, Ph. D.
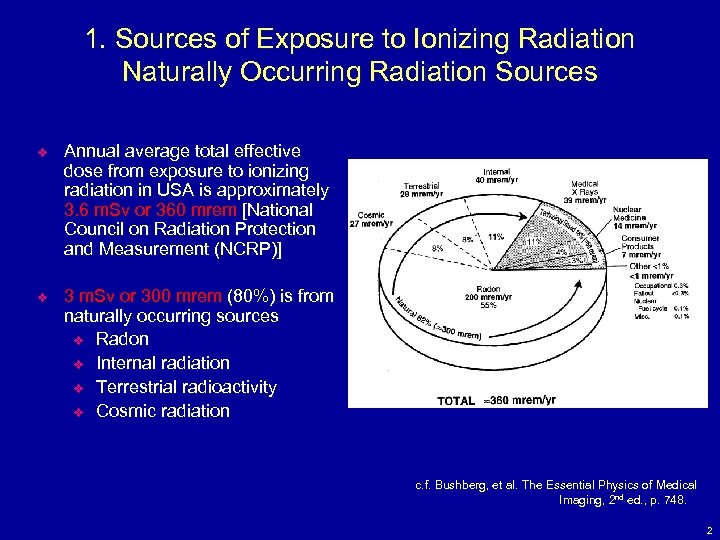
1. Sources of Exposure to Ionizing Radiation Naturally Occurring Radiation Sources v Annual average total effective dose from exposure to ionizing radiation in USA is approximately 3. 6 m. Sv or 360 mrem [National Council on Radiation Protection and Measurement (NCRP)] v 3 m. Sv or 300 mrem (80%) is from naturally occurring sources v Radon v Internal radiation v Terrestrial radioactivity v Cosmic radiation c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 748. 2
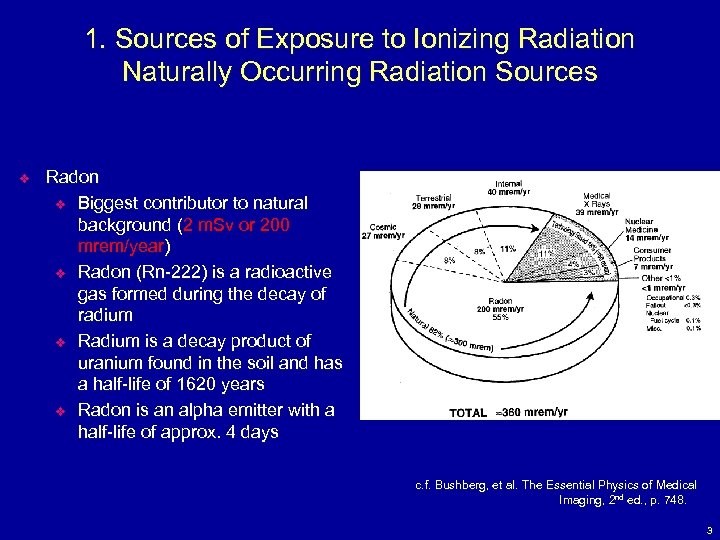
1. Sources of Exposure to Ionizing Radiation Naturally Occurring Radiation Sources v Radon v Biggest contributor to natural background (2 m. Sv or 200 mrem/year) v Radon (Rn-222) is a radioactive gas formed during the decay of radium v Radium is a decay product of uranium found in the soil and has a half-life of 1620 years v Radon is an alpha emitter with a half-life of approx. 4 days c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 748. 3
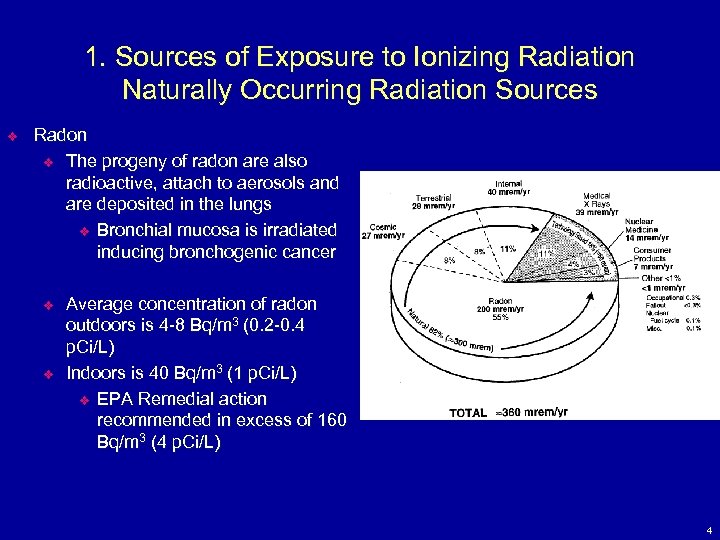
1. Sources of Exposure to Ionizing Radiation Naturally Occurring Radiation Sources v Radon v The progeny of radon are also radioactive, attach to aerosols and are deposited in the lungs v Bronchial mucosa is irradiated inducing bronchogenic cancer v v Average concentration of radon outdoors is 4 -8 Bq/m 3 (0. 2 -0. 4 p. Ci/L) Indoors is 40 Bq/m 3 (1 p. Ci/L) v EPA Remedial action recommended in excess of 160 Bq/m 3 (4 p. Ci/L) 4
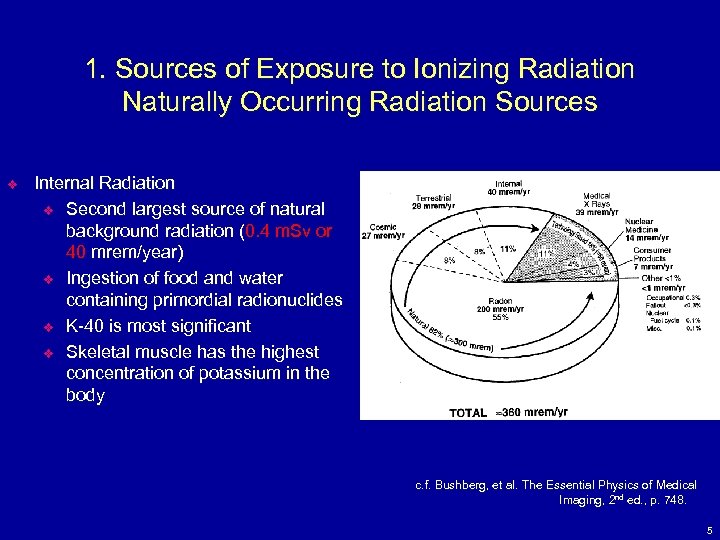
1. Sources of Exposure to Ionizing Radiation Naturally Occurring Radiation Sources v Internal Radiation v Second largest source of natural background radiation (0. 4 m. Sv or 40 mrem/year) v Ingestion of food and water containing primordial radionuclides v K-40 is most significant v Skeletal muscle has the highest concentration of potassium in the body c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 748. 5
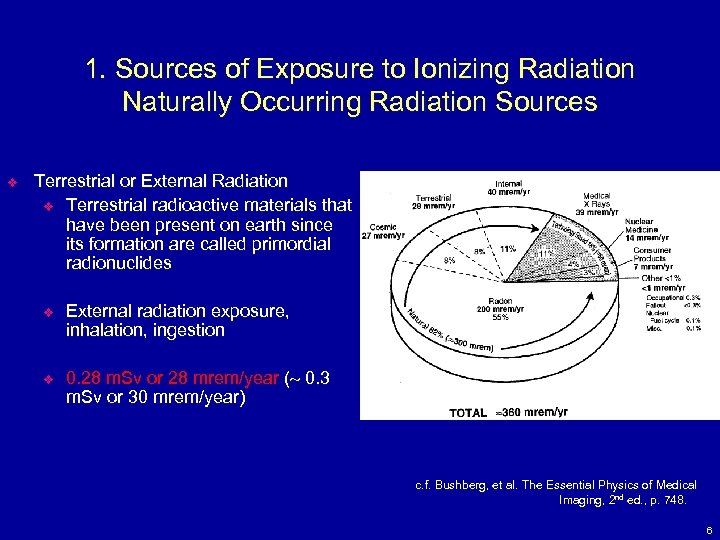
1. Sources of Exposure to Ionizing Radiation Naturally Occurring Radiation Sources v Terrestrial or External Radiation v Terrestrial radioactive materials that have been present on earth since its formation are called primordial radionuclides v v External radiation exposure, inhalation, ingestion 0. 28 m. Sv or 28 mrem/year ( 0. 3 m. Sv or 30 mrem/year) c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 748. 6
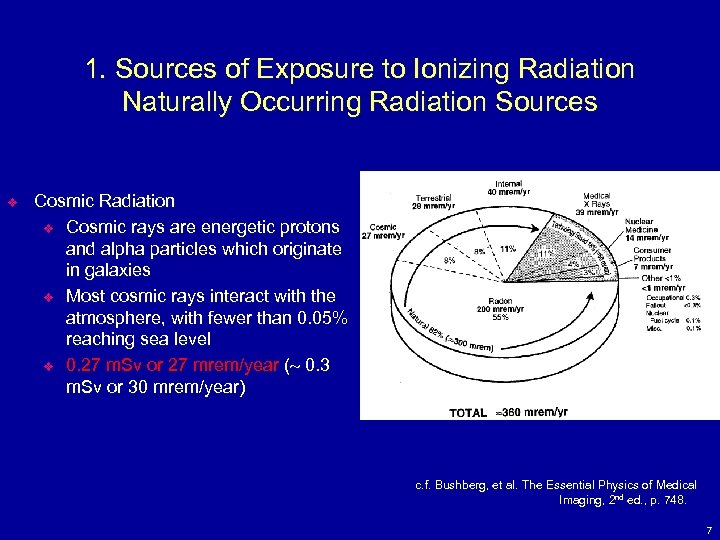
1. Sources of Exposure to Ionizing Radiation Naturally Occurring Radiation Sources v Cosmic Radiation v Cosmic rays are energetic protons and alpha particles which originate in galaxies v Most cosmic rays interact with the atmosphere, with fewer than 0. 05% reaching sea level v 0. 27 m. Sv or 27 mrem/year ( 0. 3 m. Sv or 30 mrem/year) c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 748. 7
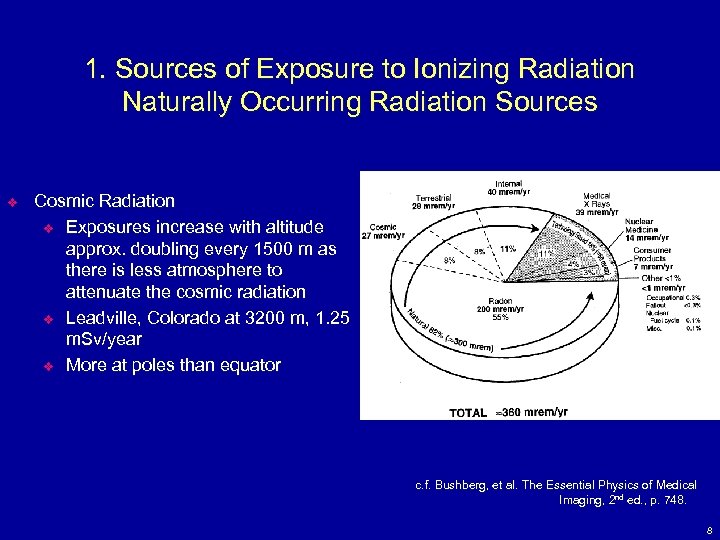
1. Sources of Exposure to Ionizing Radiation Naturally Occurring Radiation Sources v Cosmic Radiation v Exposures increase with altitude approx. doubling every 1500 m as there is less atmosphere to attenuate the cosmic radiation v Leadville, Colorado at 3200 m, 1. 25 m. Sv/year v More at poles than equator c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 748. 8
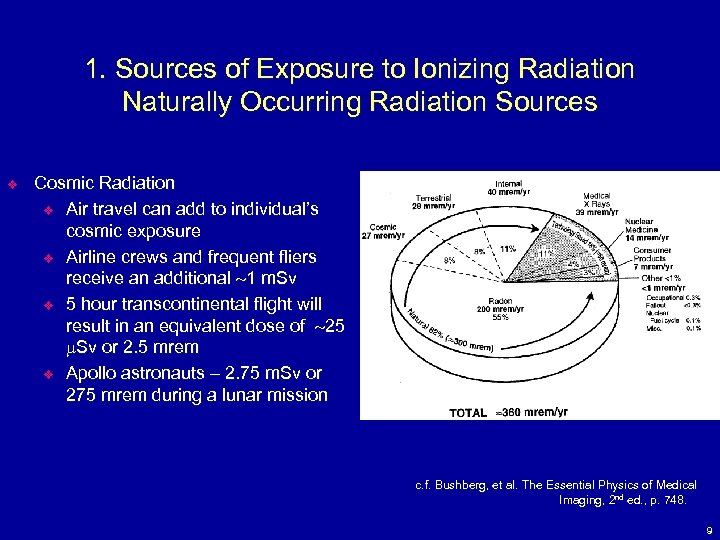
1. Sources of Exposure to Ionizing Radiation Naturally Occurring Radiation Sources v Cosmic Radiation v Air travel can add to individual’s cosmic exposure v Airline crews and frequent fliers receive an additional 1 m. Sv v 5 hour transcontinental flight will result in an equivalent dose of 25 m. Sv or 2. 5 mrem v Apollo astronauts – 2. 75 m. Sv or 275 mrem during a lunar mission c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 748. 9
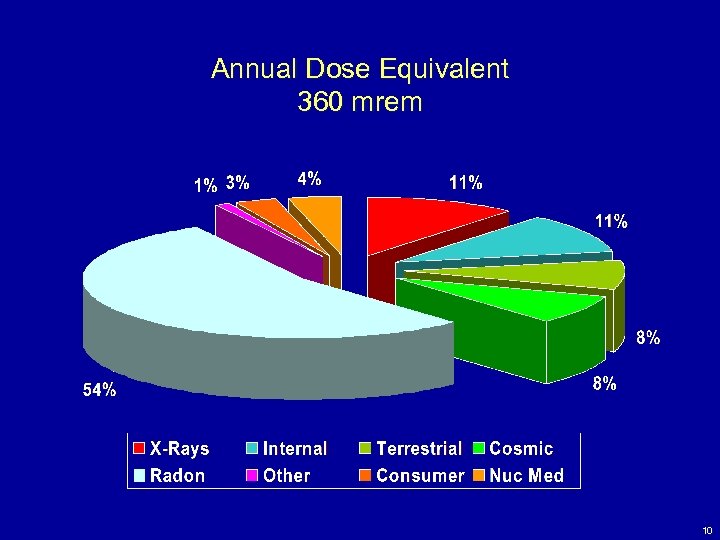
Annual Dose Equivalent 360 mrem 10
Annual Dose - Other 1% v v v Occupational Dose – 0. 3% Fallout - <0. 3% Nuclear Fuel Cycle – 0. 1% Miscellaneous – 0. 1% Natural Sources Account for 82% of total annual dose with only 18% coming from man made sources. 11
Natural Sources of Radiation v v v The variation of dose from the cosmic and terrestrial radiation is large depending on the area of the country (see handout). High altitude areas have higher cosmic radiation levels (e. g. Denver, Flagstaff) Areas that are heavily mineralized have higher terrestrial radiation levels. Radon levels also vary significantly, but vary from home to home rather than whole geographic areas (e. g. Watras house) The overall variation in cosmic and terrestrial radiations exceed 100 mrem per year and affect everyone in a city/area (e. g. Denver) Cancer incidence does not follow the background radiation levels at all. 12
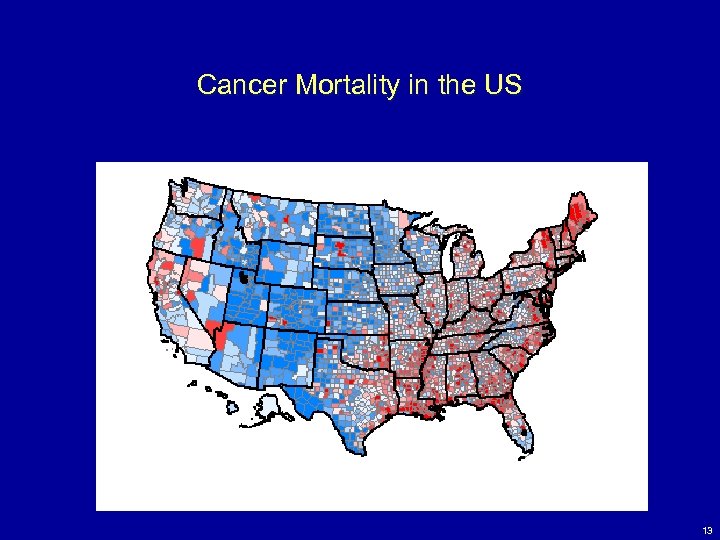
Cancer Mortality in the US 13
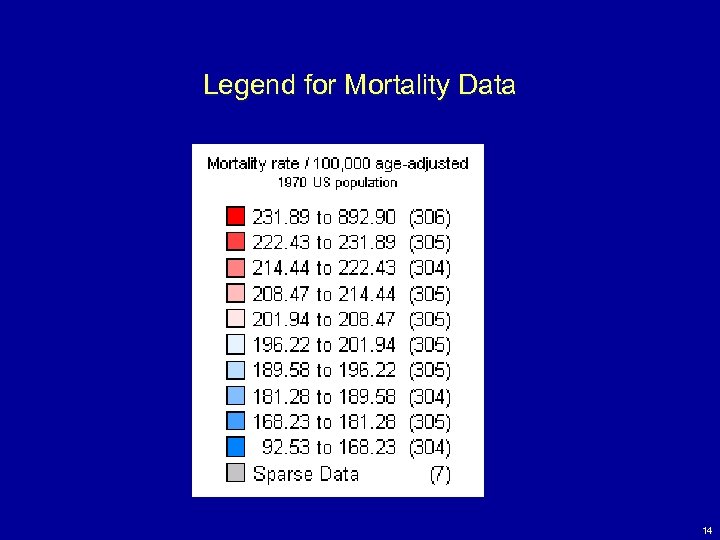
Legend for Mortality Data 14
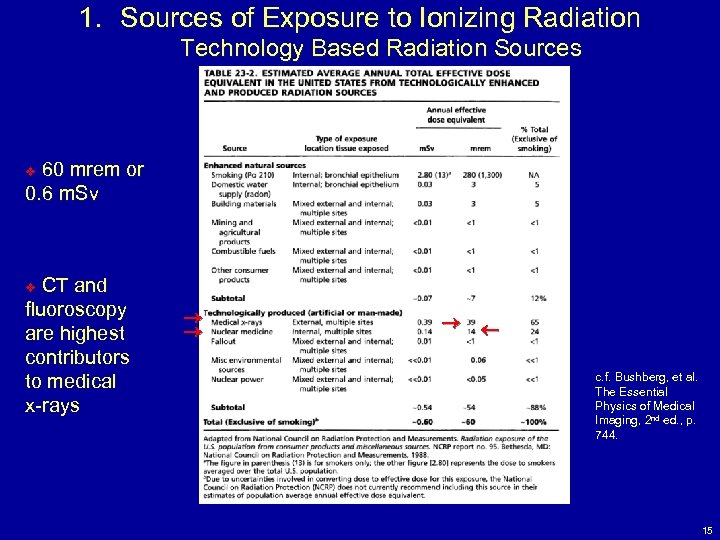
1. Sources of Exposure to Ionizing Radiation Technology Based Radiation Sources 60 mrem or 0. 6 m. Sv v CT and fluoroscopy are highest contributors to medical x-rays v c. f. Bushberg, et al. Bushberg, The Essential Physics of Medical Imaging, 2 nd ed. , p. 744. 15
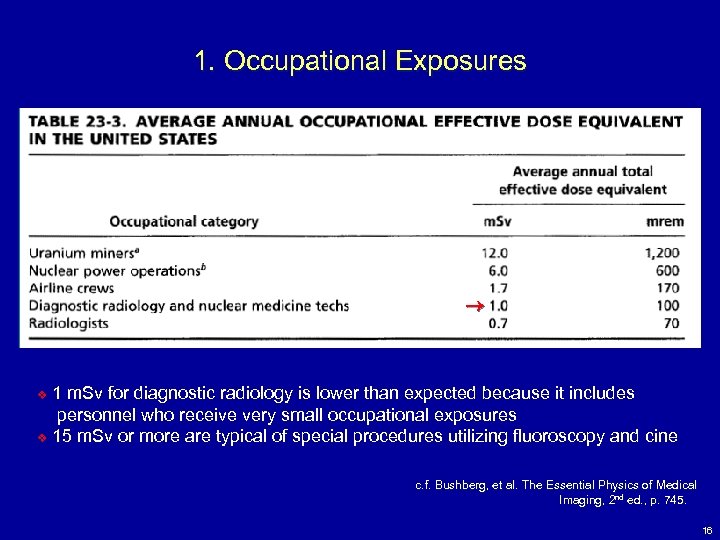
1. Occupational Exposures 1 m. Sv for diagnostic radiology is lower than expected because it includes personnel who receive very small occupational exposures v 15 m. Sv or more are typical of special procedures utilizing fluoroscopy and cine v c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 745. 16
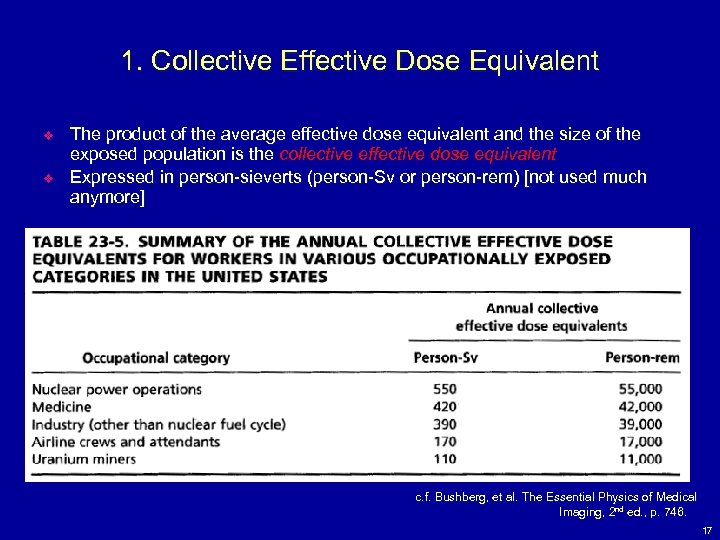
1. Collective Effective Dose Equivalent v v The product of the average effective dose equivalent and the size of the exposed population is the collective effective dose equivalent Expressed in person-sieverts (person-Sv or person-rem) [not used much anymore] c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 746. 17
1. Genetically Significant Dose (GSD) v The genetically significant equivalent dose (GSD) is a dose parameter that is an index of potential genetic damage v The GSD is defined as that equivalent dose that, if received by every member of the population, would be expected to produce the same genetic injury to the population as do the actual doses received by the irradiated individuals v GSD is determined by taking the equivalent dose to the gonads of each exposed individual and estimating the number of children expected for a person of that age and sex 18
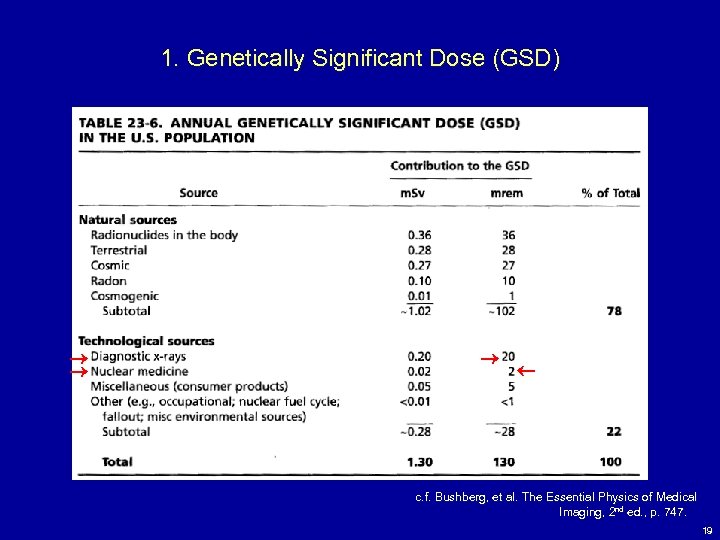
1. Genetically Significant Dose (GSD) c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 747. 19
1. Summary v The average annual effective dose equivalent to the US population from all radiation sources is 3. 6 m. Sv/year or 360 mrem/year v 3 m. Sv/year – naturally occurring sources v Radon – 2 m. Sv v 0. 6 m. Sv/year – technologically enhanced sources v Medical x-rays – 0. 39 m. Sv or 39 mrem, v Nuclear Medicine – 0. 14 m. Sv or 14 mrem v Data is from mid – 80 s. Current estimates are higher due to the increased use of CT. Recent estimates are 385 mrem with 85 mrem due to medical. 20
1. Summary v Collective effective dose equivalent (person-Sv or person-rem) v Product of the average effective dose equivalent and the size of the exposed population (No longer used commonly) v GSD (m. Sv or mrem) v Used to express genetic risk to the whole population from a source of radiation exposure v GSD from diagnostic x-rays is 0. 2 m. Sv or 20 mrem v GSD from nuclear medicine is 0. 02 m. Sv or 2 mrem 21
Raphex 2002 General Question v G 87. The annual average natural background radiation dose to members of the public in the United States, excluding radon, is approximately ____ mrem. v A. 10 B. 50 C. 100 D. 200 E. 400 v v 22
Question v 1. The Genetically significant dose (GSD) for diagnostic x-rays and nuclear medicine in the US is: v A. 2 m. Sv and 0. 20 m. Sv B. 0. 20 m. Sv and 2 m. Sv C. 0. 02 m. Sv and 0. 20 m. Sv D. 0. 20 m. Sv and 0. 02 m. Sv v 23
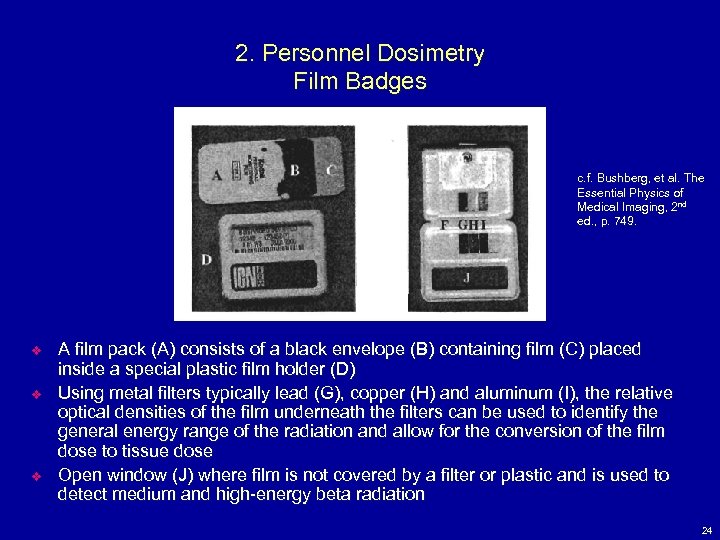
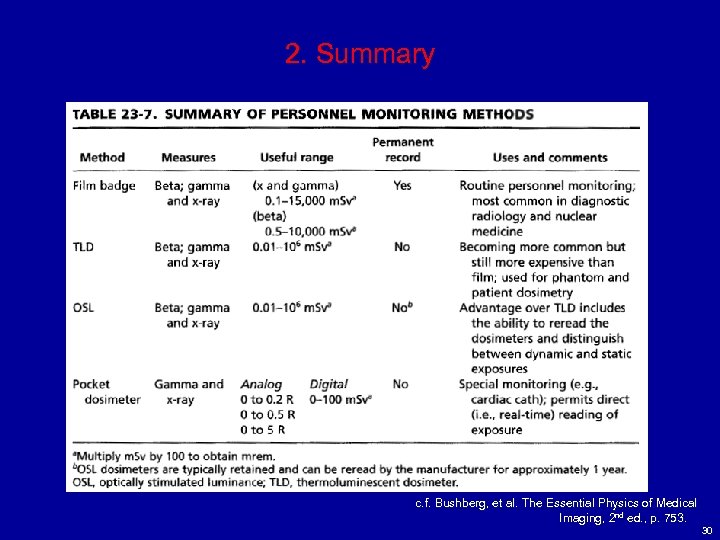
2. Personnel Dosimetry Film Badges c. f. Bushberg, et al. The Bushberg, Essential Physics of Medical Imaging, 2 nd ed. , p. 749. v v v A film pack (A) consists of a black envelope (B) containing film (C) placed inside a special plastic film holder (D) Using metal filters typically lead (G), copper (H) and aluminum (I), the relative optical densities of the film underneath the filters can be used to identify the general energy range of the radiation and allow for the conversion of the film dose to tissue dose Open window (J) where film is not covered by a filter or plastic and is used to detect medium and high-energy beta radiation 24
2. Personnel Dosimetry Film Badges v v v Most film badges can record doses from about 100 m. Gy to 15 Gy (10 mrad to 1500 rad) for photons and from 500 m. Gy to 10 Gy (50 mrad to 1, 000 rad) for beta radiation The dosimetry report lists the “shallow” equivalent dose, corresponding to the skin dose, and the “deep” equivalent dose, corresponding to penetrating radiation Generally placed at waist level or shirt-pocket level For fluoroscopy, placed at collar level outside the lead apron to measure radiation dose to thyroid and lens of eye Pregnant radiation workers typically wear a second badge at waist level (behind the lead apron, if used) to assess the fetal dose Excessive moisture or heat will damage film inside badge 25
2. Personnel Dosimetry Thermoluminescent (TLD) Dosimeters v TLD is a dosimeter in which consists of a scintillator in which electrons become trapped in excited states after interactions with ionizing radiation v If the scintillator is later heated, the electrons can then fall to their ground state with the emission of light Thermoluminescent (TL) means emitting light when heated v v The amount of light emitted by the TLD is proportional to the amount of energy absorbed by the TLD v After TLD has been read, it may be baked in an oven and reused 26
2. Personnel Dosimetry Thermoluminescent (TLD) Dosimeters v v v Lithium Fluoride (Li. F) is one of the most useful TLD materials Li. F TLDs have a wide dose response range of 10 m. Sv to 103 m. Sv (1 mrem to 105 rem) Used in nuclear medicine to record extremity exposures 27
2. Personnel Dosimetry Optically Stimulated Luminescent (OSL) Dosimeters v v The principle of OSL is similar to TLDs except that the light emission is stimulated by a laser light instead of heat Crystalline aluminum oxide activated with carbon (Al 2 O 3: C) is commonly used Broad dose response range like TLDs They can be reread several times 28
2. Personnel Dosimetry Pocket Dosimeters v v Major disadvantage to film and TLD dosimeters is that the accumulated exposure is not immediately indicated Pocket dosimeters measure radiation exposure, which can be read instantaneously Can measure exposures from 0 to 200 m. R or 0 to 5 R Analog or digital c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 752. 29
2. Summary c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 753. 30
Raphex 2002 General Questions v G 95. Film badges: v A. Can measure only the total dose of radiation, but cannot distinguish between low and high energy x-rays. B. Can measure exposures of 1 m. R. C. Are insensitive to heat. D. Use the optical density of the film to measure dose. v v v 31
3. Radiation Detection Equipment In Radiation Safety v Geiger-Mueller Survey Instruments v Measurements are in counts per minute (cpm) v Surveys radioactive contamination in nuclear medicine v Are extremely sensitive to charged particulate radiations with sufficient energy to penetrate the survey meter window v Are relatively insensitive to x- and gamma radiations v Portable Ionization Chambers v Used when accurate measurements of radiation exposure are required, measurement of x-ray machine outputs v Measure 1 m. R/hr to 500 R/hr 32
4. Radiation Protection and Exposure Control v There are four principal methods by which radiation exposures to persons can be minimized: time, distance, shielding and contamination control v Time v reducing time spend near a radiation source v Distance v inverse square law v For diagnostic x-rays, a good rule of thumb is that at 1 m from a patient at 90 degrees to the incident beam, the radiation intensity is 0. 1% to 0. 15% (0. 001 to 0. 0015) of the intensity of the beam incident upon the patient for a 400 cm 2 area field area v The NCRP recommends that personnel should stand at least 2 m from the x-ray tube and the patient and behind a shielded barrier or out of the room, whenever possible 33
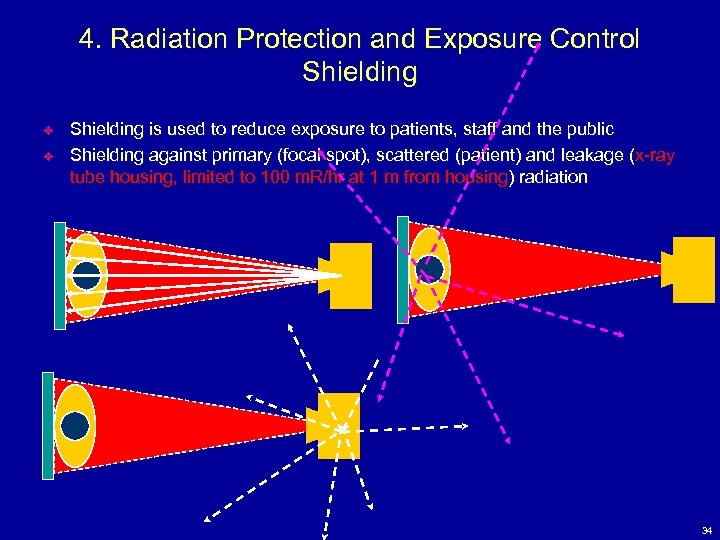
4. Radiation Protection and Exposure Control Shielding v v Shielding is used to reduce exposure to patients, staff and the public Shielding against primary (focal spot), scattered (patient) and leakage (x-ray tube housing, limited to 100 m. R/hr at 1 m from housing) radiation 34
Shielding – NCRP 49 vs. 147 v v v The Bushberg X-Ray shielding section is based on NCRP 49 which is obsolete and out of print. Bushberg notes that it is badly out of date. NCRP 147 replaced NCRP 49 in 2005. It should be used for all shielding calculations. NCRP 147 uses a different methodology to calculate the shielding values and uses much more realistic values for occupancy, tube k. Vps, weekly m. As, and film/screen speeds. It eliminates the gross overshielding resulting from the use of NCRP 49 with the lowered non-occupational dose limits. NCRP 147 also provides shielding methodologies for CT and othr modalities. 35
4. Radiation Protection and Exposure Control Shielding v Shielding calculations depend on: v radiation exposure level (m. R/week) depends on techniques and patient load v workload (amount of x-rays produced per week), W (m. A. min/week) v use factor, U, indicates the fraction of time during which the radiation under consideration is directed at a particular barrier v a wall that intercepts the primary beam is called a primary barrier and is assigned a use factor according to typical room use v U ranges between 0 and 1, secondary barriers have a use factor of 1 36
4. Radiation Protection and Exposure Control Shielding v Shielding calculations depend on: v occupancy factor, T, indicates the fraction of time during a week that a single individual might spend in an adjacent area v T = 1 for full occupancy (work areas, offices etc. ) v T = 1/5 for partial occupancy (corridors, rest rooms etc. ) v T = 1/16 for occasional occupancy (waiting rooms, toilets, etc. ) v T = 1/40 th for landscaping, etc. v Distance, d, measured from source of radiation to the area to be protected 37
4. Radiation Protection and Exposure Control Shielding v Shielding calculations determine thickness of an attenuating material required to reduce radiation exposure to acceptable levels v 1 m. Sv/year or 100 mrem/year (2 m. R/week) for non-occupational personnel (members of public and non-radiation workers) v 0. 1 or 10 m. R/week for controlled areas (pregnant worker limit) 38
4. Radiation Protection and Exposure Control Shielding v v Lead usually used for shielding and specified as weight per square foot (lb/ft 2). Typically 2 lb/ft 2 (0. 8 mm or 1/32 th inch) or 4 lb/ft 2 (1. 6 mm or 1/16 th inch) is sufficient for diagnostic radiology Calculated using HVL and TVL of the material [(1/2)n – reduction in beam intensity, n is HVL] Shielding material used from base of floor to a height of 7 feet Acrylic, leaded glass, gypsum drywall, steel are other materials used besides lead for shielding 39
4. Radiation Protection and Exposure Control v v CT scanner shielding (Use NCRP 147 with web based scatter values) Personnel protection in Dx Radiology (lead aprons, thyroid shields etc. , pg. 771 of Bushberg) Shielding in nuclear medicine Shielding in PET (Beware!) Undershielding in some clinics have led to high technologist and non-occupational doses. PET shielding guide from AAPM is not published as yet. 40
4. Radiation Protection and Exposure Control Protection of the Patient in Medical X-ray Imaging v Tube Voltage and Beam Filtration v Achieve an optimal balance between image quality and dose to the patient v Patient exposure can be reduced by using a higher k. Vp ad lower m. As v Increasing k. Vp increases transmission (less absorption) of x-rays through the patient v Even though m. R/m. As increases as k. Vp increases, an accompanying reduction in m. As will decrease the incident exposure to the patient v Contrast will decrease due to higher effective energy of the x-ray beam 41
4. Radiation Protection and Exposure Control Protection of the Patient in Medical X-ray Imaging v Tube Voltage and Beam Filtration v Filtration of the polychromatic x-ray energy spectrum can significantly reduce exposure by selectively attenuating the low-energy x-rays in the beam v As the tube filtration increases, the beam becomes hardened (effective energy increases) and dose to patient decreases because fewer lowenergy photons are in the incident beam v The amount of filtration that can be added is limited by the increased demands on tube loading to offset reduction in tube output, and the decreased contrast due to excessive beam hardening v Quality of x-ray beam is assessed by measuring the HVL 42
Depth Dose v v Recall Dose = Energy absorbed per gram. For soft radiations, the dose decreases dramatically with depth as the patient’s body attenuates the beam. The radiation dose at a given depth is the depth dose (rad). The exposure at skin entrance (ESE) is the Roentgen exposure at the point where the radiation enters the body. 43
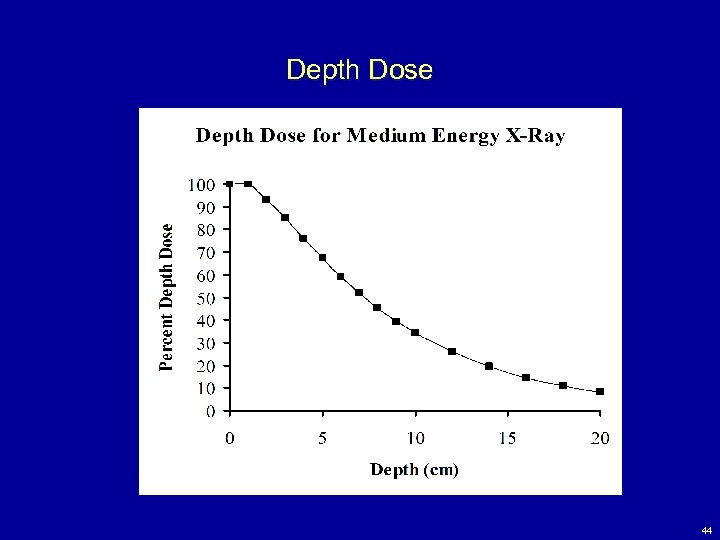
Depth Dose 44
4. Radiation Protection and Exposure Control Protection of the Patient in Medical X-ray Imaging v Field Area, Organ Shielding and Geometry v Reducing field size limits the patient volume exposed to primary beam, reduces the amount of scatter and thus radiation dose to adjacent organs (scatter being reduced improves image contrast) v Gonadal shielding can be used to protect the gonads from primary radiation when the shadow of the shield does not interfere with the anatomy under investigation v Increasing source-to-object distance (SOD) and source-to-image distance (SID) helps reduce dose (patient volume exposed decreased due to reduced beam divergence) v For fixed SID (C-arm fluoro system), patient dose is reduced by increasing the SOD as much as possible v A minimum patient to focal spot distance of 20 cm is required 45
4. Radiation Protection and Exposure Control Protection of the Patient in Medical X-ray Imaging v X-Ray Image Receptors v The speed of the image receptor determines the number of x-ray photons and thus the patient dose necessary to achieve an appropriate signal level v Higher speed system requires less exposure to produce the same optical density and thus reduces dose to patient v Either a faster screen (reduced spatial resolution) or faster film (increased quantum mottle) will reduce the incident exposure to the patient 46
4. Radiation Protection and Exposure Control Protection of the Patient in Medical X-ray Imaging v X-Ray Image Receptors v Computed Radiography (CR) devices have a wide dynamic range so they compensate to some degree for under- and overexposure and can reduce retakes v CR roughly equivalent to 200 speed screen-film systems v Techniques for extremities with CR devices should be used at higher exposure levels while exposures for pediatric patients should be used at increased speed (e. g. 400 speed) to reduce dose 47
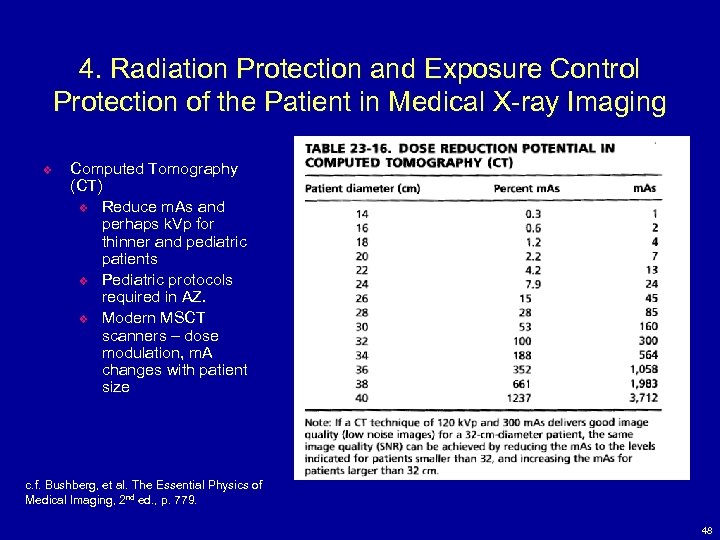
4. Radiation Protection and Exposure Control Protection of the Patient in Medical X-ray Imaging v Computed Tomography (CT) v Reduce m. As and perhaps k. Vp for thinner and pediatric patients v Pediatric protocols required in AZ. v Modern MSCT scanners – dose modulation, m. A changes with patient size c. f. Bushberg, et al. The Essential Physics of Bushberg, Medical Imaging, 2 nd ed. , p. 779. 48
4. Radiation Protection and Exposure Control Protection of the Patient in Medical X-ray Imaging v Miscellaneous Considerations v Careful identification of patients v Determination of pregnancy status v Eliminate screening exams that only rarely detect pathology v “yearly” dental exams may not be appropriate for all patients v Use of high speed dental film reduces dose v “yearly” screening mammography exams not appropriate for women younger than 35 to 40 years old v Technique errors and high repeat rates can be avoided by posting technique charts and using phototiming v Good quality control program to eliminate equipment and processor problems 49
4. Summary v v v Time, distance and shielding used to protect persons from radiation exposure Shielding calculations depend on m. R/week, workload, use factor, occupancy factor and distance from x-ray source Typically 2 or 4 lb/ft 2 lead is sufficient for shielding in diagnostic radiology Calculated using HVL and TVL of the material [(1/2)n – reduction in beam intensity, n is HVL] Protect patient by adjusting k. Vp, m. As, filtration, field size, geometry and using organ shielding, using faster film-screen systems, eliminate screening chest and yearly dental exams 50
Raphex 2000 General Questions v G 92. A shielding design for a diagnostic or therapy installation, when there is no restriction on the beam direction, must: v A. Consider all walls as primary barriers. B. Assign all walls a use factor (U) of 1. C. Assign all areas adjacent to the installation an occupancy factor (T) of 1. D. Shield all areas to a radiation level of 0. 1 rem per week. E. Shield such that adjacent areas will not receive instantaneous dose rates greater than 2 m. R/hr. v v 51
Raphex 2000 General Questions v G 93. The occupancy factor (T) is changed from 1/16 to 1/2 and the activity factor (A) is doubled for a radiation source whose HVL is 0. 3 mm Pb. In order to maintain the same level of protection, _____ mm Pb must be added to the shielding. v A. 0. 3 B. 0. 6 C. 0. 9 D. 1. 2 E. 1. 5 v v v The occupancy factor (T) is the fraction of time that the area is occupied. Since T is increased by a factor of 8 and the activity (A) is doubled, the exposure is increased by a factor of 16. Thus, 4 HVLs (24 = 16) of lead are required to maintain the same radiation level. 0. 3 mm x 4 = 1. 2 mm Pb. 52
5. Regulatory Agencies and Radiation Exposure Limits v U. S. Nuclear Regulatory Commission (NRC) regulates special nuclear material, source material, by-product material of nuclear fission, regulates the maximum permissible dose equivalent limits v Some states known as agreement states arrange with the NRC to selfregulate medically related licensing and inspection requirements of radioactive materials v Food and Drug Administration (FDA) regulates radiopharmaceutical development, manufacturing, performance and radiation safety requirements associated with the production of commercial x-ray equipment v U. S. Department of Transportation (DOT) regulates the transportation of radioactive materials 53
5. Advisory Bodies v National Council on Radiation Protection and Measurements (NCRP) v Collect, analyze, develop and disseminate, in the public interest, information and recommendations about radiation protection, radiation measurements, quantities and units v International Commission on Radiological Protection (ICRP) v Similar to NCRP, however its international membership brings to bear a variety of perspectives on radiation health issues v The NCRP and ICRP have published over 200 monographs containing recommendations on a wide variety of radiation health issues that serve as the reference documents from which many regulations are crafted 54
5. Summing internal and external doses v Dose from an internal exposure continues after the period of ingestion or inhalation, until the radioactivity is eliminated by radioactive decay or biologic removal v The committed dose equivalent (H 50, T) is the dose equivalent to a tissue or organ over the 50 years following the ingestion or inhalation of radioactivity v The committed effective dose equivalent (CEDE) is a weighted average of the committed dose equivalents to the various tissues and organs of the body v CEDE = w. T H 50, T 55
5. Summing internal and external doses v To sum the internal and external doses to any individual tissue or organ, the deep dose equivalent (indicated by the dosimeter) and the committed dose equivalent to the organ are added v The sum of the deep dose equivalent and the committed dose equivalent is called the total effective dose equivalent (TEDE) 56
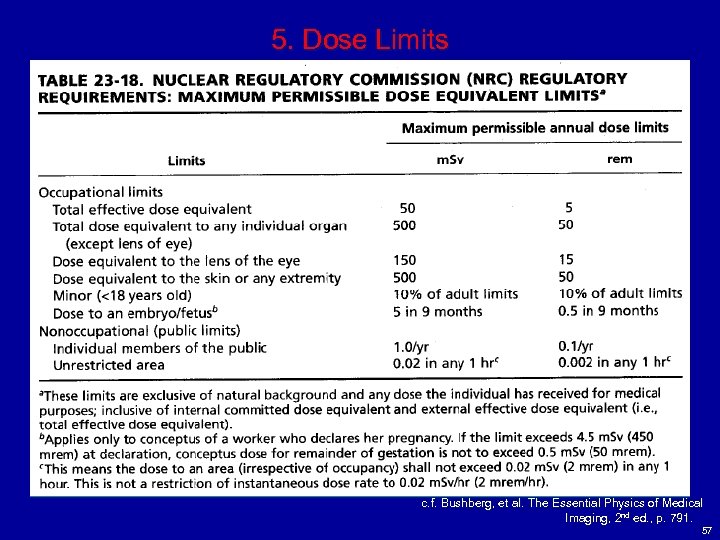
5. Dose Limits c. f. Bushberg, et al. The Essential Physics of Medical Bushberg, Imaging, 2 nd ed. , p. 791. 57
5. As Low As Reasonably Achievable (ALARA) Principle v Dose limits to workers and the public are regarded as upper limits rather than as acceptable doses or thresholds of safety v In addition to the dose limits, all licenses are required to employ good health physics practices and implement radiation safety programs to ensure that radiation exposures are kept as low as reasonably achievable (ALARA), taking societal and economic factors into consideration v The ALARA doctrine is the driving force for many of the policies, procedures, and practices in radiation laboratories, and represents a commitment by both employee and employer to minimize radiation exposure to staff, the public, and the environment to the greatest extent possible 58
5. Summary v v v Regulatory agencies, advisory bodies and their functions Dose limits v Occupational and public dose limits v Organ limits ALARA principle 59
Raphex 2001 General Questions v G 82. The annual recommended dose to the lens of the eye of a radiation worker is: v A. 500 m. Sv (50 rem) B. 150 m. Sv (15 rem) C. 50 m. Sv (5 rem) D. 5 m. Sv (500 mrem) E. 1 m. Sv (100 mrem) v v 60
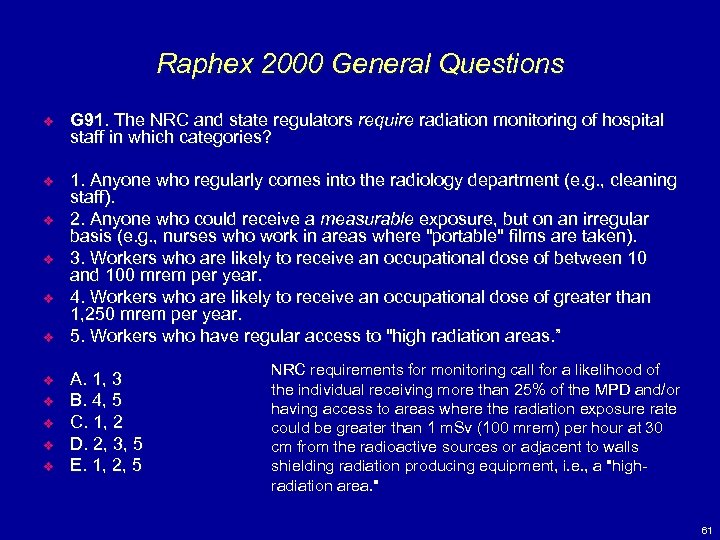
Raphex 2000 General Questions v G 91. The NRC and state regulators require radiation monitoring of hospital staff in which categories? v 1. Anyone who regularly comes into the radiology department (e. g. , cleaning staff). 2. Anyone who could receive a measurable exposure, but on an irregular basis (e. g. , nurses who work in areas where "portable" films are taken). 3. Workers who are likely to receive an occupational dose of between 10 and 100 mrem per year. 4. Workers who are likely to receive an occupational dose of greater than 1, 250 mrem per year. 5. Workers who have regular access to "high radiation areas. ” v v v v v A. 1, 3 B. 4, 5 C. 1, 2 D. 2, 3, 5 E. 1, 2, 5 NRC requirements for monitoring call for a likelihood of the individual receiving more than 25% of the MPD and/or having access to areas where the radiation exposure rate could be greater than 1 m. Sv (100 mrem) per hour at 30 cm from the radioactive sources or adjacent to walls shielding radiation producing equipment, i. e. , a "highradiation area. " 61
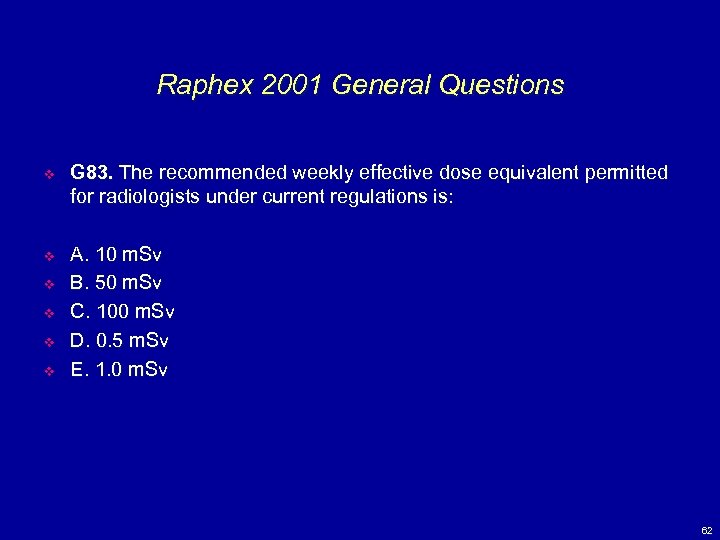
Raphex 2001 General Questions v G 83. The recommended weekly effective dose equivalent permitted for radiologists under current regulations is: v A. 10 m. Sv B. 50 m. Sv C. 100 m. Sv D. 0. 5 m. Sv E. 1. 0 m. Sv v v 62
bf7368937e8626c384539787cb252fa8.ppt