5b2025da8f1ff6b14baae572b2542dea.ppt
- Количество слайдов: 32

Quality Metrics In CRRT Dr Prabh Nayak Lead Consultant for CRRT, Liver, Kidney & Small Bowel Transplant Birmingham Children’s Hospital, UK

Where are we?
BCH 31 bedded PICU with approx 1500 admissions annually Children’s hospital with all major subspecialities represented (renal, liver, cardiac surgery, ECLS, haem-onc, neurosurgery, trauma, burns, metabolic, transplant) CRRT service model: PIC driven and PIC delivered 50 -60 patients receive CVVH/CVVHDF per year
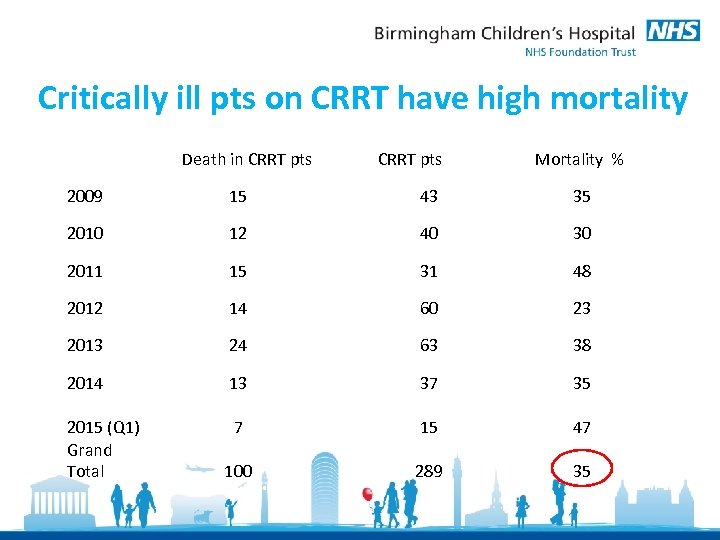
Critically ill pts on CRRT have high mortality Death in CRRT pts Mortality % 2009 15 43 35 2010 12 40 30 2011 15 31 48 2012 14 60 23 2013 24 63 38 2014 13 37 35 2015 (Q 1) Grand Total 7 15 47 100 289 35
Quality in CRRT To be able to deliver a consistent service with minimal deviation from the standard & minimise variation in practice with minimal complications. Standards & guidelines To the right patient At the right time In the right setting Using the right equipment By the right people Knowledge sharing & improvement
Quality Improvement Metrics Outcomes - Circuit life - Circuit downtime - Time to initiate in time-critical conditions (hyperammonaemia) - Ability to provide intra-operative CRRT cover Safety - Any human factors issues? Cost Improvement Process (Vascath, CVVH solutions) Morbidity and mortality case reviews; Audit against standards Service improvements Educational preparedness: Wet labs, simulation sessions
‘Standardisation’ of timing of CRRT initiation possible?
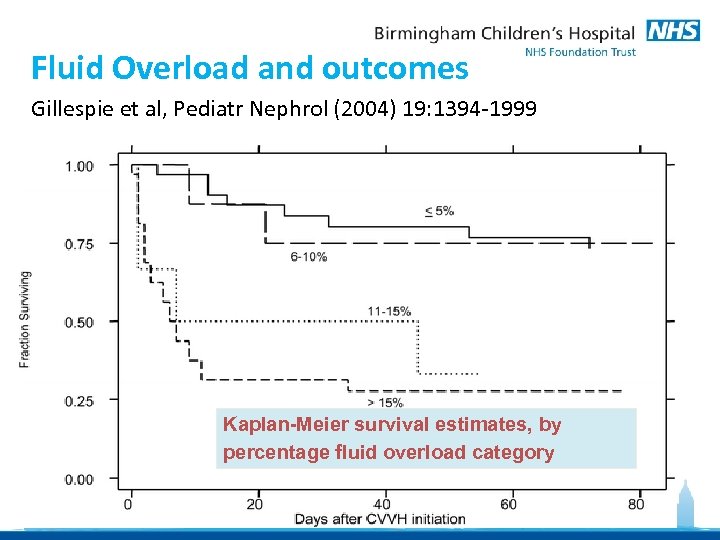
Fluid Overload and outcomes Gillespie et al, Pediatr Nephrol (2004) 19: 1394 -1999 Kaplan-Meier survival estimates, by percentage fluid overload category
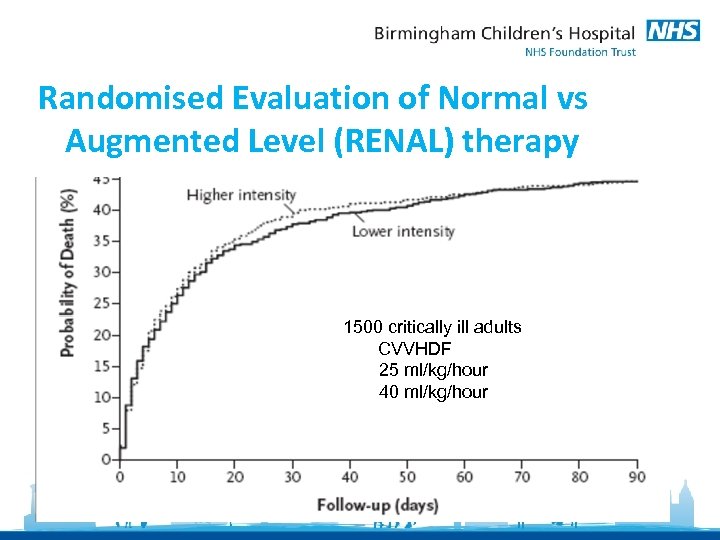
Randomised Evaluation of Normal vs Augmented Level (RENAL) therapy 1500 critically ill adults CVVHDF 25 ml/kg/hour 40 ml/kg/hour
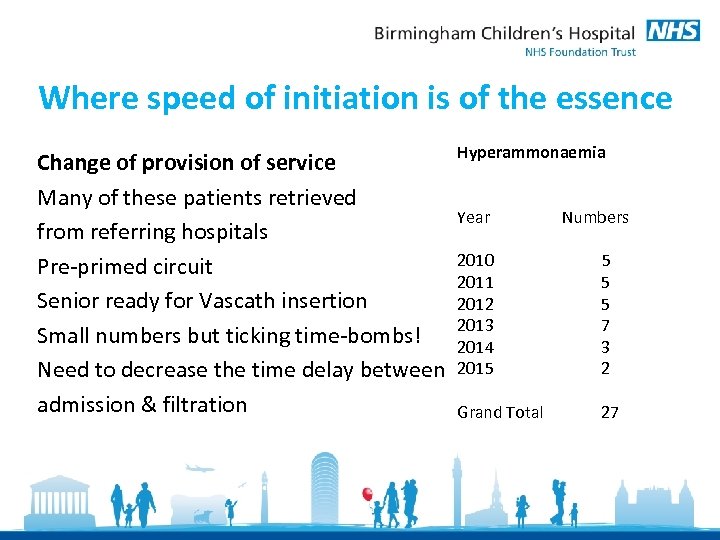
Where speed of initiation is of the essence Change of provision of service Many of these patients retrieved from referring hospitals Pre-primed circuit Senior ready for Vascath insertion Small numbers but ticking time-bombs! Need to decrease the time delay between admission & filtration Hyperammonaemia Year Numbers 2010 2011 2012 2013 2014 2015 5 7 3 2 Grand Total 27

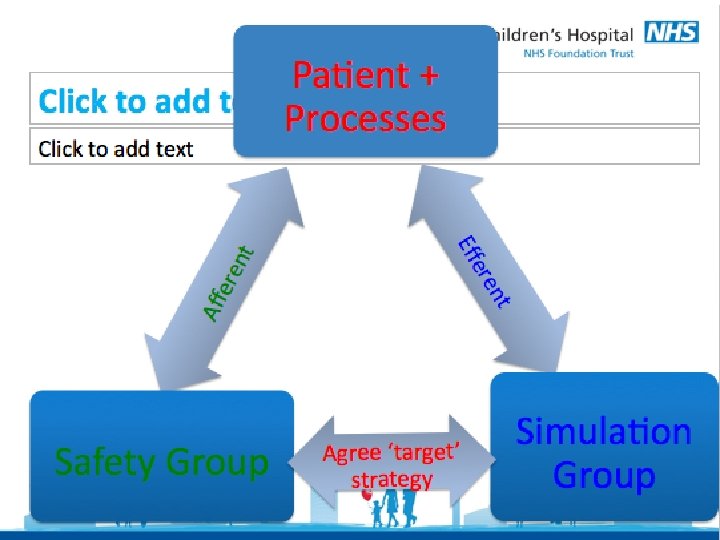
Build a good ‘CRRT team’
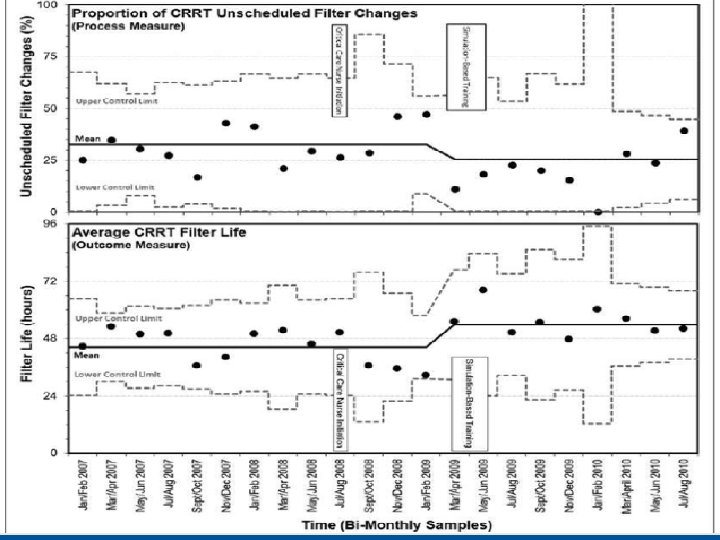
Bridging The Gap: Improving Patient Safety Through Targeted In-Situ Simulation Training Nayak PP, Kidd N, Osborne-Ricketts B, Martin J, Heward Y Pediatric Critical Care Medicine: May 2014 - Volume 15 - Issue 4 (=proof of high quality care and excellent outcomes)
Bridging The Gap: Improving Patient Safety Through Targeted In-Situ Simulation Training Nayak PP, Kidd N, Osborne-Ricketts B, Martin J, Heward Y Pediatric Critical Care Medicine: May 2014 - Volume 15 - Issue 4 (=proof of high quality care and excellent outcomes)
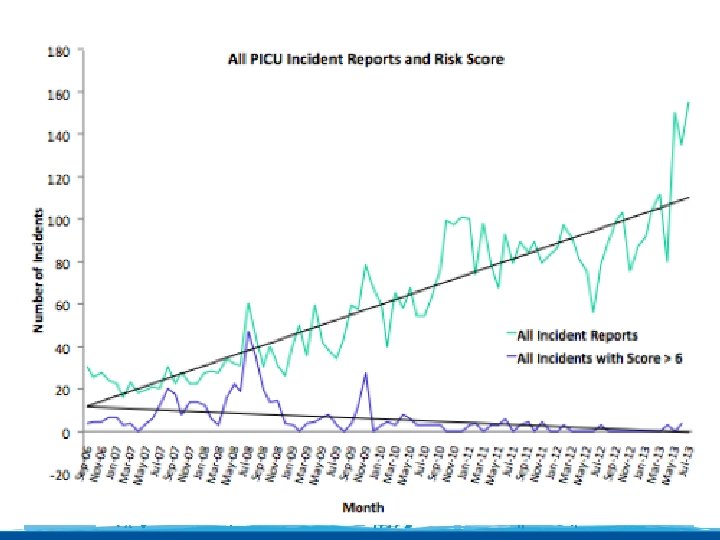
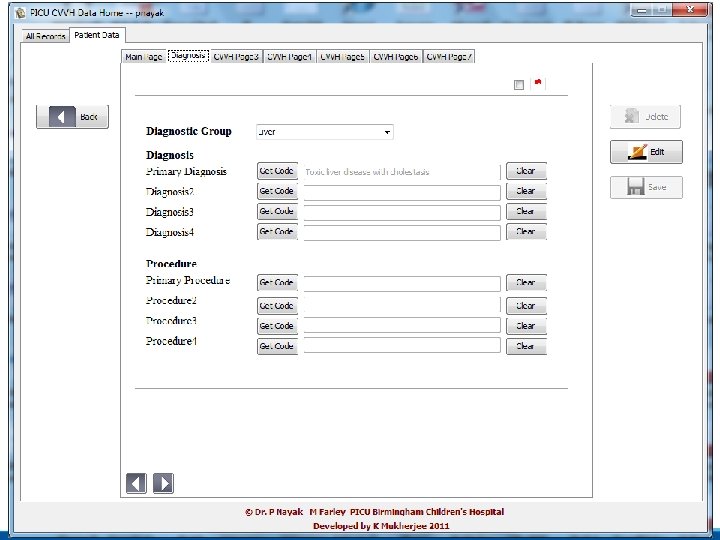
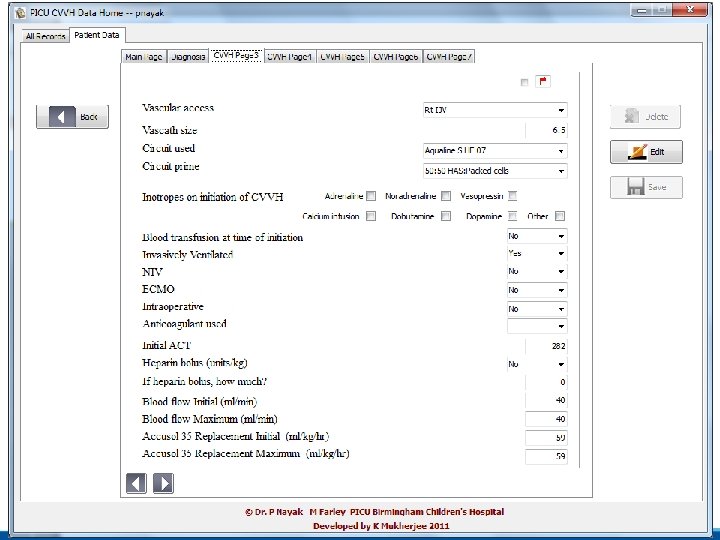
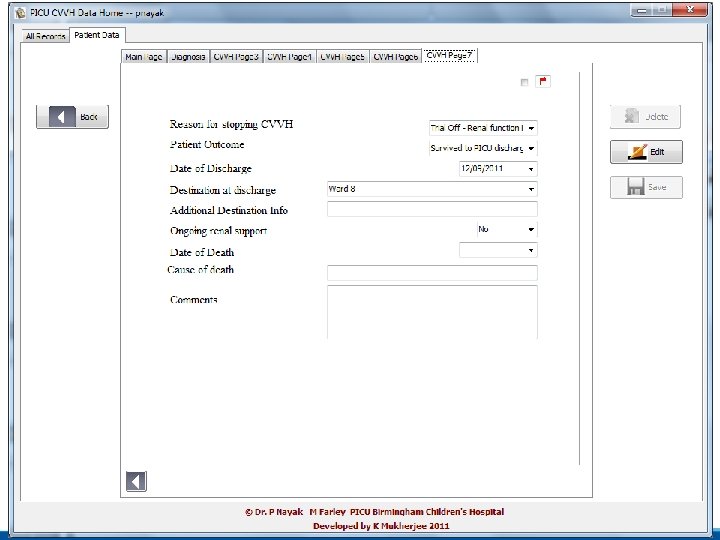
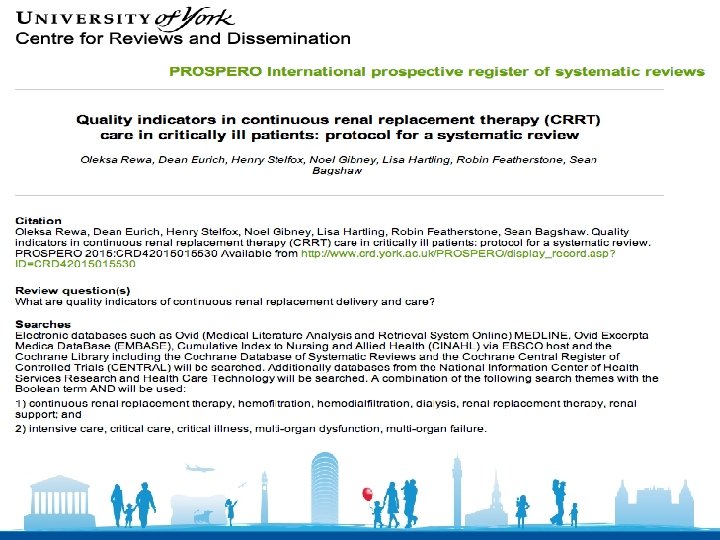
Collect data, analyse and modify practice
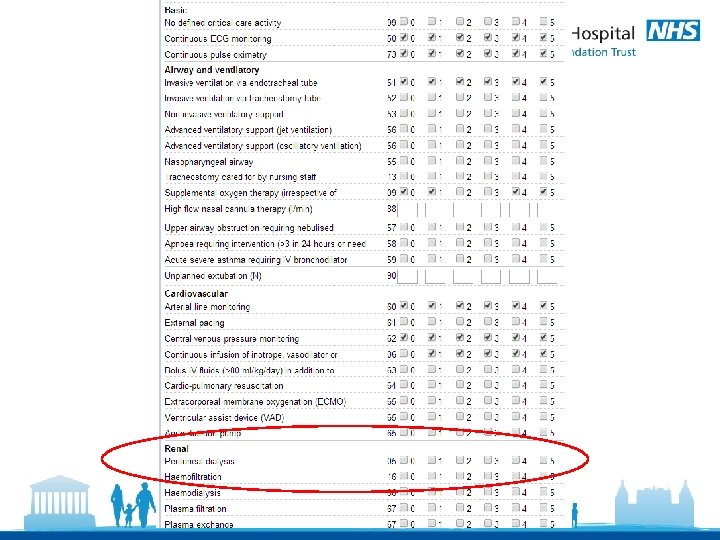
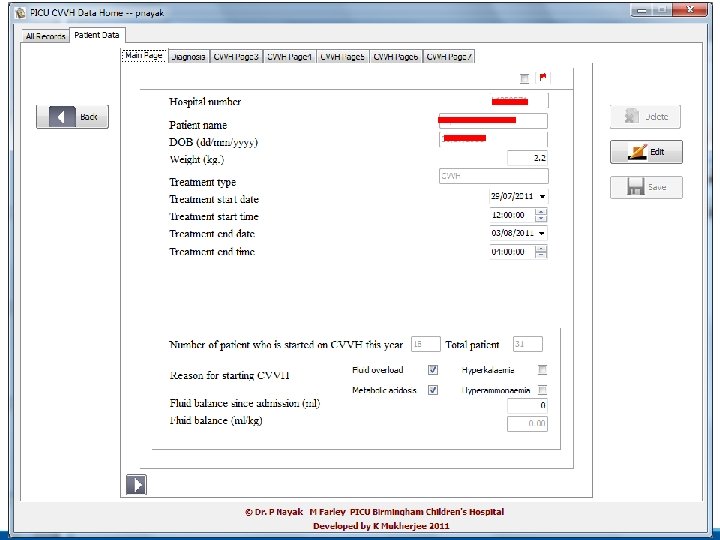
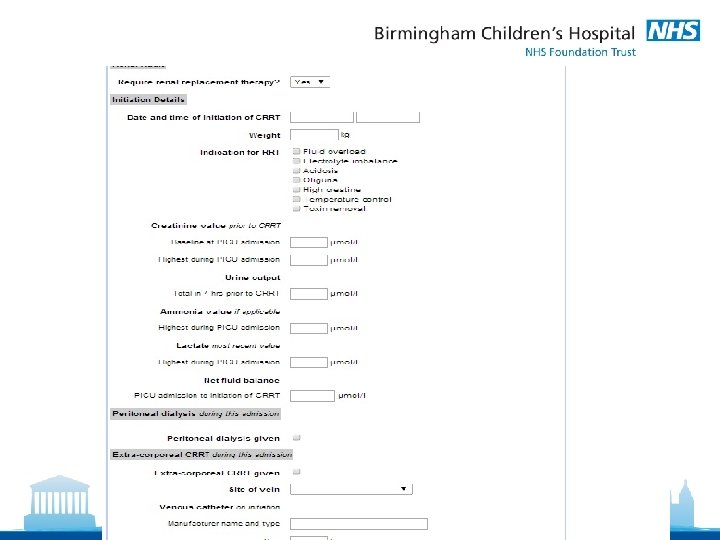
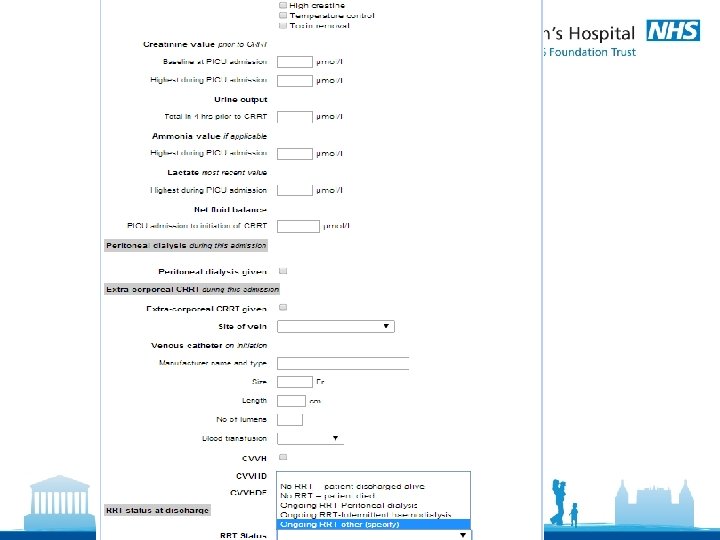
CRRT Database @ BCH
PICANET (Paediatric Intensive Care Audit Network, UK) dataset collection from 2015
What does the future hold? Timing of initiation of CRRT & role of biomarkers? Drug PK studies on extracorporeal circuit Technological innovations in circuit sizes Subspecialised CRRT teams Shared learning from pooled data; multi-centre research

Thank you
5b2025da8f1ff6b14baae572b2542dea.ppt