1a90b6b122c4a901a528c7d8bef80801.ppt
- Количество слайдов: 49
Quality Improvement 101 Lois L. Bready, M. D. Associate Dean for GME and DIO UTHSCSA
Quality Improvement 1. 2. 3. 4. What is ‘quality improvement’? Why is it important to the resident? To the practicing physician? How does QI relate to Patient Safety?
Competency Questions in your PIF b) Quality Improvement 1. List the activities in which residents actively participate to learn and apply the principles of quality improvement, and identify those who oversee these activities. 2. Give an example of a quality improvement activity/project that residents have been involved with during the past year or are currently. Describe its development, goal, implementation, evaluation of success. 3. How does the program ensure that residents provide and document continuity of care?
Quality Improvement – What is it? Incorporated in the ACGME General Competence “Practice Based Learning & Improvement” “Residents must be able to investigate and evaluate their patient care practices, appraise and assimilate scientific evidence, and improve their patient care practices. ”

Quality Improvement Components: • Self-reflection • Quality or Practice Improvement • Lectures/Seminars/Conferences • Quality Improvement Project • Evidence Based Medicine • Teaching Skills
“Systems Based Practice” Content Setting • Health Care System • Different types of medical practice and delivery systems • System resources • System issues and the reduction of errors • Conducting a root cause analysis • Clinical teaching • Patient Safety projects • Systems based approach - M & M • Lectures/Seminars/Confe rences • Interdisciplinary Teams

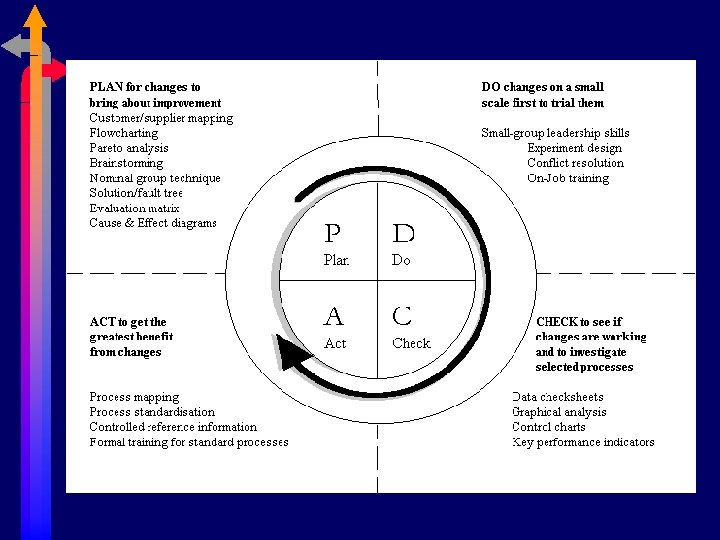
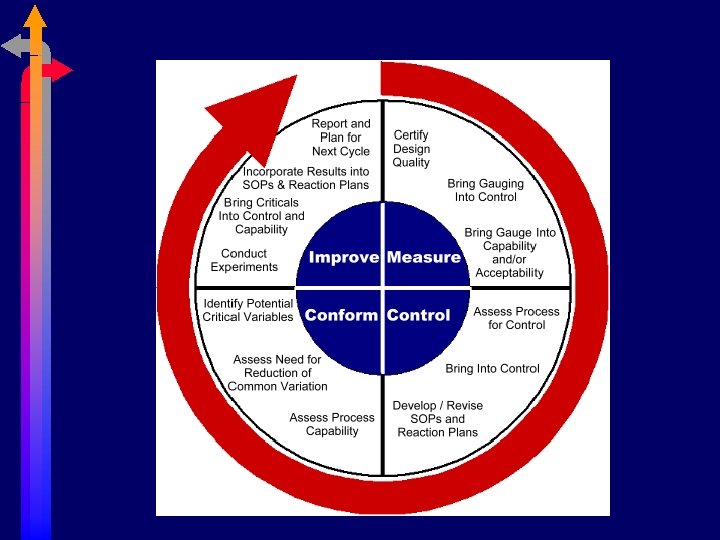
Quality Improvement Model
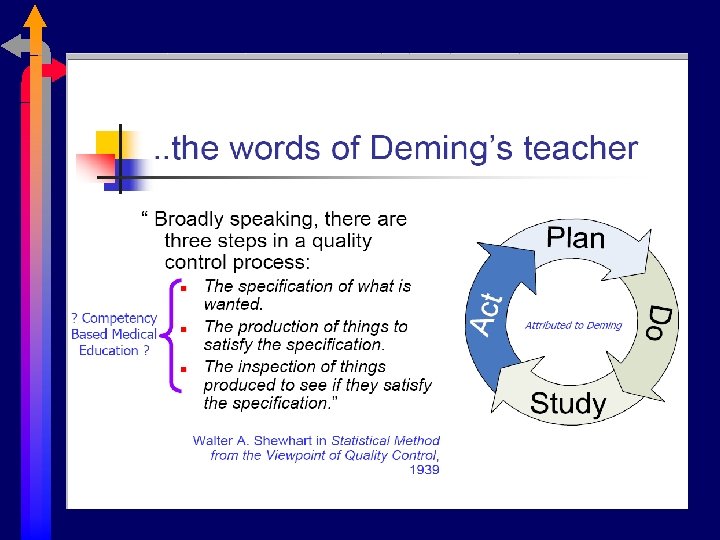
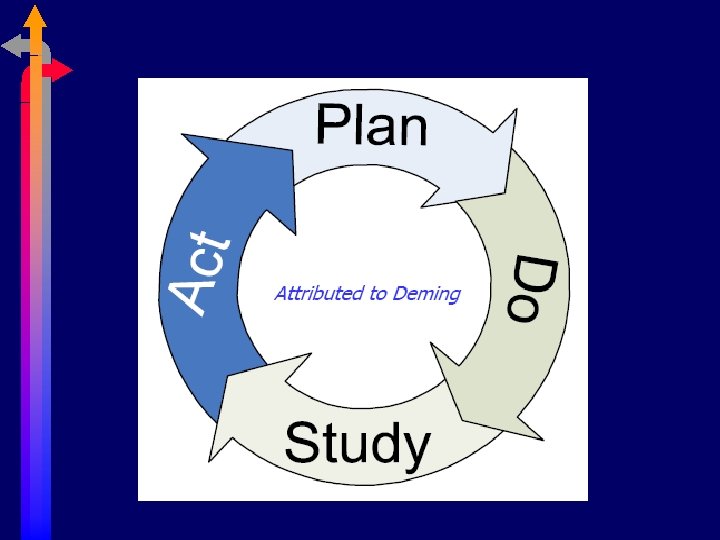
Quality Improvement W. Edwards Deming • American statistician, professor, author, lecturer, and consultant • Improved production in the U. S. during World War II and in Japan after the war • Pioneer – use of statistical analysis to achieve better industrial quality control – ‘quality movement’
Quality Improvement Quality improvement - a method for ensuring that all the activities necessary to design, develop and implement a product or service are effective and efficient with respect to the system and its performance.

Quality Improvement Health care • “Quality improvement” • “Quality & risk management” • “Quality and performance improvement” • “Compliance and quality improvement” • “TQM = total quality management” • Variations on those themes. . .
Quality Improvement General uses: 1. “How can we make ___ process more efficient? ” • • • EC patient through-put MICU bed turnover OR utilization 2. “Why did this patient receive tube feedings into the brochus? ” 3. “What are Dr. X’s patient care outcomes? ” 4. “How can we ensure that all residents pass their board exams on the first attempt? ”
Quality Improvement Quality improvement project: 1. Identify an issue 2. Build a team to address it 3. Define the problem 4. Choose a target 5. Test the change 6. Reconsider or extend the improvement efforts

Quality Improvement Quality improvement project: 1. Identify an issue A process that is causing concern or a possible opportunity for a positive change.

Quality Improvement Quality improvement project: 2. Build a team to address it Representation from groups involved – this step is critical.

Quality Improvement Quality improvement project: 3. Define the problem Identify and carefully describe what it is you really want to improve; the source of the problem you are confronting, etc.

Quality Improvement Quality improvement project: 4. Choose a target Introduce and evaluate interventions, using quality improvement tools and skills
Quality Improvement Quality improvement project: 5. Test the change Data measures to determine when a process change over time is likely to be due to chance and when it is not
Quality Improvement Quality improvement project: 6. Reconsider or extend the improvement efforts Reconsider, sustain, and/or extend process improvements
Patient Safety Issues • ‘First do no harm’ • Build systems with safety barriers • So, why do adverse outcomes continue to happen? ?

Quality Improvement Sentinel Event A sentinel event is an unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof. Serious injury specifically includes loss of limb or function. The phrase, "or the risk thereof" includes any process variation for which a recurrence would carry a significant chance of a serious adverse outcome. Such events are called "sentinel" because they signal the need for immediate investigation and response. www. jointcommission. org/Sentinel. Events/
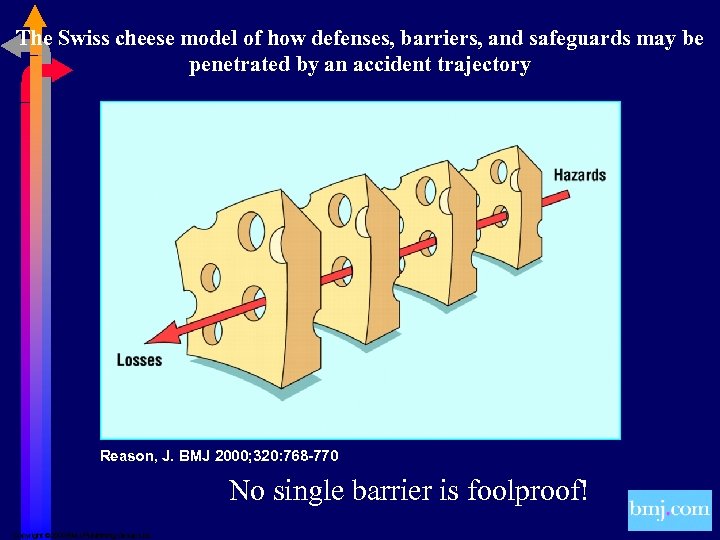
The Swiss cheese model of how defenses, barriers, and safeguards may be penetrated by an accident trajectory Reason, J. BMJ 2000; 320: 768 -770 No single barrier is foolproof! Copyright © 2000 BMJ Publishing Group Ltd.
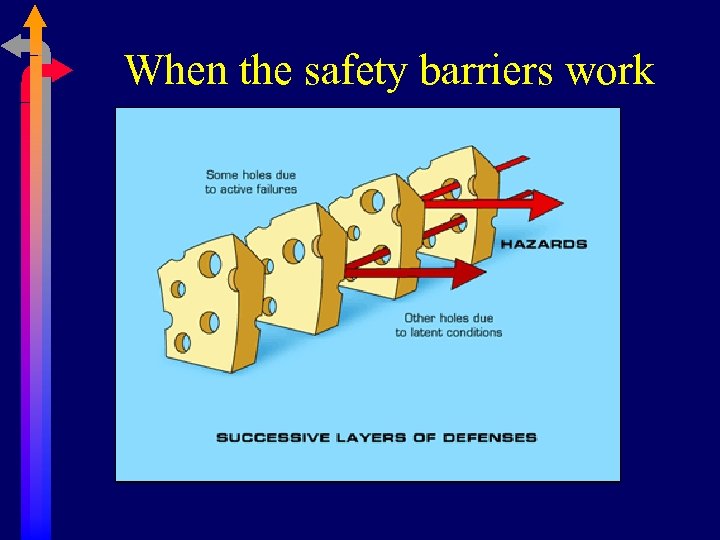
When the safety barriers work
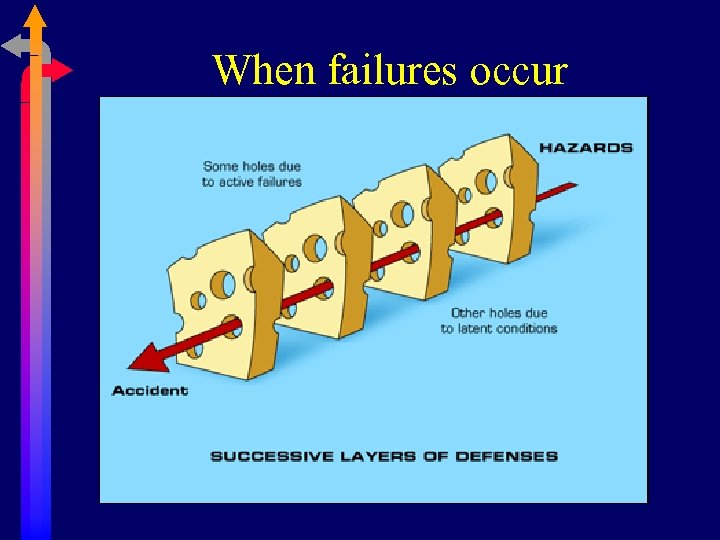
When failures occur
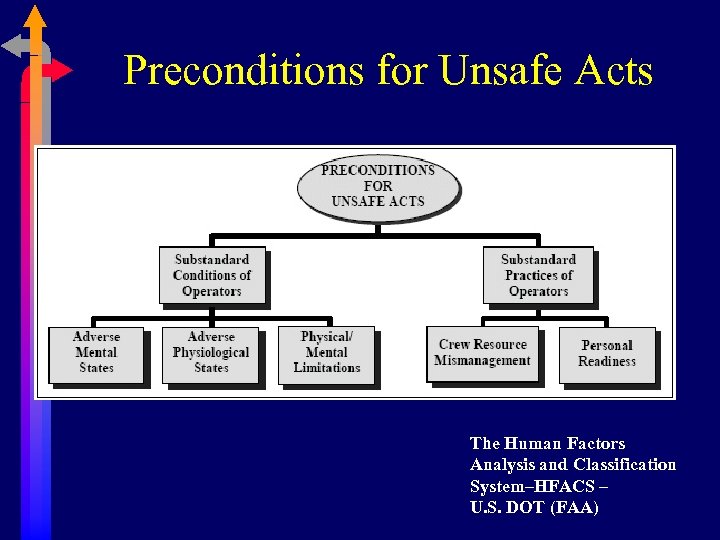
Preconditions for Unsafe Acts The Human Factors Analysis and Classification System–HFACS – U. S. DOT (FAA)
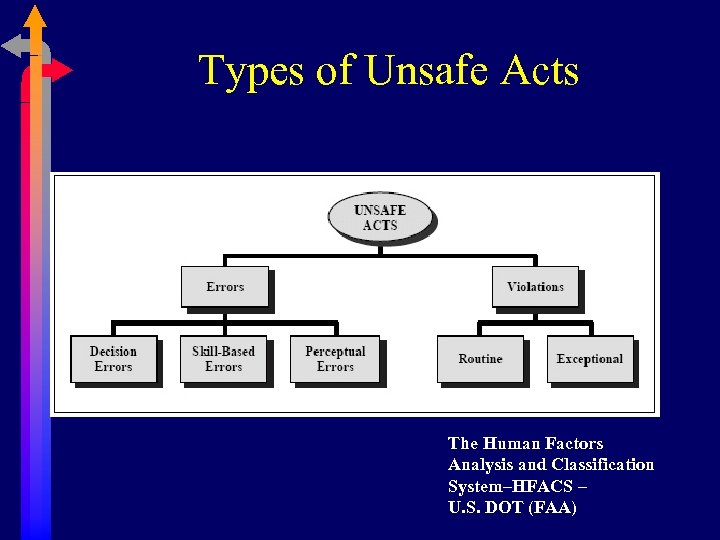
Types of Unsafe Acts The Human Factors Analysis and Classification System–HFACS – U. S. DOT (FAA)
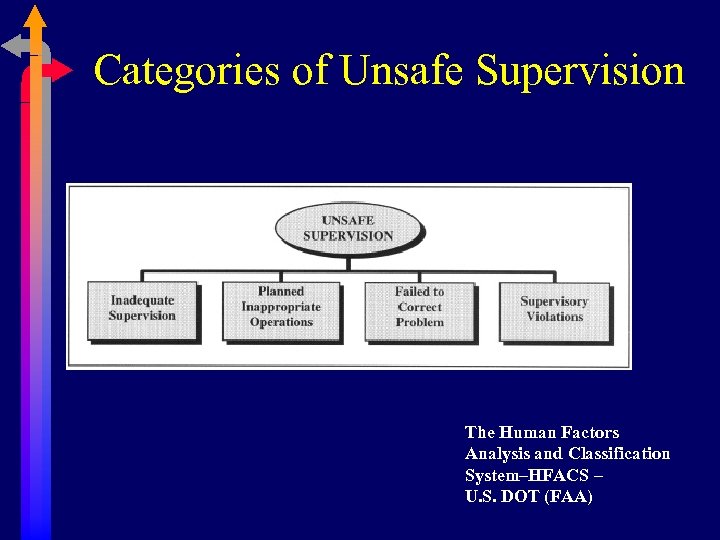
Categories of Unsafe Supervision The Human Factors Analysis and Classification System–HFACS – U. S. DOT (FAA)

Quality Improvement Tools
Quality Improvement Root cause analysis (RCA) is a class of problem solving methods aimed at identifying the root causes of problems or events. Systems need designed-in redundancy so that desired outcomes don’t depend on “the ____ being more careful. . . ”
Root Cause Analysis The practice of RCA is predicated on the belief that problems are best solved by attempting to correct or eliminate root causes, as opposed to merely addressing the immediately obvious symptoms. By directing corrective measures at root causes, it is hoped that the likelihood of problem recurrence will be minimized. However, it is recognized that complete prevention of recurrence by a single intervention is not always possible. Thus, RCA is often considered to be an iterative process, and is frequently viewed as a tool of continuous improvement.
Quality Improvement Safety-based RCA descends from the fields of accident investigation and occupational safety and health. Root causes tend to be viewed as failed or missing safety barriers, unrecognized risks or hazards, or inadequate safety engineering.
Quality Improvement General principles of root cause analysis • Aiming corrective measures at root causes is more effective than merely treating the symptoms of a problem. • To be effective, RCA must be performed systematically, and conclusions must be backed up by evidence. • There is usually more than one root cause for any given problem.
Quality Improvement General process for performing RCA • Define the problem. • Gather data/evidence. • Identify problems that contributed to problem (Causal Factors). • Find root causes for each Causal Factor. • Develop solution recommendations. • Implement the solutions.
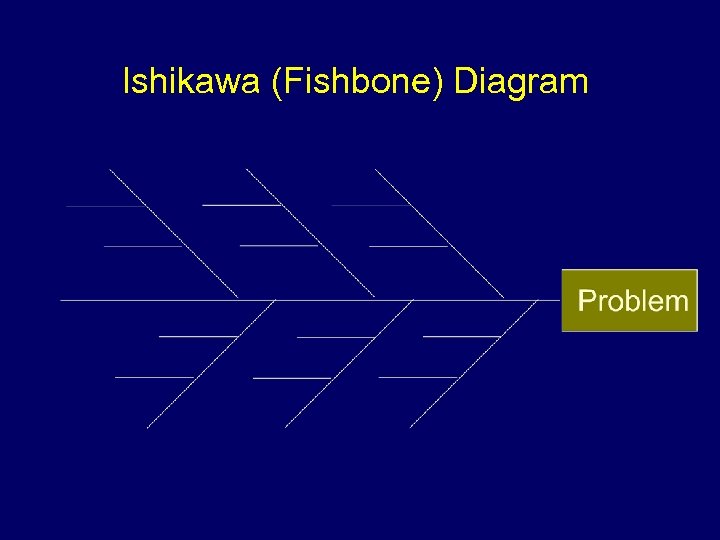
Ishikawa (Fishbone) Diagram
Ishikawa (Fishbone) Diagram The 4 M’s: • Methods, Machines, Materials, Manpower The 4 P’s: • Place, Procedure, People, Policies The 4 S’s: • Surroundings, Suppliers, Systems, Skills
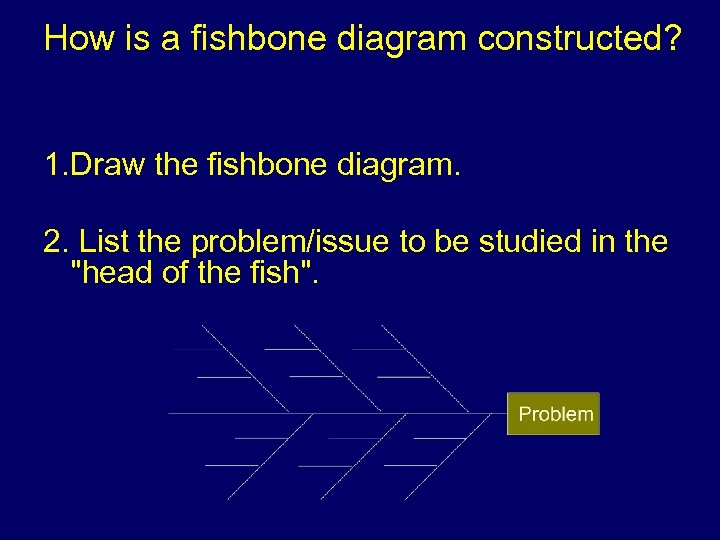
How is a fishbone diagram constructed? 1. Draw the fishbone diagram. 2. List the problem/issue to be studied in the "head of the fish".
3. Label each ""bone" of the "fish". The major categories typically utilized are: The 4 M’s: Methods, Machines, Materials, Manpower The 4 P’s: Place, Procedure, People, Policies The 4 S’s: Surroundings, Suppliers, Systems, Skills Note: You may use one of the four categories suggested, combine them in any fashion or make up your own. The categories are to help you organize your ideas.
4. Use an idea-generating technique (e. g. , brainstorming) to identify the factors within each category that may be affecting the problem/issue and/or effect being studied. The team should ask. . . "What are the machine issues affecting/causing. . . “ 5. Repeat this procedure with each factor under the category to produce sub-factors. Continue asking, "Why is this happening? " and put additional segments each factor and subsequently under each sub-factor. Continue until you no longer get useful information as you ask, "Why is that happening? "
6. Analyze the results of the fishbone after team members agree that an adequate amount of detail has been provided under each major category. Do this by looking for those items that appear in more than one category. These become the 'most likely causes". 7. For those items identified as the "most likely causes", the team should reach consensus on listing those items in priority order with the first item being the most probable" cause.

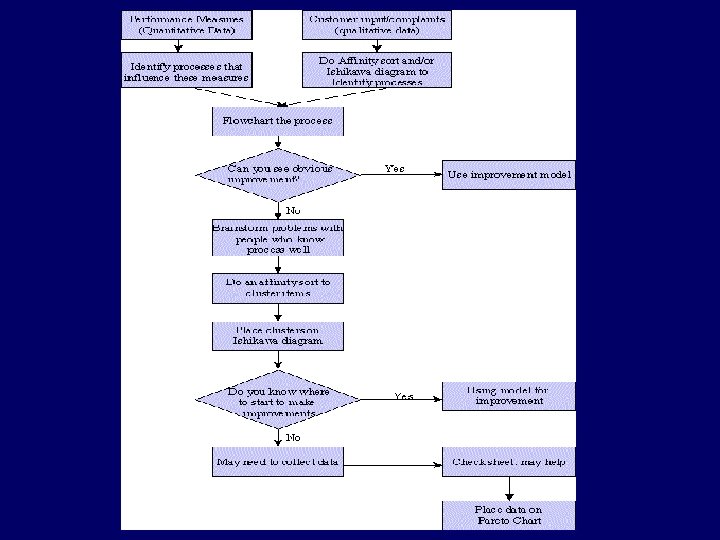
Quality Improvement Processes
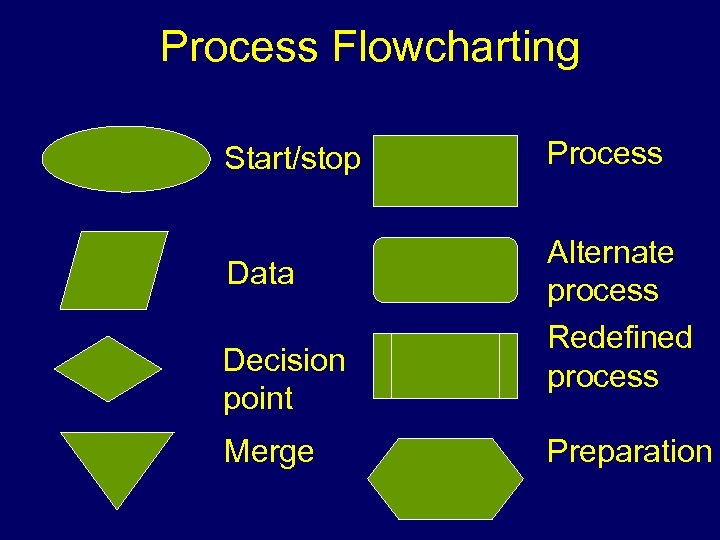
Process Flowcharting Start/stop Data Decision point Merge Process Alternate process Redefined process Preparation

Quality Improvement Control chart
Where are we now? List the activities in which residents actively participate to learn and apply the principles of quality improvement, and identify those who oversee these activities.
Where are we now? Give an example of a quality improvement activity/project that residents have been involved with during the past year or are currently. Describe its development, goal, implementation, evaluation of success.
Where are we now? How does the program ensure that residents provide and document continuity of care?
1a90b6b122c4a901a528c7d8bef80801.ppt