6e645a1a798fe8cc44cc3db453afeccb.ppt
- Количество слайдов: 35
QIPP SAFE CARE DESIGNING RELIABLE SYSTEMS AILSA BROTHERTON PROGRAMME DIRECTOR SLIDES KINDLY SUPPLIED BY: KEVIN STEWART MEDICAL DIRECTOR SAFE CARE WORK STREAM QIPP, DEPARTMENT OF HEALTH
ABOUT ME Since June 2010 Programme Director, QIPP Safe Care, Department of Health 2005 -2010 Senior Research Fellow: University of Central Lancashire 1991 -2004 Clinical Dietetics Head of Acute Dietetics Assistant Director of Operations Career Focus: improving nutritional care for patients
THE 4 PRINCIPLES OF GOOD NUTRITIONAL CARE 1. Identify those with malnutrition or at risk of malnutrition through screening and assessment e. g. the MUST Tool 2. Implement ‘individualised’ care pathways for the malnourished and those at risk appropriate to the care setting 3. Provide training on the importance of nutritional care for all care staff appropriate to care setting, profession and responsibilities 4. Ensure multidisciplinary structures to manage and monitor nutritional care
STANDARDS AND GUIDELINES IN NUTRITIONAL CARE Patient Environment Action Teams (PEAT), 2000 Better Hospital Food, 2001 Essence of Care, 2001 National minimum standards, 2001 Nutrition and Patients; A doctor’s responsibility, RCP London, 2002 Council of Europe Resolution, 10 key characteristics of good nutritional care, 2003 NICE guidance on nutrition support in adults, 2006 Delivering Nutritional Care through Food and Beverage Services, 2006 Malnutrition among Older People in the Community. Policy recommendations for change, 2006 Malnutrition, what nurses working with children and young people need to know and do, 2006 Good Practice Guide, Healthcare Food and Beverage Service Standards: A guide to ward level services, 2006 Improving nutritional care. A joint action plan from the DH & Nutrition Summit stakeholders, 2007 Nutrition Now, 2007 Care Services Improvement Partnership factsheet 22; Catering arrangements in Extra Care Housing, 2007 NICE Guidance on maternal and child nutrition, 2008 NPSA factsheets on the 10 key characteristics of good nutritional care, 2009 Social Care Institute for Excellence Guide: Dignity in Care; Nutritional Care and Hydration, 2009 Improving nutritional care and treatment. Perspectives and recommendations from population groups, patients and carers, 2009 Appropriate Use of Oral Nutritional Supplements in Older People, 2009 Malnutrition Matters: Meeting Quality Standards in Nutritional Care
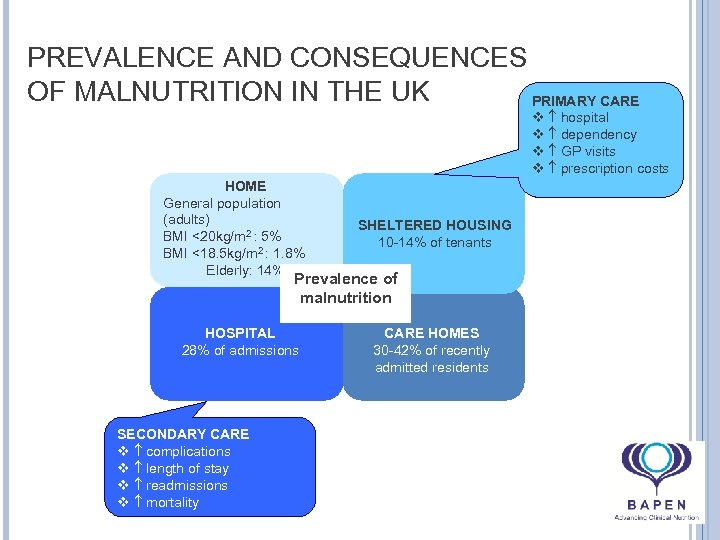
PREVALENCE AND CONSEQUENCES OF MALNUTRITION IN THE UK PRIMARY CARE v hospital v dependency v GP visits v prescription costs HOME General population (adults) BMI <20 kg/m 2 : 5% BMI <18. 5 kg/m 2 : 1. 8% Elderly: 14% SHELTERED HOUSING 10 -14% of tenants Prevalence of malnutrition HOSPITAL 28% of admissions SECONDARY CARE v complications v length of stay v readmissions v mortality CARE HOMES 30 -42% of recently admitted residents
RELIABILITY Is not; about what clinical care should be given (we know that) Is; about the process of ensuring that patients get care Reliably Consistently On time


MEASURING RELIABILITY = number of processes which achieve the desired result…. . . divided by total number of processes
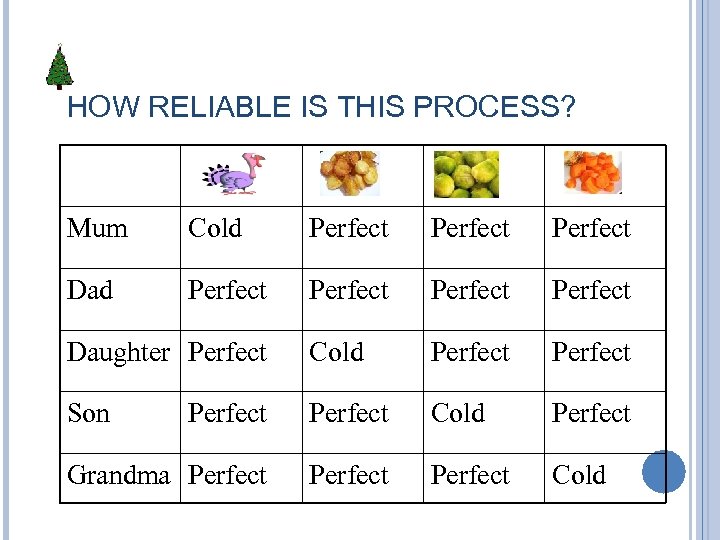
HOW RELIABLE IS THIS PROCESS? Mum Cold Perfect Dad Perfect Daughter Perfect Cold Perfect Son Perfect Cold Perfect Grandma Perfect Cold
IS IT…? 4 cold dishes out of a possible 20 = 20% failure Or 1 person out of 5 got a perfect lunch (80% failure)
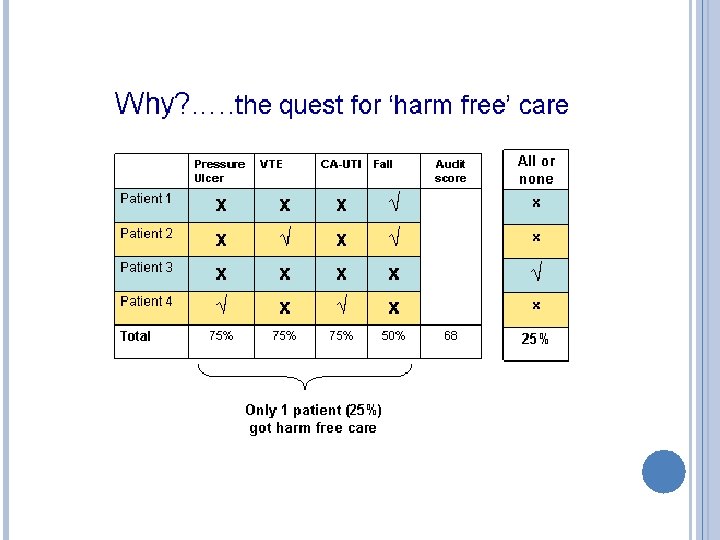
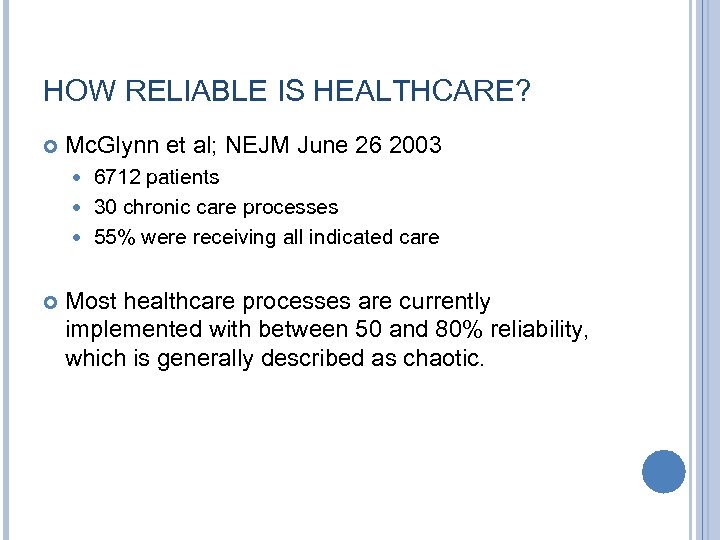
HOW RELIABLE IS HEALTHCARE? Mc. Glynn et al; NEJM June 26 2003 6712 patients 30 chronic care processes 55% were receiving all indicated care Most healthcare processes are currently implemented with between 50 and 80% reliability, which is generally described as chaotic.
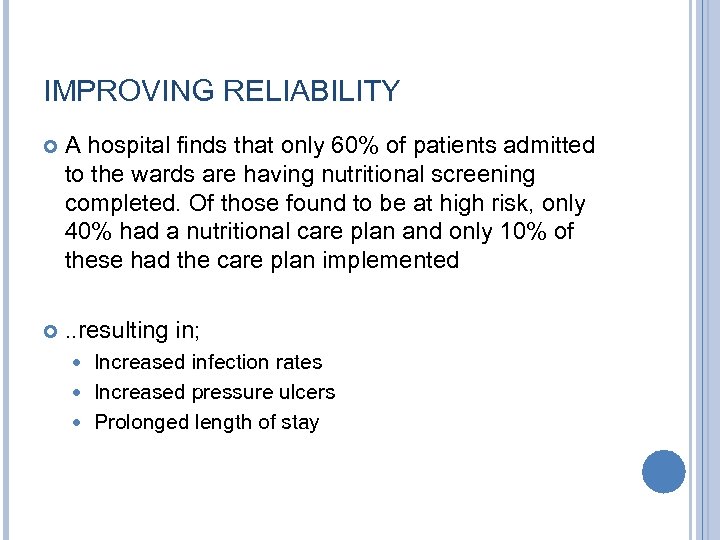
IMPROVING RELIABILITY A hospital finds that only 60% of patients admitted to the wards are having nutritional screening completed. Of those found to be at high risk, only 40% had a nutritional care plan and only 10% of these had the care plan implemented . . resulting in; Increased infection rates Increased pressure ulcers Prolonged length of stay
CHAT BOX DISCUSSION Thought to be mostly due to; Delays in using the MUST screening tool Delays in referral to the Dietician and SALT for detailed assessments Confusion about when and how to complete the MUST tool and whose responsibility it is to develop a nutritional care plan Poor management structures / nutritional care pathways – especially when patients move between care settings Type in the chat box how might we go about addressing this issue?
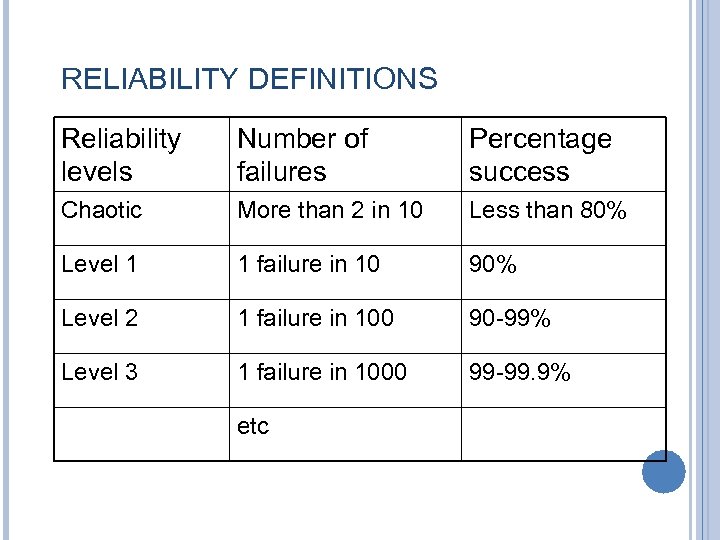
RELIABILITY DEFINITIONS Reliability levels Number of failures Percentage success Chaotic More than 2 in 10 Less than 80% Level 1 1 failure in 10 90% Level 2 1 failure in 100 90 -99% Level 3 1 failure in 1000 99 -99. 9% etc
DESIGNING FOR RELIABILITY Level 1 Level 2 Intent, vigilance, hard work, audit Design of processes informed by reliability science and knowledge of human factors Level 3 System-wide focus on becoming a highly reliable organisation
LEVEL 1 TECHNIQUES; INTENT, VIGILANCE, HARD WORK Standard equipment Feedback Training and education Reminders Standard order sets Personal checklists
LEVEL 1 TECHNIQUES …are only ever likely to achieve around 90% reliability, because; This is probably the limit of human reliability when working with complex systems Vigilance is highly dependent on uncontrollable external factors
FACTORS AFFECTING VIGILANCE Fatigue Stress Competing demands Environmental conditions Task design
LEVEL 2 TECHNIQUES Moving from level 1 (90% reliable) to level 2 (99% reliable) usually requires an understanding of human factors and reliability science

LEVEL 2 TECHNIQUES

LEVEL 2 TECHNIQUES
LEVEL 2 TECHNIQUES
LEVEL 2 APPROACHES Making the desired action the default Decision aids and reminders in the system Design changes Take advantage of habits and patterns Build in redundancy
SOME OTHER EXAMPLES? In everyday life? In healthcare?
EXAMPLES Different coloured vials for drugs which are often confused Connectors; for intravenous access Automated alerts for allergies, drug interactions etc on electronic systems Default options for drug doses Pre-printed drug charts
LEVEL 3 AND BEYOND To improve reliability beyond level 2 usually requires fundamental system redesign Based on Failure Modes and Effects analysis which analyse process failures in detail and changes the systems accordingly This will be the focus of Next Week’s Webex
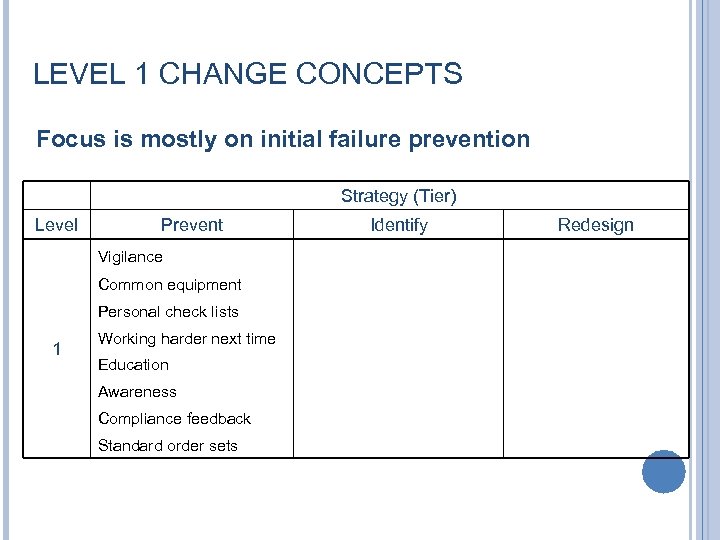
LEVEL 1 CHANGE CONCEPTS Focus is mostly on initial failure prevention Strategy (Tier) Level Prevent Vigilance Common equipment Personal check lists 1 Working harder next time Education Awareness Compliance feedback Standard order sets Identify Redesign
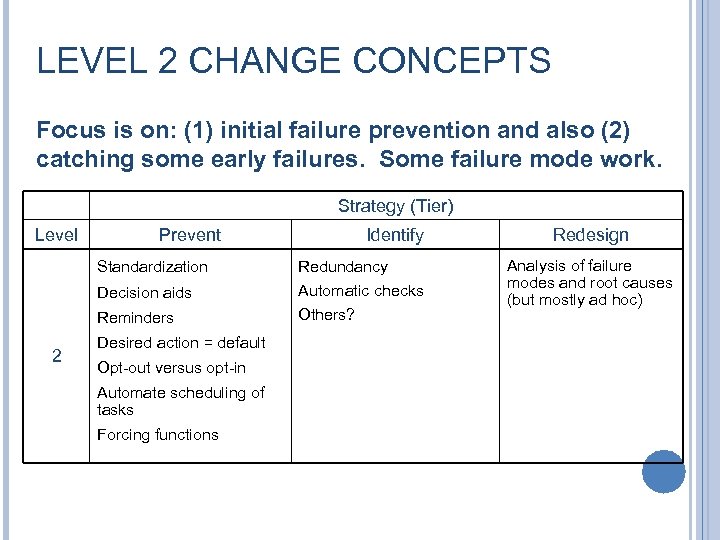
LEVEL 2 CHANGE CONCEPTS Focus is on: (1) initial failure prevention and also (2) catching some early failures. Some failure mode work. Strategy (Tier) Level Prevent Standardization Identify Decision aids Reminders 2 Redundancy Automatic checks Others? Desired action = default Opt-out versus opt-in Automate scheduling of tasks Forcing functions Redesign Analysis of failure modes and root causes (but mostly ad hoc)
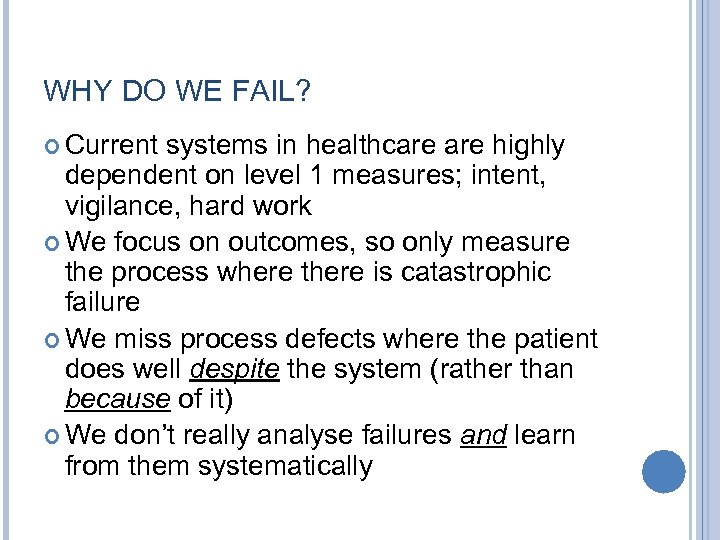
WHY DO WE FAIL? Current systems in healthcare highly dependent on level 1 measures; intent, vigilance, hard work We focus on outcomes, so only measure the process where there is catastrophic failure We miss process defects where the patient does well despite the system (rather than because of it) We don’t really analyse failures and learn from them systematically
CHAT BOX DISCUSSION Think about the last RCA or incident investigations in which you were involved List the outcomes/recommendations if you can remember them How confident are you that the incident won’t happen again
SO WHAT CAN I DO? • Go back to your last RCA. . or use a Safety Express topic • Look at a few examples of the process to identify; ØCrucial points where things go wrong ØSuggestions to improve reliability beyond the usual level 1 stuff
SUMMARY At best, most healthcare processes deliver level 1 reliability (i. e. around 90% success) Hard work, vigilence, training & audit is unlikely to make our systems more reliable than this Level 2 changes, which rely on a knowledge of human factors, can deliver up to 90 -99% success To get more reliable than this requires organisation-wide change (btw; there are no quick fixes or easy answers here!)
ACKNOWLEDGEMENTS AND REFERENCES Frank Federico & Carol Haraden, IHI white paper “Improving the reliability of healthcare” at www. ihi. org Nolan T “System change to improve patient safety” BMJ 2000; 320. 771 -3
6e645a1a798fe8cc44cc3db453afeccb.ppt