95be0a2cc0b7632bc9254ad31486d3e5.ppt
- Количество слайдов: 49
 QCOR 2010 Regionalizing Acute Stroke Care to Specialized Centers: Hype or Help? Lee H. Schwamm, MD Professor of Neurology, Harvard Medical School Director, Tele. Stroke & Acute Stroke Services, Massachusetts General Hospital Chair, National Steering Committee, AHA/ASA GWTG
QCOR 2010 Regionalizing Acute Stroke Care to Specialized Centers: Hype or Help? Lee H. Schwamm, MD Professor of Neurology, Harvard Medical School Director, Tele. Stroke & Acute Stroke Services, Massachusetts General Hospital Chair, National Steering Committee, AHA/ASA GWTG
 Disclosures l Federal l NIH l (IMS 3, MR RESCUE) Industry Clinical Trial Steering Committees l Lundbeck l (DIAS 4), Co. Axia (Flo 24) Other l Stroke Systems Consultant to MA DPH, CDC, TJC l Director Tele. Stroke Program at MGH
Disclosures l Federal l NIH l (IMS 3, MR RESCUE) Industry Clinical Trial Steering Committees l Lundbeck l (DIAS 4), Co. Axia (Flo 24) Other l Stroke Systems Consultant to MA DPH, CDC, TJC l Director Tele. Stroke Program at MGH
 Over my dead body! Phil, you and I both know the American public needs regionalization of acute stroke care
Over my dead body! Phil, you and I both know the American public needs regionalization of acute stroke care
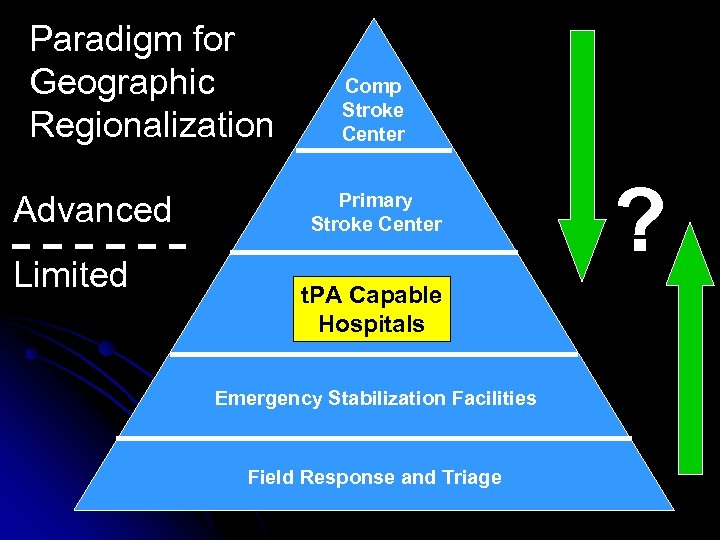 Paradigm for Geographic Regionalization Advanced Limited Comp Stroke Center Primary Stroke Center t. PA Capable Hospitals Emergency Stabilization Facilities Field Response and Triage ?
Paradigm for Geographic Regionalization Advanced Limited Comp Stroke Center Primary Stroke Center t. PA Capable Hospitals Emergency Stabilization Facilities Field Response and Triage ?
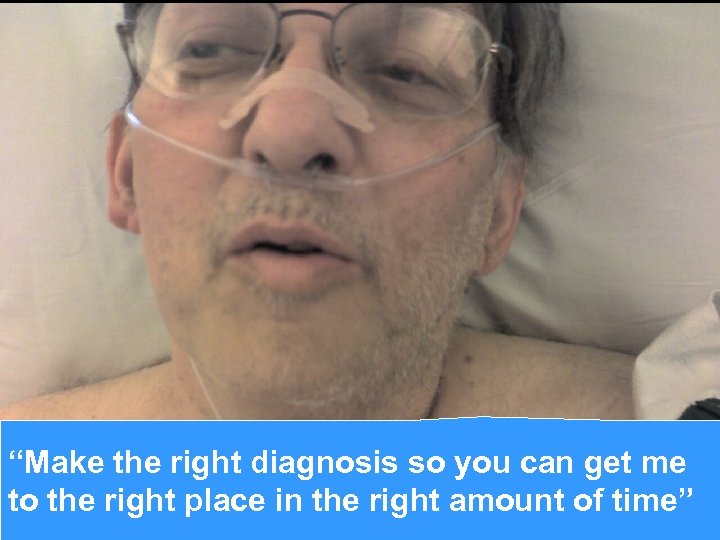 “Make the right diagnosis so you can get me to the right place in the right amount of time”
“Make the right diagnosis so you can get me to the right place in the right amount of time”
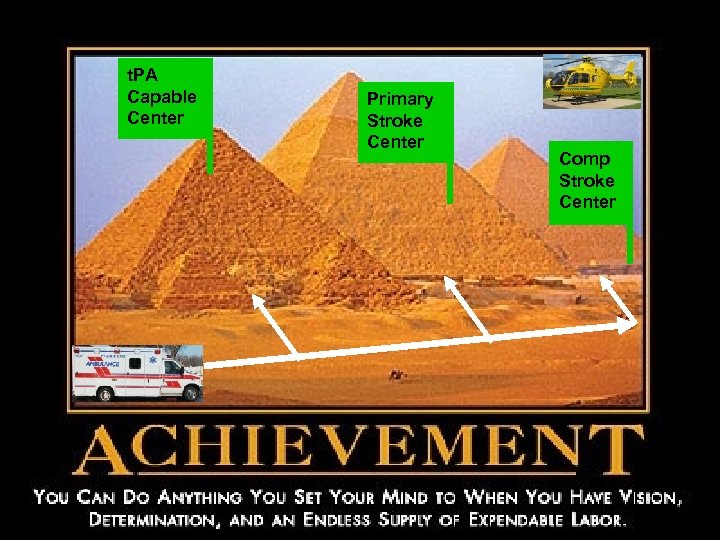 t. PA Capable Center Primary Stroke Center Comp Stroke Center
t. PA Capable Center Primary Stroke Center Comp Stroke Center
 Easy to get in Hard to get out
Easy to get in Hard to get out
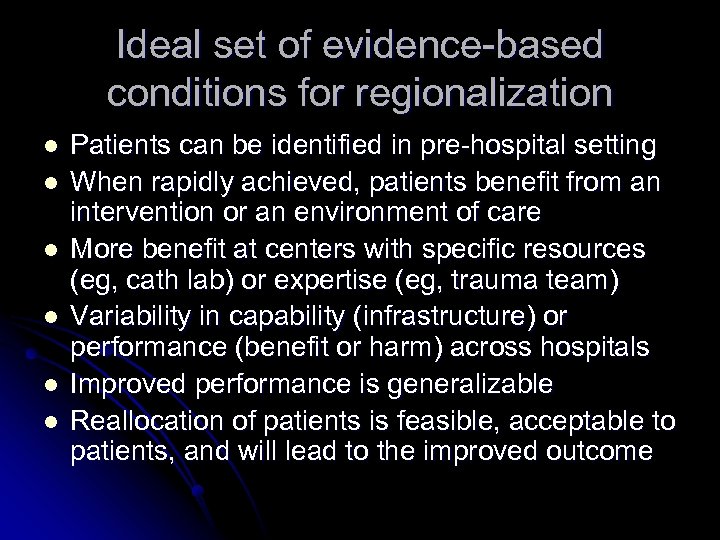 Ideal set of evidence-based conditions for regionalization l l l Patients can be identified in pre-hospital setting When rapidly achieved, patients benefit from an intervention or an environment of care More benefit at centers with specific resources (eg, cath lab) or expertise (eg, trauma team) Variability in capability (infrastructure) or performance (benefit or harm) across hospitals Improved performance is generalizable Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome
Ideal set of evidence-based conditions for regionalization l l l Patients can be identified in pre-hospital setting When rapidly achieved, patients benefit from an intervention or an environment of care More benefit at centers with specific resources (eg, cath lab) or expertise (eg, trauma team) Variability in capability (infrastructure) or performance (benefit or harm) across hospitals Improved performance is generalizable Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome
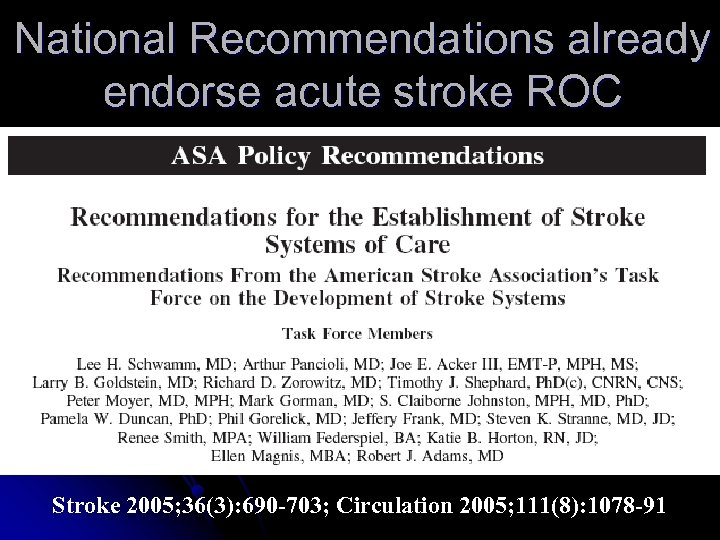 National Recommendations already endorse acute stroke ROC Stroke 2005; 36(3): 690 -703; Circulation 2005; 111(8): 1078 -91
National Recommendations already endorse acute stroke ROC Stroke 2005; 36(3): 690 -703; Circulation 2005; 111(8): 1078 -91
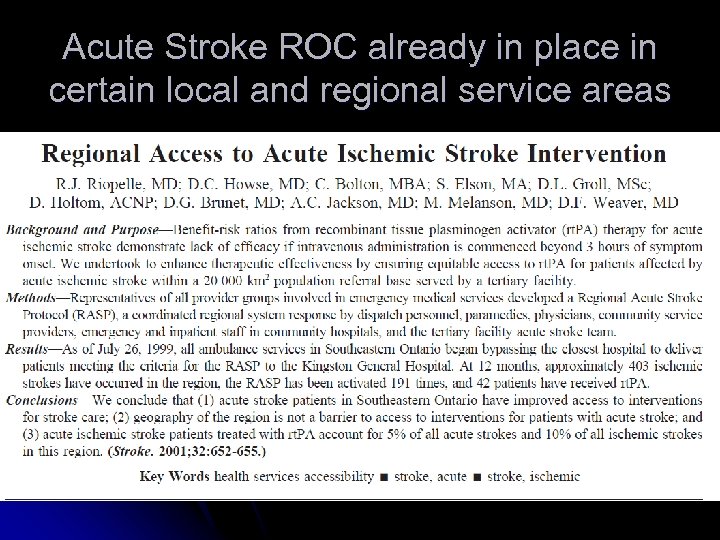 Acute Stroke ROC already in place in certain local and regional service areas
Acute Stroke ROC already in place in certain local and regional service areas
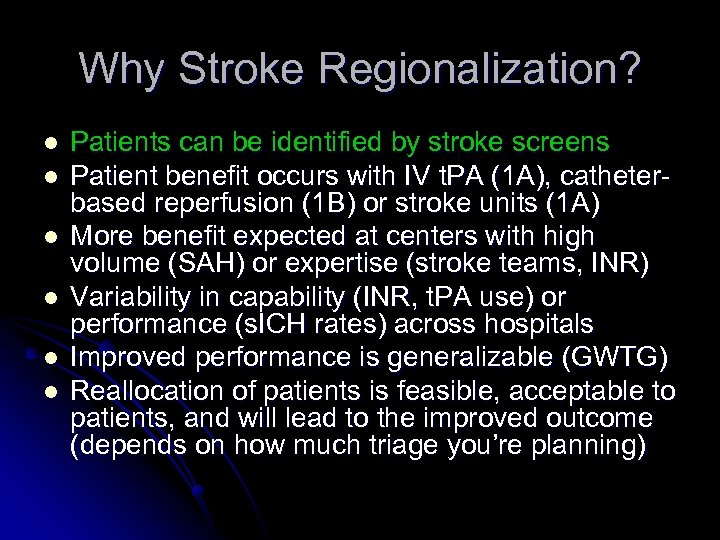 Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheterbased reperfusion (1 B) or stroke units (1 A) More benefit expected at centers with high volume (SAH) or expertise (stroke teams, INR) Variability in capability (INR, t. PA use) or performance (s. ICH rates) across hospitals Improved performance is generalizable (GWTG) Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome (depends on how much triage you’re planning)
Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheterbased reperfusion (1 B) or stroke units (1 A) More benefit expected at centers with high volume (SAH) or expertise (stroke teams, INR) Variability in capability (INR, t. PA use) or performance (s. ICH rates) across hospitals Improved performance is generalizable (GWTG) Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome (depends on how much triage you’re planning)
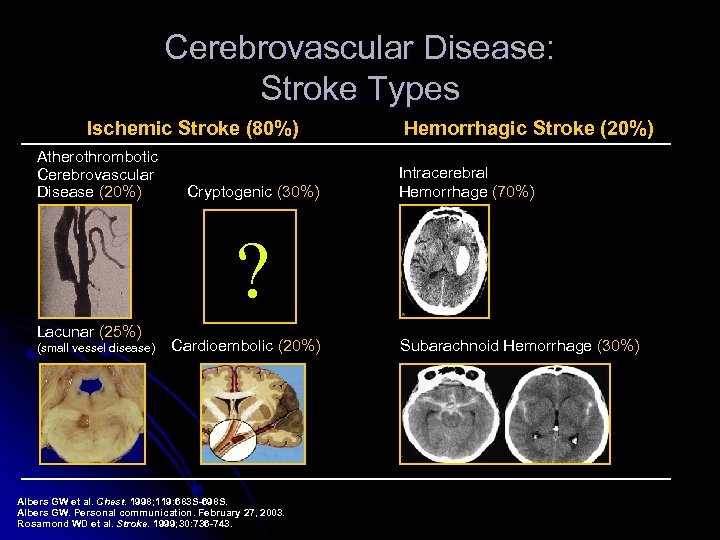 Cerebrovascular Disease: Stroke Types Ischemic Stroke (80%) Atherothrombotic Cerebrovascular Disease (20%) Cryptogenic (30%) Hemorrhagic Stroke (20%) Intracerebral Hemorrhage (70%) ? Lacunar (25%) (small vessel disease) Cardioembolic (20%) Albers GW et al. Chest. 1998; 119: 683 S-698 S. Albers GW. Personal communication. February 27, 2003. Rosamond WD et al. Stroke. 1999; 30: 736 -743. Subarachnoid Hemorrhage (30%)
Cerebrovascular Disease: Stroke Types Ischemic Stroke (80%) Atherothrombotic Cerebrovascular Disease (20%) Cryptogenic (30%) Hemorrhagic Stroke (20%) Intracerebral Hemorrhage (70%) ? Lacunar (25%) (small vessel disease) Cardioembolic (20%) Albers GW et al. Chest. 1998; 119: 683 S-698 S. Albers GW. Personal communication. February 27, 2003. Rosamond WD et al. Stroke. 1999; 30: 736 -743. Subarachnoid Hemorrhage (30%)
 Various public education and firstresponder screening tools
Various public education and firstresponder screening tools
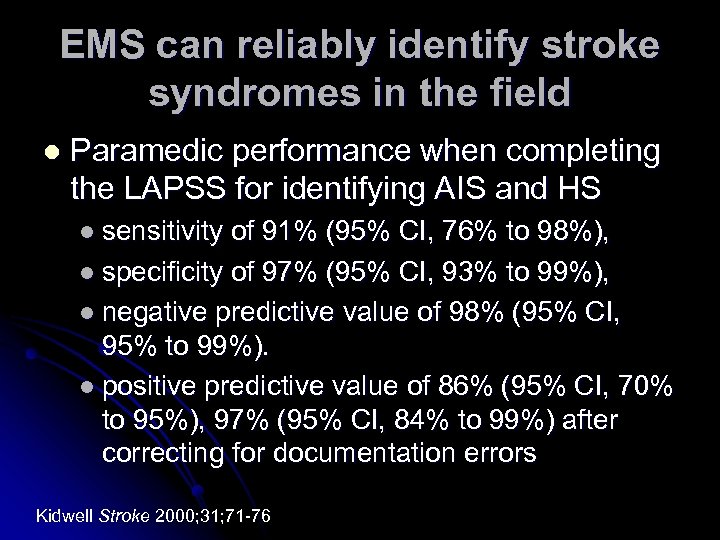 EMS can reliably identify stroke syndromes in the field l Paramedic performance when completing the LAPSS for identifying AIS and HS l sensitivity of 91% (95% CI, 76% to 98%), l specificity of 97% (95% CI, 93% to 99%), l negative predictive value of 98% (95% CI, 95% to 99%). l positive predictive value of 86% (95% CI, 70% to 95%), 97% (95% CI, 84% to 99%) after correcting for documentation errors Kidwell Stroke 2000; 31; 71 -76
EMS can reliably identify stroke syndromes in the field l Paramedic performance when completing the LAPSS for identifying AIS and HS l sensitivity of 91% (95% CI, 76% to 98%), l specificity of 97% (95% CI, 93% to 99%), l negative predictive value of 98% (95% CI, 95% to 99%). l positive predictive value of 86% (95% CI, 70% to 95%), 97% (95% CI, 84% to 99%) after correcting for documentation errors Kidwell Stroke 2000; 31; 71 -76
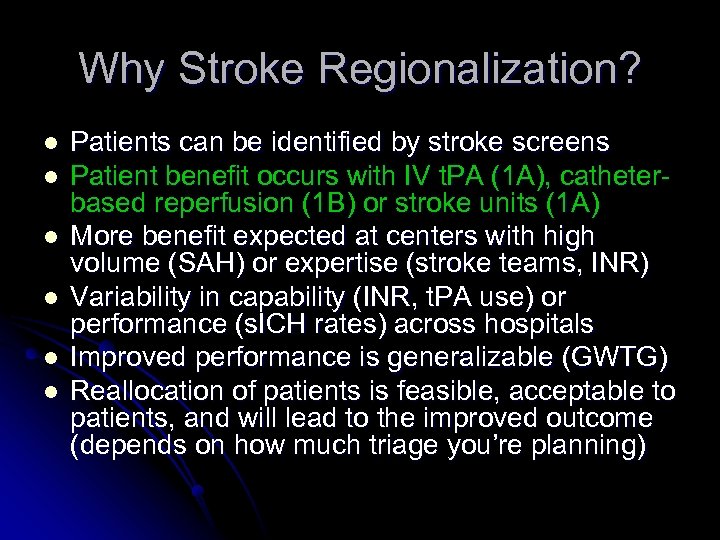 Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheterbased reperfusion (1 B) or stroke units (1 A) More benefit expected at centers with high volume (SAH) or expertise (stroke teams, INR) Variability in capability (INR, t. PA use) or performance (s. ICH rates) across hospitals Improved performance is generalizable (GWTG) Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome (depends on how much triage you’re planning)
Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheterbased reperfusion (1 B) or stroke units (1 A) More benefit expected at centers with high volume (SAH) or expertise (stroke teams, INR) Variability in capability (INR, t. PA use) or performance (s. ICH rates) across hospitals Improved performance is generalizable (GWTG) Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome (depends on how much triage you’re planning)
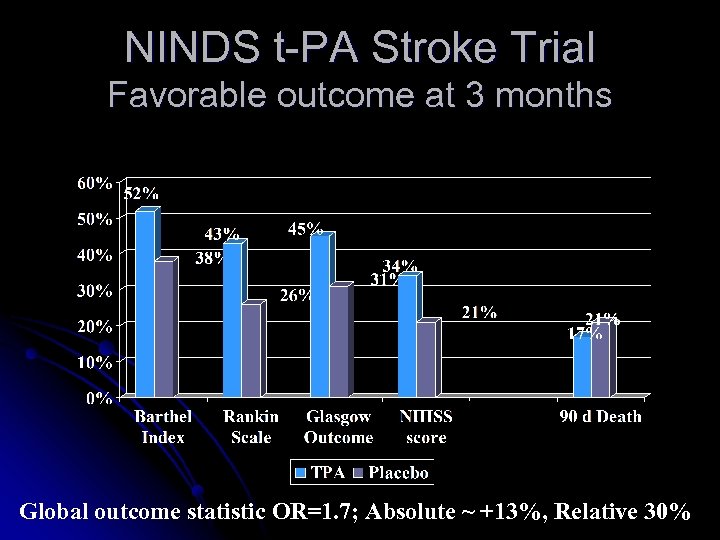 NINDS t-PA Stroke Trial Favorable outcome at 3 months Global outcome statistic OR=1. 7; Absolute ~ +13%, Relative 30%
NINDS t-PA Stroke Trial Favorable outcome at 3 months Global outcome statistic OR=1. 7; Absolute ~ +13%, Relative 30%
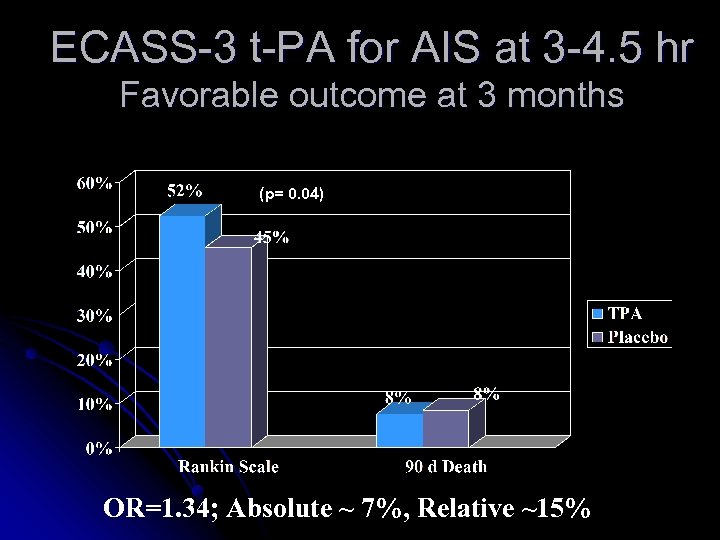 ECASS-3 t-PA for AIS at 3 -4. 5 hr Favorable outcome at 3 months (p= 0. 04) OR=1. 34; Absolute ~ 7%, Relative ~15%
ECASS-3 t-PA for AIS at 3 -4. 5 hr Favorable outcome at 3 months (p= 0. 04) OR=1. 34; Absolute ~ 7%, Relative ~15%
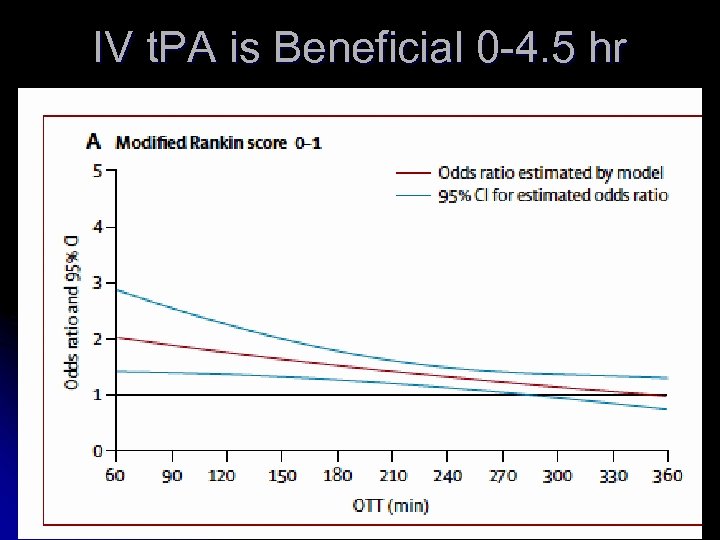 IV t. PA is Beneficial 0 -4. 5 hr
IV t. PA is Beneficial 0 -4. 5 hr
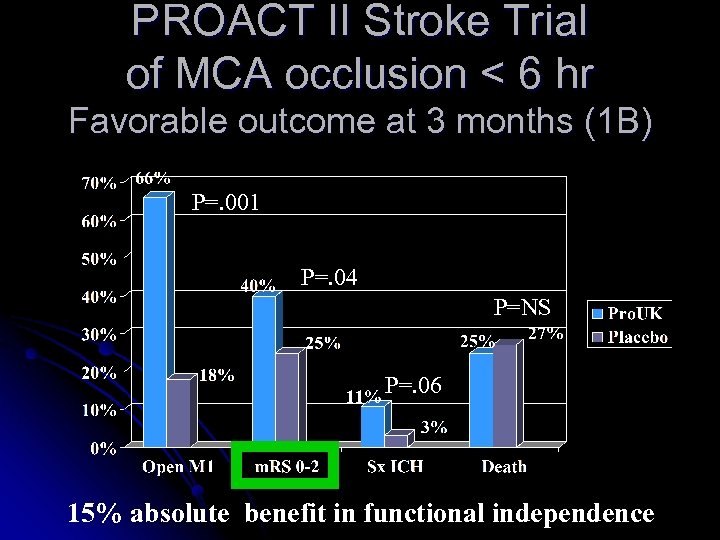 PROACT II Stroke Trial of MCA occlusion < 6 hr Favorable outcome at 3 months (1 B) P=. 001 P=. 04 P=NS P=. 06 15% absolute benefit in functional independence
PROACT II Stroke Trial of MCA occlusion < 6 hr Favorable outcome at 3 months (1 B) P=. 001 P=. 04 P=NS P=. 06 15% absolute benefit in functional independence
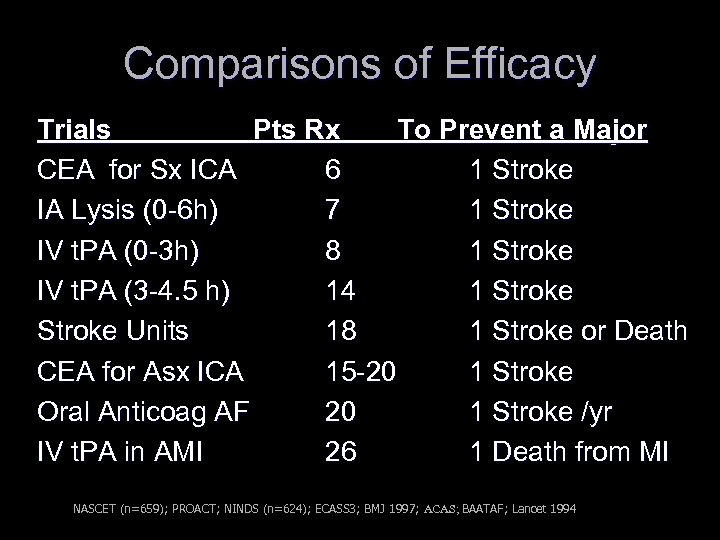 Comparisons of Efficacy Trials Pts Rx To Prevent a Major CEA for Sx ICA 6 1 Stroke IA Lysis (0 -6 h) 7 1 Stroke IV t. PA (0 -3 h) 8 1 Stroke IV t. PA (3 -4. 5 h) 14 1 Stroke Units 18 1 Stroke or Death CEA for Asx ICA 15 -20 1 Stroke Oral Anticoag AF 20 1 Stroke /yr IV t. PA in AMI 26 1 Death from MI NASCET (n=659); PROACT; NINDS (n=624); ECASS 3; BMJ 1997; ACAS; BAATAF; Lancet 1994
Comparisons of Efficacy Trials Pts Rx To Prevent a Major CEA for Sx ICA 6 1 Stroke IA Lysis (0 -6 h) 7 1 Stroke IV t. PA (0 -3 h) 8 1 Stroke IV t. PA (3 -4. 5 h) 14 1 Stroke Units 18 1 Stroke or Death CEA for Asx ICA 15 -20 1 Stroke Oral Anticoag AF 20 1 Stroke /yr IV t. PA in AMI 26 1 Death from MI NASCET (n=659); PROACT; NINDS (n=624); ECASS 3; BMJ 1997; ACAS; BAATAF; Lancet 1994
 Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheter-based reperfusion (1 B) or stroke units (1 A) More benefit expected w/ operators (CEA) or centers with high volume (SAH) or expertise (stroke teams, INR) Variability in capability (INR, t. PA use) or performance (s. ICH rates) across hospitals Improved performance is generalizable (GWTG) Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome (depends on how much triage you’re planning)
Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheter-based reperfusion (1 B) or stroke units (1 A) More benefit expected w/ operators (CEA) or centers with high volume (SAH) or expertise (stroke teams, INR) Variability in capability (INR, t. PA use) or performance (s. ICH rates) across hospitals Improved performance is generalizable (GWTG) Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome (depends on how much triage you’re planning)
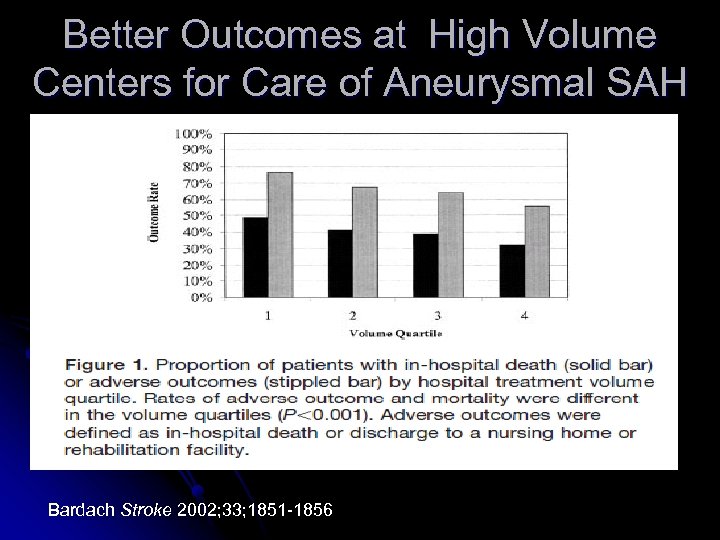 Better Outcomes at High Volume Centers for Care of Aneurysmal SAH Bardach Stroke 2002; 33; 1851 -1856
Better Outcomes at High Volume Centers for Care of Aneurysmal SAH Bardach Stroke 2002; 33; 1851 -1856
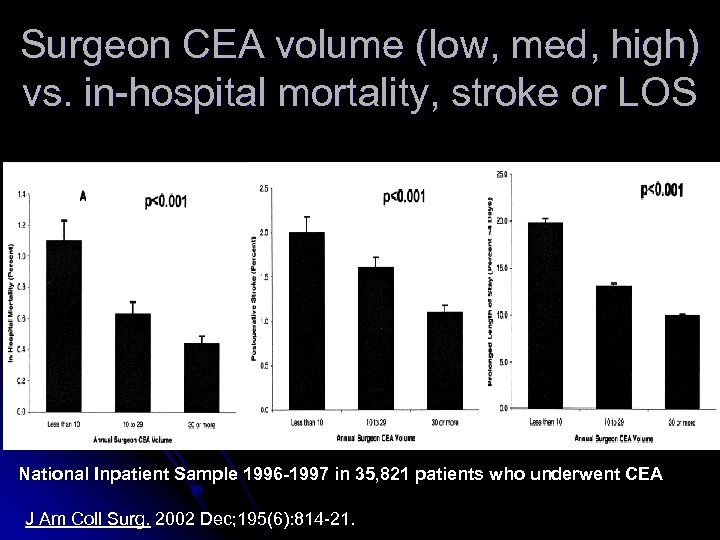 Surgeon CEA volume (low, med, high) vs. in-hospital mortality, stroke or LOS National Inpatient Sample 1996 -1997 in 35, 821 patients who underwent CEA J Am Coll Surg. 2002 Dec; 195(6): 814 -21.
Surgeon CEA volume (low, med, high) vs. in-hospital mortality, stroke or LOS National Inpatient Sample 1996 -1997 in 35, 821 patients who underwent CEA J Am Coll Surg. 2002 Dec; 195(6): 814 -21.
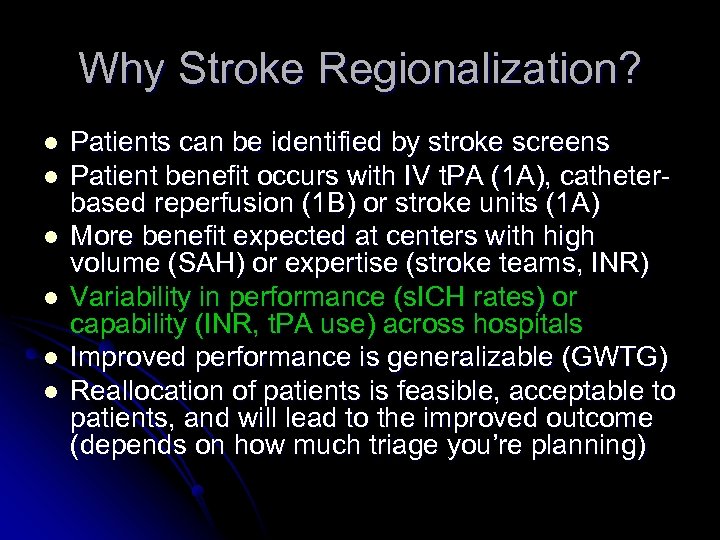 Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheterbased reperfusion (1 B) or stroke units (1 A) More benefit expected at centers with high volume (SAH) or expertise (stroke teams, INR) Variability in performance (s. ICH rates) or capability (INR, t. PA use) across hospitals Improved performance is generalizable (GWTG) Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome (depends on how much triage you’re planning)
Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheterbased reperfusion (1 B) or stroke units (1 A) More benefit expected at centers with high volume (SAH) or expertise (stroke teams, INR) Variability in performance (s. ICH rates) or capability (INR, t. PA use) across hospitals Improved performance is generalizable (GWTG) Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome (depends on how much triage you’re planning)
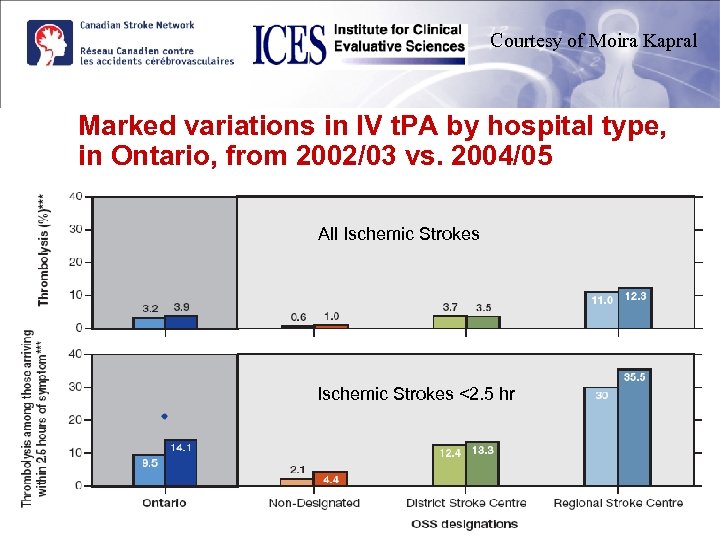 Courtesy of Moira Kapral Marked variations in IV t. PA by hospital type, in Ontario, from 2002/03 vs. 2004/05 All Ischemic Strokes <2. 5 hr
Courtesy of Moira Kapral Marked variations in IV t. PA by hospital type, in Ontario, from 2002/03 vs. 2004/05 All Ischemic Strokes <2. 5 hr
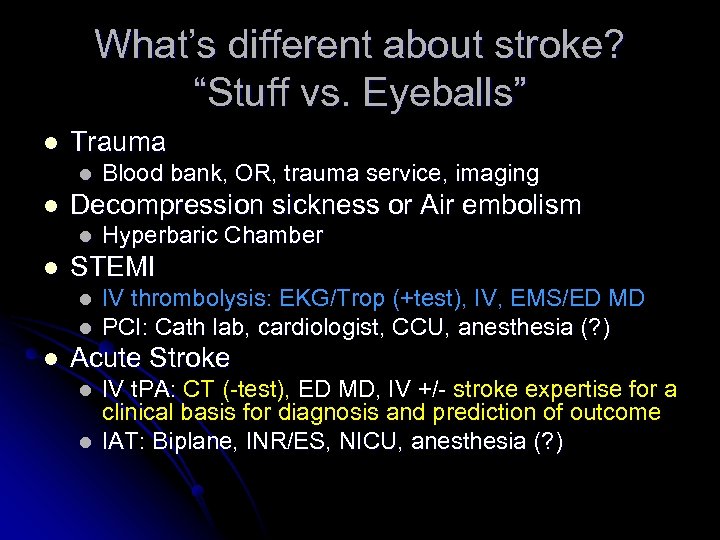 What’s different about stroke? “Stuff vs. Eyeballs” l Trauma l l Decompression sickness or Air embolism l l Hyperbaric Chamber STEMI l l l Blood bank, OR, trauma service, imaging IV thrombolysis: EKG/Trop (+test), IV, EMS/ED MD PCI: Cath lab, cardiologist, CCU, anesthesia (? ) Acute Stroke l l IV t. PA: CT (-test), ED MD, IV +/- stroke expertise for a clinical basis for diagnosis and prediction of outcome IAT: Biplane, INR/ES, NICU, anesthesia (? )
What’s different about stroke? “Stuff vs. Eyeballs” l Trauma l l Decompression sickness or Air embolism l l Hyperbaric Chamber STEMI l l l Blood bank, OR, trauma service, imaging IV thrombolysis: EKG/Trop (+test), IV, EMS/ED MD PCI: Cath lab, cardiologist, CCU, anesthesia (? ) Acute Stroke l l IV t. PA: CT (-test), ED MD, IV +/- stroke expertise for a clinical basis for diagnosis and prediction of outcome IAT: Biplane, INR/ES, NICU, anesthesia (? )
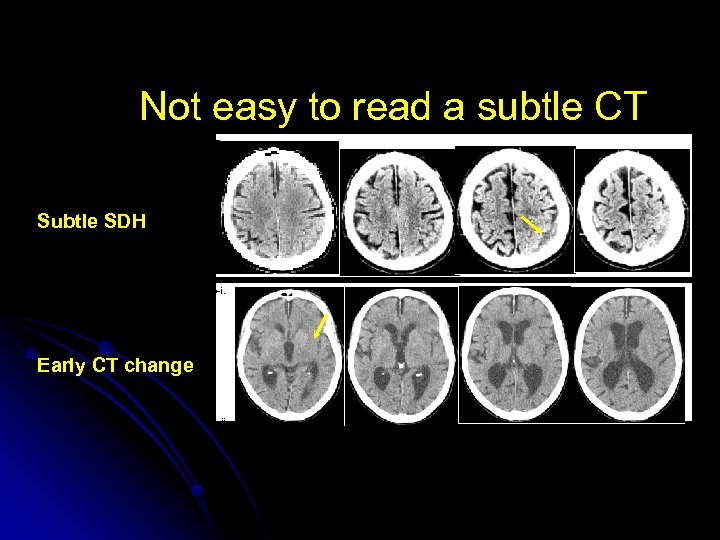 Not easy to read a subtle CT a. Subtle SDH b-i. Early CT change b-ii.
Not easy to read a subtle CT a. Subtle SDH b-i. Early CT change b-ii.
 The impact of external forces on provider tolerance for medical uncertainty at the bedside
The impact of external forces on provider tolerance for medical uncertainty at the bedside
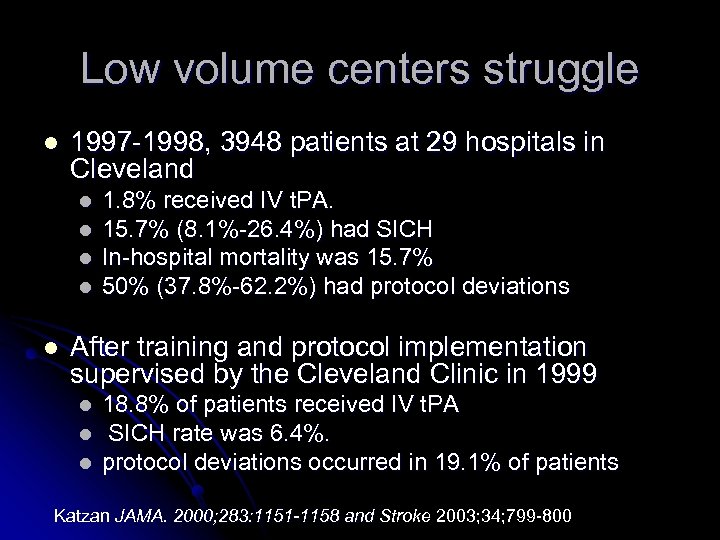 Low volume centers struggle l 1997 -1998, 3948 patients at 29 hospitals in Cleveland l l l 1. 8% received IV t. PA. 15. 7% (8. 1%-26. 4%) had SICH In-hospital mortality was 15. 7% 50% (37. 8%-62. 2%) had protocol deviations After training and protocol implementation supervised by the Cleveland Clinic in 1999 l l l 18. 8% of patients received IV t. PA SICH rate was 6. 4%. protocol deviations occurred in 19. 1% of patients Katzan JAMA. 2000; 283: 1151 -1158 and Stroke 2003; 34; 799 -800
Low volume centers struggle l 1997 -1998, 3948 patients at 29 hospitals in Cleveland l l l 1. 8% received IV t. PA. 15. 7% (8. 1%-26. 4%) had SICH In-hospital mortality was 15. 7% 50% (37. 8%-62. 2%) had protocol deviations After training and protocol implementation supervised by the Cleveland Clinic in 1999 l l l 18. 8% of patients received IV t. PA SICH rate was 6. 4%. protocol deviations occurred in 19. 1% of patients Katzan JAMA. 2000; 283: 1151 -1158 and Stroke 2003; 34; 799 -800
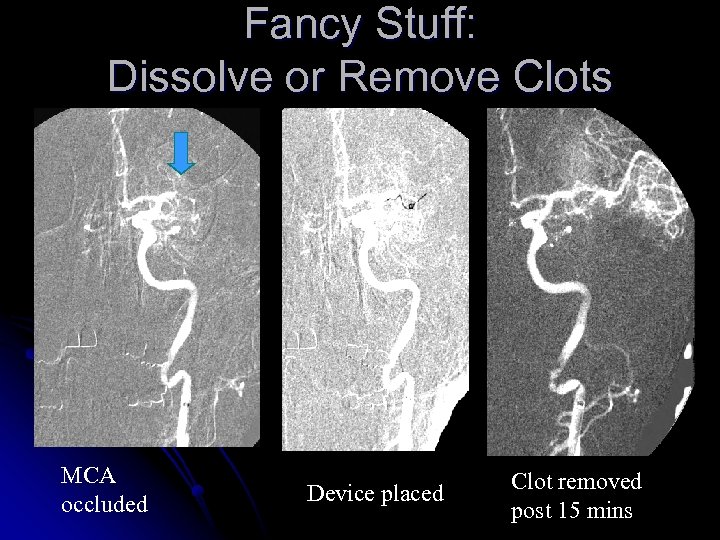 Fancy Stuff: Dissolve or Remove Clots MCA occluded Device placed Clot removed post 15 mins
Fancy Stuff: Dissolve or Remove Clots MCA occluded Device placed Clot removed post 15 mins
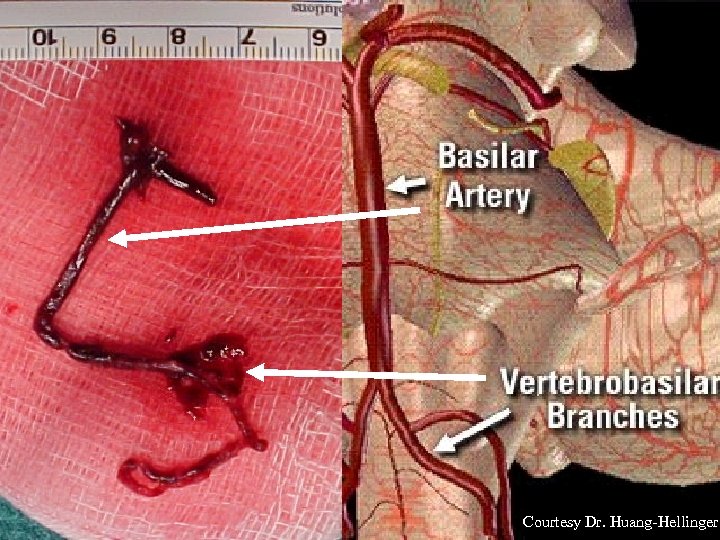 Courtesy Dr. Huang-Hellinger
Courtesy Dr. Huang-Hellinger
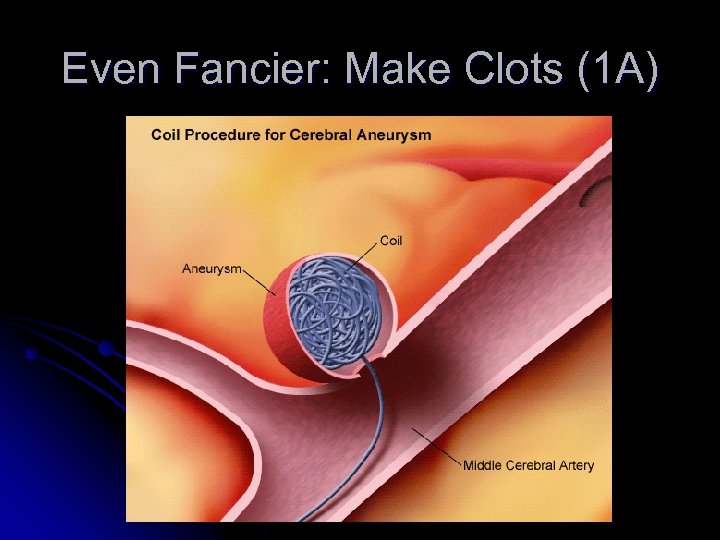 Even Fancier: Make Clots (1 A)
Even Fancier: Make Clots (1 A)
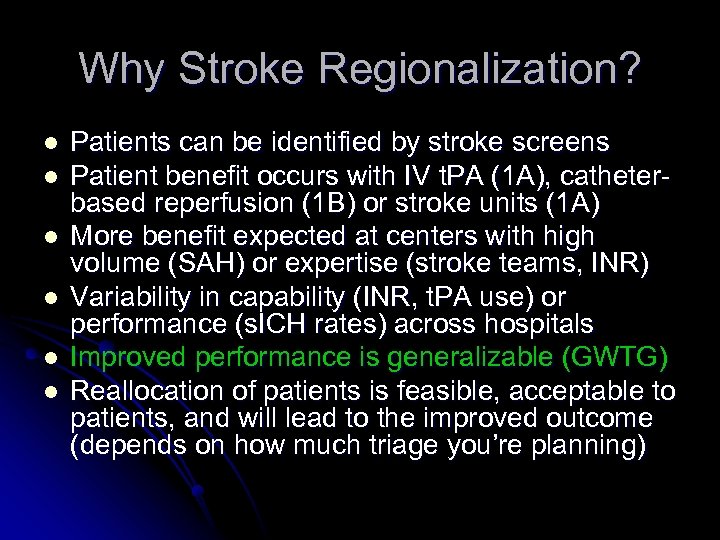 Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheterbased reperfusion (1 B) or stroke units (1 A) More benefit expected at centers with high volume (SAH) or expertise (stroke teams, INR) Variability in capability (INR, t. PA use) or performance (s. ICH rates) across hospitals Improved performance is generalizable (GWTG) Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome (depends on how much triage you’re planning)
Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheterbased reperfusion (1 B) or stroke units (1 A) More benefit expected at centers with high volume (SAH) or expertise (stroke teams, INR) Variability in capability (INR, t. PA use) or performance (s. ICH rates) across hospitals Improved performance is generalizable (GWTG) Reallocation of patients is feasible, acceptable to patients, and will lead to the improved outcome (depends on how much triage you’re planning)
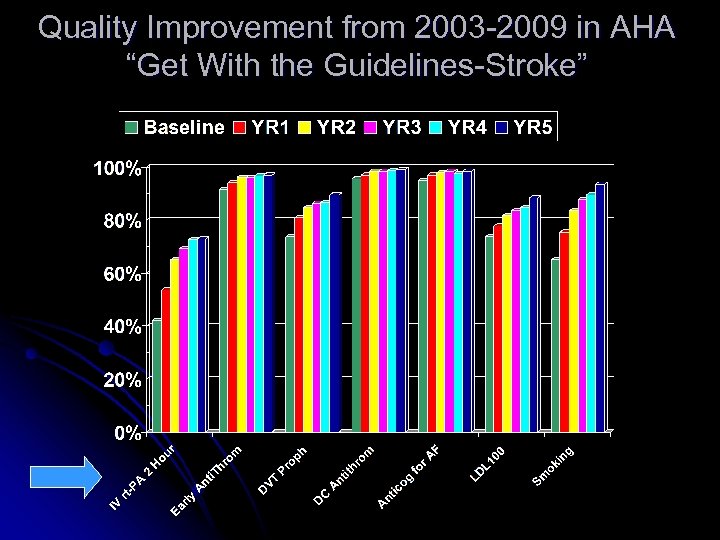 Quality Improvement from 2003 -2009 in AHA “Get With the Guidelines-Stroke”
Quality Improvement from 2003 -2009 in AHA “Get With the Guidelines-Stroke”
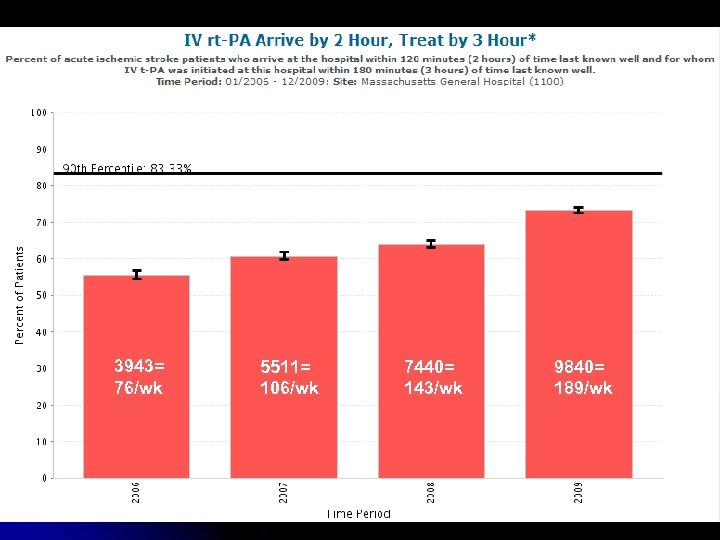 3943= 76/wk 5511= 106/wk 7440= 143/wk 9840= 189/wk
3943= 76/wk 5511= 106/wk 7440= 143/wk 9840= 189/wk
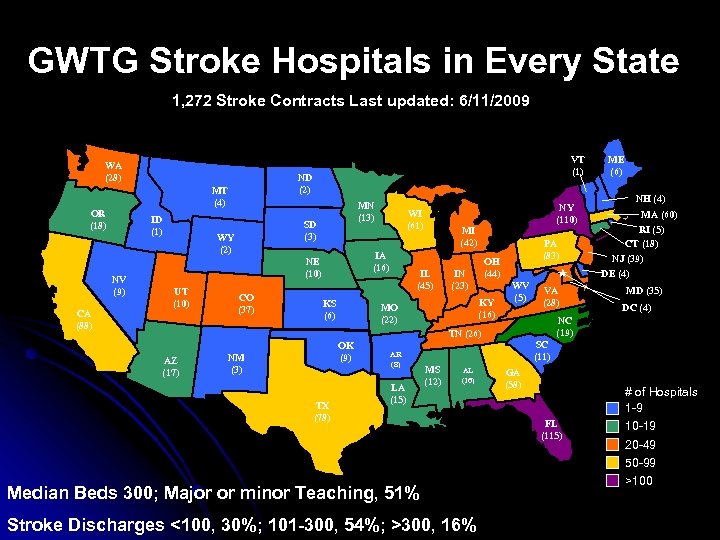 GWTG Stroke Hospitals in Every State 1, 272 Stroke Contracts Last updated: 6/11/2009 WA (28) ID (1) NV (9) CA (88) ND (2) MT (4) OR (18) VT (1) MN (13) SD (3) WY (2) IA (16) NE (10) UT (10) CO (37) WI (61) KS (6) NY (110) MI (42) IL (45) OH (44) IN (23) KY (16) MO (22) PA (83) OK (9) NM (3) TX (78) AR (8) LA (15) MS (12) AL (16) Median Beds 300; Major or minor Teaching, 51% Stroke Discharges <100, 30%; 101 -300, 54%; >300, 16% NH (4) MA (60) RI (5) CT (18) NJ (39) DE (4) WV (5) VA (28) MD (35) DC (4) NC (19) TN (26) AZ (17) ME (6) SC (11) GA (58) FL (115) # of Hospitals 1 -9 10 -19 20 -49 50 -99 >100
GWTG Stroke Hospitals in Every State 1, 272 Stroke Contracts Last updated: 6/11/2009 WA (28) ID (1) NV (9) CA (88) ND (2) MT (4) OR (18) VT (1) MN (13) SD (3) WY (2) IA (16) NE (10) UT (10) CO (37) WI (61) KS (6) NY (110) MI (42) IL (45) OH (44) IN (23) KY (16) MO (22) PA (83) OK (9) NM (3) TX (78) AR (8) LA (15) MS (12) AL (16) Median Beds 300; Major or minor Teaching, 51% Stroke Discharges <100, 30%; 101 -300, 54%; >300, 16% NH (4) MA (60) RI (5) CT (18) NJ (39) DE (4) WV (5) VA (28) MD (35) DC (4) NC (19) TN (26) AZ (17) ME (6) SC (11) GA (58) FL (115) # of Hospitals 1 -9 10 -19 20 -49 50 -99 >100
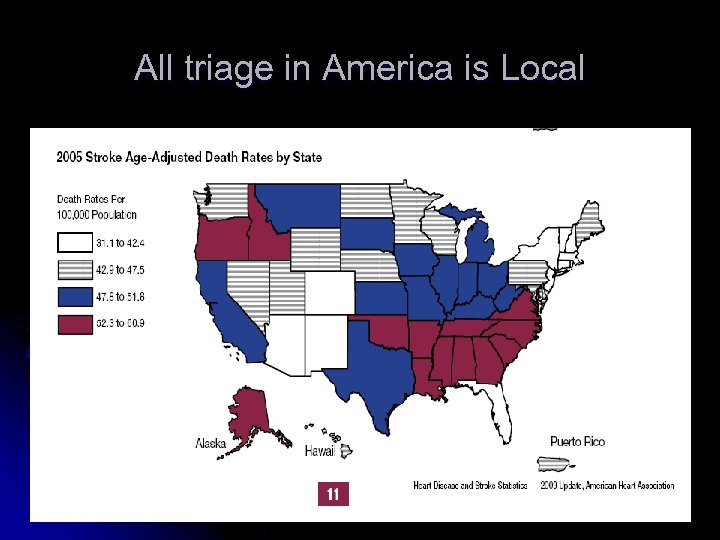 All triage in America is Local
All triage in America is Local
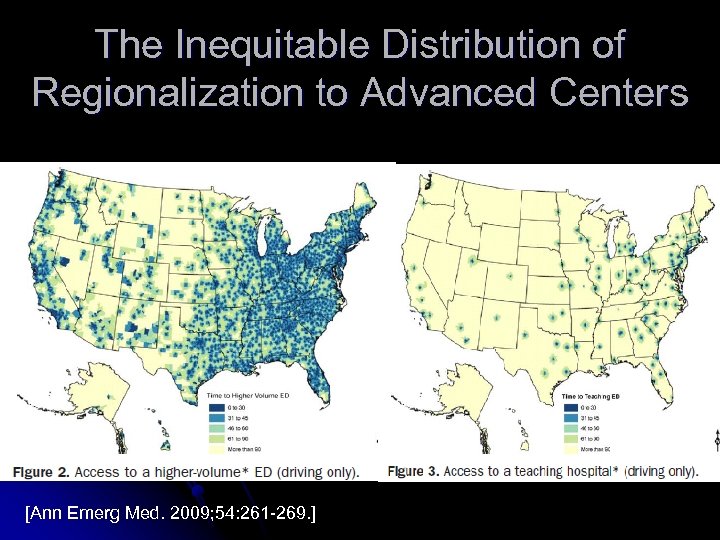 The Inequitable Distribution of Regionalization to Advanced Centers [Ann Emerg Med. 2009; 54: 261 -269. ]
The Inequitable Distribution of Regionalization to Advanced Centers [Ann Emerg Med. 2009; 54: 261 -269. ]
 Time lost in transit is brain lost in transit
Time lost in transit is brain lost in transit
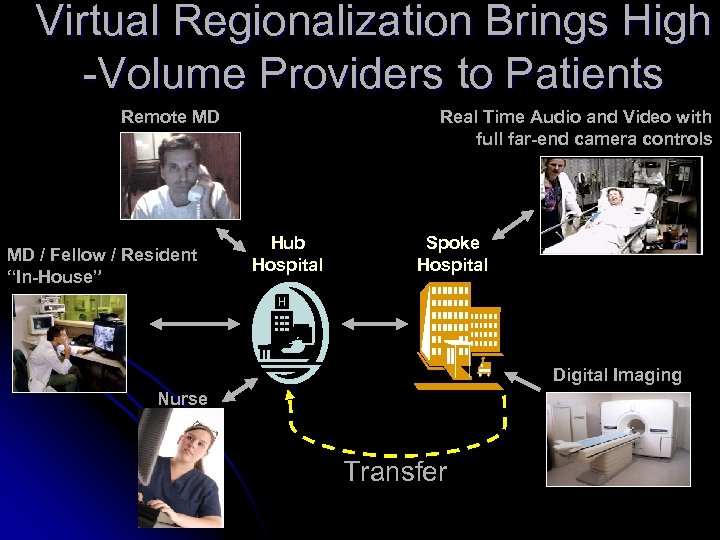 Virtual Regionalization Brings High -Volume Providers to Patients Remote MD MD / Fellow / Resident “In-House” Real Time Audio and Video with full far-end camera controls Hub Hospital Spoke Hospital Digital Imaging Nurse Transfer
Virtual Regionalization Brings High -Volume Providers to Patients Remote MD MD / Fellow / Resident “In-House” Real Time Audio and Video with full far-end camera controls Hub Hospital Spoke Hospital Digital Imaging Nurse Transfer
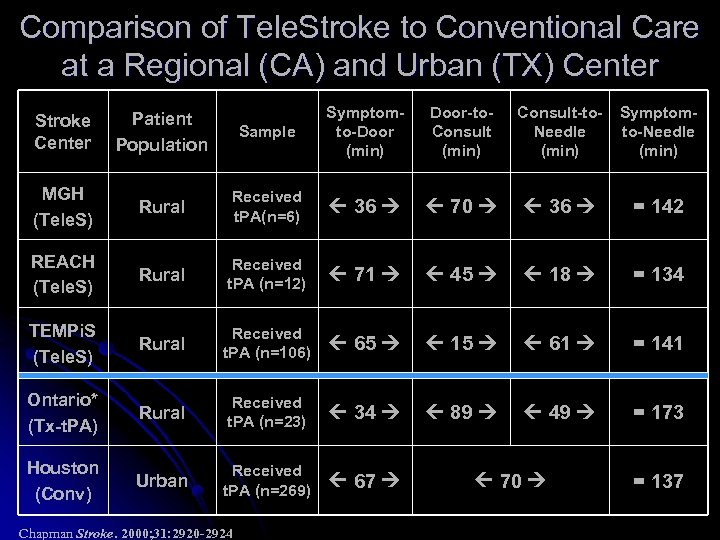 Comparison of Tele. Stroke to Conventional Care at a Regional (CA) and Urban (TX) Center Sample Symptomto-Door (min) Door-to. Consult (min) Consult-to. Needle (min) Symptomto-Needle (min) Rural Received t. PA(n=6) 36 70 36 = 142 REACH (Tele. S) Rural Received t. PA (n=12) 71 45 18 = 134 TEMPi. S (Tele. S) Rural Received t. PA (n=106) 65 15 61 = 141 Ontario* (Tx-t. PA) Rural Received t. PA (n=23) 34 89 49 = 173 Houston (Conv) Urban Received t. PA (n=269) 67 Stroke Center Patient Population MGH (Tele. S) Chapman Stroke. 2000; 31: 2920 -2924 70 = 137
Comparison of Tele. Stroke to Conventional Care at a Regional (CA) and Urban (TX) Center Sample Symptomto-Door (min) Door-to. Consult (min) Consult-to. Needle (min) Symptomto-Needle (min) Rural Received t. PA(n=6) 36 70 36 = 142 REACH (Tele. S) Rural Received t. PA (n=12) 71 45 18 = 134 TEMPi. S (Tele. S) Rural Received t. PA (n=106) 65 15 61 = 141 Ontario* (Tx-t. PA) Rural Received t. PA (n=23) 34 89 49 = 173 Houston (Conv) Urban Received t. PA (n=269) 67 Stroke Center Patient Population MGH (Tele. S) Chapman Stroke. 2000; 31: 2920 -2924 70 = 137
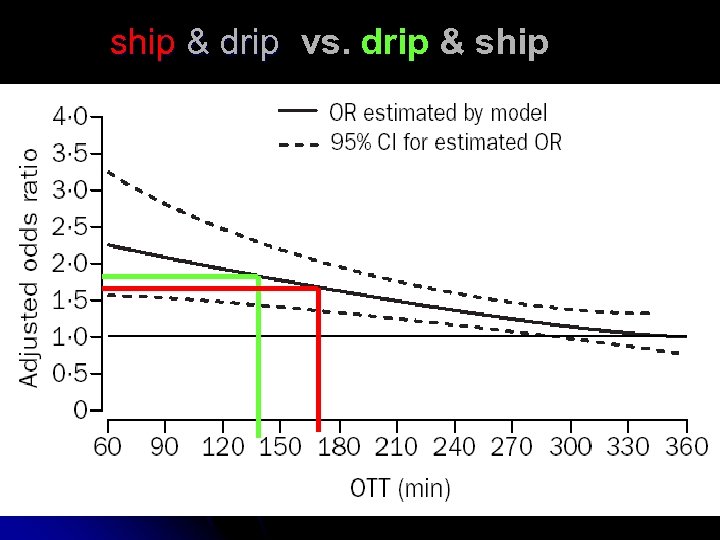 ship & drip vs. drip & ship
ship & drip vs. drip & ship
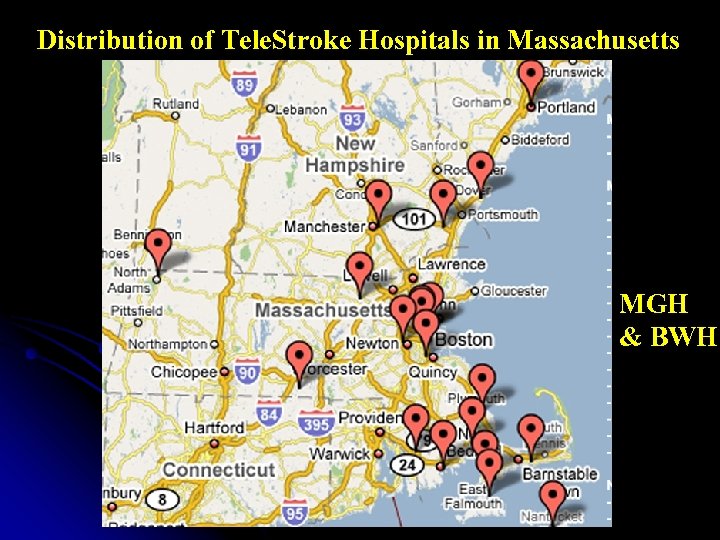 Distribution of Tele. Stroke Hospitals in Massachusetts MGH & BWH 21 hospitals in Network 6 hospitals Considering ---------------66 t. PA-Capable Centers
Distribution of Tele. Stroke Hospitals in Massachusetts MGH & BWH 21 hospitals in Network 6 hospitals Considering ---------------66 t. PA-Capable Centers
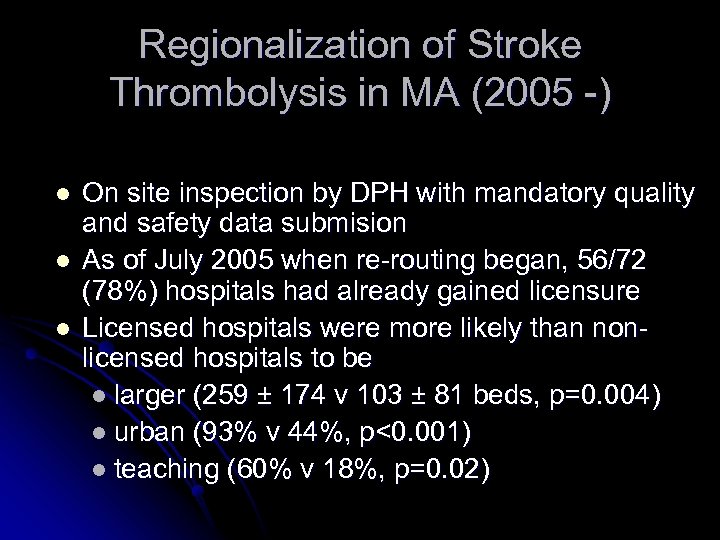 Regionalization of Stroke Thrombolysis in MA (2005 -) l l l On site inspection by DPH with mandatory quality and safety data submision As of July 2005 when re-routing began, 56/72 (78%) hospitals had already gained licensure Licensed hospitals were more likely than nonlicensed hospitals to be l larger (259 ± 174 v 103 ± 81 beds, p=0. 004) l urban (93% v 44%, p<0. 001) l teaching (60% v 18%, p=0. 02)
Regionalization of Stroke Thrombolysis in MA (2005 -) l l l On site inspection by DPH with mandatory quality and safety data submision As of July 2005 when re-routing began, 56/72 (78%) hospitals had already gained licensure Licensed hospitals were more likely than nonlicensed hospitals to be l larger (259 ± 174 v 103 ± 81 beds, p=0. 004) l urban (93% v 44%, p<0. 001) l teaching (60% v 18%, p=0. 02)
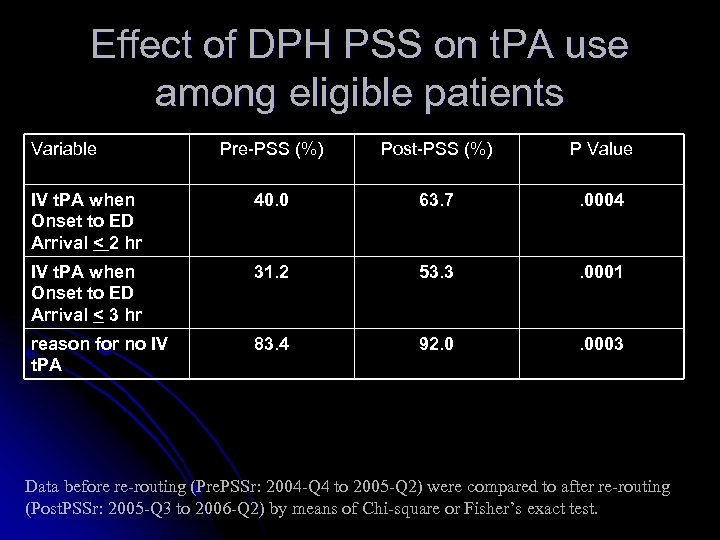 Effect of DPH PSS on t. PA use among eligible patients Variable Pre-PSS (%) Post-PSS (%) P Value IV t. PA when Onset to ED Arrival < 2 hr 40. 0 63. 7 . 0004 IV t. PA when Onset to ED Arrival < 3 hr 31. 2 53. 3 . 0001 reason for no IV t. PA 83. 4 92. 0 . 0003 Data before re-routing (Pre. PSSr: 2004 -Q 4 to 2005 -Q 2) were compared to after re-routing (Post. PSSr: 2005 -Q 3 to 2006 -Q 2) by means of Chi-square or Fisher’s exact test.
Effect of DPH PSS on t. PA use among eligible patients Variable Pre-PSS (%) Post-PSS (%) P Value IV t. PA when Onset to ED Arrival < 2 hr 40. 0 63. 7 . 0004 IV t. PA when Onset to ED Arrival < 3 hr 31. 2 53. 3 . 0001 reason for no IV t. PA 83. 4 92. 0 . 0003 Data before re-routing (Pre. PSSr: 2004 -Q 4 to 2005 -Q 2) were compared to after re-routing (Post. PSSr: 2005 -Q 3 to 2006 -Q 2) by means of Chi-square or Fisher’s exact test.
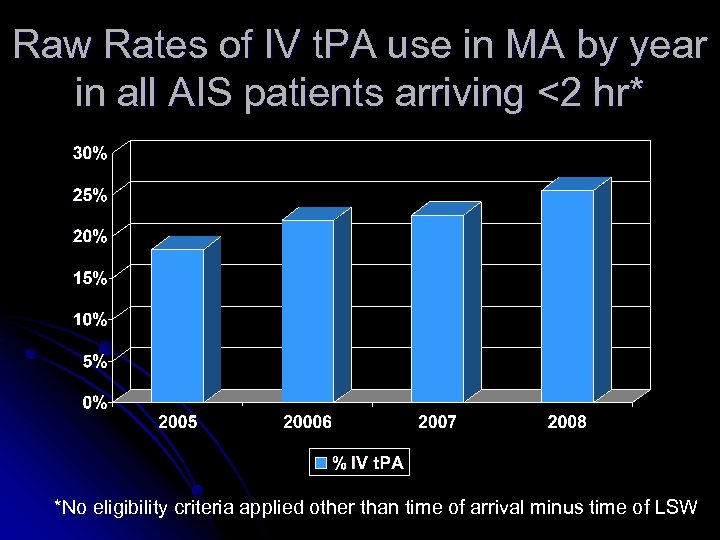 Raw Rates of IV t. PA use in MA by year in all AIS patients arriving <2 hr* *No eligibility criteria applied other than time of arrival minus time of LSW
Raw Rates of IV t. PA use in MA by year in all AIS patients arriving <2 hr* *No eligibility criteria applied other than time of arrival minus time of LSW
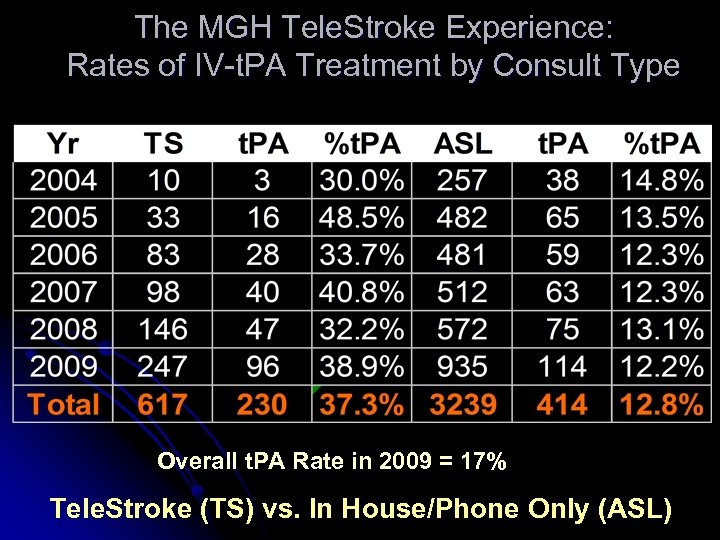 The MGH Tele. Stroke Experience: Rates of IV-t. PA Treatment by Consult Type Overall t. PA Rate in 2009 = 17% Tele. Stroke (TS) vs. In House/Phone Only (ASL)
The MGH Tele. Stroke Experience: Rates of IV-t. PA Treatment by Consult Type Overall t. PA Rate in 2009 = 17% Tele. Stroke (TS) vs. In House/Phone Only (ASL)
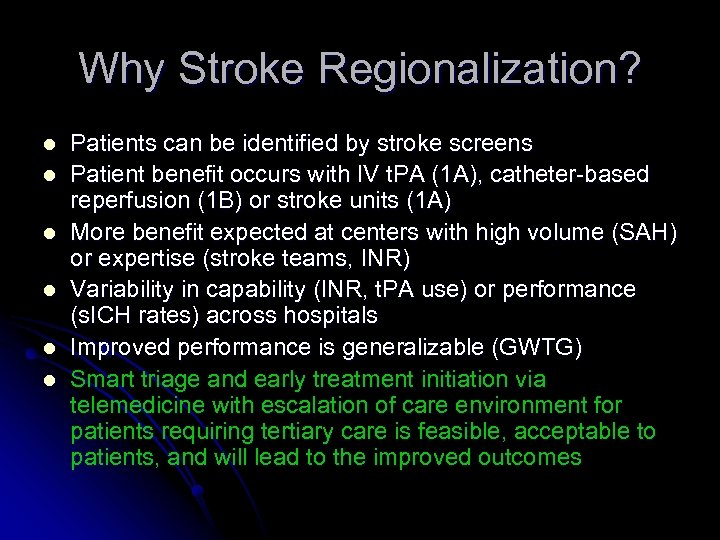 Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheter-based reperfusion (1 B) or stroke units (1 A) More benefit expected at centers with high volume (SAH) or expertise (stroke teams, INR) Variability in capability (INR, t. PA use) or performance (s. ICH rates) across hospitals Improved performance is generalizable (GWTG) Smart triage and early treatment initiation via telemedicine with escalation of care environment for patients requiring tertiary care is feasible, acceptable to patients, and will lead to the improved outcomes
Why Stroke Regionalization? l l l Patients can be identified by stroke screens Patient benefit occurs with IV t. PA (1 A), catheter-based reperfusion (1 B) or stroke units (1 A) More benefit expected at centers with high volume (SAH) or expertise (stroke teams, INR) Variability in capability (INR, t. PA use) or performance (s. ICH rates) across hospitals Improved performance is generalizable (GWTG) Smart triage and early treatment initiation via telemedicine with escalation of care environment for patients requiring tertiary care is feasible, acceptable to patients, and will lead to the improved outcomes
 World Leaders Embrace Acute Stroke Care Regionalization. Middle East Declares Lasting Peace Tea Party Suffers Stunning Nov. Losses
World Leaders Embrace Acute Stroke Care Regionalization. Middle East Declares Lasting Peace Tea Party Suffers Stunning Nov. Losses


