36acdbc7b15daceb074592ee00d3bcad.ppt
- Количество слайдов: 33
 Pyramidal (Voluntary Motor) System Dr. G. R. Leichnetz
Pyramidal (Voluntary Motor) System Dr. G. R. Leichnetz
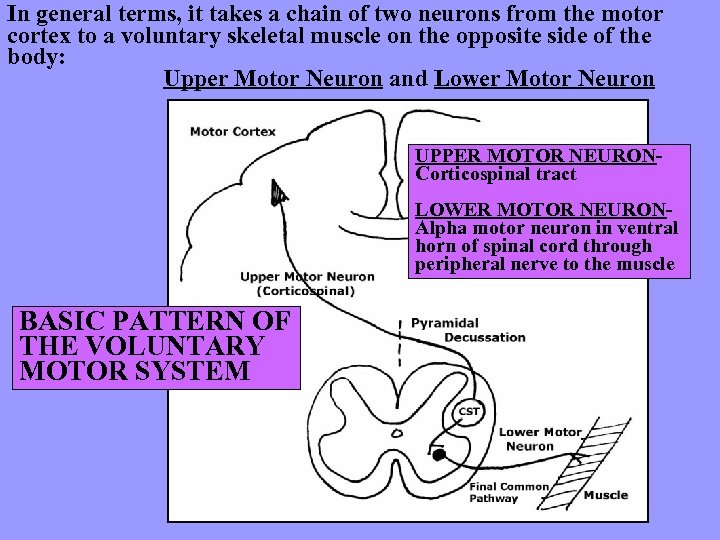 In general terms, it takes a chain of two neurons from the motor cortex to a voluntary skeletal muscle on the opposite side of the body: Upper Motor Neuron and Lower Motor Neuron UPPER MOTOR NEURONCorticospinal tract LOWER MOTOR NEURONAlpha motor neuron in ventral horn of spinal cord through peripheral nerve to the muscle BASIC PATTERN OF THE VOLUNTARY MOTOR SYSTEM
In general terms, it takes a chain of two neurons from the motor cortex to a voluntary skeletal muscle on the opposite side of the body: Upper Motor Neuron and Lower Motor Neuron UPPER MOTOR NEURONCorticospinal tract LOWER MOTOR NEURONAlpha motor neuron in ventral horn of spinal cord through peripheral nerve to the muscle BASIC PATTERN OF THE VOLUNTARY MOTOR SYSTEM
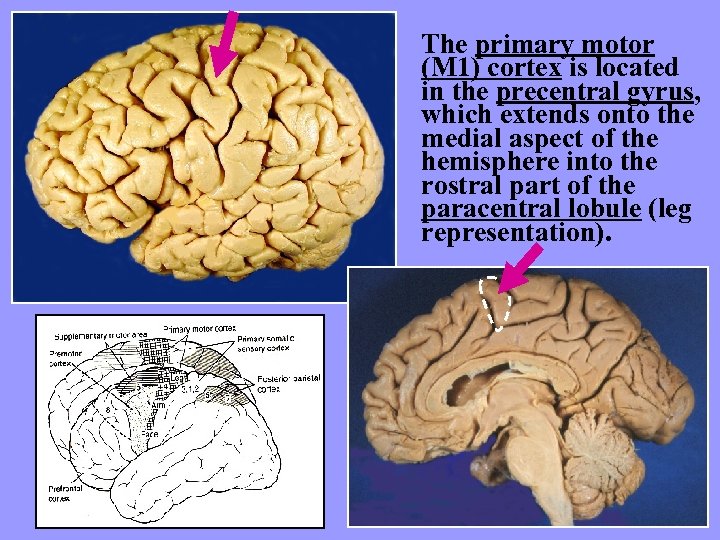 The primary motor (M 1) cortex is located in the precentral gyrus, which extends onto the medial aspect of the hemisphere into the rostral part of the paracentral lobule (leg representation).
The primary motor (M 1) cortex is located in the precentral gyrus, which extends onto the medial aspect of the hemisphere into the rostral part of the paracentral lobule (leg representation).
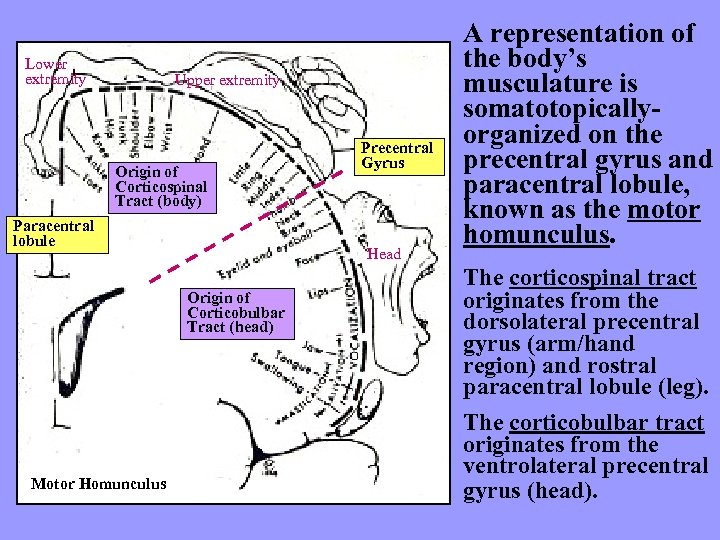 Lower extremity Upper extremity Origin of Corticospinal Tract (body) Paracentral lobule Head Origin of Corticobulbar Tract (head) Motor Homunculus Precentral Gyrus A representation of the body’s musculature is somatotopicallyorganized on the precentral gyrus and paracentral lobule, known as the motor homunculus. The corticospinal tract originates from the dorsolateral precentral gyrus (arm/hand region) and rostral paracentral lobule (leg). The corticobulbar tract originates from the ventrolateral precentral gyrus (head).
Lower extremity Upper extremity Origin of Corticospinal Tract (body) Paracentral lobule Head Origin of Corticobulbar Tract (head) Motor Homunculus Precentral Gyrus A representation of the body’s musculature is somatotopicallyorganized on the precentral gyrus and paracentral lobule, known as the motor homunculus. The corticospinal tract originates from the dorsolateral precentral gyrus (arm/hand region) and rostral paracentral lobule (leg). The corticobulbar tract originates from the ventrolateral precentral gyrus (head).
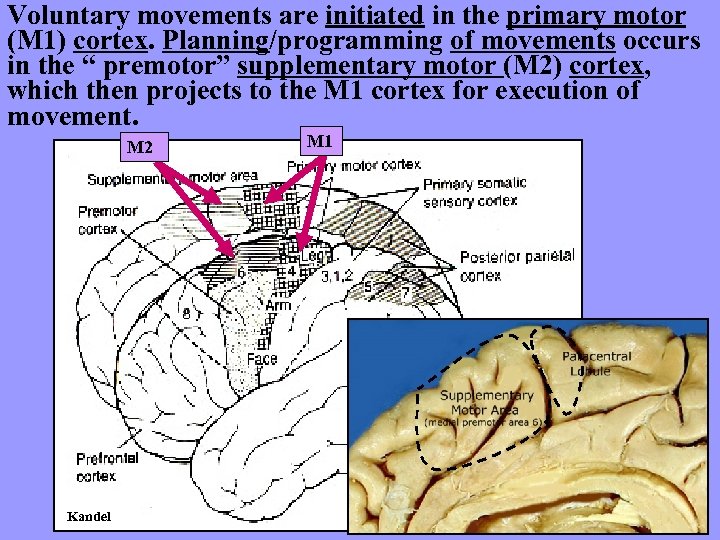 Voluntary movements are initiated in the primary motor (M 1) cortex. Planning/programming of movements occurs in the “ premotor” supplementary motor (M 2) cortex, which then projects to the M 1 cortex for execution of movement. M 2 Kandel M 1
Voluntary movements are initiated in the primary motor (M 1) cortex. Planning/programming of movements occurs in the “ premotor” supplementary motor (M 2) cortex, which then projects to the M 1 cortex for execution of movement. M 2 Kandel M 1
 Corticospinal Tract
Corticospinal Tract
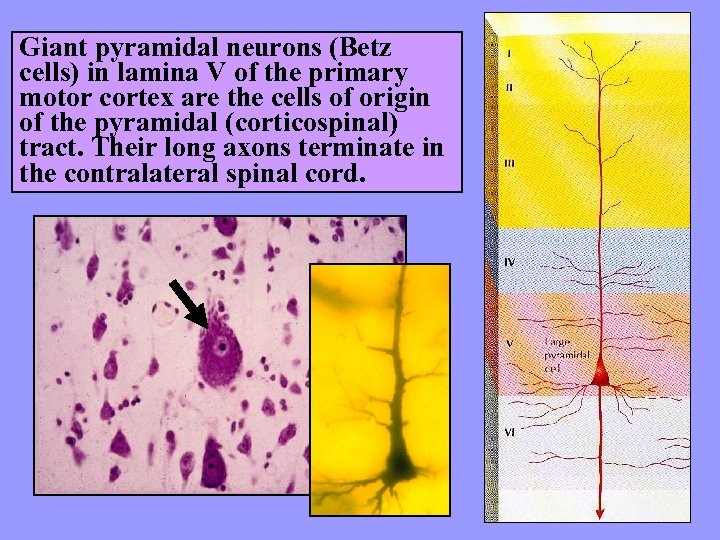 Giant pyramidal neurons (Betz cells) in lamina V of the primary motor cortex are the cells of origin of the pyramidal (corticospinal) tract. Their long axons terminate in the contralateral spinal cord.
Giant pyramidal neurons (Betz cells) in lamina V of the primary motor cortex are the cells of origin of the pyramidal (corticospinal) tract. Their long axons terminate in the contralateral spinal cord.
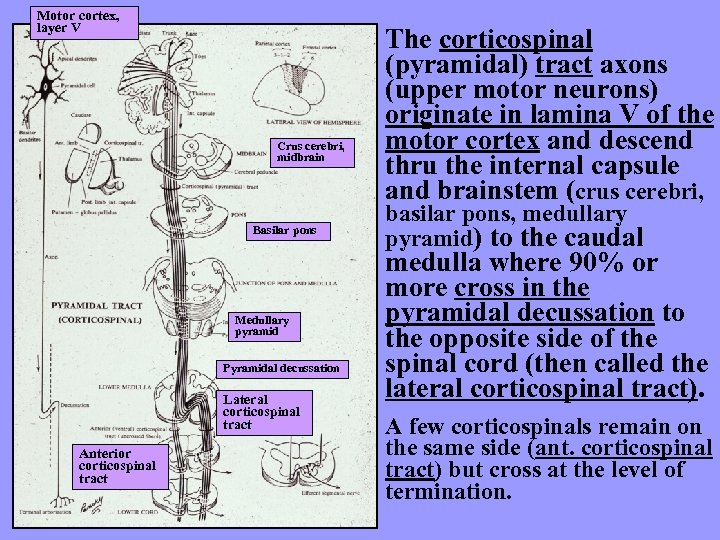 Motor cortex, layer V Crus cerebri, midbrain Basilar pons Medullary pyramid Pyramidal decussation Lateral corticospinal tract Anterior corticospinal tract The corticospinal (pyramidal) tract axons (upper motor neurons) originate in lamina V of the motor cortex and descend thru the internal capsule and brainstem (crus cerebri, basilar pons, medullary pyramid) to the caudal medulla where 90% or more cross in the pyramidal decussation to the opposite side of the spinal cord (then called the lateral corticospinal tract). A few corticospinals remain on the same side (ant. corticospinal tract) but cross at the level of termination.
Motor cortex, layer V Crus cerebri, midbrain Basilar pons Medullary pyramid Pyramidal decussation Lateral corticospinal tract Anterior corticospinal tract The corticospinal (pyramidal) tract axons (upper motor neurons) originate in lamina V of the motor cortex and descend thru the internal capsule and brainstem (crus cerebri, basilar pons, medullary pyramid) to the caudal medulla where 90% or more cross in the pyramidal decussation to the opposite side of the spinal cord (then called the lateral corticospinal tract). A few corticospinals remain on the same side (ant. corticospinal tract) but cross at the level of termination.
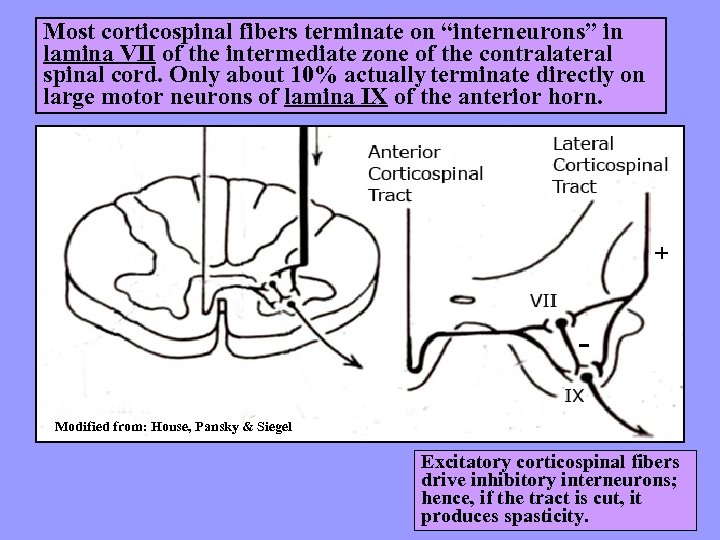 Most corticospinal fibers terminate on “interneurons” in lamina VII of the intermediate zone of the contralateral spinal cord. Only about 10% actually terminate directly on large motor neurons of lamina IX of the anterior horn. + Modified from: House, Pansky & Siegel Excitatory corticospinal fibers drive inhibitory interneurons; hence, if the tract is cut, it produces spasticity.
Most corticospinal fibers terminate on “interneurons” in lamina VII of the intermediate zone of the contralateral spinal cord. Only about 10% actually terminate directly on large motor neurons of lamina IX of the anterior horn. + Modified from: House, Pansky & Siegel Excitatory corticospinal fibers drive inhibitory interneurons; hence, if the tract is cut, it produces spasticity.
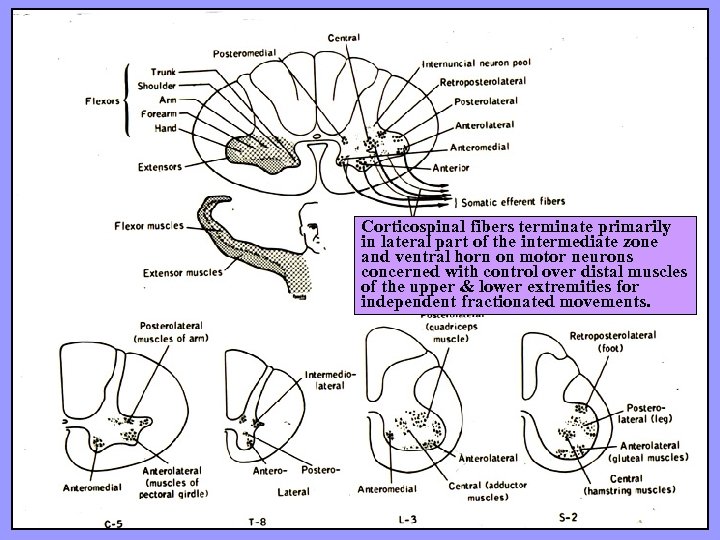 Corticospinal fibers terminate primarily in lateral part of the intermediate zone and ventral horn on motor neurons concerned with control over distal muscles of the upper & lower extremities for independent fractionated movements.
Corticospinal fibers terminate primarily in lateral part of the intermediate zone and ventral horn on motor neurons concerned with control over distal muscles of the upper & lower extremities for independent fractionated movements.
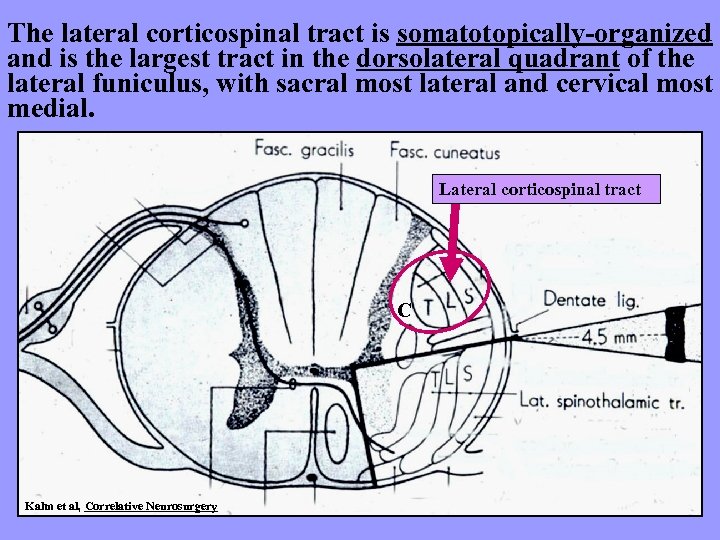 The lateral corticospinal tract is somatotopically-organized and is the largest tract in the dorsolateral quadrant of the lateral funiculus, with sacral most lateral and cervical most medial. Lateral corticospinal tract C Kahn et al, Correlative Neurosurgery
The lateral corticospinal tract is somatotopically-organized and is the largest tract in the dorsolateral quadrant of the lateral funiculus, with sacral most lateral and cervical most medial. Lateral corticospinal tract C Kahn et al, Correlative Neurosurgery
 Corticobulbar Tract
Corticobulbar Tract
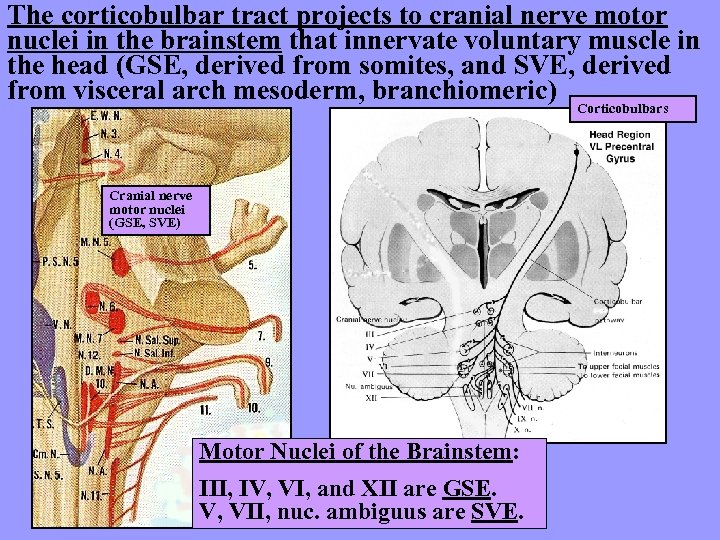 The corticobulbar tract projects to cranial nerve motor nuclei in the brainstem that innervate voluntary muscle in the head (GSE, derived from somites, and SVE, derived from visceral arch mesoderm, branchiomeric) Corticobulbars Cranial nerve motor nuclei (GSE, SVE) Motor Nuclei of the Brainstem: III, IV, VI, and XII are GSE. V, VII, nuc. ambiguus are SVE.
The corticobulbar tract projects to cranial nerve motor nuclei in the brainstem that innervate voluntary muscle in the head (GSE, derived from somites, and SVE, derived from visceral arch mesoderm, branchiomeric) Corticobulbars Cranial nerve motor nuclei (GSE, SVE) Motor Nuclei of the Brainstem: III, IV, VI, and XII are GSE. V, VII, nuc. ambiguus are SVE.
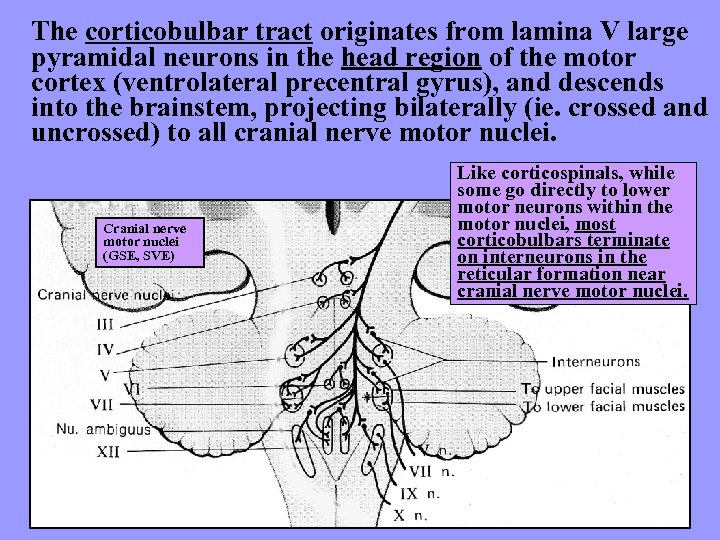 The corticobulbar tract originates from lamina V large pyramidal neurons in the head region of the motor cortex (ventrolateral precentral gyrus), and descends into the brainstem, projecting bilaterally (ie. crossed and uncrossed) to all cranial nerve motor nuclei. Cranial nerve motor nuclei (GSE, SVE) Like corticospinals, while some go directly to lower motor neurons within the motor nuclei, most corticobulbars terminate on interneurons in the reticular formation near cranial nerve motor nuclei.
The corticobulbar tract originates from lamina V large pyramidal neurons in the head region of the motor cortex (ventrolateral precentral gyrus), and descends into the brainstem, projecting bilaterally (ie. crossed and uncrossed) to all cranial nerve motor nuclei. Cranial nerve motor nuclei (GSE, SVE) Like corticospinals, while some go directly to lower motor neurons within the motor nuclei, most corticobulbars terminate on interneurons in the reticular formation near cranial nerve motor nuclei.
 Since corticobulbars project bilaterally to cranial nerve motor nuclei, how does the clinician diagnose a unilateral corticobulbar tract lesion? since there would be no profound paralysis in head muscles because the other side (intact contralateral corticobulbar tract) would still innervate the nucleus. Diagnosis of a corticobulbar tract lesion is facilitated by the unique corticobulbar innervation of the facial nucleus.
Since corticobulbars project bilaterally to cranial nerve motor nuclei, how does the clinician diagnose a unilateral corticobulbar tract lesion? since there would be no profound paralysis in head muscles because the other side (intact contralateral corticobulbar tract) would still innervate the nucleus. Diagnosis of a corticobulbar tract lesion is facilitated by the unique corticobulbar innervation of the facial nucleus.
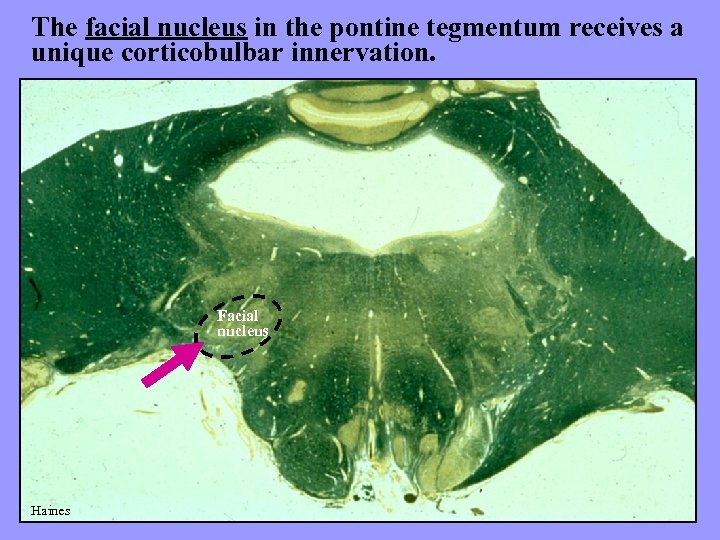 The facial nucleus in the pontine tegmentum receives a unique corticobulbar innervation. Facial nucleus Haines
The facial nucleus in the pontine tegmentum receives a unique corticobulbar innervation. Facial nucleus Haines
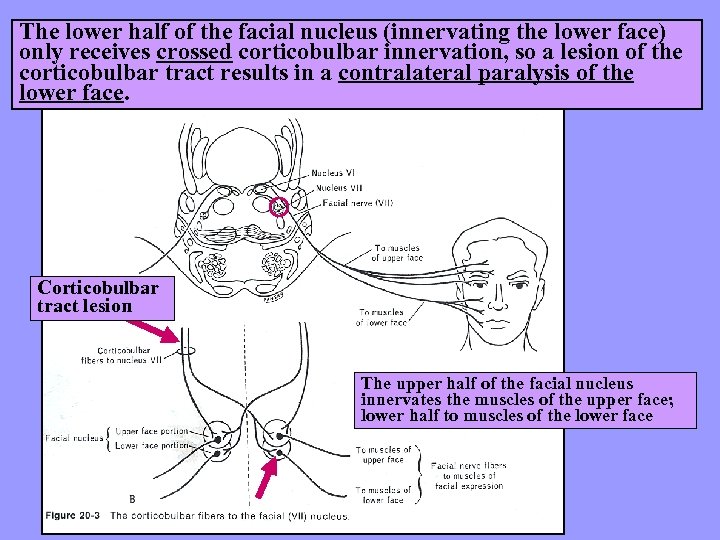 The lower half of the facial nucleus (innervating the lower face) only receives crossed corticobulbar innervation, so a lesion of the corticobulbar tract results in a contralateral paralysis of the lower face. Corticobulbar tract lesion The upper half of the facial nucleus innervates the muscles of the upper face; lower half to muscles of the lower face
The lower half of the facial nucleus (innervating the lower face) only receives crossed corticobulbar innervation, so a lesion of the corticobulbar tract results in a contralateral paralysis of the lower face. Corticobulbar tract lesion The upper half of the facial nucleus innervates the muscles of the upper face; lower half to muscles of the lower face
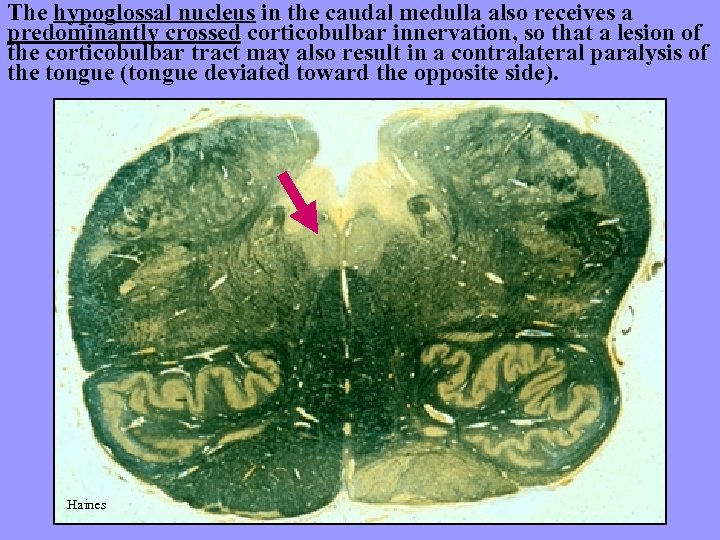 The hypoglossal nucleus in the caudal medulla also receives a predominantly crossed corticobulbar innervation, so that a lesion of the corticobulbar tract may also result in a contralateral paralysis of the tongue (tongue deviated toward the opposite side). Haines
The hypoglossal nucleus in the caudal medulla also receives a predominantly crossed corticobulbar innervation, so that a lesion of the corticobulbar tract may also result in a contralateral paralysis of the tongue (tongue deviated toward the opposite side). Haines
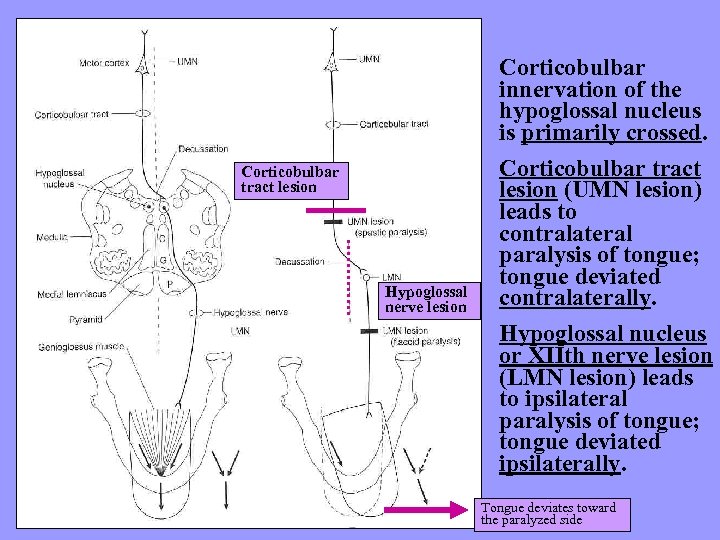 Corticobulbar tract lesion Hypoglossal nerve lesion Corticobulbar innervation of the hypoglossal nucleus is primarily crossed. Corticobulbar tract lesion (UMN lesion) leads to contralateral paralysis of tongue; tongue deviated contralaterally. Hypoglossal nucleus or XIIth nerve lesion (LMN lesion) leads to ipsilateral paralysis of tongue; tongue deviated ipsilaterally. Tongue deviates toward the paralyzed side
Corticobulbar tract lesion Hypoglossal nerve lesion Corticobulbar innervation of the hypoglossal nucleus is primarily crossed. Corticobulbar tract lesion (UMN lesion) leads to contralateral paralysis of tongue; tongue deviated contralaterally. Hypoglossal nucleus or XIIth nerve lesion (LMN lesion) leads to ipsilateral paralysis of tongue; tongue deviated ipsilaterally. Tongue deviates toward the paralyzed side
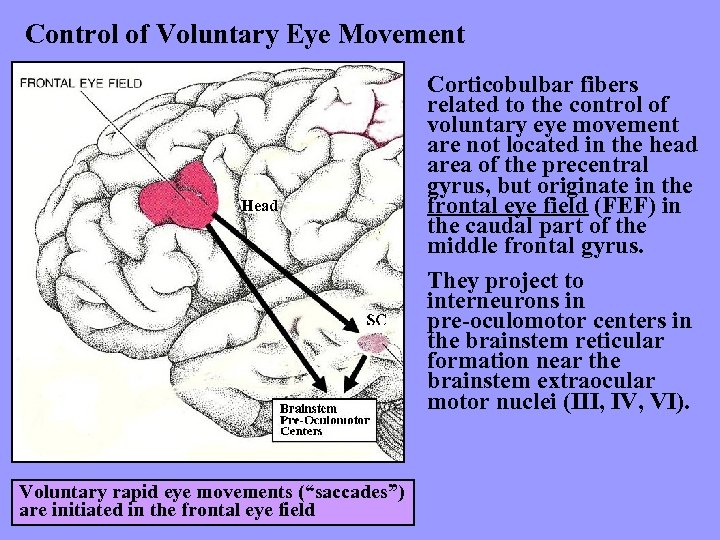 Control of Voluntary Eye Movement Head Voluntary rapid eye movements (“saccades”) are initiated in the frontal eye field Corticobulbar fibers related to the control of voluntary eye movement are not located in the head area of the precentral gyrus, but originate in the frontal eye field (FEF) in the caudal part of the middle frontal gyrus. They project to interneurons in pre-oculomotor centers in the brainstem reticular formation near the brainstem extraocular motor nuclei (III, IV, VI).
Control of Voluntary Eye Movement Head Voluntary rapid eye movements (“saccades”) are initiated in the frontal eye field Corticobulbar fibers related to the control of voluntary eye movement are not located in the head area of the precentral gyrus, but originate in the frontal eye field (FEF) in the caudal part of the middle frontal gyrus. They project to interneurons in pre-oculomotor centers in the brainstem reticular formation near the brainstem extraocular motor nuclei (III, IV, VI).
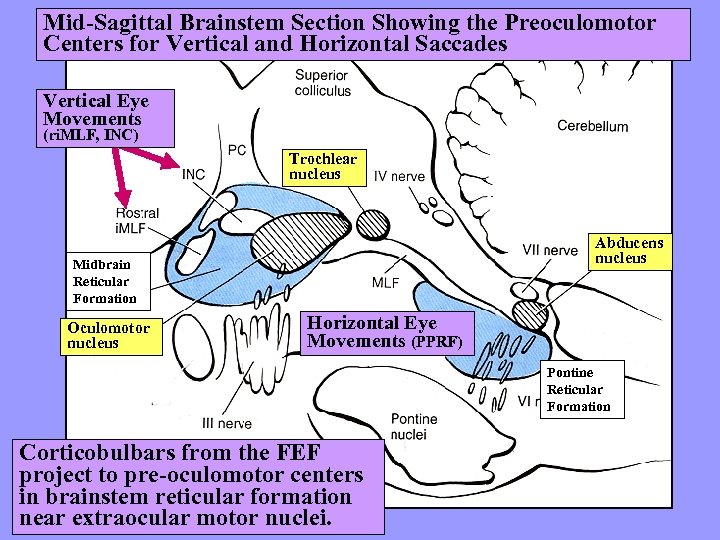 Mid-Sagittal Brainstem Section Showing the Preoculomotor Centers for Vertical and Horizontal Saccades Vertical Eye Movements (ri. MLF, INC) Trochlear nucleus Abducens nucleus Midbrain Reticular Formation Oculomotor nucleus Horizontal Eye Movements (PPRF) Pontine Reticular Formation Corticobulbars from the FEF project to pre-oculomotor centers in brainstem reticular formation near extraocular motor nuclei.
Mid-Sagittal Brainstem Section Showing the Preoculomotor Centers for Vertical and Horizontal Saccades Vertical Eye Movements (ri. MLF, INC) Trochlear nucleus Abducens nucleus Midbrain Reticular Formation Oculomotor nucleus Horizontal Eye Movements (PPRF) Pontine Reticular Formation Corticobulbars from the FEF project to pre-oculomotor centers in brainstem reticular formation near extraocular motor nuclei.
 Clinical Applications
Clinical Applications
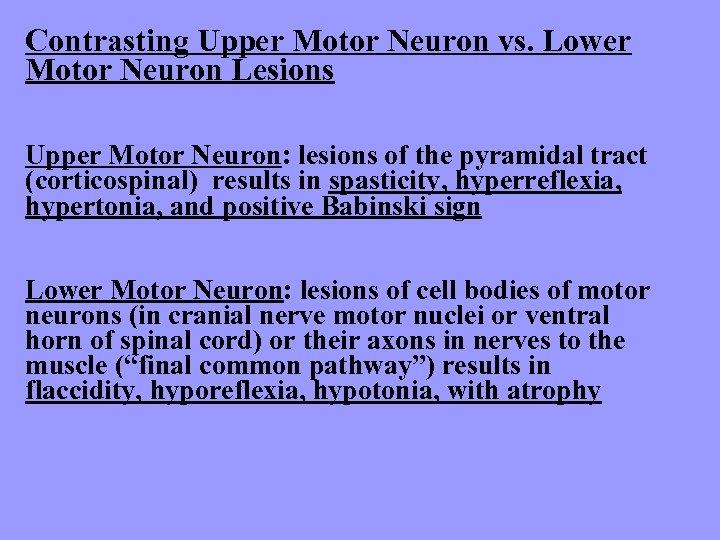 Contrasting Upper Motor Neuron vs. Lower Motor Neuron Lesions Upper Motor Neuron: lesions of the pyramidal tract (corticospinal) results in spasticity, hyperreflexia, hypertonia, and positive Babinski sign Lower Motor Neuron: lesions of cell bodies of motor neurons (in cranial nerve motor nuclei or ventral horn of spinal cord) or their axons in nerves to the muscle (“final common pathway”) results in flaccidity, hyporeflexia, hypotonia, with atrophy
Contrasting Upper Motor Neuron vs. Lower Motor Neuron Lesions Upper Motor Neuron: lesions of the pyramidal tract (corticospinal) results in spasticity, hyperreflexia, hypertonia, and positive Babinski sign Lower Motor Neuron: lesions of cell bodies of motor neurons (in cranial nerve motor nuclei or ventral horn of spinal cord) or their axons in nerves to the muscle (“final common pathway”) results in flaccidity, hyporeflexia, hypotonia, with atrophy
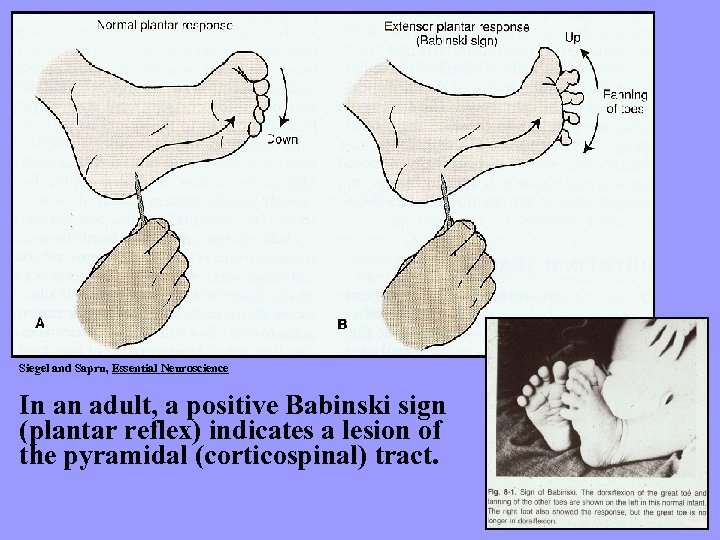 Siegel and Sapru, Essential Neuroscience In an adult, a positive Babinski sign (plantar reflex) indicates a lesion of the pyramidal (corticospinal) tract.
Siegel and Sapru, Essential Neuroscience In an adult, a positive Babinski sign (plantar reflex) indicates a lesion of the pyramidal (corticospinal) tract.
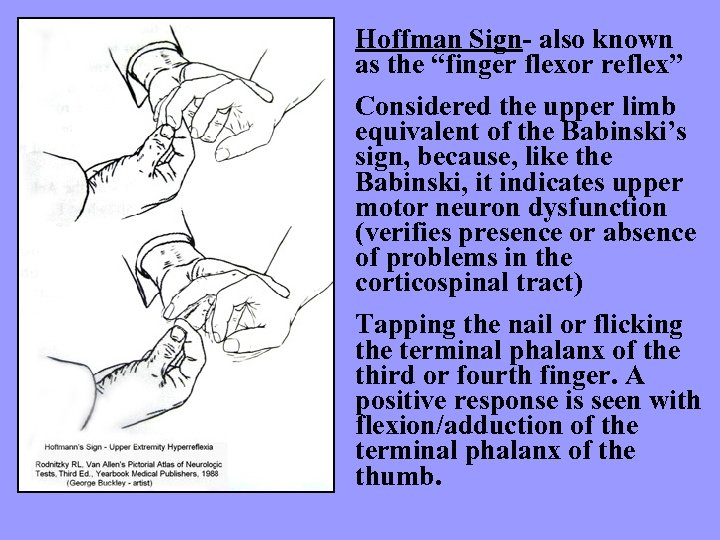 Hoffman Sign- also known as the “finger flexor reflex” Considered the upper limb equivalent of the Babinski’s sign, because, like the Babinski, it indicates upper motor neuron dysfunction (verifies presence or absence of problems in the corticospinal tract) Tapping the nail or flicking the terminal phalanx of the third or fourth finger. A positive response is seen with flexion/adduction of the terminal phalanx of the thumb.
Hoffman Sign- also known as the “finger flexor reflex” Considered the upper limb equivalent of the Babinski’s sign, because, like the Babinski, it indicates upper motor neuron dysfunction (verifies presence or absence of problems in the corticospinal tract) Tapping the nail or flicking the terminal phalanx of the third or fourth finger. A positive response is seen with flexion/adduction of the terminal phalanx of the thumb.
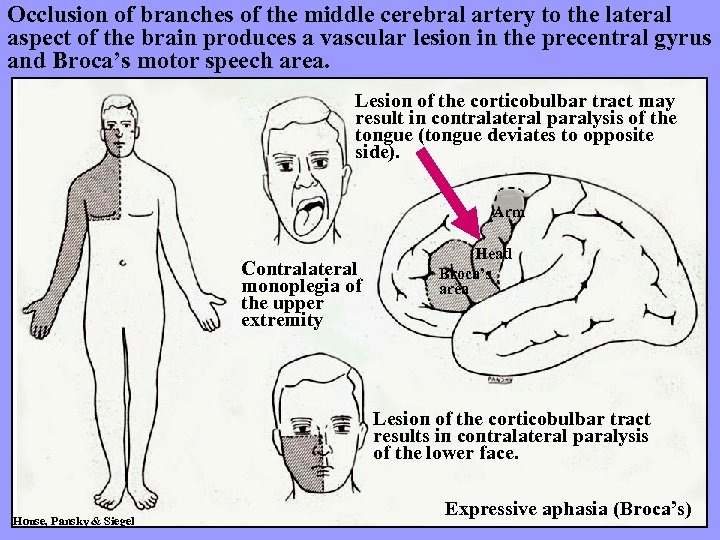 Occlusion of branches of the middle cerebral artery to the lateral aspect of the brain produces a vascular lesion in the precentral gyrus and Broca’s motor speech area. Lesion of the corticobulbar tract may result in contralateral paralysis of the tongue (tongue deviates to opposite side). Arm Contralateral monoplegia of the upper extremity Head Broca’s area Lesion of the corticobulbar tract results in contralateral paralysis of the lower face. House, Pansky & Siegel Expressive aphasia (Broca’s)
Occlusion of branches of the middle cerebral artery to the lateral aspect of the brain produces a vascular lesion in the precentral gyrus and Broca’s motor speech area. Lesion of the corticobulbar tract may result in contralateral paralysis of the tongue (tongue deviates to opposite side). Arm Contralateral monoplegia of the upper extremity Head Broca’s area Lesion of the corticobulbar tract results in contralateral paralysis of the lower face. House, Pansky & Siegel Expressive aphasia (Broca’s)
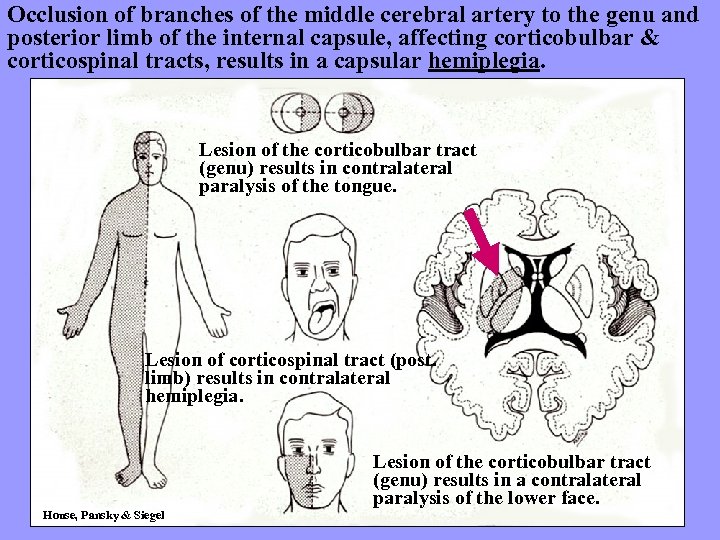 Occlusion of branches of the middle cerebral artery to the genu and posterior limb of the internal capsule, affecting corticobulbar & corticospinal tracts, results in a capsular hemiplegia. Lesion of the corticobulbar tract (genu) results in contralateral paralysis of the tongue. Lesion of corticospinal tract (post. limb) results in contralateral hemiplegia. Lesion of the corticobulbar tract (genu) results in a contralateral paralysis of the lower face. House, Pansky & Siegel
Occlusion of branches of the middle cerebral artery to the genu and posterior limb of the internal capsule, affecting corticobulbar & corticospinal tracts, results in a capsular hemiplegia. Lesion of the corticobulbar tract (genu) results in contralateral paralysis of the tongue. Lesion of corticospinal tract (post. limb) results in contralateral hemiplegia. Lesion of the corticobulbar tract (genu) results in a contralateral paralysis of the lower face. House, Pansky & Siegel
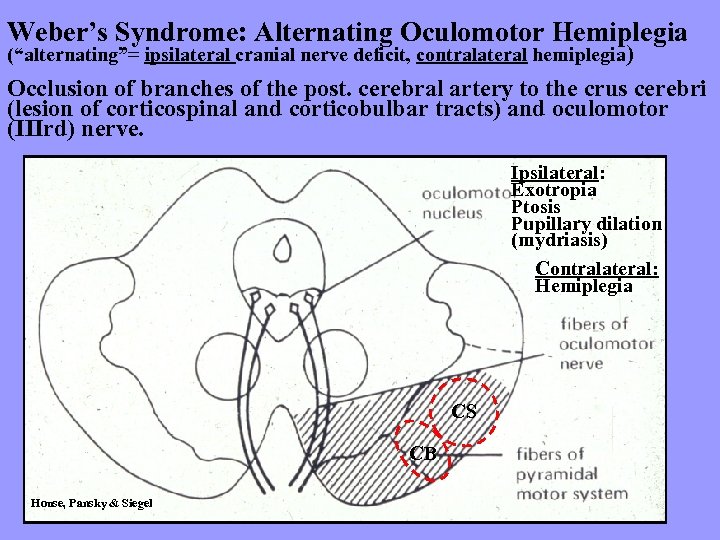 Weber’s Syndrome: Alternating Oculomotor Hemiplegia (“alternating”= ipsilateral cranial nerve deficit, contralateral hemiplegia) Occlusion of branches of the post. cerebral artery to the crus cerebri (lesion of corticospinal and corticobulbar tracts) and oculomotor (IIIrd) nerve. Ipsilateral: Exotropia Ptosis Pupillary dilation (mydriasis) Contralateral: Hemiplegia CS CB House, Pansky & Siegel
Weber’s Syndrome: Alternating Oculomotor Hemiplegia (“alternating”= ipsilateral cranial nerve deficit, contralateral hemiplegia) Occlusion of branches of the post. cerebral artery to the crus cerebri (lesion of corticospinal and corticobulbar tracts) and oculomotor (IIIrd) nerve. Ipsilateral: Exotropia Ptosis Pupillary dilation (mydriasis) Contralateral: Hemiplegia CS CB House, Pansky & Siegel
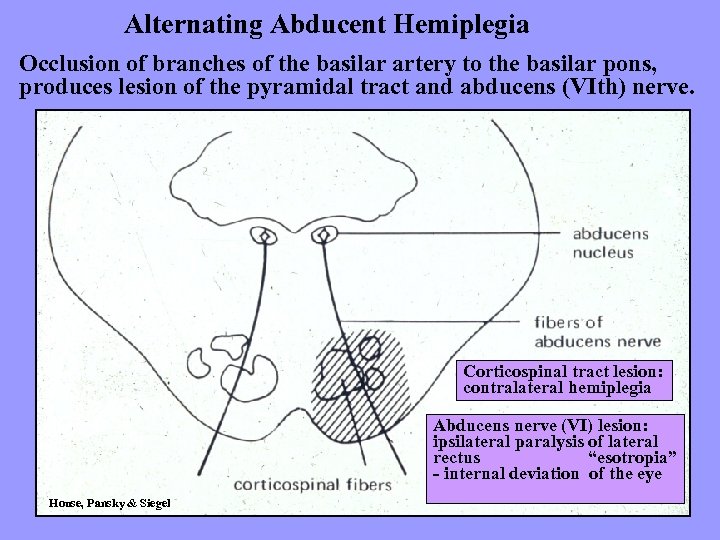 Alternating Abducent Hemiplegia Occlusion of branches of the basilar artery to the basilar pons, produces lesion of the pyramidal tract and abducens (VIth) nerve. Corticospinal tract lesion: contralateral hemiplegia Abducens nerve (VI) lesion: ipsilateral paralysis of lateral rectus “esotropia” - internal deviation of the eye House, Pansky & Siegel
Alternating Abducent Hemiplegia Occlusion of branches of the basilar artery to the basilar pons, produces lesion of the pyramidal tract and abducens (VIth) nerve. Corticospinal tract lesion: contralateral hemiplegia Abducens nerve (VI) lesion: ipsilateral paralysis of lateral rectus “esotropia” - internal deviation of the eye House, Pansky & Siegel
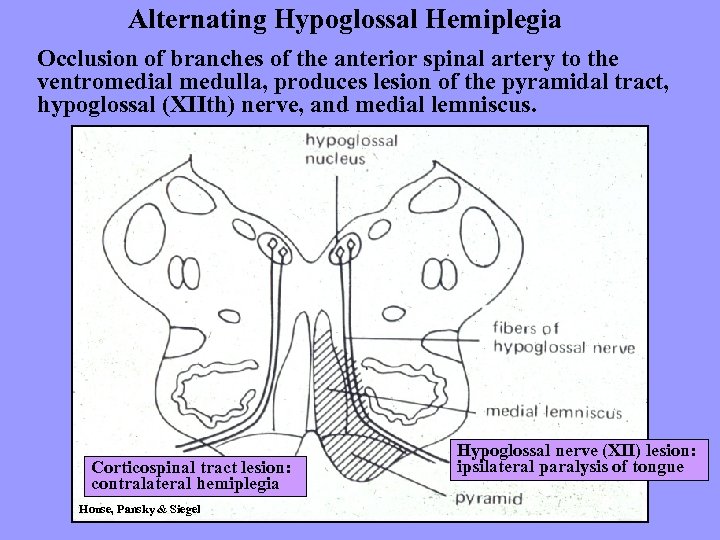 Alternating Hypoglossal Hemiplegia Occlusion of branches of the anterior spinal artery to the ventromedial medulla, produces lesion of the pyramidal tract, hypoglossal (XIIth) nerve, and medial lemniscus. Corticospinal tract lesion: contralateral hemiplegia House, Pansky & Siegel Hypoglossal nerve (XII) lesion: ipsilateral paralysis of tongue
Alternating Hypoglossal Hemiplegia Occlusion of branches of the anterior spinal artery to the ventromedial medulla, produces lesion of the pyramidal tract, hypoglossal (XIIth) nerve, and medial lemniscus. Corticospinal tract lesion: contralateral hemiplegia House, Pansky & Siegel Hypoglossal nerve (XII) lesion: ipsilateral paralysis of tongue
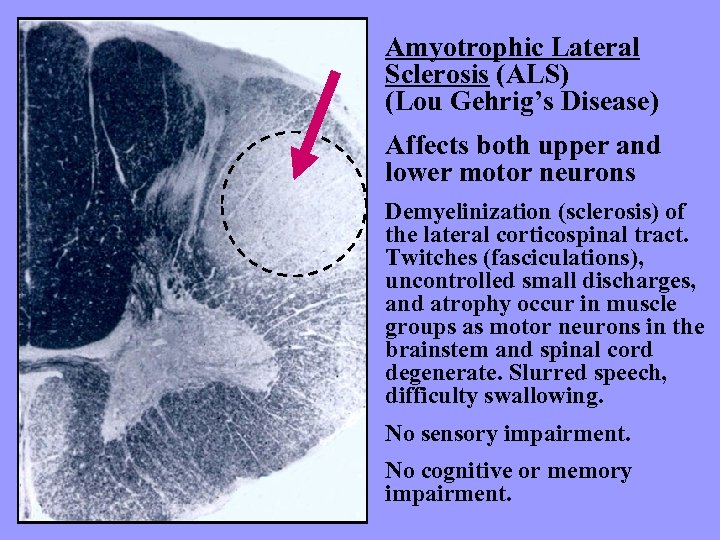 Amyotrophic Lateral Sclerosis (ALS) (Lou Gehrig’s Disease) Affects both upper and lower motor neurons Demyelinization (sclerosis) of the lateral corticospinal tract. Twitches (fasciculations), uncontrolled small discharges, and atrophy occur in muscle groups as motor neurons in the brainstem and spinal cord degenerate. Slurred speech, difficulty swallowing. No sensory impairment. No cognitive or memory impairment.
Amyotrophic Lateral Sclerosis (ALS) (Lou Gehrig’s Disease) Affects both upper and lower motor neurons Demyelinization (sclerosis) of the lateral corticospinal tract. Twitches (fasciculations), uncontrolled small discharges, and atrophy occur in muscle groups as motor neurons in the brainstem and spinal cord degenerate. Slurred speech, difficulty swallowing. No sensory impairment. No cognitive or memory impairment.
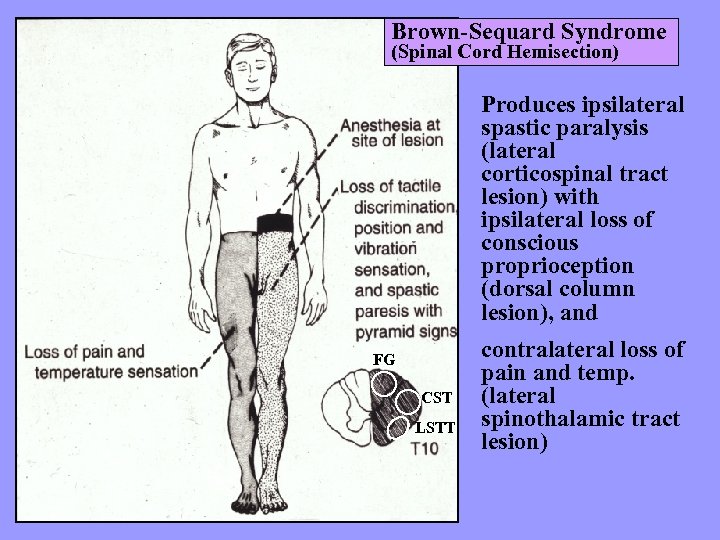 Brown-Sequard Syndrome (Spinal Cord Hemisection) Produces ipsilateral spastic paralysis (lateral corticospinal tract lesion) with ipsilateral loss of conscious proprioception (dorsal column lesion), and FG CST LSTT contralateral loss of pain and temp. (lateral spinothalamic tract lesion)
Brown-Sequard Syndrome (Spinal Cord Hemisection) Produces ipsilateral spastic paralysis (lateral corticospinal tract lesion) with ipsilateral loss of conscious proprioception (dorsal column lesion), and FG CST LSTT contralateral loss of pain and temp. (lateral spinothalamic tract lesion)
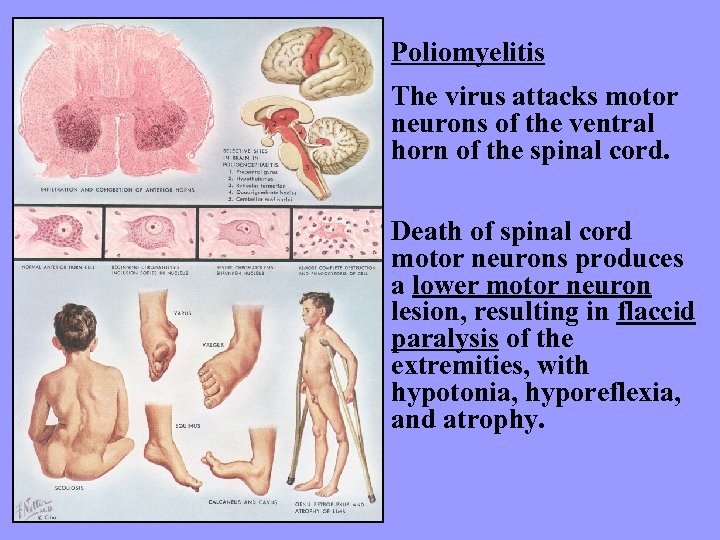 Poliomyelitis The virus attacks motor neurons of the ventral horn of the spinal cord. Death of spinal cord motor neurons produces a lower motor neuron lesion, resulting in flaccid paralysis of the extremities, with hypotonia, hyporeflexia, and atrophy.
Poliomyelitis The virus attacks motor neurons of the ventral horn of the spinal cord. Death of spinal cord motor neurons produces a lower motor neuron lesion, resulting in flaccid paralysis of the extremities, with hypotonia, hyporeflexia, and atrophy.


