urology_5_pyelonephritis.ppt
- Количество слайдов: 30
 Pyelonephritis 1
Pyelonephritis 1
 Contents • • • Definition Types Etiology Clinical features Management 2
Contents • • • Definition Types Etiology Clinical features Management 2
 Definition • Inflammation of the renal parenchyma • Maybe acute or chronic 3
Definition • Inflammation of the renal parenchyma • Maybe acute or chronic 3
 Acute pyelonephritis • Inflammation of the renal parenchyma with local and systemic manifestations of infection ❏ may be classified as uncomplicated or complicated – uncomplicated: in the absence of conditions predisposing to anatomic or functional impairment of urine flow – complicated: occurring in the setting of renal or ureteric stones, strictures, prostatic obstruction (hypertrophy or malignancy), vesicoureteric reflux, neurogenic bladder, catheters, DM, sickle-cell hemoglobinopathies, polycystic kidney disease, immunosuppression, and post-renal transplant 4
Acute pyelonephritis • Inflammation of the renal parenchyma with local and systemic manifestations of infection ❏ may be classified as uncomplicated or complicated – uncomplicated: in the absence of conditions predisposing to anatomic or functional impairment of urine flow – complicated: occurring in the setting of renal or ureteric stones, strictures, prostatic obstruction (hypertrophy or malignancy), vesicoureteric reflux, neurogenic bladder, catheters, DM, sickle-cell hemoglobinopathies, polycystic kidney disease, immunosuppression, and post-renal transplant 4
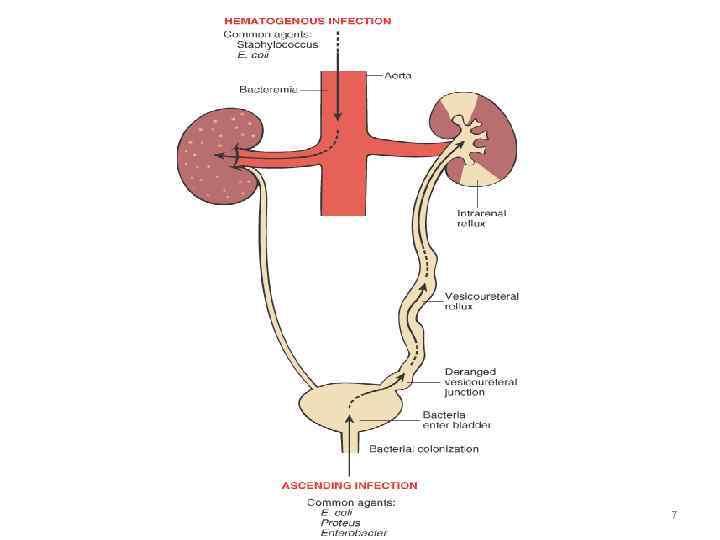
 Etiology ❏ usually ascending microorganisms, most often bacteria ❏ in females with uncomplicated pyelonephritis usually E. coli ❏ causative microorganisms are usually E. coli, Klebsiella, Proteus, Serratia, Pseudomonas, Enterococcus, and S. aureus ❏ if S. aureus is found, suspect bacteremic spread from a distant focus (e. g. septic emboli in infective endocarditis) and suspect (possible multiple intra-renal microabscesses or perinephric abscess) 5
Etiology ❏ usually ascending microorganisms, most often bacteria ❏ in females with uncomplicated pyelonephritis usually E. coli ❏ causative microorganisms are usually E. coli, Klebsiella, Proteus, Serratia, Pseudomonas, Enterococcus, and S. aureus ❏ if S. aureus is found, suspect bacteremic spread from a distant focus (e. g. septic emboli in infective endocarditis) and suspect (possible multiple intra-renal microabscesses or perinephric abscess) 5
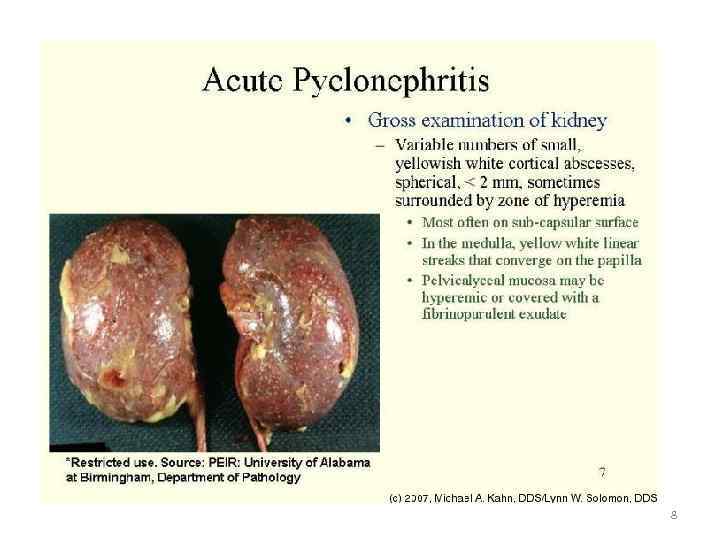
 Pathology • Loss of demarcation between the cortex & medulla • Multiple abscesses with widespread interstitial infiltration with polymorphonuclear leucocytes 6
Pathology • Loss of demarcation between the cortex & medulla • Multiple abscesses with widespread interstitial infiltration with polymorphonuclear leucocytes 6
 7
7
 8
8
 Clinical Presentation ❏ rapid onset (hours to a day) ❏ lethargic and unwell, fever, tachycardia, shaking, chills, nausea and vomiting, myalgias ❏ marked CVA or flank tenderness; possible abdominal pain on deep palpation ❏ symptoms of lower UTI may be absent (urgency, frequency, dysuria) ❏ may have symptoms of Gram negative sepsis 9
Clinical Presentation ❏ rapid onset (hours to a day) ❏ lethargic and unwell, fever, tachycardia, shaking, chills, nausea and vomiting, myalgias ❏ marked CVA or flank tenderness; possible abdominal pain on deep palpation ❏ symptoms of lower UTI may be absent (urgency, frequency, dysuria) ❏ may have symptoms of Gram negative sepsis 9
 Note ❏ Patients (especially the elderly) with acute pyelonephritis +/– sepsis may present initially with only back pain, abdominal pain, symptoms of disturbed GI function, or mental status changes 10
Note ❏ Patients (especially the elderly) with acute pyelonephritis +/– sepsis may present initially with only back pain, abdominal pain, symptoms of disturbed GI function, or mental status changes 10
 Investigations ❏ urine dipstick: +ve for leukocytes and nitrites, possible hematuria ❏ microscopy: > 5 WBC/HPF in unspun urine or > 10 WBC/HPF in spun urine, bacteria ❏ Gram stain: Gram negative rods, Gram positive cocci ❏ culture: > 105 colony forming units (CFU)/m. L in clean catch midstream urine or > 102 CFU/m. L in suprapubic aspirate or catheterized specimen ❏ CBC and differential: leukocytosis, high % neutrophils ❏ blood cultures: may be positive in 20% of cases, especially in S. aureus infection ❏ consider investigation of complicated pyelonephritis: if fever, pain, leukocytosis not resolving with treatment within 72 hr, if male patient, or if there is history of urinary tract abnormalities (abdo /pelvis U/S, CT for renal abscess, spiral CT for stones, cystoscopy) 11
Investigations ❏ urine dipstick: +ve for leukocytes and nitrites, possible hematuria ❏ microscopy: > 5 WBC/HPF in unspun urine or > 10 WBC/HPF in spun urine, bacteria ❏ Gram stain: Gram negative rods, Gram positive cocci ❏ culture: > 105 colony forming units (CFU)/m. L in clean catch midstream urine or > 102 CFU/m. L in suprapubic aspirate or catheterized specimen ❏ CBC and differential: leukocytosis, high % neutrophils ❏ blood cultures: may be positive in 20% of cases, especially in S. aureus infection ❏ consider investigation of complicated pyelonephritis: if fever, pain, leukocytosis not resolving with treatment within 72 hr, if male patient, or if there is history of urinary tract abnormalities (abdo /pelvis U/S, CT for renal abscess, spiral CT for stones, cystoscopy) 11
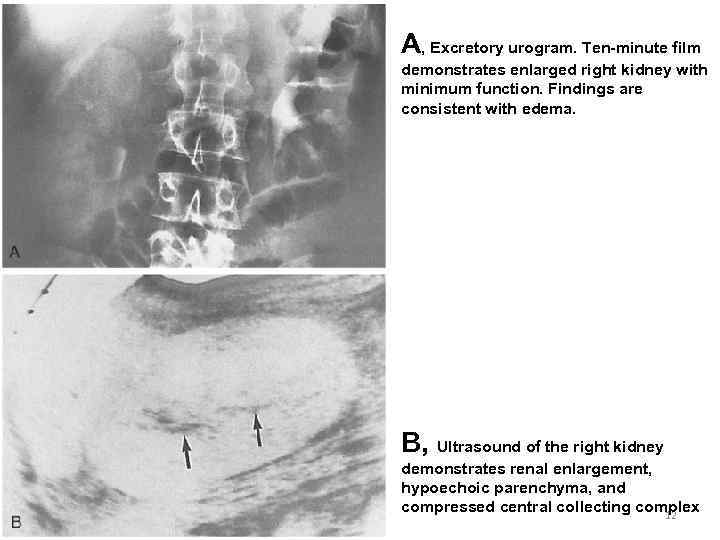 A, Excretory urogram. Ten-minute film demonstrates enlarged right kidney with minimum function. Findings are consistent with edema. B, Ultrasound of the right kidney demonstrates renal enlargement, hypoechoic parenchyma, and compressed central collecting complex 12
A, Excretory urogram. Ten-minute film demonstrates enlarged right kidney with minimum function. Findings are consistent with edema. B, Ultrasound of the right kidney demonstrates renal enlargement, hypoechoic parenchyma, and compressed central collecting complex 12
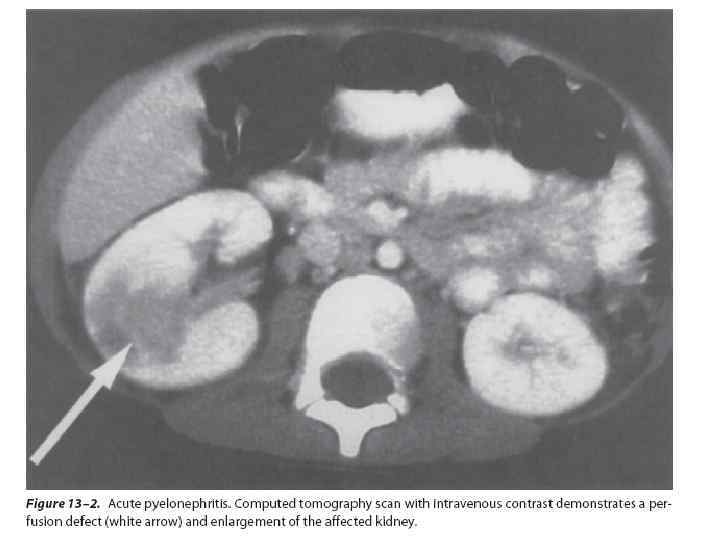 13
13
 Complications • Chronicity • Bacteraemia or Septicaemia 14
Complications • Chronicity • Bacteraemia or Septicaemia 14
 Differential diagnosis • • • Acute appendicitis Acute cholecystitis Acute diverticulitis Pancreatitis Basal pneumonia Herpes zoster affecting somatic segments of T 12 & L 1 15
Differential diagnosis • • • Acute appendicitis Acute cholecystitis Acute diverticulitis Pancreatitis Basal pneumonia Herpes zoster affecting somatic segments of T 12 & L 1 15
 Treatment ❏ uncomplicated pyelonephritis with mild symptoms • 14 day course of TMP/SMX (trimethoprim-sulfamethoxazole) or fluoroquinolone or third generation cephalosporin • start with IV for several days and then switch to PO (can then be treated as outpatient) ❏ patient more than mildly symptomatic or complicated pyelonephritis in the setting of stone obstruction is an urologic emergency (placing patient at risk of kidney loss or septic shock) • start broad spectrum IV antibiotics until cultures return (imipenem or emropenem or piperacillin /tazobactam or ampicillin+gentamicin) and treat 2 -3 weeks • follow-up cultures 2 -4 weeks after stopping treatment ❏ if no improvement in 48 -72 hr, need to continue on IV antibiotics, assess for complicated pyelonephritis or possible renal or perinephric abscess 16
Treatment ❏ uncomplicated pyelonephritis with mild symptoms • 14 day course of TMP/SMX (trimethoprim-sulfamethoxazole) or fluoroquinolone or third generation cephalosporin • start with IV for several days and then switch to PO (can then be treated as outpatient) ❏ patient more than mildly symptomatic or complicated pyelonephritis in the setting of stone obstruction is an urologic emergency (placing patient at risk of kidney loss or septic shock) • start broad spectrum IV antibiotics until cultures return (imipenem or emropenem or piperacillin /tazobactam or ampicillin+gentamicin) and treat 2 -3 weeks • follow-up cultures 2 -4 weeks after stopping treatment ❏ if no improvement in 48 -72 hr, need to continue on IV antibiotics, assess for complicated pyelonephritis or possible renal or perinephric abscess 16
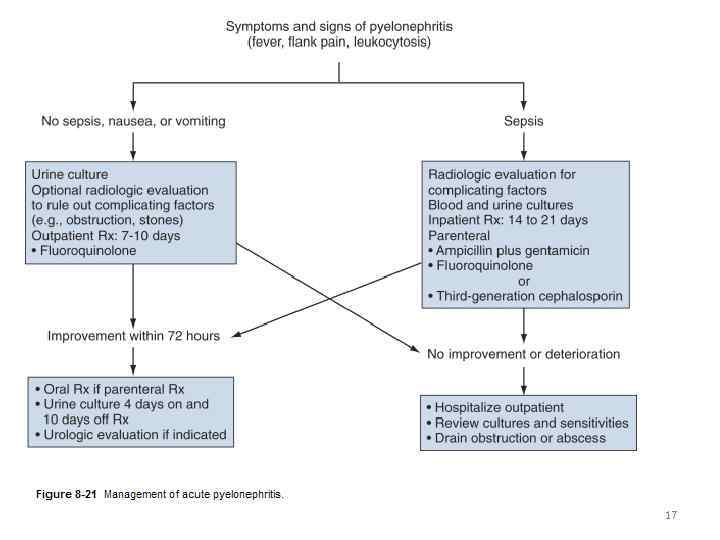 17
17
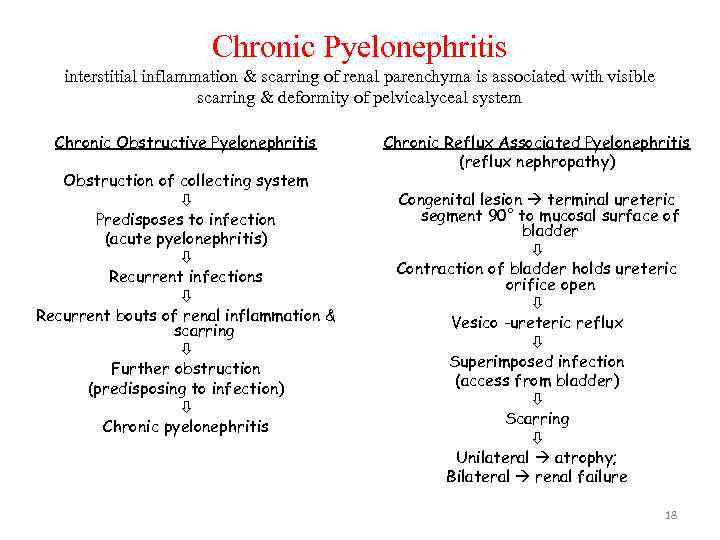 Chronic Pyelonephritis interstitial inflammation & scarring of renal parenchyma is associated with visible scarring & deformity of pelvicalyceal system Chronic Obstructive Pyelonephritis Obstruction of collecting system Predisposes to infection (acute pyelonephritis) Recurrent infections Recurrent bouts of renal inflammation & scarring Further obstruction (predisposing to infection) Chronic pyelonephritis Chronic Reflux Associated Pyelonephritis (reflux nephropathy) Congenital lesion terminal ureteric segment 90° to mucosal surface of bladder Contraction of bladder holds ureteric orifice open Vesico -ureteric reflux Superimposed infection (access from bladder) Scarring Unilateral atrophy; Bilateral renal failure 18
Chronic Pyelonephritis interstitial inflammation & scarring of renal parenchyma is associated with visible scarring & deformity of pelvicalyceal system Chronic Obstructive Pyelonephritis Obstruction of collecting system Predisposes to infection (acute pyelonephritis) Recurrent infections Recurrent bouts of renal inflammation & scarring Further obstruction (predisposing to infection) Chronic pyelonephritis Chronic Reflux Associated Pyelonephritis (reflux nephropathy) Congenital lesion terminal ureteric segment 90° to mucosal surface of bladder Contraction of bladder holds ureteric orifice open Vesico -ureteric reflux Superimposed infection (access from bladder) Scarring Unilateral atrophy; Bilateral renal failure 18
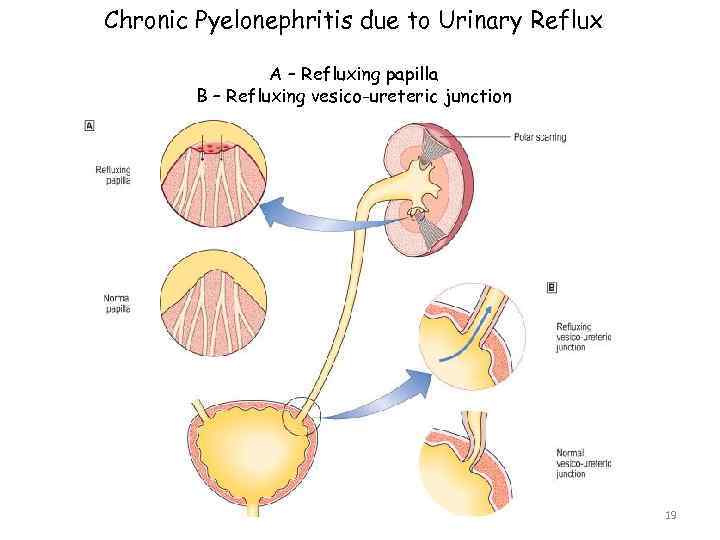 Chronic Pyelonephritis due to Urinary Reflux A – Refluxing papilla B – Refluxing vesico-ureteric junction 19
Chronic Pyelonephritis due to Urinary Reflux A – Refluxing papilla B – Refluxing vesico-ureteric junction 19
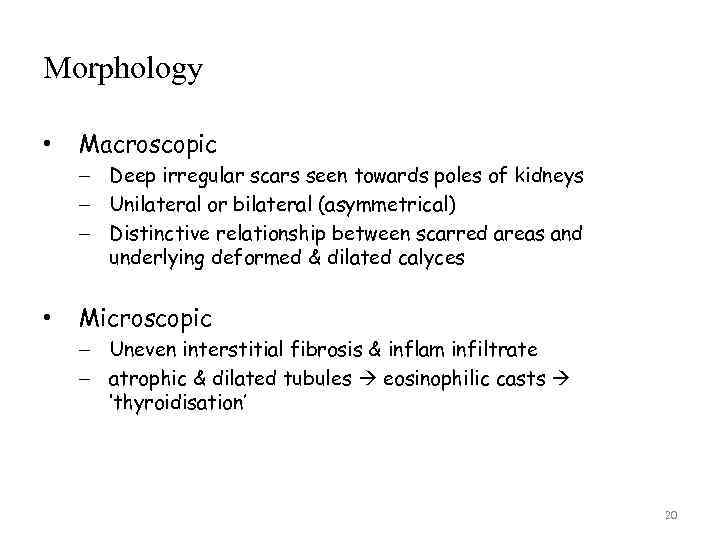 Morphology • Macroscopic – Deep irregular scars seen towards poles of kidneys – Unilateral or bilateral (asymmetrical) – Distinctive relationship between scarred areas and underlying deformed & dilated calyces • Microscopic – Uneven interstitial fibrosis & inflam infiltrate – atrophic & dilated tubules eosinophilic casts ‘thyroidisation’ 20
Morphology • Macroscopic – Deep irregular scars seen towards poles of kidneys – Unilateral or bilateral (asymmetrical) – Distinctive relationship between scarred areas and underlying deformed & dilated calyces • Microscopic – Uneven interstitial fibrosis & inflam infiltrate – atrophic & dilated tubules eosinophilic casts ‘thyroidisation’ 20
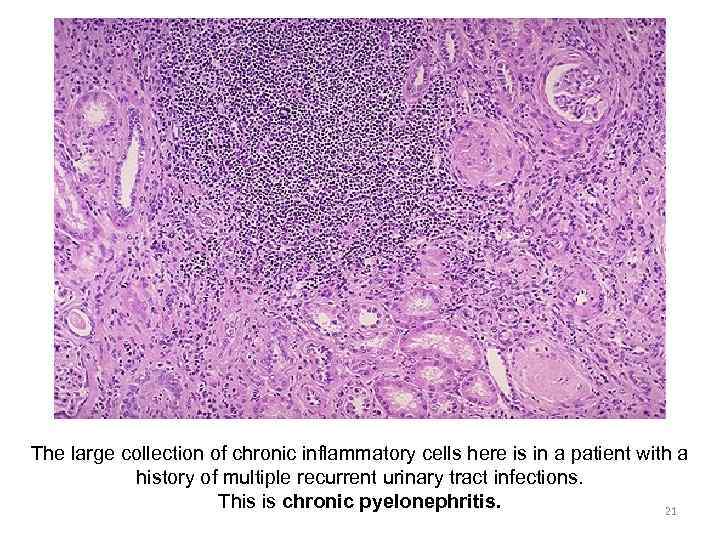 The large collection of chronic inflammatory cells here is in a patient with a history of multiple recurrent urinary tract infections. This is chronic pyelonephritis. 21
The large collection of chronic inflammatory cells here is in a patient with a history of multiple recurrent urinary tract infections. This is chronic pyelonephritis. 21
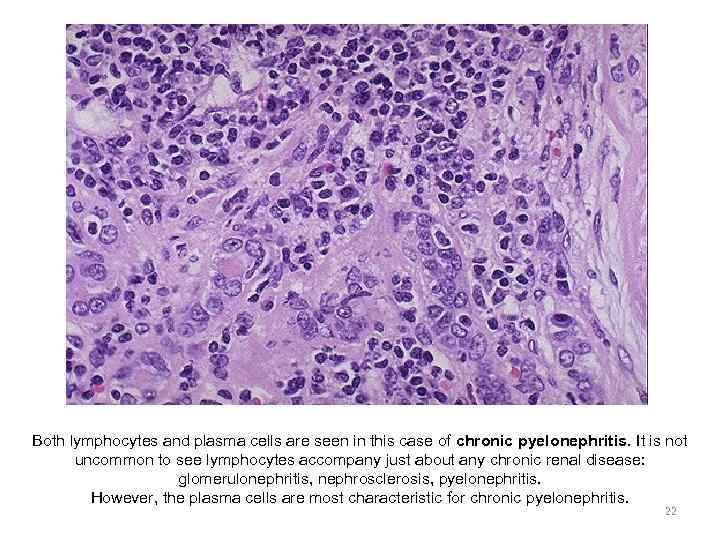 Both lymphocytes and plasma cells are seen in this case of chronic pyelonephritis. It is not uncommon to see lymphocytes accompany just about any chronic renal disease: glomerulonephritis, nephrosclerosis, pyelonephritis. However, the plasma cells are most characteristic for chronic pyelonephritis. 22
Both lymphocytes and plasma cells are seen in this case of chronic pyelonephritis. It is not uncommon to see lymphocytes accompany just about any chronic renal disease: glomerulonephritis, nephrosclerosis, pyelonephritis. However, the plasma cells are most characteristic for chronic pyelonephritis. 22
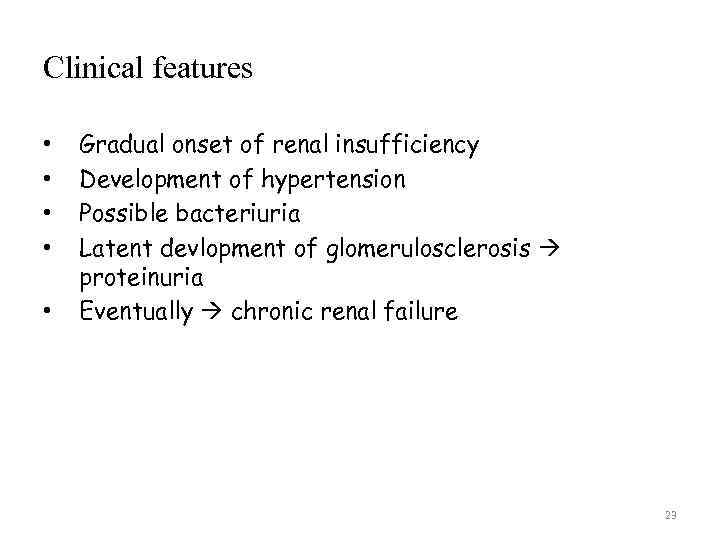 Clinical features • • • Gradual onset of renal insufficiency Development of hypertension Possible bacteriuria Latent devlopment of glomerulosclerosis proteinuria Eventually chronic renal failure 23
Clinical features • • • Gradual onset of renal insufficiency Development of hypertension Possible bacteriuria Latent devlopment of glomerulosclerosis proteinuria Eventually chronic renal failure 23
 Investigations • • Blood Urine X- ray Cystoscopy 24
Investigations • • Blood Urine X- ray Cystoscopy 24
 Treatment • • • Treatment of the cause Medical treatment Surgical treatment: – – Removal of obstruction Repair of vesicoureteric reflux Partial nephrectomy Nephrectomy 25
Treatment • • • Treatment of the cause Medical treatment Surgical treatment: – – Removal of obstruction Repair of vesicoureteric reflux Partial nephrectomy Nephrectomy 25
 Chronic pyelonephritis • Persistent presence of bacteria in the kidney ❏ a form of chronic tubulointerstitial nephritis of bacterial origin ❏ cortical scarring, tubulointerstitial damage, and calyceal deformities seen ❏ may be active (persistent infection) or inactive (persistent focal sterile scars post-infection) ❏ histologically indistinguishable from many other forms of TIN (severe vesicoureteric reflux, hypertensive disease, analgesic nephropathy) ❏ active chronic pyelonephritis may respond to antibiotics ❏ need to rule out TB 26
Chronic pyelonephritis • Persistent presence of bacteria in the kidney ❏ a form of chronic tubulointerstitial nephritis of bacterial origin ❏ cortical scarring, tubulointerstitial damage, and calyceal deformities seen ❏ may be active (persistent infection) or inactive (persistent focal sterile scars post-infection) ❏ histologically indistinguishable from many other forms of TIN (severe vesicoureteric reflux, hypertensive disease, analgesic nephropathy) ❏ active chronic pyelonephritis may respond to antibiotics ❏ need to rule out TB 26
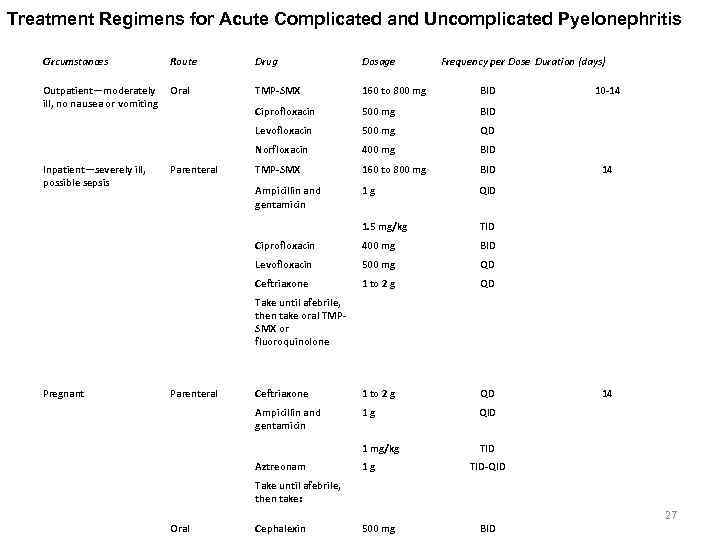 Treatment Regimens for Acute Complicated and Uncomplicated Pyelonephritis Circumstances Route Drug Dosage Outpatient—moderately ill, no nausea or vomiting Oral TMP-SMX 160 to 800 mg BID Ciprofloxacin 500 mg BID Levofloxacin 500 mg QD Norfloxacin 400 mg BID Parenteral TMP-SMX 160 to 800 mg BID Ampicillin and gentamicin 1 g QID 1. 5 mg/kg TID Ciprofloxacin 400 mg BID Levofloxacin 500 mg QD Ceftriaxone 1 to 2 g QD Take until afebrile, then take oral TMPSMX or fluoroquinolone Parenteral Ceftriaxone 1 to 2 g QD Ampicillin and gentamicin 1 g QID 1 mg/kg TID Aztreonam 1 g TID-QID Take until afebrile, then take: Oral Cephalexin 500 mg Inpatient—severely ill, possible sepsis Pregnant Frequency per Dose Duration (days) 10 -14 14 BID 27
Treatment Regimens for Acute Complicated and Uncomplicated Pyelonephritis Circumstances Route Drug Dosage Outpatient—moderately ill, no nausea or vomiting Oral TMP-SMX 160 to 800 mg BID Ciprofloxacin 500 mg BID Levofloxacin 500 mg QD Norfloxacin 400 mg BID Parenteral TMP-SMX 160 to 800 mg BID Ampicillin and gentamicin 1 g QID 1. 5 mg/kg TID Ciprofloxacin 400 mg BID Levofloxacin 500 mg QD Ceftriaxone 1 to 2 g QD Take until afebrile, then take oral TMPSMX or fluoroquinolone Parenteral Ceftriaxone 1 to 2 g QD Ampicillin and gentamicin 1 g QID 1 mg/kg TID Aztreonam 1 g TID-QID Take until afebrile, then take: Oral Cephalexin 500 mg Inpatient—severely ill, possible sepsis Pregnant Frequency per Dose Duration (days) 10 -14 14 BID 27
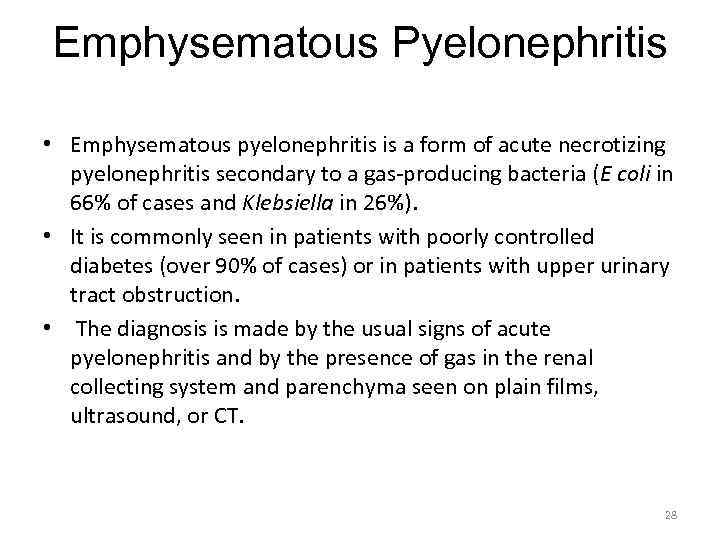 Emphysematous Pyelonephritis • Emphysematous pyelonephritis is a form of acute necrotizing pyelonephritis secondary to a gas-producing bacteria (E coli in 66% of cases and Klebsiella in 26%). • It is commonly seen in patients with poorly controlled diabetes (over 90% of cases) or in patients with upper urinary tract obstruction. • The diagnosis is made by the usual signs of acute pyelonephritis and by the presence of gas in the renal collecting system and parenchyma seen on plain films, ultrasound, or CT. 28
Emphysematous Pyelonephritis • Emphysematous pyelonephritis is a form of acute necrotizing pyelonephritis secondary to a gas-producing bacteria (E coli in 66% of cases and Klebsiella in 26%). • It is commonly seen in patients with poorly controlled diabetes (over 90% of cases) or in patients with upper urinary tract obstruction. • The diagnosis is made by the usual signs of acute pyelonephritis and by the presence of gas in the renal collecting system and parenchyma seen on plain films, ultrasound, or CT. 28
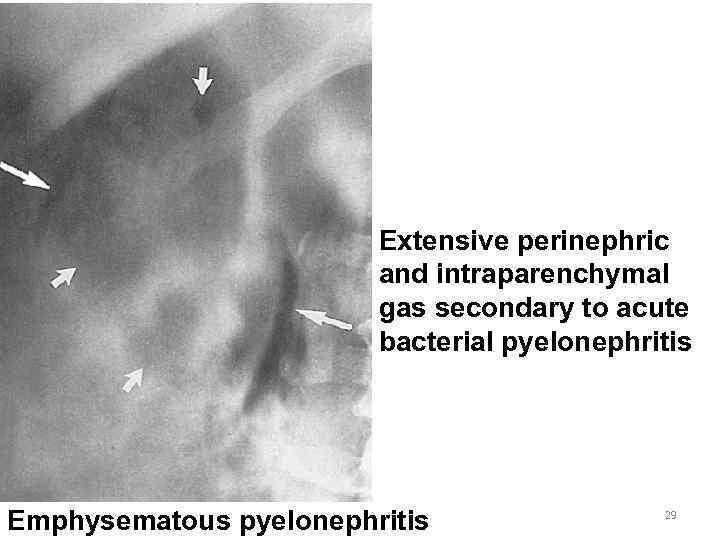 Extensive perinephric and intraparenchymal gas secondary to acute bacterial pyelonephritis Emphysematous pyelonephritis 29
Extensive perinephric and intraparenchymal gas secondary to acute bacterial pyelonephritis Emphysematous pyelonephritis 29
 • The condition is life threatening, with a mortality rate of 40% to 80% with intravenous antibiotics alone. • Obstruction requires drainage either percutaneously or by stent placement. • Operative treatment, including nephrectomy and drainage along with antibiotics, decreases the mortality rate to less than 20%. 30
• The condition is life threatening, with a mortality rate of 40% to 80% with intravenous antibiotics alone. • Obstruction requires drainage either percutaneously or by stent placement. • Operative treatment, including nephrectomy and drainage along with antibiotics, decreases the mortality rate to less than 20%. 30


