822844eff3da19b5f2ae26f4fa497761.ppt
- Количество слайдов: 26
 Putting food allergy in to perspective Jan Sinclair Paediatric Allergy & Clinical Immunology Starship
Putting food allergy in to perspective Jan Sinclair Paediatric Allergy & Clinical Immunology Starship
 The problem Allergy blamed for death at dinner By Martin Johnston 5: 00 AM Thurs Apr 26, 2007 Grant Freeman sat down to a tomato entree on Tuesday night last week at a work dinner. Ten minutes later he collapsed in the toilet. Two days later he was dead, a suspected victim of a food allergy
The problem Allergy blamed for death at dinner By Martin Johnston 5: 00 AM Thurs Apr 26, 2007 Grant Freeman sat down to a tomato entree on Tuesday night last week at a work dinner. Ten minutes later he collapsed in the toilet. Two days later he was dead, a suspected victim of a food allergy
 Outline • Food allergy risks – Available data – Factors influencing risk • Impact of food allergy – Quality of life – Resilience factors • Questions and discussion
Outline • Food allergy risks – Available data – Factors influencing risk • Impact of food allergy – Quality of life – Resilience factors • Questions and discussion
 Risks • Aim of management to avoid reactions – Nuisance reactions – unpleasant but not dangerous – Life threatening reactions • Data difficult – Severe reactions not always recognized • Differentiation from asthma – Fatal reactions not always classified as such
Risks • Aim of management to avoid reactions – Nuisance reactions – unpleasant but not dangerous – Life threatening reactions • Data difficult – Severe reactions not always recognized • Differentiation from asthma – Fatal reactions not always classified as such
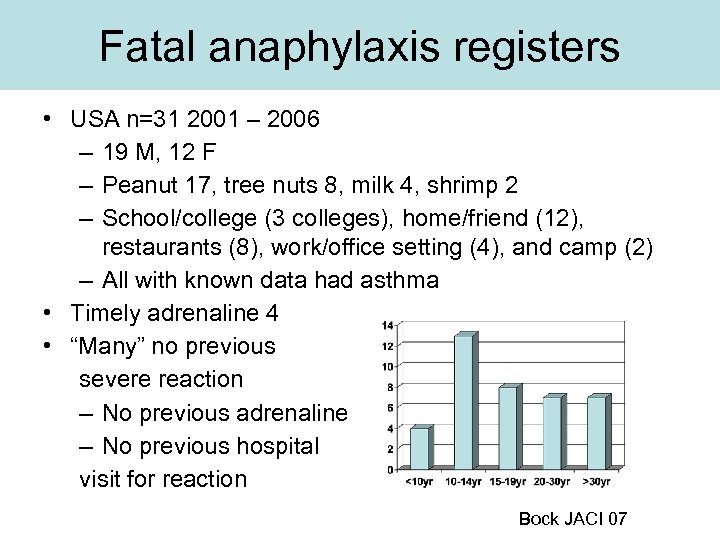 Fatal anaphylaxis registers • USA n=31 2001 – 2006 – 19 M, 12 F – Peanut 17, tree nuts 8, milk 4, shrimp 2 – School/college (3 colleges), home/friend (12), restaurants (8), work/office setting (4), and camp (2) – All with known data had asthma • Timely adrenaline 4 • “Many” no previous severe reaction – No previous adrenaline – No previous hospital visit for reaction Bock JACI 07
Fatal anaphylaxis registers • USA n=31 2001 – 2006 – 19 M, 12 F – Peanut 17, tree nuts 8, milk 4, shrimp 2 – School/college (3 colleges), home/friend (12), restaurants (8), work/office setting (4), and camp (2) – All with known data had asthma • Timely adrenaline 4 • “Many” no previous severe reaction – No previous adrenaline – No previous hospital visit for reaction Bock JACI 07
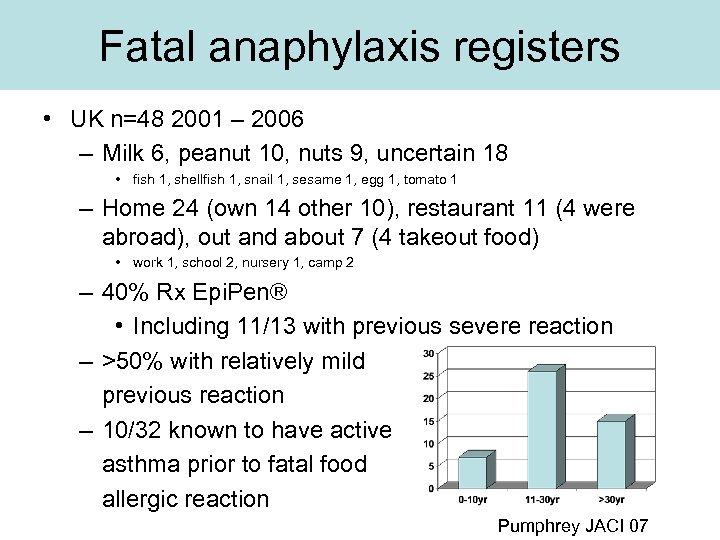 Fatal anaphylaxis registers • UK n=48 2001 – 2006 – Milk 6, peanut 10, nuts 9, uncertain 18 • fish 1, shellfish 1, snail 1, sesame 1, egg 1, tomato 1 – Home 24 (own 14 other 10), restaurant 11 (4 were abroad), out and about 7 (4 takeout food) • work 1, school 2, nursery 1, camp 2 – 40% Rx Epi. Pen® • Including 11/13 with previous severe reaction – >50% with relatively mild previous reaction – 10/32 known to have active asthma prior to fatal food allergic reaction Pumphrey JACI 07
Fatal anaphylaxis registers • UK n=48 2001 – 2006 – Milk 6, peanut 10, nuts 9, uncertain 18 • fish 1, shellfish 1, snail 1, sesame 1, egg 1, tomato 1 – Home 24 (own 14 other 10), restaurant 11 (4 were abroad), out and about 7 (4 takeout food) • work 1, school 2, nursery 1, camp 2 – 40% Rx Epi. Pen® • Including 11/13 with previous severe reaction – >50% with relatively mild previous reaction – 10/32 known to have active asthma prior to fatal food allergic reaction Pumphrey JACI 07
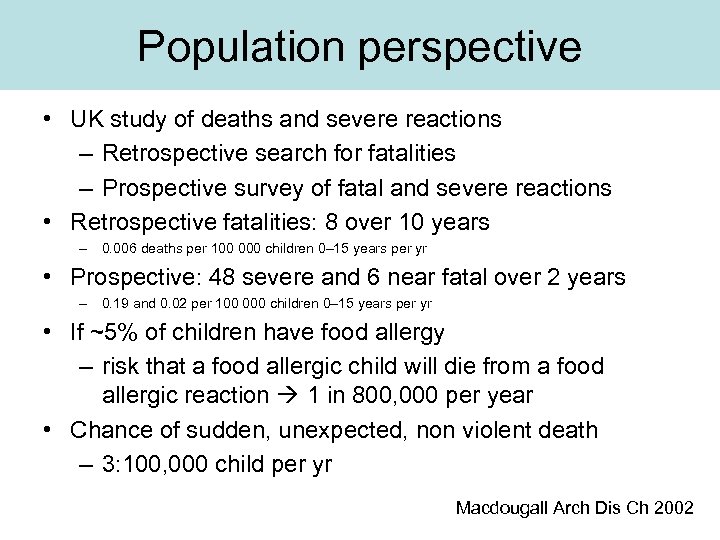 Population perspective • UK study of deaths and severe reactions – Retrospective search for fatalities – Prospective survey of fatal and severe reactions • Retrospective fatalities: 8 over 10 years – 0. 006 deaths per 100 000 children 0– 15 years per yr • Prospective: 48 severe and 6 near fatal over 2 years – 0. 19 and 0. 02 per 100 000 children 0– 15 years per yr • If ~5% of children have food allergy – risk that a food allergic child will die from a food allergic reaction 1 in 800, 000 per year • Chance of sudden, unexpected, non violent death – 3: 100, 000 child per yr Macdougall Arch Dis Ch 2002
Population perspective • UK study of deaths and severe reactions – Retrospective search for fatalities – Prospective survey of fatal and severe reactions • Retrospective fatalities: 8 over 10 years – 0. 006 deaths per 100 000 children 0– 15 years per yr • Prospective: 48 severe and 6 near fatal over 2 years – 0. 19 and 0. 02 per 100 000 children 0– 15 years per yr • If ~5% of children have food allergy – risk that a food allergic child will die from a food allergic reaction 1 in 800, 000 per year • Chance of sudden, unexpected, non violent death – 3: 100, 000 child per yr Macdougall Arch Dis Ch 2002
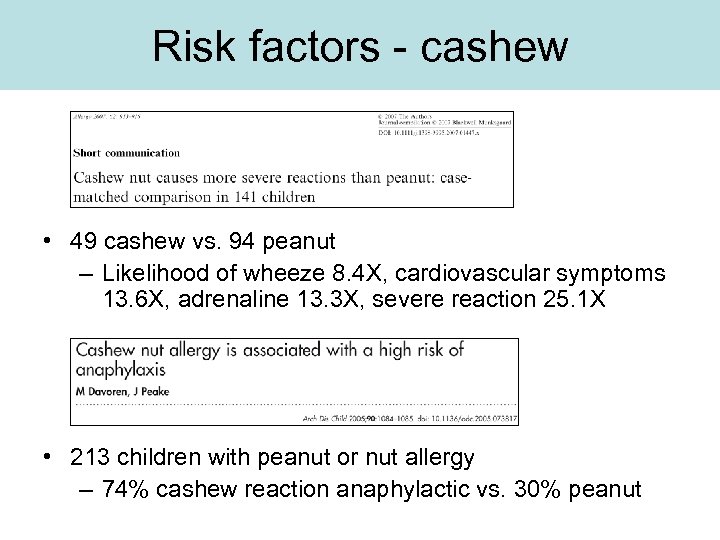 Risk factors - cashew • 49 cashew vs. 94 peanut – Likelihood of wheeze 8. 4 X, cardiovascular symptoms 13. 6 X, adrenaline 13. 3 X, severe reaction 25. 1 X • 213 children with peanut or nut allergy – 74% cashew reaction anaphylactic vs. 30% peanut
Risk factors - cashew • 49 cashew vs. 94 peanut – Likelihood of wheeze 8. 4 X, cardiovascular symptoms 13. 6 X, adrenaline 13. 3 X, severe reaction 25. 1 X • 213 children with peanut or nut allergy – 74% cashew reaction anaphylactic vs. 30% peanut
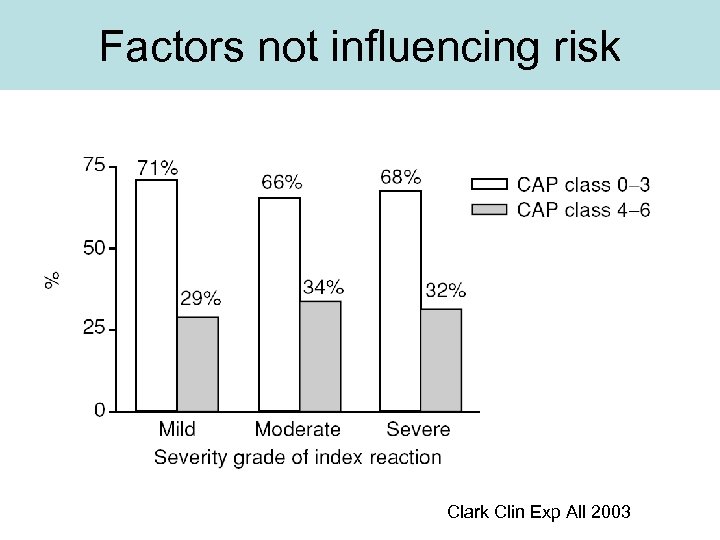 Factors not influencing risk Clark Clin Exp All 2003
Factors not influencing risk Clark Clin Exp All 2003
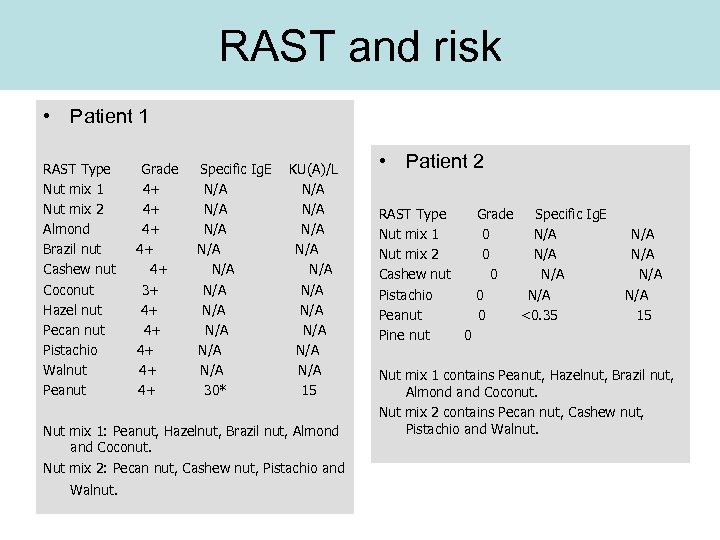 RAST and risk • Patient 1 RAST Type Nut mix 1 Nut mix 2 Almond Brazil nut Cashew nut Coconut Hazel nut Pecan nut Pistachio Walnut Peanut Grade 4+ 4+ 4+ 3+ 4+ 4+ 4+ Specific Ig. E N/A N/A N/A 30* KU(A)/L N/A N/A N/A 15 Nut mix 1: Peanut, Hazelnut, Brazil nut, Almond and Coconut. Nut mix 2: Pecan nut, Cashew nut, Pistachio and Walnut. • Patient 2 RAST Type Nut mix 1 Nut mix 2 Cashew nut Pistachio Peanut Pine nut 0 Grade Specific Ig. E 0 N/A 0 <0. 35 N/A N/A 15 Nut mix 1 contains Peanut, Hazelnut, Brazil nut, Almond and Coconut. Nut mix 2 contains Pecan nut, Cashew nut, Pistachio and Walnut.
RAST and risk • Patient 1 RAST Type Nut mix 1 Nut mix 2 Almond Brazil nut Cashew nut Coconut Hazel nut Pecan nut Pistachio Walnut Peanut Grade 4+ 4+ 4+ 3+ 4+ 4+ 4+ Specific Ig. E N/A N/A N/A 30* KU(A)/L N/A N/A N/A 15 Nut mix 1: Peanut, Hazelnut, Brazil nut, Almond and Coconut. Nut mix 2: Pecan nut, Cashew nut, Pistachio and Walnut. • Patient 2 RAST Type Nut mix 1 Nut mix 2 Cashew nut Pistachio Peanut Pine nut 0 Grade Specific Ig. E 0 N/A 0 <0. 35 N/A N/A 15 Nut mix 1 contains Peanut, Hazelnut, Brazil nut, Almond and Coconut. Nut mix 2 contains Pecan nut, Cashew nut, Pistachio and Walnut.
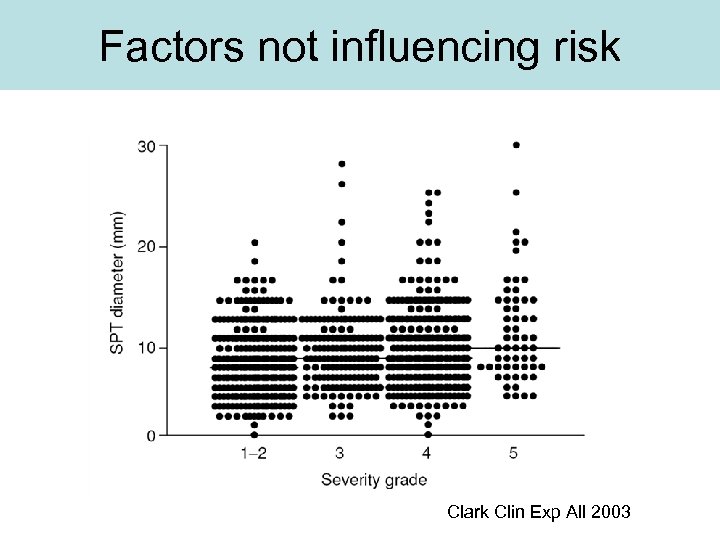 Factors not influencing risk Clark Clin Exp All 2003
Factors not influencing risk Clark Clin Exp All 2003
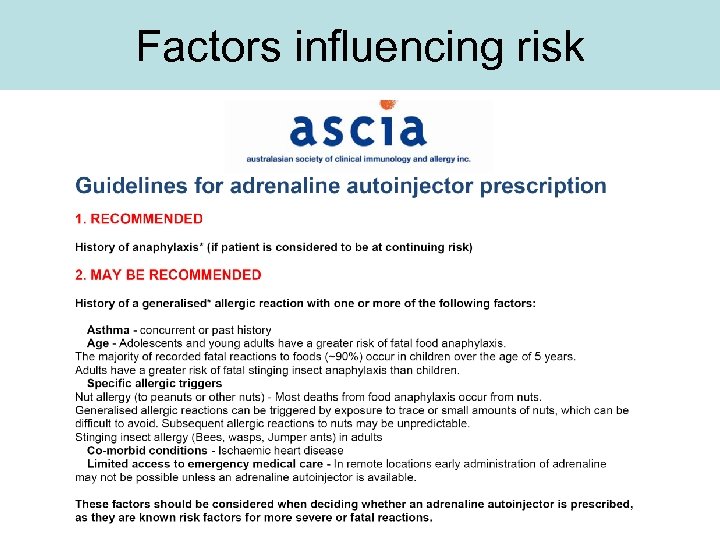 Factors influencing risk
Factors influencing risk

 Food allergy psychological burden • Peanut allergy c. f. rheumatologic disease – 153 vs. 69 children, and 37 vs. 42 adults – Peanut allergy associated with more disruption of daily activity and impact on family relations in children • Rheumatologic disease associated with more impact than peanut allergy in adults Primeau, Clin Exp All, 2000
Food allergy psychological burden • Peanut allergy c. f. rheumatologic disease – 153 vs. 69 children, and 37 vs. 42 adults – Peanut allergy associated with more disruption of daily activity and impact on family relations in children • Rheumatologic disease associated with more impact than peanut allergy in adults Primeau, Clin Exp All, 2000
 Food allergy quality of life • Quality of life of 20 children with peanut allergy compared with 20 children with IDDM – Self reported lower Qo. L for children with peanut allergy c. f. IDDM – More fear of an adverse event – Anxiety symptoms particularly when eating away from home – More threatened by perceived hazards within the environment Avery, Ped All Imm 2003
Food allergy quality of life • Quality of life of 20 children with peanut allergy compared with 20 children with IDDM – Self reported lower Qo. L for children with peanut allergy c. f. IDDM – More fear of an adverse event – Anxiety symptoms particularly when eating away from home – More threatened by perceived hazards within the environment Avery, Ped All Imm 2003
 Management and Qo. L • 41 peanut / nut allergic children and their mothers • Maternal and child Qo. L and anxiety were not influenced by the severity of previous reactions – Not influenced by sensitised vs allergic – 14 with hospital care, 5 Rx adrenaline • Mother and child reported lower anxiety was prescribed an epinephrine auto-injector (36 of 41 had autoinjector) – Anxiety was not associated with whether the child carried the auto-injector (25 often or always) • Anxiety not associated with whether they strictly avoided “traces” of nuts in foods – 29 who ate “may contain” with better Qo. L than 11 who didn’t Cummings Ped All Imm 2010
Management and Qo. L • 41 peanut / nut allergic children and their mothers • Maternal and child Qo. L and anxiety were not influenced by the severity of previous reactions – Not influenced by sensitised vs allergic – 14 with hospital care, 5 Rx adrenaline • Mother and child reported lower anxiety was prescribed an epinephrine auto-injector (36 of 41 had autoinjector) – Anxiety was not associated with whether the child carried the auto-injector (25 often or always) • Anxiety not associated with whether they strictly avoided “traces” of nuts in foods – 29 who ate “may contain” with better Qo. L than 11 who didn’t Cummings Ped All Imm 2010
 Challenge and Qo. L • 131 egg allergic, 36 sensitised never exposed • Challenge reduced adverse parental concerns – For 6/10 parameters, expectations concerning egg allergy in children who had been challenged were significantly better than those who had never been challenged irrespective of the challenge outcome. • The greater certainty provided by the performance of a food challenge may be a positive outcome in both CP and CN children Kemp Paed All Imm 09
Challenge and Qo. L • 131 egg allergic, 36 sensitised never exposed • Challenge reduced adverse parental concerns – For 6/10 parameters, expectations concerning egg allergy in children who had been challenged were significantly better than those who had never been challenged irrespective of the challenge outcome. • The greater certainty provided by the performance of a food challenge may be a positive outcome in both CP and CN children Kemp Paed All Imm 09
 Education and Qo. L Vickers 1997
Education and Qo. L Vickers 1997
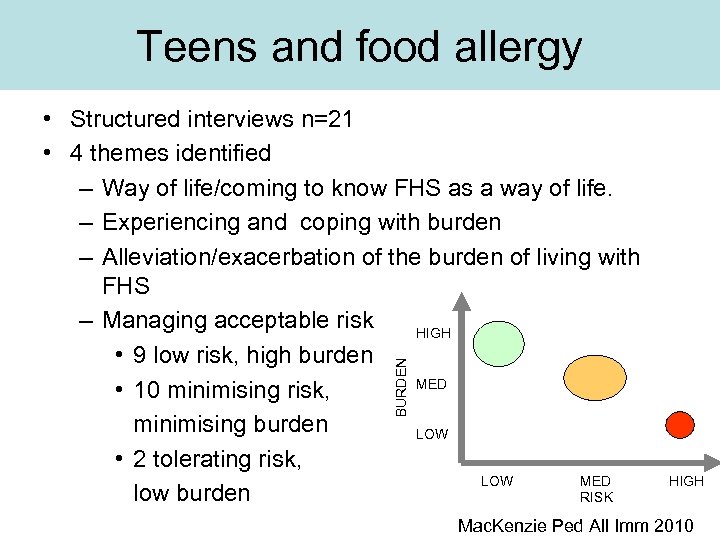 Teens and food allergy BURDEN • Structured interviews n=21 • 4 themes identified – Way of life/coming to know FHS as a way of life. – Experiencing and coping with burden – Alleviation/exacerbation of the burden of living with FHS – Managing acceptable risk HIGH • 9 low risk, high burden MED • 10 minimising risk, minimising burden LOW • 2 tolerating risk, LOW MED low burden RISK HIGH Mac. Kenzie Ped All Imm 2010
Teens and food allergy BURDEN • Structured interviews n=21 • 4 themes identified – Way of life/coming to know FHS as a way of life. – Experiencing and coping with burden – Alleviation/exacerbation of the burden of living with FHS – Managing acceptable risk HIGH • 9 low risk, high burden MED • 10 minimising risk, minimising burden LOW • 2 tolerating risk, LOW MED low burden RISK HIGH Mac. Kenzie Ped All Imm 2010
 Developmental trajectory • Children <8 – Own food is “special” – Confident in parent’s control • Around 8 -9 years – “Special” develops negative connotations – Awareness of uncertainty • Older and more independent – Increasing uncertainty – Reinforced by lack of awareness of others – Awareness of anxiety of parents – “Difference” as isolation Dunn. Galvin Adv Food Nutr Res 2009
Developmental trajectory • Children <8 – Own food is “special” – Confident in parent’s control • Around 8 -9 years – “Special” develops negative connotations – Awareness of uncertainty • Older and more independent – Increasing uncertainty – Reinforced by lack of awareness of others – Awareness of anxiety of parents – “Difference” as isolation Dunn. Galvin Adv Food Nutr Res 2009
 Strategy – avoidance – 40% • Specifically allergen related ↔ generalised of places, people, situations • Generalised related to high levels of anxiety and low levels of self efficacy – Not related to severity previous reactions “It is better to not go to restaurants. . . you never know…the waiters don't know” “I only go to places where I know I am safe” “We wouldn't go to restaurants because they are not safe” “I only go to friends houses who I know for ages. . . its safer that way” Dunn. Galvin Allergy 2009
Strategy – avoidance – 40% • Specifically allergen related ↔ generalised of places, people, situations • Generalised related to high levels of anxiety and low levels of self efficacy – Not related to severity previous reactions “It is better to not go to restaurants. . . you never know…the waiters don't know” “I only go to places where I know I am safe” “We wouldn't go to restaurants because they are not safe” “I only go to friends houses who I know for ages. . . its safer that way” Dunn. Galvin Allergy 2009
 Strategy - minimisation • Minimisation strategies 30% – Rejection of food allergic identity, adopting risky behavior “I just want to be like the other kids…and bringing up about the allergy, that just makes you weird” “Sometimes I forget my pen on purpose; you just got to chance it will be ok…you'd go mad otherwise” “I was sitting in a friends house with a group of guys and they started firing peanuts at me…they didn't know, I don’t tell people but that was a freaky moment” Dunn. Galvin Allergy 2009
Strategy - minimisation • Minimisation strategies 30% – Rejection of food allergic identity, adopting risky behavior “I just want to be like the other kids…and bringing up about the allergy, that just makes you weird” “Sometimes I forget my pen on purpose; you just got to chance it will be ok…you'd go mad otherwise” “I was sitting in a friends house with a group of guys and they started firing peanuts at me…they didn't know, I don’t tell people but that was a freaky moment” Dunn. Galvin Allergy 2009
 Strategy - adaptive • Positive emotional, cognitive or behavioural strategies used to cope with the everyday experience of living with food allergy • Children whose parents encouraged independence and self-management were more likely to describe positive coping strategies “If there's food around, I will be careful, but otherwise I don't think about it” “I’m lucky cause I don't like cake…well if I tried it, I might like it, but I decided I didn't like it” “I always tell people I'm food allergic…its safer that way and then you don't have to keep explaining Dunn. Galvin Allergy 2009
Strategy - adaptive • Positive emotional, cognitive or behavioural strategies used to cope with the everyday experience of living with food allergy • Children whose parents encouraged independence and self-management were more likely to describe positive coping strategies “If there's food around, I will be careful, but otherwise I don't think about it” “I’m lucky cause I don't like cake…well if I tried it, I might like it, but I decided I didn't like it” “I always tell people I'm food allergic…its safer that way and then you don't have to keep explaining Dunn. Galvin Allergy 2009
 Building resilience • Age appropriate strategies – Peanut minimisation in preschools, won’t work by intermediate – Review and adapt with time and developmental progress • Focus on avoiding ingestion – Reactions to touch and inhalation possible but rare • Systemic reactions not reproduced with peanut smell • Education re allergen – Identification – Hidden sources – Following the family rules
Building resilience • Age appropriate strategies – Peanut minimisation in preschools, won’t work by intermediate – Review and adapt with time and developmental progress • Focus on avoiding ingestion – Reactions to touch and inhalation possible but rare • Systemic reactions not reproduced with peanut smell • Education re allergen – Identification – Hidden sources – Following the family rules
 Building resilience • Confidence about – Avoidance strategies • Age appropriate – Child needs to be ready for these to change • Managing uncertainty – What won’t hurt • Recognition about – Reaction signs and symptoms – How to get help – Practice with autoinjector (parents older child)
Building resilience • Confidence about – Avoidance strategies • Age appropriate – Child needs to be ready for these to change • Managing uncertainty – What won’t hurt • Recognition about – Reaction signs and symptoms – How to get help – Practice with autoinjector (parents older child)



