64078421a6303f759ac8fde7e4feae5a.ppt
- Количество слайдов: 52
 Pulmonary Physiology and Lung Function Tests Conor O’Dochartaigh FRACP Teaching 24/10/07
Pulmonary Physiology and Lung Function Tests Conor O’Dochartaigh FRACP Teaching 24/10/07
 Lung Function Testing (PFTs) Spirometry (FV loop spirometry, dynamic lung volumes) Reversibility testing Bronchial challenge testing Static lung volumes (TLC, FRC) Gas Transfer (DLCO, TLCO Transfer factor, KCO, ) Maximal respiratory pressures (Mouth pressures) CPEST (Cardiopulmonary exercise test)
Lung Function Testing (PFTs) Spirometry (FV loop spirometry, dynamic lung volumes) Reversibility testing Bronchial challenge testing Static lung volumes (TLC, FRC) Gas Transfer (DLCO, TLCO Transfer factor, KCO, ) Maximal respiratory pressures (Mouth pressures) CPEST (Cardiopulmonary exercise test)
 General principles Technical factors – operator – patient within test repeatability – confounding factors Quality control – between test repeatability Appropriate reference values
General principles Technical factors – operator – patient within test repeatability – confounding factors Quality control – between test repeatability Appropriate reference values
 Spirometry Measures the ability to move air rapidly – Depends on nervous system, musc skel, skin + connective tissue, lungs, airways, inhaled gas
Spirometry Measures the ability to move air rapidly – Depends on nervous system, musc skel, skin + connective tissue, lungs, airways, inhaled gas
 How is the test done Apparatus – true spirometers - volume & time – pneumotach, vane & hotwire anenometers flow Method – Full inspiration, forced maximal expiration – Minimum 3 technically acceptable attempts – within 5% repeatability FEV 1 and FVC Slow Vital Capacity may also be checked
How is the test done Apparatus – true spirometers - volume & time – pneumotach, vane & hotwire anenometers flow Method – Full inspiration, forced maximal expiration – Minimum 3 technically acceptable attempts – within 5% repeatability FEV 1 and FVC Slow Vital Capacity may also be checked
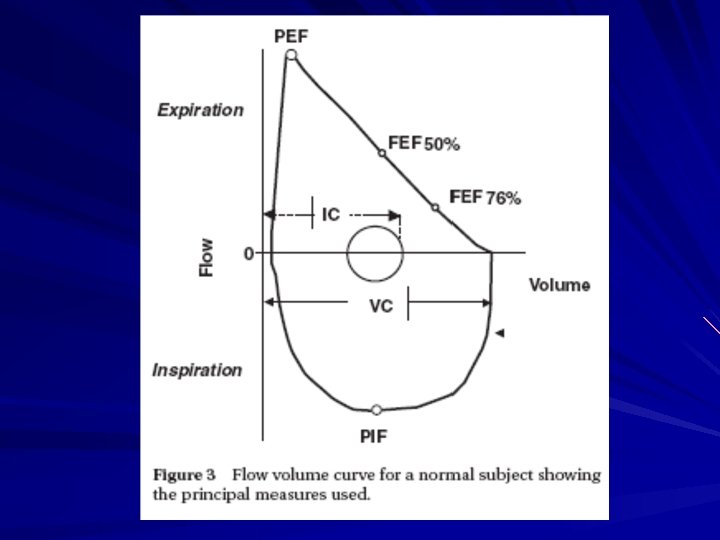
 Data generated Volume time curve (spirogram) – FEV 1, FVC, Ratio Flow volume loop – Peak flow – FVC – FEF 25 -75% – MEF 75, 50, and 25 – Inspiratory flow data
Data generated Volume time curve (spirogram) – FEV 1, FVC, Ratio Flow volume loop – Peak flow – FVC – FEF 25 -75% – MEF 75, 50, and 25 – Inspiratory flow data
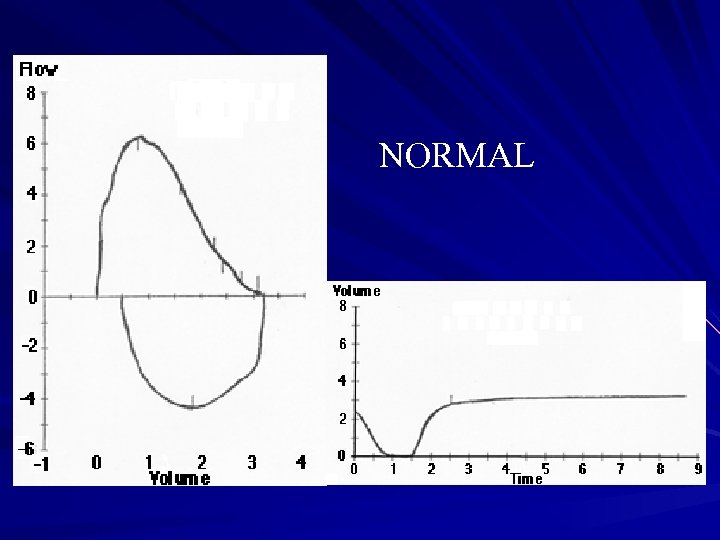 NORMAL
NORMAL
 Spirometry interpretation Obstructive v. Restrictive Mid flow obstruction Shape of the FV loop – Obstruction v. restriction – Fixed large airway obstruction – Variable airway obstruction Extrathoracic Intrathoracic
Spirometry interpretation Obstructive v. Restrictive Mid flow obstruction Shape of the FV loop – Obstruction v. restriction – Fixed large airway obstruction – Variable airway obstruction Extrathoracic Intrathoracic
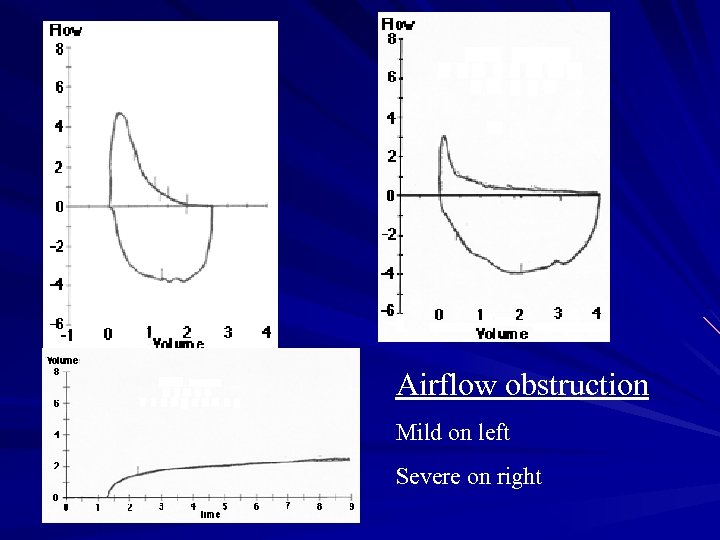 Airflow obstruction Mild on left Severe on right
Airflow obstruction Mild on left Severe on right
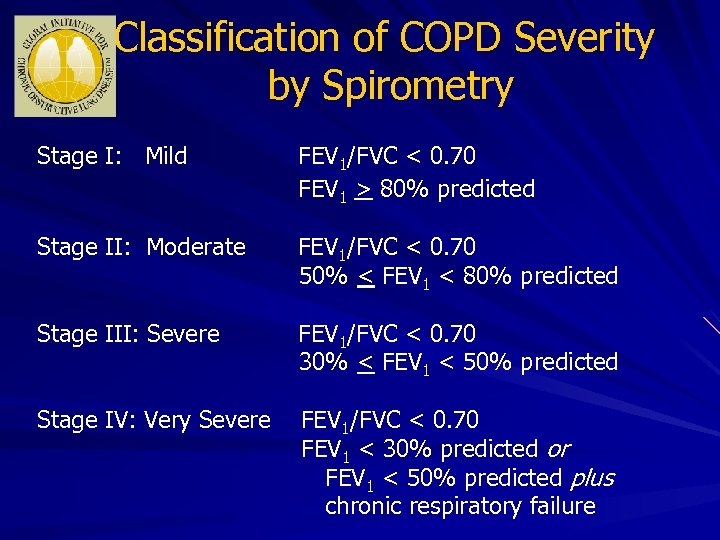 Classification of COPD Severity by Spirometry Stage I: Mild FEV 1/FVC < 0. 70 FEV 1 > 80% predicted Stage II: Moderate FEV 1/FVC < 0. 70 50% < FEV 1 < 80% predicted Stage III: Severe FEV 1/FVC < 0. 70 30% < FEV 1 < 50% predicted Stage IV: Very Severe FEV 1/FVC < 0. 70 FEV 1 < 30% predicted or FEV 1 < 50% predicted plus chronic respiratory failure
Classification of COPD Severity by Spirometry Stage I: Mild FEV 1/FVC < 0. 70 FEV 1 > 80% predicted Stage II: Moderate FEV 1/FVC < 0. 70 50% < FEV 1 < 80% predicted Stage III: Severe FEV 1/FVC < 0. 70 30% < FEV 1 < 50% predicted Stage IV: Very Severe FEV 1/FVC < 0. 70 FEV 1 < 30% predicted or FEV 1 < 50% predicted plus chronic respiratory failure
 True or False Spirometry showing FEV 1 < 80% of predicted and FEV 1/FVC ratio <70% is diagnostic of COPD
True or False Spirometry showing FEV 1 < 80% of predicted and FEV 1/FVC ratio <70% is diagnostic of COPD
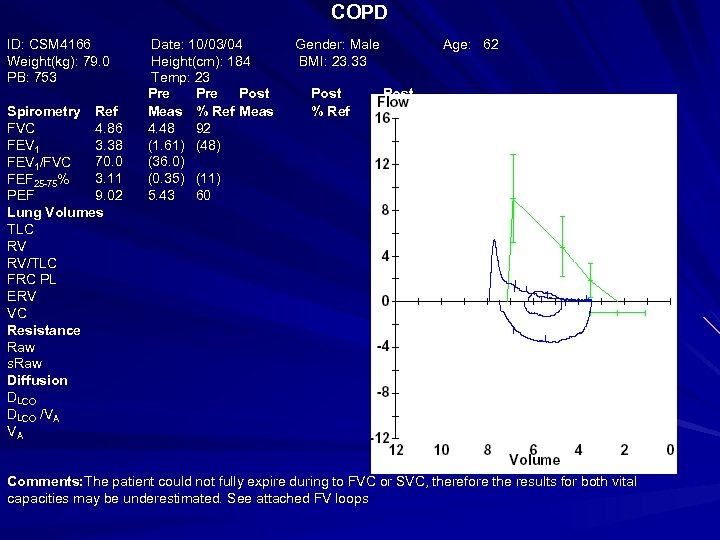 COPD ID: CSM 4166 Weight(kg): 79. 0 PB: 753 Spirometry Ref 4. 86 FVC 3. 38 FEV 1 70. 0 FEV 1/FVC 3. 11 FEF 25 -75% 9. 02 PEF Lung Volumes TLC RV RV/TLC FRC PL ERV VC Resistance Raw s. Raw Diffusion DLCO /VA VA Date: 10/03/04 Height(cm): 184 Temp: 23 Pre Post Meas % Ref Meas 4. 48 92 (1. 61) (48) (36. 0) (0. 35) (11) 5. 43 60 Gender: Male BMI: 23. 33 Post % Ref Age: 62 Post % Chg Comments: The patient could not fully expire during to FVC or SVC, therefore the results for both vital capacities may be underestimated. See attached FV loops
COPD ID: CSM 4166 Weight(kg): 79. 0 PB: 753 Spirometry Ref 4. 86 FVC 3. 38 FEV 1 70. 0 FEV 1/FVC 3. 11 FEF 25 -75% 9. 02 PEF Lung Volumes TLC RV RV/TLC FRC PL ERV VC Resistance Raw s. Raw Diffusion DLCO /VA VA Date: 10/03/04 Height(cm): 184 Temp: 23 Pre Post Meas % Ref Meas 4. 48 92 (1. 61) (48) (36. 0) (0. 35) (11) 5. 43 60 Gender: Male BMI: 23. 33 Post % Ref Age: 62 Post % Chg Comments: The patient could not fully expire during to FVC or SVC, therefore the results for both vital capacities may be underestimated. See attached FV loops
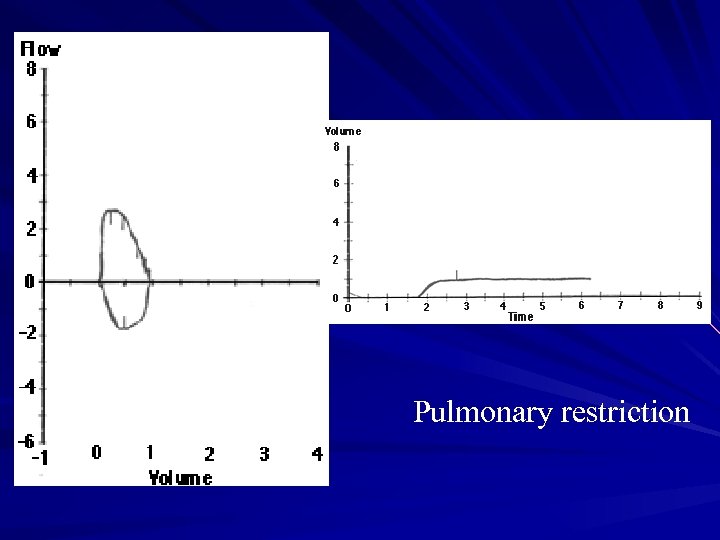 Pulmonary restriction
Pulmonary restriction
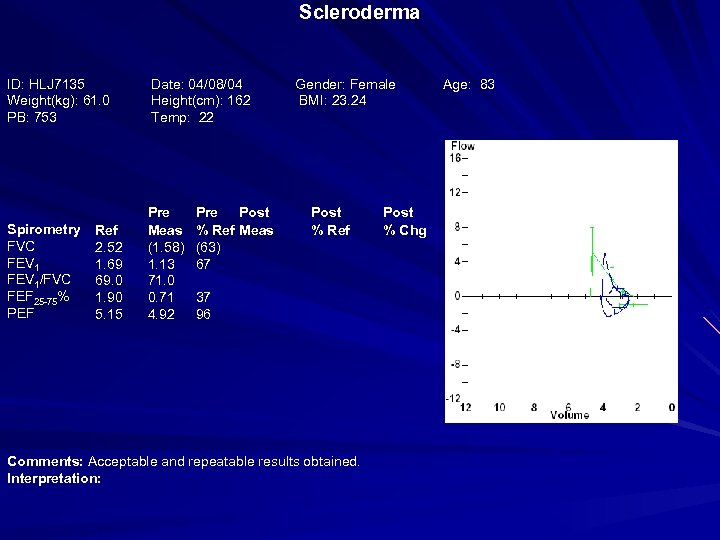 Scleroderma ID: HLJ 7135 Weight(kg): 61. 0 PB: 753 Date: 04/08/04 Height(cm): 162 Temp: 22 Spirometry FVC FEV 1/FVC FEF 25 -75% PEF Pre Meas (1. 58) 1. 13 71. 0 0. 71 4. 92 Ref 2. 52 1. 69 69. 0 1. 90 5. 15 Pre Post % Ref Meas (63) 67 Gender: Female BMI: 23. 24 Post % Ref 37 96 Comments: Acceptable and repeatable results obtained. Interpretation: Post % Chg Age: 83
Scleroderma ID: HLJ 7135 Weight(kg): 61. 0 PB: 753 Date: 04/08/04 Height(cm): 162 Temp: 22 Spirometry FVC FEV 1/FVC FEF 25 -75% PEF Pre Meas (1. 58) 1. 13 71. 0 0. 71 4. 92 Ref 2. 52 1. 69 69. 0 1. 90 5. 15 Pre Post % Ref Meas (63) 67 Gender: Female BMI: 23. 24 Post % Ref 37 96 Comments: Acceptable and repeatable results obtained. Interpretation: Post % Chg Age: 83
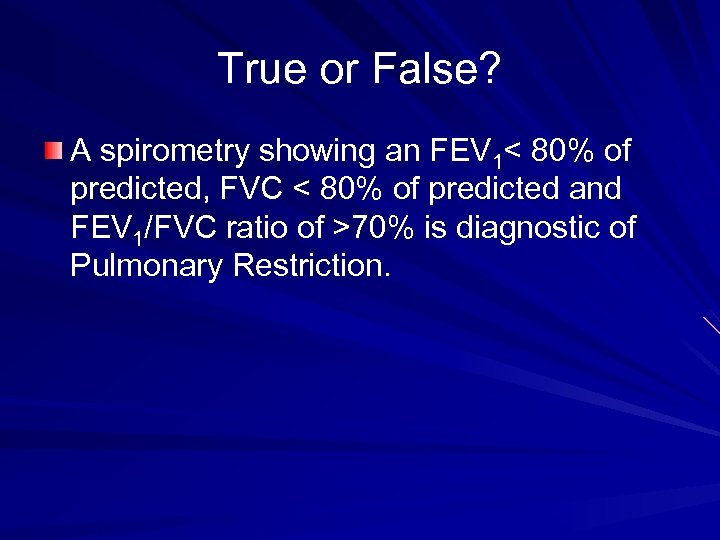 True or False? A spirometry showing an FEV 1< 80% of predicted, FVC < 80% of predicted and FEV 1/FVC ratio of >70% is diagnostic of Pulmonary Restriction.
True or False? A spirometry showing an FEV 1< 80% of predicted, FVC < 80% of predicted and FEV 1/FVC ratio of >70% is diagnostic of Pulmonary Restriction.
 Large Airway obstruction Tracheal – Fixed obstruction – expiratory and inspiratory limitation – Variable obstruction Inspiratory limitation indicates extrathoracic obstruction Expiratory limitation indictaes intrathoracic obstruction
Large Airway obstruction Tracheal – Fixed obstruction – expiratory and inspiratory limitation – Variable obstruction Inspiratory limitation indicates extrathoracic obstruction Expiratory limitation indictaes intrathoracic obstruction
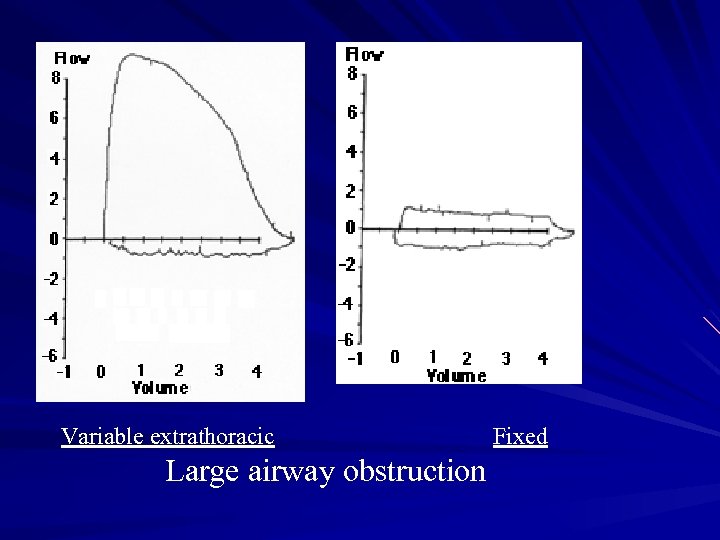 Variable extrathoracic Large airway obstruction Fixed
Variable extrathoracic Large airway obstruction Fixed
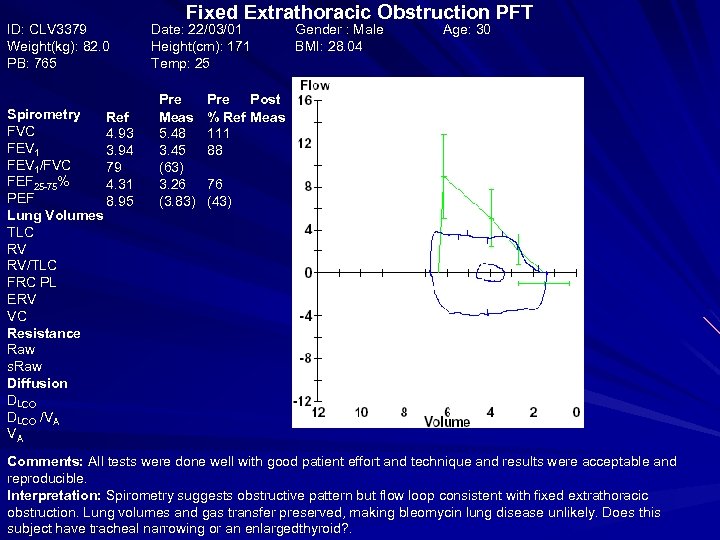 ID: CLV 3379 Weight(kg): 82. 0 PB: 765 Spirometry Ref FVC 4. 93 FEV 1 3. 94 FEV 1/FVC 79 FEF 25 -75% 4. 31 PEF 8. 95 Lung Volumes TLC RV RV/TLC FRC PL ERV VC Resistance Raw s. Raw Diffusion DLCO /VA VA Fixed Extrathoracic Obstruction PFT Date: 22/03/01 Height(cm): 171 Temp: 25 Pre Meas 5. 48 3. 45 (63) 3. 26 (3. 83) Pre Post % Ref Meas 111 88 Gender : Male BMI: 28. 04 Post % Ref Age: 30 Post % Chg 76 (43) Comments: All tests were done well with good patient effort and technique and results were acceptable and reproducible. Interpretation: Spirometry suggests obstructive pattern but flow loop consistent with fixed extrathoracic obstruction. Lung volumes and gas transfer preserved, making bleomycin lung disease unlikely. Does this subject have tracheal narrowing or an enlargedthyroid? .
ID: CLV 3379 Weight(kg): 82. 0 PB: 765 Spirometry Ref FVC 4. 93 FEV 1 3. 94 FEV 1/FVC 79 FEF 25 -75% 4. 31 PEF 8. 95 Lung Volumes TLC RV RV/TLC FRC PL ERV VC Resistance Raw s. Raw Diffusion DLCO /VA VA Fixed Extrathoracic Obstruction PFT Date: 22/03/01 Height(cm): 171 Temp: 25 Pre Meas 5. 48 3. 45 (63) 3. 26 (3. 83) Pre Post % Ref Meas 111 88 Gender : Male BMI: 28. 04 Post % Ref Age: 30 Post % Chg 76 (43) Comments: All tests were done well with good patient effort and technique and results were acceptable and reproducible. Interpretation: Spirometry suggests obstructive pattern but flow loop consistent with fixed extrathoracic obstruction. Lung volumes and gas transfer preserved, making bleomycin lung disease unlikely. Does this subject have tracheal narrowing or an enlargedthyroid? .
 Reversibility How? – Off inhalers – Spiro – Inhaled bronchodilator – Check spiro again Data – Absolute and %predicted pre&post FEV 1 & FVC
Reversibility How? – Off inhalers – Spiro – Inhaled bronchodilator – Check spiro again Data – Absolute and %predicted pre&post FEV 1 & FVC
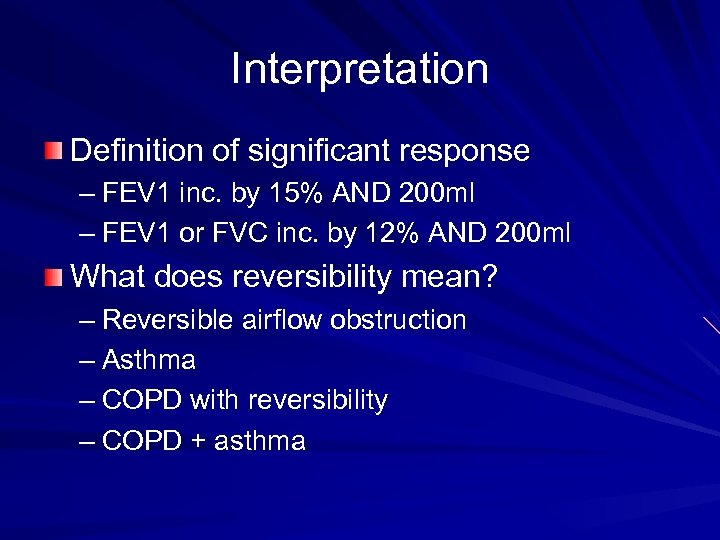 Interpretation Definition of significant response – FEV 1 inc. by 15% AND 200 ml – FEV 1 or FVC inc. by 12% AND 200 ml What does reversibility mean? – Reversible airflow obstruction – Asthma – COPD with reversibility – COPD + asthma
Interpretation Definition of significant response – FEV 1 inc. by 15% AND 200 ml – FEV 1 or FVC inc. by 12% AND 200 ml What does reversibility mean? – Reversible airflow obstruction – Asthma – COPD with reversibility – COPD + asthma
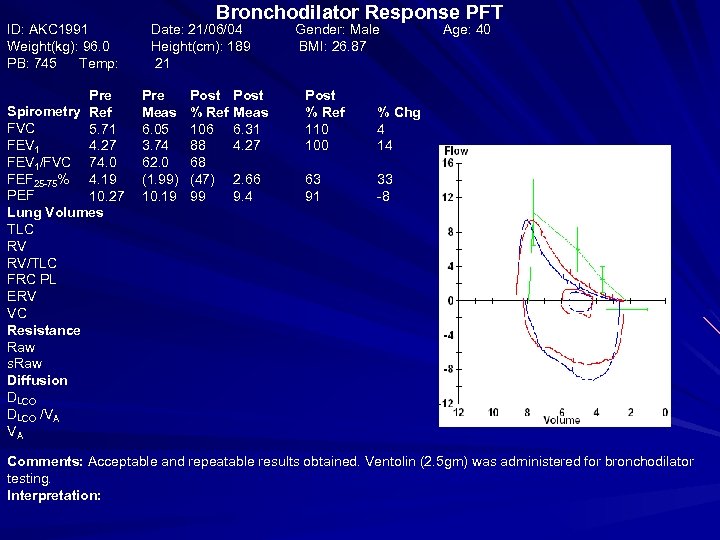 ID: AKC 1991 Weight(kg): 96. 0 PB: 745 Temp: Pre Spirometry Ref FVC 5. 71 FEV 1 4. 27 FEV 1/FVC 74. 0 FEF 25 -75% 4. 19 PEF 10. 27 Lung Volumes TLC RV RV/TLC FRC PL ERV VC Resistance Raw s. Raw Diffusion DLCO /VA VA Bronchodilator Response PFT Date: 21/06/04 Height(cm): 189 21 Pre Meas 6. 05 3. 74 62. 0 (1. 99) 10. 19 Post % Ref 106 88 68 (47) 99 Gender: Male BMI: 26. 87 Post Meas 6. 31 4. 27 Post % Ref 110 100 % Chg 4 14 2. 66 9. 4 63 91 Age: 40 33 -8 Comments: Acceptable and repeatable results obtained. Ventolin (2. 5 gm) was administered for bronchodilator testing. Interpretation:
ID: AKC 1991 Weight(kg): 96. 0 PB: 745 Temp: Pre Spirometry Ref FVC 5. 71 FEV 1 4. 27 FEV 1/FVC 74. 0 FEF 25 -75% 4. 19 PEF 10. 27 Lung Volumes TLC RV RV/TLC FRC PL ERV VC Resistance Raw s. Raw Diffusion DLCO /VA VA Bronchodilator Response PFT Date: 21/06/04 Height(cm): 189 21 Pre Meas 6. 05 3. 74 62. 0 (1. 99) 10. 19 Post % Ref 106 88 68 (47) 99 Gender: Male BMI: 26. 87 Post Meas 6. 31 4. 27 Post % Ref 110 100 % Chg 4 14 2. 66 9. 4 63 91 Age: 40 33 -8 Comments: Acceptable and repeatable results obtained. Ventolin (2. 5 gm) was administered for bronchodilator testing. Interpretation:
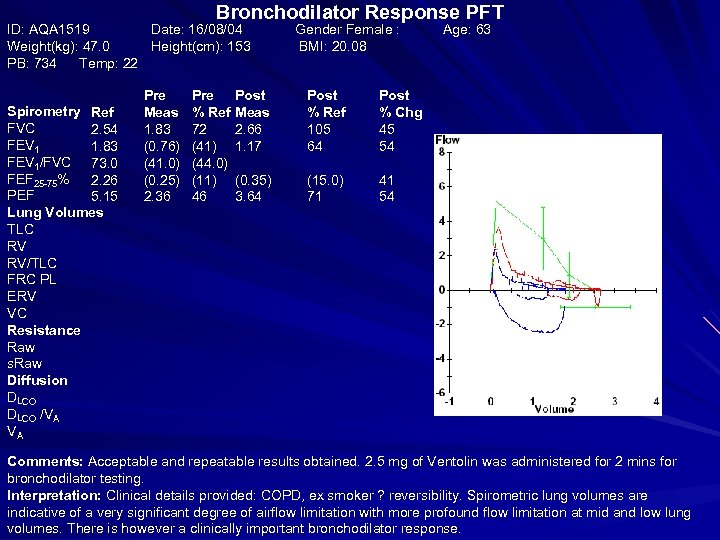 Bronchodilator Response PFT ID: AQA 1519 Date: 16/08/04 Weight(kg): 47. 0 Height(cm): 153 PB: 734 Temp: 22 Spirometry Ref FVC 2. 54 FEV 1 1. 83 FEV 1/FVC 73. 0 FEF 25 -75% 2. 26 PEF 5. 15 Lung Volumes TLC RV RV/TLC FRC PL ERV VC Resistance Raw s. Raw Diffusion DLCO /VA VA Pre Meas 1. 83 (0. 76) (41. 0) (0. 25) 2. 36 Pre % Ref 72 (41) (44. 0) (11) 46 Gender Female : BMI: 20. 08 Post Meas 2. 66 1. 17 Post % Ref 105 64 Post % Chg 45 54 (0. 35) 3. 64 (15. 0) 71 Age: 63 41 54 Comments: Acceptable and repeatable results obtained. 2. 5 mg of Ventolin was administered for 2 mins for bronchodilator testing. Interpretation: Clinical details provided: COPD, ex smoker ? reversibility. Spirometric lung volumes are indicative of a very significant degree of airflow limitation with more profound flow limitation at mid and low lung volumes. There is however a clinically important bronchodilator response.
Bronchodilator Response PFT ID: AQA 1519 Date: 16/08/04 Weight(kg): 47. 0 Height(cm): 153 PB: 734 Temp: 22 Spirometry Ref FVC 2. 54 FEV 1 1. 83 FEV 1/FVC 73. 0 FEF 25 -75% 2. 26 PEF 5. 15 Lung Volumes TLC RV RV/TLC FRC PL ERV VC Resistance Raw s. Raw Diffusion DLCO /VA VA Pre Meas 1. 83 (0. 76) (41. 0) (0. 25) 2. 36 Pre % Ref 72 (41) (44. 0) (11) 46 Gender Female : BMI: 20. 08 Post Meas 2. 66 1. 17 Post % Ref 105 64 Post % Chg 45 54 (0. 35) 3. 64 (15. 0) 71 Age: 63 41 54 Comments: Acceptable and repeatable results obtained. 2. 5 mg of Ventolin was administered for 2 mins for bronchodilator testing. Interpretation: Clinical details provided: COPD, ex smoker ? reversibility. Spirometric lung volumes are indicative of a very significant degree of airflow limitation with more profound flow limitation at mid and low lung volumes. There is however a clinically important bronchodilator response.
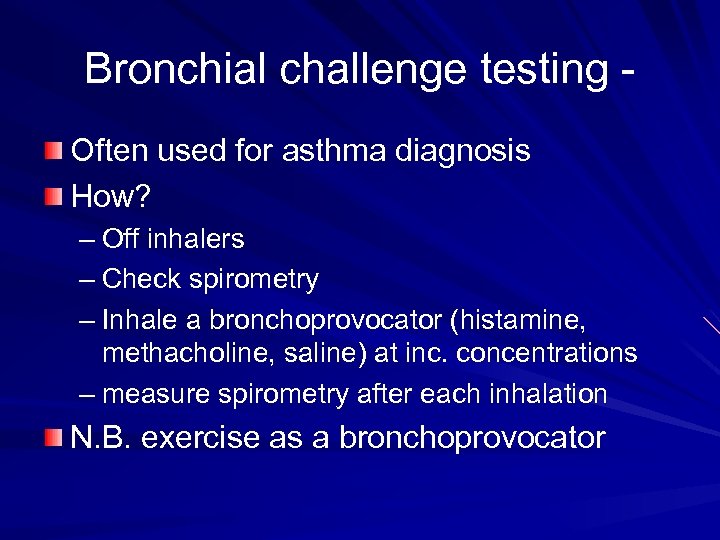 Bronchial challenge testing Often used for asthma diagnosis How? – Off inhalers – Check spirometry – Inhale a bronchoprovocator (histamine, methacholine, saline) at inc. concentrations – measure spirometry after each inhalation N. B. exercise as a bronchoprovocator
Bronchial challenge testing Often used for asthma diagnosis How? – Off inhalers – Check spirometry – Inhale a bronchoprovocator (histamine, methacholine, saline) at inc. concentrations – measure spirometry after each inhalation N. B. exercise as a bronchoprovocator
 Bronchial challenge testing Data PD 20 = ‘Provocative Dose’ required to produce a 20% drop in FEV 1 – Histamine + if <4 micromol PC 20 = ‘Provocative Concentration’ required to produce a 20% drop in FEV 1 – Histamine + if <8 mg/ml PC 20/PD 20 also used for Methacholine Hypertonic saline
Bronchial challenge testing Data PD 20 = ‘Provocative Dose’ required to produce a 20% drop in FEV 1 – Histamine + if <4 micromol PC 20 = ‘Provocative Concentration’ required to produce a 20% drop in FEV 1 – Histamine + if <8 mg/ml PC 20/PD 20 also used for Methacholine Hypertonic saline
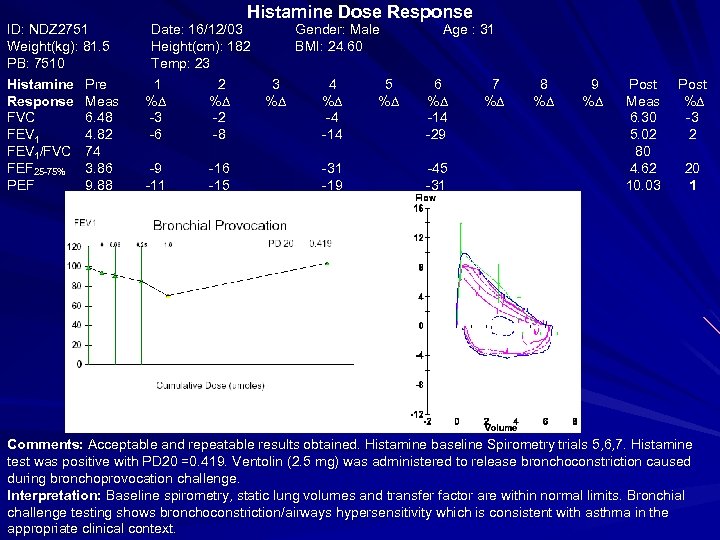 ID: NDZ 2751 Weight(kg): 81. 5 PB: 7510 Histamine Response FVC FEV 1/FVC FEF 25 -75% PEF Pre Meas 6. 48 4. 82 74 3. 86 9. 88 Histamine Dose Response Date: 16/12/03 Height(cm): 182 Temp: 23 1 % -3 -6 2 % -2 -8 -9 -11 -16 -15 Gender: Male BMI: 24. 60 3 % 4 % -4 -14 -31 -19 5 % Age : 31 6 % -14 -29 -45 -31 7 % 8 % 9 % Post Meas 6. 30 5. 02 80 4. 62 10. 03 Post % -3 2 20 1 Comments: Acceptable and repeatable results obtained. Histamine baseline Spirometry trials 5, 6, 7. Histamine test was positive with PD 20 =0. 419. Ventolin (2. 5 mg) was administered to release bronchoconstriction caused during bronchoprovocation challenge. Interpretation: Baseline spirometry, static lung volumes and transfer factor are within normal limits. Bronchial challenge testing shows bronchoconstriction/airways hypersensitivity which is consistent with asthma in the appropriate clinical context.
ID: NDZ 2751 Weight(kg): 81. 5 PB: 7510 Histamine Response FVC FEV 1/FVC FEF 25 -75% PEF Pre Meas 6. 48 4. 82 74 3. 86 9. 88 Histamine Dose Response Date: 16/12/03 Height(cm): 182 Temp: 23 1 % -3 -6 2 % -2 -8 -9 -11 -16 -15 Gender: Male BMI: 24. 60 3 % 4 % -4 -14 -31 -19 5 % Age : 31 6 % -14 -29 -45 -31 7 % 8 % 9 % Post Meas 6. 30 5. 02 80 4. 62 10. 03 Post % -3 2 20 1 Comments: Acceptable and repeatable results obtained. Histamine baseline Spirometry trials 5, 6, 7. Histamine test was positive with PD 20 =0. 419. Ventolin (2. 5 mg) was administered to release bronchoconstriction caused during bronchoprovocation challenge. Interpretation: Baseline spirometry, static lung volumes and transfer factor are within normal limits. Bronchial challenge testing shows bronchoconstriction/airways hypersensitivity which is consistent with asthma in the appropriate clinical context.
 Bronchial challenge interpretation Threshold for positive may vary centre to centre Indicates ‘Bronchial hyperresponsiveness’ Negative test virtually excludes asthma False positives post-infection
Bronchial challenge interpretation Threshold for positive may vary centre to centre Indicates ‘Bronchial hyperresponsiveness’ Negative test virtually excludes asthma False positives post-infection
 Static lung volumes Why? – Measure residual volume (and therefore TLC) How? – Measure the FRC – Plethysmography or Gas dilution – Plethysmography (bodybox) preferred measures poorly ventilated airspaces 2 types - volume-displacement & volume-constant
Static lung volumes Why? – Measure residual volume (and therefore TLC) How? – Measure the FRC – Plethysmography or Gas dilution – Plethysmography (bodybox) preferred measures poorly ventilated airspaces 2 types - volume-displacement & volume-constant
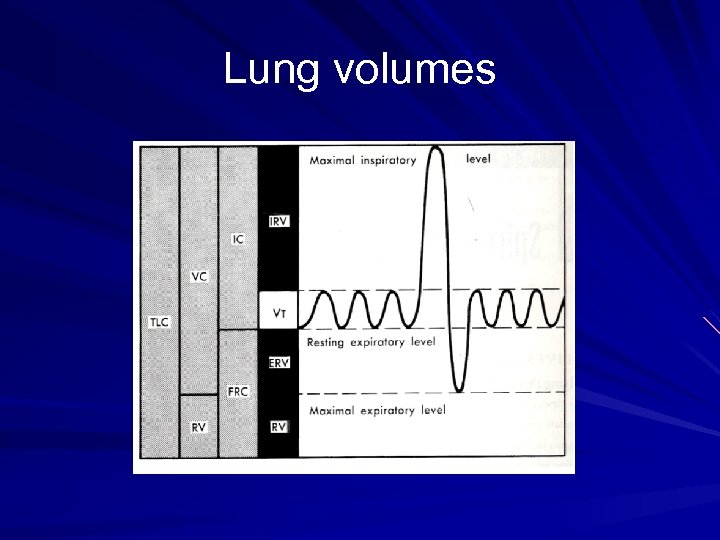 Lung volumes
Lung volumes
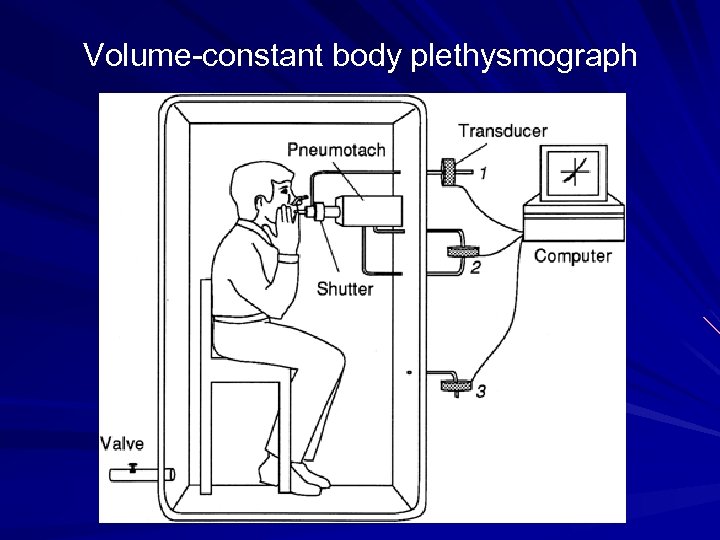 Volume-constant body plethysmograph
Volume-constant body plethysmograph
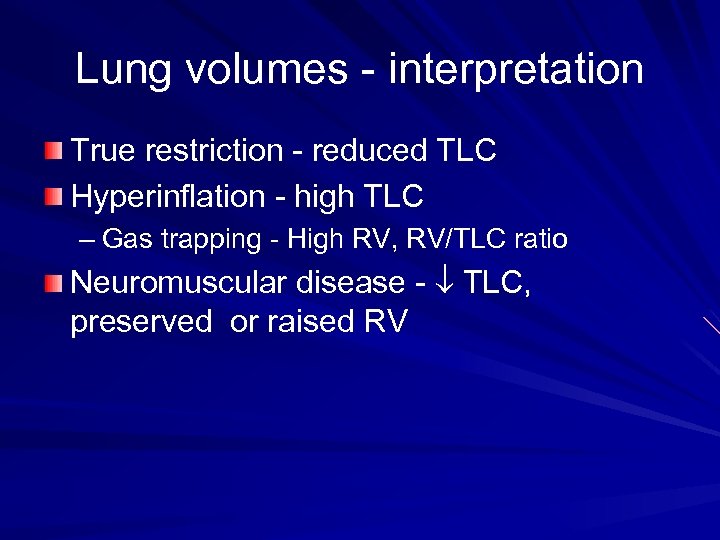 Lung volumes - interpretation True restriction - reduced TLC Hyperinflation - high TLC – Gas trapping - High RV, RV/TLC ratio Neuromuscular disease - TLC, preserved or raised RV
Lung volumes - interpretation True restriction - reduced TLC Hyperinflation - high TLC – Gas trapping - High RV, RV/TLC ratio Neuromuscular disease - TLC, preserved or raised RV
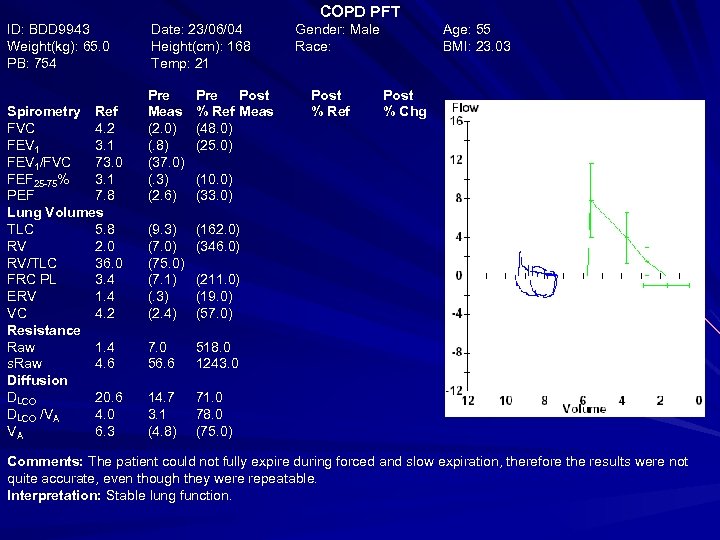 COPD PFT ID: BDD 9943 Weight(kg): 65. 0 PB: 754 Spirometry Ref FVC 4. 2 FEV 1 3. 1 FEV 1/FVC 73. 0 FEF 25 -75% 3. 1 PEF 7. 8 Lung Volumes TLC 5. 8 RV 2. 0 RV/TLC 36. 0 FRC PL 3. 4 ERV 1. 4 VC 4. 2 Resistance Raw 1. 4 s. Raw 4. 6 Diffusion DLCO 20. 6 DLCO /VA 4. 0 VA 6. 3 Date: 23/06/04 Height(cm): 168 Temp: 21 Pre Meas (2. 0) (. 8) (37. 0) (. 3) (2. 6) Pre Post % Ref Meas (48. 0) (25. 0) (9. 3) (7. 0) (75. 0) (7. 1) (. 3) (2. 4) 518. 0 1243. 0 14. 7 3. 1 (4. 8) Post % Ref Age: 55 BMI: 23. 03 (162. 0) (346. 0) 7. 0 56. 6 Gender: Male Race: Post % Chg 71. 0 78. 0 (75. 0) (10. 0) (33. 0) (211. 0) (19. 0) (57. 0) Comments: The patient could not fully expire during forced and slow expiration, therefore the results were not quite accurate, even though they were repeatable. Interpretation: Stable lung function.
COPD PFT ID: BDD 9943 Weight(kg): 65. 0 PB: 754 Spirometry Ref FVC 4. 2 FEV 1 3. 1 FEV 1/FVC 73. 0 FEF 25 -75% 3. 1 PEF 7. 8 Lung Volumes TLC 5. 8 RV 2. 0 RV/TLC 36. 0 FRC PL 3. 4 ERV 1. 4 VC 4. 2 Resistance Raw 1. 4 s. Raw 4. 6 Diffusion DLCO 20. 6 DLCO /VA 4. 0 VA 6. 3 Date: 23/06/04 Height(cm): 168 Temp: 21 Pre Meas (2. 0) (. 8) (37. 0) (. 3) (2. 6) Pre Post % Ref Meas (48. 0) (25. 0) (9. 3) (7. 0) (75. 0) (7. 1) (. 3) (2. 4) 518. 0 1243. 0 14. 7 3. 1 (4. 8) Post % Ref Age: 55 BMI: 23. 03 (162. 0) (346. 0) 7. 0 56. 6 Gender: Male Race: Post % Chg 71. 0 78. 0 (75. 0) (10. 0) (33. 0) (211. 0) (19. 0) (57. 0) Comments: The patient could not fully expire during forced and slow expiration, therefore the results were not quite accurate, even though they were repeatable. Interpretation: Stable lung function.
 True or False Transfer factor is a specific measure of gas transfer at the alveolo-capillary membrane
True or False Transfer factor is a specific measure of gas transfer at the alveolo-capillary membrane
 Transfer factor Gas exchange by the lung depends on: 1. Ventilation of the airways and some air spaces by bulk flow of gas; 2. Mixing and diffusion of gases in the alveolar ducts, air sacs and alveoli; 3. Transfer of gases across the gaseous to liquid interface of the alveolar membrane; 4. Mixing and diffusion in the lung parenchyma and alveolar capillary plasma; 5. Chemical reaction with constituents of blood; 6. Circulation of blood between the pulmonary and systemic vascular beds.
Transfer factor Gas exchange by the lung depends on: 1. Ventilation of the airways and some air spaces by bulk flow of gas; 2. Mixing and diffusion of gases in the alveolar ducts, air sacs and alveoli; 3. Transfer of gases across the gaseous to liquid interface of the alveolar membrane; 4. Mixing and diffusion in the lung parenchyma and alveolar capillary plasma; 5. Chemical reaction with constituents of blood; 6. Circulation of blood between the pulmonary and systemic vascular beds.
 Transfer factor – How? Inhale to TLC a gas mix containing known concentrations of CO & He Hold breath 10 sec Exhale – Discard dead space – Collect ‘alveolar’ gas Use He dilution to calculate VA & starting Alveolar CO
Transfer factor – How? Inhale to TLC a gas mix containing known concentrations of CO & He Hold breath 10 sec Exhale – Discard dead space – Collect ‘alveolar’ gas Use He dilution to calculate VA & starting Alveolar CO
 DLCO – Data generated Then DLCO is calculated from the difference between ‘starting’ CO conc. , and CO conc. after 10 sec in contact with alveoli Expressed in ml/mm. Hg/min VA = TLC by single breath helium dilution DLCO/VA = transfer coefficient (KCO)
DLCO – Data generated Then DLCO is calculated from the difference between ‘starting’ CO conc. , and CO conc. after 10 sec in contact with alveoli Expressed in ml/mm. Hg/min VA = TLC by single breath helium dilution DLCO/VA = transfer coefficient (KCO)
 DLCO - interpretation DLCO ↓ by: – Pulmonary vascular diseases – Conditions affecting alveoli – Cardiac diseases – Anaemia – Pregnancy – Recent smoking
DLCO - interpretation DLCO ↓ by: – Pulmonary vascular diseases – Conditions affecting alveoli – Cardiac diseases – Anaemia – Pregnancy – Recent smoking
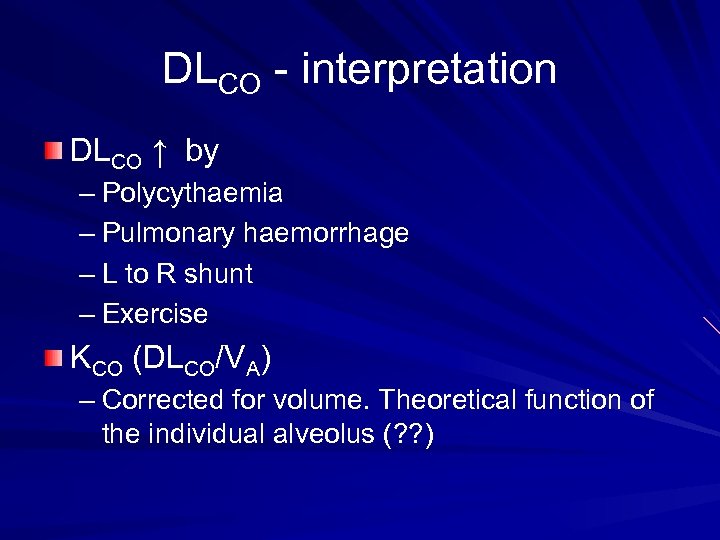 DLCO - interpretation DLCO ↑ by – Polycythaemia – Pulmonary haemorrhage – L to R shunt – Exercise KCO (DLCO/VA) – Corrected for volume. Theoretical function of the individual alveolus (? ? )
DLCO - interpretation DLCO ↑ by – Polycythaemia – Pulmonary haemorrhage – L to R shunt – Exercise KCO (DLCO/VA) – Corrected for volume. Theoretical function of the individual alveolus (? ? )
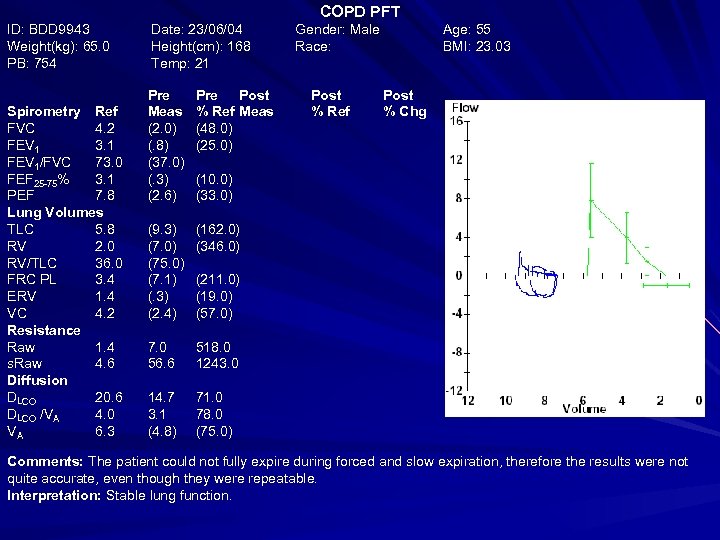 COPD PFT ID: BDD 9943 Weight(kg): 65. 0 PB: 754 Spirometry Ref FVC 4. 2 FEV 1 3. 1 FEV 1/FVC 73. 0 FEF 25 -75% 3. 1 PEF 7. 8 Lung Volumes TLC 5. 8 RV 2. 0 RV/TLC 36. 0 FRC PL 3. 4 ERV 1. 4 VC 4. 2 Resistance Raw 1. 4 s. Raw 4. 6 Diffusion DLCO 20. 6 DLCO /VA 4. 0 VA 6. 3 Date: 23/06/04 Height(cm): 168 Temp: 21 Pre Meas (2. 0) (. 8) (37. 0) (. 3) (2. 6) Pre Post % Ref Meas (48. 0) (25. 0) (9. 3) (7. 0) (75. 0) (7. 1) (. 3) (2. 4) 518. 0 1243. 0 14. 7 3. 1 (4. 8) Post % Ref Age: 55 BMI: 23. 03 (162. 0) (346. 0) 7. 0 56. 6 Gender: Male Race: Post % Chg 71. 0 78. 0 (75. 0) (10. 0) (33. 0) (211. 0) (19. 0) (57. 0) Comments: The patient could not fully expire during forced and slow expiration, therefore the results were not quite accurate, even though they were repeatable. Interpretation: Stable lung function.
COPD PFT ID: BDD 9943 Weight(kg): 65. 0 PB: 754 Spirometry Ref FVC 4. 2 FEV 1 3. 1 FEV 1/FVC 73. 0 FEF 25 -75% 3. 1 PEF 7. 8 Lung Volumes TLC 5. 8 RV 2. 0 RV/TLC 36. 0 FRC PL 3. 4 ERV 1. 4 VC 4. 2 Resistance Raw 1. 4 s. Raw 4. 6 Diffusion DLCO 20. 6 DLCO /VA 4. 0 VA 6. 3 Date: 23/06/04 Height(cm): 168 Temp: 21 Pre Meas (2. 0) (. 8) (37. 0) (. 3) (2. 6) Pre Post % Ref Meas (48. 0) (25. 0) (9. 3) (7. 0) (75. 0) (7. 1) (. 3) (2. 4) 518. 0 1243. 0 14. 7 3. 1 (4. 8) Post % Ref Age: 55 BMI: 23. 03 (162. 0) (346. 0) 7. 0 56. 6 Gender: Male Race: Post % Chg 71. 0 78. 0 (75. 0) (10. 0) (33. 0) (211. 0) (19. 0) (57. 0) Comments: The patient could not fully expire during forced and slow expiration, therefore the results were not quite accurate, even though they were repeatable. Interpretation: Stable lung function.
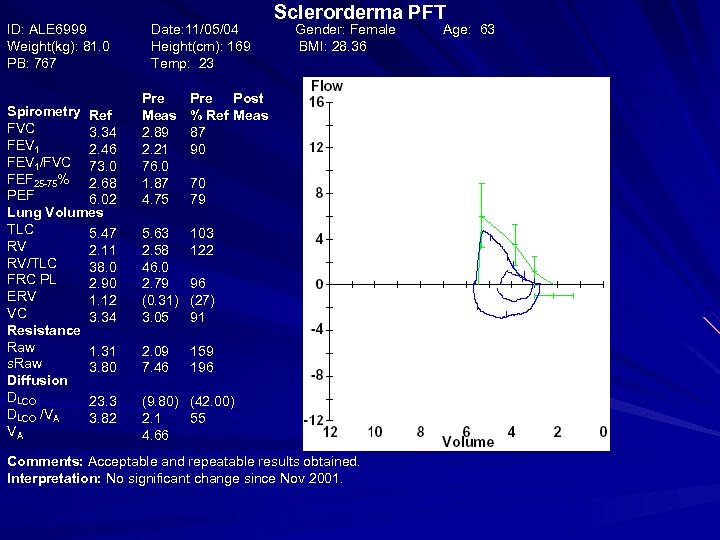 ID: ALE 6999 Weight(kg): 81. 0 PB: 767 Spirometry Ref FVC 3. 34 FEV 1 2. 46 FEV 1/FVC 73. 0 FEF 25 -75% 2. 68 PEF 6. 02 Lung Volumes TLC 5. 47 RV 2. 11 RV/TLC 38. 0 FRC PL 2. 90 ERV 1. 12 VC 3. 34 Resistance Raw 1. 31 s. Raw 3. 80 Diffusion DLCO 23. 3 DLCO /VA 3. 82 VA Date: 11/05/04 Height(cm): 169 Temp: 23 Pre Meas 2. 89 2. 21 76. 0 1. 87 4. 75 Pre Post % Ref Meas 87 90 5. 63 2. 58 46. 0 2. 79 (0. 31) 3. 05 Gender: Female BMI: 28. 36 103 122 2. 09 7. 46 Sclerorderma PFT Post % Ref 159 196 70 79 96 (27) 91 (9. 80) (42. 00) 2. 1 55 4. 66 Comments: Acceptable and repeatable results obtained. Interpretation: No significant change since Nov 2001. Post % Chg Age: 63
ID: ALE 6999 Weight(kg): 81. 0 PB: 767 Spirometry Ref FVC 3. 34 FEV 1 2. 46 FEV 1/FVC 73. 0 FEF 25 -75% 2. 68 PEF 6. 02 Lung Volumes TLC 5. 47 RV 2. 11 RV/TLC 38. 0 FRC PL 2. 90 ERV 1. 12 VC 3. 34 Resistance Raw 1. 31 s. Raw 3. 80 Diffusion DLCO 23. 3 DLCO /VA 3. 82 VA Date: 11/05/04 Height(cm): 169 Temp: 23 Pre Meas 2. 89 2. 21 76. 0 1. 87 4. 75 Pre Post % Ref Meas 87 90 5. 63 2. 58 46. 0 2. 79 (0. 31) 3. 05 Gender: Female BMI: 28. 36 103 122 2. 09 7. 46 Sclerorderma PFT Post % Ref 159 196 70 79 96 (27) 91 (9. 80) (42. 00) 2. 1 55 4. 66 Comments: Acceptable and repeatable results obtained. Interpretation: No significant change since Nov 2001. Post % Chg Age: 63
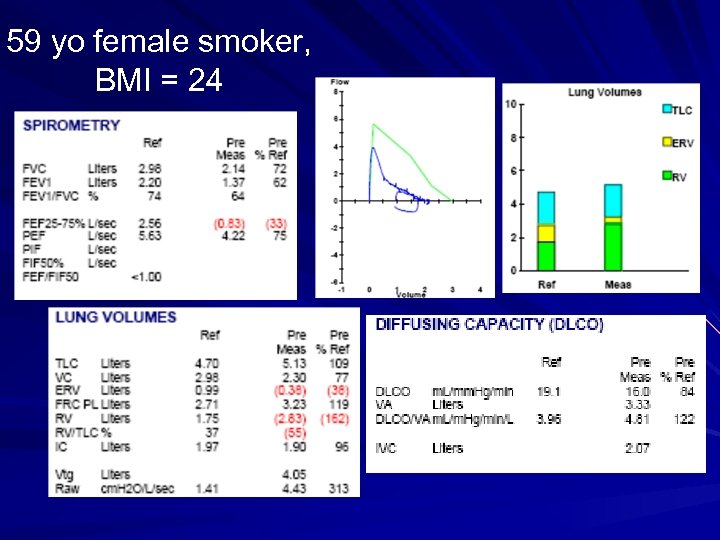 59 yo female smoker, BMI = 24
59 yo female smoker, BMI = 24
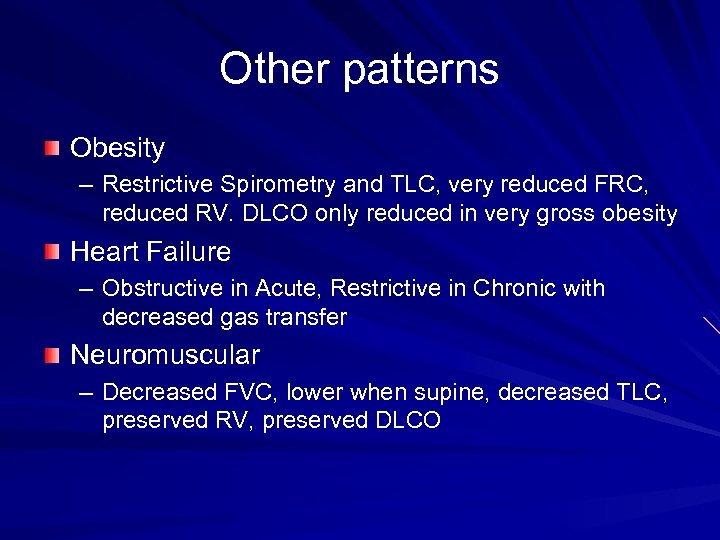 Other patterns Obesity – Restrictive Spirometry and TLC, very reduced FRC, reduced RV. DLCO only reduced in very gross obesity Heart Failure – Obstructive in Acute, Restrictive in Chronic with decreased gas transfer Neuromuscular – Decreased FVC, lower when supine, decreased TLC, preserved RV, preserved DLCO
Other patterns Obesity – Restrictive Spirometry and TLC, very reduced FRC, reduced RV. DLCO only reduced in very gross obesity Heart Failure – Obstructive in Acute, Restrictive in Chronic with decreased gas transfer Neuromuscular – Decreased FVC, lower when supine, decreased TLC, preserved RV, preserved DLCO
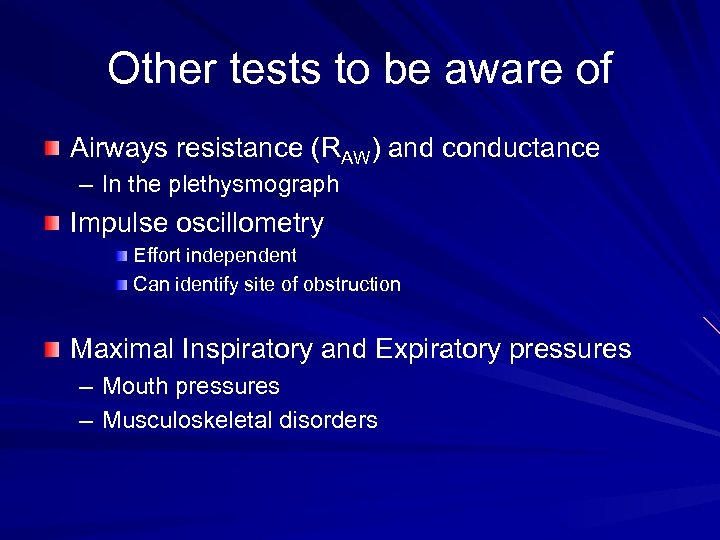 Other tests to be aware of Airways resistance (RAW) and conductance – In the plethysmograph Impulse oscillometry Effort independent Can identify site of obstruction Maximal Inspiratory and Expiratory pressures – Mouth pressures – Musculoskeletal disorders
Other tests to be aware of Airways resistance (RAW) and conductance – In the plethysmograph Impulse oscillometry Effort independent Can identify site of obstruction Maximal Inspiratory and Expiratory pressures – Mouth pressures – Musculoskeletal disorders
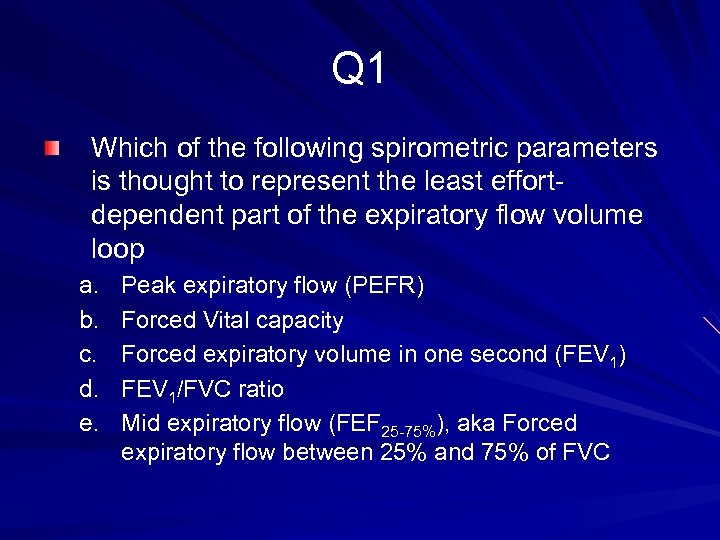 Q 1 Which of the following spirometric parameters is thought to represent the least effortdependent part of the expiratory flow volume loop a. b. c. d. e. Peak expiratory flow (PEFR) Forced Vital capacity Forced expiratory volume in one second (FEV 1) FEV 1/FVC ratio Mid expiratory flow (FEF 25 -75%), aka Forced expiratory flow between 25% and 75% of FVC
Q 1 Which of the following spirometric parameters is thought to represent the least effortdependent part of the expiratory flow volume loop a. b. c. d. e. Peak expiratory flow (PEFR) Forced Vital capacity Forced expiratory volume in one second (FEV 1) FEV 1/FVC ratio Mid expiratory flow (FEF 25 -75%), aka Forced expiratory flow between 25% and 75% of FVC
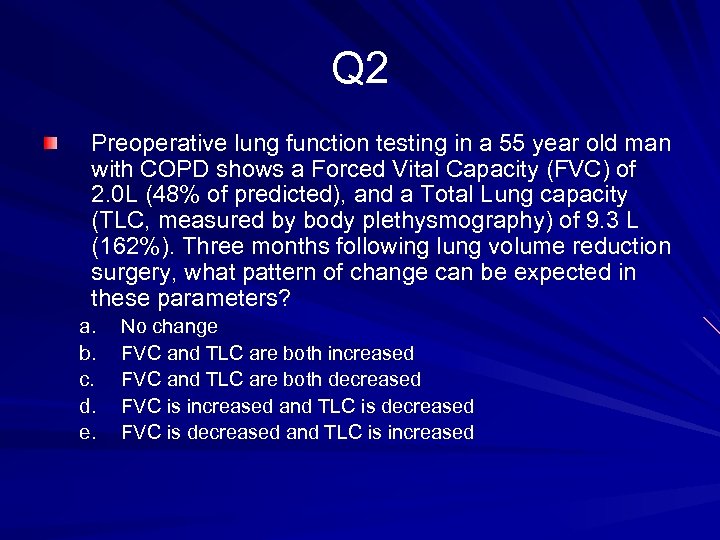 Q 2 Preoperative lung function testing in a 55 year old man with COPD shows a Forced Vital Capacity (FVC) of 2. 0 L (48% of predicted), and a Total Lung capacity (TLC, measured by body plethysmography) of 9. 3 L (162%). Three months following lung volume reduction surgery, what pattern of change can be expected in these parameters? a. b. c. d. e. No change FVC and TLC are both increased FVC and TLC are both decreased FVC is increased and TLC is decreased FVC is decreased and TLC is increased
Q 2 Preoperative lung function testing in a 55 year old man with COPD shows a Forced Vital Capacity (FVC) of 2. 0 L (48% of predicted), and a Total Lung capacity (TLC, measured by body plethysmography) of 9. 3 L (162%). Three months following lung volume reduction surgery, what pattern of change can be expected in these parameters? a. b. c. d. e. No change FVC and TLC are both increased FVC and TLC are both decreased FVC is increased and TLC is decreased FVC is decreased and TLC is increased
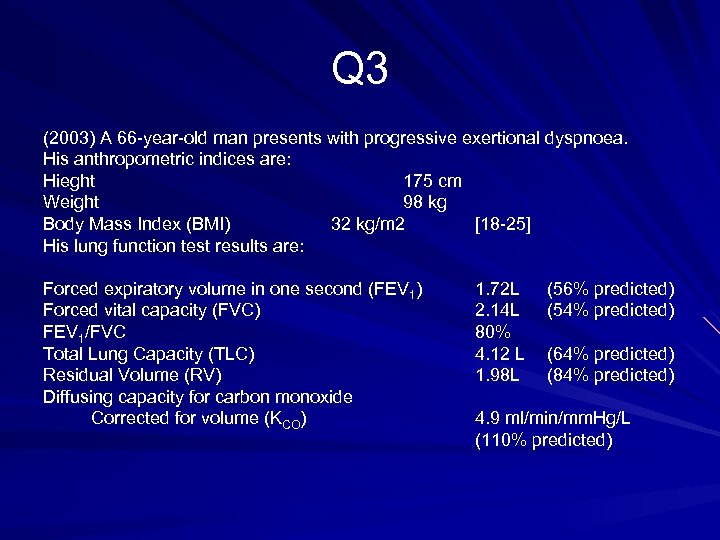 Q 3 (2003) A 66 -year-old man presents with progressive exertional dyspnoea. His anthropometric indices are: Hieght 175 cm Weight 98 kg Body Mass Index (BMI) 32 kg/m 2 [18 -25] His lung function test results are: Forced expiratory volume in one second (FEV 1) Forced vital capacity (FVC) FEV 1/FVC Total Lung Capacity (TLC) Residual Volume (RV) Diffusing capacity for carbon monoxide Corrected for volume (KCO) 1. 72 L 2. 14 L 80% 4. 12 L 1. 98 L (56% predicted) (54% predicted) (64% predicted) (84% predicted) 4. 9 ml/min/mm. Hg/L (110% predicted)
Q 3 (2003) A 66 -year-old man presents with progressive exertional dyspnoea. His anthropometric indices are: Hieght 175 cm Weight 98 kg Body Mass Index (BMI) 32 kg/m 2 [18 -25] His lung function test results are: Forced expiratory volume in one second (FEV 1) Forced vital capacity (FVC) FEV 1/FVC Total Lung Capacity (TLC) Residual Volume (RV) Diffusing capacity for carbon monoxide Corrected for volume (KCO) 1. 72 L 2. 14 L 80% 4. 12 L 1. 98 L (56% predicted) (54% predicted) (64% predicted) (84% predicted) 4. 9 ml/min/mm. Hg/L (110% predicted)
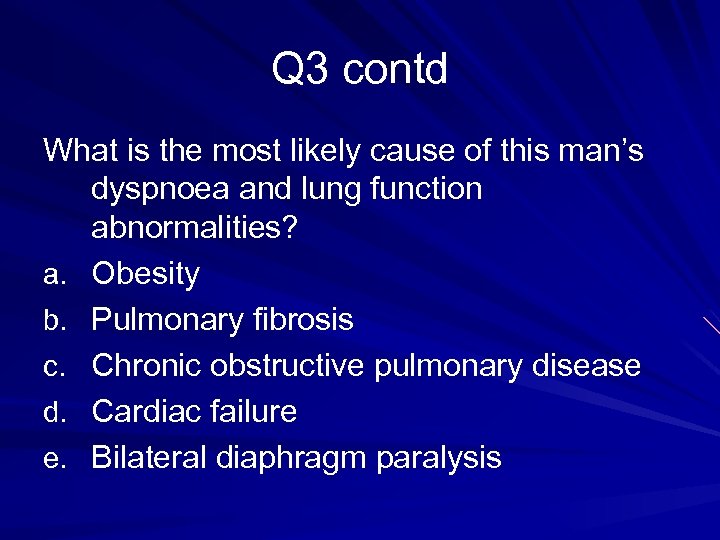 Q 3 contd What is the most likely cause of this man’s dyspnoea and lung function abnormalities? a. Obesity b. Pulmonary fibrosis c. Chronic obstructive pulmonary disease d. Cardiac failure e. Bilateral diaphragm paralysis
Q 3 contd What is the most likely cause of this man’s dyspnoea and lung function abnormalities? a. Obesity b. Pulmonary fibrosis c. Chronic obstructive pulmonary disease d. Cardiac failure e. Bilateral diaphragm paralysis
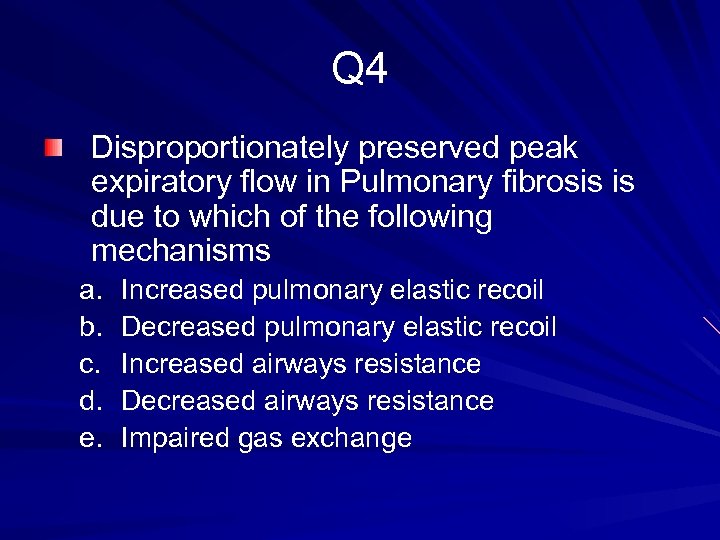 Q 4 Disproportionately preserved peak expiratory flow in Pulmonary fibrosis is due to which of the following mechanisms a. b. c. d. e. Increased pulmonary elastic recoil Decreased pulmonary elastic recoil Increased airways resistance Decreased airways resistance Impaired gas exchange
Q 4 Disproportionately preserved peak expiratory flow in Pulmonary fibrosis is due to which of the following mechanisms a. b. c. d. e. Increased pulmonary elastic recoil Decreased pulmonary elastic recoil Increased airways resistance Decreased airways resistance Impaired gas exchange
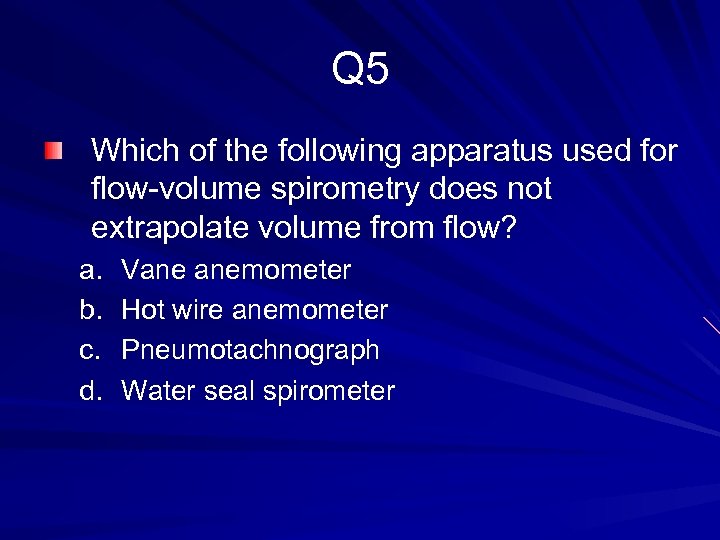 Q 5 Which of the following apparatus used for flow-volume spirometry does not extrapolate volume from flow? a. b. c. d. Vane anemometer Hot wire anemometer Pneumotachnograph Water seal spirometer
Q 5 Which of the following apparatus used for flow-volume spirometry does not extrapolate volume from flow? a. b. c. d. Vane anemometer Hot wire anemometer Pneumotachnograph Water seal spirometer
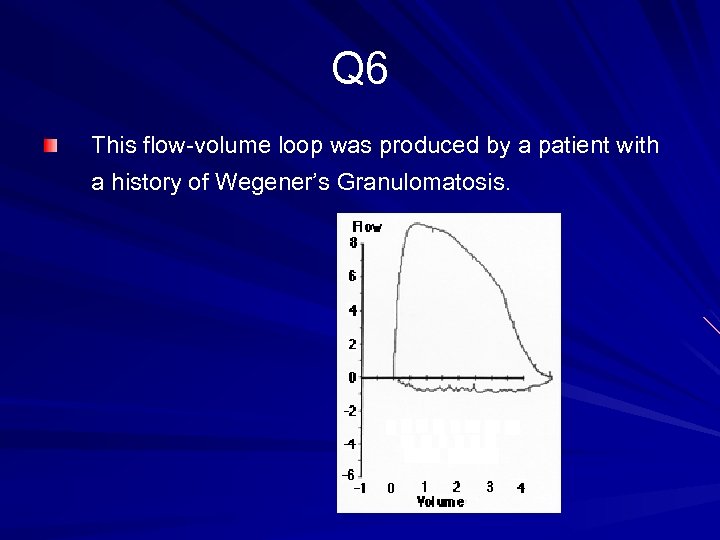 Q 6 This flow-volume loop was produced by a patient with a history of Wegener’s Granulomatosis.
Q 6 This flow-volume loop was produced by a patient with a history of Wegener’s Granulomatosis.
 Q 6 contd The most likely cause of the abnormality is a. Cyclophosphamide therapy b. Asthma c. Pulmonary fibrosis d. Extrathoracic tracheal stenosis e. Intrathoracic tracheal stenosis
Q 6 contd The most likely cause of the abnormality is a. Cyclophosphamide therapy b. Asthma c. Pulmonary fibrosis d. Extrathoracic tracheal stenosis e. Intrathoracic tracheal stenosis
 END
END


