d3701ebcea95b7effad6c79bb463692b.ppt
- Количество слайдов: 42
PUBLIC -PRIVATE PARTNERSHIP FOR HEALTH CARE DEVELOPMENT ` fi!LH fiajdfjss ixj. O—kh i|yd rdc. H yd fm!oa. , sl wx. Yhka fldgialrejka ùu by Dr A. K. S. B. DE Alwis Dr Luxman Edirisinghe 1
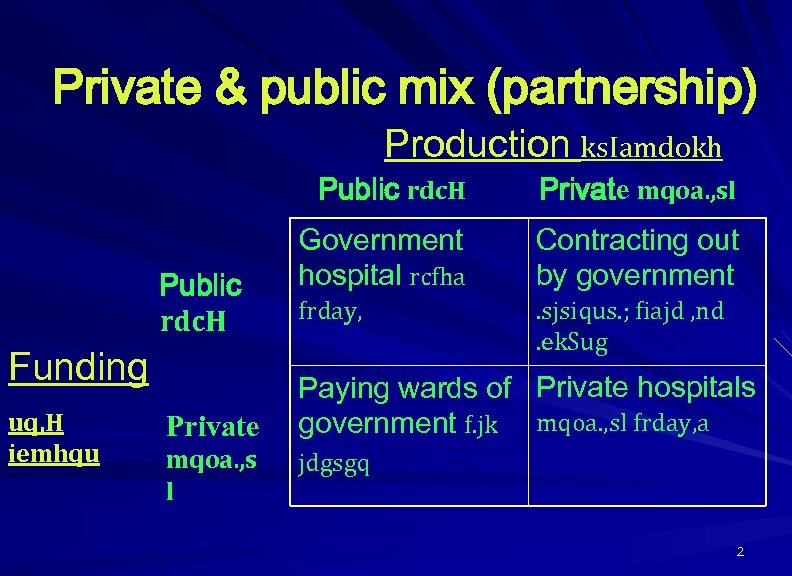
Private & public mix (partnership) Production ks. Iamdokh Public rdc. H Funding uq, H iemhqu Private mqoa. , s l Private mqoa. , sl Government hospital rcfha Contracting out by government frday, . sjsiqus. ; fiajd , nd. ek. Sug Paying wards of Private hospitals government f. jk mqoa. , sl frday, a jdgsgq 2
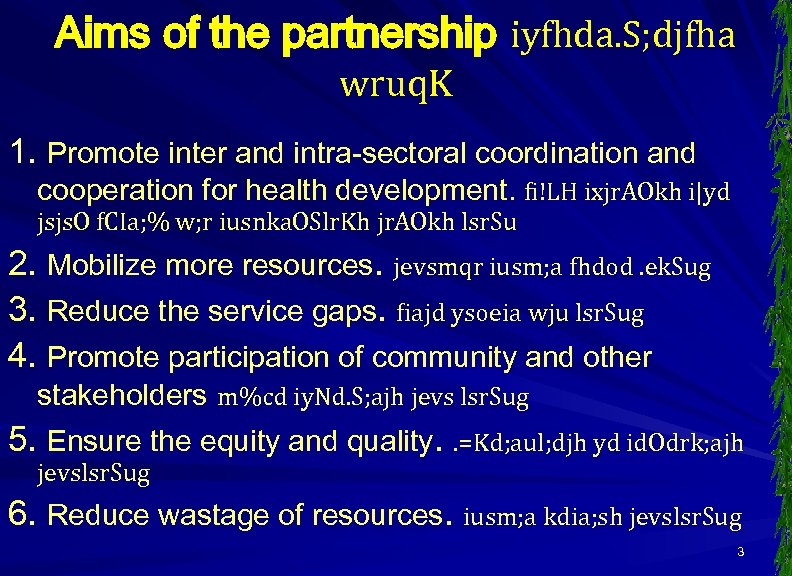
Aims of the partnership iyfhda. S; djfha wruq. K 1. Promote inter and intra-sectoral coordination and cooperation for health development. fi!LH ixjr. AOkh i|yd jsjs. O f. CIa; % w; r iusnka. OSlr. Kh jr. AOkh lsr. Su 2. Mobilize more resources. jevsmqr iusm; a fhdod. ek. Sug 3. Reduce the service gaps. fiajd ysoeia wju lsr. Sug 4. Promote participation of community and other stakeholders m%cd iy. Nd. S; ajh jevs lsr. Sug 5. Ensure the equity and quality. . =Kd; aul; djh yd id. Odrk; ajh jevslsr. Sug 6. Reduce wastage of resources. iusm; a kdia; sh jevslsr. Sug 3
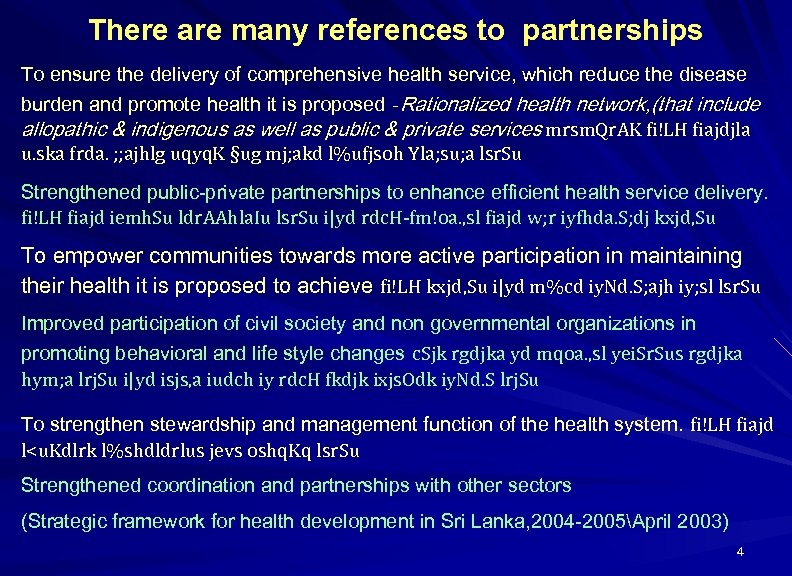
There are many references to partnerships To ensure the delivery of comprehensive health service, which reduce the disease burden and promote health it is proposed -Rationalized health network, (that include allopathic & indigenous as well as public & private services mrsm. Qr. AK fi!LH fiajdjla u. ska frda. ; ; ajhlg uqyq. K §ug mj; akd l%ufjsoh Yla; su; a lsr. Su Strengthened public-private partnerships to enhance efficient health service delivery. fi!LH fiajd iemh. Su ldr. AAhla. Iu lsr. Su i|yd rdc. H-fm!oa. , sl fiajd w; r iyfhda. S; dj kxjd, Su To empower communities towards more active participation in maintaining their health it is proposed to achieve fi!LH kxjd, Su i|yd m%cd iy. Nd. S; ajh iy; sl lsr. Su Improved participation of civil society and non governmental organizations in promoting behavioral and life style changes c. Sjk rgdjka yd mqoa. , sl yei. Sr. Sus rgdjka hym; a lrj. Su i|yd isjs, a iudch iy rdc. H fkdjk ixjs. Odk iy. Nd. S lrj. Su To strengthen stewardship and management function of the health system. fi!LH fiajd l<u. Kdlrk l%shdldrlus jevs oshq. Kq lsr. Su Strengthened coordination and partnerships with other sectors (Strategic framework for health development in Sri Lanka, 2004 -2005April 2003) 4
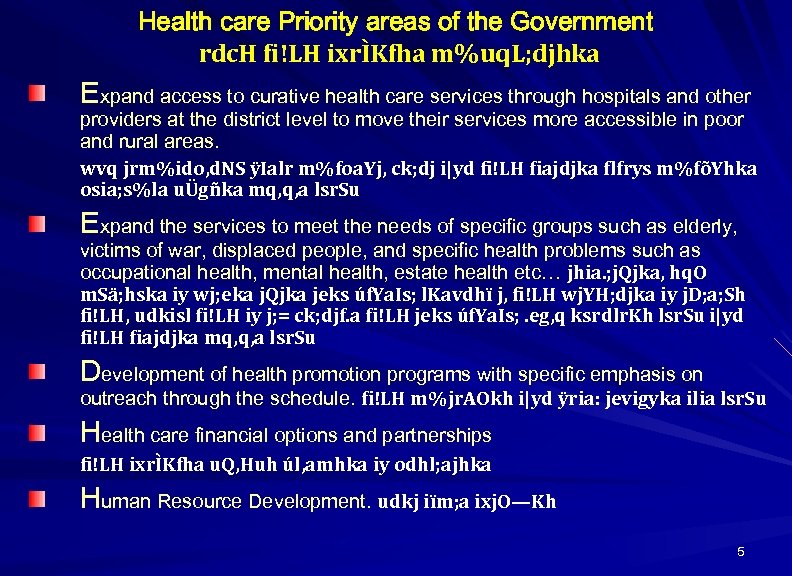
Health care Priority areas of the Government rdc. H fi!LH ixrÌKfha m%uq. L; djhka Expand access to curative health care services through hospitals and other providers at the district level to move their services more accessible in poor and rural areas. wvq jrm%ido, d. NS ÿIalr m%foa. Yj, ck; dj i|yd fi!LH fiajdjka flfrys m%fõYhka osia; s%la uÜgñka mq, q, a lsr. Su Expand the services to meet the needs of specific groups such as elderly, victims of war, displaced people, and specific health problems such as occupational health, mental health, estate health etc… jhia. ; j. Qjka, hq. O m. Sä; hska iy wj; eka j. Qjka jeks úf. Ya. Is; l. Kavdhï j, fi!LH wj. YH; djka iy j. D; a; Sh fi!LH, udkisl fi!LH iy j; = ck; djf. a fi!LH jeks úf. Ya. Is; . eg, q ksrdlr. Kh lsr. Su i|yd fi!LH fiajdjka mq, q, a lsr. Su Development of health promotion programs with specific emphasis on outreach through the schedule. fi!LH m%jr. AOkh i|yd ÿria: jevigyka ilia lsr. Su Health care financial options and partnerships fi!LH ixrÌKfha u. Q, Huh úl, amhka iy odhl; ajhka Human Resource Development. udkj iïm; a ixj. O—Kh 5
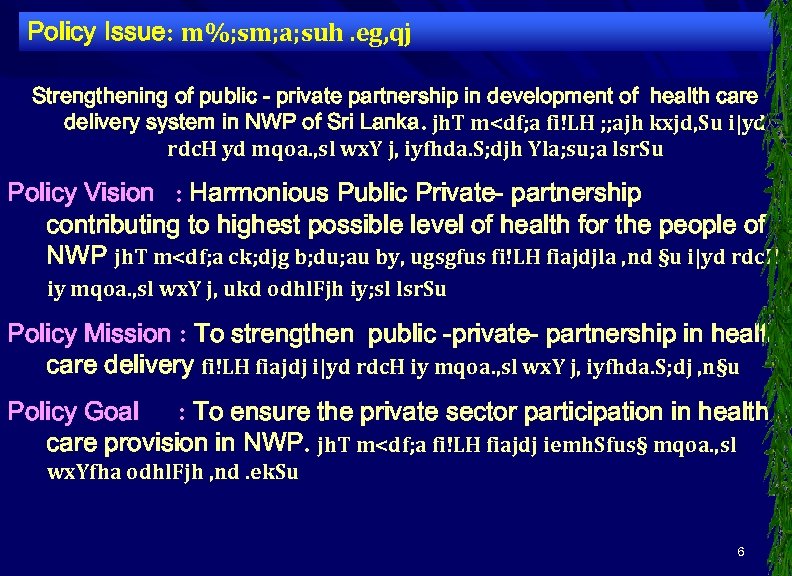
Policy Issue: m%; sm; a; suh. eg, qj Strengthening of public - private partnership in development of health care delivery system in NWP of Sri Lanka. jh. T m<df; a fi!LH ; ; ajh kxjd, Su i|yd rdc. H yd mqoa. , sl wx. Y j, iyfhda. S; djh Yla; su; a lsr. Su Policy Vision : Harmonious Public Private- partnership contributing to highest possible level of health for the people of NWP jh. T m<df; a ck; djg b; du; au by, ugsgfus fi!LH fiajdjla , nd §u i|yd rdc. H iy mqoa. , sl wx. Y j, ukd odhl. Fjh iy; sl lsr. Su Policy Mission : To strengthen public -private- partnership in health care delivery fi!LH fiajdj i|yd rdc. H iy mqoa. , sl wx. Y j, iyfhda. S; dj , n§u Policy Goal : To ensure the private sector participation in health care provision in NWP. jh. T m<df; a fi!LH fiajdj iemh. Sfus§ mqoa. , sl wx. Yfha odhl. Fjh , nd. ek. Su 6

7
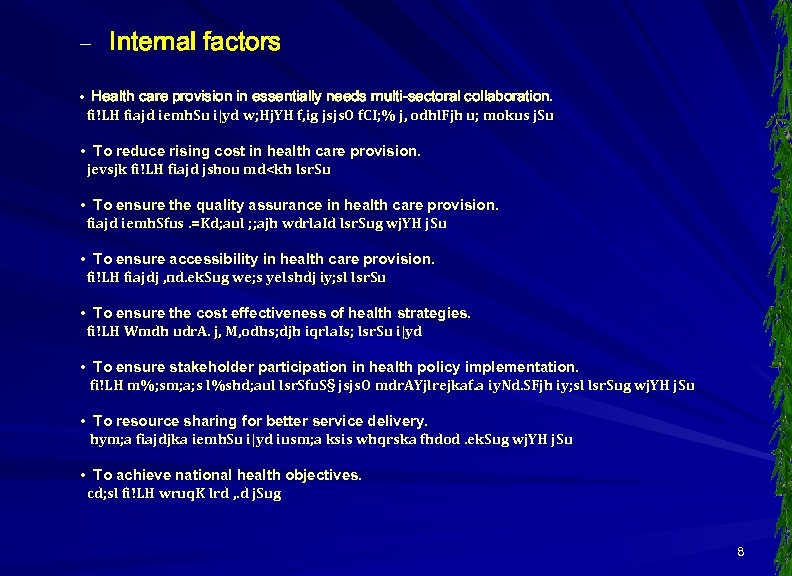
– Internal factors • Health care provision in essentially needs multi-sectoral collaboration. fi!LH fiajd iemh. Su i|yd w; Hj. YH f, ig jsjs. O f. CI; % j, odhl. Fjh u; mokus j. Su • To reduce rising cost in health care provision. jevsjk fi!LH fiajd jshou md<kh lsr. Su • To ensure the quality assurance in health care provision. fiajd iemh. Sfus. =Kd; aul ; ; ajh wdrla. Id lsr. Sug wj. YH j. Su • To ensure accessibility in health care provision. fi!LH fiajdj , nd. ek. Sug we; s yelshdj iy; sl lsr. Su • To ensure the cost effectiveness of health strategies. fi!LH Wmdh udr. A. j, M, odhs; djh iqrla. Is; lsr. Su i|yd • To ensure stakeholder participation in health policy implementation. fi!LH m%; sm; a; s l%shd; aul lsr. Sfu. S§ jsjs. O mdr. AYjlrejkaf. a iy. Nd. SFjh iy; sl lsr. Sug wj. YH j. Su • To resource sharing for better service delivery. hym; a fiajdjka iemh. Su i|yd iusm; a ksis whqrska fhdod. ek. Sug wj. YH j. Su • To achieve national health objectives. cd; sl fi!LH wruq. K lrd , . d j. Sug 8
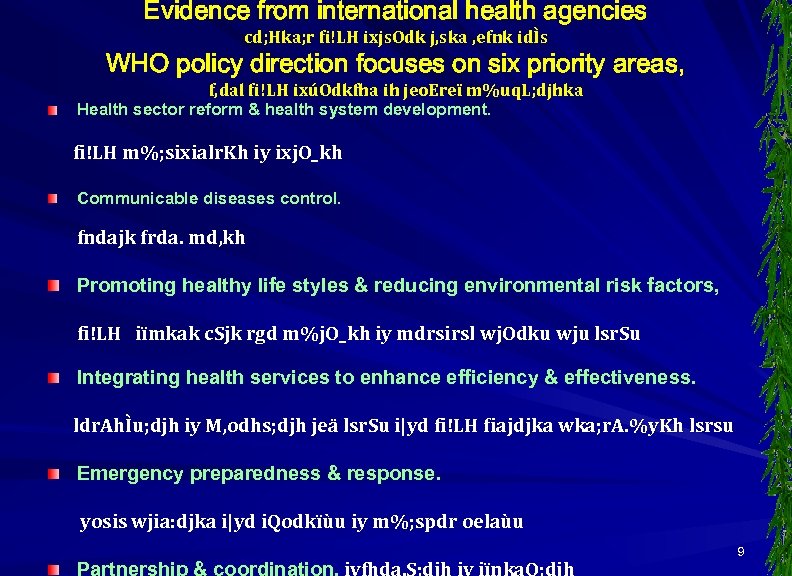
Evidence from international health agencies cd; Hka; r fi!LH ixjs. Odk j, ska , efnk idÌs WHO policy direction focuses on six priority areas, f, dal fi!LH ixúOdkfha ih jeo. Ereï m%uq. L; djhka Health sector reform & health system development. fi!LH m%; sixialr. Kh iy ixj. O_kh Communicable diseases control. fndajk frda. md, kh Promoting healthy life styles & reducing environmental risk factors, fi!LH iïmkak c. Sjk rgd m%j. O_kh iy mdrsirsl wj. Odku wju lsr. Su Integrating health services to enhance efficiency & effectiveness. ldr. AhÌu; djh iy M, odhs; djh jeä lsr. Su i|yd fi!LH fiajdjka wka; r. A. %y. Kh lsrsu Emergency preparedness & response. yosis wjia: djka i|yd i. Qodkïùu iy m%; spdr oelaùu 9
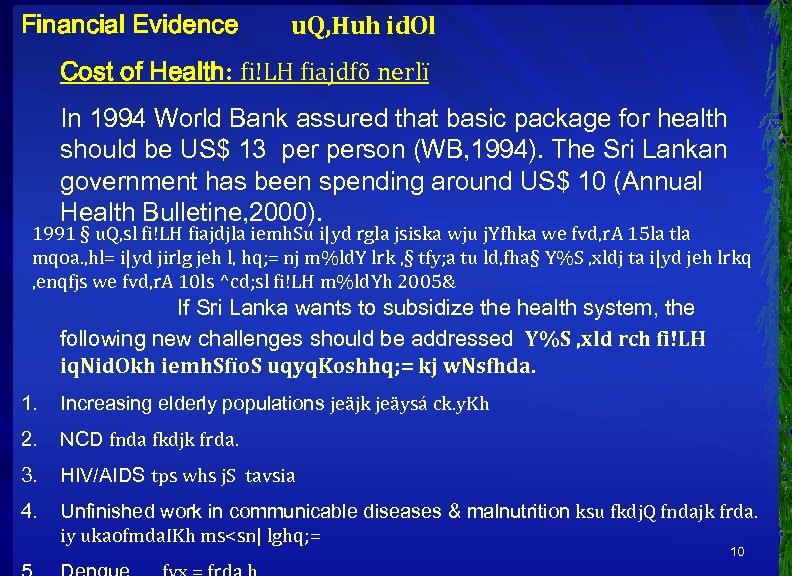
Financial Evidence u. Q, Huh id. Ol Cost of Health: fi!LH fiajdfõ nerlï In 1994 World Bank assured that basic package for health should be US$ 13 person (WB, 1994). The Sri Lankan government has been spending around US$ 10 (Annual Health Bulletine, 2000). 1991 § u. Q, sl fi!LH fiajdjla iemh. Su i|yd rgla jsiska wju j. Yfhka we fvd, r. A 15 la tla mqoa. , hl= i|yd jirlg jeh l, hq; = nj m%ld. Y lrk , § tfy; a tu ld, fha§ Y%S , xldj ta i|yd jeh lrkq , enqfjs we fvd, r. A 10 ls ^cd; sl fi!LH m%ld. Yh 2005& If Sri Lanka wants to subsidize the health system, the following new challenges should be addressed Y%S , xld rch fi!LH iq. Nid. Okh iemh. Sfïo. S uqyq. Koshhq; = kj w. Nsfhda. 1. Increasing elderly populations jeäjk jeäysá ck. y. Kh 2. NCD fnda fkdjk frda. 3. HIV/AIDS tps whs j. S tavsia 4. Unfinished work in communicable diseases & malnutrition ksu fkdj. Q fndajk frda. iy ukaofmda. IKh ms<sn| lghq; = 10
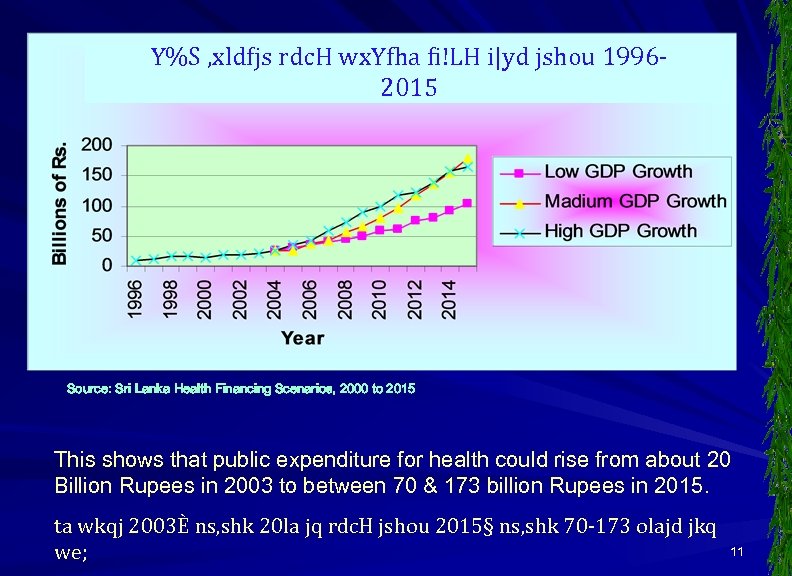
Y%S , xldfjs rdc. H wx. Yfha fi!LH i|yd jshou 19962015 Source: Sri Lanka Health Financing Scenarios, 2000 to 2015 This shows that public expenditure for health could rise from about 20 Billion Rupees in 2003 to between 70 & 173 billion Rupees in 2015. ta wkqj 2003È ns, shk 20 la jq rdc. H jshou 2015§ ns, shk 70 -173 olajd jkq we; 11

Source: National health Accounts-2002 12
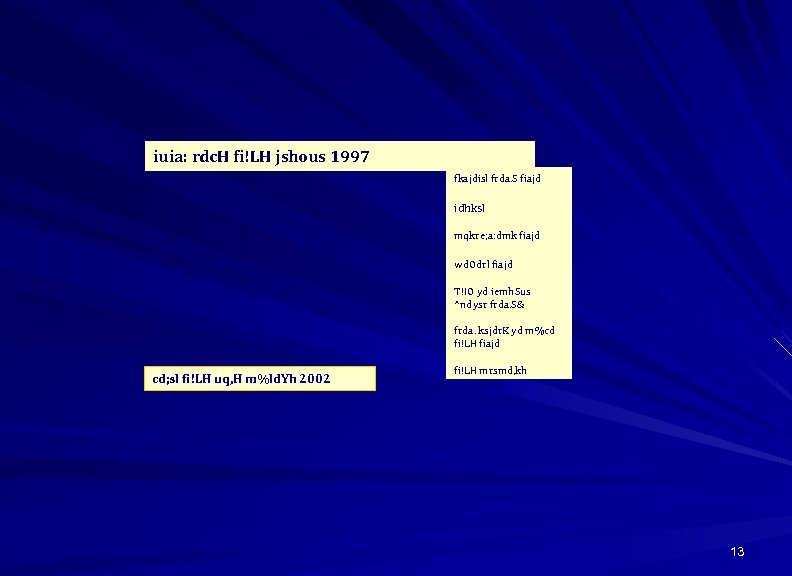
iuia: rdc. H fi!LH jshous 1997 fkajdisl frda. S fiajd idhksl mqkre; a: dmk fiajd wd. Odrl fiajd T!IO yd iemh. Sus ^ndysr frda. S& frda. ksjdr. K yd m%cd fi!LH fiajd cd; sl fi!LH uq, H m%ld. Yh 2002 fi!LH mrsmd, kh l<u. Kdlr. Kh 13
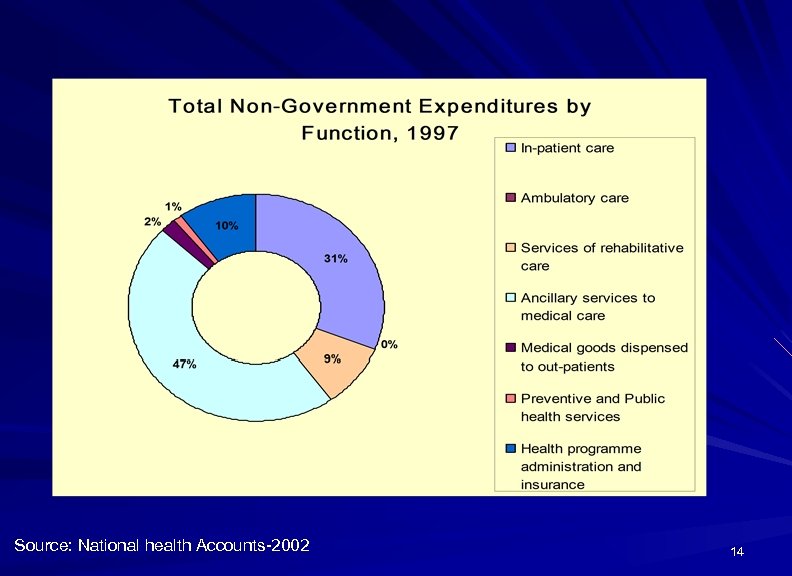
Source: National health Accounts-2002 14
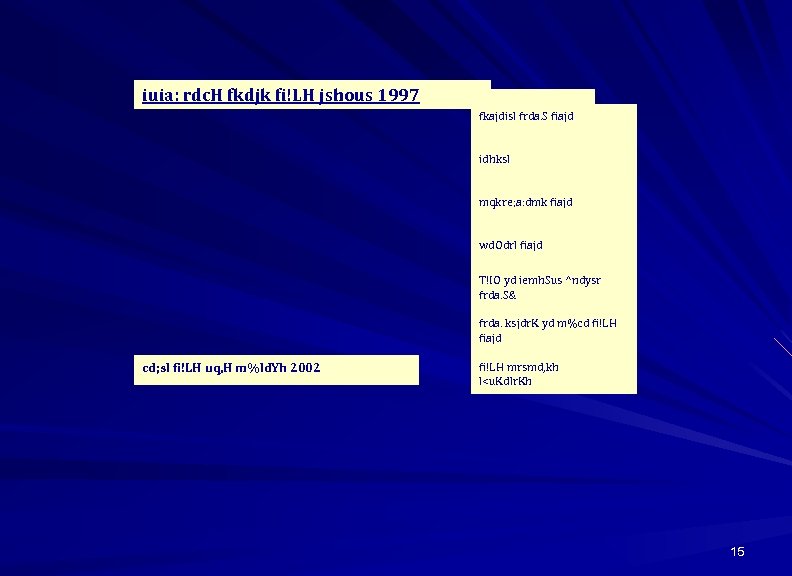
iuia: rdc. H fkdjk fi!LH jshous 1997 fkajdisl frda. S fiajd idhksl mqkre; a: dmk fiajd wd. Odrl fiajd T!IO yd iemh. Sus ^ndysr frda. S& frda. ksjdr. K yd m%cd fi!LH fiajd cd; sl fi!LH uq, H m%ld. Yh 2002 fi!LH mrsmd, kh l<u. Kdlr. Kh 15
rdc. H jshous j, m<d; a wkqj fjkialus 16
1999 – 1999 jir j, fi!LH wdfhdack 17
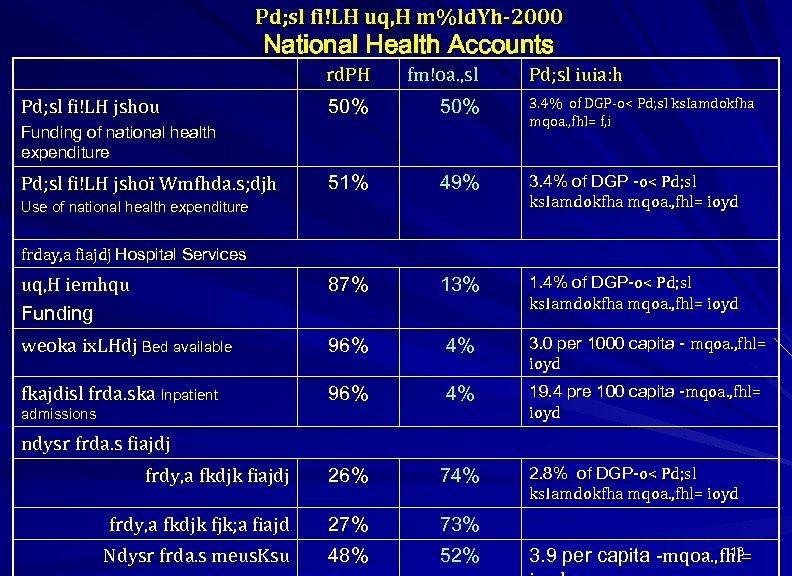
Pd; sl fi!LH uq, H m%ld. Yh-2000 National Health Accounts rd. PH fm!oa. , sl 50% 3. 4% of DGP-o< Pd; sl ks. Iamdokfha mqoa. , fhl= f, i 51% 49% 3. 4% of DGP -o< Pd; sl ks. Iamdokfha mqoa. , fhl= ioyd uq, H iemhqu Funding 87% 13% 1. 4% of DGP-o< Pd; sl ks. Iamdokfha mqoa. , fhl= ioyd weoka ix. LHdj Bed available 96% 4% 3. 0 per 1000 capita - mqoa. , fhl= ioyd fkajdisl frda. ska Inpatient 96% 4% 19. 4 pre 100 capita -mqoa. , fhl= ioyd frdy, a fkdjk fiajdj 26% 74% frdy, a fkdjk fjk; a fiajd 27% 73% Ndysr frda. s meus. Ksu 48% 52% Pd; sl fi!LH jshou Funding of national health expenditure Pd; sl fi!LH jshoï Wmfhda. s; djh Use of national health expenditure Pd; sl iuia: h frday, a fiajdj Hospital Services admissions ndysr frda. s fiajdj 2. 8% of DGP-o< Pd; sl ks. Iamdokfha mqoa. , fhl= ioyd 18 3. 9 per capita -mqoa. , fhl=
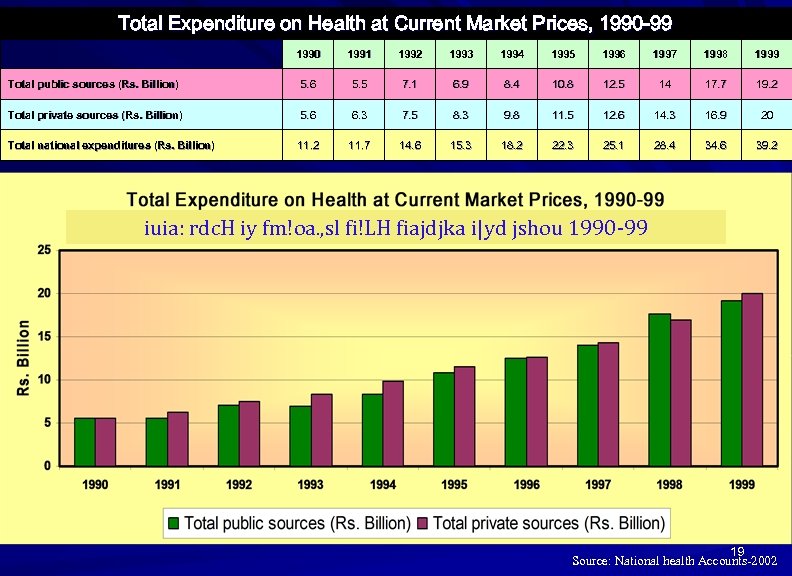
Total Expenditure on Health at Current Market Prices, 1990 -99 1990 1991 1992 1993 1994 1995 1996 1997 1998 1999 Total public sources (Rs. Billion) 5. 6 5. 5 7. 1 6. 9 8. 4 10. 8 12. 5 14 17. 7 19. 2 Total private sources (Rs. Billion) 5. 6 6. 3 7. 5 8. 3 9. 8 11. 5 12. 6 14. 3 16. 9 20 Total national expenditures (Rs. Billion) 11. 2 11. 7 14. 6 15. 3 18. 2 22. 3 25. 1 28. 4 34. 6 39. 2 iuia: rdc. H iy fm!oa. , sl fi!LH fiajdjka i|yd jshou 1990 -99 19 Source: National health Accounts-2002
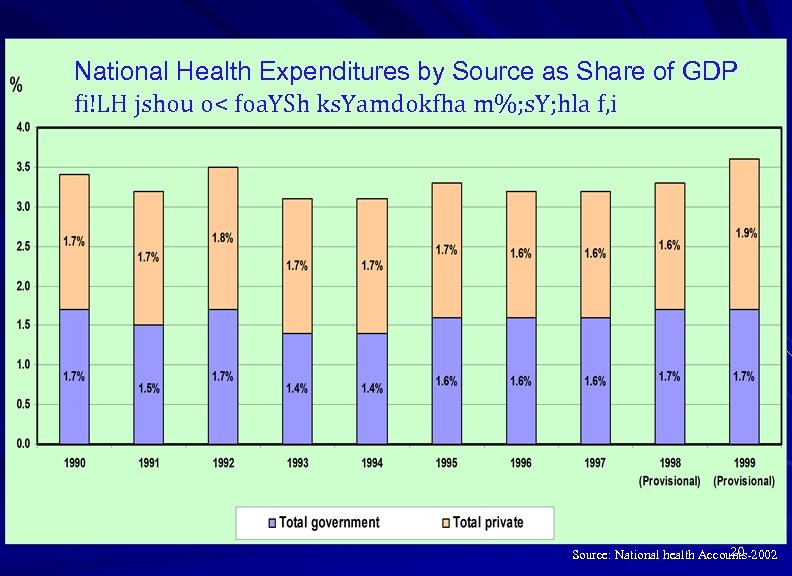
National Health Expenditures by Source as Share of GDP fi!LH jshou o< foa. YSh ks. Yamdokfha m%; s. Y; hla f, i 20 Source: National health Accounts-2002
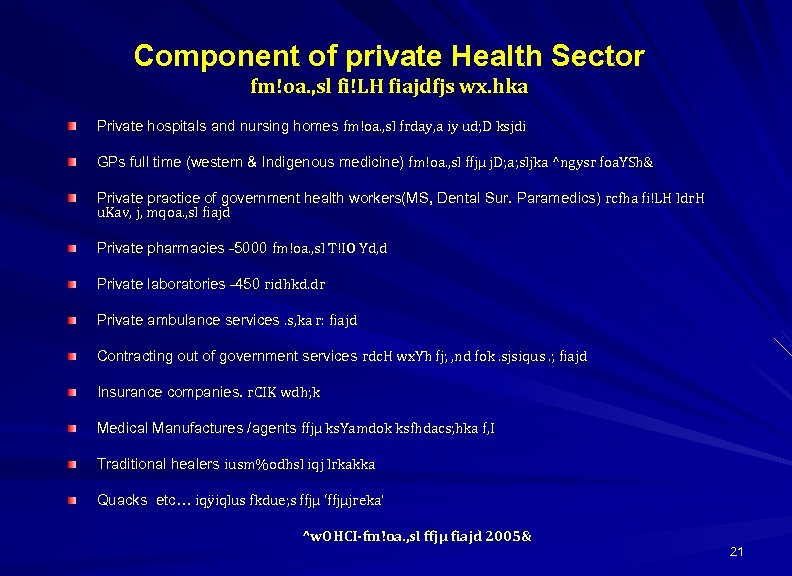
Component of private Health Sector fm!oa. , sl fi!LH fiajdfjs wx. hka Private hospitals and nursing homes fm!oa. , sl frday, a iy ud; D ksjdi GPs full time (western & Indigenous medicine) fm!oa. , sl ffjµ j. D; a; sljka ^ngysr foa. YSh& Private practice of government health workers(MS, Dental Sur. Paramedics) rcfha fi!LH ldr. H u. Kav, j, mqoa. , sl fiajd Private pharmacies -5000 fm!oa. , sl T!IO Yd, d Private laboratories -450 ridhkd. dr Private ambulance services. s, ka r: fiajd Contracting out of government services rdc. H wx. Yh fj; , nd fok. sjsiqus. ; fiajd Insurance companies. r. CIK wdh; k Medical Manufactures /agents ffjµ ks. Yamdok ksfhdacs; hka f, I Traditional healers iusm%odhsl iqj lrkakka Quacks etc… iqÿiqlus fkdue; s ffjµ ‘ffjµjreka’ ^w. OHCI-fm!oa. , sl ffjµ fiajd 2005& 21
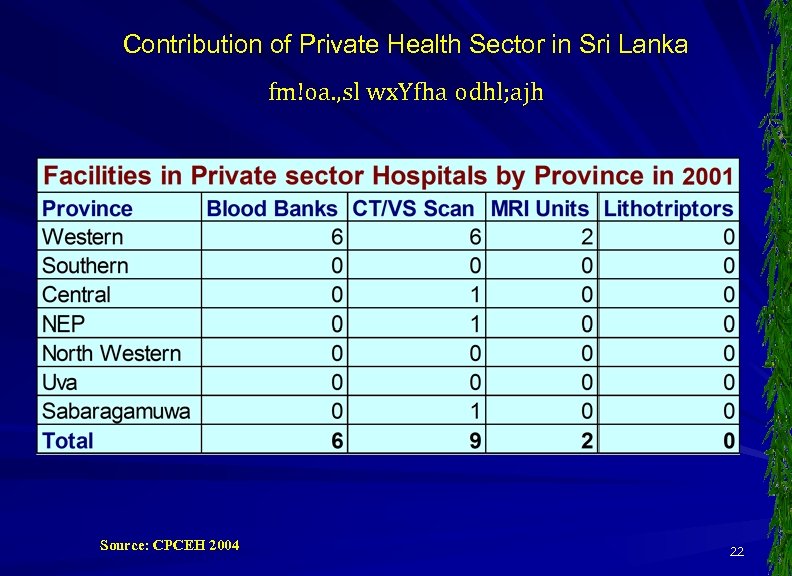
Contribution of Private Health Sector in Sri Lanka fm!oa. , sl wx. Yfha odhl; ajh Source: CPCEH 2004 22
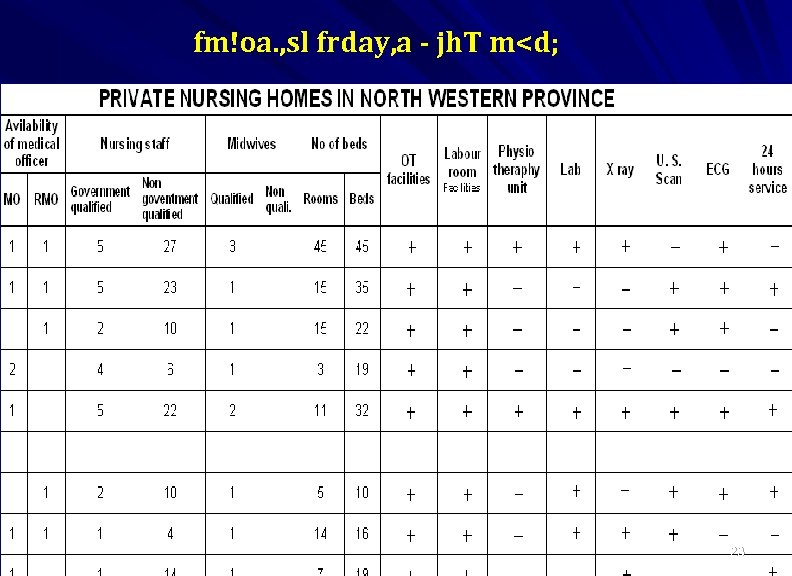
fm!oa. , sl frday, a - jh. T m<d; 23
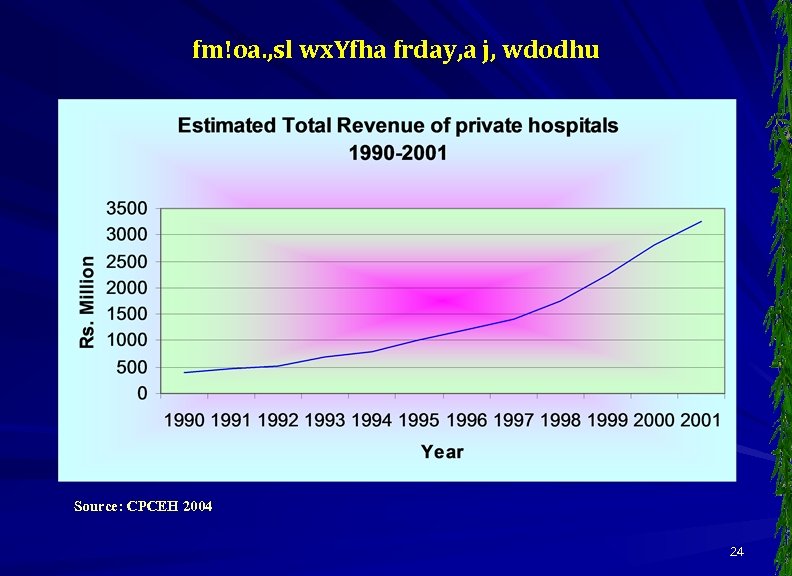
fm!oa. , sl wx. Yfha frday, a j, wdodhu Source: CPCEH 2004 24
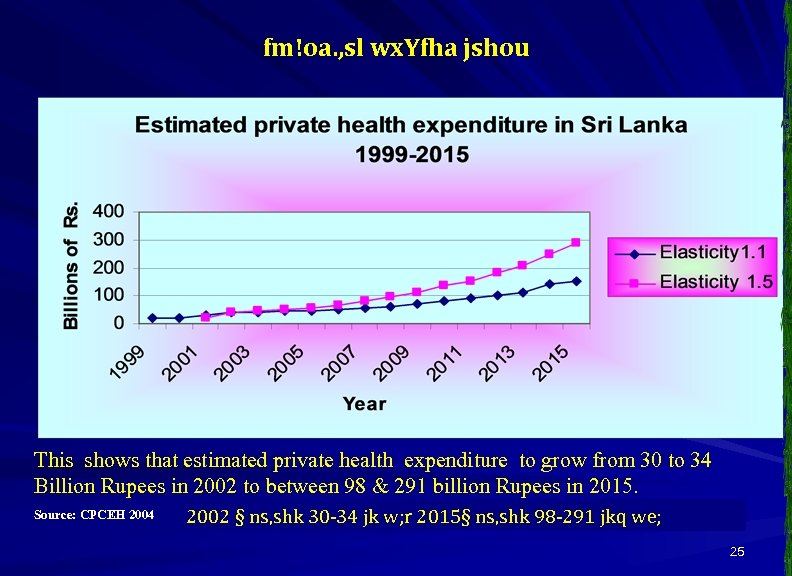
fm!oa. , sl wx. Yfha jshou This shows that estimated private health expenditure to grow from 30 to 34 Billion Rupees in 2002 to between 98 & 291 billion Rupees in 2015. Source: CPCEH 2004 2002 § ns, shk 30 -34 jk w; r 2015§ ns, shk 98 -291 jkq we; 25
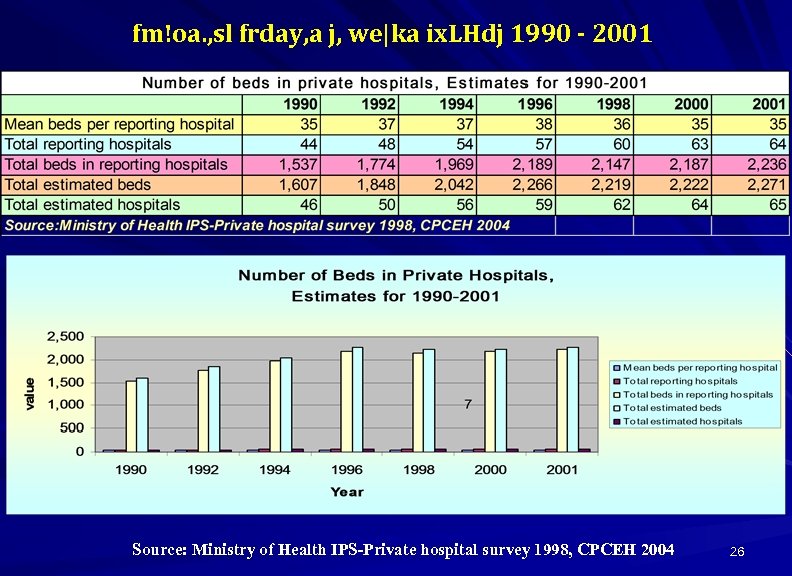
fm!oa. , sl frday, a j, we|ka ix. LHdj 1990 - 2001 Source: Ministry of Health IPS-Private hospital survey 1998, CPCEH 2004 26
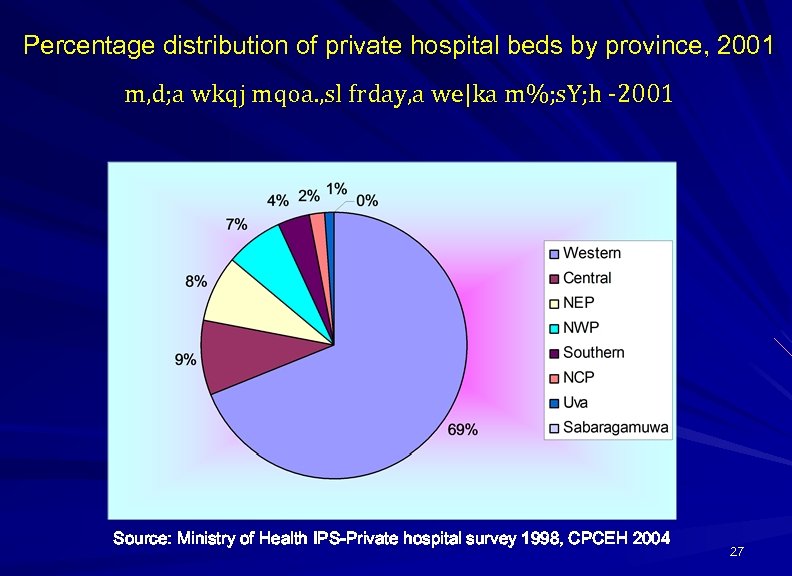
Percentage distribution of private hospital beds by province, 2001 m, d; a wkqj mqoa. , sl frday, a we|ka m%; s. Y; h -2001 Source: Ministry of Health IPS-Private hospital survey 1998, CPCEH 2004 27
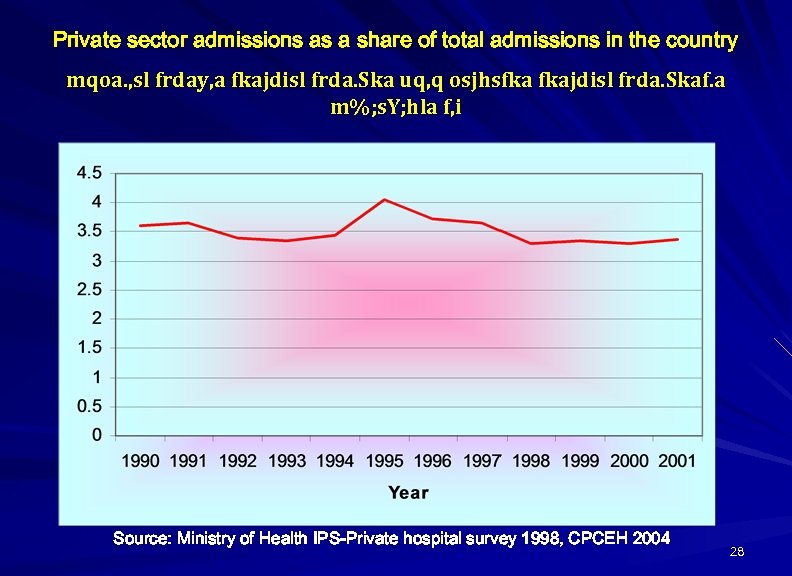
Private sector admissions as a share of total admissions in the country mqoa. , sl frday, a fkajdisl frda. Ska uq, q osjhsfka fkajdisl frda. Skaf. a m%; s. Y; hla f, i Source: Ministry of Health IPS-Private hospital survey 1998, CPCEH 2004 28
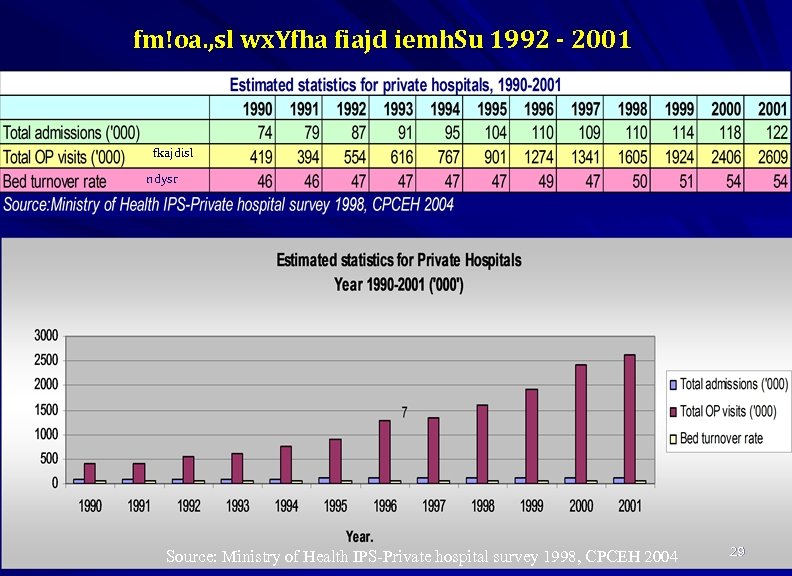
fm!oa. , sl wx. Yfha fiajd iemh. Su 1992 - 2001 fkajdisl ndysr Source: Ministry of Health IPS-Private hospital survey 1998, CPCEH 2004 29
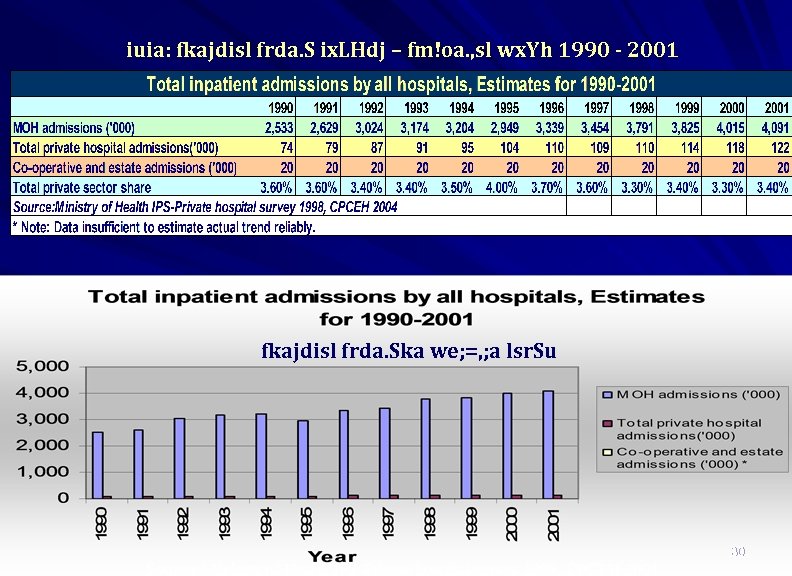
iuia: fkajdisl frda. S ix. LHdj – fm!oa. , sl wx. Yh 1990 - 2001 fkajdisl frda. Ska we; =, ; a lsr. Su 30 Source: Ministry of Health IPS-Private hospital survey 1998, CPCEH 2004
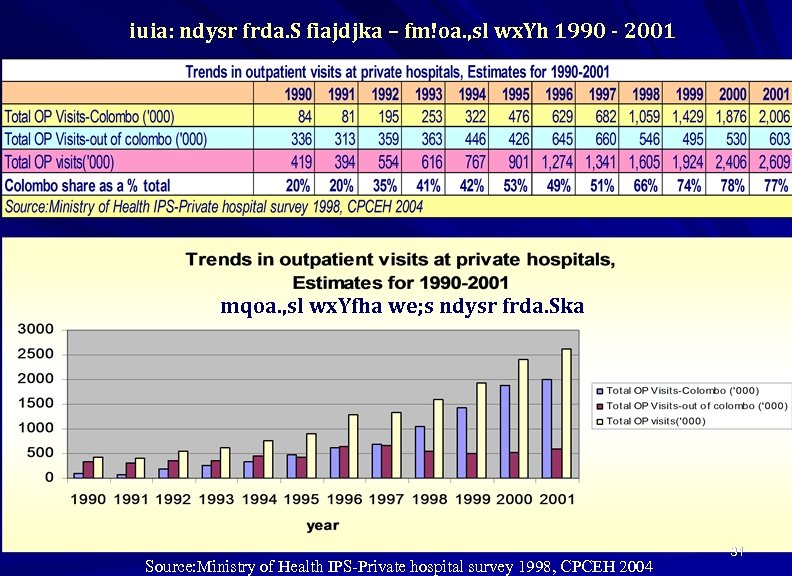
iuia: ndysr frda. S fiajdjka – fm!oa. , sl wx. Yh 1990 - 2001 mqoa. , sl wx. Yfha we; s ndysr frda. Ska Source: Ministry of Health IPS-Private hospital survey 1998, CPCEH 2004 31
Current situation in partnership iyfhda. S; djfha jr. A; udk ; ; ajh 1. No proper legal frame work ukd k. S; suh mokula ke; 2. No coordination between two sectors wx. Y foflys iyiïnka. O; djhla fkdue; 1. 2. 4. 4. 5. 5. 6. No feedback mechanisms js. Osu; a ixksfj. Sok l%ufõohla fkdue; 3. 3. Private sector institutions are not registered in health department mqoa. , sl fi!LH wdh; k rcfha , shdmosxÑ lr fkdue; No monitoring mechanisms wëÌK ms<sfj; la fkdue; No participation in health planning & implementation fi!LH ie, iqï lsr. Sfï iy l%shd; aul lsr. Sfï iy. Nd. S; ajhla fkdue; No quality assurance mechanism for private sector mqoa. , sl wx. Yfha ; ; ajmd, k l%uhla fkdue; No sharing of resources for the benefit to community fmdq iïm; a mrsyr. K l%ufõohla fkdue; 6. Wastage and Duplication of works lghq; = oaú. =Kùfuka iïm; a wmf; a hdu 32

33
Possible causes for weak partnership qr. Aj, iyfhda. S; djhg fya; = 01. Lack of tradition in collaboration between two sectors. tjeks iïm%odhla fkdmej; Su 02. Objectives are differ tlu wruq. Kla fkd; sîu 03. The weak information system. ÿr. Aj, ikaksfõokh 04. Lack of capacity in public sector to manage and regulate relationship with private sector. mqoa. , sl wx. Yh iu. iïnka. O; d meje; aùfï oÌ; d rdc. H wx. Yh fj; fkd; sîu 05. Political pressure. foa. Ymd, k n, m. Eï 06. Pressure from trade unions other stakeholders in health. j. D; a; Sh iñ; s we; =, q wfkl=; a md. Y_jlrejkaf. a n, m. Eï 07. Mistrust. wúYajdih 08. Weakly organized private sector in the country. mqoa. , sl wx. Yh ; =, ukd ixúOdkh ùula fkd; sîu 34
cont…. Possible causes for weak partnership 09. Strong public confidence on government health system (socio-cultural influences). rdc. H wx. Yh flfrys we; s oeäúYajdih 10. Weaknesses of private sector in maintaining quality assurance mechanism and fulfilling social responsibilities as expected by the people ck; d wfmaÌdjkag wkqj fiajh ie, i. Sug mqoa. , sl wx. Yh wiu; a ùu 11. Dependency of private sector on public sector for human resources mqoa. , sl wx. Yh rdc. H wx. Yfha udkj iïm; a u; hem. Su 12. No legal framework for partnership k. S; s iïmdok fkd; sîu 13. Less public interest. ck; d Wkkaÿj wvq nj 14. Unsuccessful out comes from partnerships in other sector 35 fjk; a wx. Yj, rdc. H-mqoa. , sl iúnka. O; djhka widr. A: l ùu
Outcome of weak partnership. ÿr. Aj, iyfhda. S; djfha m%; s. M, 01. Uncoordinated activities. wixúOdkd; aul l%shdldrlï The health authorities have no information on private sector investments or activities and private sector, therefore not involved in national health policy formulation and their contribution towards implementation of national health strategies are not significant. 02. Waste of resources from both sectors due to duplication or overlapping of investments. iïm; a wmf; a hdu 03. Lack of sound quality- assurance mechanism in private mqoa. , sl wx. Yfha ukd ; ; aj md, khla fkd; sîu sector. 04. Increasing cost to the government in health care provision. rdc. H wx. Yh wkj. YH úhoula oer. Su 05. Reluctance from donor agencies m%; smdok imhk wdh; k ukafoda; aidy. S ùu 36
Policy options in public-private partnership m%; sm; a; suh úl, am 1. A national policy should be developed to allow private and other non- government sectors to actively participate and contribute in optimum manner to achieve national health objectives in maximum cost effective manner. rcfha ueosy; aùfuka m%; sm; a; s ilia lsr. Su’ 2. Policymakers should achieve this task with the participation and consultation with all internal and external stakeholders of health. ish, q odhl; ajhka iu. tl. ; djhlg meñKSu 3. Formulation of guidelines and protocols for partnership, including modalities for monitoring. fldgialrejka ùu ms<sn|j ish, q k. S; s iy Wmfoia iïmdokh lsr. Su 4. Orientation of private and other non-government sectors on national health policies and strategies. wfkl=; a rdc. H fkdjk iy mqoa. , sl wx. Y rcfha fi!LH m%; sm; a; s iy Wmdh udr. A. ms<sn| oekqj; a lsr. Su Development of consensus among all stakeholders on partnerships. md. Y_jlrejka w; r wfk. Hdk. H wjfnda. Ohla we; s lsr. Su Cont. . 37
6. The areas of possible partnerships should be identified, both in central and peripheral level. fldgialrejka ùu wj. YH wx. Y yÿkd. ek. Su 7. Address to the barriers for partnership. nd. Ol yÿkd. ek. Su 8. Capacity building and sharing of information in both sectors initially and provision of necessary assistance to the private sector for its development and participation. mqoa. , sl wx. Yfha iïm; a ixj. O_kh i|yd iydh o. Su 9. Formulation of coordinating committees in national and peripheral level. cd; sl iy m%dfoa. YSh kshdul lñgq msysgqùu 10. Formulation of legal frame works for partnerships. k. S; s iïmdokh lsr. Su 11. Operational research to evaluate the existing and identified areas of partnership. ióÌK u. ska l%shdldrlï we. eh. Su 38
Areas where public- private sector partnerships could be established rdc. H-mqoa. , sl iyfhda. S; djh we; s l<yels fldgia * Joint policy formulation bodies and coordinated implementation of national health strategies. cd; sl fi!LH m%; sm; a; Ska l%shd; aul lsr. Su * Supportive services, CleaningTransport Training Security Wmldrl fiajdjka ^msrsisÿ lsr. Su/ m%jdykh/ mqyq. Kqj/ wdrÌl fiajd& * Sharing of information f; dr; =re fnodyod. ek. Su * Coordinated curative activities. taldnoa. O m%; sldr fiajd * High tech laboratory & curative services wë; dla. Iksl ridhkd. dr iy m%; sldr fiajd * Long-term care o. S. _ ld, Sk m%; sldr * Community based care m%cd fi!LH fiajd * Rehabilitation mqkre; a: dmkh * Coordinated investments. taldnoa. O wdfhdackh * Training of human resource for private sector. mqoa. , sl wx. Yh i|yd udkj iïm; a ixj. O_kh * Quality assurance mechanism ; ; ajmd, k l%ufõo 39

40
Possible stakeholder reaction wfmaÌs; m%; spdr 1. Possible antagonism by trade unions j. D; Sh iñ; s úfrda. O; d 2. Political sensitivity foa. Ymd, k m%; spdr 3. Cooperation or resistance by health care managers fi!LH l<ukdlr. Kfha m%; sfrda. Ohka 4. Low Interest from private sector mqoa. , sl wx. Yfha Wodi. Sk nj 5. Possible resistance of private sector mqoa. , sl wx. Yfha m%; sfrda. Oh 6. Support from donor agencies m%; smdok imhkakkaf. a iyfhda. h 7. Resistance from the public uyck úfrda. O; d 41

THANK YOU 42
d3701ebcea95b7effad6c79bb463692b.ppt