3ef3d11900d2aee238c77333167f2776.ppt
- Количество слайдов: 31
Providing Comprehensive Faculty Development to Community-based Faculty Using Continuous Quality Improvement Joe Florence, M. D. Jim Shine, M. D. Bruce Bennard, Ph. D. Department of Family Medicine Quillen College of Medicine East Tennessee State University
Lecture-Discussion Presentation for: 33 rd Annual Predoctoral STFM Education Conference January 27, 2007 Memphis, TN
Session Objectives: • Describe Community Preceptor Advisory Group and faculty development program. • Describe Rural Primary Track Program taught by community faculty • Explain QI process as related to our faculty development program. • Provide first hand account of community physician “development” as faculty • Answer questions and solicit audience input
Faculty Development and the Community Preceptor Advisory Group • Community faculty play significant role in our Department • Role has increased over 10 years due to curricular change/expansion (RPCT) • Community-based faculty and preceptor involvement in programs increasingly varied
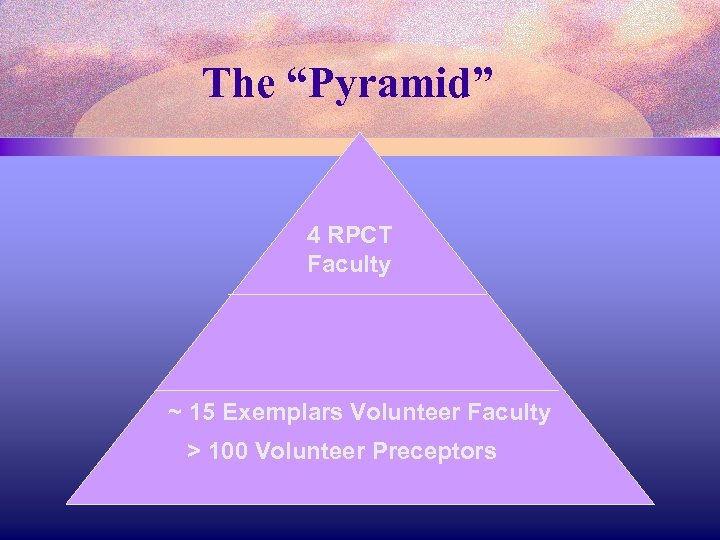
The “Pyramid” 4 RPCT Faculty ~ 15 Exemplars Volunteer Faculty > 100 Volunteer Preceptors
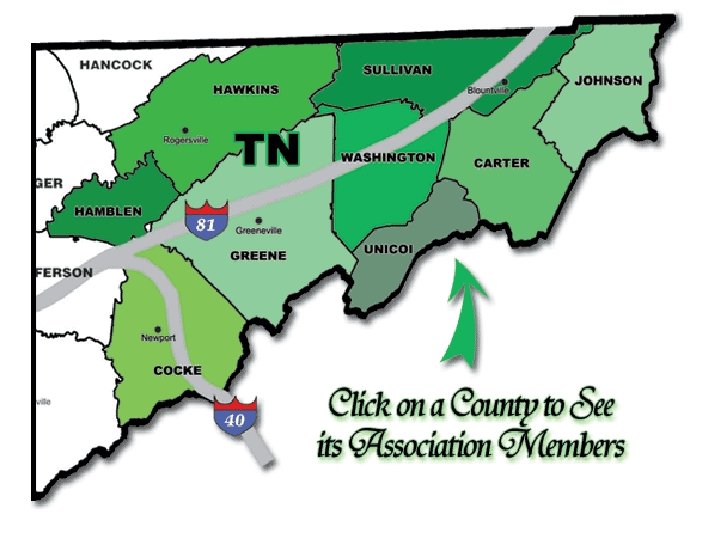
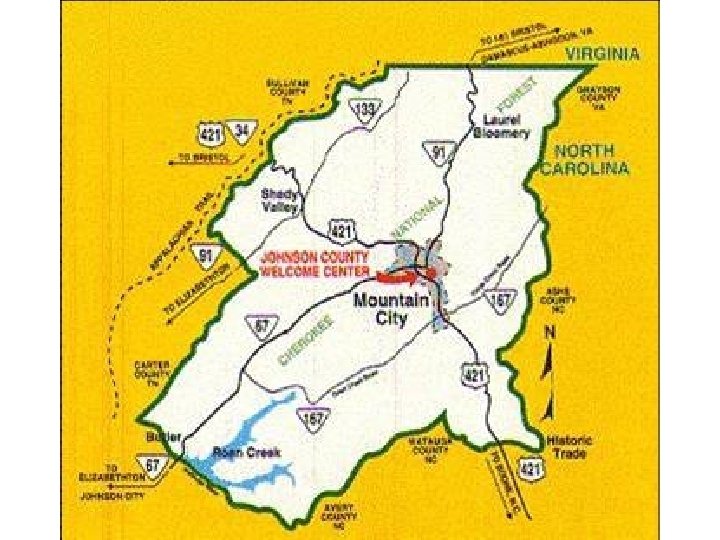
• RPCT Faculty - 2 each in Rogersville and Mountain City • EXEMPLARS - mostly rural based – they go beyond precepting – i. e. host health fairs, travel to campus for panels, special programs • PRECEPTORS – Tri-cities based, some rural, take students one week or less
Community Preceptor Advisory Group • RPCT and Exemplars • Meet with faculty-health professions leaders once a year (5 meetings to date) • Advise Department /COM on community-based education • Raise and respond to issues • “What’s new in medical school curriculum” • Involved in planning • Sessions deliberately informal/ under planned
• Dr. Bruce Bennard – established Advisory Group • Dr. Jim Shine – member of Advisory Group • Dr. Joe Florence – regular attendee of Advisory Group
ETSU Mission/ Institutional Purpose University pursues partnerships… … with emphasis on community-based and interdisciplinary education …special emphasis on addressing the needs of Southern Appalachia in the area of rural health care
The Quality Improvement Process The model has two parts: • Three fundamental questions, which can be addressed in any order • The Plan-Do-Study-Act (PDSA) cycle to test and implement changes in real work settings. The PDSA cycle guides the test of a change to determine if the change is an improvement
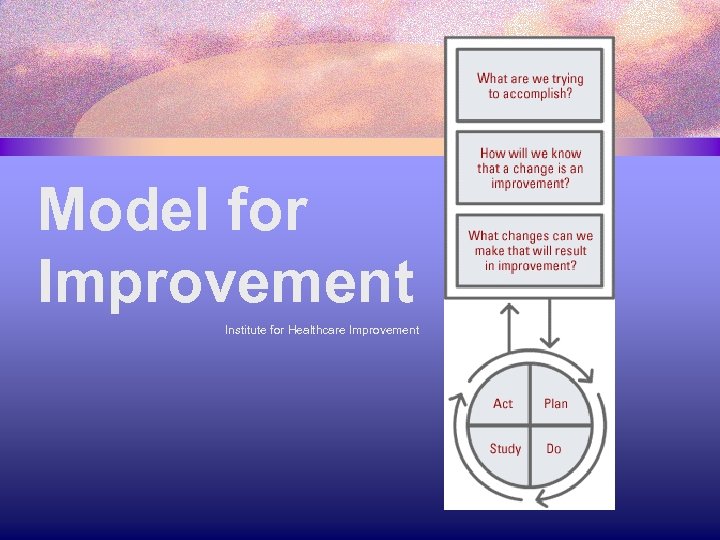
Model for Improvement Institute for Healthcare Improvement
Goals of Rural Primary Care Track at ETSU since 1992 • • Characteristics • A curricular experience that is efficient, consistent and adds value for health professions students • Oriented first to student learning • Continuously improving with new ideas, people and health issues Key elements • Community-based learning • Experiential learning • Interdisciplinary • Community partnerships
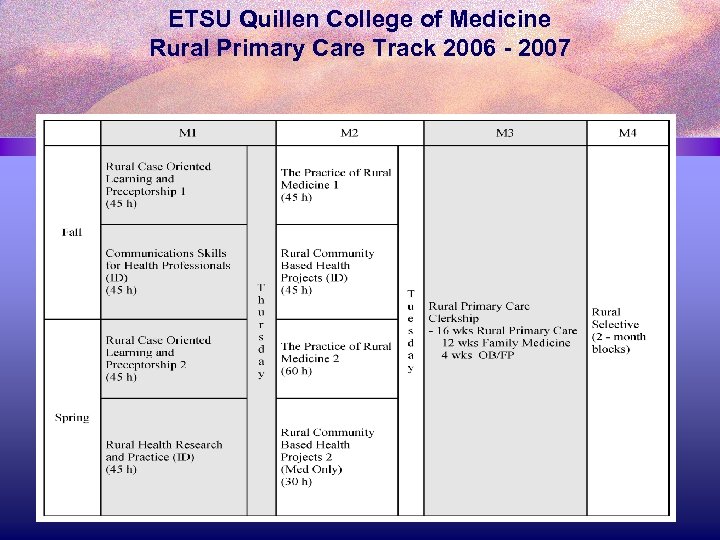
ETSU Quillen College of Medicine Rural Primary Care Track 2006 - 2007

Give – Get of Faculty Development Give Rural Faculty University Get • Time • Experience • Mentorship for students Relationships with faculty • Understanding of community needs and resources • New Knowledge • New Skills • Relationships • Identity with the university • Faculty • Consultants • Dollars (Grants) • Time • “All purpose” community faculty • Community faculty buy in • Representation in community
Typical Faculty Development Issues from the University’s Viewpoint • Pedagogy: • Case Oriented Learning (COL) • OSCE • Blackboard • Content • • • Community Diagnosis/ Assessment Community Based Participatory Research Evidence Based Medicine Medical Literature Data Bases and search techniques Care Model/ Quality Improvement IRB
Typical Faculty Development Issues from the Rural Faculty Viewpoint • Course Curriculum – What do you want me to teach? • Best Pedagogy for teaching • What are the Resources from campus • How do I get the university to address what is really needed? • Personal agenda – I want to know more about? ?
Role of the Rural Community-based Faculty • Crucial to success • Must establish a learning environment where students take more responsibility • for their own learning • and the learning of others • Ideally, the faculty uses facilitation skills as a coach
Attributes of Competent Faculty • Competence is a habit • Health care is a cooperative art; performance occurs in relationships; competence in relationships • Competence is developed along a continuum • Knowing the rules is not enough; values are important Adapted from “Residency Training and Systems Based Practice” (2004) David C. Leach, MD, Exec Director ACGME
Quality Improvement PDSA = People Doing Something Awesome!
Dr. Jim Shine’s Story • How I got to Mountain City • What am I doing there • What keeps me going






Remember Our Mission
3ef3d11900d2aee238c77333167f2776.ppt